Abstract
Introduction:
Information on morbidity-related productivity losses attributable to cigarette smoking, an important component of the economic burden of cigarette smoking, is limited. This study fills this gap by estimating these costs in the U.S. and by state.
Methods:
A human capital approach was used to estimate the cost of the morbidity-related productivity losses (absenteeism, presenteeism, household productivity, and inability to work) attributable to cigarette smoking among adults aged ≥18 years in the U.S. and by state. A combination of data, including the 2014–2018 National Health Interview Survey, 2018 Current Population Survey Annual Social and Economic Supplement, 2018 Behavioral Risk Factor Surveillance System, 2018 value of daily housework, and literature-based estimate of lost productivity while at work (presenteeism), was used. Costs were estimated for 2018, and all analyses were conducted in 2021.
Results:
Estimated total cost of morbidity-related productivity losses attributable to cigarette smoking in the U.S. in 2018 was $184.9 billion. Absenteeism, presenteeism, home productivity, and the inability to work accounted for $9.4 billion, $46.8 billion, $12.8 billion, and $116.0 billion, respectively. State-level total costs ranged from $291 million to $16.9 billion with a median cost of $2.7 billion.
Conclusions:
The cost of morbidity-related productivity losses attributable to cigarette smoking in the U.S. and in each state was substantial in 2018 and varied across the states. These estimates can guide public health policymakers and practitioners planning and evaluating interventions designed to alleviate the burden of cigarette smoking at the state and national levels.
INTRODUCTION
The economic cost of cigarette smoking exceeds $300 billion annually in the U.S., including >$225 billion for direct healthcare spending1 and >$156 billion in productivity losses attributable to premature mortality from smoking and exposure to second-hand smoke.2 However, smoking-attributable productivity losses are often underestimated because they do not account for morbidity-related productivity losses.2 The few studies that have estimated the absenteeism and/or presenteeism costs attributable to cigarette smoking are either dated or are limited to selected employers at the national level.3–7 Moreover, none of these previous studies have estimated other important components of cigarette smoking–attributable morbidity cost such as the inability to work at the national level, and none of the previous studies have estimated all components of morbidity-related productivity losses (absenteeism, presenteeism, inability to work, and household productivity losses) for all the states.
Morbidity-related productivity loss attributable to cigarette smoking is a key component of total economic costs attributable to cigarette smoking and thus is important to include in evaluating the impact of tobacco-related interventions from the societal perspective. Because many tobacco-related health policy decisions are made at a state or national level, detailed information on the economic costs of cigarette smoking at both levels can be useful for public health planners and policymakers. This study fills this evidence gap by providing the 2018 cost estimates of morbidity-related productivity losses (absenteeism, presenteeism, inability to work, and household productivity losses) attributable to cigarette smoking in total and per person who smoked cigarettes aged ≥18 years (referred to as adults in the remaining parts of this paper) in the U.S. and by state, including the District of Columbia (referred to as state in the remaining parts of this paper). These estimates can be combined with estimates of productivity loss because of premature mortality to inform the overall productivity losses attributable to cigarette smoking.
METHODS
Study Sample
The data for this study came primarily from the 2014–2018 National Health Interview Survey (NHIS). The NHIS is an annual, nationally representative, cross-sectional household survey of the non-institutionalized U.S. civilian population.8 Pooled NHIS data from 2014 to 2018 were used for an adequate sample for adults aged ≥18 years (N=83,046) who currently smoke (n=13,638), formerly smoked (n=17,133), and never smoked (n=52,275) cigarettes. Other data sources used in morbidity cost estimation have been provided in Appendix Table 1 (available online).
Measures
Cigarette smoking status (currently smoke, formerly smoked, or never smoked) was defined using self-reported responses to these NHIS questions: (1) Have you smoked at least 100 cigarettes in your entire life? (2) Do you now smoke cigarettes every day, some days or not at all? and (3) How long has it been since you quit smoking cigarettes? Adults who currently smoke cigarettes were those who smoked ≥100 cigarettes in their lifetime and smoked some days or every day at the time of the interview. Adults who formerly smoked were defined as having smoked at least 100 cigarettes in their lifetime but had quit smoking at the time of the interview. Adults who never smoked were identified as those who reported smoking fewer than 100 cigarettes in their lifetime.1
The cost of morbidity-related productivity losses attributable to cigarette smoking was computed as the sum of the cigarette smoking–attributable costs from absenteeism and presenteeism among those employed and inability to work and household productivity losses regardless of person’s employment status. Absenteeism cost arises when employees miss workdays because of illness. Presenteeism cost arises when employees become unproductive while at work.4 The cost of inability to work reflects the lost productivity because of disability. The cost of household productivity losses arises when people cannot perform household services, such as cooking, cleaning, gardening, household management, and caring for children or nonmarket production.
Statistical Analysis
Using the human capital approach,9,10 the state-level costs of morbidity-related productivity losses were estimated for all adults who currently or formerly smoked cigarettes compared with those who never smoked. Because of data limitations, estimates of work loss days, probability of inability to work, and people in bed days for each state were derived from corresponding U.S. Census region–specific estimates. To value these losses, the state-level age group– and sex-specific daily average earnings were used. The overall costs for the U.S. were estimated as a sum of estimates across the states.
