Abstract
Objective:
Traditionally, illness severity, social factors, and comorbid conditions have been examined as predictors of hospital outcomes. However, recent research in the rehabilitation setting demonstrated that physical function outperformed comorbidity indices as a predictor of 30-day readmission. The purpose of this study was to review the literature examining the association between acute hospital physical function and various hospital outcomes and health care utilization.
Type:
Systematic review.
Literature Survey:
A review of the MEDLINE database was performed. Search terms included acute functional outcomes and frailty outcomes. Studies up to September 2017 were included if they were in English and examined how functional metrics collected at acute care hospitalization affected hospital outcomes.
Methodology:
Cohort characteristics and measures of associations were extracted from the studies. Outcomes include hospital readmission, length of stay, mortality, discharge location, and physical function post acute care. The studies were assessed for potential confounders as well as selection, attrition, and detection bias.
Synthesis:
A total of 30 studies were identified (hospital readmissions: 6; discharge location: 11; length of stay: 4; mortality: 15; function: 6). Thirteen different metrics assessed function during acute care. Lower function during acute care was associated with statistically significant higher odds of hospital readmission, lower likelihood of discharge to home, longer hospital length of stay, increased mortality, and worse functional recovery when compared to patients with higher function during acute care, when adjusted for age and gender. The Barthel Index may be a useful marker for mortality in the elderly whereas the Functional Independence Measure instrument may be valuable for examining discharge location.
Conclusions:
There is increasing evidence that function measured during acute care predicts a broad array of meaningful clinical outcomes. Further research would help direct the use of practical, yet parsimonious functional metrics that effectively screen high-need, high-cost patients to deliver optimal care.
Level of Evidence:
I
Introduction
Predictors of hospital outcomes such as 30-day readmission, length of stay (LOS), mortality, and discharge location are multifactorial and difficult to assess. Poor hospital outcomes such as early hospital readmission remain a significant source of rising health care costs, leading to $52 billion in health care spending in 2013.1 It is valuable to identify patients who may be at high risk for a decline in health. Previous models for predicting health care utilization have incorporated variables such as demographic characteristics, insurance status, and comorbid medical conditions.2–6 Notably, the use of functional metrics has been comparatively lacking. Functional metrics are increasingly important as health care moves from binary outcomes such as mortality to meaningful metrics of survival and community participations such as cognitive outcomes. Functional metrics such as the Functional Independence Measure (FIM) correlate with burden of disease7 and demonstrate that moving toward patient-centered quality metrics more closely aligns with risk-adjusted payment systems that reflect health care utilizations.
There is a growing body of research in the inpatient rehabilitation setting that has examined functional metrics as predictors of acute hospital readmissions.8,9 Studies have shown that the FIM is a better predictor of 30-day readmission compared to comorbidity indices alone.10,11 Recent research has also highlighted the importance of early mobility, and there is increasing interest to see whether functional status measures in the acute care setting are significant predictors of various hospital outcomes.12–14 Just as functional status plays a central role in the rehabilitation setting, it may be important to include functional assessment as a more routine part of acute hospital evaluation as well. Patients with acute medical episodes such as sepsis have been shown to experience rapid functional decline with long-lasting dysfunction.15 As such, early assessment of function as a predictor for poor health outcomes is critical and can meaningfully inform and direct care.
The purpose of this review was to examine the role of functional metrics during acute care on hospital outcomes in published literature to date. We hypothesized that lower functional status during the acute hospital admission would be associated with increased risk of hospital readmission, lower likelihood of discharge to home compared to inpatient rehabilitation, increased postacute mortality, and lower functional status post acute care.
Materials and Methods
Search Strategy
A systematic review of the MEDLINE database was performed in September 2017. A search term was constructed using the following phrases: “acute functional assessment outcome”; “acute functional predictor outcome”; “acute functional status outcome”; “acute functional metric outcome”; “acute functional assessment length of stay”; “acute functional predictor length of stay”; “acute functional status length of stay”; “acute functional metric length of stay”; “acute functional assessment disposition”; “acute functional predictor disposition”; “acute functional status disposition”; “acute functional metric disposition”; “acute functional assessment readmission”; “acute functional predictor readmission”; “acute functional status readmission”; “acute functional metric readmission”; and “frailty functional outcome.”
