Abstract
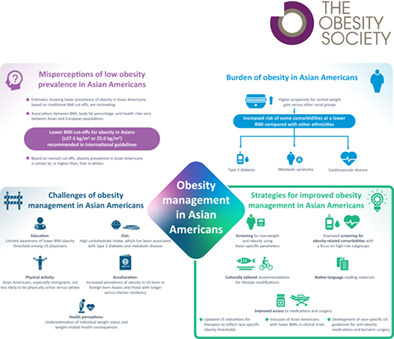
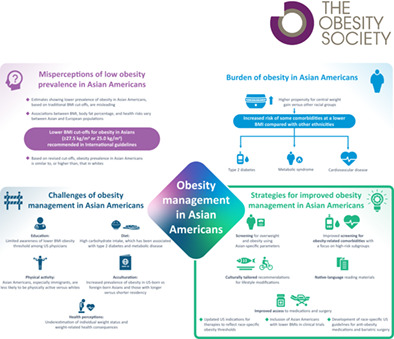
Standard measures of obesity, i.e., body weight and BMI, suggest that Asian American people have a lower obesity prevalence than other racial groups in the United States. However, Asian American people face a unique challenge in their pattern of adiposity with central obesity, which raises the risk for multiple comorbidities, such as type 2 diabetes, metabolic syndrome, and cardiovascular disease, at a lower BMI compared with other populations. Several organizations recommend lower BMI cutoffs for obesity in Asian people (BMI ≥25.0 or ≥27.5 kg/m2) instead of the standard ≥30.0 kg/m2 threshold. The risks of obesity and related comorbidities in this population are further influenced by diet, physical activity, perceptions of health, and access to information and therapies. Asian‐specific parameters for assessing obesity should become a standard part of clinical practice. Asian American people should equally be offered subgroup‐specific tailored interventions owing to heterogeneity of this population. Access to medications and surgery should be improved, in part by updating US indications for therapies to reflect race‐specific obesity thresholds and through inclusion of Asian American people of all subtypes with lower BMI values in clinical trials.
Study Importance.
What is already known?
Obesity is a growing public health crisis driven by a complex set of causes and is associated with a wide range of comorbidities.
Asian people have a greater propensity for gaining weight centrally relative to other racial groups.
Major reviews that have already been published include Yi et al. [27] and recent reviews.
What does this review add?
As highlighted in this review, the prevalence of obesity among Asian American individuals is lower than for the US general population when using current uniform BMI criteria; however, this is misleading because the use of Asian‐specific obesity cutoffs brings the prevalence of obesity among Asian American people in line with or above that of the general US population.
Obesity‐related comorbidities are more prevalent and occur at a lower BMI in Asian American people compared with White American people.
How might these results change the direction of research or the focus of clinical practice?
This review article raises awareness of the lower BMI thresholds for overweight and obesity in Asian American people and encourages the use of Asian‐specific parameters for assessing obesity in clinical practice.
This review also emphasizes the need to increase screening for obesity‐related comorbidities and to improve access to information on weight management and obesity therapies for Asian American people.
INTRODUCTION
Body mass index (BMI) has been widely adopted as a screening tool for overweight and obesity because it is correlated with other estimates of adiposity in Western countries [1]. Current assessment and management guidelines in the United States (US) recommend measuring BMI as a first screening step in evaluating obesity [1]. However, BMI is insufficient in evaluating obesity across all racial groups. A World Health Organization (WHO) expert consultation found that there are different associations between BMI, body fat percentage, and health risks in Asian populations versus European populations. The WHO panel recommended a lower BMI cutoff for obesity in Asian people of ≥27.5 kg/m2 instead of the standard ≥30.0 kg/m2 [2], whereas other bodies have recommended cutoffs of ≥25.0 kg/m2 [3, 4, 5]. Smaller race‐specific waist circumferences to measure visceral adiposity cutoffs have also been recommended by the International Diabetes Federation in the assessment of central obesity within metabolic syndrome in Asian people (Table 1) [6].
TABLE 1.
Definitions of obesity for the overall population and Asian individuals
| Classification | BMI (kg/m2) | ||||
|---|---|---|---|---|---|
| International classification (WHO) [2] | Asian population (WHO) [2] | Asian Indian population (Consensus Statement for Asian Indians of the Metabolic and Obesity Summit) [3] | Japanese population (JASSO) [4] | Korean population (KSSO) [5] | |
| Underweight | <18.5 | <18.5 | ‐ | <18.5 | <18.5 |
| Normal range | ≥18.5 and <25.0 | ≥18.5 and <23.0 | ≥18.0 and <23.0 | ≥18.5 and <25.0 | 18.5‐22.9 |
| Overweight | ≥25.0 and <30.0 | ≥23.0 and <27.5 | ≥23.0 and <25.0 | ‐ | 23.0‐24.9 |
| Obesity | ≥30.0 | ≥27.5 | ≥25.0 | ‐ | ‐ |
| Obesity class I | ≥30.0 and <35.0 | ‐ | ‐ | ≥25.0 and <30.0 | 25.0‐29.9 |
| Obesity class II | ≥35.0 and <40.0 | ‐ | ‐ | ≥30.0 and <35.0 | 30.0‐34.9 |
| Obesity class III | ≥40.0 | ‐ | ‐ | ≥35.0 and <40.0 | ≥35.0 |
| Obesity class IV | ‐ | ‐ | ‐ | ≥40.0 | ‐ |
| Classification | Waist circumference (cm) | ||||
|
International Diabetes Federation [ 6 ] Central obesity defined as BMI > 30.0; if BMI ≤30.0, then waist circumference should be assessed |
KSSO [ 5 ] Increased risk of comorbidity (T2D, hypertension, and dyslipidemia) according to abdominal obesity |
||||
| Central obesity |
|
|
|||
Abbreviations: JASSO, Japan Society for the Study of Obesity; KSSO, Korean Society for the Study of Obesity; T2D, type 2 diabetes; WHO, World Health Organization.
In the US, the Adult Treatment Panel III values (102 cm for men; 88 cm for women) are likely to continue to be used for clinical purposes.
The goal of this review is to explore the available evidence on obesity in Asian American individuals and subpopulations, particularly focusing on the use of BMI and alternative measures of obesity in this population and the need for Asian‐specific cutoffs. The review also discusses the challenges and strategies in obesity management in Asian American people.
LITERATURE SEARCH
A narrative literature search was conducted on May 22, 2021. Search terms included those related to background (“Asian” OR “Chinese” OR “Indian” OR “Filipino” OR “Vietnamese” OR “Korean” OR “Japanese”); location (“United States” OR “US” OR “America*”); obesity (“obese” OR “obesity” OR “overweight” OR “waist circumference”); and topics of interest (“prevalence” OR “etiology” OR “barrier*” OR “disparit*” OR “comorbidit*” OR “risk*”), which included Medical Subject Headings (MeSH) terms ([Asian Continental Ancestry Group AND United States] and [morbidity OR mortality OR epidemiology OR comorbidity OR diabetes mellitus, type 2 OR prediabetic state OR breast neoplasms OR hypercholesterolemia OR hyperlipidemias OR hypertriglyceridemia OR coronary disease OR hypertension OR metabolic syndrome]).
