Abstract
Background:
Alzheimer’s disease and Alzheimer’s disease related dementias (AD/ADRD) research typically requires participants to enroll with a “study partner” (SP). Little is known about what predicts who steps into the SP role or whether the SP’s relationship to the participant affects their reports of disease severity.
Methods:
Health and Retirement Study data (HRS), collected prior to the Aging, Demographics and Memory Study (ADAMS), was used to identify sociocultural factors that predict who serves as a SP in ADAMS. SP-reported outcomes were compared between three types of participant-SP relationships: spousal, adult child, and other.
Results:
Spouses (35%) and adult children (39%) were similarly likely to serve as SPs. Factors predicting who served differed. In multivariable analyses, adult children rated participants less impaired than spouses on measures of memory, judgment, and organizational abilities (p < .05).
Conclusions:
The participant-SP relationship has independent effects on the SP’s reports of the severity of cognitive impairments.
Keywords: study partners, informants, alzheimer’s, dementia, research
Introduction
Participants in Alzheimer’s disease and Alzheimer’s disease related dementias (AD/ADRD) research are often required to enroll as part of a dyad composed of the participant and the participant’s “study partner” (SP). SPs act as knowledgeable informants, providing investigators with insights into the participant’s cognition, function, and wellbeing—insights that often inform eligibility assessments as well as measurement of study outcomes (Ferris et al., 2006; Grill & Karlawish, 2017; Morris et al., 1997). Moreover, SPs influence participants’ enrollment decisions, attendance at study visits, and trial completion (Black et al., 2014; 2018; Grill & Karlawish, 2017; Karlawish et al., 2001; Nuño et al., 2019). They have been identified as essential collaborators as well as ethically significant figures in AD/ADRD research.
Yet, while the importance of the SP role is widely acknowledged, relatively little is known about how SPs are chosen or about how a SP’s relationship to the participant might affect their reports on the participant’s cognition and function. Knowing the factors that predict who steps into the SP role and how a SP’s relationship to the participant affects the SP’s insights may help inform recruitment strategies and ensure the validity of AD/ADRD research.
In understanding how SPs are chosen, we must ask which sociocultural characteristics make certain types of SP-relationships more likely. Sociocultural characteristics are forces within a society that influence the thoughts, feelings, and beliefs of individuals, as well as how one behaves, such as deciding to serve as a SP (Adams & Markus, 2004). Understanding this may help advance understanding of the sociocultural factors that facilitate or hinder AD/ADRD research participation. For example, prior work suggests that structural barriers exist to the participation of some individuals as study partners and this contributes to the lack of racial representativeness in AD/ADRD research (Manly et al., 2021; Wilkins et al., 2020).
Until recently, research that involved persons living with dementia often relied on caregivers to serve as SPs (Cary et al., 2015). Thus, clinical characteristics related to severity of impairment and sociocultural characteristics that are correlates of being a caregiver were understood to be correlates of serving as a SP. Research has shown spouses often serve as caregivers for persons living with dementia, and, in the absence of a spouse, an adult child (Grill et al., 2012, 2013). Thus, spouses and adult children are typically SPs in studies that enroll persons living with dementia. Notably, compared to spouses, adult children more often face logistical barriers to serving as a SP—for instance, having young children, being employed full time, and living apart from the participant (Grill et al., 2012, 2013). Consistent with this, adult children are more likely to view the SP role as burdensome (Conde-Sala et al., 2010). As a result, we hypothesized not having a spouse and having more living children would predict that an adult child would serve as SP.
In recent years, AD/ADRD research has expanded to include persons who do not presently have dementia but are at increased risk of developing dementia in the future. Unlike research that involves persons living with dementia, in which a caregiver typically steps into the SP role (Cary et al., 2015), persons who are cognitively unimpaired do not typically have caregivers. Stated otherwise, there is no default person to step into the SP role. This can be a barrier to participation in AD/ADRD research, which typically requires a participant to co-enroll with a SP (Largent et al., 2018). Thus, it may be useful to study who becomes a study partner of an older adult, regardless of whether they have dementia or not. The same sociocultural characteristics that influence who serves as SPs for individuals with dementia might foreshadow who serves as SP for persons who are not cognitively impaired. If they do, they might also be expected to influence who does or does not have a SP and, therefore, who is or is not eligible for research participation.
A second important question is whether the type of participant-SP relationship influences how the SP reports on the participant’s cognition and function. Prior studies have focused on how closely SPs’ reports correspond to participants’ cognitive testing data (Nuño et al., 2019; Ready et al., 2004). Findings from these studies prioritize spousal SP reports over adult child reports as more closely corresponding to a participant’s performance on cognitive testing. No published studies have directly compared SP-reported outcomes between relationship types: spousal, adult child, and other.
Such direct comparison is important given that data provided by SPs can inform study outcomes, it is important to understand how SP reporting varies across types of SPs, as this may offer information about threats to validity in AD/ADRD research. If differences exist by relationship type, researchers may be able to develop statistical methods to accommodate reporting differences. We expect, for example, that adult child SPs might underestimate a participant’s cognitive and functional problems (i.e., rate them less impaired) because they are more likely than spouses to live apart from participants, observing them less frequently and under differing conditions than do spouses (Grill et al., 2012, 2013).
Additionally, the results of direct comparisons may foster practices that promote sociocultural diversity in AD/ADRD research. A proposition of prior studies that compare SP-reports to cognitive test performance is that one type of SP—a spousal study partner—is preferred over another. But, the fewer requirements that are imposed on who can serve as a SP, the broader the pool of potential AD/ADRD research participants. Understanding how SP reports compare, and developing adjustments if necessary, may reduce the restrictions on who can serve as a SP. In addition, prior studies use cognitive testing data as the comparator for SP reporting. Cognitive testing has limitations that can differentially impact individuals from certain ethnoracial groups and other groups underrepresented in AD/ADRD research (Barnes, 2021; González et al., 2021; Gross et al., 2015). Direct comparison of SP reports is essential to remove the influence of this potentially intervening variable.
The purpose of this study was to examine sociocultural and clinical characteristics that predict the participant-SP relationship and to compare how differences in the participant-SP relationship impact on SP-reported outcomes. The Health and Retirement Study (HRS) is a longitudinal cohort study of a representative sample of American adults over age 50; the Aging, Demographics and Memory Study (ADAMS) is a longitudinal study of cognition (Crimmins et al., 2011). ADAMS recruited HRS panel members ages 70 and older and, for each panel member, a SP. We analyzed data from HRS and ADAMS. We hypothesized that (H1) not having a spouse and having more living children would predict that an adult child served as a participant’s SP and that (H2) adult children would rate participants’ cognition and function as less impaired than spouses would.
Methods
Sample Selection
Older adults ages 70 and older with a range of cognitive function from typical to moderately clinically impaired were recruited from the HRS to participate in ADAMS (N = 730). To participate in the ADAMS, the older adults had to identity an individual to serve as their SP. Given the older adult was the primary focus in the ADAMS, we refer to this individual as the “participant” and the individual who co-participated with them as the SP. All individuals enrolled into ADAMS were eligible for the current study, which included 730 participant-SP dyads. For these individuals, we analyze data from both HRS and ADAMS.
Measures
Sociocultural variables include basic demographic data for participants and SPs as well as more detailed data about relationship statuses and living arrangements. Demographic data (i.e., age, sex/gender, and years of education) were collected for participants and their SPs in both HRS and ADAMS. These data allowed classification of three exclusive groups defined by SP’s relationship to the participant: Spousal, Adult Child, and Other. The “Other” category was an aggregate of many other relationships that were not either spousal or adult child and that had cell sizes insufficient to include in the analysis as independent groups. Detailed records of participants’ living, legal and biologic, relatives—including spouses, adult children, and other relatives—were available in HRS data, which were collected prior to ADAMS. The records permitted estimation of: number of siblings; indicator variables for presence of spouse, one or more brothers, one of more sisters; number of children; number of living children, number children living within 10 miles of participant; youngest child’s age; indicator variables for one or more living daughters, and one or more living sons. Spouse self-rated health was a single-item rating of health status on a 5-point scale from excellent (5) to poor (1).
