Abstract
Intraluminal thrombus adjunct to internal carotid artery plaque is a rare finding on traditional diagnostic imaging. Prompt diagnosis is important as it carries a high risk of recurrent stroke. We describe 2 symptomatic patients with severe stenosis on duplex scanning and internal carotid artery thrombus (ICAT) identified on subsequent computed tomographic angiography. Histology of the surgical specimen confirmed the composition predicted by computed tomography. Computed tomographic angiography can provide accurate diagnosis and characterization of internal carotid thrombus and lead to prompt therapeutic intervention.
Keywords: internal carotid thrombus, computed tomographic angiography, embolic stroke
Data from the North American Symptomatic Carotid Endarterectomy Trial (NASCET) study have demonstrated that the 30-day risk of recurrent stroke for symptomatic patients with internal carotid artery thrombus (ICAT), who are treated medically is 10.7% which is almost 5 times higher than in similar patients without intraluminal thrombus.1,2 The optimal diagnostic approach for this high-risk subgroup of patients is yet to be defined.3 In the literature, the prevalence of ICAT in patients with stroke ranges from 1/2000 (0.05%) by duplex ultrasound to 9/2250 (0.4%) by conventional angiography.4,5 We describe the first 2 cases of ICAT accurately defined by multidetector computed tomographic angiography (MD-CTA) imaging and correlated with intraoperative findings.
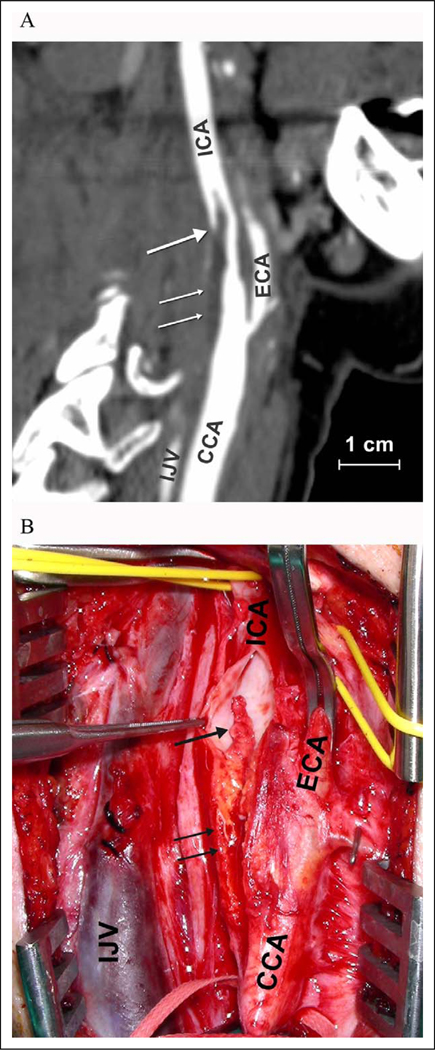
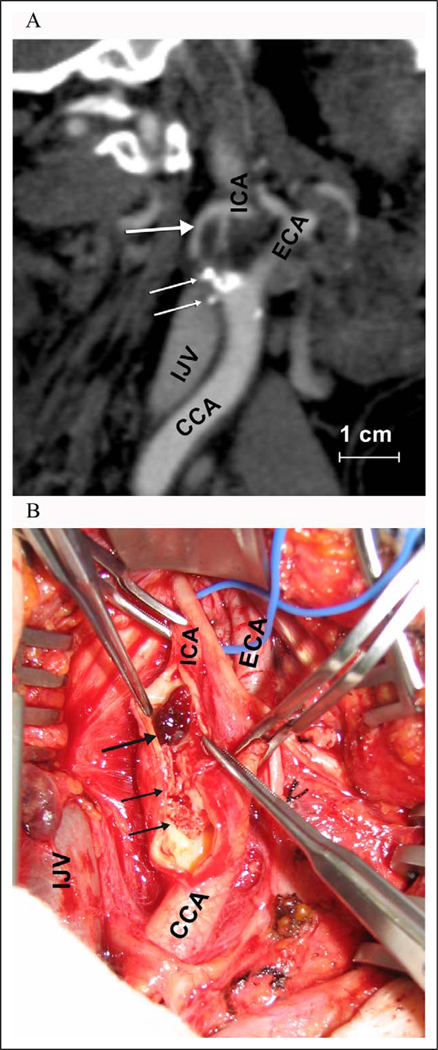
The first patient, a 59-year-old female, presented with a 2-week history of transient, recurrent episodes of left hemiparesis. Five years prior, she had radiation therapy to her neck for B-cell lymphoma. Magnetic resonance imaging (MRI) of her brain demonstrated multiple punctate ischemic infarcts in the right hemisphere. The second patient, a 68-year-old man, presented with acute left hemiparesis. Brain MRI showed a suba-cute stroke in the right middle cerebral artery distribution. Both patients had normal echocardiogram, electrocardiogram, and hypercoagulable studies. Carotid duplex ultrasound revealed significant right carotid artery stenosis (70%–99%) in both cases. In the first case, a MD-CTA confirmed a 70% carotid stenosis in the right internal carotid and revealed an associated 2-cm long pedicled thrombus (Figure 1A). The average computed tomographic number in the thrombus was 18 Hounsfield units (HU). In the second case, a MD-CTA showed a calcified plaque causing 80% stenosis of the proximal internal carotid artery and a 9-mm elongated thrombus attached to the plaque (Figure 2A). The average computed tomographic number in the thrombus was 73 HU. Both patients underwent urgent carotid thromboendarterectomy. In the first case, a 2-cm tan mobile thrombus attached to an ulcerated plaque at the carotid bulb was identified (Figure 1B), which on histology featured characteristics of organized thrombus consisting of platelets, fibrin, and neutrophils. In the second case, a dark red mobile thrombus measuring 1.1 cm attached to the distal end of the plaque was identified (Figure 2B). Histology showed fresh thrombus primarily consisting of erythrocytes attached to a ruptured plaque. Postoperatively, both patients had an uneventful recovery and almost complete resolution of neurologic symptoms at 3-month follow-up.