The PubMed database was searched using a combination of these key words, with results limited to 2011 through 2021 and English language. The articles were reviewed for relevance based on the title and abstract.
Additional references were identified from the bibliographies of retrieved articles, through additional targeted searches, and through author suggestions.
DISCUSSION
Pathophysiology of obesity in Asian people
Obesity rates have been increasing sharply in the US since the 1970s [1]. Obesity is associated with adiposity‐based comorbidities such as type 2 diabetes (T2D), hypertension, cardiovascular disease, and increased mortality [1]. Obesity is defined as the excessive accumulation or abnormal distribution of body fat that affects health [7].
Increasing evidence has indicated that obesity is more than the passive accumulation of excess weight and that it involves dysfunction of adipose tissue, the endocrine system, and the central nervous system [8]. External factors that may influence obesity include diet and lifestyle, socioeconomic factors, exposure to endocrine‐disrupting chemicals, drugs causing weight gain, infections, and changes in the microbiome [8].
According to the 2019 Census Bureau, Asian American individuals account for 5.7% of the US population [9]. The number of Asian American people is projected to reach nearly 33 million by 2050 [10]. The Asian American racial group is defined as people having origins in either East Asia, Southeast Asia, or the Indian subcontinent [9]. Thus, this racial group is heterogenous in nature, comprising populations from China, India, Japan, Korea, the Philippines, and Vietnam. Asian American people are equally diverse in socioeconomic status, which impacts access to health care among other factors.
Asian people have been shown to gain weight centrally, at a faster rate than other ethnic groups [11]. When adjusted for age, BMI, and total fat mass, Chinese and South Asian people (i.e., Asian people from the Indian subcontinent) have significantly more visceral adipose tissue than White people among Canadian men and women [12]. In addition, Asian Indian men and women in India have a significantly higher waist‐weight ratio than White people in the US despite having significantly lower BMI [13], indicating a predisposition for central adiposity.
Although obesity is associated with multiple adiposity‐based comorbidities [1], central adiposity has been shown to be more closely associated with certain comorbidities than peripheral adiposity, and ethnicity‐specific waist circumference thresholds have been proposed as a vital sign for cardiometabolic risk [14]. The total body fat content of Asian people without obesity with T2D is similar to that of Asian people without diabetes [15]. However, the proportion of visceral fat and intra‐hepatic fat is greater, likely contributing to the development of insulin resistance and increased cardiovascular risk [15]. In Chinese adults in Asia, waist circumference and waist‐height ratio were significantly more closely associated with the risk of T2D than BMI [16], whereas waist circumference was significantly more closely associated with metabolic syndrome [17, 18]. In Korean adults, visceral fat was more strongly associated with T2D than with waist circumference or BMI [19]. Moreover, in a 10‐year study in Japanese American people with overweight, intra‐abdominal fat, along with BMI and waist circumference, was positively associated with the risk of T2D, whereas subcutaneous abdominal fat and subcutaneous thigh fat had no association [20].
Genetics play an important role in obesity pathophysiology, including fat distribution. Genetic variants have been identified that are related to fat distribution and cardiovascular disease risk [11]. Genome‐wide association studies have identified approximately 500 loci influencing fat distribution, waist circumference, and waist‐hip ratio. Although the number of loci identified in Asian people is very small (only 27), most of these loci do not overlap with loci identified in European and African people [21].
Burden of obesity in the Asian American population
Prevalence of obesity
Obesity has been observed to be less prevalent in Asian American people compared with other American populations when using the BMI cutoff for the general population (≥30.0 kg/m2; Table 2) [22, 23, 24, 25, 26, 27]. As a result of this, as well as their relatively small population in the US (6% in 2010) [28], Asian American people have received less attention in the obesity literature compared with other racial groups. However, conservatively, when using the WHO‐defined BMI cutoff (BMI ≥ 27.5) for Asian people, obesity prevalence in Asian American people has been found to be similar to, or higher than, that in White people (Table 2) [22, 23, 27, 29, 30, 31, 32]. Moreover, a survey in New York City covering the period of 2004 and 2013 through 2014 showed that the largest increase in the prevalence of obesity, as measured by race‐specific BMI cutoffs, was among Asian people compared with other racial groups [32]. Differences in obesity prevalence between Asian American ethnic groups have also been observed with the Asian‐specific BMI cutoff [27, 30, 33, 34, 35], with the highest rate of obesity consistently seen among Filipino people (Table 2) [30, 33, 34]. These results demonstrate a need for detailed ethnicity data collection for Asian American people because the BMI cutoff may need to be different to adequately define obesity in this population.
TABLE 2.
Studies reporting obesity prevalence with standard or race‐specific obesity cutoffs in Asian American individuals covering the period from 2011 to 2018
| Reference | Data source and key relevant findings | General obesity cutoffs | Race‐specific obesity cutoffs |
|---|---|---|---|
| Aoki et al. [ 54 , 77 ] | High BMI in Asian adults included in NHANES 2011‐2012 | ‐ |
BMI ≥ 25.0 (n = 733) Sex, %:
Birthplace, %:
|
| Becerra et al. [ 33 ] | Data from the 2010‐2011 CHIS on adults with obesity | BMI ≥ 30.0 for all groups, %
|
BMI ≥ 27.5, %
|
| Chen et al. [ 22 ] | Obesity in racially and ethnically diverse men and women aged 54 to 93 y in the Multi‐Ethnic Study of Atherosclerosis Sleep Cohort (2010‐2013) | BMI ≥ 30.0 for all groups, %
|
BMI ≥ 25.0 for Asian individuals, BMI ≥ 30.0 for non‐Asian individuals, %
|
| Echeverria et al. [ 23 ] | Obesity in a nationally representative sample of US adults aged ≥20 y in NHANES 2011‐2014 | BMI ≥ 30.0 for all groups, %
|
BMI ≥ 25.0, %
|
| Golabi et al. [ 38 ] | Adults with and without NAFLD included in NHANES 2011‐2016 | ‐ |
