Abstract
Acupuncture is widely accepted as a therapeutic option for managing depression. However, evidence from clinical trials remains controversial. This review aims to synthesize the best available evidence on the efficacy and safety of acupuncture in managing depression. The review was performed according to PRISMA (Preferred Reporting Items for Systematic Reviews and Meta‐Analysis) guidelines. Five databases and the relevant trial registries were searched from the inception to October 2021. Randomized clinical trials of acupuncture for managing depression, published in English, were selected for inclusion. The quality of included studies was assessed using the Cochrane risk of bias tool. Netmeta and dmetar of R packages were used to conduct a network meta‐analysis. Twenty‐two trials with 2391 participants were eligible and included in the analysis. This review found evidence that electroacupuncture (EA) plus antidepressant achieved superior outcomes compared with the waitlist (standardized mean difference = −8.86, 95% confidence interval: −14.78 to −2.93). The treatment ranking of different interventions in improving depression symptoms indicated that EA plus antidepressant with a probability of 0.8294, followed by manual acupuncture (MA) plus antidepressant (0.6470) and MA (0.5232). Acupuncture, either in isolation or as an adjunct to pharmacological treatment, has clinical benefits and can be considered a safe option for managing depression.
Keywords: acupuncture point, clinical trial, literature review, mental health, network meta‐analysis
1. INTRODUCTION
Depression usually features a low mood and or a loss of pleasure. This is often accompanied by somatic symptoms, psychomotor disturbance, insomnia, and cognitive symptoms; some people experience excessive guilt, hopelessness, and suicidal ideation (Williams & First, 2013). Depression is the leading cause of disease burden; more importantly, no reduction in global prevalence or burden has been detected since 1990 (Vos et al., 2020). Globally, an estimated 5.0% of adults suffer from depression (World Health Organization, 2021). One in ten Australians had depression or feelings of depression, an increase from 9% in 2014–2015 (Australian Bureau of Statistics, 2018). Depression is becoming increasingly common, especially during the COVID‐19 pandemic (Santomauro et al., 2021).
Pharmacological management is the first‐line treatment for depression (Malhi et al., 2020). Unfortunately, antidepressants have limitations and side effects, and 30%–60% of patients have nonresponse or partially respond to antidepressants (Bauer et al., 2013; De Carlo et al., 2016). A literature review has reported adverse events (AEs) for antidepressants, including nausea, dizziness, sedation, headache, insomnia, and sexual dysfunction (Maguire et al., 2021). The study has shown that antidepressants can cause damage to the nervous system, liver, and heart of patients and worsen suicidal ideation (Dobson et al., 2019).
Complementary and alternative medicine, such as acupuncture, are frequently used for people with depression (Hansen & Kristoffersen, 2016). Acupuncture is widely accepted in treating various health conditions (H. Wang et al., 2018). A study analyzing data collected between 2012 and 2013 in Australia found that 19.3% of young women and 16.8% of middle‐aged women who had acupuncture consultations had experienced depression within the previous 12 months (Yang et al., 2017). Acupuncture includes three main forms, namely manual acupuncture (MA), electroacupuncture (EA), and laser acupuncture (LA). MA involves stimulating acupuncture points with metallic needles manipulated by the hands to achieve therapeutic effects; EA is the application of the pulsed current through acupuncture needles, whereas LA uses a low‐level laser beam instead of an acupuncture needle to stimulate the acupoints. Acupuncture has been shown to affect the nervous system and provide advantages for treating depression (L. Lu et al., 2016; Shin et al., 2017). Like antidepressant medications, acupuncture can affect serotonin and noradrenaline neurotransmitter levels, along with adenylate cyclase cyclic adenosine monophosphate protein kinase A, cascading within the central nervous system (Leung et al., 2014).
A systematic review of high‐quality randomized controlled trials (RCTs) provides the best evidence on healthcare interventions. In recent decades, there has been an increasing number of RCTs and systematic reviews assessing the efficacy of acupuncture for depression. Some systematic reviews have detailed the beneficial effects of acupuncture in reducing the severity of depression and suggested it may be a suitable adjunct to usual care (UC) and standard antidepressant medication (Armor et al., 2019; Stub et al., 2011); while other studies have found insufficient evidence for the efficacy of acupuncture on depression compared with sham acupuncture (SA) or antidepressants (Fan et al., 2010; H. Wang et al., 2008); overall results have remained mixed and inconclusive (Leo & Ligot, 2007; Smith et al., 2018). Mental health is the priority for action in Australia's health sector. Therefore, this review aimed to assess acupuncture's efficacy and safety in managing depression by synthesizing high‐quality RCTs.
2. METHODS
2.1. Protocol and registration
This systematic review was reported following Preferred Reporting Items for Systematic Reviews and Meta‐Analysis (PRISMA) guidelines (Page et al., 2021). The review protocol was registered in the Prospective Register of Systematic Reviews (PROSPERO‐CRD42020168512) (https://www.crd.york.ac.uk/prospero/display_record.php?RecordID=168512).
2.2. Search strategy and study selection
We searched five English databases, namely, Allied and Complementary Medicine Database (AMED), Cochrane Central Register of Controlled Trials (CENTRAL), Excerpta Medica database (EMBASE), PubMed, and Web of Sciences. We also searched international trial registries via the World Health Organization International Clinical Trials Registry Platform (WHO ICTRP), the Australian New Zealand Clinical Trials Registry (anzctr.org.au), and the US National Library of Medicine database (ClinicalTrials.gov) to identify unpublished and ongoing studies. The above databases were searched from the inception to October 2021. Additional studies were identified from other sources to avoid publication bias, including the reference lists of all included studies and systematic reviews. We searched gray literature, including dissertations and theses, clinical guidelines, and reports from regulatory agencies. We included studies published in the English language only because studies conducted in China and published in English journals tend to show better reporting quality, as high‐quality English journals have the standard requirement of following a specific reporting guideline and framework (e.g., PRISMA and Consolidated Standards of Reporting Trials [CONSORT] guidelines). Chinese‐language publications tend to have overestimated effect sizes (T. Wang et al., 2017). According to the Cochrane review, there may be an association between more significant effect sizes and the high risk of bias (Rob) in these trials, especially performance bias and publication bias (Smith et al., 2018). Search strategies were developed using medical subject headings (MeSH) terms and keywords: acupuncture, acupuncture therapy, EA, LA, acupuncture point, acupoint, depression, depressive disorder, major depressive disorder, bipolar disorder, and dysthymic disorder. The search strategy was adapted to different database demands.
We included all relevant RCTs meeting the following criteria: (1) Participants of all genders and aged 18 years or older with a clinical diagnosis of depression were included. (2) Interventions included acupuncture alone or in combination with antidepressant medication; the types of acupuncture included MA, EA, and LA. (3) Eligible comparator groups were antidepressants, waitlist (WL), UC, SA, and placebo acupuncture (PA). (4) The outcome measures were the reduction in the severity of depression with validated tools.
Two reviewers (Chen and Luo) independently reviewed the titles and abstracts of studies searched from the database and then screened and excluded ineligible studies based on inclusion criteria. A PRISMA flowchart was used to record the selection process. A third independent reviewer (Wang) resolved disagreements and conflicting opinions.
2.3. Data extraction and quality assessment
Two reviewers (Chen and Luo) undertook the data extraction using predefined data extraction forms. For each study, the following data were extracted: author's name, year of publication, country, study design, types of depression, characteristics of participants, treatment regime, outcome measures, the time point of outcome assessment, and AEs. The reviewers of this study sought to contact the authors when research data records in the literature were missing or unclear.
Two reviewers (Chen and Luo) independently assessed study quality by using Version 2 of the Cochrane risk‐of‐bias tool for randomized trials (Rob2) (Sterne et al., 2019). The evaluation domains of Rob2 include “randomization process,” “deviations from intended interventions,” “missing outcome data,” “measurement of the outcome,” “selection of the reported result,” and “overall bias.” Judgment for each domain can be “high risk,” “some concerns,” or “low risk.”
2.4. Data synthesis and analysis
We undertook a statistical summary of the data and expressed the continuous data as standardized mean difference (SMD). The significance level was set to 0.05 with a confidence interval (CI). Cochrane's Q and I 2 statistics indicated the homogeneity of effects between studies (Higgins & Thompson, 2002), where I 2 greater than or equal to 50% indicated significant heterogeneity. When considerable heterogeneity occurred, random effects model was used; otherwise, a fixed effects model was used (Lu & Ades, 2006). The I 2 statistics in the head‐to‐head comparison meta‐analysis were assessed before the network meta‐analysis (NMA). An indirect treatment comparison meta‐analysis was performed using a frequentist method (Rücker, 2012). The network's consistency was assessed using a generalized Cochrane's Q test, where within‐the‐study and between‐study heterogeneity/inconsistency were evaluated and summarized to evaluate consistency (Krahn et al., 2013). Forest plots presented a summary and individual study effect sizes with a 95% CI. Publication bias was assessed through a visual examination of the funnel plots. A comparison‐adjusted funnel plot was used to detect small study effects as a signal of publication bias within our networks. The funnel plots' symmetry was assessed using Egger's asymmetry test (Egger et al., 1997). Funnel plots were analyzed only if at least 10 studies were included in the meta‐analyses. All analyses were performed using the “Netmeta” and “dmetar” packages of R software (Version 4.2.1) (Harrer et al., 2021).
3. RESULTS
3.1. Study selection
A total of 6455 studies were identified, of which 2263 were duplicates, and a subsequent 3887 studies were removed based on title and abstract screening. Two hundred and eighty‐five articles remained for full‐text assessment based on inclusion criteria, where 252 studies were further excluded due to: applications of study design other than RCT (n = 89), participants not meeting inclusion criteria (n = 29), outcomes not meeting inclusion criteria (n = 41), and publication in languages other than English (n = 34). Thirty‐three studies were included for quality assessment, and 11 studies were rated with a high Rob. Twenty‐two studies were retained and included for data synthesis (Figure 1).
Figure 1.
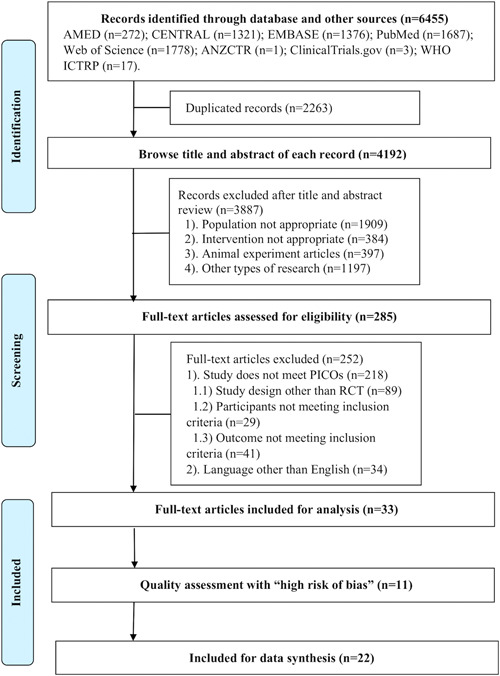
Flowchart of literature selection on randomized controlled trials of acupuncture for depression. AMED, Allied and Complementary Medicine Database; ANZCTR, Australian New Zealand Clinical Trials Registry; CENTRAL, Cochrane Central Register of Controlled Trials; EMBASE, Excerpta Medica database; WHO ICTRP, World Health Organization International Clinical Trials Registry Platform. [Color figure can be viewed at wileyonlinelibrary.com]
3.2. Characteristics of the included studies
A total of 22 studies with 2391 participants were included in this review. Table 1 outlines the characteristic of the included studies. Those studies were conducted in China (n = 13), Australia (n = 3), the USA (n = 3), the UK (n = 2), and Germany (n = 1). Thirteen of the 22 studies included two arms (intervention vs. control), while the remaining nine had three arms (intervention vs. control 1 and 2) (Allen et al., 1998, 2006; Chung et al., 2015; MacPherson et al., 2013; Ormsby et al., 2020; Qu et al., 2013; Röschke et al., 2000; Yeung et al., 2011; Zhao et al., 2019).
