Abstract
Dual left anterior descending artery (or dual anterior interventricular artery) is a rare coronary anomaly. It is important to know the anatomic variants of this anomaly in patients with coronary artery disease who are undergoing either surgical myocardial revascularization or coronary angioplasty.
We report the cases of 4 patients who had anatomic variants of dual left anterior descending coronary artery. These patients had developed coronary artery disease in the long or the short left anterior descending artery, or in both. The long left anterior descending artery was diseased in 1 patient, and the short left anterior descending artery was diseased in another. In the 3rd and 4th patients, both the long and the short arteries were atherosclerotic and had developed severe stenosis.
All 4 patients underwent successful myocardial revascularization. There was no electrocardiographic evidence of perioperative myocardial infarction. All patients were asymptomatic during the follow-up period, which ranged from 3 months to 1.5 years.
Angiographers and surgeons alike must be aware of the variants of dual left anterior descending coronary artery, so that the diseased vessels can be correctly identified even if 1 of the dual arteries is 100% occluded.
Key words: Coronary artery bypass grafting, coronary disease/radiography, coronary vessel anomalies/radiography, coronary vessels/surgery, dual left anterior descending coronary artery, myocardial revascularization
Coronary artery anomalies occur in 0.64% to 1.3% of patients undergoing coronary arteriography. 1,2 Variations in origin, course, and distribution of the left anterior descending coronary arteries (LADs) are rare, even though such variations are fairly common in the right coronary artery. 3,4 Morettin 5 reported complete duplication of a coronary artery or one of its branches in approximately 1% of his cases. According to Spindola-Franco and colleagues, 6 the incidence of dual LAD (also called dual anterior interventricular artery) in otherwise normal hearts is about 1%. This anomaly is found relatively often in conjunction with congenital malformations such as complete transposition of the great arteries and tetralogy of Fallot. In patients with tetralogy of Fallot, the origin of the LAD from the right coronary artery is particularly important, since the LAD courses the potential site of surgical reconstruction.
As described by Spindola-Franco's group, 6 the anomaly known as dual LAD can be recognized by an early bifurcation of the proximal LAD (the LAD proper). Of the resulting 2 vessels, one is too short to reach the apex; this “short LAD” stays in the anterior interventricular sulcus (AIVS). The other, the “long LAD,” travels to the apex, 1st along the AIVS, then leaving it, and then reentering the distal AIVS. However, 1 relatively frequent variation consists of a long LAD that arises not from the LAD proper but from the right coronary artery. In this case, the short LAD arises from the LAD proper as described above, and the long LAD courses outside the AIVS until it enters the distal AIVS. The LAD proper is defined as that portion of the LAD that starts at the bifurcation of the left main stem and is so called until its level of bifurcation.
Spindola-Franco and co-authors 6 also provided an angiographic description of the important variants of dual LAD as follows:
Type I. Running in the AIVS, the short LAD is generally the source of all the major proximal septal perforators. The long LAD also runs in the AIVS, descending on the left ventricular side of the AIVS, and then reentering the distal AIVS.
Type II. The short LAD is the same as in Type I. The long LAD is different only in that it descends on the right ventricular side, rather than the left, before reentering the AIVS. Types I and II are very similar. They can be better differentiated from one another angiographically in the left anterior oblique (LAO) view than in the right anterior oblique view (RAO).
Type III. The short LAD is consistent with that described in Types I and II. The long LAD travels intramyocardially in the ventricular septum. This vessel is most visible in 2 angiographic projections: RAO and lateral.
Type IV. High in the AIVS, a very short vessel is formed by the LAD proper and the short LAD. From this vessel, the major septal perforators, as well as the diagonal branches, originate. The long LAD is unusual in its origin, arising from the right coronary artery.
These authors have also provided a discussion of the surgical importance of dual LAD. 6
Patients and Methods
From April 1996 through April 1999, 3,070 patients underwent coronary angiography at our institution. Of these, 4 patients had a dual LAD and coronary artery disease that required surgical myocardial revascularization (Table I).
Table I. Variants of the Dual LAD System and Description of Treatment in 4 Patients
Patient 1
A 60-year-old man presented at our institution with history of angina. He was evaluated by use of coronary angiography, which showed 70% to 80% stenosis of the distal part of the left main coronary artery. This patient had a dual LAD, in which the short LAD arose from the left main, and the long LAD arose from the proximal right coronary artery. The mid portion of the right coronary artery had 80% to 90% stenosis, the short LAD had minimal stenosis, and the ramus intermedius showed 80% stenosis. The left circumflex artery was small and normal (Figs. 1A-D).