The titles were first screened to see whether the study was clinically relevant to the scope of the study. The abstracts were then reviewed. Inclusion criteria were English language, measurement of function in the acute hospital setting, and primary outcome related to readmission, mortality, length of stay, discharge location, or physical functional status post acute care. After applying the inclusion criteria, the remaining studies were examined in full. The references for each included study were also assessed. We extracted functional metrics (FIM, AcuteFIM, activities of daily living [ADL] dependencies/scores, Barthel Index[BI], Modified BI), clinical covariates (location prior to admission, number of medications, social isolation, depression, comorbidities, length of stay, discharge location, Glasgow outcome scale, NIH Stroke Score [NIHSS], Acute Physiology and Chronic Health Evaluation [APACHE] score, cognition scores), demographic data (gender, race, body mass index, education, age), and clinical outcomes (readmission, discharge location, length of stay, mortality, and function). Odds ratios, risk ratios, hazard ratios, and linear regression beta coefficients were reported when available. The final study population consisted of 30 studies.12–14,16–42 The quality and methodologies of the studies were assessed using adapted criteria from the Cochrane Handbook.43 Studies were categorized based on the risk of confounding, selection bias, attrition bias, and detection bias. Risk of confounding was based on the number of covariates accounted for. Concern for selection bias was assessed by whether the authors defined inclusion and exclusion criteria, whether the population was representative, and whether there exposure was ascertained. Detection bias accounted for standardized outcome measurements, blinding, quality, and recall bias.
Results
Study Characteristics
A total of 30 studies were identified12–14, 16–42 (Table 1). Six studies reported on hospital readmissions,14,18,25,28,38,41 11 reported on discharge location,19,20,23,25,26,28,32–34,39,40 4 reported on length of stay,16,25,39,40 15 reported on mortality,13,17,20–22,24,25,27,29,30,35–38,42 and 6 reported on function postacute care.12,31,32,36,38,42 Three of the studies examined trauma patients,13,31,347studies examined stroke patients,19,23,26,28,35,40,41 and 18 studies examined elderly patients.12–14,16–18,21,22,24,25,27,28,30,32,36–38,42 Thirteen functional metrics were used: BI (best to worst score of 100–0), BI (20–0), the modified BI, Katz ADL, Lawton ADL, Global ADL, Braden Activity Scale, the number of ADL and IADL (instrumental activities of daily living) dependencies, the Short Physical Performance Battery walking activity, the number of steps/day, AcuteFIM, and FIM (Figure 1). The majority of the studies were of moderate to poor quality with a moderate to high risk of detection bias and a significant number of missing covariates and confounders (Table 2).
Table 1.
Characteristics of studies contributing to each hospital outcome
| Studies with multiple outcomes measured | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Hospital outcome measured |
||||||||||||
| Author | Year | Sample size | LOE | Mean age (SD) | Patient type | Functional metric | Re-admission | Discharge location | LOS | Mortality | Physical function post-acute care | Key findings |
|
| ||||||||||||
| Barnes | 2013 | 449 | 2 | NR (NR) | Elderly | ADL | – | – | – | Yes | Yes | Key predictors of recovery (dependence or death) were age, gender, number of IADL dependencies 2 wk prior to admission, number of ADL dependencies at discharge, dementia, cancer, number of other chronic conditions, reason for admission, and creatinine levels |
| Bohannon | 2002 | 92 | 2 | 70.0 (12.4) | Acute stroke | BI | – | Yes | Yes | – | – | Postadmission Barthel Index scores are predictors of the hospital length of stay, hospital charges, and hospital discharge destination |