During the initial ADAMS interview, participants completed cognitive testing and SP-reported clinical measures were gathered. SPs reported on participants’ cognition. The Blessed Dementia Rating Scale (BDRS) is a 22-item measure of 2-year change in the individual’s cognition (Blessed et al., 1968). Items ask about changes in performance of everyday activities like using money and finding one’s way (8 items), changes in behaviors like eating and dressing (3 items), and changes in personality, interests, and drive like rigidity in thinking and affect (11 items). Scores on the BDRS range from 0 to 28; higher numbers indicate greater loss in functional capacity. SPs also completed three single-item questions (Crimmins et al., 2011; Ofstedal et al., 2005). Response options for each of the single-item questions range from “excellent” (1) to “poor” (5). Participants’ current memory was assessed by asking: “How would you rate your friend or relative’s memory at the present time?” This question has been shown to discriminate between individuals who are and are not cognitively impaired (Ayalon, 2011). Judgment was assessed by asking: “How would you rate your friend or relative in making judgments and decisions?” Organization was assessed by asking: “How would you rate your friend or relative’s ability to organize his/her daily activities?” The single-item questions pertaining to judgment and organization have been shown to discriminate between persons with dementia and cognitively typical persons (Jorm, 1994; Jorm et al., 1989; Jorm & Jacomb, 1989).
By including these multiple discrete measures in our analyses, we aimed to include items that could capture impairment across a continuum of symptoms. In addition, while we had no formal hypotheses, we were interested to learn whether SPs demonstrated predictable patterns in how they assessed domains of an individual’s cognitive function (i.e., memory, judgment, and organization).
SPs completed four measures about the participant’s function (Adams Questionnaires, 2020). Activity level was assessed through informant ratings for 10 items, where higher scores reflect more activity. SPs completed Instrumental Activities of Daily Living (IADL) and Basic Activities of Daily Living (BADL) questionnaires about the participant. The IADL questionnaire contains five items that evaluate the participant’s ability to complete tasks such as preparing meals and shopping for groceries; higher scores indicate more impairment (Fillenbaum, 1985). The BADL questionnaire contains six items that evaluate the participant’s ability to complete tasks such as getting across a room, dressing, and bathing; higher scores indicate more impairment (Katz et al., 1963). Impairments in IADLs are expected to present earlier in the disease course, while impairments in BADLs are anticipated later in the course. Finally, a caregiving questionnaire asked about limits of the participant’s cognition and function and the SP’s experience providing care to the participant.
We included SP-reported measures of both cognition and function as these are common endpoints in AD/ADRD research. We included multiple measures that capture varying domains of cognition and function that can be affected across differing stages of impairment.
Participants underwent a battery of psychological tests. Global cognition was assessed using the Mini Mental Status Exam (MMSE), a 30-point test where higher scores reflect better cognitive function (Brandt et al., 1988; Folstein et al., 1975). The CERAD Boston Naming test was used to assess participants’ word finding ability (Kaplan et al., 1978; Morris et al., 1989). Trail Making Test, Parts A and B were used to assess executive function (Reitan, 1992). Serial 7s, counting down from one hundred by sevens, was used to assess attention (Brandt et al., 1988). Animal Naming was used to assess category fluency (Isaacs & Kennie, 1973).
We included measures of cognitive testing to capture differences between groups in cognitive function that could be expected to influence SP-reporting. We incorporated multiple measures to capture differences in global cognition as well as varying domains of cognition that can be affected across differing types and stages of cognitive impairment.
Statistical Analyses
We used a two-part approach to examine effects of participant-SP relationships defined as: Spousal, Adult Child, and Other. First, we examined characteristics that predicted being a SP. In these analyses, bivariate and multivariable regression models were used to analyze data from 730 SPs and their respective participants. Three distinct models were built to identify characteristics that predicted each participant-SP relationship. The statistical universe for each model was defined by the outcome (i.e., models predicting spousal SPs were defined by a universe of participants with spouses). Candidate covariates included: participant age, sex/gender, years of education, IADL score, BADL score, number of siblings, brother, sister, spouse present, spouse self-rated health, number of children, number children in <10 miles, and number of living children, youngest child age, living daughter, living son. Models were built using forward stepwise regression with alpha-to-keep of 0.05. Covariates that were conceptually contraindicated in a model were dropped; however, post-hoc testing showed that had they not been dropped for conceptual reasons they would have been dropped for not meeting the alpha-to-keep. In models predicting spousal SPs, for example, only participants with spouses were included. Thus, the covariate indicating whether a spouse was present was conceptually contraindicated.
Second, we conducted cross-sectional between-group comparisons to estimate mean effects of the participant-SP relationship on SP-reported outcomes. In these analyses, bivariate regression models were used to analyze data from participant-SP dyads. All participants with SP-reported outcome data were included in these analyses (N = 714). Logistic and linear regression were used for binary and continuous outcomes, respectively. To control for differences between groups in cognition and function that could be expected to influence SP-reporting, multivariable models were built using forward stepwise regression with alpha-to-keep of 0.15. Candidate covariates included the following clinical instruments: MMSE, Trails A, Trails B, IADL, BADL, Serial 7s, Boston Naming, and Animal Fluency.
p < .05 defined statistical significance. 95%CIs that do not overlap denote statistical significance. 95%CIs of mean differences that exclude zero denote statistical significance. Analyses were conducted in Stata 16.0.
Results
Sample Characteristics
Participants were mostly White (79.2%), women (58.1%), with a mean age of 82 years and a mean MMSE score of 21.7 (Table 1). SPs were mostly White (75.8%), women (74%), with a mean age of 63.3 years. SPs identified as spouses (34.9%), adult children (38.5%), or persons with some other relationship to the participant (26.6%). About half of SPs (51%) lived with the participant.
Table 1.
Characteristics of Study Partners and Primary Participants.
| Characteristic | Respondent (N = 730) |
|---|---|
| Study Partner | |
| Age (years), mean (SD) | 63.3 (14.4) |
| Women, % (n) | 74.0 (531) |
| White, Non-Latino, % (n) | 75.8 (543) |
| Education, % (n) | |
| < High school | 18.4 (134) |
| High school/GED or less | 30.3 (221) |
| Some college or 2-year degree | 27.5 (201) |
| 4-year college degree or beyond | 23.8 (174) |
| Lives with participant, % (n) | 51.0 (370) |
| Relationship to participant, % (n) | |
| Spouse | 34.9 (255) |
| Child | 38.5 (281) |
| Othera | 26.6 (194) |
| Caregiver to participant,b % (n) | 34.0 (255) |
| Length of time providing care, % (n) | |
| Up to 6 months | 12.0 (28) |
| 6–12 months | 12.4 (29) |
| 12–24 months | 23.1 (54) |
| >24 months | 52.6 (123) |
| Primary Participant | |
| Age, mean (SD) | 82.0 (7.1) |
| women, % (n) | 58.1 (424) |
| White, Non-Latino, % (n) | 79.2 (578) |
| Education, % (n) | |
| < High school | 50.6 (369) |
| High school/GEDc | 23.8 (174) |
| Some college or 2-year degree | 14.3 (104) |
| 4-year college degree or beyond | 11.4 (83) |
| Cognitive status, % (n) | |
| Dementia | 43 (314) |
| Mild impairment | 11 (81) |
| Cognitively typical | 46 (335) |
| Mini-mental status exam (MMSE),d mean (SD) | 21.7 (7.2) |
| Number living siblings, mean (SD) | 0.8 (2.2) |
| Number children,e mean (SD) | 3.4 (2.6) |
| Number spouses (lifetime), mean (SD) | 1.2 (0.6) |
Note. Column percentages may not total 100 due to rounding. SD = standard deviation.