Table 1.
Characteristics of included randomized controlled trials on acupuncture for depression
| Author, year, country | Study designs | Diagnostic tools used | Type of depression | Characteristics of participants: M/F, mean age (SD) | Treatment regimen (acupoints, duration, frequency, intensity, and total session) | Outcome measures | Time‐point of outcome assessments | AEs |
|---|---|---|---|---|---|---|---|---|
| Ai, 2018, China |
2‐arm RCT (n = 100) I: MA + Paroxetine (n = 50) C: Paroxetine (n = 50) |
DSM‐5 | Depression (type NR) |
I: 22/28, 20.1 (3.6) C: 23/27, 20.2 (3.5) |
Points: Yin Guan, Guan Ren, Zhen Ren, Coronal Suture, Zygomaticotemporal Suture, Lambdoid Suture, adjunct acupoints based on syndrome differentiation Intensity: twirling manipulation 180–200 times/min, De qi feeling Duration: 50 min Frequency: 1/day Total session: 6 weeks, 42 sessions |
HAMD | Baseline, Week 1, Week 2, Week 4, Week 6. |
I: nausea(n = 1), dry mouth and dizziness (n = 1). C: nausea (n = 4), increased heart rate(n = 1), dry mouth and dizziness(n = 1). |
| Allen, 2006, USA |
3‐arm RCT (n = 151) I: MA (n = 50) C1: SA (n = 49) C2: WL (n = 52) |
DSM‐4 | MDD |
I: 16/33, 39.7 (9.9) C1: 17/33, 42.2 (10.6) C2: 15/37, 41.6 (12.5) |
Points: no details provided. The number of needles (rang 10–16) Duration: 20 min Frequency: 2/week for 4 weeks, followed by 1/week for 4 weeks Total: 8 weeks, 12 sessions |
HAMD, BDI | Baseline, Week 4, Week 8. Follow‐up at Week 12. |
I: pain (n = 5). C: NR by participants (n = 0). |
| Allen, 1998, USA |
3‐arm RCT (n = 34) I: MA (n = 12) C1: SA (n = 11) C2: WL (n = 11) |
DSM‐4, SCID | MDD |
I: 0/12, age NR C1: 0/11, age NR C2: 0/11, age NR |
Points: no details provided. Points selected according to the treatment manual Duration: 20 min Frequency: 2/week for 4 weeks, followed by 1/week for 4 weeks Total: 8 weeks, 12 sessions |
HAMD, BDI | Baseline, Week 8, follow‐up at Week 16. | NR. |
| Andreescu, 2011, USA |
2‐arm RCT (n = 53) I: EA (n = 28) C: SA (n = 25) |
DSM‐4, SCID | MDD |
I: 7/28, 46.0 (11.5) C: 8/25, 49.1 (14.0) |
Points: Baihui (GV20), Yintang (EX‐HN3) Duration: over 30 min Frequency: 2/week Intensity: electric stimulator 4. C connected current 3–5 mA had a frequency of 2 Hz. (Pantheon Research, USA) Total: 6 weeks, 12 sessions |
HAMD, | Baseline, Week 1, Week 2, Week 3, Week 4, Week 5, Week 6. Follow up at Week 8. | Side effects rating scale used. No serious adverse event. |
| Chung, 2015, China |
3‐arm RCT (n = 150) I: EA (n = 60) C1: minimal acupuncture (n = 60) C2: SA (n = 30) |
DSM‐4 | MDD |
I: 14/46, 48.8 (9.9) C1: 14/46, 50.9 (9.5) C2: 3/27, 47.4 (9.5) |
Points: Baihui (GV20), Ear Shenmen, Sishencong (EX‐HN1), Yintang (EX‐HN3), Anmian (EX‐HN22), Shenmen (HT7), Neiguan (PC6), Sanyinjiao (SP6) Duration: 30 min Frequency: 3/week Dosage: electric stimulator (ITO ES160, Japan) current 0.4 ms at a 4 Hz frequency Total: 3 weeks, nine sessions |
HAMD | Baseline, Week 4, follow up at Week 8. | 42.2% of the participants reported adverse events. No serious adverse events. |
| Duan, 2009, China |
2‐arm RCT (n = 95) I: EA + Fluoxetine (n = 48) C: Fluoxetine (n = 47) |
ICD‐10 | Depression (type NR) |
I: 17/31, 38 (10.17) C: 19/28, 37 (11.22) |
Points: Baihui (GV20), Yintang (EX‐HN3), selective points were chosen according to individual symptoms Duration: 30 min Frequency: 6/week Intensity: electric stimulator (G68052‐I, China) current 0.4‐ms at a 2 Hz frequency Total: 6 weeks, 36 sessions |
HAMD | Baseline, Week 1, Week 2, Week 3, Week 4, Week 5, Week 6. | TESS scores between groups show a significant difference in the 2nd, 4th, and 6th weeks of treatment. |
| Li, 2020, China |
2‐arm RCT (n = 60) I: EA + antidepressants (name NR) (n = 30) C: antidepressants (name NR) (n = 30) |
DSM‐4 | Depression (type NR) |
I: 11/19, 40.30 (10.99) C: 11/19, 38.75 (11.45) |
Points: Baihui (GV20), Shenting (GV24), Yintang (EX‐NH3), Shenmen (HT7), Neiguan (PC6), Zusanli (ST36), Sanyinjiao (SP6) Duration: 30 min Frequency: 3/week Intensity: electric stimulator (Han's stimulator, China) 10‐Hz of continuous waves for 8 weeks Total: 8 weeks, 24 sessions |
HAMD | Baseline, Week 4, Week 8. Follow up at Week 12. | NR. |
| Luo, 1998, China |
2‐arm RCT (n = 241) I: EA (n = 133) C: amitriptyline (n = 108) |
HAMD | Depression (type NR) | T: 109/132, 32 |
Points: Baihui (GV20), Yintang (EX‐HN3) Duration: 45 min Frequency: 6/week Intensity: electric stimulator (G6805) current 3–5 mA at 2 Hz Total: 6 weeks, 36 sessions |
HAMD | Baseline, Week 6. |
I: physical tiredness (n = 26), headache (n = 14), dizziness (n = 14). C: physical tiredness (n = 38), headache (n = 25), dizziness (n = 28). Side effects rating scale used. |
| MacPherson, 2013, UK |
3‐arm RCT (n = 775) I: MA (n = 302) C1: counseling (n = 302) C2: UC (n = 151) |
BDI‐II | Depression (type NR) |
I: 88/214, 43.4 (13.24) C1: 69/233, 43.5 (13.26) C2: 44/107, 43.5 (13.93) |
Points: 246 different points were used. Common points were Hegu (LI4), Taichong (LR3), Sanyinjiao (SP6), Zusanli (ST36) Duration: average 53 min (rang 28–95 min) Frequency: approximately 1/week Total: 3 months, 12 sessions |
PHQ‐9 |
Baseline, Week 12, follow up at Week 26, Week 39, and Week 52. |
I: n = 56. C1: n = 47. C2: n = 40. |
| Ormsby, 2020, Australia |
3‐arm RCT (n = 57) I: MA (n = 19) C1: muscle relaxation (n = 19) C2: UC (n = 19) |
EPDS | Antenatal depression |
I: 0/19, 28.95 (6.75) C1: 0/19, 27.37 (3.64) C2: 0/19, 29.95 (4.82) |
Points: 2 to 10 needles were gently inserted into “live” points Duration: 10‐15 min Frequency: 1/week Total: 8 weeks, eight sessions |
EPDS | Baseline, Week 4, Week 8. Follow up at Week 14. | NR by participants (n = 0). |
| Qu, 2013, China |
3‐arm RCT (n = 160) I1: MA + Paroxetine (n = 54) I2: EA + Paroxetine (n = 58) C: Paroxetine (n = 48) |
ICD‐10 | MDD |
I: 23/31, 32.3 (9.6) C1: 33/25, 33.2 (9.0) C2: 19/29, 34.4 (10.8) |
Points: Dazhui (GV14), Fengfu (GV16), Baihui (GV20), Yintang (EX‐HN3), Fengchi (GB20), Neiguan (PC6), Sanyinjiao (SP6) Duration: 30 min Frequency: 3/week Total: 6 weeks, 18 sessions |
HAMD, SDS | Baseline, Week 1, Week 2, Week 4, Week 6, follow up at Week 10. |
I1: physical tiredness (n = 28), headache (n = 11), sleep disturbance (n = 28). I2: physical tiredness (n = 27), headache (n = 5), sleep disturbance (n = 21). C: physical tiredness (n = 19), headache (n = 11), sleep disturbance (n = 18). |
| Quah‐Smith, 2013, Australia |
2‐arm RCT (n = 47) I: LA (n = 31) C: SA (n = 16) |
DSM‐4 | MDD |
I: 5/20, 40.08 (9.37) C: 11/14, 36.27 (10.13) |
Points: Shenmen (HT7), Taixi (KI3), Qimen (LR14), Ququan (LR8), Juque (CV14) Frequency: 2/week for the first 4 weeks, then 1/week Intensity: 100 mW low‐intensity infrared (808 nm) units, 5 J for five acupoints per session Total: 12 sessions |
HAMD | Baseline, Week 8. | AEs with mean scores > 0.50 were: LA group, transient fatigue (0.67); and PA group, aches (0.11), transient fatigue (1.0), and vagueness (0.52) |
| Quah‐Smith, 2005, Australia |
2‐arm RCT (n = 30) I: LA (n = 16) C: SA (n = 14) |
BDI | Depression (type NR) |
I: 3/13, 38.9 (9.0) C: 4/10, 38.1 (2.3) |
Points: Shenmen (HT7), Qimen (LR14), Ququan (LR8), Juque (CV14), Jiuwei (CV15), adjunctive points Baihui (DV20), Yingu (KI10), Hegu (LI4), Sanyinjiao (SP6) Duration: 30–40 s Frequency: 2/week for the first four weeks, then 1/week Intensity: the low‐level laser unit 100 mW (Meyer, Melbourne, Australia), 3–4 J per session Total: 8 weeks, 12 sessions |
HAMD, BDI | Baseline, Week 4, Week 8 Follow up at Week 12, Week 20. |
I: n = 4, C: n = 2. |
| Röschke, 2000, Germany |
2‐arm RCT (n = 70) I: MA + Mianserin (n = 22) C1: SA + Mianserin (n = 24) C2: Mianserin (n = 24) |
DSM‐4 | MDD |
I: 3/19, 49 (13) C1: 9/15, 47 (9) C2: 10/14, 49 (11) |
Points: Xinshu (BL15), Geshu (BL17), Ganshu (BL18), Shenmen (HT7), Neiguan (PC6), Shangqu (SP5), Sanyinjiao (SP6), Fenglong (ST40) Duration: 30 min Frequency: 3/week Total: 4 weeks, 12 sessions |
BRMS | Baseline, twice/week (Week 1–8). | NR. |
| Wang, 2018, China |
2‐arm RCT (n = 64) I: MA (n = 32) C: escitalopram (n = 32) |
CCMD‐3 | Post‐stroke Depression |
I: 20/12, 55.22 (5.82) C: 19/13, 57.28 (7.01) |