Obesity: BMI ≥ 25.0 for Asian individuals, BMI ≥ 30.0 for non‐Asian individuals, weighted % (SE)
Central obesity: waist circumference ≥90 cm for Asian men, ≥94 cm for other men, ≥80 cm for all women, % (SE)
|
| Gong et al. [ 34 ] | Obesity in Asian adults included in 2013‐2014 CHIS | ‐ |
BMI ≥ 27.5 Ethnicity, %
Sex, %
|
| Janevic et al. [ 24 ] | Obesity in women in New York City who gave birth in 2010‐2014 | BMI ≥ 30.0 for all groups, %
|
‐ |
| Liu et al. [ 29 ] | Nationally representative sample of US adults aged 20 y or older in NHANES 2011‐2018; n = 21,093, 2732 were non‐Hispanic Asian (5.6%), 7757 were non‐Hispanic White (64.8%) (data here reported from 2017‐2018) | Waist circumference ≥102 cm for men, ≥88 cm for women, % (95% CI)
|
BMI ≥ 27.5 for Asian individuals, BMI ≥ 30.0 for non‐Asian individuals, % (95% CI)
|
| McEligot et al. [ 78 ] | Obesity (definition unclear but no distinction for Asian individuals made) at a metropolitan university from fall 2006 to fall 2013 | BMI ≥ 30.0 for all groups, %
|
‐ |
| Mui et al. [ 30 ] | Obesity prevalence in the 2002‐2015 National Health Interview Surveys | ‐ | BMI ≥ 27.5 for Asian individuals, BMI ≥ 30.0 for non‐Asian individuals, %
|
| Ogden et al. [ 79 ] | Data from NHANES 2011‐2014 | BMI ≥ 30.0 for obesity in adults aged ≥20 y, % (n values not reported)
|
‐ |
| Pu et al. [ 31 ] | Obesity in pregnant women in 2007‐2012 in the electronic health records of a large mixed‐payer ambulatory care organization in Northern California | BMI ≥ 30.0 for all groups, %
|
BMI ≥ 27.5 for Asian individuals, BMI ≥ 30.0 for non‐Asian individuals, %
|
| Rodriguez et al. [ 25 ] | Obesity (BMI ≥ 30.0) in participants in the prospective community‐based Multi‐Ethnic Study of Atherosclerosis aged 45‐84 y and without known clinical cardiovascular disease at baseline | BMI ≥ 30.0 for all groups, %
|
‐ |
| Rummo et al. [ 32 ] | Obesity prevalence among New York City adults aged ≥20 y in 2013‐2014 | BMI ≥ 27.5 for Asian individuals, BMI ≥ 30.0 for non‐Asian individuals, % (95% CI)
|
|
| Sa et al. [ 80 ] | Obesity (BMI ≥ 30.0) in a nationally representative sample of 319,342 US college students (mean age 20.4 y; 67.7% female) from fall 2011 to spring 2015 | BMI ≥ 30.0 for all groups for spring 2015 only, % (95% CI) (subgroup n values not reported)
|
‐ |
| Tung et al. [ 26 ] | Obesity (BMI ≥ 30.0) in adults eligible for T2D screening (age ≥45 y) in 2012‐2014 | BMI ≥ 30.0 for all groups, weighted %
|
‐ |
| Vargas [ 50 ] | Comparison of BMI categories of obesity in adult Filipino American individuals in New Jersey in 2014 | BMI ≥ 30.0, %
|
BMI ≥ 27.5, %
|
| Yi et al. [ 27 ] | Age‐standardized prevalence of obesity (BMI ≥ 27.5 for Asian American individuals [n = 783], BMI ≥ 30.0 for White individuals [n = 3525]) in New York City in 2012 | BMI ≥ 30.0 for all groups, % (95% CI) (subgroup n values not reported)
|
BMI ≥ 27.5 for Asian individuals, BMI ≥ 30.0 for non‐Asian individuals, % (95% CI) (subgroup n values not reported)
|
Abbreviations: CHIS, California Health Interview Survey; NAFLD, nonalcoholic fatty liver disease; NHANES, National Health and Nutrition Examination Survey; T2D, type 2 diabetes; WHO, World Health Organization.
Comorbidities and mortality
Consistent with their increased propensity for central weight gain, Asian people are at greater risk of obesity‐related comorbidities. In a population‐based cohort aged 40 to 69 years, a study in the UK attempted to establish race‐based cutoff points for developing T2D equivalent to set cutoffs for White people (BMI of 30.0 kg/m2 or waist circumference 102 cm in men and 88 cm in women). The equivalent cutoffs for South Asian people were much lower, with BMI of 25.2 kg/m2 or waist circumference of 90.4 cm for men and 84.0 cm for women [36], demonstrating that South Asian people are susceptible to comorbidities with lower levels of weight gain than White people. In the US, the Centers for Disease Control and Prevention (CDC) reported the prevalence of diagnosed T2D for adults (2017‐2018) to be higher for Asian American compared with White individuals in both sexes and after age adjustment (9.2% vs. 7.5%) [37]. Despite having a consistently lower BMI, Asian American people, as an aggregated group, have a higher prevalence of T2D, gestational diabetes, dyslipidemia, hypertension, and sleep apnea than White people (Table 3) [22, 23, 25, 31, 38, 39, 40]. Disparities exist between the subgroups of Asian American people in terms of risk of comorbidities and are discussed in more depth in the following section.
TABLE 3.
Studies in Asian and non‐Asian (only White individuals shown) populations comparing the prevalence of comorbidities with BMI in the US
| Reference | Population | Obesity (according to BMI or waist circumference) | Obesity‐related comorbidities |
|---|---|---|---|
| Chen et al. [ 22 ] | Men and women aged 54‐93 y in the Multi‐Ethnic Study of Atherosclerosis Sleep Cohort (2010‐2013) | BMI, mean (SD)
|
Diagnosed sleep apnea, %
Apnea‐hypopnea index (events/h), mean (SD)
|
| Chen et al. [ 39 ] | Community‐based cross‐sectional study of 2053 adults in the Multi‐Ethnic Study of Atherosclerosis |
BMI, mean (SD)
Waist circumference (cm), mean (SD)
|
T2D, %
Hypertension, %
Apnea‐hypopnea index (events/h), median (IQR)
|
| Echeverria et al. [ 23 ] | Obesity in a nationally representative sample of US adults aged ≥20 y in NHANES 2011‐2014 | BMI: 18.5 to <25.0, %
|
T2D, %
|
| Golabi et al. [ 38 ] | Adults with and without NAFLD included in NHANES 2011‐2016 |
BMI, mean (SE)
Waist circumference (cm), mean (SE)
|
T2D, % (SE)
Hypertension (%), mean (SE)
Hyperlipidemia (%), mean (SE)
Metabolic syndrome (%), mean (SE)
|
| Pu et al. [ 31 ] | Pregnant women in 2007‐2012 included in the electronic health records of a large mixed‐payer ambulatory care organization in Northern California | BMI < 25.0, %
|
Gestational diabetes, %
|
| Rodriguez et al. [ 25 ] | Participants in the prospective community‐based Multi‐Ethnic Study of Atherosclerosis aged 45‐84 y and without known clinical cardiovascular disease at baseline | Mean BMI, % (SD)
|
T2D, %
Hypertension, %
|
| Silbiger et al. [ 40 ] | Coronary artery disease risk factors and angiograms of South Asian individuals and White individuals consecutively referred with stable angina pectoris or acute coronary syndrome in New York City | Mean BMI
|
T2D, %
Hypertension, %
Obesity, %
Dyslipidemia, %
|
Abbreviations: NAFLD, non‐alcoholic fatty liver disease; NHANES, National Health and Nutrition Examination Survey; T2D, type 2 diabetes.