14 unknown
Asked respondent about providing or supervising care for a friend or relative in past month. Care was defined by actively helping with Activities of Daily Living.
GED = General Education Diploma.
Scores have a possible range of 0–30.
of whom respondent is in contact.
Most participants who had a living spouse also had at least one adult child though the reciprocal was not observed; many participants with adult child(ren) did not have living spouses (Figure 1a). More adult children identified as caregivers of participants than did spousal SPs (Figure 1b). The statistical models were constructed to be interpreted in the context of these patterns.
Figure 1.
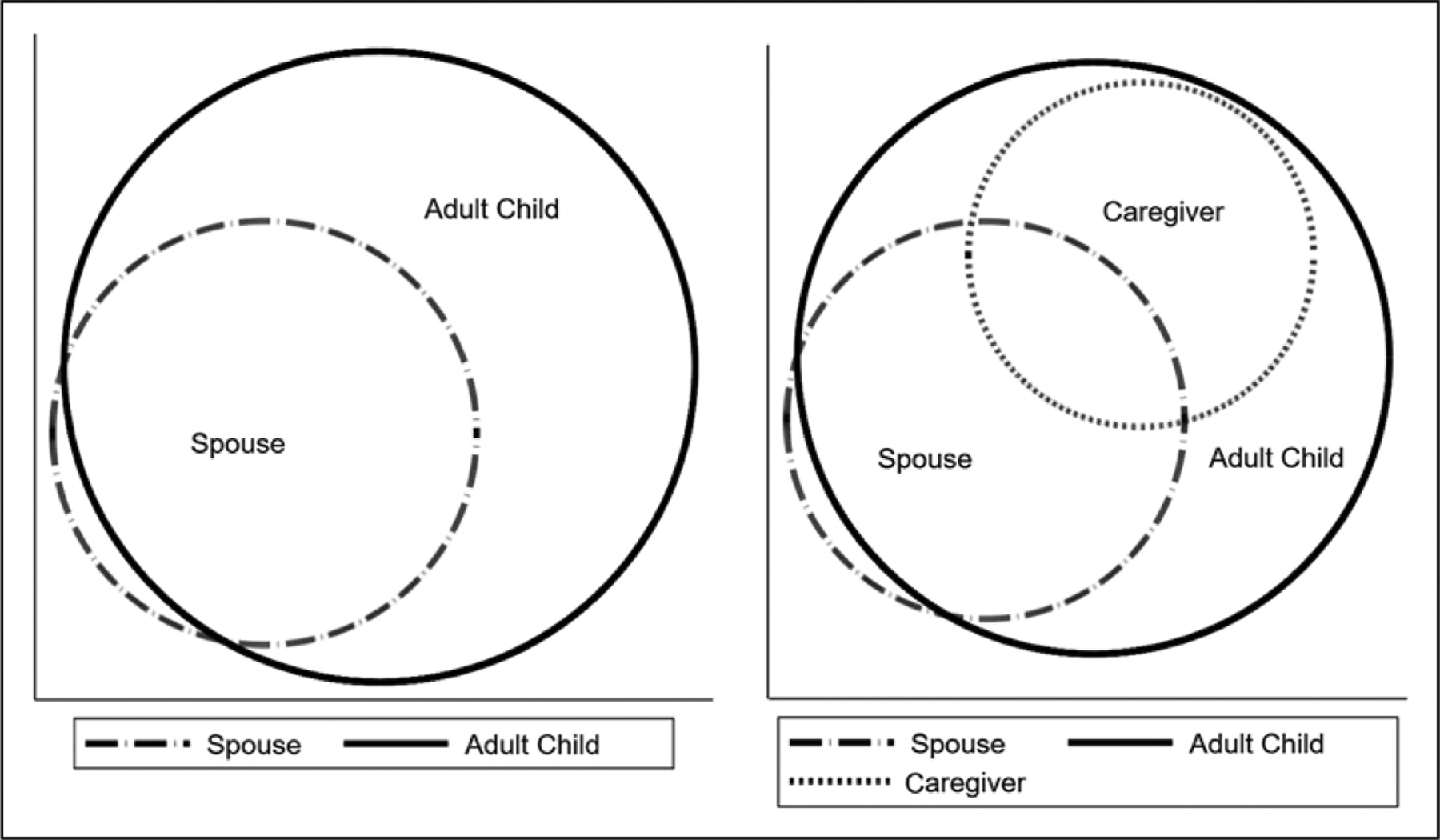
Venn Diagram of (a) relationship between participants with living spouses and adult children and (b) relationship among participants with living spouses and adult children who also identify as caregivers of the participants.
Sociocultural and Clinical Predictors of the Participant-SP Relationship
Among participants with spouses, older age and no living sister predicted that a spouse was more likely to serve as SP in a multivariable analysis (both p < .05). To examine our hypothesis (H1) that not having a spouse and having more living children would predict that an adult child served as SP, we conducted an analysis of participants with adult children. In these multivariable analyses, we found being a woman, being older, having more children, more impairments in IADLS, and not having a spouse predicted that an adult child was more likely to serve as SP (all p < .05).
Among all participants, not having a spouse, not being a woman, and more years of education predicted that a person other than a spouse or adult child was more likely to serve as SP in a multivariable analysis (all p < .05). In the same multivariable analysis, more children and no living daughter also predicted that a person other than a spouse or adult child was more likely to serve as SP (all p < .05, Table 2).
Table 2.
Participant Sociocultural and Clinical Predictors of Study Partner (SP) Relationship (N = 730).
| Bivariate Model OR (95%CI) | Full Model OR (95%CI) | |
|---|---|---|
| Spousal SP | (N = 323) | (N = 323) |
| Spouse self-rated healtha | 0.61 (0.40–0.95)*** | 0.68 (0.41–1.13) |
| Age | 1.35 (1.14–1.60)*** | 1.19 (1.00–1.41)* |
| Woman | 0.83 (0.32–2.16) | |
| Years of education | 1.11 (1.00–1.23) | 1.01 (0.88–1.16) |
| IADLb | 0.98 (0.75–1.29) | |
| BADLc | 0.89 (0.70–1.15) | |
| Brother | 0.12 (0.04–0.32)*** | 0.49 (0.15–1.58) |
| Sister | 0.09 (0.03–0.26)*** | 0.27 (0.08–0.93)* |
| Number of children | 0.85 (0.77–1.08)* | 0.87 (0.72–1.04) |
| Adult Child SP | (N = 675) | (N = 616) |
| No spouse | 17.40 (6.97–43.43)*** | 11.96 (2.07–69.16)** |
| Age youngest childd | 0.97 (0.89–1.06) | |
| Living daughter | 0.12 (0.06–0.24)*** | 0.95 (0.15–6.19) |
| Living son | 0.13 (0.07–0.26)*** | 1.28 (0.24–6.75) |
| Number of children in <10 milese | 1.22 (1.08–1.37)*** | 1.13 (0.96–1.33) |
| Number of children | 1.08 (1.02–1.15)* | 1.21 (1.10–1.33)*** |
| Age | 1.11 (1.09–1.14)*** | 1.07 (1.04–1.11)*** |
| Woman | 3.37 (2.42–4.70*** | 2.74 (1.81–4.15)*** |
| Years of education | 0.93 (0.90–0.97)*** | 0.97 (0.92–1.02) |
| IADLb | 1.38 (1.28–1.50)*** | 1.25 (1.10–1.42)*** |
| BADLc | 1.26 (1.17–1.36)*** | 1.02 (0.91–1.15) |
| Other SP | (N = 730) | (N = 664) |
| No spouse | 0.37 (0.20–0.68)*** | 0.22 (0.05–0.86)* |
| Living childrenf | 1.29 (1.16–1.43)*** | 1.41 (1.28–1.56)*** |
| Age youngest childd | 0.92 (0.85–0.99)* | |
| Living daughter | 1.92 (0.09–3.38)* | 0.25 (0.06–0.94)* |
| Age | 0.97 (0.95–0.998) | 1.02 (0.97–1.03) |
| Woman | 0.48 (0.34–0.68)*** | 0.67 (0.45–0.99)* |
| Years of education | 1.05 (1.01–1.08)* | 1.07 (1.02–1.13)** |
| IADLb | 0.99 (0.92–1.08) | |
| BADLc | 0.94 (0.87–1.01) | 1.00 (0.92–1.09) |
Note. All predictors found to be statistically significant (p < .05) in bivariate analyses were included in full models; OR = odds ratio; 95%CI = 95% confidence interval; IADL = Instrumental Activities of Daily Living; BADL = Basic Activities of Daily Living; SP = Study Partner.