All the regression models for estimating outcomes using NHIS data are described below by component, accounting for survey weights and controlling for sociodemographics, health-related status, and survey year. Consistent with the literature,1,11 sociodemographic variables included age, age squared, race/ethnicity (non-Hispanic White, non-Hispanic Black, Hispanic, or non-Hispanic other [non-Hispanic Asian or non-Hispanic all other race groups]), educational attainment (less than high school, high-school diploma or GED, some college, or college and above), annual family income (<100%, 100% to <125%, 125% to <200%, 200% to <400%, or ≥400% of the federal poverty level), occupation (management, production, or service related), and marital status (married or cohabitating; never married; or widowed, divorced or separated). Health-related variables included health insurance coverage status (yes or no), receipt of influenza vaccine in the past 12 months (yes or no), BMI (weight [kg]/height [meter]2 categories: underweight [<18.5], normal weight [18.5 to <25], overweight [25 to <30], obese [≥30]), and alcohol drinking status. Alcohol drinking status was grouped using a recoded variable in NHIS: lifetime abstainer (<12 drinks in a lifetime), former infrequent or regular drinker (≥12 drinks in a lifetime but ≤12 in 1 year and none in the past year), current light drinker (≥12 drinks in a lifetime and ≤3 drinks per week in the past year), current infrequent or moderate drinker (≥12 drinks in a lifetime and <12 drinks in the past year or >3 to 14 drinks per week [male] or >3 to 7 drinks per week [female]), or current heavy drinker (≥12 drinks in a lifetime and >14 drinks [male] or >7 drinks [female] per week in the past year).12 All cost components were estimated by Census region, age group–specific (18–24, 25–44, 45–64, 65–74, or ≥75 years), and sex-specific categories using 2014–2018 NHIS data and then applied to states within each region.9 The approaches used to estimate each component by state are described below.
State-level absenteeism cost was estimated using age group– and sex-specific missed workdays per adult who smoked cigarettes in a respondent’s corresponding Census region attributable to cigarette smoking multiplied by the state-level age group– and sex-specific daily earnings and the estimated number of state-level age group– and sex-specific employed adults who smoked cigarettes. The number of missed workdays owing to cigarette smoking, was estimated among adults who smoked (formerly or currently) compared with those who never smoked at the region level, by age group and sex, using a standard negative binomial model after specification tests for model selection and using Akaike information criterion and Bayesian information criterion,13 controlling for the same set of covariates described earlier (Appendix Table 2, available online). The state-level age group– and sex-specific daily average earnings were calculated by dividing the corresponding 2018 average annual earnings by 250, assuming 250 as the total workdays in a year.9 The 2018 average annual state-level earnings were obtained from the Current Population Survey Annual Social and Economic Supplement.14 The earnings estimates used in the analysis include the 2018 earnings plus 22.4% fringe benefits.9,15 The state-level age group– and sex-specific numbers of adults who smoked (currently or formerly) cigarettes and were employed were obtained by multiplying the corresponding region’s age group– and sex-specific employment rates among adults who smoked cigarettes by the corresponding state-level age group– and sex-specific number of adults. The region-level age group– and sex-specific employment rates were estimated using 2014–2018 NHIS data.8 The state-level age group– and sex-specific numbers of adults who smoked cigarettes were estimated using the 2018 Behavioral Risk Factors Surveillance System.16
The state-level age group– and sex-specific presenteeism costs attributable to cigarette smoking were estimated among those who smoked (formerly or currently) compared with that among those who never smoked and were estimated by multiplying the average number of presenteeism days lost by the corresponding state-level age group– and sex-specific daily earnings. The average number of presenteeism days lost was estimated by multiplying the presenteeism rates by the total annual workdays after accounting for absenteeism days (i.e., 250 minus estimated absenteeism days).9 The presenteeism rates among adults, 1.68% among those who currently smoke and 0.66% among those who formerly smoked cigarettes, were derived from the literature4 (Appendix Table 2, available online).
The state-level age group– and sex-specific household productivity losses were estimated by multiplying the days of household productivity losses by the daily value of household production. The days of household productivity losses attributable to cigarette smoking were estimated by the number of bed days per year because of illness or injuries10,17 at the region level by age group and sex using the same approach (negative binomial model) used for estimating missed workdays (Appendix Table 2, available online). For those employed, sick days in bed would also result in absenteeism days. However, although absenteeism cost measures labor-market productivity losses, the home productivity costs value nonmarket production and do not result in double counting of costs.18 The average value of household production per day was obtained from the Expectancy Data Economic Demographer’s “The Dollar Value of a Day: 2018 Dollar Valuation.”19 Because the Expectancy Data reports the average value of household production per day at the national level by age group and sex, the Bureau of Labor Statistics state-to-national wage ratios20 were applied to estimate the average value of household production for the corresponding state by the same age group and sex.9
The state-level age- and sex-specific cost of inability to work was estimated by multiplying the number of adults who smoked and were unable to work because of cigarette smoking-related disability at the region-level by age group and sex by state-level annual earnings. The number of people unable to work was estimated by multiplying the corresponding region-level age group– and sex-specific cigarette smoking-attributable probability of being unable to work owing to disability (Appendix Table 2, available online) by the state-level age group– and sex-specific number of adults who smoked cigarettes. The region-level age group– and sex-specific probability of being unable to work was estimated using a logistic regression model using the 2014–2018 NHIS data, controlling for the same sets of covariates used in the estimation of missed workdays.