Points: Xinshu (BL15), Ganshu (BL18), Shenshu (BL23), Yamen (GV15), Baihui (GV20), Shenting (GV24), Shenmen (HT7), Taixi (KI3), Taichong (LR3), Neiguan (PC6), Danzhong (CV17) Duration: 30 min Frequency: 5/week Total: 8 weeks, 40 sessions. |
HAMD | Baseline, Week 4, Week 8. | NR. |
| Whiting, 2008, UK |
2‐arm RCT (n = 19) I: MA (n = 13) C: SA (n = 6) |
BDI, CIS‐R | Depression (type NR) |
I: 9/4, 39.9 (12.1) C: 5/1, 48.5 (10.2) |
Points: Baihui (GV20), Shuigou (GV26), Yintang (EX‐HN3), Neiguan (PC6), Sanyinjiao (SP6) Duration: 20 min Frequency: unclear Total: 12 sessions |
BDI | Baseline, at the end of treatment. |
I: pain (n = 1); symptoms worsening (n = 2). C: NR by participants (n = 0) |
| Yeung, 2011, China |
2‐arm RCT (n = 78) I: EA (n = 26) C1: minimal acupuncture (n = 26) C2: SA (n = 26) |
DSM‐4 | MDD |
I: 6/20, 47.5 (8.5) C1: 7/19, 46.7 (9.7) C2: 3/23, 50.1 (9.1) |
Points: Baihui (GV20), Yintang (EX‐HN3), Sishencong (EX‐HN1), Anmian (EX‐HN22), Ear Shenmen Duration: 30 min Frequency: 3/week Intensity: electric stimulator (CE‐FAR Acus II) constant current 0.45‐ms square wave at 4 Hz Total: 3 weeks, nine sessions |
HAMD |
Baseline, Week 4, follow up at Week 7. |
I: headache (n = 2), dizziness (n = 1). C1: insomnia (n = 1), hand numbness (n = 2), hematoma (n = 1), palpitation (n = 1), pain (n = 1). C2: headache (n = 2), dizziness (n = 2), hand numbness (n = 1). |
| Zhang, 2012, China |
2‐arm RCT (n = 70) I: EA + Fluoxetine (n = 34) C: SA + Fluoxetine (n = 36) |
DSM‐4 | MDD |
I: 1/33, 48.2 (9.8) C: 11/25, 46.3 (9.9) |
Points: Baihui (GV20), Sishencong (EX‐HN1), Yintang (EX‐HN3), Taiyang (EX‐HN5), Shuaigu (GB8), Toulinqi (GB15), Touwei (ST8) Duration: 30 min Frequency: 3/week Intensity: electric stimulator (Hwarto, SDZ‐II) 2 Hz and voltage (9 V) frequency Total: 3 weeks, nine sessions |
HAMD | Baseline, Week 1, Week 2, Week 3. |
I: uncomfortable (n = 7, 20.6%). C: uncomfortable (n = 14, 38.9%). |
| Zhang, 2009, China |
2‐arm RCT (n = 80) I: MA + Fluoxetine (n = 40) C: SA + Fluoxetine (n = 40) |
DSM‐4 | MDD |
I: 12/28, 36.2 (11.7) C: 15/25, 35.5 (12.0) |
Points: Baihui (GV20), Shuigou (GV26), Sishencong (EX‐HN1), Yintang (EX‐HN3), Shenmen (HT7), Hegu (LI4), Taichong (LR3), Neiguan (PC6) Duration: 30 min Frequency: 5/week Total: 6 weeks, 30 sessions |
HAMD | Baseline, Week 2, Week 4, Week 6. |
I: pain (n = 5), skin erythema (n = 1). C: pain (n = 1). |
| Zhang, 2007, China |
2‐arm RCT (n = 42) I: EA + Paroxetine (n = 22) C: Paroxetine (n = 20) |
CCMD‐3 | Depression (type NR) |
I: 10/12, 36.6 (9.7) C: 9/11, 37.1 (10.2) |
Points: Baihui (GV20), Yintang (EX‐HN3), adjunctive points: Shenmen (HT7), Hegu (LI4), Taichong (LR3), Taiyuan (LU9), Neiguan (PC6), Waiguan (TE5), Sanyinjiao (SP6), Zusanli (ST36), Fenglong (ST40), etc. Duration: 30 min Frequency: 6/week Intensity: electro stimulator (G6805), 2 Hz of frequency, sparse‐dense wave, 6 V of quantity Total: 6 weeks, 36 sessions. |
HAMD | Baseline, Week 1, Week 2, Week 4, Week 6 | AEs were nausea, dry mouth, headache, listlessness, and hidrosis. No action was taken. |
| Zhao, 2019, China |
2‐arm RCT (n = 477) I1: EA + SSRIs (n = 160) I2: MA + SSRIs (n = 161) C: SSRIs (n = 156) |
ICD‐10 | Depression (type NR) |
I1: 52/108, 41.18 (12.00) I2: 56/105, 41.42 (12.53) C: 57/99, 41.76 (12.85) |
Points: Baihui (GV20), Yintang (EX‐HN3), adjunctive points: Dazhui (GV14), Fengfu (GV16), Fengchi (GB20), Neiguan (PC6), Sanyinjiao (SP6) Duration: 30 min Frequency: 3/week Intensity: electro stimulator (LH‐202H) at 2/15 Hz Total: 6 weeks, 18 sessions |
HAMD, SDS | Baseline, Week 6. Follow up at Week 10 |
I1: n = 9. I2: n = 10. C: n = 9. Side effects rating scale used. |
| Yong, 2021, China |
2‐arm RCT (n = 145) I: MA (n = 73) C: UC (n = 72) |
CCMD‐3 | Post‐stroke Depression |
I: 35/38, 56.9 (10.5) C: 38/34, 57.6 (9.0) |
Points: Baihui (GV20), Zusanli (ST36), adjunctive points according to symptom Duration: 30 min Frequency: 2/day Total: 4 weeks, 56 sessions |
HAMD | Baseline, Week 4. | I: hematoma (n = 2). C: nausea and vomiting (n = 3). |
Abbreviations: AE, adverse event; BDI, Beck's depression inventory; BRMS, Bech‐Rafaelsen Melancholia Scale; CCMD‐3, Chinese classification of mental disorders; DSM‐5, diagnostic and statistical manual of mental disorders (5th Edition); EA, electroacupuncture; EPDS, Edinburgh Postnatal Depression Scale; HAMD, Hamilton Rating Scale for Depression; ICD‐10, International Statistical Classification of Diseases and Related Health Problem (10th Revision); LA, laser acupuncture; MA, manual acupuncture; NR, not reported; PHQ‐9, Patient Health Questionnaire‐9; SA, sham acupuncture; SCI‐R, clinical interview schedule‐revised; SCID, structured clinical interview for DSM‐IV; SDS, Self‐rating Depression Scale; SERS, Side Effect Rating Scale; SSRI, selective serotonin reuptake inhibitor; TESS, Treatment Emergent Symptoms Scale; UC, usual care; WL, waitlist.
For the interventions, treatment modalities included MA (n = 6) (Allen et al., 1998, 2006; MacPherson et al., 2013; Ormsby et al., 2020; Y. Wang et al., 2018; Whiting et al., 2008), EA (n = 4) (Andreescu et al., 2011; Chung et al., 2015; Luo et al., 1998; Yeung et al., 2011), LA (n = 2) (J. I. Quah‐Smith et al., 2005; I. Quah‐Smith et al., 2013), and the combination of acupuncture and antidepressants (n = 10) (Ai et al., 2018; Duan et al., 2009; Li et al., 2020; Qu et al., 2013; Röschke et al., 2000; G. Zhang et al., 2007, W.‐J. Zhang et al., 2009, Z. J. Zhang et al., 2012; Zhao et al., 2019; Yong et al., 2021).
For the comparators, control modalities include SA (n = 6) (Allen et al., 1998, 2006; Andreescu et al., 2011; Chung et al., 2015; Whiting et al., 2008; Yeung et al., 2011), PA (n = 2) (J. I. Quah‐Smith et al., 2005; I. Quah‐Smith et al., 2013), antidepressants (n = 9) (Ai et al., 2018; Duan et al., 2009; Li et al., 2020; Luo et al., 1998; Qu et al., 2013; Röschke et al., 2000; Y. Wang et al., 2018; G. Zhang et al., 2007; Zhao et al., 2019), SA combined with antidepressants (n = 3) (Röschke et al., 2000; W.‐J. Zhang et al., 2009, Z. J. Zhang et al., 2012), WL (n = 2) (Allen et al., 1998, 2006), and UC (n = 3) (MacPherson et al., 2013; Ormsby et al., 2020; Yong et al., 2021).
Outcome measurements used to assess depression included Hamilton Rating Scale for Depression (HAMD) (n = 14), Beck's Depression Inventory (BDI) (n = 2), both HAMD and Self‐Rating Depression Scale (SDS) (n = 3), Edinburgh Postnatal Depression Scale (EPDS) (n = 1), Patient Health Questionaire‐9 (PHQ‐9) (n = 1), and Bech‐Rafaelsen Melancholia Scale (BRMS) (n = 1).
Twelve studies reported follow‐up outcomes between 1 week and 9 months after the end of the intervention. The remaining studies did not report any follow‐up outcomes.
3.2.1. Treatment regimen of the included studies
Although 18 studies recorded acupoints in their treatment, four studies did not report the name of each acupoint but rather the number of acupoints used (Allen et al., 1998, 2006; MacPherson et al., 2013; Ormsby et al., 2020). The number of acupoints selected for each trial varied from 2 acupoints (Andreescu et al., 2011; Luo et al., 1998) to 246 acupoints (MacPherson et al., 2013), depending on the standardized or individualized acupuncture formula. The most frequently used acupoints were Baihui (GV20), Shenting (GV24), Yingtang (EX‐HN3), Hegu (LI4), Taichong (LR3), Sanyinjiao (SP6). Treatment sessions were reported between 8 sessions (Ormsby et al., 2020) and 56 sessions in total (Yong et al., 2021), with treatment frequency ranging from twice per day (Yong et. al., 2021) to once per week (Ormsby et al., 2020), and treatment duration from 3 weeks (Chung et al., 2015) to 3 months (He et al., 2012). Needle retention times ranged from 20 to 60 min. Eighteen studies reported 30 min duration for each session, while one mentioned an average time of 53 min (range 28–95 min) (MacPherson et al., 2013). The intervention parameter was partially reported for MA, where various frequencies and intensities of MA stimulation have been utilized in each study. For EA, the low frequency of the electro stimulator at 2–4 Hz was commonly used, whereas one study used a frequency of 10 Hz (Li et al., 2020).