1 to 5 with higher rankings being better.
IADL = Informant rating of participant’s functioning on five IADLs, where higher scores reflect greater impairment.
BADL = Informant rating of participant ‘s functioning on six BADLs, where higher scores reflect greater impairment.
Two missing observations.
6.5% missing data (n=44).
9.0% missing data (n=66).
<0.05
<0.01
<0.001.
Bivariate Mean Estimates of Participant Characteristics, SP Characteristics, and SP Reports on Participants’ Cognition and Function by Participant-SP Relationship
Participants with adult child SPs were more likely to be women and to have, on average, lower MMSE scores than participants with spousal SPs (both p < .05). Years of education did not appear to differ between participants with spousal SPs and those with adult child SPs (p > .05).
Adult child SPs were similarly likely to spousal SPs to be women and to identify as Black (p > .05), but more likely to have a college degree and to identify as a caregiver for the participant than spousal SPs (all p < .05). How adult child SPs reported on participants also differed from spousal SPs; adult child SPs rated participants as more impaired than did spousal SPs on the BDRS, IADLs, and the three single-item measures of memory, judgment, and organizational abilities (all p < .05, Table 3).
Table 3.
Bivariate Mean Estimates of Study Partner (SP) Characteristics, Participants’ Characteristics, and SP Reports on Participants’ Cognition and Function by SP Relationship.
| Characteristic | Spouse (n = 255) | Adult Child (n = 281) | Other (n = 194) |
|---|---|---|---|
| Participant Characteristic | |||
| Age, mean (95%CI) | 78.5 (77.8–79.1)y,z | 84.6 (83.8–85.5)x | 83.0 (81.9–84.0)x |
| Women, % (95%CI) | 31.3 (26.0–37.3)y,z | 73.7 (68.2–78.5)x | 70.6 (63.8–76.6)x |
| White, % (95%CI) | 85.9 (81.0–89.6)z | 77.9 (72.7–82.4) | 72.2 (65.4–78.0)x |
| Black, % (95%CI) | 11.0 (7.7–15.5) | 20.3 (16.0–25.4) | 20.6 (15.5–26.9) |
| MMSE,h mean (95%CI) | 24.4 (23.7–25.1)y,z | 19.7 (18.8–20.6)x | 21.0 (20.0–22.1)x |
| SP Characteristic | |||
| Age, mean (95%CI) | 74.7 (73.8–75.6)y,z | 55.9 (54.7–57.1)x | 59.1 (56.6–61.7)x |
| Woman, % (95%CI) | 67.5 (61.4–73.0)z | 74.2 (68.7–79.0) | 82.1 (76.0–86.9)x |
| White, % (95%CI) | 85.4 (80.4–89.2)y,z | 72.7 (67.1–77.7)x | 67.6 (60.5–73.9)x |
| Black, % (95%CI) | 11.1 (7.7–15.6)y,z | 20.7 (16.3–25.9)x | 22.3 (16.9–28.9) |
| College degree, % (95%CI) | 14.9 (11.0–19.8)y | 33.1 (27.8–38.8)x | 22.2 (16.9–28.6) |
| Caregiver,g % (95%CI) | 20.8 (16.2–26.2)y,z | 49.1 (43.3–55.0)x,z | 33.0 (26.7–39.9)x,y |
| Live with participant, % (95%CI) | 87.8 (83.2–91.3)y,z | 33.2 (27.9–39.0)x | 28.3 (22.3–35.1)x |
| articipant’s Cognition & Function | |||
| Activity level,a mean (95%CI) | 2.6 (2.5–2.7)y,z | 3.0 (2.9–3.1)x | 2.9 (2.8–3.0)x |
| Current memory,b mean (95%CI) | 2.6 (2.5–2.8)y,z | 3.2 (3.0–3.4)x | 3.0 (2.8–3.2)x |
| Judgment,c mean (95%CI) | 2.5 (2.4–2.7)y | 3.2 (3.0–3.3)x | 2.9 (2.7–3.1) |
| Organization,d mean (95%CI) | 2.4 (2.2–2.6)y,z | 3.1 (2.9–3.3)x | 2.9 (2.7–3.1)x |
| BDRS,e mean (95%CI) | 1.6 (1.2–2.0)y,z | 3.7 (3.1–4.3)x | 2.7 (2.1–3.3)x |
| IADL,f mean (95%CI) | 0.9 (0.7–1.1)y,z | 2.4 (2.1–2.6)x,z | 1.6 (1.4–1.9)x,y |
| IADL>0,f % (95%CI) | 27.8 (22.3–33.3)y,z | 64.1 (58.4–69.7)x | 51.5 (44.5–58.6)x |
Note. 95%CI = 95% confidence interval. Statistical significance (p < 0.05) shown by: “x” = different from “Spouse” group, “y” = different from “Child” group, “z” = different from “Other” group.
Activity level= Average of informant ratings on 10 items, where higher scores reflect more activity.
Current memory = A single item of informant ranking from 1 to 5 where higher scores reflect greater impairment.
Judgment = A single item of informant ranking from 1 to 5 where higher scores reflect greater impairment.
Organization = A single item of informant ranking from 1 to 5 where higher scores reflect greater impairment.
BDRS = Blessed Dementia Ratings Scale is a 22-item informant measure of 2-year change in participant’s cognition.
IADL = Informant rating of participant’s functioning on five IADLs, where higher scores reflect greater impairment.
Asked respondent about providing or supervising care for a friend or relative in past month. Care was defined by actively helping with Activities of Daily Living.
MMSE = Mini-Mental Status Exam, scores range from 0 to 30 with higher scores reflecting better global cognitive function.
SPs who were neither spouses nor adult children had characteristics similar to those of adult children (all p > .05).
Multivariable Adjusted Mean Differences in Ratings of Participants by Adult Child SPs and Other SPs as Compared to Spousal SPs
In analyses testing our hypothesis (H2) that adult children would rate the cognition and function of participants as less impaired than spouses would, we found adult children SPs rated participants as less impaired, on average, on measures of memory (−0.20, 95%CI −0.38 to −0.03; p < .05), judgment (−0.16, 95%CI −0.33 to 0.01; p = .007), and organizational (−0.18, 95%CI −0.35 − to 0.02) abilities than spousal SPs in multivariable analyses that adjusted for differences in participants’ cognition and function (Table 4).
Table 4.