The influence of the subtype of Asian American on incidence of obesity and comorbidities
Despite the diversity of Asian American subpopulations, the majority of studies still group them into one large category, potentially missing important heterogeneity in disease burden and risk. However, studies are emerging to identify subpopulation‐specific health concerns.
In a study of 47,970 adults in California, being Chinese, Korean, or Vietnamese was associated with a lower prevalence of obesity compared with non‐Hispanic White individuals. Among Asian people, compared with being Chinese, being Japanese or Filipino was associated with a higher prevalence of obesity [34].
A retrospective analysis of more than 95,000 patient records from Asian American and non‐Hispanic White people showed that, among Asian subpopulations, Asian Indian and Filipino people had the highest average BMI for both women and men [41]. Equally, Asian Indian and Filipino people emerged as having the highest prevalence of T2D (21.3% and 25.3%, respectively) compared with the non‐Hispanic White population (8.1%) or Asian American people as a combined group (14.3%), even after adjustment for age and BMI. These results mirror a parallel study evaluating T2D prevalence by BMI groups in the US. T2D prevalence, adjusted for age, sex, and birthplace, was significantly higher for Filipino, Korean, South Asian, and Vietnamese people with BMI of 23.0 to 24.9 and for Chinese, Filipino, Japanese, Korean, South Asian, and Vietnamese people with BMI of 25.0 to 27.49 compared with White people in these same BMI ranges [35]. A study evaluating T2D risk in Native Hawaiian people compared the effect of mixed ancestry in adults aged 50 years or older [42]. Asian admixture was associated with a higher risk for T2D than for any other admixture or for Native Hawaiian people alone, independent of BMI status, diet, and other known lifestyle‐related factors [42].
An evaluation of racial and ethnic differences in the relative contribution of risk factors for gestational diabetes mellitus (GDM) among Asian subpopulations (Asian Indian, Chinese, Filipino, Japanese, Korean, and Vietnamese) and non‐Hispanic White people revealed that age‐adjusted GDM was most prevalent among South Asian people (19.3%) [31]. This was followed closely by Filipino (19.0%) and Vietnamese (18.8%) populations, with the percentage of non‐Hispanic White people with GDM reported as 7.0%. Among Asian American people, the frequency of obesity (BMI ≥27.5) varied from 2.8% in the Japanese and South Asian populations to 16.4% in the Filipino population [31].
A systematic review, published in 2013, analyzing the available literature on overweight, obesity, and T2D in Asian American subtypes concluded that, similar to the aforementioned studies, of all the subgroups, Filipino people had the highest reported mean BMI compared with the other subgroups [43]. However, Asian Indian people with BMI ≥ 30 had the highest rates of diabetes [43].
Collectively, these studies indicate the heterogeneity among Asian American populations and highlight the need for further efforts to analyze and understand overweight, obesity, and associated comorbidities of each racial subgroup within the Asian American population.
Impact of sex on obesity
The role of sex in the context of race and obesity is less clear. According to the CDC, in 2013 through 2016, the proportion of Asian American people who were over 20 years old and had obesity (BMI ≥ 30.0) was lower for men than for women (10.9% vs. 13.6%), whereas the proportion of Asian people who were classified as having overweight (BMI ≥ 25.0) was higher for men than for women (39.0% vs. 23.0%) [44]. During 2004 through 2014 in New York City, obesity prevalence measured using race‐specific BMI cutoffs showed a greater change over time in Asian women than in Asian men (65.2% vs. 17.6%) [32]. A national survey covering 2011 through 2018 also found that obesity prevalence increased across race and sex groups significantly, using race‐specific BMI cutoffs [29]. However, BMI increased significantly for Asian men and women, whereas waist circumference increased significantly only for Asian men [29]. This is in accord with CDC data from 2018, showing that the age‐adjusted prevalence of T2D (10.0% vs. 8.5%) and the age‐adjusted mortality rate linked to T2D (19.0 vs. 12.7 per 100,000) were both higher for Asian men than for Asian women [37]. Further work is needed to separate the effects of race and sex on obesity and related comorbidities.
Challenges in managing obesity in Asian American individuals
Race‐specific obesity criteria
There are factors specific to Asian American individuals that add to the challenges in obesity management in this population. Foremost is the limited awareness among physicians in the US of the lower BMI obesity threshold for Asian individuals, as suggested by the paucity of articles identified in this review and the many articles published in the last decade that continue to use the BMI obesity threshold for the general population when assessing obesity (Table 2).
Physical activity and exercise
Environmental factors such as physical activity and diet also influence obesity management in Asian American individuals. Unfortunately, data on physical activity in Asian American individuals are limited [45]. In a nationwide survey, the prevalence of Asian American individuals reporting no physical activity increased from 21.5% (in 2011‐2012) to 32.4% (in 2015‐2016), which was paralleled by a decrease in the prevalence of those with normal weight (BMI < 25.0), from 60.5% (in 2011‐2012) to 55.3% (in 2015‐2016) [46]. In Houston, Texas, Asian people were less likely than White people to have sufficient levels of physical activity (38.6% vs. 49.9%), and Asian immigrant people were also less likely to be physically active compared with US‐born Asian people [45]. A study in 2007 through 2009 found no association between self‐reported moderate‐to‐vigorous‐intensity physical activity and obesity among Asian men and women, in contrast to inverse associations found in most other groups, suggesting that factors other than physical activity and exercise may be more important for Asian people or that there may be errors or bias in these self‐reported data [47]. These results indicate a need for more data on exercise in managing obesity in Asian American people and suggest that diet may be an important environmental factor.
Diet
The influence of diet on obesity is significant, and the high carbohydrate intake in Asian diets has been associated with T2D and metabolic disease [48, 49]. Among Filipino American people in New Jersey, fat intake decreased and carbohydrate intake increased with age at the time of migration to the US, but this had no significant effect on total calorie intake [50]. In a study of Japanese American people, developing obesity was positively associated with total and simple carbohydrate intake, as well as inversely associated with intake of vegetable protein and complex carbohydrates [51]. A study of students and their mothers in Chinese language schools in the San Francisco Bay Area found that low levels of maternal acculturation, i.e., the extent to which minority groups have adapted their lifestyles to a new environment, and unhealthy food choices were predictors of high BMI in Chinese American children, although the relationship between maternal acculturation and diet was unclear [52]. For South Asian people in Europe, migration led to an increase in fat intake and a reduction in carbohydrates and fiber, with carbohydrates derived from more refined sources post‐migration [53], suggesting that migration has a direct impact on diet and the risk of obesity.
Acculturation
Obesity in Asian American people is also influenced by length of residence in the US and acculturation. BMI is higher in US‐born Asian people than in foreign‐born Asian people in the US (Table 2) [23, 24, 54]. BMI is also higher in Asian people who have resided in the US for at least 20 years versus fewer than 20 years [23]. Additionally, mean BMI and prevalence of obesity were shown to increase among Asian people in successive generations in the US [55]. A study looking at second‐generation Japanese American people found that they had higher BMI and fasting insulin compared with first‐generation Japanese American people and Japanese people residing in Japan [56]. The prevalence of obesity, metabolic syndrome, and T2D also increased with each generation after migration to the US [56].
