Abstract
Lipomas are rarely found in the mediastinum. Although they may reach large proportions, they rarely compress vascular structures. We present a case in which a lipoma produced superior vena cava syndrome. Urgent surgical decompression was required.
Key words: Lipoma/complications, lipoma/diagnosis, mediastinal neoplasms/surgery, superior vena cava syndrome/etiology
Lipomas are rarely found in the mediastinum. Excision is indicated only when the tumor causes pain or when compression by the tumor compromises the function of adjacent structures. We present a case in which a lipoma produced superior vena cava syndrome.
Case Report
In February 1999, a 61-year-old woman presented with progressive symptoms of dyspnea, tachypnea, hoarseness, headaches, dizziness, facial edema, and cyanosis of the head and shoulders. There was no hepatomegaly or lower-extremity edema. She had a history of 140 pack/year cigarette smoking, and she had received silicone injections in both breasts at age 27. An electrocardiogram was negative for ischemia, and a radiograph of the chest did not reveal pulmonary vascular congestion, pulmonary edema, or cardiomegaly. Computed tomography (CT) of the chest disclosed a soft-tissue, low-density mass that was compressing the superior vena cava (SVC) posteriorly. The mass, which was suspected to be a lipoma, measured 3 × 5 cm, ending above the area of the right atrium. It appeared to be extrapericardial. The lumen of the SVC was severely narrowed, as shown on the CT scan by the anterior displacement of contrast material caused by extraluminal posterior compression (Fig. 1).
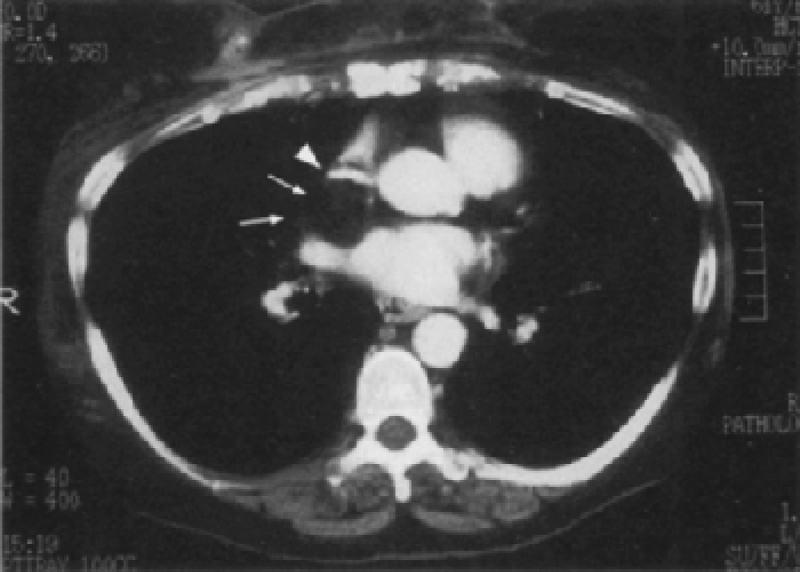
Fig. 1 Computed tomography of the chest. Contrast in the superior vena cava (SVC) demonstrates severe posterior external compression with almost complete occlusion of the vessel (arrowhead). The lipoma is compressing the SVC posteriorly (arrows).
The patient was taken to the operating room, where an anterior cervical mediastinoscopy was performed. All lymph nodes were negative for malignancy, but even though fat tissue was also biopsied, it could not be established with certainty that the tissue samples were from the tumor. A median sternotomy was performed, and a lipoma that weighed 12 grams was removed from behind the SVC. A thin layer of fibrous tissue in the anterior mediastinum, anterior to the SVC, was also removed. The pericardium was opened, which enabled us to confirm that the tumor was entirely extrapericardial and did not involve the interatrial septum.
The SVC expanded immediately upon removal of the tumor. Multiple small dilated venules, compatible with collateral drainage and distension from the SVC obstruction, were present throughout both operative fields. These vessels decreased extensively in volume after decompression.
Histologic examination confirmed that the tumor was a lipoma. Postoperatively, the patient's upper-body cyanosis disappeared almost immediately, followed over the next few days by her facial edema and hoarseness. At the time of discharge, no signs or symptoms of SVC compression were present. She remained asymptomatic through 7 months of follow-up.
Discussion
Our patient presented with symptoms typical of upper-body venous hypertension, specifically upper-body cyanosis, facial edema, and hoarseness secondary to pharyngeal edema and rapid progression of dyspnea. 1 Congestive heart failure was ruled out by the absence of pulmonary edema, pulmonary venous congestion, cardiomegaly, or peripheral edema. There was no evidence of myocardial ischemia.
Mesenchymal tumors constitute approximately 6% of all mediastinal mass lesions. Lipomas are the most common tumors but rarely produce symptoms, even when they are large. 2,3 Mediastinal lipomas are usually found in the anterior mediastinum. Previously, cases have been reported in which lipomas were found to compress vascular structures, but our search of the literature failed to identify any reports of mediastinal lipomas that compressed the SVC. Although lipomas have a relatively soft consistency, they can grow to gigantic proportions and cause the patient's death. Jack and co-workers 4 reported a large intrathoracic lipoma that impaired left ventricular function by direct compression. Their patient died after refusing surgical intervention.
We considered the therapeutic option of intravascular stenting. This idea was discarded, however; even though the tumor appeared on radiography to be a lipoma, we had to rule out associated malignancy because none of these tumors had been reported to produce SVC syndrome. The operation was performed urgently because of the rapid progression of laryngeal edema as manifested by dyspnea and hoarseness. The presence of fibrous tissue anterior to the SVC provided a rigid plane against which the lipoma was able to compress the SVC. Whether the lipoma may have continued to enlarge, eventually compressing the SVC by itself, is not known, again, because of the lack of previous reports. The layer of fibrous tissue did not encase the SVC. It was anterior to the SVC and was too thin to compress it by itself. Therefore, without the lipoma, the SVC would not have been compressed (Fig. 1). The fibrous tissue might have developed as the result of an old reaction induced by the silicone injections in both breasts and might have been a mild case of localized chronic fibrous mediastinitis that remained anterior to the SVC. The lymphatic drainage of the breast and anterior chest wall into the anterior mediastinum via the internal mammary chain appears to support this theory. After this thin layer of tissue was transected and the lipoma and lymph nodes posterior to the SVC were removed, the SVC distended easily and fully intraoperatively, and the patient's symptoms disappeared in the early postoperative period.
Footnotes
Address for reprints: C. Del Campo, MD, Suite 195, 301 W. Bastanchury Road, Fullerton, CA 92835
References
- 1.Effler DB, Groves LK. Superior vena caval obstruction. J Thorac Cardiovasc Surg 1962;43:574–84.
- 2.Rubush JL, Gardner IR, Boyd WC, Ehrenhaft JL. Mediastinal tumors. Review of 186 cases. J Thorac Cardiovasc Surg 1973;65:216–22. [PubMed]
- 3.Schweitzer DL, Aguam AS. Primary liposarcoma of the mediastinum. Report of a case and review of the literature. J Thorac Cardiovasc Surg 1977;74:83–97. [PubMed]
- 4.Jack AI, Blohm ME, Lye M. An intrathoracic lipoma impairing left ventricular function. Br Heart J 1995;74:95. [DOI] [PMC free article] [PubMed]