The cost estimates were generated as total and per adult who smoked in the U.S. and by state. The estimated costs were also generated as per capita adult population. All analyses were conducted in 2021, using Stata, version 17 (StataCorp, LLC). Because the analysis was based on secondary and deidentified data, an IRB review was not required.
RESULTS
The total cost of morbidity-related productivity losses attributable to cigarette smoking in the U.S. in 2018 was $184.9 billion, including $105.9 billion for adults who currently smoke and $79.0 billion for adults who formerly smoked (Table 1). Of the total morbidity cost, absenteeism accounted for $9.4 billion (5.1%), presenteeism accounted for $46.8 billion (25.3%), home productivity accounted for $12.8 billion (6.9%), and inability to work accounted for $116.0 billion (62.7%) (Table 1).
Table 1.
Annual Morbidity-Related Productivity Losses (2018 $) Attributable to Cigarette Smoking, U.S.
| Cost category/cigarette smoking status | U.S. total (millions, $) | State total (millions, $) |
U.S. average ($)a | State average ($)a |
||||
|---|---|---|---|---|---|---|---|---|
| Median | Min | Max | Median | Min | Max | |||
|
| ||||||||
| Total morbidityb | ||||||||
| Currently or formerly smoked | 184,912 (125,625–244,254) |
2,697 AL |
291 WY |
16,946 CA |
1,938 (1,317–2,561) |
1,879 NC |
1,363 ID |
3,395 DC |
| Currently smoke | 105,870 (80,609–131,128) |
1,580 CO |
158 VT |
9,034 TX |
2,830 (2,155–3,506) |
2,707 CA |
1,996 ID |
4,974 DC |
| Formerly smoked | 79,042 (45,016–113,126) |
1,021 AL |
119 WY |
8,268 CA |
1,363 (776–1,951) |
1,317 TN |
959 ID |
2,342 DC |
| Absenteeismc | ||||||||
| Currently or formerly smoked | 9,354 (4,048–14,660) |
135 AL |
17 VT |
1,004 CA |
98 (42–154) |
98 LA, WA, NH, MO |
75 FL |
164 DC |
| Currently smoke | 6,661 (3,508–9,813) |
99 AL |
11 VT |
682 CA |
178 (94–262) |
179 NM, OR |
117 MS |
285 DC |
| Formerly smoked | 2,693 (540–4,847) |
37 CT |
6 AK |
322 CA |
46 (9–84) |
45 MA, IL, GA, AK, AZ |
30 ME, MI |
84 DC |
| Presenteeismd | ||||||||
| Currently or formerly smoked | 46,757 (46,477–47,033) |
653 AL |
86 WY |
4,878 CA |
490 (487–493) |
476 MO |
382 WV |
822 DC |
| Currently smoke | 30,510 (30,307–30,711) |
458 AL |
49 VT |
2,939 CA |
816 (810–821) |
785 OH, OR |
559 WV |
1,338 DC |
| Formerly smoked | 16,246 (16,170–16,323) |
227 OR |
29 WY |
1,938 CA |
280 (279–281) |
266 OH, OR |
197 MS |
478 DC |
| Home productivitye | ||||||||
| Currently or formerly smoked | 12,791 (7,163–18,420) |
188 OR |
24 VT |
1,354 CA |
134 (75–193) |
128 WY, AZ, WV |
105 SD |
239 DC |
| Currently smoke | 6,759 (4,438–9,079) |
106 CO |
10 VT |
594 CA |
181 (119–243) |
173 HI |
138 SD |
343 DC |
| Formerly smoked | 6,033 (2,725–9,340) |
82 CT |
11 WY |
760 CA |
104 (47–161) |
97 NV |
80 SD |
170 DC |
| Inability to workf | ||||||||
| Currently or formerly smoked | 116,010 (67,937–164,141) |
1,686 CO |
161 WY |
10,314 TX |
1,216 (712–1,721) |
1,189 IN |
766 ID |
2,170 DC |
| Currently smoke | 61,941 (42,356–81,525) |
863 AZ |
87 VT |
5,671 TX |
1,656 (1,132–2,180) |
1,573 IA, SD |
1,014 ID |
3,008 DC |
| Formerly smoked | 54,069 (25,581–82,616) |
708 AL |
73 WY |
5,248 CA |
932 (441–1,425) |
899 OK |
595 NM |
1,611 DC |
Note: Values in parentheses are 95% prediction intervals calculated on the basis of 95% CIs of regression-based estimates.