| Choo | 2006 | 36 | 3 | 47.3 (17.4) | Burns | FIM | – | Yes | Yes | – | – | A discharge FIM score of 110 or lower was strongly associated with the need for inpatient rehabilitation, whereas a FIM score greater than 110 indicates the patient is independent enough to be managed at home |
| Corsonello | 2012 | 506 | 2 | 80.1 (5.9) | Elderly | SPPB | Yes | – | – | Yes | Yes | Higher SPPB score was associated with reduced 1 y mortality and functional decline, but not readmission |
| Covinsky | 2000 | 2877 | 2 | 80.5 (NR) | Elderly | Katz ADL | – | – | – | Yes | Yes | The number of ADLs reported as dependent 2 wk before admission was significantly associated with 1-y mortality and functional independence 3 mo after hospitalization; the number of ADLs reported as dependent on admission was not associated with 1-y mortality among patient respondents |
| Fortinsky | 1999 | 551 | 2 | 80 (7) | Elderly | ADL | – | Yes | – | – | Yes | Patients in the decline-no improvement group and patients in the stable-decline group were at greater risk for nursing home admission than patients in the stable-stable group. |
| Kane | 1998 | 1093 | 2 | NR (NR) | Elderly with strokes or hip fractures | ADL | Yes | Yes | – | – | – | For both stroke and hip patients, greater ADL disability was associated with discharge to nursing homes and rehabilitation; discharge to nursing home and rehabilitation was associated with greater 1 y readmission |
| Narain | 1988 | 396 | 2 | 76.9 (0.34) | Elderly | Lawton ADL | Yes | Yes | Yes | Yes | – | Functional status was a stronger predictor of length of stay, mortality, and nursing home placement than principal admitting diagnosis |
| Sood | 2011 | 1286 | 2 | NR (NR) | Dialysis | Katz ADL | – | Yes | – | Yes | – | A single ADL score measurement at admission combined with age was highly predictive of poor outcomes in the hospitalized dialysis population. |
| Studies examining re-admission only | ||||||||||||
| Bohannon | 2004 | 228 | 2 | 70.6 (NR) | Acute stroke | BI | Yes | – | – | – | – | Lower prestroke and postadmission physical functioning were weak but significant predictors of readmission at 1 y |
| Fisher | 2016 | 164 | 2 | 76.2 (7.0) | Elderly | Katz ADL, steps | Yes | – | – | – | – | Walking activity during hospitalization was more strongly and significantly associated with 30-d readmission than ADL function after adjusting for readmission risk factors |
| Tonkikh | 2016 | 559 | 2 | 78.8 (5.6) | Elderly | mBI | Yes | – | – | – | – | Higher in-hospital ADL decline was significantly associated with 30 d readmission |
| Studies examining discharge location only | ||||||||||||
| Emhoff | 1991 | 109 | 2 | NR (NR) | Trauma | FIM | – | Yes | – | – | – | Patients who were discharged to home had a statistically greater improvement of FIM scores from admission to discharge compared to patients who were discharged to a rehabilitation facility |
| Farrell | 2006 | 202 | 2 | 42.6 (17.8) | Burns | FIM | – | Yes | – | – | – | Patients with a FIM locomotion score of 4 or greater were likely to be discharged to home, whereas those with scores 3 or lower were likely discharged to another setting |
| Mauthe | 1996 | 279 | 2 | 72.9 (NR) | Stroke | FIM | – | Yes | – | – | – | FIM scores were statistically different among patients who were discharged home vs. nursing home vs. rehabilitation. Bathing, bowel, toileting, social interaction, dressing lower body, and eating FIM scores predicted disposition with 70% accuracy |
| Roberts | 2016 | 481 | 3 | 69.0 (23.3) | Stroke | AcuteFIM | – | Yes | – | – | – | Higher AcuteFIM score was associated with discharge to the home/assisted living community from the acute hospital |
| Stein | 2015 | 736 | 2 | 68.9 (14.8) | Stroke | BI | – | Yes | – | – | – | Higher BI score was associated with discharge to home vs. discharge to a rehabilitation facility |
| Studies examining length of stay only | ||||||||||||
| Volpato | 2008 | 157 | 2 | 77.7 (6.4) | Elderly | SPPB | – | – | Yes | – | – | In the elderly, a higher SPPB score at admission is associated with shorter length of stay when adjusted for age, gender, and illness severity |
| Studies examining mortality only | ||||||||||||