Figure 1.
A, Patient 1: MD-CTA, sagittal view of the right carotid bifurcation. A 2-cm long mobile thrombus (thick arrow) attached proximally to a mildly calcified plaque (thin arrows). B, Intraoperative findings after arteriotomy: a mobile thrombus (thick arrow) attached to an ulcerated plaque (thin arrows) at the carotid bulb was identified. CCA indicates common carotid artery; ECA = external carotid artery; ICA = internal carotid artery; IJV = internal jugular vein; MD-CTA = multidetector computed tomographic angiography.
Figure 2.
A, Patient 2: MD-CTA, sagittal view of the right carotid bifurcation. A mobile lesion measuring 9 mm (thick arrow) proximally attached to a highly calcified plaque (thin arrows) was identified. B, Arteriotomy confirmed a mobile thrombus (thick arrow) attached to an ulcerated calcified plaque (thin arrows) at the carotid bulb. CCA indicates common carotid artery; ECA = external carotid artery; ICA, internal carotid artery; IJV = internal jugular vein; MD-CTA = multidetector computed tomographic angiography.
The choice of optimal diagnostic testing in symptomatic patients with suspected ICAT is challenging, and advanced imaging modalities may offer new possibilities. In both patients, the detailed information obtained by MD-CTA following detection of severe stenosis on duplex ultrasound allowed for accurate diagnosis and prompt surgical treatment that resulted in safe and complete removal of the ICAT. Tissue characterization and thrombus detection by noninvasive plaque imaging with MD-CTA is an important field of research.6,7 Thrombi rich in platelets, fibrin, and leukocytes are relatively resistant to thrombolysis and have CT numbers of 24 + 8 HU, whereas thrombi rich in erythrocytes, which appear to be more susceptible to thrombolytic therapy, have computed tomographic numbers approximately 76 + 9 HU.7,8 These reports correlate with the imaging and histology findings in both cases. Further research is needed to explore the full potential of MD-CTA in the imaging of complex vascular pathology.
Funding
The author(s) disclosed receipt of the following financial support for the research and/or authorship of this article: This work was partially funded by grants from the National Institute of Biomedical Engineering and Imaging (RO1 EBO7986-01B) to Dr B. Kantor and from the National Heart, Lung, and Blood Institute (1 K08 HL079967-01) to Dr I. I. Pipinos.
Footnotes
Declaration of Conflicting Interests
The author(s) declared no conflicts of interest with respect to the authorship and/or publication of this article.
References
- 1.Beneficial effect of carotid endarterectomy in symptomatic patients with high-grade carotid stenosis. North American Symptomatic Carotid Endarterectomy Trial Collaborators. N Engl J Med. 1991;325(7):445–453. [DOI] [PubMed] [Google Scholar]
- 2.Villarreal J, Silva J, Eliasziw M, Meldrum HE, Barnett HJM, forthe North American Symptomatic Carotid Endarterectomy Trial (NASCET) Group. Prognosis of patients with intraluminal thrombus in the internal carotid artery. Stroke. 1998;29:276. [Google Scholar]
- 3.Bhatti AF, Leon LR Jr, Labropoulos N, et al. Free-floating thrombus of the carotid artery: literature review and case reports. J Vasc Surg. 2007;45(1):199–205. [DOI] [PubMed] [Google Scholar]
- 4.Arning C, Herrmann HD. Floating thrombus in the internal carotid artery disclosed by B-mode ultrasonography. J Neurol. 1988; 235(7):425–427. [DOI] [PubMed] [Google Scholar]
- 5.Biller J, Adams HP Jr, Boarini D, Godersky JC, Smoker WR, Kongable G. Intraluminal clot of the carotid artery. A clinical-angiographic correlation of nine patients and literature review. Surg Neurol. 1986;25(5):467–477. [DOI] [PubMed] [Google Scholar]
- 6.Gerber T, Kantor B, Williamson E. Computed Tomography of the cardiovascular System. Vol 29, London, UK: Informa Healthcare; 2008. [Google Scholar]
- 7.Kirchhof K, Welzel T, Mecke C, Zoubaa S, Sartor K. Differentiation of white, mixed, and red thrombi: value of CT in estimation of the prognosis of thrombolysis phantom study. Radiology.2003; 228(1):126–130. [DOI] [PubMed] [Google Scholar]
- 8.Kim EY, Heo JH, Lee SK, et al. Prediction of thrombolytic efficacy in acute ischemic stroke using thin-section noncontrast CT. Neurology. 2006;67(10):1846–1848. [DOI] [PubMed] [Google Scholar]