Per adult who smoked cigarettes.
Total morbidity costs attributable to cigarette smoking were computed as the sum of the absenteeism, presenteeism, household productivity, and inability to work costs. The total morbidity cost per adult who smoked cigarettes was computed by dividing the total morbidity cost by the number of adults who smoked cigarettes.
Absenteeism costs attributable to cigarette smoking were computed by multiplying the total missed workdays attributable to cigarette smoking by daily earnings. A standard negative binomial regression, which controlled for sociodemographic factors, was used with the 2014–2018 NHIS data to estimate the missed workdays attributable to cigarette smoking. Daily earnings were computed by dividing annual earnings, available from the CPS Table Creator, by 250 days. The total absenteeism cost per adult who smoked cigarettes was computed by dividing the total absenteeism cost by the number of adults who smoked cigarettes.
Presenteeism costs attributable to cigarette smoking were computed by multiplying the total presenteeism days (250 days minus missed workdays among adults who smoked cigarettes obtained from the 2014–2018 NHIS data) by daily earnings. To estimate presenteeism days per adult who smoked cigarettes, the authors assumed a 1.685% presenteeism rate for adults who currently smoke cigarettes and a 0.66% presenteeism rate for adults who formerly smoked cigarettes, per Bunn et al. (2006).4 The presenteeism cost per adult who smoked was computed by dividing the total presenteeism cost by the number of adults who smoked cigarettes.
Home productivity costs attributable to cigarette smoking were computed by multiplying the total number of bed days attributable to cigarette smoking by the dollar value of housework, available from the 2018 Expectancy Data. A standard negative binomial regression, which controlled for sociodemographic factors, was used with the 2014–2018 NHIS data to estimate the number of bed days attributable to cigarette smoking. The home productivity cost per adult who smoked a cigarette was computed by dividing the total home productivity cost by the number of adults who smoked cigarettes.
Inability to work costs attributable to cigarette smoking were computed by multiplying the total number of adults who smoked cigarettes and who were unable to work by annual earnings. A logistic regression model, which controlled for sociodemographic factors, was used with the 2014–2018 NHIS data to estimate the percentage of adults who smoked cigarettes and who were unable to work or the total number of adults who smoked a cigarette and were unable to work. The inability to work cost per adult who smoked cigarettes was computed by dividing the total inability to work cost by the number of adults who smoked cigarettes.
AK, Alaska; AL, Alabama; AZ, Arizona; CA, California; CO, Colorado; CPS, Current Population Survey; CT, Connecticut; DC, District of Columbia; FL, Florida; GA, Georgia; HI, Hawaii; IA, Iowa; ID, Idaho; IL, Illinois; IN, Indiana; LA, Louisiana; MA, Massachusetts; Max, maximum; ME, Maine; MI, Michigan; Min, minimum; MO, Missouri; MS, Mississippi; NC, North Carolina; NH, New Hampshire; NHIS, National Health Interview Survey; NM, New Mexico; NV, Nevada; OH, Ohio; OK, Oklahoma; OR, Oregon; SD, South Dakota; TN, Tennessee; TX, Texas; VT, Vermont; WA, Washington; WV, West Virginia.
By state, the total cost ranged from $291 million in Wyoming to $16.9 billion in California, with a median cost of $2.7 billion in Alabama (Table 1 and Figure 1). By cost component, absenteeism cost ranged from $17 million in Vermont to $1.0 billion in California, with a median cost of $135 million in Alabama; the presenteeism cost ranged from $86 million in Wyoming to $4.9 billion in California, with a median cost of $653 million in Alabama; the home productivity cost ranged from $24 million in Vermont to $1.4 billion in California, with a median cost of $188 million in Oregon; and inability to work cost ranged from $161 million in Wyoming to $10.3 billion in Texas, with the median cost of $1.7 billion in Colorado. By morbidity component, costs were higher among adults who currently smoke than among those who formerly smoked cigarettes (Table 1, Figure 1 and Appendix Table 3, available online).
Figure 1.