| Covinsky | 1997 | 823 | 2 | 80.7 (NR) | Elderly | ADL | – | – | – | Yes | – | Patients dependent in 4+ ADLs were at statistically significant greater risk of hospital mortality, 1-y mortality, and 90-d nursing home use compared to those with no ADL dependence when adjusted for APACHE score, Charlson comorbidity index, age, race, and gender |
| Davis | 1995 | 2169 | 3 | NR (NR) | CVA and PNA | ADL | – | – | – | Yes | – | Patients that required total assistance for bathing was associated with increased in-hospital mortality for patients with cerebrovascular accidents when adjusted for gender, age, and lactic dehydrogenase levels and for patients with pneumonia when adjusted for gender, age, metastatic cancer, and blood urea nitrogen levels |
| Socorro Garcia | 2015 | 434 | 2 | 94.0 (3.0) | Elderly | BI | – | – | – | Yes | – | Greater functional impairment at admission measured by the BI was associated with increased odds of 30 d mortality |
| Inouye | 1998 | 318 | 2 | 79.0 (6.0) | Elderly | IADL | – | – | – | Yes | – | Patients with any IADL impairment had an increased relative risk of 2 y mortality compared to patients without IADL impairment |
| Justice | 1996 | 1003 | 2 | NR (NR) | AIDS | Global ADL | – | – | – | Yes | – | Greater ADL dependency was associated with increased hazard rates of hospital mortality when CD4 cell count, clinical AIDS prognostic staging and severity classification for AIDS hospitalization were held constant |
| Matzen | 2012 | 5087 | 2 | 81.8 (6.8) | Elderly | BI | – | – | – | Yes | – | Patients with lower BI scores had lower odds of 3 mo and 1 y survival compared to patients with BI scores of 81–100 when adjusted for gender, age, Charlson Comorbidity Index, and past medical history |
| Ostir | 2013 | 224 | 2 | NR (NR) | Elderly | Steps | – | – | – | Yes | – | A decline in the number of steps taken per day when comparing last 24 h to first 24 h of hospitalization was associated with an increased hazard rate of 2-y mortality |
| Rozzini | 2005 | 950 | 2 | 78.3 (8.5) | Elderly | BI | – | – | – | Yes | – | A decrease in BI scores when comparing function 2 wk prior to admission to function at admission was associated with increased relative risk of 6-mo mortality |
| Torres | 2004 | 99 | 2 | NR (NR) | Elderly with PNA | BI | – | – | – | Yes | – | Higher BI scores were associated with lower 30-d and 1.5-y mortality when Charlson Comorbidity Index, age, living in residential home, aspiration pneumonia, pneumonia severity index, and hospital admission risk profile were held constant |
| Valiani | 2017 | 19 769 | 3 | 74.7 (7.5) | Elderly, trauma | BAS | – | – | – | Yes | – | Elderly patients who developed mobility impairment during hospitalization had higher odds of death compared to those who remained mobile when age, gender, race, and length of stay were held constant |
| Studies examining physical functional status post-acute care only | ||||||||||||
| Gabbe | 2008 | 243 | 2 | NR (NR) | Trauma | FIM | – | – | – | – | Yes | Higher FIM motor scores at hospital discharge were associated with greater odds of returning to work/study at 6 mo |
| Zaslavsky | 2015 | 691 | 2 | 79.9 (5.8) | Elderly | mBI | – | – | – | – | Yes | Patients who remained stable before and during hospitalization had the highest odds of maintaining their premorbid functional levels at 1 mo. Those who experienced functional improvement during hospitalization, despite previous functional loss, were 2.3–2.9 times more likely than persistent decliners to experience 1-mo functional recovery |
NR = not reported; CVA = cerebrovascular accident; PNA = pneumonia; ADL = activities of daily living; IADL = instrumental activities of daily living; BI = Barthel Index; mBI = modified Barthel Index; FIM = Functional Independence Measure; SPPB = Short Physical Performance Battery; LOE = level of evidence; BAS = Braden Activity Subscale.
Figure 1.
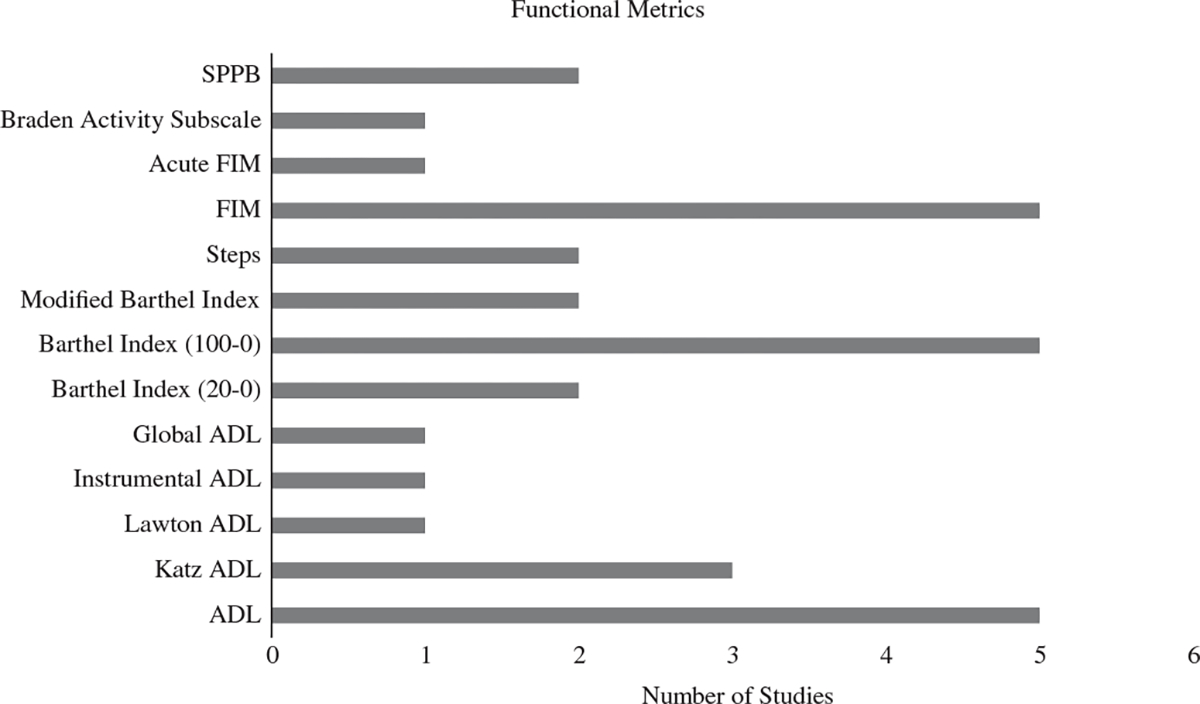
Functional metrics measured in the acute care setting. SPPB = short physical performance battery; FIM = Functional Independence Measure; ADL = activities of daily living.