3.3. Quality assessment
A summary of the Rob assessments for the 33 initially selected studies is shown in Figure 2. Seventeen studies had some concerns with the randomization process, mainly due to a lack of allocation concealment. Nearly half of the studies (15/33) had a low risk of deviations from intended interventions. Most studies had a low risk of missing outcome data. Two studies were classified as having some concerns with the measurement of the outcome, and seven studies were high risk. One study had a high risk with the selection of the reported result. Overall, eight studies had a low risk for all domains. Only 22 studies were included in this review after excluding 11 studies with a high Rob.
Figure 2.
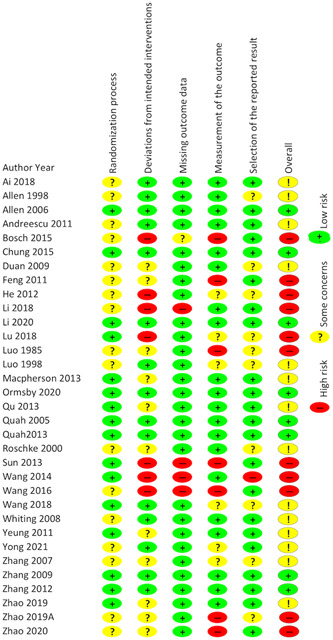
Quality assessment results included randomized controlled trials (a) risk of bias graph and (b) risk of bias summary. Green+, low risk; yellow?, some concerns; red−, high risk. [Color figure can be viewed at wileyonlinelibrary.com]
3.4. The efficacy of acupuncture for depression
The qualitative and quantitative analyses for outcome measures of 22 studies were categorized into three groups according to different modalities: (1) MA or plus antidepressant (n = 15), (2) EA or plus antidepressant (n = 10), and (3) LA (n = 2). Subgroups were established based on the intervention modalities recorded in the review protocol.
3.4.1. MA
MA versus UC (n = 3)
Three studies compared MA with UC (MacPherson et al., 2013; Ormsby et al., 2020; Yong et al., 2021), showing MA was superior to UC. One study demonstrated that the HAMD score was reduced in both groups but lower in the MA group (p < 0.05) (Yong et al., 2021). Another study showed statistically significant reduction in PHQ‐9 scores for the MA group at 3 months (MD = −2.26, 95% CI [−3.72, −1.21]) and over 12 months (MD = −1.55, 95% CI [−2.46, −0.70]) (MacPherson et al., 2013). The remaining study found lower EPDS scores in the MA group at the end of the intervention (MD = −5.84, 95% CI [−9.10, −2.58], p < 0.001) (Ormsby et al., 2020).
MA versus WL (n = 2)
Two studies compared MA with WL and showed that MA is superior to WL (Allen et al., 1998, 2006). Both studies demonstrated that the HAMD score was reduced in both groups but significantly lower in the MA group (p < 0.05).
MA versus SA (n = 3)
Three studies compared MA with SA (Allen et al., 1998, 2006; Whiting et al., 2008). Two studies showed MA was more effective than SA (Allen et al., 1998; Whiting et al., 2008), while the remaining study showed no difference between the two groups (Allen et al., 2006). One study revealed a significant reduction in both HAMD and BDI scores (p < 0.05) (Allen et al., 1998), while the other study found a substantial decline in BDI scores (Whiting et al., 2008). The remaining study found that the MA and SA groups did not differ in scores of HAMD (p > 0.2) and BDI (p > 0.17), showing no beneficial evidence of MA compared with SA (Allen et al., 2006).
MA versus antidepressant (n = 1)
One study compared MA with antidepressants and showed that MA was superior to antidepressants (Y. Wang et al., 2018). This study demonstrated that HAMD scores in the MA group were significantly lower than in the antidepressants group after 4 weeks of treatment (p < 0.05).
MA + antidepressant versus antidepressant (n = 4)
Four studies compared MA plus antidepressants with antidepressants alone (Ai et al., 2018; Qu et al., 2013; Röschke et al., 2000; Zhao et al., 2019), with all these indicating that MA plus antidepressants could significantly reduce depressive symptoms compared with antidepressants alone. Two studies found a statistically significant difference in HAMD scores between two groups at various measuring points during the 6‐week intervention (p < 0.05). Accordingly, the authors concluded that MA plus antidepressants could reduce the symptom of depression with a quicker response and greater therapeutic efficacy than antidepressants alone (Ai et al., 2018). Similarly, another study found that MA plus antidepressants were significantly better than antidepressants alone in HAMD scores at 6‐week treatment (RR = 1.21, 95% CI [1.04, 1.42], p = 0.013) (Zhao et al., 2019). A study measuring HAMD and SDS scores found that MA plus antidepressants could significantly reduce depression compared to antidepressants only. MA plus antidepressants outperformed antidepressants by 28.1% in clinical response (Qu et al., 2013). The remaining study, which measured BRMS, found that MA plus antidepressants improved slightly more than antidepressants alone; however, the MA plus antidepressants group showed significant benefit during the second half of the study (Röschke et al., 2000).
MA + antidepressant versus SA + antidepressant (n = 2)
Two studies compared MA with SA as an add‐on to antidepressants and showed no statistical difference between the two groups (Röschke et al., 2000; W.‐J. Zhang et al., 2009). One study demonstrated better improvement in the side effects of antidepressants between the two groups (z = 23.60, p < 0.001). In contrast, no statistical significance in response rates (80.0% for the MA group and 77.5% for the SA group) or HAMD score change (z = 1.80, p = 0.07) (W.‐J. Zhang et al., 2009).
3.4.2. EA
EA versus SA (n = 3)
Three studies compared EA with SA and found no difference between EA and SA (Andreescu et al., 2011; Chung et al., 2015; Yeung et al., 2011). A study found that the absolute HAMD mean (SD) score decreased with −6.6 (5.9) in the EA group and −7.6 (6.6) in the SA group, corresponding to a 37.5% and 41.3% relative decrease from baseline, respectively. The author concluded that both groups were equally well tolerated and showed similar absolute and relative improvement in depressive symptoms (Andreescu et al., 2011). HAMD total scores of the remaining studies were not significantly different between the two groups, although a significant reduction in depressive symptoms was observed (Yeung et al., 2011).
EA versus antidepressant (n = 1)
One study compared EA with antidepressants and showed no difference between the two groups (Luo et al., 1998). The result indicated that the therapeutic efficacy of EA was equal to that of antidepressants for depressive disorders (p > 0.05) (Luo et al., 1998).
EA + antidepressant versus antidepressant (n = 5)
Five studies compared EA plus antidepressants (Duan et al., 2009; Li et al., 2020; Qu et al., 2013; G. Zhang et al., 2007; Zhao et al., 2019), where four studies showed EA plus antidepressants to be superior to antidepressants alone (Li et al., 2020; Qu et al., 2013; G. Zhang et al., 2007; Zhao et al., 2019). In contrast, the remaining study showed no difference between the two groups (Duan et al., 2009). One study demonstrated that EA plus antidepressants was significantly better than antidepressants at Week 6 on HAMD response rate (relative risk [RR] = 1.27, 95% CI [1.09, 1.48], p = 0.014) and showed beneficial effects and were well tolerated (Zhao et al., 2019). Similarly, three studies found EA plus antidepressants to significantly reduce HAMD at most measuring points compared with antidepressants alone (all p < 0.05). The authors concluded that EA plus antidepressants had better clinical effectiveness than antidepressants alone, as EA could accelerate clinical responses to antidepressants (Li et al., 2020; Qu et al., 2013; G. Zhang et al., 2007). In contrast, one study identified a total effective rate of 78.26% in the EA plus antidepressants group and 77.27% in the antidepressants group, showing no statistical difference (p > 0.05) (Duan et al., 2009).
EA + antidepressant versus SA + antidepressant (n = 1)
A study that compared EA with SA as an add‐o showed EA to be a safe and effective intervention that augments antidepressant efficacy (Duan et al., 2009). The EA plus antidepressants group displayed a significant reduction from baseline in HAMD and SDS scores compared with the SA plus antidepressants group; the response rate was 19.4% versus 8.8%, respectively.
3.4.3. LA
LA versus PA (n = 2)
Two studies compared LA with PA (J. I. Quah‐Smith et al., 2005; I. Quah‐Smith et al., 2013), showing LA to have a clinically and statistically significant benefit compared with PA. One study showed greater improvement in the laser group on HAMD scores (mean 9.28, SD 6.55) compared with the PA group (mean 14.14, SD 4.78, p < 0.001). Response rates were 72.0% and 18.2% (p < 0.001), remission rates were 56.0% and 4.5% (p < 0.001) at 8 weeks of intervention (I. Quah‐Smith et al., 2013). Another study found that immediately posttreatment, BDI scores fell from baseline by 16.1 points in the LA group and by 6.8 points in the PA group (p < 0.001) (J. I. Quah‐Smith et al., 2005).
3.4.4. Meta‐analysis
Due to different acupuncture interventions, comparators, and outcome measurement tools, it was challenging to run a meta‐analysis for the included 22 studies. However, 20 studies measured the reduction of the severity of depression at the end of treatment. Therefore, we conducted a head‐to‐head comparison meta‐analysis of these studies into five groups. The meta‐analysis result of the selected outcome indicated a high heterogeneity (I 2 = 91%, p < 0.01) (Figure 3). When analyzed together in meta‐analysis with random effects modeling, overall, there was a statistical difference between the intervention and control group (SMD = −0.53, 95% CI [−0.95, −0.10], p < 0.01).
Figure 3.
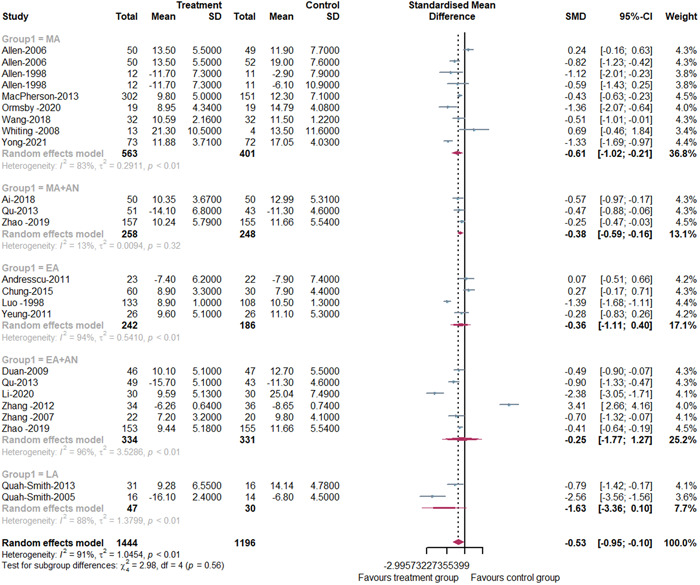
Forest plot of comparison for the severity of depression at the end of treatment. AN, antidepressant; EA, electroacupuncture; LA, laser acupuncture, MA, manual acupuncture. [Color figure can be viewed at wileyonlinelibrary.com]
3.4.5. NMA
The network plot was presented in Figure 4; 11 interventions were involved: antidepressant, EA, LA, MA, PA, SA, WL, UC, EA plus antidepressant, MA plus antidepressant, and SA plus antidepressants. The intervention with the most randomized participants was identified as EA plus antidepressant, antidepressant, and MA plus antidepressant. There were five disconnected interventions: EA, LA, PA, SA plus antidepressant, and UC, and these disconnected interventions could not be compared with the rest of the network. Therefore, these five disconnected interventions were not compared in the main NMA.