Multivariable Adjusted Mean Differences in Ratings of Participants by Adult Child Study Partners (SPs) And Other SPs as Compared to Spousal SPs.
| Characteristic | Adult Child SP | Other SP |
|---|---|---|
| Mean Difference (95%CI) | Mean Difference (95%CI) | |
| Activity levela | 0.0(−0.08–0.09) | 0.01(−0.10 to 0.08) |
| Current memoryb | −0.20(−0.38–−0.03)* | −0.09(−0.27 to 0.09) |
| Judgmentc | −0.16(−0.33–0.01) | −0.11(−0.30 to 0.07) |
| Organizationd | −0.18(−0.35–−0.02)* | −0.06(−0.24 to 0.11) |
| BDRSe | −0.10(−0.52–0.32) | −0.06(−0.39 to 0.51) |
Note. SP = study partner. 95%CI = 95% confidence interval. Spousal SPs are reference group. Multivariable models were built using forward stepwise regression with alpha-to-keep of 0.15. All models statistically control for cognition as measured by the Mini-Mental Status Exam (MMSE), Trails B, and number of impairments in instrumental activities of daily living (IADLs). Models of activity level and organization also control for Trails A and number of impairments in basic activities of daily living (BADLs). Model of BDRS also controls for Serial 7s, Boston Naming, Animal Fluency, and BADLs.
Activity level = Average of ratings on 10 items. Higher scores reflect more activity.
Current memory = Single item ranking from 1 to 5. Higher scores reflect worse memory.
Judgment = Single item ranking from 1 to 5. Higher scores represent poorer judgment.
Organization = Single item ranking from 1 to 5. Higher scores represent worse organization.
BDRS = Blessed Dementia Ratings Scale is a 22-item measure 2-year change in participant’s cognition.
<0.05
<0.01
<0.001.
In a subanalysis, we included only participants with no IADL impairments and global cognition in the unimpaired range (MMSE scores > 28). In this group, the floor rating of participants’ current memory for spousal SPs, which corresponded to a qualitative classification of “Fair” (4 of 5), was lower than that of adult child SPs (Figure 2).
Figure 2.
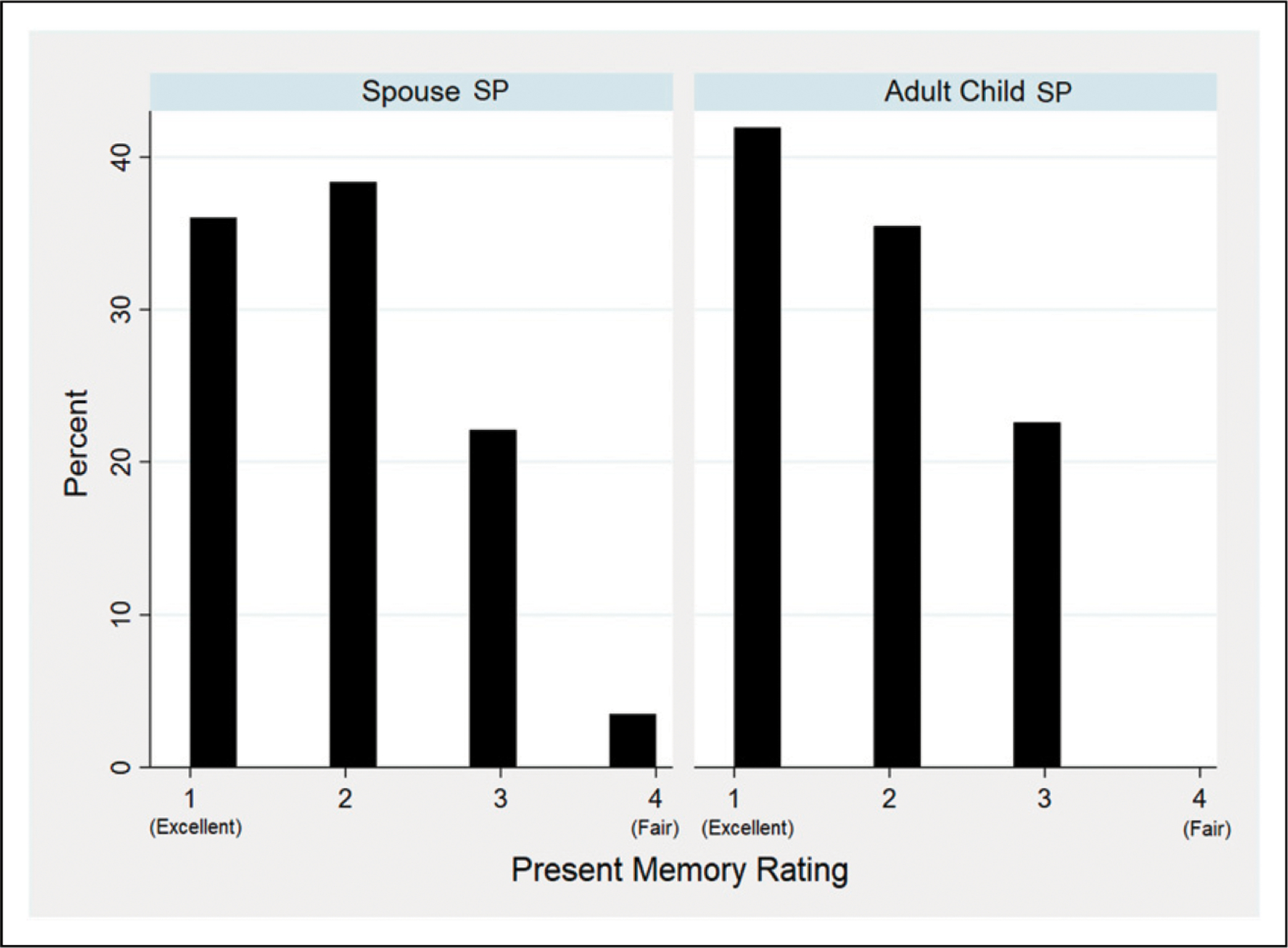
Study partner’s (SP’s) ratings of present memory in participants with no instrumental activities of daily living impairments and mini-mental status exam scores >28. Higher scores reflect SP reports of worse memory functioning.
No statistically significant differences were observed in BDRS scores between adult child SPs and spousal SPs in analyses that controlled for differences in participants’ cognition and function as measure by MMSE, Trails B, IADLs, BADLS, Serial 7s, Boston Naming, and Animal Fluency tasks. No statistically significant differences were observed in measures rated by other SPs compared to spousal SPs.
Discussion
We used a two-part approach in this study. First, we identified sociocultural factors that predicted who served as a SP: a spouse, an adult child, or other. Second, we examined differences in sociocultural characteristics and measures of SP-reported cognition and function by participant-SP relationship. We discuss our findings from the two parts in turn.
Factors that Predict Who Steps into the SP Role
Predictive analyses suggest that gender—in terms of identity but also social role—is a salient factor in determining who serves as a SP. We found that, independent of relationship to the participant, women are more likely than men to be SPs. In the spousal model, the majority of participants were men (68.7%) with women as SPs (67.5%), whereas women comprised the majority of both participants and SPs in the adult child model (73.7% and 74.2%, respectively) and the other relationship model (70.6% and 82.1%, respectively). Our findings suggest that women facilitate others’ participation in research. As spousal SPs, women support their husbands enrolling in research, and as adult daughters, extended family members, and friends they facilitate other women enrolling in research.
The presence of multiple women in the participant’s family network also appeared to affect who stepped into the SP role. In the spousal model, where the majority of SPs were women (67.5%), the participant having a living sister lowered the probability that a spouse was SP (OR = 0.27, 95% CI 0.08–0.93). Notably, the presence of a brother was not a statistically significant predictor in this model. Thus, the sibling relationship coupled with gender-role dynamics impact on who serves as SP.
Gender role dynamics in parent-child relationships also appeared to affect who served as SP. Unsurprisingly, the strongest predictor that an adult child would serve as SP was the absence of a participant’s spouse. Among participants with adult children, the absence of a spouse was associated with a more than 10 times higher probability that an adult child would serve as SP rather than, for example, a grandchild or friend (OR = 11.96, 95%CI 2.07–69.16). In instances where an adult child was the SP, 74.2% were women. This suggests that the SP role is typically filled by the spouse, and then, if a spouse is not present, an adult child, and that child is typically a daughter. These findings are consistent with our hypothesis that (H1) not having a spouse and having more living children would predict an adult child would serve as SP.