Table 2.
Quality assessment for included studies
| Author | Year | Quality assessment |
|||
|---|---|---|---|---|---|
| Confounder | Selection bias | Attrition bias | Detection bias | ||
|
| |||||
| Barnes | 2013 | Moderate | Mild | <10% | Moderate |
| Bohannon | 2004 | Moderate | Mild | Not reported | Moderate |
| Bohannon | 2002 | High | Mild | Not reported | Moderate |
| Choo | 2006 | High | Moderate | <10% | Moderate |
| Corsonello | 2012 | Moderate | Mild | <10% | Moderate |
| Covinsky | 2000 | Moderate | Mild | >20% | High |
| Covinsky | 1997 | Moderate | Moderate | Not reported | Moderate |
| Davis | 1995 | High | Mild | <10% | Moderate |
| Emhoff | 1991 | High | Mild | Not reported | Moderate |
| Farrell | 2006 | High | Mild | Not reported | Moderate |
| Fisher | 2016 | Mild | Mild | 10%–20% | High |
| Fortinsky | 1999 | Moderate | Mild | <10% | High |
| Gabbe | 2008 | Moderate | Mild | <10% | High |
| Socorro Garcia | 2015 | Moderate | Mild | Not reported | Moderate |
| Inouye | 1998 | Moderate | Mild | >20% | Mild |
| Justice | 1996 | Moderate | Mild | >20% | Moderate |
| Kane | 1998 | Moderate | Moderate | >20% | Moderate |
| Matzen | 2012 | High | Mild | 10%–20% | Moderate |
| Mauthe | 1996 | High | Mild | Not reported | Moderate |
| Narain | 1988 | Moderate | Mild | <10% | High |
| Ostir | 2013 | Moderate | Mild | Not reported | Moderate |
| Roberts | 2016 | Moderate | Mild | Not reported | Moderate |
| Rozzini | 2005 | Moderate | Mild | 10%–20% | High |
| Sood | 2011 | Moderate | Mild | <10% | Moderate |
| Stein | 2015 | Moderate | Mild | 10%–20% | High |
| Tonkikh | 2016 | Mild | Mild | 10%–20% | Moderate |
| Torres | 2004 | Moderate | Mild | <10% | High |
| Valiani | 2017 | Moderate | Moderate | Not reported | Moderate |
| Volpato | 2008 | Moderate | Mild | <10% | High |
| Zaslavsky | 2015 | Moderate | Mild | <10% | High |
Confounder risk:
Mild: 8 or more covariates/possible confounders accounted for.
Moderate: 4–7 covariates/possible confounders accounted for.
High: 0–3 covariates/possible confounders accounted for.
Selection bias (inclusion/exclusion criteria, representative population, ascertainment of exposure):
Mild: 0 areas of concern.
Moderate: 1 area of concern.
High: 2 or more areas of concern.
Detection bias (standardized outcome measurement, blinding, quality of reporting source, recall bias):
Mild: 0 areas of concern.
Moderate: 1 area of concern.
High: 2 or more areas of concern.
Outcomes
Gender, age, cognition level, and existing comorbidities are significant predictors or confounders of physical function and hospital outcomes so ideally all studies would adjust for these variables.44,45 Gender and age were frequently reported among the eligible studies. However, only a limited number of studies adjusted for cognition and comorbidities, so measures of associations were extracted if the authors adjusted for gender and age, even if cognition and comorbidities were not included in the model. Other potential confounders such as social isolation, depression, and body mass index (BMI) were infrequently reported so it was not a requisite for inclusion.
Three of four studies14,18,41 that examined hospital readmission odds ratios reported that patients with higher function during acute hospital care had statistically significant lower odds of readmission compared to patients with lower function when adjusted for gender and age (Figure 2); one study also adjusted for existing comorbidities41; one study also adjusted for cognition and existing comorbidities18 (Table S1). All four studies19,20,23,32 that compared the odds of discharge to skilled nursing facilities (SNF) and inpatient rehabilitation facilities (IRF) found that patients with a decline in function/lower function during acute care had statistically significant higher odds of discharge to SNF/IRF compared to patients with higher function when adjusted for age and gender (Figure 2); two of the four also adjusted for cognition. One study used medical records to screen for dementia32 and the other used the Short Portable Mental Status Questionnaire (SPMSQ).19 The SPMSQ46 has moderate sensitivity to mild cognitive deficits and is limited by the number of cognitive domains that it evaluates.47 Two other studies also adjusted for comorbidities20,32 (Table S1). All three studies16,25,39 that reported mean LOS or the linear regression coefficient for LOS noted that patients with higher function during acute care had statistically significant shorter length of stays compared to patients with lower function when adjusted for gender and age (Figure 2); two of the three studies also adjusted for cognition and comorbidity16,25 (Table S1). Thirteen of 14 studies13,17,20–22,24,27,29,30,35,37,38,42 that reported odds ratios, hazard ratios, or relative risk ratios demonstrated that higher function during acute care had statistically significant decreased odds, relative risks, or hazard rates of mortality compared to patients with lower function when adjusted for age and gender (Figure 2); 12 of the 13 also adjusted for comorbidities13,17,20–22,24,27,29,30,37,38,42 and 7 of the 13 also adjusted for cognition17,21,22,30,35,38,42 (Table S1). All four studies12,31,38,42 that reported odds ratios found that patients with higher function during acute care had statistically significant higher odds of functional independence/recovery compared to patients with lower function when adjusted for age, gender, and comorbidities (Figure 2); three of the four also adjusted for cognition12,38,42 (Table S1).