Role of cultural beliefs
Potential cultural challenges in obesity management can also emerge from a lack of knowledge or misperceptions on obesity and its comorbidities. South Asian American people may underestimate their weight status and weight‐related health consequences, consistent with findings from the general population in the US [57]. Although weight stigma is a pervasive problem among people with obesity, there is limited literature available on the impact of overweight or obesity on the health outcomes among Asian American people. Among Chinese immigrant mothers of young children in the US, culture‐specific feeding beliefs and practices (specifically, offering children their favorite foods and valuing plumper children) were negatively associated with mothers' perceptions of their children's body size [58]. Over the longer term, analysis of data from foreign‐born Asian American people who participated in the National Health Interview Surveys in 1994 through 2009 showed that, in cohorts based on duration of residence in the US, older cohorts had improving self‐rated health while also having increasing obesity [59].
Strategies for managing obesity in Asian American people
Screening for overweight or obesity in Asian American people
Multiple strategies can be implemented for managing obesity in Asian American people. Of immediate concern is the need to identify overweight and obesity in Asian American people. Therefore, development of national guidelines with appropriate BMI criteria should be considered. Until then, international guidelines for Asian people should be used for assessing overweight and obesity in Asian American people (Table 1). These BMI criteria should also be supplemented with the use of appropriate waist measurements and body composition analysis (if available) [60]. An added benefit is that body composition analysis can provide an estimate of resting metabolic rate [61] that could guide appropriate dietary counseling. The standard assessment of energy requirement [61] does not take into account the lower absolute resting energy expenditure in Asian people compared with White people [62].
Lifestyle interventions
Lifestyle interventions relevant to Asian people with obesity are key to obesity management. Any lifestyle intervention should include three components: diet, physical activity, and behavior modification [63]. Dietary recommendations are most challenging owing to cultural differences. Traditional Asian Indian diets, for example, can have an excess of saturated fats, sugar, and refined carbohydrates and can be low in protein [64]. Therefore, when creating a nutrition plan, culturally sensitive content may assist with adherence [65, 66]. In programs for T2D prevention in Chinese‐speaking immigrants in New York [66] and atherosclerotic cardiovascular disease prevention in South Asian people in Chicago [65], the use of native‐language reading materials as well as culturally tailored interactive sessions on physical activity and dieting advice was shown to be highly effective in improving outcomes. Both programs also encouraged family involvement to improve adherence [65, 66]. In the program for Chinese‐speaking immigrants with prediabetes, participants achieved significant weight loss after 6 months that was maintained after 12 months compared with a control group receiving only mailed diabetes‐prevention information [66]. Participants in the program for South Asian people with increased atherosclerotic cardiovascular disease risk showed significant weight loss at 6 months compared with a control group receiving printed materials only, and study retention was an impressive 100% [65]. Both studies indicate the importance of engagement, language, and family participation in influencing program retention and health outcomes.
Screening for obesity‐related comorbidities is also important to manage those at risk. However, despite their higher risk of T2D, Asian American people were shown to be significantly less likely than other groups to receive recommended T2D screening based on the criteria of age ≥ 45 years or age < 45 years with BMI ≥ 25.0 [26]. Therefore, improved screening for related comorbidities should be a part of any obesity program directed toward Asian American people with a focus on subgroups at particular risk, such as Filipino and South Asian people.
Antiobesity medications
Antiobesity medications (AOMs) are a useful tool in obesity management [1]. Orlistat was shown to significantly reduce body weight and improve glycemic control in Chinese people with overweight and obesity and newly diagnosed T2D [67]. In a meta‐analysis of randomized controlled trials, glucagon‐like peptide‐1 receptor agonists (liraglutide, dulaglutide, exenatide, and lixisenatide) were effective in reducing weight in Asian people with T2D and obesity [68]. The recent Semaglutide Treatment Effect in People with obesity (STEP) 6 trial also showed that Japanese and South Korean people with overweight and obesity had superior and clinically meaningful reductions in body weight with semaglutide compared with placebo [69]. In a study of the electronic health records of 2,248,407 adults in the US eligible for AOMs, White people were prescribed these medications at almost twice the rate of Asian people, although in both racial groups it was <2% [70]. This disparity is likely exacerbated by the use of eligibility criteria in the US that do not consider race: only BMI ≥ 30.0 or BMI ≥27.0 with comorbidities [71, 72]. Studies of AOMs in Asian people with lower BMI (<27.0) are lacking. Therefore, pharmaceutical companies should consider performing clinical trials in Asian people with BMI of <27.0 as well as seeking approval for AOMs in indications with lower Asian‐specific BMI limits to ensure that these therapies are available to the Asian population.
Bariatric surgery
Bariatric surgery has been reported to be effective in improving weight and glycemic control in Asian people with T2D and BMI ≥ 30.0 [73]. In a US study using data for 1,729,245 bariatric‐surgery‐eligible participants extracted from the hospital discharge Healthcare Cost and Utilization Project‐National (Nationwide) Inpatient Sample (HCUP‐NIS) data set (2008‐2016), Asian people were significantly less likely to receive inpatient bariatric surgery than White people after adjusting for demographic, socioeconomic, and clinical variables [74]. In the US, bariatric surgery is recommended for people with BMI ≥ 40.0 or ≥35.0 with a related comorbidity, again regardless of race [1, 71, 72]. The BMI cutoff for bariatric surgery for the treatment of obesity in Asian countries is considerably lower (BMI ≥ 32.5‐37.5 or ≥30.0‐32.5 with one or more related comorbidities) [75]. Therefore, there should be an effort to develop race‐specific US guidelines for obesity therapies, for both AOMs as well as bariatric surgery, to improve access for Asian people.
CONCLUSION
The prevalence of obesity among Asian American people is lower than for the US general population when using current uniform BMI criteria; however, this is misleading because the use of Asian‐specific obesity cutoffs brings the prevalence of obesity among Asian American people in line with, or above, that of the general US population. Therefore, there is a need to broaden awareness among health care providers of the lower BMI thresholds for overweight and obesity in Asian American people and for more research on the burden of obesity among Asian American people.
Attention in clinical practice to lower BMI cutoff points among Asian American people may be an important factor to identify and address metabolic and cardiovascular risks prior to progression to obesity‐related comorbidities. The American Diabetes Association in its position statement suggestsd that lower BMI cutoffs (≥23) should be applied to Asian American people when screening for GDM and T2D [76]. Further research is equally needed to identify optimal BMI cutoffs for overweight and obesity in each Asian subgroup.
Filipino people in particular, along with South Asian people, have been identified as subgroups at high risk of obesity and diabetes. Greater efforts are required to boost specific screening for comorbidities and to improve access to information on weight management and personalized treatment plans for obesity in Asian American subpopulations.