Normative American values and social structures rely heavily on gender roles and the notion of the nuclear family. Our findings are largely consistent with these normative patterns. The SP role reflects broader patterns of the society in which it operates. It raises a question as to whether, by interrogating these patterns, we may be able to identify ways to make SPs more representative of a more diverse range of sociocultural subgroups.
For example, in our analyses of spousal dyads, we found that older, White women in heterosexual relationships described the normative pattern of the SP role for spouses. Spouses of participants who deviate from this pattern may encounter barriers to being SPs. Unique features of the normative group may reveal factors that facilitate the group’s prominence in the SP role. In a subgroup analysis informed by these findings, we found wife SPs (mean age = 72 years) were much younger than husband SPs (mean age 79 years). Moreover, White wife SPs were younger (average age = 73 years) than Black wife SPs (average age = 79 years). Public education campaigns that aim to educate and stimulate interest in AD/ADRD research participation among relatively younger but otherwise socioculturally diverse groups of spouses may enhance SP availability.
Our results from analyses of participant-spouse SP dyads offer an unexpected observation. The participants in this group clinically resemble participants in AD/ADRD secondary prevention trials: older adults (age, mean = 78.5) with no functional impairments (IADL = 0, 72.2%) and no or mild cognitive impairment (MMSE, mean = 24.4, 95%CI 23.7–25.1). However, this group was mostly men (68.7%). This is quite different from those who volunteer for secondary prevention trials, mostly women (Jefferson et al., 2011; Johnson et al., 2017; Langbaum et al., 2019, 2020).
A number of factors may explain this discrepancy. HRS and ADAMS are observational cohort studies. Therefore, participation was less risky and less burdensome than participation in a secondary prevention trial. It is possible that men and women have different willingness to assume risks and burdens of clinical research, but this is unlikely to explain the disparity, as a prior study showed that women were more averse to risk in clinical research than were men (Chen et al., 2017). Another possibility is that wives are more likely to facilitate their husbands’ participation in HRS and ADAMS than husbands are to facilitate their wives’ participation. This would be consistent with the SP role being one of social facilitation (Kashima et al., 1995; Mosley, 2019), which similar to the caregiver role (Robinson et al., 2014), is filled mostly by women. If this is the case, however, why aren’t women bringing men to secondary prevention trials? Public education efforts that promote the value of women as SPs in combination with campaigns that call for men to enroll as participants may help enhance recruitment in secondary prevention trials.
If women must rely on other women to facilitate participation in research, women who enroll in research may not be representative of all women but rather represent a subset of women who had other women in their lives who could be their SP. A key part of a multipronged education campaign to enhance recruitment into AD/ADRD secondary trials should be addressing gender bias and gender stereotypes to decrease barriers to men being SPs.
How the Participant-SP Relationship Affects SP Reporting on Cognition and Function
We hypothesized that (H2) adult children would rate the cognition and function of participants as less impaired than spouses would. Instead, we found that, in bivariate analyses, adult child SPs rated participants as more impaired than spousal SPs on multiple measures of cognition and function. We found the opposite, however, in multivariable analyses that adjusted for differences in performance-based measures of participants’ cognition and function. In these analyses, adult child SPs rated participants as less impaired on those measures than did spousal SPs.
Our findings raise questions about how the effects we observed could influence the validity of AD/ADRD research, including secondary prevention trials. Our findings suggest that if study arms or groups are not balanced on relevant SP characteristics, the results could be biased by sociocultural differences in how SPs report—for example, if functional and cognitive measures reliant on SP input are used to assess disease progression. Further investigation is needed. Changes to recruitment strategies or trial design might be needed to assure the validity of AD/ADRD research.
Our results are consistent with two prior studies that found differences in spousal and adult child SP reports (Nuño et al., 2019; Ready et al., 2004). Findings from these prior studies prioritize spouses as SPs as spousal SP reports more closely correspond to a participant’s performance on cognitive testing. This approach may differentially impact on individuals from ethnoracial groups that are underrepresented in AD/ADRD research, as they are more likely to be cared for by a non-spouse and more likely to enroll in a trial with an adult child as their SP (Grill et al., 2013). Moreover, variance shared between a participant’s cognitive test performance and the reporting of his or her SP may differ across sociocultural groups. This could be due to cultural biases in cognitive testing (Aiken Morgan et al., 2010), relationship factors (Grill et al., 2013), or other factors.
Our findings are also notably distinct from those of prior studies. We compared the reporting of spousal SPs to that of adult child SPs while controlling for participant-level factors. Our goal was to determine whether differences existed in SP reports based on their relationship to the participant. Given that we found differences, future studies are needed to replicate our findings. If they are replicated, research will be needed to identify the importance of specific group differences and the methods needed to address them. How scientists choose to address differences in SP reporting in AD/ADRD research will influence efforts to increase representation of diverse sociocultural groups.
In about a quarter of instances (26.6%, n = 194), SPs had a relationship to the participant other than spouse or adult child. This “other” category contained a variety of family members (e.g., grandchildren, aunts or uncles, nieces, nephews), friends, and also paid aides. Our analyses focused on spouses and adult children, as they comprised the two most common SP relationships. Nevertheless, further study of this “other” category may yield important data. Understanding the sociocultural factors that support a grandchild, friend, paid aide, or other person in serving as a SP may offer information on social and cultural mechanisms that could be leveraged through education and policy to enhance recruitment.
Results of our bivariate analyses of the “other” category showed characteristics of SPs and participants that fell into this category were different than both the spouse and adult child group. On many measures, they appeared to fall between the spousal and adult child groups. There were, however, two exceptions. SPs who were not either spouses or adult children were less likely to identify as White (67.6% vs. 85.4% and 72.7%, respectively) and much less likely to reside with the participant (28.3% vs. 87.8% and 33.2%, respectively). The multivariable predictive model showed having a spouse, more living children, no living daughter, being a man, and having more years of education increase the likelihood that someone other than a spouse or adult child will serve as SP. Together the results suggest the absence of a wife or daughter to take on the role of SP in the context of extended families, economically solvent families, or both may lend to a SP who is neither a spouse or adult child of the participant. While no differences in reporting were identified between SPs in this category and SPs who were spouses, this result should be cautiously interpreted given the relatively low cell size (n = 194) and the heterogeneity of the category.
Our results should be interpreted in light of the following limitations. Our study sample was a fairly homogenous group of older, White Americans. Studies are needed to examine SP effects in other sociocultural groups, such as those defined by race and ethnicity. Cross-cultural studies are also needed, particularly those that help elucidate values and practices that vary significantly between individualist and collectivist cultures. Such studies might compare societies with similar cultural values but varying socio-economic structures and contrast societies with differing cultural values and practices but similar economic structures. This line of study may help understand how sociocultural factors enable or impede the SP role.
In this correlational study, it was not possible to evaluate all possible confounders. Even in statistical analyses that distinguish between the spousal relationship and living together, it is difficult to fully disentangle the respective effects (Ready et al., 2004). Moreover, our models statistically controlled for functioning using IADL scales that are completed by SPs. Thus, they could be subject to the same bias or misreporting as the other SP-reported measures. Future investigation is needed that replicates this study with a function measure that is fully independent of potential influence of SPs. Additionally, there is no documented protocol for how the SP was chosen or enrolled for ADAMS. Our understanding is that individuals were asked to identify a person who could be approached to co-participate with him or her. It is also important to note that the ADAMS sample of 730 dyads is small relative to large populations. In addition, our analyses identified gender as a salient determinant of the SP role. However, our analyses were limited in evaluating the full range of sex and gender identities on the SP role given limitations in measurement of sex and gender and representation of sexual and gender minoritized populations in the source data.