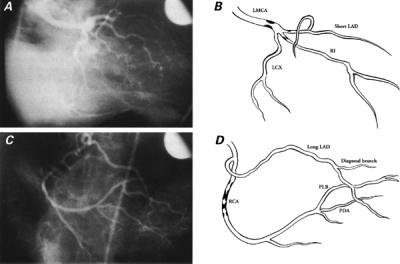
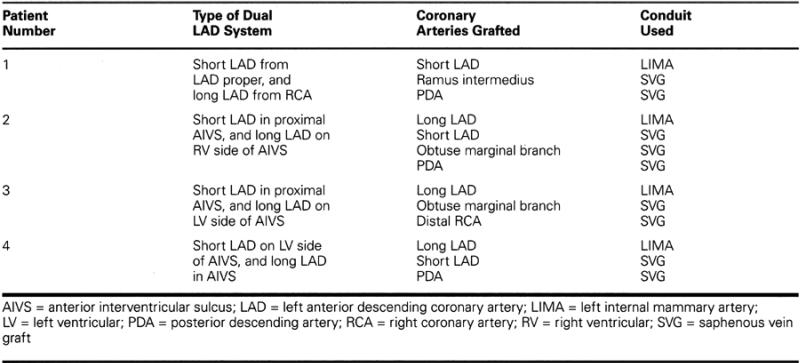
Fig. 1 A) Coronary angiogram of the LCA in the right anterior oblique projection, showing the short LAD arising from the left main. Stenosis of the LMCA and the ramus intermedius is evident. B) Diagrammatic representation of Fig. 1A. C) Angiographic view of the RCA in the right anterior oblique projection showing the origin of the distal LAD from the proximal RCA and stenosis of the mid portion of the RCA. D) Diagrammatic representation of Fig. 1C.
LAD = left anterior descending coronary artery; LCA = left coronary artery; LCX = left circumflex artery; LMCA = left main coronary artery; PDA = posterior descending coronary artery; PLB = posterolateral branch; RCA = right coronary artery; RI = ramus intermedius
The patient underwent coronary artery bypass grafting of 3 vessels, with anastomosis of the left internal mammary artery (LIMA) to the short LAD, and saphenous vein grafts to the ramus intermedius and the posterior descending coronary artery. We recognized this dual LAD anomaly (Type IV) perioperatively when we found a Type III LAD despite angiographic evidence of a Type I LAD. We exposed the short LAD very proximally in the AIVS and made an arteriotomy. When we probed the LAD distally with a 1-mm probe, the probe did not reach the LAD in the distal part of the AIVS. After we created the LIMA anastomosis to the short LAD, blood flowed only to the proximal LAD and to the 1st diagonal branch. After we released the aortic cross-clamp, however, the distal (long) LAD filled with bright red blood. Later, reviewing the coronary angiogram, we could appreciate this LAD anomaly. In 1939, Waterston and colleagues 7 reported the case of Sir James Mackenzie, who had the same arrangement of dual anterior interventricular arteries in addition to ischemic heart disease.
Patient 2
A 51-year-old man presented at our institution with a history of exertional angina. He was evaluated by use of coronary angiography, which showed a dual LAD pattern. The long LAD was 100% occluded immediately below its origin, and the short LAD had 95% discrete stenosis. The left circumflex artery showed 60% stenosis proximal to the origin of the 1st obtuse marginal branch (Figs. 2A-B). The right coronary artery showed multiple stenoses in the middle segment.
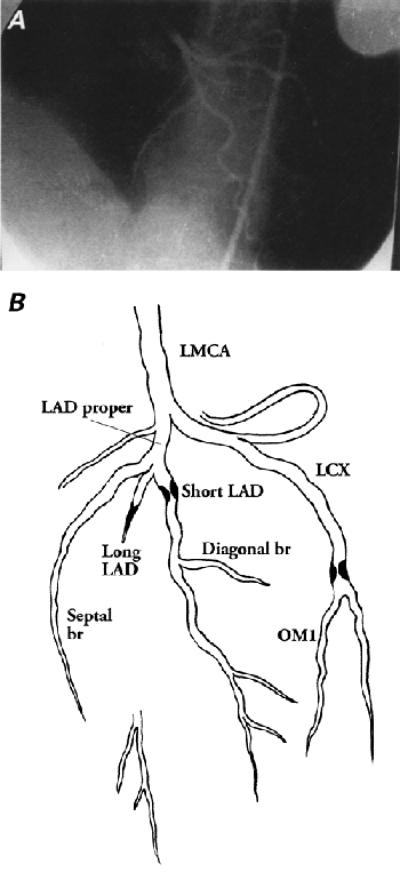
Fig. 2 A) Angiogram of the LCA in the left anterior oblique projection, showing 100% stenosis of the long LAD, severe stenosis of the short LAD, and stenosis of the LCA proximal to the origin of the obtuse marginal branch. The septal artery originates from the LAD proper. B) Diagrammatic representation of Fig. 2A.