Figure 4.
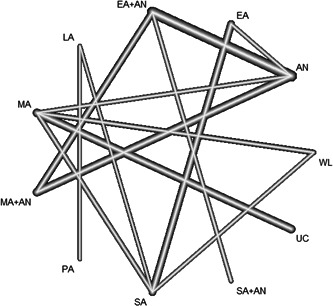
Network plot (node represents individual interventions and nodes connected by edges indicate that these two interventions have previously been compared directly in a study. The edges are weighted by the number of studies evaluating this treatment comparison. AN, antidepressant; EA, electroacupuncture; LA, laser acupuncture; MA, manual acupuncture; PA, placebo acupuncture; SA, sham acupuncture; UC, usual care; WL, waitlist.
The results of the NMA of different interventions are displayed in Table 2. For the combined intervention, the result of the NMA indicated that EA plus antidepressant was more effective compared with antidepressant and WL (SMD = −4.98, 95% CI: −7.24 to −2.71; SMD = −8.86, 95% CI: −14.78 to −2.93), but showed no beneficial evidence for SA (SMD = −4.03, 95% CI: −8.82 to 0.75). As for MA plus antidepressant, it seemed to be more beneficial as compared with antidepressant and WL (SMD = −2.85, 95% CI: −5.60 to −0.10; SMD = −6.73, 95% CI: −12.86 to −0.61), while not superior to SA (SMD = −1.91, 95% CI: −6.94 to 3.12). For acupuncture alone, MA was better than WL in reducing depression symptoms (SMD = −5.28, 95% CI: −9.70 to −0.85); however, there were no significant differences when compared with antidepressant and SA (SMD = −1.39, 95% CI: −5.33 to 2.54; SMD = −0.45, 95% CI: −4.10 to 3.20). Among all the interventions with the main NMA, EA plus antidepressant seemed to achieve superior outcomes compared with WL (SMD = −8.86, 95% CI: −14.78 to −2.93) (Figure 5).
Table 2.
Result of network meta‐analysis for treatment effects
| AN | 1.13 (−2.77, 5.03) | 4.98 (2.71, 7.24) | 5.80 (−1.29, 12.90) | 1.39 (−2.54, 5.33) | 2.85 (0.10, 5.60) |
|---|---|---|---|---|---|
| −1.13 (−5.03, 2.77) | EA | 3.85 (−0.66, 8.36) | 4.67 (−1.74, 11.09) | 0.26 (−3.86, 4.39) | 1.72 (−3.05, 6.50) |
| − 4.98 ( − 7.24, − 2.71) | −3.85 (−8.36, 0.66) | EA + AN | 0.83 (−6.62, 8.28) | −3.58 (−8.12, 0.96) | −2.12 (−5.12, 0.87) |
| −5.80 (−12.90, 1.29) | −4.67 (−11.09, 1.74) | −0.83 (−8.28, 6.62) | LA | −4.41 (−11.18, 2.37) | −2.95 (−10.56, 4.66) |
| −1.39 (−5.33, 2.54) | −0.26 (−4.39, 3.86) | 3.58 (−0.96, 8.12) | 4.41 (−2.37, 11.18) | MA | 1.46 (− 3.34, 6.26) |
| − 2.85 ( − 5.60, − 0.10) | −1.72 (−6.50, 3.05) | 2.12 (−0.87, 5.12) | 2.95 (−4.66, 10.56) | −1.46 (−6.26, 3.34) | MA + AN |
| 3.50 (−5.40, 12.39) | 4.63 (−3.74, 12.99) | 8.47 (−0.70, 17.65) | 9.30 (3.94, 14.66) | 4.89 (−3.75, 13.53) | 6.35 (−2.96, 15.66) |
| −0.94 (−5.16,3.27) | 0.19 (−2.75, 3.12) | 4.03 (−0.75, 8.82) | 4.86 (−0.85, 10.57) | 0.45 (−3.20, 4.10) | 1.91 (−3.12, 6.94) |
| − 7.37 ( − 12.56, − 2.17) | −6.24 (−12.74, 0.26) | −2.39 (−7.07, 2.29) | −1.56 (−10.36, 7.23) | −5.97 (−12.49, 0.55) | −4.51 (−10.07, 1.04) |
| 3.02 (−1.86,7.90) | 4.15 (−0.89, 9.18) | 7.99 (2.62, 13.37) | 8.8 2 (1.46, 16.18) | 4.41 (1.53, 7.30) | 5.87 (0.27, 11.47) |
| 3.88 (−1.59, 9.36) | 5.01 (−0.15, 10.17) | 8.86 (2.93, 14.78) | 9.69 (2.39, 16.98) | 5.28 (0.85, 9.70) | 6.37 (0.61, 12.86) |
| AN | −3.50 (−12.39, 5.40) | 0.94 (−3.27, 5.16) | 7.37 (2.17, 12.56) | −3.02 (−7.90, 1.86) | −3.88 (−9.36, 1.59) |
|---|---|---|---|---|---|
| −1.13 (−5.03, 2.77) | −4.63 (−12.99, 3.74) | −0.19 (−3.12, 2.75) | 6.24 (−0.26, 12.74) | −4.15 (−9.18, −0.89) | −5.01 (−10.17, 0.15) |
| − 4.98 ( − 7.24, − 2.71) | −8.47 (−17.65, 0.70) | −4.03 (−8.82, 0.75) | 2.39 (−2.29, 7.07) | − 7.99 ( − 13.37, −2.62) | − 8.86 ( − 14.78, − 2.93) |
| −5.80 (−12.90, 1.29) | − 9.30 ( − 14.66, − 3.94) | −4.86 (−10.57, 0.85) | 1.56 (−7.23, 10.36) | − 8.82 ( − 16.18, − 1.46) | − 9.69 (−16.98, −2.39) |
| −1.39 (−5.33, 2.54) | −4.89 (−13.53, 3.75) | −0.45 (−4.10, 3.20) | 5.97 (−0.55, 12.49) | − 4.41 ( − 7.30, − 1.53) | − 5.28 (−9.70, − 0.85) |
| − 2.85 ( − 5.60, − 0.10) | −6.35 (−15.66, 2.96) | −1.91 (−6.94, 3.12) | 4.51 (−1.04, 10.07) | − 5.87 ( − 11.47, − 0.27) | − 6.73 (−12.86, −0.61 |
| 3.50 (−5.40, 12.39) | PA | 4.44 (−3.39, 12.27) | 10.86 (0.56, 21.16) | 0.48 (−8.63, 9.59) | −0.39 (−9.44, 8.67) |
| −0.94 (−5.16,3.27) | −4.44 (−12.27, 3.39) | SA | 6.42 (−0.27, 13.11) | −3.69 (−8.61, 0.69) | − 4.83 (−9.37, − 0.28) |
| − 7.37 ( − 12.56, − 2.17) | − 10.86 ( − 21.16, − 0.56) | −6.42 (−13.11, 0.27) | SA + AN | − 10.38 ( − 17.51, − 3.26) | − 11.25 ( − 18.80, − 3.70 |
| 3.02 (−1.86,7.90) | −0.48 (−9.59, 8.63) | 3.96 (−0.69, 8.61) | 10.8 (3.26, 17.51) | UC | −0.87 (−6.15, 4.42 |
| 3.88 (−1.59, 9.36) | 0.39 (−8.67, 9.44) | 4.83 (0.28, 9.37) | 11.25 (3.70, 18.80) | 0.87 (−4.42, 6.15) | WL |
Note: The estimates of SMD of treatment in the columns versus rows are presented in the upper diagonal elements (while those of the row treatment vs. column treatment are shown in the lower diagonal elements). The significant results are in bold and underscored.
Abbreviations: AN, antidepressant; EA, electroacupuncture; LA, laser acupuncture; MA, manual acupuncture; PA, placebo acupuncture; SA, sham acupuncture; UC, usual care; WL, waitlist.
Figure 5.
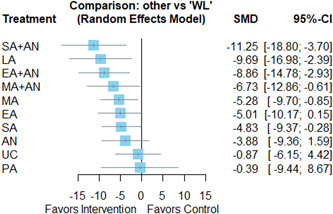
Forest plot of the estimates of standardized mean difference between each treatment and the reference group, waitlist. AN, antidepressant; EA, electroacupuncture; LA, laser acupuncture; MA, manual acupuncture; PA, placebo acupuncture, SA, sham acupuncture; UC, usual care. [Color figure can be viewed at wileyonlinelibrary.com]
Consistency between indirect and direct evidence was tested by comparing the results of pairwise comparisons in the net splitting analysis. The within‐design heterogeneity is highly significant (Q = 75.37, p < 0.0001). The between‐design inconsistency is insignificant (Q = 7.93, p = 0.0942), indicating good coherence between direct and indirect comparisons. The treatment ranking of different interventions in improving depression symptoms indicated that EA plus antidepressant has the highest p‐score (0.8294), followed by MA plus antidepressant (0.6470) and MA (0.5232), indicating that these treatment forms may be beneficial (Table 3).
Table 3.
Ranking probability of different interventions
| Rank | p‐score |
|---|---|
| SA + AN | 0.9300 |
| LA | 0.8432 |
| EA + AN | 0.8294 |
| MA + AN | 0.6470 |
| MA | 0.5232 |
| EA | 0.4887 |
| SA | 0.4681 |
| AN | 0.3522 |
| PA | 0.1764 |
| UC | 0.1415 |
| WL | 0.1004 |
Abbreviations: AN, antidepressant; EA, electroacupuncture; LA, laser acupuncture; MA, manual acupuncture; PA, placebo acupuncture; SA, sham acupuncture; UC, usual care; WL, waitlist.
3.5. AEs of acupuncture
A total of 18 out of the 22 studies reported AEs. Four studies described the measures for assessing the side effects, including Treatment Emergent Symptoms Scale (n = 1) (Duan et al., 2009) and Side Effect Rating Scale (n = 3) (Andreescu et al., 2011; Luo et al., 1998; Zhao et al., 2019). The specific AEs reported from nine studies included headaches, dizziness, fatigue, hematoma, and nausea. Three studies said participants withdrew due to AEs associated with acupuncture. However, these reactions were mild, and all recovered without further action.
3.6. Analysis of publication bias
The comparison‐adjusted funnel plot indicated no significant publication bias and this result was corroborated by Egger's test, which did not show significant differences (p = 0.8977) (Figure 6). In addition, the comparison‐adjusted funnel plot indicated an absence of small‐study effects (Figure 6).
Figure 6.