Figure 2.
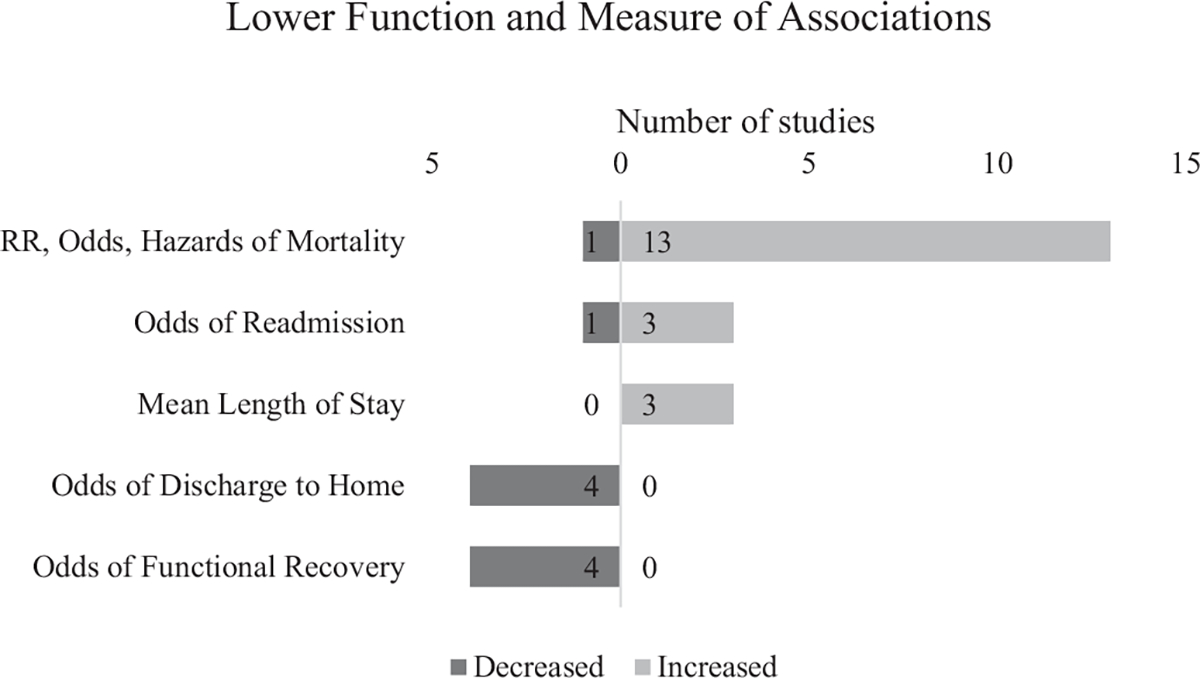
Association between lower function and various measures of associations. RR = relative risk. All reported measures of associations are from the original manuscripts without independent statistical analysis or calculations.
The most frequently used metrics among the 30 studies were BI (best to worst score of 100–0) and the FIM. BI and FIM were each used in five studies (Table S2). Four of five studies that used BI reported on mortality rates adjusted for age, gender, and comorbidities in the elderly patients,17,21,22,27 and three of the four also adjusted for cognition.17,21,22 All four studies found that patients in the highest functioning category had statistically significant lower mortality rates when compared to patients with the lowest functional score category when adjusted for age, gender, and comorbidities; the four studies had varied time periods ranging from 30 days to 1.5 years. The remaining study19 examined discharge location for stroke patients using BI (a score of 100 represents full independence) and reported that patients with a BI of 65 to 80 have 9.43 (5.10–15.54) times the odds of discharge to SNF/IRF compared to patients with a BI of 85 to 100 when adjusted for demographic and clinical characteristics.
Of the five studies that used the FIM, two examined trauma patients,31,34 two examined patients with burns,33,39 one examined stroke patients26; four studied how function affects discharge location26,33,34,39 and one assessed function post acute care.31 Higher FIM scores were associated with greater likelihood of discharge to home and function post acute care in the trauma, burn, and stroke population. One study demonstrated that in the burn population, when the FIM score is greater than 110, the likelihood of discharge to home is statistically significant (P value <.0001).39 (Table S2).