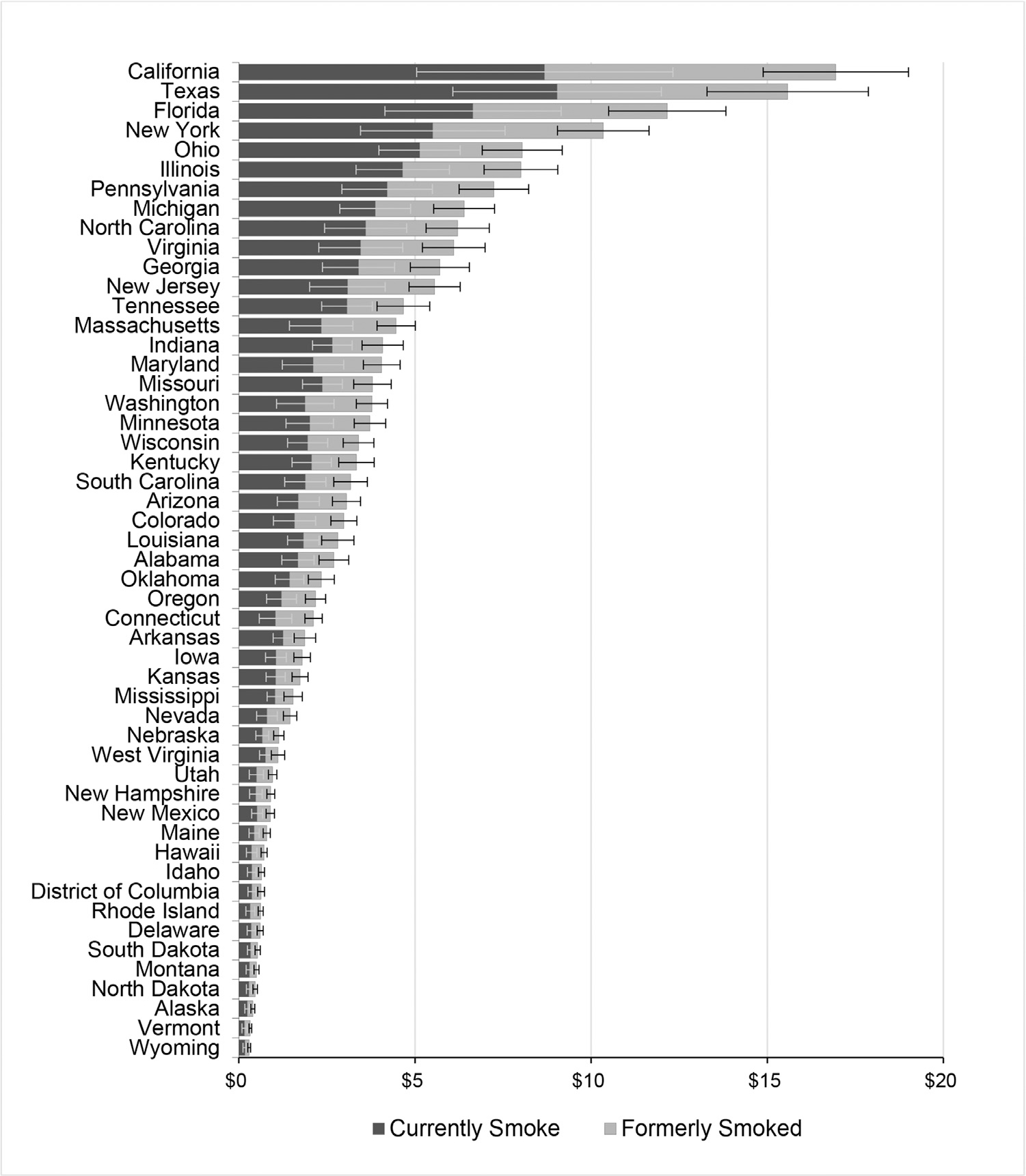
Total annual morbidity-related productivity losses (billions, 2018 $) attributable to cigarette smoking, U.S. state.
The total annual morbidity costs per adult who smoked cigarettes in the U.S. in 2018 was $1,938 (Table 1). Of this cost, absenteeism accounted for $98, presenteeism accounted for $490, home productivity accounted for $134, and inability to work accounted for $1,216. Total morbidity costs per adult who smoked cigarettes were $2,830 among those who currently smoke compared with $1,363 among those who formerly smoked. By state, the morbidity cost per adult who smoked cigarettes ranged from $1,363 in Idaho to $3,395 in the District of Columbia, with a median cost of $1,879 in North Carolina. By component and state, absenteeism costs per adult who smoked cigarettes ranged from $75 in Florida to $164 in the District of Columbia, with the median cost of $98 in 4 states (Missouri, Washington, New Hampshire, and Louisiana). Presenteeism cost per adult who smoked cigarettes ranged from $382 in West Virginia to $822 in the District of Columbia, with the median cost of $476 in Missouri. Home productivity cost per adult who smoked cigarettes ranged from $105 in South Dakota to $239 in the District of Columbia, with the median cost of $128 in Wyoming, Arizona, and West Virginia; and inability to work cost per adult who smoked cigarettes ranged from $766 in Idaho to $2,170 in the District of Columbia, with the median cost of $1,189 in Indiana. Across all components, average costs were higher for those who currently smoke than for those who formerly smoked cigarettes (Table 1, Figure 2 and Appendix Table 4, available online).
Figure 2.