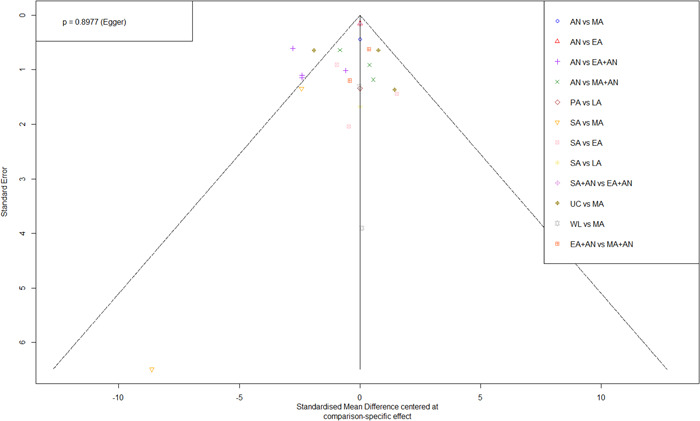
Comparison‐adjusted funnel plot of the publication bias) (Different colors represent different comparisons). AN, antidepressant; EA, electroacupuncture; LA, laser acupuncture; MA, manual acupuncture; PA, placebo acupuncture; SA, sham acupuncture; UC, usual care, WL, waitlist. [Color figure can be viewed at wileyonlinelibrary.com]
4. DISCUSSION
4.1. Main findings
Our review includes 22 trials with 2391 participants. The finding demonstrated that acupuncture could reduce the severity of depression, which is consistent with the Cochrane review (Smith et al., 2018). The main NMA showed that the combination of acupuncture and antidepressant achieved better efficacy when compared with antidepressants alone and WL. The estimated ranking probabilities indicated that the top three interventions are EA plus antidepressant, MA plus antidepressant, and MA. Our review reveals that acupuncture alone or combined with antidepressants shows no beneficial evidence when compared with SA. Other studies have suggested that SA is associated with more significant treatment effects than other physical placebos (Linde et al., 2010; Lund et al., 2009). The high clinical effectiveness of SA can be caused by stimulating the body's natural physiological response, such as pain‐relieving and anti‐inflammatory chemistry (Chen et al., 2014; McDonald et al., 2015), physiological alteration of blood circulation, and neural pathway (Le Bars et al., 1992). Given these reasons, using SA may underestimate acupuncture's treatment effect (Kaptchuk et al., 2010). In addition, sham‐controlled trials have significant clinical heterogeneity related to the diversity of controls, such as invasive or noninvasive SA. Acupuncture critics have used these findings to argue against the use of acupuncture and even against the need for acupuncture research (MacLennan & Morrison, 2012). Therefore, sham‐controlled trials may not be the best way to answer questions concerning the therapeutic effect of acupuncture until there is more physiological evidence of acupuncture (Birch et al., 2016; Langevin et al., 2011).
Our review reveals that studies conducted in China involve an average of 33 treatment sessions compared with studies conducted in Western countries that provide an average of 12 treatment sessions. The clinically relevant total number of treatments between studies undertaken in China and Western countries requires further interpretation, as treatment dosage can impact the treatment effect (White et al., 2008). Reviews found higher effectiveness rates observed when a higher treatment dosage was used, for example, higher treatment frequency (Liu et al., 2015) and more treatment sessions (Linde et al., 2016). Our findings are consistent with the Cochrane review, in which many studies administered inadequate treatment dosages (Smith et al., 2018). Also, participants from different cultural backgrounds in China and Western countries can affect the treatment effect in the clinical trial, such as participants' expectations for acupuncture can modify the treatment effect (Linde et al., 2007; Mao et al., 2010) and prior expectation toward acupuncture influence patient enrollment and retention (Cao et al., 2020).
Although several studies have emphasized the importance of using EA on acupoints Baihui (GV20) and Yintang (EX‐HN3) for treating depression, this review found that the treatment regimen of each study was different. The inability to standardize a treatment regimen in acupuncture‐related clinical trials is understandable, considering that the development of acupuncture has taken place in different countries for over 2000 years, while controlled clinical trials on acupuncture only started in the 1970s in Western countries (Bauer et al., 2020). The idea of “standardizing” is against the essence of the “individualized” approach, which is the guiding principle of traditional acupuncture treatment. The heterogeneity of acupuncture treatment regimens has been described as “the most formidable issue confronting systematic research” (Leo & Ligot, 2007). Therefore, a lack of knowledge about the appropriate acupuncture treatment regimen limits the value of systematic review, increases heterogeneity, and leads to unreliable review conclusions (Bauer et al., 2020).
Our review found that the AEs are usually mild, including headaches, dizziness, fatigue, and nausea, where recovery can occur without further action. However, even mild AEs can affect intervention uptake (Smith et al., 2018). Our review suggests acupuncture is well tolerated and has a low rate of AEs when performed by a trained practitioner. We also found that AEs were poorly reported, which is in line with a previous review. Future studies should focus more on reporting AEs (C. C. Wang et al., 2019).
4.2. Strength and limitation
This review has included the latest 22 RCTs published to October 2021, employing the quality assessment tool (Rob2) and providing updated evidence on using acupuncture to manage depression. Overall, the quality of evidence for most comparisons is moderate to high. During the quality assessment process, the high Rob is most frequently detected in the domain of deviation from intended interventions and measurement of the outcome, related to the blinding of participants, people delivering the interventions, and outcome assessors. The lack of blinding may increase the nonspecific effect in the intervention group and result in overestimating the effect size. Also, A high risk is associated with larger effect sizes. Most high Rob studies are conducted in China, which can explain the more significant effect of studies conducted in China (Armour et al., 2019). We subsequently excluded 11 studies deemed high Rob to ensure quality. The review is registered with PROSPERO, which provides another level of quality control. In addition, we have employed an NMA approach, a more appropriate technique to analyze the multiple comparisons for all interventions. We have only included trials published in English to ensure research and reporting quality; however, this could be a limitation as the results may not necessarily represent RCTs published in other languages. The lack of long‐term follow‐up in most included studies (10/22 did not report follow‐up outcomes) is another limitation, as there is insufficient evidence to determine if the benefits are sustained with the posttrial follow‐up.
4.3. Implication for future research and practice
Research needs to focus on the appropriate control design because of the unique feature of acupuncture. It is encouraged that future clinical trials should include both UC (to test the effectiveness of acupuncture) and an appropriate control group designed to test the efficacy of specific treatment components (e.g., adequacy of dosage and different treatment regimens). Research into what constitutes an adequate dosage has long been neglected, and a dose‐finding endeavor before establishing a clinical trial is highly recommended. The standards for reporting interventions in clinical trials of acupuncture (STRICTA) guidelines added to the CONSORT statement should be recommended to report the dosage of the trials transparently.
Our findings provided updated evidence in line with the current American College of Physicians clinical practice guideline suggesting acupuncture as a potential monotherapy and combination therapy with antidepressants in treating patients with MDD (Qaseem et al., 2016). We hope that our study can aid in filling the existing gap between research findings and clinical practice. However, the optimal types of acupuncture and ideal dosage when managing depression remain unanswered. Our study's evidence was insufficient to answer this question due to variations in the severity of depression, types of antidepressants, and comparators. In addition, policymakers' lack of cost‐effectiveness analysis represents a significant limitation of evidence‐based practice. Future research in these fields is warranted.
5. CONCLUSION
Acupuncture, either in isolation or as an adjunction to pharmacological treatment, has clinical benefits and could be considered a safe option for managing depression if qualified practitioners perform the intervention. More well‐designed higher‐quality studies are required, which need careful consideration of the control group, treatment dosage, blinding, and follow‐up. The registration of the review protocol before conducting a review should be a mandatory requirement for journal submission.
AUTHOR CONTRIBUTIONS
Binglei Chen: conceptualization; data curation; formal analysis; investigation; methodology; software; visualization; writing‐original draft; writing‐review and amp; editing. Carol Chunfeng Wang: conceptualization; data curation; investigation; methodology; supervision; validation; writing‐review and amp; editing. Khui Hung Lee: data curation; formal analysis; investigation; software; supervision; visualization; writing‐review and amp; editing. Jianhong Cecilia Xia: formal analysis; investigation; software; supervision; visualization; writing‐review and amp; editing. Zongting Luo: data curation; resources; validation; visualization; writing‐review and amp; editing. All authors contributed to this study.
CONFLICT OF INTEREST
The authors declare no conflict of interest.
PEER REVIEW
The peer review history for this article is available at https://publons.com/publon/10.1002/nur.22284
ACKNOWLEDGMENT
The project is supported by the Edith Cowan University and Industry Collaboration Scholarship (G1005429). Open access publishing facilitated by Edith Cowan University, as part of the Wiley ‐ Edith Cowan University agreement via the Council of Australian University Librarians.
Chen, B. , Wang, C. C. , Lee, K. H. , Xia, J. C. , & Luo, Z. (2023). Efficacy and safety of acupuncture for depression: A systematic review and meta‐analysis. Research in Nursing & Health, 46, 48–67. 10.1002/nur.22284
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available on request from the corresponding author. The data are not publicly available due to privacy or ethical restrictions.