Conclusion
We used a two-part approach in this study. First, we identified sociocultural factors that predicted who served as a SP: a spouse, adult child, or other person. Second, we examined differences in sociocultural characteristics and measures of SP reported cognition and function by participant-SP relationship. In the first stage of our analyses, our findings suggest that gender—as an identity and social role—is a salient factor in determining who serves as a SP. Women appear to facilitate others’ participation in research as spouses, adult daughters, extended family members, and friends. Educational campaigns informed by these findings may aid in enhancing recruitment of socioculturally diverse samples in AD/ADRD research. We suggest such campaigns promote the value of women as SPs in combination with calls for men to enroll as participants; encourage research participation among relatively younger but otherwise socioculturally diverse groups of spouses; and address gender bias and gender stereotypes in order to decrease barriers to men being SPs.
In the second stage of our analyses, we found that SP reporting differed accordingly to a SP’s relationship with the participant. Adult child SPs rated participants as less impaired than did spousal SPs. Our findings suggest that if study arms or groups are not balanced on relevant SP characteristics, results could be biased by differences in SP reporting. If our findings bare out with replication, research will be needed to develop methods—whether changes to recruitment strategies, trial design, or data analysis—to address them. Contrary to earlier studies that prioritized spousal SPs over SPs with other relationships to participants, we contend that, in order to promote diversity, inclusion, and representation in research, individuals should be encouraged to serve as SPs regardless of relationship type. This may contribute to increased representativeness of study samples.
SPs make valuable contributions to AD/ADRD research. Yet, the precise nature of the role has long been overlooked, and the effect on data ignored. Our findings suggest SPs influence who can participate in AD/ADRD research and what is understood about the individuals who participate. More work is needed to understand how the role can be designed and data can be analyzed to improve AD/ADRD research.
Acknowledgments
The authors thank Jessica Langbaum, PhD, for her contributions in interpreting the results of the study and Norma Coe, PhD, for her consultation on the data source.
Funding
The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This work was supported by grants from the National Institute of Aging (NIA P30AG012836-25-S2 and NIA P30AG010124). Dr. Stites is supported by the Alzheimer’s Association (AARF-17-528934) and the NIA (K23AG065442).
Biographies
S. Stites is a clinical psychologist and researcher studying sociocultural diversity and disease biomarkers in dementia.
E. Largent is a lawyer and ethicist.
J. Gill and K. Harkins focus on public health in aging.
A. Gurian is a student of economics.
J. Karlawish is an ethicist, researcher, and geriatrician.
Footnotes
Declaration of Conflicting Interests
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Human Participant Protection
The Institutional Review Board of the University of Pennsylvania approved all procedures involving human subjects.
References
- Adams G, & Markus HR (2004). Toward a conception of culture suitable for a social psychology of culture. In The psychological foundations of culture (pp. 335–360). Lawrence Erlbaum Associates Publishers. [Google Scholar]
- Adams Questionnaires Forms. HRS Health and Retirement Study. https://hrs.isr.umich.edu/documentation/questionnaires/adams-forms. 2020. Accessed March 9, 2022.
- Aiken Morgan AT, Marsiske M, Dzierzewski J, Jones RN, Whitfield KE, Johnson KE, & Cresci MK (2010). Race-related cognitive test bias in the ACTIVE study: A MIMIC model approach. Experimental Aging Research, 36(4), 426–452. 10.1080/0361073X.2010.507427 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ayalon L (2011). The IQCODE versus a single-item informant measure to discriminate between cognitively intact individuals and individuals with dementia or cognitive impairment. Journal of Geriatric Psychiatry and Neurology, 24(3), 168–173. 10.1177/0891988711418506 [DOI] [PubMed] [Google Scholar]
- Barnes LL (2021). Alzheimer disease in African American individuals: increased incidence or not enough data? Nature Reviews Neurology, 18, 56–62. 10.1038/s41582-021-00589-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Black BS, Taylor H, Rabins PV, & Karlawish J (2014). Researchers’ perspectives on the role of study partners in dementia research. International Psychogeriatrics, 26(10), 1649–1657. 10.1017/S1041610214001203 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Black BS, Taylor HA, Rabins PV, & Karlawish J (2018). Study partners perform essential tasks in dementia research and can experience burdens and benefits in this role. Dementia, 17(4), 494–514. 10.1177/1471301216648796 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blessed G, Tomlinson BE, & Roth M (1968). The association between quantitative measures of dementia and of senile change in the cerebral grey matter of elderly subjects. The British Journal of Psychiatry, 114(512), 797–811. 10.1192/bjp.114.512.797 [DOI] [PubMed] [Google Scholar]
- Brandt J, Spencer M, & Folstein M (1988). The telephone interview for cognitive status. Neuropsychiatry, Neuropsychology and Behavioral Neurology, 1(2), 111–117. [Google Scholar]
- Cary MS, Rubright JD, Grill JD, & Karlawish J (2015). Why are spousal caregivers more prevalent than nonspousal caregivers as study partners in AD dementia clinical trials? Alzheimer Disease & Associated Disorders, 29(1), 70–74. 10.1097/WAD.0000000000000047 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen SC, Sinaii N, Bedarida G, Gregorio MA, Emanuel E, & Grady C (2017). Phase 1 healthy volunteer willingness to participate and enrollment preferences. Clinical Trials (London, England), 14(5), 537–546. 10.1177/1740774517722131 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Conde-Sala JL, Garre-Olmo J, Turró-Garriga O, Vilalta-Franch J, & López-Pousa S (2010). Differential features of burden between spouse and adult-child caregivers of patients with Alzheimer’s disease: an exploratory comparative design. International Journal of Nursing Studies, 47(10), 1262–1273. 10.1016/j.ijnurstu.2010.03.001 [DOI] [PubMed] [Google Scholar]
- Crimmins EM, Kim JK, Langa KM, & Weir DR (2011). Assessment of cognition using surveys and neuropsychological assessment: The health and retirement study and the aging, demographics, and memory study. The Journals of Gerontology Series B: Psychological Sciences and Social Sciences, 66B(suppl 1), i162–il71. 10.1093/geronb/gbr048 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ferris SH, Aisen PS, Cummings J, Galasko DM, Salmon DP, Schneider LM, Sano M, Whitehouse PJ, Edland S, & Thal LJ, Group, for the A. D. C. S. (2006). ADCS prevention instrument project: overview and initial results. Alzheimer disease & associated disorders, 20(4 suppl 3), S109–S123. 10.1097/01.wad.0000213870.40300.21 [DOI] [PubMed] [Google Scholar]
- Fillenbaum GG (1985). Screening the elderly. Journal of the American Geriatrics Society, 33(10), 698–706. 10.1111/j.1532-5415.1985.tb01779.x [DOI] [PubMed] [Google Scholar]
- Folstein MF, Folstein SE, & McHugh PR (1975). “Mini-mental state”: A practical method for grading the cognitive state of patients for the clinician. Journal of Psychiatric Research, 12(3), 189–198. 10.1016/0022-3956(75)90026-6 [DOI] [PubMed] [Google Scholar]