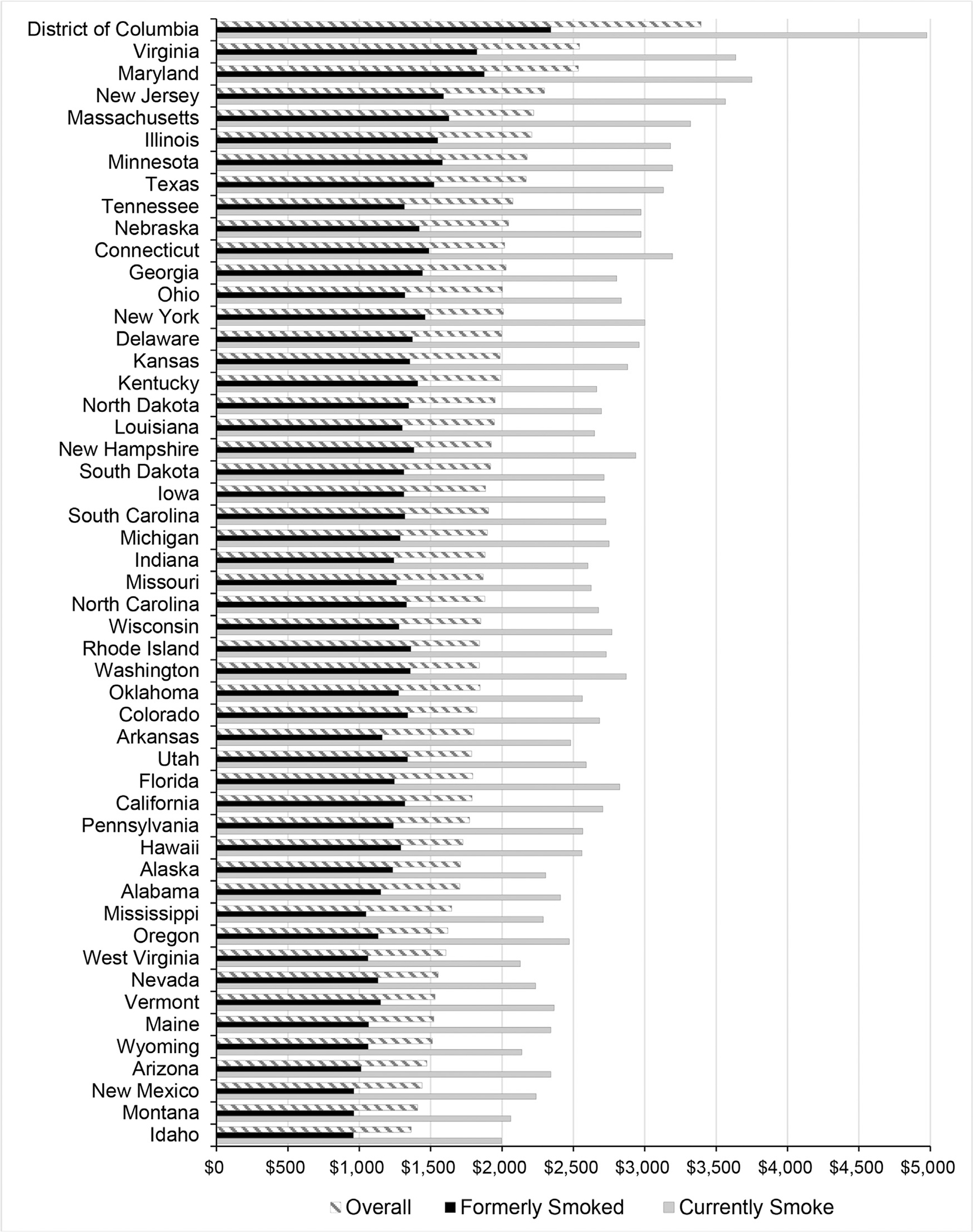
Annual morbidity-related productivity losses (2018 $) attributable to cigarette smoking, per adult who smoked, U.S. state.
The state-level median annual morbidity cost per capita adult population in the U.S. in 2018 was $748. By state, the total annual morbidity costs per capita in the adult population ranged from $429 to $1,099 (Appendix Table 5, available online).
DISCUSSION
This study is the first to provide comprehensive cost estimates of the cigarette smoking-attributable morbidity-related productivity losses in the U.S. and by state. The estimated cost in 2018 is $184.9 (95% prediction intervals: $125.6–$244.3) billion. This cost is larger than the average annual cost of productivity losses because of premature death attributable to cigarette smoking of $151 billion in 2007 ($180 billion in 2018 dollars).2 Accounting for the cost of morbidity-related productivity losses attributable to cigarette smoking, the recent estimates of healthcare spending attributable to cigarette smoking of $226.7 billion in 2014 ($241.4 billion in 2018 dollars),1 and the cost of premature mortality-related productivity losses attributable to cigarette smoking,2 the economic cost of cigarette smoking in the U.S. exceeded $600 billion in 2018.
Overall and the average costs across all components were consistently higher for those who currently smoke cigarettes than for those who formerly smoked cigarettes, which is consistent with previous literature.4 This difference by smoking status highlights the benefits of quitting and cessation interventions. However, persons who quit because of adverse health events, which is the major predictor of smoking cessation,4,21,22 and persons who quit proactively can be different in terms of length of quitting. Hence, the difference in productivity losses between adults who currently smoke and formerly smoked may underestimate the benefits of cessation interventions.