AUTHOR CONTRIBUTIONS
All authors contributed to manuscript writing (assisted by a medical writer paid for by the funder) and approved the final version of the manuscript. All authors had final responsibility for the decision to submit for publication.
CONFLICT OF INTEREST
Zhaoping Li and Sunil Daniel declared no conflict of interest. Ken Fujioka reports consultancy fees from Amgen Inc.; Boehringer Ingelheim; Gelesis; Janssen Global Services, LLC; Nalpropion Pharmaceuticals, Inc.; Novo Nordisk; and Rhythm Pharmaceuticals, Inc. Devika Umashanker reports consultancy fees from Novo Nordisk.
ACKNOWLEDGMENTS
All of those who contributed significantly to this work have been listed as authors. Medical writing and editorial support were provided by Dan Hami of Axis, a division of Spirit Medical Communications Group Limited, under the direction of the authors. Novo Nordisk Inc. performed a medical accuracy review.
Li Z, Daniel S, Fujioka K, Umashanker D. Obesity among Asian American people in the United States: A review. Obesity (Silver Spring). 2023;31(2):316‐328. doi: 10.1002/oby.23639
Funding information Novo Nordisk Inc., Plainsboro, New Jersey, USA
REFERENCES
- 1. Bray GA, Heisel WE, Afshin A, et al. The science of obesity management: an Endocrine Society scientific statement. Endocr Rev. 2018;39:79‐132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. WHO Expert Consultation . Appropriate body‐mass index for Asian populations and its implications for policy and intervention strategies. Lancet. 2004;363:157‐163. [DOI] [PubMed] [Google Scholar]
- 3. Misra A, Chowbey P, Makkar BM, et al. Consensus statement for diagnosis of obesity, abdominal obesity and the metabolic syndrome for Asian Indians and recommendations for physical activity, medical and surgical management. J Assoc Physicians India. 2009;57:163‐170. [PubMed] [Google Scholar]
- 4. Kohda Y. Paradigm change to future health enhancement through comprehending the concept of obesity disease in Japan. J Clin Toxicol. 2018;8:1000389. doi:10.4172/2161-0495.1000389. [Google Scholar]
- 5. Seo MH, Lee WY, Kim SS, et al. 2018 Korean Society for the Study of Obesity guideline for the management of obesity in Korea. J Obes Metab Syndr. 2019;28:40‐45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. International Diabetes Federation . IDF consensus worldwide definition of the metabolic syndrome. Updated July 29, 2020. Accessed June 1, 2021. https://www.idf.org/e-library/consensus-statements/60-idfconsensus-worldwide-definitionof-the-metabolic-syndrome.html
- 7. Mayoral LP, Andrade GM, Mayoral EP, et al. Obesity subtypes, related biomarkers & heterogeneity. Indian J Med Res. 2020;151:11‐21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Schwartz MW, Seeley RJ, Zeltser LM, et al. Obesity pathogenesis: an Endocrine Society scientific statement. Endocr Rev. 2017;38:267‐296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. U.S. Department of Health and Human Services Office of Minority Health . Minority population profiles: Asian Americans. Updated October 12, 2021. Accessed September 8, 2022. https://minorityhealth.hhs.gov/omh/browse.aspx?lvl=3&lvlid=63
- 10. U.S. Census Bureau . Projected race and Hispanic origin: Main Projections Series for the United States, 2017 to 2060. Updated September 2018. Accessed September 26, 2022. https://www2.census.gov/programs-surveys/popproj/tables/2017/2017-summary-tables/np2017-t4.xlsx
- 11. Yaghootkar H, Whitcher B, Bell JD, Thomas EL. Ethnic differences in adiposity and diabetes risk ‐ insights from genetic studies. J Intern Med. 2020;288:271‐283. [DOI] [PubMed] [Google Scholar]
- 12. Lear SA, Humphries KH, Kohli S, Chockalingam A, Frohlich JJ, Birmingham CL. Visceral adipose tissue accumulation differs according to ethnic background: results of the Multicultural Community Health Assessment Trial (M‐CHAT). Am J Clin Nutr. 2007;86:353‐359. [DOI] [PubMed] [Google Scholar]
- 13. Bajaj HS, Pereira MA, Anjana RM, et al. Comparison of relative waist circumference between Asian Indian and US adults. J Obes. 2014;2014:461956. doi: 10.1155/2014/461956 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Ross R, Neeland IJ, Yamashita S, et al. Waist circumference as a vital sign in clinical practice: a Consensus Statement from the IAS and ICCR Working Group on Visceral Obesity. Nat Rev Endocrinol. 2020;16:177‐189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Rattarasarn C. Dysregulated lipid storage and its relationship with insulin resistance and cardiovascular risk factors in non‐obese Asian patients with type 2 diabetes. Adipocyte. 2018;7:71‐80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Fan Y, Wang R, Ding L, et al. Waist circumference and its changes are more strongly associated with the risk of type 2 diabetes than body mass index and changes in body weight in Chinese adults. J Nutr. 2020;150:1259‐1265. [DOI] [PubMed] [Google Scholar]
- 17. Liu L, Liu Y, Sun X, et al. Identification of an obesity index for predicting metabolic syndrome by gender: the rural Chinese cohort study. BMC Endocr Disord. 2018;18:54. doi: 10.1186/s12902-018-0281-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Nurjono M, Lee J. Waist circumference is a potential indicator of metabolic syndrome in Singaporean Chinese. Ann Acad Med Singap. 2013;42:241‐245. [PubMed] [Google Scholar]
- 19. Jung SH, Ha KH, Kim DJ. Visceral fat mass has stronger associations with diabetes and prediabetes than other anthropometric obesity indicators among Korean adults. Yonsei Med J. 2016;57:674‐680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Hoyer D, Boyko EJ, McNeely MJ, Leonetti DL, Kahn SE, Fujimoto WY. Subcutaneous thigh fat area is unrelated to risk of type 2 diabetes in a prospective study of Japanese Americans. Diabetologia. 2011;54:2795‐2800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Sun C, Kovacs P, Guiu‐Jurado E. Genetics of body fat distribution: comparative analyses in populations with European, Asian and African ancestries. Genes (Basel). 2021;12:841. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Chen X, Wang R, Zee P, et al. Racial/ethnic differences in sleep disturbances: the Multi‐Ethnic Study of Atherosclerosis (MESA). Sleep. 2015;38:877‐888. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Echeverria SE, Mustafa M, Pentakota SR, et al. Social and clinically‐relevant cardiovascular risk factors in Asian Americans adults: NHANES 2011–2014. Prev Med. 2017;99:222‐227. [DOI] [PubMed] [Google Scholar]