REFERENCES
- Ai, C. , Wang, Q. , Wang, X. , Wang, Y. , Chen, S. , & Chen, X. (2018). Therapeutic observation of cranial suture acupuncture in treating depression. Journal of Acupuncture and Tuina Science, 16(3), 161–166. 10.1007/s11726-018-1043-1 [DOI] [Google Scholar]
- Allen, J. J. B. , Schnyer, R. N. , Chambers, A. S. , Hitt, S. K. , Moreno, F. A. , & Manber, R. (2006). Acupuncture for depression: A randomized controlled trial. The Journal of Clinical Psychiatry, 67(11), 1665–1673. 10.4088/jcp.v67n1101 [DOI] [PubMed] [Google Scholar]
- Allen, J. J. B. , Schnyer, R. N. , & Hitt, S. K. (1998). The efficacy of acupuncture in the treatment of major depression in women. Psychological Science, 9(5), 397–401. 10.1111/1467-9280.00074 [DOI] [Google Scholar]
- Andreescu, C. , Glick, R. M. , Emeremni, C. A. , Houck, P. R. , & Mulsant, B. H. (2011). Acupuncture for the treatment of major depressive disorder: A randomized controlled trial. The Journal of Clinical Psychiatry, 72(8), 1129–1135. 10.4088/JCP.10m06105 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Armour, M. , Smith, C. , Wang, L.‐Q. , Naidoo, D. , Yang, G.‐Y. , MacPherson, H. , Lee, M. , & Hay, P. (2019). Acupuncture for depression: A systematic review and meta‐analysis. Journal of Clinical Medicine, 8(8), 1140. 10.3390/jcm8081140 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Australian Bureau of Statistics . (2018). Mental Health, 2017–2018 financial year. Retrieved from https://www.abs.gov.au/statistics/health/mental-health/mental-health/latest-release
- Bauer, M. , McDonald, J. L. , & Saunders, N. (2020). Is acupuncture dose dependent? Ramifications of acupuncture treatment dose within clinical practice and trials. Integrative Medicine Research, 9(1), 21–27. 10.1016/j.imr.2020.01.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bauer, M. , Pfennig, A. , Severus, E. , Whybrow, P. C. , Angst, J. , & Möller, H.‐J. (2013). World Federation of Societies of Biological Psychiatry (WFSBP) guidelines for biological treatment of unipolar depressive disorders, part 1: Update 2013 on the acute and continuation treatment of unipolar depressive disorders. The World Journal of Biological Psychiatry, 14(5), 334–385. 10.3109/15622975.2013.804195 [DOI] [PubMed] [Google Scholar]
- Birch, S. , Alraek, T. , Kim, K. H. , & Lee, M. S. (2016). Placebo‐controlled trials in acupuncture: Problems and solutions. In: Leung S., & Hu H. (eds), Evidence‐based research methods for Chinese medicine (pp. 55–64). Springer. 10.1007/978-981-10-2290-6_4 [DOI] [Google Scholar]
- Cao, H.‐J. , Li, X. , Li, X.‐L. , Ward, L. , Xie, Z.‐G. , Hu, H. , Zhang, Y.‐J. , & Liu, J.‐P. (2020). Factors influencing participant compliance in acupuncture trials: An in‐depth interview study. PLoS One, 15(4), e0231780. 10.1371/journal.pone.0231780 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen, S. , Wang, S. , Rong, P. , Wang, J. , Qiao, L. , Feng, X. , Liu, J. , & Zhang, J. (2014). Acupuncture for visceral pain: Neural substrates and potential mechanisms. Evidence‐Based Complementary and Alternative Medicine, 2014, 609594. 10.1155/2014/609594 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chung, K.‐F. , Yeung, W.‐F. , Yu, Y.‐M. , Yung, K.‐P. , Zhang, S.‐P. , Zhang, Z.‐J. , Wong, M.‐T. , Lee, W.‐K. , & Chan, L.‐W. (2015). Acupuncture for residual insomnia associated with major depressive disorder: A placebo‐ and sham‐controlled, subject‐ and assessor‐blind, randomized trial. The Journal of Clinical Psychiatry, 76(6), e752–e760. 10.4088/JCP.14m09124 [DOI] [PubMed] [Google Scholar]
- De Carlo, V. , Calati, R. , & Serretti, A. (2016). Socio‐demographic and clinical predictors of non‐response/non‐remission in treatment resistant depressed patients: A systematic review. Psychiatry Research, 240, 421–430. 10.1016/j.psychres.2016.04.034 [DOI] [PubMed] [Google Scholar]
- Dobson, E. T. , Bloch, M. H. , & Strawn, J. R. (2019). Efficacy and tolerability of pharmacotherapy for pediatric anxiety disorders: A network meta‐analysis. The Journal of Clinical Psychiatry, 80(1), 14375. 10.4088/JCP.17r12064 [DOI] [PubMed] [Google Scholar]
- Duan, D. , Tu, Y. , Chen, L. , & Wu, Z. (2009). Efficacy evaluation for depression with somatic symptoms treated by electroacupuncture combined with fluoxetine. Journal of Traditional Chinese Medicine, 29(3), 167–173. 10.1016/s0254-6272(09)60057-1 [DOI] [PubMed] [Google Scholar]
- Egger, M. , Smith, G. D. , Schneider, M. , & Minder, C. (1997). Bias in meta‐analysis detected by a simple, graphical test. BMJ, 315(7109), 629–634. 10.1136/bmj.315.7109.629 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fan, L. , Fu, W. , Xu, N. , Liu, J. , Ou, A. , & Wang, Y. (2010). Meta‐analysis of 20 clinical, randomized, controlled trials of acupuncture for depression. Neural Regeneration Research, 5(24), 1862–1869. 10.3969/j.issn.1673-5374.2010.24.004 [DOI] [Google Scholar]
- Hansen, A. H. , & Kristoffersen, A. E. (2016). The use of CAM providers and psychiatric outpatient services in people with anxiety/depression: A cross‐sectional survey. BMC Complementary and Alternative Medicine, 16(1), 461. 10.1186/s12906-016-1446-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harrer, M. , Cuijpers, P. , Furukawa, T. A. , & Ebert, D. D. (2021). Doing meta‐analysis with R: A hands‐on guide. CRC Press. 10.1201/9781003107347 [DOI] [Google Scholar]
- He, Y. , Wu, Y. , Ouyang, M. , Li, G. , Li, H. , & Xie, H. E. (2012). Efficacy observation of depression in nicotine withdrawal treated with acupuncture. World Journal of Acupuncture ‐ Moxibustion, 22(1), 13–16. 10.1016/S1003-5257(12)60003-8 [DOI] [Google Scholar]
- Higgins, J. P. T. , & Thompson, S. G. (2002). Quantifying heterogeneity in a meta‐analysis. Statistics in Medicine, 21(11), 1539–1558. 10.1002/sim.1186 [DOI] [PubMed] [Google Scholar]
- Kaptchuk, T. J. , Chen, K. , & Song, J. (2010). Recent clinical trials of acupuncture in the West: Responses from the practitioners. Chinese Journal of Integrative Medicine, 16(3), 197–203. 10.1007/s11655-010-0197-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krahn, U. , Binder, H. , & König, J. (2013). A graphical tool for locating inconsistency in network meta‐analyses. BMC Medical Research Methodology, 13(1), 35. 10.1186/1471-2288-13-35 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Langevin, H. M. , Wayne, P. M. , MacPherson, H. , Schnyer, R. , Milley, R. M. , Napadow, V. , Lao, L. , Park, J. , Harris, R. E. , Cohen, M. , Sherman, K. J. , Haramati, A. , & Hammerschlag, R. (2011). Paradoxes in acupuncture research: Strategies for moving forward. Evidence‐Based Complementary and Alternative Medicine, 2011, 180805. 10.1155/2011/180805 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Le Bars, D. , Villanueva, L. , Bouhassira, D. , & Willer, J. C. (1992). Diffuse noxious inhibitory controls (DNIC) in animals and in man. Patologicheskaia Fiziologiia i Eksperimental'naia Terapiia, 4, 55–65. [PubMed] [Google Scholar]
- Leo, R. J. , & Ligot, J. S. A., Jr. (2007). A systematic review of randomized controlled trials of acupuncture in the treatment of depression. Journal of Affective Disorders, 97(1–3), 13–22. 10.1016/j.jad.2006.06.012 [DOI] [PubMed] [Google Scholar]
- Leung, M. C. P. , Yip, K. K. , Ho, Y. S. , Siu, F. K. W. , Li, W. C. , & Garner, B. (2014). Mechanisms underlying the effect of acupuncture on cognitive improvement: A systematic review of animal studies. Journal of Neuroimmune Pharmacology, 9(4), 492–507. 10.1007/s11481-014-9550-4 [DOI] [PubMed] [Google Scholar]
- Li, W. , Sun, M. , Yin, X. , Lao, L. , Kuang, Z. , & Xu, S. (2020). The effect of acupuncture on depression and its correlation with metabolic alterations: A randomized controlled trial. Medicine, 99(43), e22752. 10.1097/MD.0000000000022752 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Linde, K. , Allais, G. , Brinkhaus, B. , Fei, Y. , Mehring, M. , Vertosick, E. A. , Vickers, A. , & White, A. R. (2016). Acupuncture for the prevention of episodic migraine. The Cochrane Database of Systematic Reviews, 2016(6), CD001218. 10.1002/14651858.CD001218.pub3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Linde, K. , Niemann, K. , & Meissner, K. (2010). Are sham acupuncture interventions more effective than (other) placebos? A re‐analysis of data from the Cochrane review on placebo effects. Complementary Medicine Research, 17(5), 259–264. 10.1159/000320374 [DOI] [PubMed] [Google Scholar]
- Linde, K. , Witt, C. M. , Streng, A. , Weidenhammer, W. , Wagenpfeil, S. , Brinkhaus, B. , Willich, S. N. , & Melchart, D. (2007). The impact of patient expectations on outcomes in four randomized controlled trials of acupuncture in patients with chronic pain. Pain, 128(3), 264–271. 10.1016/j.pain.2006.12.006 [DOI] [PubMed] [Google Scholar]
- Liu, W.‐H. , Hao, Y. , Han, Y.‐J. , Wang, X.‐H. , Li, C. , & Liu, W.‐N. (2015). Analysis and thoughts about the negative results of international clinical trials on acupuncture. Evidence‐Based Complementary and Alternative Medicine, 2015, 671242. 10.1155/2015/671242 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lu, G. , & Ades, A. E. (2006). Assessing evidence inconsistency in mixed treatment comparisons. Journal of the American Statistical Association, 101(474), 447–459. 10.1198/016214505000001302 [DOI] [Google Scholar]
- Lu, L. , Zhang, X.‐G. , Zhong, L. L. , Chen, Z.‐X. , Li, Y. , Zheng, G.‐Q. , & Bian, Z.‐X. (2016). Acupuncture for neurogenesis in experimental ischemic stroke: A systematic review and meta‐analysis. Scientific Reports, 6(1), 1–16. 10.1038/srep19521 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lund, I. , Näslund, J. , & Lundeberg, T. (2009). Minimal acupuncture is not a valid placebo control in randomised controlled trials of acupuncture: A physiologist's perspective. Chinese Medicine, 4(1), 1–9. 10.1186/1749-8546-4-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luo, H. , Meng, F. , Jia, Y. , & Zhao, X. (1998). Clinical research on the therapeutic effect of the electro‐acupuncture treatment in patients with depression. Psychiatry and Clinical Neurosciences, 52, S338–S340. 10.1111/j.1440-1819.1998.tb03262.x [DOI] [PubMed] [Google Scholar]
- MacLennan, A. H. , & Morrison, R. G. B. (2012). Tertiary education institutions should not offer pseudoscientific medical courses. Medical Journal of Australia, 196(4), 225–226. 10.5694/mja12.10128 [DOI] [PubMed] [Google Scholar]
- MacPherson, H. , Richmond, S. , Bland, M. , Brealey, S. , Gabe, R. , Hopton, A. , Keding, A. , Lansdown, H. , Perren, S. , Sculpher, M. , Spackman, E. , Torgerson, D. , & Watt, I. (2013). Acupuncture and counselling for depression in primary care: A randomised controlled trial. PLoS Medicine, 10(9), e1001518. 10.1371/journal.pmed.1001518 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maguire, M. J. , Marson, A. G. , & Nevitt, S. J. (2021). Antidepressants for people with epilepsy and depression. Cochrane Database of Systematic Reviews, 4(4), CD010682. 10.1002/14651858.CD010682.pub [DOI] [PMC free article] [PubMed] [Google Scholar]