The morbidity cost of cigarette smoking is also large at the state level, with a median morbidity cost of $2.7 billion in 2018, ranging from $291 million to $16.9 billion. As expected, total morbidity cost was higher in larger or more populous states and lower in smaller or less populous states23 and does not necessarily reflect smoking prevalence in those states. The higher morbidity cost in certain states was driven by higher average earnings. By morbidity component, costs were largest for inability to work, followed by presenteeism, absenteeism, and home productivity. The higher presenteeism cost than absenteeism cost is consistent with previous findings.4
The cost per adult who smoked cigarettes varied across states (ranging from $1,363 to $3,395). In general, morbidity cost per adult who smoked cigarettes was higher in states with higher per capita earnings.14 The state-level estimated median absenteeism days, that is, 0.90 and 0.34 days annually for those who currently and formerly smoked cigarettes, respectively (Appendix Table 2, available online), are comparable with previous findings that ranged from 1.07 to 2.60 and from 0.28 to 1.35 days for persons who currently and formerly smoked cigarettes in the U.S., respectively.4–6,24,25
Limitations
These study findings are subject to some limitations. The identification of smoking status is subject to recall bias because responses were self-reported and not biochemically validated. However, self-reported smoking status correlates highly with serum cotinine levels.26 This study used average earnings to estimate productivity losses, but average earnings are likely to be lower among those who smoked than among those who never smoked,27 and average earnings can vary by education or employment type. However, this information was not available. There may have been uncontrolled confounding of other factors such as illicit drug use and abuse not accounted for by the sociodemographic and health-related factors controlled for in the models, which may lead to overestimation of productivity losses. Furthermore, the human capital approach used in this study likely overestimated the productivity losses in comparison with the friction cost approach, which estimates productivity losses as the short-term lost worker replacement costs.28 The use of respondent’s disability as the main reason for not working in the last week as a proxy for estimating the probability of inability to work may have led to an overestimation of the cost of inability to work. This study also did not consider the value of the time spent on smoking breaks and the cost of informal care,28 resulting in an underestimation of total productivity losses.
CONCLUSIONS
The cost of morbidity-related productivity losses attributable to cigarette smoking overall and by individual component poses a substantial burden in the U.S. and in each state in 2018. Both overall and component-specific costs varied by state. These estimates can provide policymakers and planners a better understanding of morbidity-related productivity losses attributable to cigarette smoking, an important component of the overall economic cost of cigarette smoking. These estimates can also provide useful information for better planning and evaluation of interventions designed to reduce cigarette smoking at both the state and national levels.
Supplementary Material
ACKNOWLEDGMENTS
The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the U.S. Centers for Disease Control and Prevention.
Footnotes
No financial disclosures were reported by the authors of this paper.
CREDIT AUTHOR STATEMENT
Sundar S. Shrestha: Conceptualization, Investigation, Methodology, Project administration, Writing - original draft, Writing - review and editing. Ramesh Ghimire: Data curation, Formal analysis, Writing - original draft, Writing - review and editing. Xu Wang: Writing - review and editing. Katrina F. Trivers: Writing - review and editing. David M. Home: Conceptualization, Writing - review and editing. Brian S. Armour: Conceptualization, Writing - review and editing.
SUPPLEMENTAL MATERIAL
Supplemental materials associated with this article can be found in the online version at https://doi.org/10.1016/j.amepre.2022.04.032.
REFERENCES
- 1.Xu X, Shrestha SS, Trivers KF, Neff L, Armour BS, King BA. U.S.healthcare spending attributable to cigarette smoking in 2014. Prev Med. 2021;150:106529. 10.1016/j.ypmed.2021.106529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.2014 Surgeon General’s Report: the health consequences of smoking—50 years of progress. U.S. Department of Health and Human Services, Centers for Disease Controls and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health; 2021. https://www.cdc.gov/tobacco/data_statistics/sgr/50th-anniversary/index.htm.
- 3.Asay GR, Roy K, Lang JE, Payne RL, Howard DH. Absenteeism and employer costs associated with chronic diseases and health risk factors in the U.S. workforce. Prev Chronic Dis. 2016;13:150503. 10.5888/pcd13.150503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bunn WB 3rd, Stave GM, Downs KE, Alvir JM, Dirani R. Effect of smoking status on productivity loss. J Occup Environ Med. 2006;48 (10):1099–1108. 10.1097/01.jom.0000243406.08419.74. [DOI] [PubMed] [Google Scholar]
- 5.Berman M, Crane R, Seiber E, Munur M. Estimating the cost of a smoking employee. Tob Control. 2014;23(5):428–433. 10.1136/tobaccocontrol-2012-050888. [DOI] [PubMed] [Google Scholar]
- 6.Halpern MT, Shikiar R, Rentz AM, Khan ZM. Impact of smoking status on workplace absenteeism and productivity. Tob Control. 2001;10(3):233–238. 10.1136/tc.10.3.233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Mitchell RJ, Bates P. Measuring health-related productivity loss. Popul Health Manag. 2011;14(2):93–98. 10.1089/pop.2010.0014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.National Health Interview Survey 1997–2018. Centers for Disease Control and Prevention. National Center for Health Statistics; 2021. https://www.cdc.gov/nchs/nhis/1997-2018.htm.