br = branch; LAD = left anterior descending coronary artery; LCA = left coronary artery; LCX = left circumflex artery; LMCA = left main coronary artery; OM1 = 1st obtuse marginal branch
The patient underwent quadruple coronary artery bypass grafting with anastomosis of the LIMA to the long LAD, and saphenous vein grafts to the short LAD, the obtuse marginal artery, and the posterior descending artery. Preoperatively, we had viewed the coronary angiogram and thought that the patient had Type I LAD, with small-caliber vessels and severe stenosis. However, during surgery, we found a 2.5-mm-caliber long LAD in the distal AIVS. Moreover, after the arteriotomy, a 2-mm coronary probe easily entered the proximal LAD. We saw another vessel in the mid portion of the AIVS that resembled a short LAD morphologically and was recognizable as such on the angiogram. We also noticed that the long LAD descended on the right ventricular side of the AIVS, and we therefore classified this as a Type II anomaly.
Patient 3
A 58-year-old man presented with a history of exertional angina. Coronary angiography revealed a dual LAD pattern, which was thus identified preoperatively. Both the short and the long LAD had 60% to 70% stenosis proximally. The 1st obtuse marginal branch had 75% stenosis (Figs. 3A-B). A long segment of the proximal right coronary artery showed 70% stenosis.
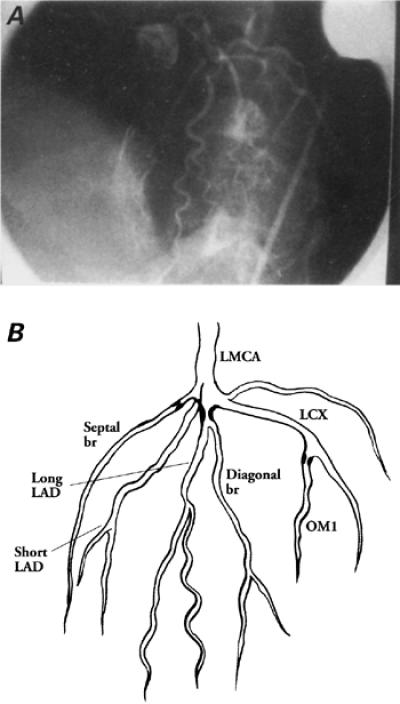
Fig. 3 A) Angiogram of the LCA in the left anterior oblique projection, showing stenosis of the short and the long LAD. The long LAD gives rise to the diagonal branches, and the short LAD gives rise to the septal branch. There is stenosis in the 1st obtuse marginal branch. B) Diagrammatic representation of Fig. 3A.
br = branch; LAD = left anterior descending coronary artery; LCA = left coronary artery; LCX = left circumflex artery; LMCA = left main coronary artery; OM1 = 1st obtuse marginal branch
The patient underwent a triple bypass with anastomosis of a LIMA to the long LAD, and saphenous vein grafts to the 1st obtuse marginal branch and the distal right coronary artery. Intraoperatively, we noticed that the long LAD descended on the left ventricular side of the AIVS. Therefore, we classified this as a Type I anomaly.
Patient 4
A 46-year-old man presented with an acute inferior wall myocardial infarction. He was evaluated by use of coronary angiography, which showed a Type II anomaly. Both the short and the long LAD showed severe stenosis at their origins (Fig. 4). The posterior descending branch of the right coronary artery showed 99% occlusion. The patient underwent a triple bypass with anastomosis of the LIMA to the long LAD, and saphenous vein grafts to the short LAD and the posterior descending artery.
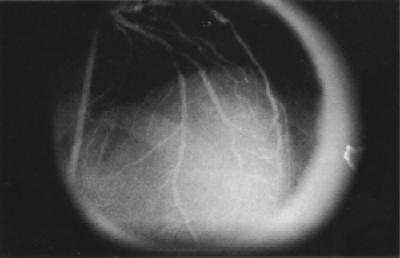
Fig. 4 Angiogram of the LCA, showing stenosis of the long and the short LAD. The long LAD gives rise to all the septal branches throughout and to 1 diagonal branch in the distal third. The short LAD gives rise to diagonal branches only.