- 24. Janevic T, Zeitlin J, Egorova N, Balbierz A, Howell EA. The role of obesity in the risk of gestational diabetes among immigrant and U.S.‐born women in New York City. Ann Epidemiol. 2018;28:242‐248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Rodriguez CJ, Soliman EZ, Alonso A, et al. Atrial fibrillation incidence and risk factors in relation to race‐ethnicity and the population attributable fraction of atrial fibrillation risk factors: the Multi‐Ethnic Study of Atherosclerosis. Ann Epidemiol. 2015;25:71‐76.e1. doi: 10.1016/j.annepidem.2014.11.024 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Tung EL, Baig AA, Huang ES, Laiteerapong N, Chua KP. Racial and ethnic disparities in diabetes screening between Asian Americans and other adults: BRFSS 2012–2014. J Gen Intern Med. 2017;32:423‐429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Yi SS, Kwon SC, Wyatt L, Islam N, Trinh‐Shevrin C. Weighing in on the hidden Asian American obesity epidemic. Prev Med. 2015;73:6‐9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. U.S. Census Bureau . Asian/Pacific American Heritage Month: May 2011. Facts for Features. Revised April 29, 2011. Accessed June 1, 2021. https://www.census.gov/newsroom/releases/archives/facts_for_features_special_editions/cb11-ff06.html
- 29. Liu B, Du Y, Wu Y, Snetselaar LG, Wallace RB, Bao W. Trends in obesity and adiposity measures by race or ethnicity among adults in the United States 2011‐18: population based study. BMJ. 2021;372:n365. doi: 10.1136/bmj.n365 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Mui P, Hill SE, Thorpe RJ Jr. Overweight and obesity differences across ethnically diverse subgroups of Asian American men. Am J Mens Health. 2018;12:1958‐1965. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Pu J, Zhao B, Wang EJ, et al. Racial/ethnic differences in gestational diabetes prevalence and contribution of common risk factors. Paediatr Perinat Epidemiol. 2015;29:436‐443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Rummo P, Kanchi R, Perlman S, Elbel B, Trinh‐Shevrin C, Thorpe L. Change in obesity prevalence among New York City adults: the NYC Health and Nutrition Examination Survey, 2004 and 2013–2014. J Urban Health. 2018;95:787‐799. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Becerra BJ, Scroggins CM, Becerra MB. Association between asthma and obesity among immigrant Asian Americans, California Health Interview Survey, 2001–2011. Prev Chronic Dis. 2014;11:E209. doi: 10.5888/pcd11.140333 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Gong S, Wang K, Li Y, Alamian A. Geographic differences in obesity prevalence and its risk factors among Asian Americans: findings from the 2013–2014 California Health Interview Survey. Sci Rep. 2018;8:12510. doi: 10.1038/s41598-018-29906-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Jih J, Mukherjea A, Vittinghoff E, et al. Using appropriate body mass index cut points for overweight and obesity among Asian Americans. Prev Med. 2014;65:1‐6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Tillin T, Sattar N, Godsland IF, Hughes AD, Chaturvedi N, Forouhi NG. Ethnicity‐specific obesity cut‐points in the development of type 2 diabetes ‐ a prospective study including three ethnic groups in the United Kingdom. Diabet Med. 2015;32:226‐234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. U.S. Department of Health and Human Services Office of Minority Health . Diabetes and Asian Americans. Updated March 1, 2021. Accessed May 3, 2021. https://minorityhealth.hhs.gov/omh/browse.aspx?lvl=4&lvlid=48
- 38. Golabi P, Paik J, Hwang JP, Wang S, Lee HM, Younossi ZM. Prevalence and outcomes of non‐alcoholic fatty liver disease (NAFLD) among Asian American adults in the United States. Liver Int. 2019;39:748‐757. [DOI] [PubMed] [Google Scholar]
- 39. Chen X, Wang R, Lutsey PL, et al. Racial/ethnic differences in the associations between obesity measures and severity of sleep‐disordered breathing: the Multi‐Ethnic Study of Atherosclerosis. Sleep Med. 2016;26:46‐53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Silbiger JJ, Stein R, Roy M, et al. Coronary artery disease in South Asian immigrants living in New York City: angiographic findings and risk factor burdens. Ethn Dis. 2013;23:292‐295. [PubMed] [Google Scholar]
- 41. Wang EJ, Wong EC, Dixit AA, Fortmann SP, Linde RB, Palaniappan LP. Type 2 diabetes: identifying high risk Asian American subgroups in a clinical population. Diabetes Res Clin Pract. 2011;93:248‐254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Maskarinec G, Morimoto Y, Jacobs S, Grandinetti A, Mau MK, Kolonel LN. Ethnic admixture affects diabetes risk in native Hawaiians: the Multiethnic Cohort. Eur J Clin Nutr. 2016;70:1022‐1027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Staimez LR, Weber MB, Venkat Narayan KM, Oza‐Frank R. A systematic review of overweight, obesity, and type 2 diabetes among Asian American subgroups. Curr Diab Rev. 2013;9:312‐331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. U.S. Department of Health and Human Services Office of Minority Health . Obesity and Asian Americans. Updated March 26, 2020. Accessed May 3, 2021. https://minorityhealth.hhs.gov/omh/browse.aspx?lvl=4&lvlid=55
- 45. Kao D, Carvalho Gulati A, Lee RE. Physical activity among Asian American adults in Houston, Texas: data from the Health of Houston Survey 2010. J Immigr Minor Health. 2016;18:1470‐1481. [DOI] [PubMed] [Google Scholar]
- 46. Kalra R, Patel N, Arora P, Arora G. Cardiovascular health and disease among Asian‐Americans (from the National Health and Nutrition Examination Survey). Am J Cardiol. 2019;124:270‐277. [DOI] [PubMed] [Google Scholar]
- 47. Kwon S, Wang M, Hawkins M. Association between self‐reported physical activity and obesity among White, Black, Hispanic, and Asian Americans: 2007 and 2009 BRFSS. Ethn Dis. 2013;23:129‐135. [PubMed] [Google Scholar]
- 48. Mohan V, Unnikrishnan R, Shobana S, Malavika M, Anjana RM, Sudha V. Are excess carbohydrates the main link to diabetes & its complications in Asians? Indian J Med Res. 2018;148:531‐538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Song S, Lee JE, Song WO, Paik HY, Song Y. Carbohydrate intake and refined‐grain consumption are associated with metabolic syndrome in the Korean adult population. J Acad Nutr Diet. 2014;114:54‐62. [DOI] [PubMed] [Google Scholar]
- 50. Vargas P. Dietary intake and obesity among Filipino Americans in New Jersey. J Environ Public Health. 2018;2018:6719861. doi: 10.1155/2018/6719861 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Sugihiro T, Yoneda M, Ohno H, Oki K, Hattori N. Associations of nutrient intakes with obesity and diabetes mellitus in the longitudinal medical surveys of Japanese Americans. J Diabetes Investig. 2019;10:1229‐1236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Chen JL, Weiss S, Heyman MB, Lustig R. Risk factors for obesity and high blood pressure in Chinese American children: maternal acculturation and children's food choices. J Immigr Minor Health. 2011;13:268‐275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Holmboe‐Ottesen G, Wandel M. Changes in dietary habits after migration and consequences for health: a focus on South Asians in Europe. Food Nutr Res. 2012;56:18891. doi: 10.3402/fnr.v56i0.18891 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Aoki Y, Yoon SS, Chong Y, Carroll MD. Hypertension, abnormal cholesterol, and high body mass index among non‐Hispanic Asian adults: United States, 2011–2012. NCHS Data Brief, no. 140. National Center for Health Statistics; 2014. [PubMed] [Google Scholar]