- González DA, Gonzales MM, Jennette KJ, Soble JR, & Fongang B (2021). Cognitive screening with functional assessment improves diagnostic accuracy and attenuates bias. Alzheimer’s & Dementia: Diagnosis, Assessment & Disease Monitoring, 13(1), Article e12250. 10.1002/dad2.12250 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grill JD, & Karlawish J (2017). Study partners should be required in preclinical Alzheimer’s disease trials. Alzheimer’s Research & Therapy, 9(1), 93. 10.1186/s13195-017-0327-x. Gale Academic OneFile; [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grill JD, Monsell S, & Karlawish J (2012). Are patients whose study partners are spouses more likely to Be eligible for Alzheimer’s disease clinical trials? Dementia and Geriatric Cognitive Disorders; Basel, 33(5), 334–340. http://dx.doi.org.proxy.library.upenn.edu/10.1159/000339361 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grill JD, Raman R, Ernstrom K, Aisen P, & Karlawish J (2013). Effect of study partner on the conduct of Alzheimer disease clinical trials. Neurology, 80(3), 282–288. 10.1212/WNL.0b013e31827debfe [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gross AL, Mungas DM, Crane PK, Gibbons LE, MacKay-Brandt A, Manly JJ, Mukherjee S, Romero H, Sachs B, Thomas M, Potter GG, & Jones RN (2015). Effects of education and race on cognitive decline: An integrative study of generalizability versus study-specific results. Psychology and Aging, 30(4), 863–880. 10.1037/pag0000032 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Isaacs B, & Kennie AT (1973). The set test as an aid to the detection of dementia in old people. The British Journal of Psychiatry, 123(575), 467–470. 10.1192/bjp.123.4.467 [DOI] [PubMed] [Google Scholar]
- Jefferson AL, Lambe S, Chaisson C, Palmisano J, Horvath KJ, & Karlawish J (2011). Clinical research participation among aging adults enrolled in an Alzheimer’s disease center research registry. Journal of Alzheimer’s Disease : JAD, 23(3), 443–452. 10.3233/JAD-2010-101536 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson SC, Koscik RL, Jonaitis EM, Clark LR, Mueller KD, Berman SE, Bendlin BB, Engelman CD, Okonkwo OC, Hogan KJ, Asthana S, Carlsson CM, Hermann BP, & Sager MA (2017). The wisconsin registry for Alzheimer’s prevention: A review of findings and current directions. Alzheimer’s & Dementia : Diagnosis, Assessment & Disease Monitoring, 10, 130–142. 10.1016/j.dadm.2017.11.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jorm AF (1994). A short form of the informant questionnaire on cognitive decline in the elderly (IQCODE): Development and cross-validation. Psychological Medicine, 24(1), 145–153. 10.1017/S003329170002691X [DOI] [PubMed] [Google Scholar]
- Jorm AF, & Jacomb PA (1989). The informant questionnaire on cognitive decline in the elderly (IQCODE): Socio-demographic correlates, reliability, validity and some norms. Psychological Medicine, 19(4), 1015–1022. 10.1017/s0033291700005742 [DOI] [PubMed] [Google Scholar]
- Jorm AF, Scott R, & Jacomb PA (1989). Assessment of cognitive decline in dementia by informant questionnaire. International Journal of Geriatric Psychiatry, 4(1), 35–39. 10.1002/gps.930040109 [DOI] [Google Scholar]
- Kaplan E, Goodglass H, & Weintraub S (1978). The Boston naming test. Veterans Administration Medical Center. [Google Scholar]
- Karlawish JHT, Casarett D, Klocinski J, & Sankar P (2001). How do AD patients and their caregivers decide whether to enroll in a clinical trial? Neurology, 56(6), 789–792. 10.1212/WNL.56.6.789 [DOI] [PubMed] [Google Scholar]
- Kashima Y, Yamaguchi S, Kim U, Choi S-C, Gelfand MJ, & Yuki M (1995). Culture, gender, and self: A perspective from individualism-collectivism research. Journal of Personality and Social Psychology, 69(5), 925–937. 10.1037/0022-3514.69.5.925 [DOI] [PubMed] [Google Scholar]
- Katz S, Ford AB, Moskowitz RW, Jackson BA, & Jaffe MW (1963). Studies OF illness IN the aged. The index of adl: A standardized measure of biological and psychosocial function. JAMA, 185(12), 914–919. 10.1001/jama.1963.03060120024016 [DOI] [PubMed] [Google Scholar]
- Langbaum JB, High N, Nichols J, Kettenhoven C, Reiman EM, & Tariot PN (2020). The Alzheimer’s prevention registry: A large internet-based participant recruitment registry to accelerate referrals to alzheimer’s-focused studies. Springer. 10.14283/jpad.2020.31 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Langbaum JB, Karlawish J, Roberts JS, Wood EM, Bradbury A, High N, Walsh T, Gordon D, Aggarwal R, Davis P, Stowell C, Trisko L, Langlois CM, Reiman EM, & Tariot PN (2019). GeneMatch: A novel recruitment registry using at-home APOE genotyping to enhance referrals to Alzheimer’s prevention studies. Alzheimer’s & Dementia : The Journal of the Alzheimer’s Association, 15(4), 515–524. 10.1016/j.jalz.2018.12.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Largent EA, Karlawish J, & Grill JD (2018). Study partners: Essential collaborators in discovering treatments for Alzheimer’s disease. Alzheimer’s Research & Therapy, 10(1), 101. 10.1186/s13195-018-0425-4. Gale Academic OneFile; [DOI] [PMC free article] [PubMed] [Google Scholar]
- Manly JJ, Gilmore-Bykovskyi A, & Deters KD (2021). Inclusion of underrepresented groups in preclinical Alzheimer disease trials—opportunities abound. JAMA Network Open, 4(7), Article e2114606. 10.1001/jamanetworkopen.2021.14606 [DOI] [PubMed] [Google Scholar]
- Morris JC, Ernesto CM, Schafer KM, Coats MR, Leon SR, Sano M, Thal LJ, & Woodbury P (1997). Clinical dementia rating training and reliability in multicenter studies: The Alzheimer’s disease cooperative study experience. Neurology, 48(6), 1508–1510. 10.1212/wnl.48.6.1508 [DOI] [PubMed] [Google Scholar]
- Morris JC, Heyman A, Mohs RC, Hughes JP, Belle GV, Fillenbaum G, Mellits ED, & Clark C (1989). The consortium to establish a registry for Alzheimer’s disease (CERAD). Part I. Clinical and neuropsychological assesment of Alzheimer’s disease. Neurology, 39(9), 1159–1165. 10.1212/WNL.39.9.1159 [DOI] [PubMed] [Google Scholar]
- Mosley A (2019). Gender discrepancies in social facilitation. PMC. [Google Scholar]
- Nuño MM, Gillen DL, & Grill JD, Studyfor the, A. D. C. (2019). Study partner types and prediction of cognitive performance: Implications to preclinical Alzheimer’s trials. Alzheimer’s Research & Therapy, 11(1), 1–7. 10.1186/s13195-019-0544-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ofstedal MB, Fisher GG, & Herzog AR (2005). Documentation of cognitive functioning measures in the health and retirement study. Institute for Social Research, University of Michigan. http://hrsonline.isr.umich.edu/sitedocs/userg/dr-006.pdf. [Google Scholar]
- Ready RE, Ott BR, & Grace J (2004). Validity of informant reports about AD and MCI patients’ memory. Alzheimer Disease & Associated Disorders, 18(1), 11–16. 10.1097/00002093-200401000-00003 [DOI] [PubMed] [Google Scholar]
- Reitan RM (1992). Trail making test: Manual for administration and scoring. Reitan Neuropsychology Laboratory. [Google Scholar]
- Robinson CA, Bottorff JL, Pesut B, Oliffe JL, & Tomlinson J (2014). The male face of caregiving: A scoping review of men caring for a person with dementia. American Journal of Men’s Health, 8(5), 409–426. 10.1177/1557988313519671 [DOI] [PubMed] [Google Scholar]
- Wilkins CH, Schindler SE, & Morris JC (2020). Addressing health disparities among minority populations: Why clinical trial recruitment is not enough. JAMA Neurology, 77(9), 1063–1064. 10.1001/jamaneurol.2020.1614 [DOI] [PMC free article] [PubMed] [Google Scholar]