LAD = left anterior descending coronary artery; LCA = left coronary artery
Results
The incidence of a dual LAD arrangement in our series of 3,070 patients was 0.13% (4 patients). In all 4, myocardial revascularization was successful. There was no electrocardiographic evidence of perioperative myocardial infarction. The patients were asymptomatic during the follow-up period, which ranged from 3 months to 1.5 years.
Discussion
Although anomalies associated with the origin, course, branching pattern, and distribution of the coronary arteries have been described in autopsy specimens, these findings have become more relevant since the widespread application of coronary arteriography and surgical revascularization for atherosclerotic coronary artery disease. Clearly, these technical advances make it necessary for all angiographers and cardiac surgeons to be familiar with the variants of dual LAD, because accurate identification and delineation of the coronary arteries in the presence of coronary artery disease is integral to proper surgical revascularization of the myocardium. Variants of the dual LAD pattern have been identified in 1% of all patients undergoing selective coronary angiography, who had otherwise normal hearts. 4
Awareness of dual LAD can increase surgical precision. For example, when a short LAD is being grafted, the vessel must be exposed higher in the anterior AIVS. When a diseased long LAD is identified in the AIVS, complete revascularization can be achieved with less risk of postoperative myocardial infarction. Familiarity with dual LAD variants can also help the surgeon avoid an incorrectly placed arteriotomy. For example, in our 1st patient, the arteriotomy could have been made inadvertently in the distal LAD and the unobstructed long LAD would have been revascularized, leaving the obstructed short LAD intact. Postoperatively, this would likely have led to ischemia or infarction in the short LAD territory. The case of our 2nd patient illustrates that if only 1 of the 2 LADs has 100% ostial stenosis, particular care must be taken to revascularize the correct vessel.
It is often difficult to identify a short LAD, because it descends in the proximal part of the AIVS and sometimes runs deep within the epicardial fat or within the myocardium. The vessel cannot be traced proximally by opening the LAD at the apex and probing proximally with coronary probes, because the short LAD doesn't reach the apex. In our 4 patients, we identified a short LAD proximally, high in the AIVS, where it was crossed consistently by a small vein that drained into the anterior cardiac vein to the left of the LAD. To recognize the vessels of a dual LAD intraoperatively, the surgeon must remember the morphology of the diseased coronary arteries. If there is any gross disparity between the expected morphology of the vessel and that which is encountered perioperatively, it is worthwhile to review the coronary angiogram again.
In conclusion, our case reports of 4 patients with dual LAD emphasize that familiarity with this anomaly and its variants is a necessity for every angiographer and cardiac surgeon. A detailed angiographic description of important variants of dual LAD, along with the surgical implications, is available in a 1983 publication by Spindola-Franco and colleagues. 6
Acknowledgment
We are grateful to Professor Robert H. Anderson, BSc, MD, FRC, Path, of the Imperial College School of Medicine, National Heart & Lung Institute, London, for his encouragement and assistance in preparing this manuscript.
Footnotes
Address for reprints: Lokeswara Rao Sajja, MCh, FACS, Medwin Heart Institute, Medwin Hospitals, Raghava Ratna Towers, Chirag ali Lane, Hyderabad 500 001, A.P., India
References
- 1.Yamanaka O, Hobbs RE. Coronary artery anomalies in 126,595 patients undergoing coronary arteriography. Cathet Cardiovasc Diagn 1990:21;28–40. [DOI] [PubMed]
- 2.Kimbiris D, Iskandrian AS, Segal BL, Bemis CE. Anomalous aortic origin of coronary arteries. Circulation 1978: 58;606–15. [DOI] [PubMed]
- 3.Chaitman BR, Lesperance J, Saltiel J, Bourassa MG. Clinical, angiographic, and hemodynamic findings in patients with anomalous origin of the coronary arteries. Circulation 1976:53;122–31. [DOI] [PubMed]
- 4.Baltaxe HA, Wixson D. The incidence of congenital anomalies of the coronary arteries in the adult population. Radiology 1977:122;47–52. [DOI] [PubMed]
- 5.Morettin LB. Coronary arteriography: uncommon observations. Radiol Clin North Am 1976:14;189–208. [PubMed]
- 6.Spindola-Franco H, Grose R, Solomon N. Dual left anterior descending coronary artery: angiographic description of important variants and surgical implications. Am Heart J 1983:105;445–55. [DOI] [PubMed]
- 7.Waterston D, Orr J, Cappell DF. Sir James Mackenzie's heart. Br Heart J 1939:1:237–48. [DOI] [PMC free article] [PubMed]