- 9.Shrestha SS, Honeycutt AA, Yang W, et al. Economic costs attributable to diabetes in each U.S. state. Diabetes Care. 2018;41(12):2526–2534. 10.2337/dc18-1179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ekwueme DU, Trogdon JG, Khavjou OA, Guy GP Jr. Productivity costs associated with breast cancer among survivors aged 18–44 years. Am J Prev Med. 2016;50(2):286–294. 10.1016/j.amepre.2015.10.006. [DOI] [PubMed] [Google Scholar]
- 11.Xu X, Bishop EE, Kennedy SM, Simpson SA, Pechacek TF. Annual healthcare spending attributable to cigarette smoking: an update. Am J Prev Med. 2015;48(3):326–333. 10.1016/j.amepre.2014.10.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.National Health Interview Survey, 2018: sample adult. Atlanta, GA: Centers for Disease Control and Prevention, National Center for Health Statistics; 2021. https://ftp.cdc.gov/pub/Health_Statistics/NCHS/Dataset_Documentation/NHIS/2018/samadult_layout.pdf. [Google Scholar]
- 13.Deb P, Norton EC. Modeling health care expenditures and use. Annu Rev Public Health. 2018;39:489–505. 10.1146/annurev-publhealth-040617-013517. [DOI] [PubMed] [Google Scholar]
- 14.Current Population Survey (CPS) Annual Social and Economic (March) Supplement. U.S. Census Bureau. https://data.census.gov/mdat/#/. Accessed March 23, 2021.
- 15.Haddix AC, Teutsch SM, Corso PS. Prevention Effectiveness: a Guide to Decision Analysis and Economic Evaluation. 2nd edition Oxford, United Kingdom: Oxford University Press, 2003. [Google Scholar]
- 16.2018 BRFSS survey data and documentation. Centers for Disease Control and Prevention. https://www.cdc.gov/brfss/annual_data/annual_2018.html. Updated December 9, 2019. Accessed April 3, 2021.
- 17.Trogdon JG, Liu X, Reeder-Hayes KE, Rotter J, Ekwueme DU, Wheeler SB. Productivity costs associated with metastatic breast cancer in younger, midlife, and older women. Cancer. 2020;126 (18):4118–4125. 10.1002/cncr.33077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Centers for Disease Control and Prevention. Diabetes state burden toolkit. Atlanta, GA: Centers for Disease Control and Prevention; 2022. Technical report https://nccd.cdc.gov/Toolkit/DiabetesBurden/images/docs/technical_documentation.pdf. [Google Scholar]
- 19.Expectancy Data, The Dollar Value of a Day; 2018 Dollar Valuation.Kansas: Shawnee Mission, 2019.
- 20.Occupational employment and wage statistics. Bureau of Labor Statistics. https://www.bls.gov/oes/special.requests/oesm18all.zip. Accessed April 5, 2021.
- 21.Twardella D, Loew M, Rothenbacher D, Stegmaier C, Ziegler H, Brenner H. The diagnosis of a smoking-related disease is a prominent trigger for smoking cessation in a retrospective cohort study. J Clin Epidemiol. 2006;59(1):82–89. 10.1016/j.jclinepi.2005.05.003. [DOI] [PubMed] [Google Scholar]
- 22.Lindsay HG, Wamboldt FS, Holm KE, et al. Impact of a medical diagnosis on decision to stop smoking and successful smoking cessation. Chronic Obstr Pulm dis. 2021;8(3):360–370. 10.15326/jcopdf.2020.0167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.American community survey data. Demographic and housing estimates. U.S. Census Bureau; 2021. https://www.census.gov/programs-surveys/acs/data.html. [Google Scholar]
- 24.Baker CL, Flores NM, Zou KH, Bruno M, Harrison VJ. Benefits of quitting smoking on work productivity and activity impairment in the United States, the European Union and China. Int J Clin Pract. 2017;71(1):e12900. 10.1111/ijcp.12900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Sherman BW, Lynch WD. The relationship between smoking and health care, workers’ compensation, and productivity costs for a large employer. J Occup Environ Med. 2013;55(8):879–884. 10.1097/JOM.0b013e31829f3129. [DOI] [PubMed] [Google Scholar]
- 26.Caraballo RS, Giovino GA, Pechacek TF, Mowery PD. Factors associated with discrepancies between self-reports on cigarette smoking and measured serum cotinine levels among persons aged 17 years or older: third National Health and Nutrition Examination Survey, 1988–1994. Am J Epidemiol. 2001;153(8):807–814. 10.1093/aje/153.8.807. [DOI] [PubMed] [Google Scholar]
- 27.Darden ME, Hotchkiss JL, Pitts MM. The dynamics of the smoking wage penalty. J Health Econ. 2021;79:102485. 10.1016/j.jhealeco.2021.102485. [DOI] [PubMed] [Google Scholar]
- 28.Pike J, Grosse SD. Friction cost estimates of productivity costs in cost-of-illness studies in comparison with human capital estimates: a review. Appl Health Econ Health Policy. 2018;16(6):765–778. 10.1007/s40258-018-0416-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