- Malhi, G. S. , Bell, E. , Singh, A. B. , Bassett, D. , Berk, M. , Boyce, P. , Bryant, R. , Gitlin, M. , Hamilton, A. , Hazell, P. , Hopwood, M. , Lyndon, B. , McIntyre, R. S. , Morris, G. , Mulder, R. , Porter, R. , Yatham, L. N. , Young, A. , & Murray, G. (2020). The 2020 Royal Australian and New Zealand College of Psychiatrists clinical practice guidelines for mood disorders: Major depression summary. Bipolar Disorders, 22(8), 788–804. 10.1111/bdi.13035 [DOI] [PubMed] [Google Scholar]
- Mao, J. J. , Xie, S. X. , & Bowman, M. A. (2010). Uncovering the expectancy effect: The validation of the Acupuncture Expectancy Scale. Alternative Therapies in Health and Medicine, 16(6), 22–27. [PMC free article] [PubMed] [Google Scholar]
- McDonald, J. L. , Cripps, A. W. , & Smith, P. K. (2015). Mediators, receptors, and signalling pathways in the anti‐inflammatory and antihyperalgesic effects of acupuncture. Evidence‐Based Complementary and Alternative Medicine, 2015, 975632. 10.1155/2015/975632 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ormsby, S. M. , Smith, C. A. , Dahlen, H. G. , & Hay, P. J. (2020). The feasibility of acupuncture as an adjunct intervention for antenatal depression: a pragmatic randomised controlled trial. Journal of Affective Disorders, 275, 82–93. 10.1016/j.jad.2020.05.089 [DOI] [PubMed] [Google Scholar]
- Page, M. J. , McKenzie, J. E. , Bossuyt, P. M. , Boutron, I. , Hoffmann, T. C. , Mulrow, C. D. , Shamseer, L. , Tetzlaff, J. M. , Akl, E. A. , Brennan, S. E. , Chou, R. , Glanville, J. , Grimshaw, J. M. , Hróbjartsson, A. , Lalu, M. M. , Li, T. , Loder, E. W. , Mayo‐Wilson, E. , McDonald, S. , … Moher, D. (2021). The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. International Journal of Surgery, 88, 105906. 10.1186/s13643-021-01626-4 [DOI] [PubMed] [Google Scholar]
- Qaseem, A. , Barry, M. J. , & Kansagara, D. (2016). Nonpharmacologic versus pharmacologic treatment of adult patients with major depressive disorder: A clinical practice guideline from the American College of Physicians. Annals of Internal Medicine, 164(5), 350–359. 10.7326/M15-2570 [DOI] [PubMed] [Google Scholar]
- Qu, S.‐S. , Huang, Y. , Zhang, Z.‐J. , Chen, J.‐Q. , Lin, R.‐Y. , Wang, C.‐Q. , Li, G.‐L. , Wong, H. K. , Zhao, C.‐H. , Pan, J.‐Y. , Guo, S.‐C. , & Zhang, Y.‐C. (2013). A 6‐week randomized controlled trial with 4‐week follow‐up of acupuncture combined with paroxetine in patients with major depressive disorder. Journal of Psychiatric Research, 47(6), 726–732. 10.1016/j.jpsychires.2013.02.004 [DOI] [PubMed] [Google Scholar]
- Quah‐Smith, I. , Smith, C. , Crawford, J. D. , & Russell, J. (2013). Laser acupuncture for depression: A randomised double blind controlled trial using low intensity laser intervention. Journal of Affective Disorders, 148(2–3), 179–187. 10.1016/j.jad.2012.11.058 [DOI] [PubMed] [Google Scholar]
- Quah‐Smith, J. I. , Tang, W. M. , & Russell, J. (2005). Laser acupuncture for mild to moderate depression in a primary care setting—A randomised controlled trial. Acupuncture in Medicine, 23(3), 103–111. 10.1136/aim.23.3.103 [DOI] [PubMed] [Google Scholar]
- Röschke, J. , Wolf, C. , Müller, M. J. , Wagner, P. , Mann, K. , Grözinger, M. , & Bech, S. (2000). The benefit from whole body acupuncture in major depression. Journal of Affective Disorders, 57(1–3), 73–81. 10.1016/s0165-0327(99)00061-0 [DOI] [PubMed] [Google Scholar]
- Rücker, G. (2012). Network meta‐analysis, electrical networks and graph theory. Research Synthesis Methods, 3(4), 312–324. 10.1002/jrsm.1058 [DOI] [PubMed] [Google Scholar]
- Santomauro, D. F. , Mantilla Herrera, A. M. , Shadid, J. , Zheng, P. , Ashbaugh, C. , Pigott, D. M. , Abbafati, C. , Adolph, C. , Amlag, J. O. , Aravkin, A. Y. , Bang‐Jensen, B. L. , Bertolacci, G. J. , Bloom, S. S. , Castellano, R. , Castro, E. , Chakrabarti, S. , Chattopadhyay, J. , Cogen, R. M. , Collins, J. K. , … Ferrari, A. J. (2021). Global prevalence and burden of depressive and anxiety disorders in 204 countries and territories in 2020 due to the COVID‐19 pandemic. The Lancet, 398(10312), 1700–1712. 10.1016/S0140-6736(21)02143-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shin, H. K. , Lee, S.‐W. , & Choi, B. T. (2017). Modulation of neurogenesis via neurotrophic factors in acupuncture treatments for neurological diseases. Biochemical Pharmacology, 141, 132–142. 10.1016/j.bcp.2017.04.029 [DOI] [PubMed] [Google Scholar]
- Smith, C. A. , Armour, M. , Lee, M. S. , Wang, L. Q. , & Hay, P. J. (2018). Acupuncture for depression. Cochrane Database of Systematic Reviews, 2018(3), CD004046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sterne, J. , Savović, J. , Page, M. J. , Elbers, R. G. , Blencowe, N. S. , Boutron, I. , Cates, C. J. , Cheng, H.‐Y. , Corbett, M. S. , Eldridge, S. M. , Emberson, J. R. , Hernán, M. A. , Hopewell, S. , Hróbjartsson, A. , Junqueira, D. R. , Jüni, P. , Kirkham, J. J. , Lasserson, T. , Li, T. , … Higgins, J. (2019). RoB 2: A revised tool for assessing risk of bias in randomised trials. BMJ, 366, 4898. 10.1136/bmj.l4898 [DOI] [PubMed] [Google Scholar]
- Stub, T. , Alræk, T. , & Liu, J. (2011). Acupuncture treatment for depression—A systematic review and meta‐analysis. European Journal of Integrative Medicine, 3(4), e259–e270. 10.1016/j.eujim.2011.09.003 [DOI] [Google Scholar]
- Vos, T. , Lim, S. S. , Abbafati, C. , Abbas, K. M. , Abbasi, M. , Abbasifard, M. , Abbasi‐Kangevari, M. , Abbastabar, H. , Abd‐Allah, F. , Abdelalim, A. , Abdollahi, M. , Abdollahpour, I. , Abolhassani, H. , Aboyans, V. , Abrams, E. M. , Abreu, L. G. , Abrigo, M. R. M. , Abu‐Raddad, L. J. , Abushouk, A. I. , … Bhutta, Z. A. (2020). Global burden of 369 diseases and injuries in 204 countries and territories, 1990–2019: A systematic analysis for the Global Burden of Disease Study 2019. The Lancet, 396(10258), 1204–1222. 10.1016/S0140-6736(20)30925-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang, C. C. , Tan, J.‐Y. , & Williams, A. (2019). Safety and side effects of acupuncture therapy in Australia: A systematic review. European Journal of Integrative Medicine, 27, 81–89. 10.1016/j.eujim.2019.03.004 [DOI] [Google Scholar]
- Wang, H. , Qi, H. , Wang, B. , Cui, Y. , Zhu, L. , Rong, Z. , & Chen, H. (2008). Is acupuncture beneficial in depression: A meta‐analysis of 8 randomized controlled trials? Journal of Affective Disorders, 111(2‐3), 125–134. 10.1016/j.jad.2008.04.020 [DOI] [PubMed] [Google Scholar]
- Wang, H. , Yang, G. , Wang, S. , Zheng, X. , Zhang, W. , & Li, Y. (2018). The most commonly treated acupuncture indications in the United States: A cross‐sectional study. The American Journal of Chinese Medicine, 46(07), 1387–1419. 10.1142/S0192415X18500738 [DOI] [PubMed] [Google Scholar]
- Wang, T. , Xu, C. , Pan, K. , & Xiong, H. (2017). Acupuncture and moxibustion for chronic fatigue syndrome in traditional Chinese medicine: A systematic review and meta‐analysis. BMC Complementary and Alternative Medicine, 17(1), 163. 10.1186/s12906-017-1647-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang, Y. , Han, Y. , Hu, Y. , & Zhang, L. (2018). Evaluation of the curative effect of acupuncture manipulation of regulating governor vessel and unblocking brain on the patients with post stroke depression associated with anxiety. World Journal of Acupuncture‐Moxibustion, 28(1), 4–9. 10.1016/j.wjam.2018.03.009 [DOI] [Google Scholar]
- White, A. , Cummings, M. , Barlas, P. , Cardini, F. , Filshie, J. , Foster, N. E. , Lundeberg, T. , Stener‐Victorin, E. , & Witt, C. (2008). Defining an adequate dose of acupuncture using a neurophysiological approach—A narrative review of the literature. Acupuncture in Medicine, 26(2), 111–120. 10.1136/aim.26.2.111 [DOI] [PubMed] [Google Scholar]
- Whiting, M. , Leavey, G. , Scammell, A. , Au, S. , & King, M. (2008). Using acupuncture to treat depression: A feasibility study. Complementary Therapies in Medicine, 16(2), 87–91. 10.1016/j.ctim.2007.07.005 [DOI] [PubMed] [Google Scholar]
- Williams, J. B. , & First, M. (2013). Diagnostic and statistical manual of mental disorders. Encyclopedia of Social Work. 10.1093/acrefore/9780199975839.013.104 [DOI] [Google Scholar]
- World Health Organization . (2021). Depression. Accessed September 13, 2021. Retrieved from: https://www.who.int/news-room/fact-sheets/detail/depression
- Yang, L. , Adams, J. , & Sibbritt, D. (2017). Prevalence and factors associated with the use of acupuncture and Chinese medicine: Results of a nationally representative survey of 17161 Australian women. Acupuncture in Medicine, 35(3), 189–199. 10.1136/acupmed-2016-011179 [DOI] [PubMed] [Google Scholar]
- Yeung, W.‐F. , Chung, K.‐F. , Tso, K.‐C. , Zhang, S.‐P. , Zhang, Z.‐J. , & Ho, L.‐M. (2011). Electroacupuncture for residual insomnia associated with major depressive disorder: A randomized controlled trial. Sleep, 34(6), 807–815. 10.5665/SLEEP.1056 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yong, Z. , Xin‐Hui, H. , & Pan, L. (2021). Efficacy observation of Zhi Shen Tiao Sui acupuncture method for depression after ischemic stroke. Journal of Acupuncture and Tuina Science, 19(3), 180–186. 10.1007/s11726-021-1244-x [DOI] [Google Scholar]
- Zhang, G. , Shi, Z. , Liu, S. , Gong, S. , Liu, J. , & Liu, J. (2007). Clinical observation on treatment of depression by electro‐acupuncture combined with Paroxetine. Chinese Journal of Integrative Medicine, 13(3), 228–230. 10.1007/s11655-007-0228-0 [DOI] [PubMed] [Google Scholar]
- Zhang, W.‐J. , Yang, X.‐B. , & Zhong, B.‐L. (2009). Combination of acupuncture and fluoxetine for depression: A randomized, double‐blind, sham‐controlled trial. The Journal of Alternative and Complementary Medicine, 15(8), 837–844. 10.1089/acm.2008.0607 [DOI] [PubMed] [Google Scholar]
- Zhang, Z. J. , Ng, R. , Man, S. C. , Li, T. Y. , Wong, W. , Tan, Q. R. , Wong, H. K. , Chung, K. F. , Wong, M. T. , Tsang, W. K. , Yip, K. C. , Ziea, E. , & Wong, V. T. (2012). Dense cranial electroacupuncture stimulation for major depressive disorder—A single‐blind, randomized, controlled study. PLoS One, 7(1), e29651. 10.1371/journal.pone.0029651 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhao, B. , Li, Z. , Wang, Y. , Ma, X. , Wang, X. , Wang, X. , Liu, J. , Huang, Y. , Zhang, J. , Li, L. , Hu, X. , Jiang, J. , Qu, S. , Chai, Q. , Song, M. , Yang, X. , Bao, T. , & Fei, Y. (2019). Manual or electroacupuncture as an add‐on therapy to SSRIs for depression: A randomized controlled trial. Journal of Psychiatric Research, 114, 24–33. 10.1016/j.jpsychires.2019.04.005 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data that support the findings of this study are available on request from the corresponding author. The data are not publicly available due to privacy or ethical restrictions.