Discussion
Our review of the literature demonstrates that functional measures obtained in the acute hospital setting can be important predictors of health care utilization and clinical outcomes in the acute care setting and points to the importance of including these measures in future studies of health care utilization, including readmissions, length of stay, discharge location, mortality, functional status, and postacute care utilization. Immobility has profound impacts on short-term and long-term health,12–14 and there has been a number of studies evaluating the role of function prior to hospitalization and in the rehabilitation setting. However, the role of functional metrics in the acute care setting has historically been understudied. As the body of work assessing the role of function metrics in the acute care setting grows, we can better evaluate the impact on readmission, costs, and patient centered outcomes. Recent studies by Fisher et al, Valiani et al, and Zaslavsky et al found that early mobility and functional recovery in the acute care setting reduces mortality, improves physical function after hospital discharge, and decreases hospital readmissions.12–14 Together, these studies suggest that early functional recovery improves hospital outcomes and decreases health care utilization. More important, as quality measures expand to encompass more granular outcomes and facets of patient experience across episodes of care,48 physical function demonstrates value as an outcome measure with meaningful patient benefit that translates across health care settings because improved physical function has been associated with a faster return to community participation, decreased patient costs, and less time spent in the hospital.
We found that there is strong evidence that functional metrics such as BI and FIM are significant predictors of multiple hospitals outcomes. Lower functional status during acute care was associated with worse hospital outcomes: increased readmission, lower likelihood of discharge to home, increased mortality, and poorer functional status post acute care. However, given the disparate and heterogeneous data, it remains unclear which functional metrics are best suited for different subsets of patients or for a given outcome. Nonetheless, both BI and FIM have been used to evaluate mortality and discharge location, so additional research examining how functional status using these measures in acute care impact readmission and length of stay would be valuable because these outcomes have not been closely investigated. Early interventions may disproportionately benefit certain populations such as the elderly and cognitively impaired49,50 who are at greater risk of avoidable complications and unnecessary health care costs.
The available evidence suggests that BI may be a useful tool to predict mortality in the elderly population. All four studies17,21,22,27 that examined BI reported moderate clinical significance and varying levels of statistical significance depending on the categorical group. A systematic review by Sainsbury et al recommends that BI is appropriate for use in the elderly population but also concludes that the reliability of the metric remains unknown in the elderly.51 Because the four studies17,21,22,27 that used BI in the elderly population all examined mortality, it would be valuable for future research to assess whether its use during acute care can predict other meaningful clinical outcomes such as hospital readmissions, avoidable complications, and overall costs of care. The BI has a number of limitations: evaluators need training to differentiate between “minor” and “major” dependence and the lengthy questionnaire hinders widespread use. Therefore, patients in the acute setting may benefit from a shorter screening tool prior to evaluation with the BI.
The FIM may be a useful tool to predict discharge location. Four studies26,33,34,39 investigated the utility of the FIM to predict discharge location and found a clinically significant association between higher FIM scores and discharge to home. Given the paucity of available literature, it is difficult to conclude what patient population the FIM is most appropriate for in the acute setting. Further work in the trauma, burn, and stroke populations would be beneficial to see if these results are reproducible, and additional research in the general medicine and surgical populations would enhance generalizability. In addition to conventional clinical outcomes such as readmission and mortality, newer care models such as accountable care organizations (ACOs) have incorporated basic measures of functional status (climbing stairs, dressing/bathing, and visiting a doctor’s office alone)52 in consumer surveys to track population health outcomes across the care continuum.53 For the subset of patients who transfer from acute care to IRF, use of the FIM in the two settings would enhance continuity of care, help evaluate patients as they progress, and aid with hospitalization resource management. However, conducting the FIM has similar drawbacks as the BI, including requiring training and a lengthy set of questions. The FIM also has ceiling effects in patients with dementia or severe brain injury,54 where executive impairment can limit the patient’s ability and safety despite intact physical function. In addition, the FIM has floor effects for patients with neuromuscular diseases or spinal cord injuries,55 where they can score low on the FIM without assistive devices but high when they have the appropriate support. Novel, standardized functional metrics such as the AM-PAC 6-Clicks Score that evaluates patient mobility and function with only six clicks may represent the future of physical functional assessment. The AM-PAC 6-Clicks score uses algorithms that automatically adjust the questions based on the patient’s response, allowing it to incorporate the breadth of functional classification while maintaining clinical efficiency and responsiveness. As AM-PAC 6-Clicks continue to be adopted by major health systems, it may serve as an important next step in linking function to clinical outcomes.56
This systematic review has a number of limitations. There was significant heterogeneity in the 30 eligible studies. Within each clinical outcome, few studies used the same functional metric, so it was difficult to compare studies or draw an aggregate conclusion regarding the predictive role of function. The methodology did not restrict eligible studies based on study design, which limits the strength of the findings. Furthermore, because of the scarcity of eligible studies, studies that did not adjust for potential confounders such as comorbid conditions and cognition still had their measures of associations reviewed. Eligible studies were not restricted by the sample size or population type due to the limited available studies. Because comorbid conditions and decreased cognition would likely cause the crude measure of association to be greater than the adjusted value (bias away from the null), the reported odds ratios are likely overestimating the true measure of association. Finally, the moderate to poor quality level of evidence also limits the strength of the findings and conclusions. In spite of these limitations, this study represents a valuable contribution to the literature because functional metrics are not routinely collected as part of acute care hospital clinical care and administrative datasets. This study represents an important step in understanding the value of functional metrics in acute care.