- 55. Bates LM, Acevedo‐Garcia D, Alegría M, Krieger N. Immigration and generational trends in body mass index and obesity in the United States: results of the National Latino and Asian American Survey, 2002–2003. Am J Public Health. 2008;98:70‐77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Shiwa M, Yoneda M, Nakanishi S, Oki K, Yamane K, Kohno N. Japanese lifestyle during childhood prevents the future development of obesity among Japanese‐Americans. PLoS One. 2015;10(3):e0120804. doi: 10.1371/journal.pone.0120804 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Tang JW, Mason M, Kushner RF, Tirodkar MA, Khurana N, Kandula NR. South Asian American perspectives on overweight, obesity, and the relationship between weight and health. Prev Chronic Dis. 2012;9:E107. doi: 10.5888/pcd9.110284 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Vu KTT, Cheah CSL, Sun S, Zhou N, Xue X. Adaptation and assessment of the Child Feeding Questionnaire for Chinese immigrant families of young children in the United States. Child Care Health Dev. 2020;46:74‐82. [DOI] [PubMed] [Google Scholar]
- 59. Ro A, Geronimus A, Bound J, Griffith D, Gee G. Cohort and duration patterns among Asian immigrants: comparing trends in obesity and self‐rated health. Biodemography Soc Biol. 2015;61:65‐80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Bray GA. Evaluation of obesity. Who are the obese? Postgrad Med. 2003;114:19‐38. [DOI] [PubMed] [Google Scholar]
- 61. McMurray RG, Soares J, Caspersen CJ, McCurdy T. Examining variations of resting metabolic rate of adults: a public health perspective. Med Sci Sports Exerc. 2014;46:1352‐1358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Wouters‐Adriaens MP, Westerterp KR. Low resting energy expenditure in Asians can be attributed to body composition. Obesity (Silver Spring). 2008;16:2212‐2216. [DOI] [PubMed] [Google Scholar]
- 63. Wadden TA, Webb VL, Moran CH, Bailer BA. Lifestyle modification for obesity: new developments in diet, physical activity, and behavior therapy. Circulation. 2012;125:1157‐1170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. Gulati S, Misra A. Abdominal obesity and type 2 diabetes in Asian Indians: dietary strategies including edible oils, cooking practices and sugar intake. Eur J Clin Nutr. 2017;71:850‐857. [DOI] [PubMed] [Google Scholar]
- 65. Kandula NR, Dave S, De Chavez PJ, et al. Translating a heart disease lifestyle intervention into the community: the South Asian Heart Lifestyle Intervention (SAHELI) study; a randomized control trial. BMC Public Health. 2015;15:1064. doi: 10.1186/s12889-015-2401-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66. Yeh MC, Heo M, Suchday S, et al. Translation of the Diabetes Prevention Program for diabetes risk reduction in Chinese immigrants in New York City. Diabet Med. 2016;33:547‐551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67. Shi YF, Pan CY, Hill J, Gao Y. Orlistat in the treatment of overweight or obese Chinese patients with newly diagnosed type 2 diabetes. Diabet Med. 2005;22:1737‐1743. [DOI] [PubMed] [Google Scholar]
- 68. Zhang F, Tang L, Zhang Y, Lü Q, Tong N. Glucagon‐like peptide‐1 mimetics, optimal for Asian type 2 diabetes patients with and without overweight/obesity: meta‐analysis of randomized controlled trials. Sci Rep. 2017;7:15997. doi: 10.1038/s41598-017-16018-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69. Kadowaki T, Isendahl J, Khalid U, et al. Semaglutide once a week in adults with overweight or obesity, with or without type 2 diabetes in an east Asian population (STEP 6): a randomised, double‐blind, double‐dummy, placebo‐controlled, phase 3a trial. Lancet Diabetes Endocrinol. 2022;10:193‐206. [DOI] [PubMed] [Google Scholar]
- 70. Saxon DR, Iwamoto SJ, Mettenbrink CJ, et al. Antiobesity medication use in 2.2 million adults across eight large health care organizations: 2009‐2015. Obesity (Silver Spring). 2019;27:1975‐1981. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71. Apovian CM, Aronne LJ, Bessesen DH, et al. Pharmacological management of obesity: an Endocrine Society clinical practice guideline. J Clin Endocrinol Metab. 2015;100:342‐362. [DOI] [PubMed] [Google Scholar]
- 72. Jensen MD, Ryan DH, Apovian CM, et al. 2013 AHA/ACC/TOS guideline for the management of overweight and obesity in adults: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines and The Obesity Society. Circulation. 2014;129(25 suppl 2):S102‐S138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73. Ji G, Li P, Li W, et al. The effect of bariatric surgery on Asian patients with type 2 diabetes mellitus and body mass index < 30 kg/m2: a systematic review and meta‐analysis. Obes Surg. 2019;29:2492‐2502. [DOI] [PubMed] [Google Scholar]
- 74. Al‐Sumaih I, Nguyen N, Donnelly M, Johnston B, Khorgami Z, O'Neill C. Ethnic disparities in use of bariatric surgery in the USA: the experience of Native Americans. Obes Surg. 2020;30:2612‐2619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75. Ohta M, Seki Y, Wong SK, et al. Bariatric/metabolic surgery in the Asia‐Pacific region: APMBSS 2018 survey. Obes Surg. 2019;29:534‐541. [DOI] [PubMed] [Google Scholar]
- 76. American Diabetes Association . 2. Classification and diagnosis of diabetes: Standards of Medical Care in Diabetes‐2021 . Diabetes Care. 2021;44(suppl 1):S15‐S33. [DOI] [PubMed] [Google Scholar]
- 77. National Center for Health Statistics . Prevalence of high BMI among non‐Hispanic Asian adults, by sex, age, education, and foreign‐born status: United States, 2011–2012. Accessed July 1, 2021. https://www.cdc.gov/nchs/data/databriefs/db140_table.pdf#5
- 78. McEligot AJ, Mitra S, Beam W. The association between fitness and obesity in diverse multi‐ethnic college students. J Am Coll Health. 2021;69:290‐297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79. Ogden CL, Carroll MD, Fryar CD, Flegal KM. Prevalence of obesity among adults and youth: United States, 2011–2014. NCHS Data Brief, no. 219. National Center for Health Statistics; 2015. [PubMed] [Google Scholar]
- 80. Sa J, Cho BY, Chaput JP, et al. Sex and racial/ethnic differences in the prevalence of overweight and obesity among U.S. college students, 2011–2015. J Am Coll Health. 2021;69:413‐421. [DOI] [PubMed] [Google Scholar]