Future efforts at standardizing and systematically collecting functional data will be essential to further understand the relationship between functional status and the aforementioned outcomes.4,57,58 There is limited information on when measuring functional status is most meaningful. For example, although functional status prior to hospitalization has been shown to be predictive of hospital readmission,59 it is unclear whether initial admission functional status, change in function, or function prior to discharge is most predictive of health care utilizations. Further work would help elucidate this relationship and would also establish continuity of care. Two of the challenges of performing the BI or FIM on every patient in the acute setting is the additional training required to accurately evaluate patients and maintaining interrater reliability when using these functional measures. Nevertheless, collaboration among different disciplines, settings, and caregivers can help balance clinical variations and the burden of data collection on providers given the universal importance of evaluating physical function. It may be valuable for clinicians to use shortened functional metrics such as the AcuteFIM or the AM-PAC 6-Clicks Score56,60 as a screening tool. However, future more widespread use will need to balance the benefit of existing evidence that supports metrics that have logistical challenges of implementation, with newer measures that have not been as widely studied but offer easier large-scale administration.
Conclusion
Although this review was limited by the heterogeneity of functional measures and hospital outcomes, there is a growing body of evidence that functional metrics assessed in acute care are significant predictors of a broad array of hospital outcomes. The BI and FIM have been used to predict mortality and discharge location, but their clinical use is limited by the lengthy questions and required training. Newer adaptive-algorithmic tools such as the AM-PAC 6-Click that assess physical function may be easier to implement. Future research would benefit from more widespread, standardized collection of functional data and recommended functional metrics for use in acute care hospitals.
Supplementary Material
Acknowledgments
Disclosure
C.S. Department of Physical Medicine and Rehabilitation, Spaulding Rehabilitation Hospital, Boston, MA; and University of Maryland School of Medicine, Baltimore, MD
Disclosure: Grants, National Institute on Disability, Independent Living, and Rehabilitation Research (Grant numbers 90DPBU0001, 90DPTB0011, 90S15021)
D.E.L. Department of Medicine, Massachusetts General Hospital, Boston, MA; and Harvard Medical School, Boston, MA Disclosure: Nothing to disclose
C.S.S. Department of Physical Medicine and Rehabilitation, Spaulding Rehabilitation Hospital, Boston, MA; and Harvard Medical School, Boston, MA Disclosure: Grants, National Institute on Disability, Independent Living, and Rehabilitation Research (Grant numbers 90DPBU0001, 90DPTB0011, 90S15021)
R.D.Z. Department of Physical Medicine and Rehabilitation, Spaulding Rehabilitation Hospital, Boston, MA; Department of Medicine, Massachusetts General Hospital, Boston, MA; and Harvard Medical School, Boston, MA
Disclosure related to this publication: Grants, National Institute on Disability, Independent Living, and Rehabilitation Research (Grant numbers 90DPBU0001, 90DPTB0011, 90S15021)
Disclosure outside this publication: Board membership, Oxeia Biopharma, ElMINDA, Myomo; grant, Avanir; royalties, Demos, Oakstone (money to author) J.C.S. Department of Physical Medicine and Rehabilitation, Spaulding Rehabilitation Hospital, Boston, MA; and Harvard Medical School, Boston, MA. Address correspondence to: J.C.S.; e-mail: jcschneider@partners.org
Disclosure related to this publication: Dept of HHS, National Institute on Disability, Independent Living, and Rehabilitation Research (grant number 90DPBU0001)
Disclosure outside this publication: Grant, Dept of HHS, NIDILRR (#90DP0055); royalties, Oakstone Publishing
The contents of this manuscript were developed under a grant from the National Institute on Disability, Independent Living, and Rehabilitation Research (NIDILRR grant numbers 90DPBU0001, 90DPTB0011, 90S15021). NIDILRR is a center within the Administration for Community Living (ACL), Department of Health and Human Services (HHS). The contents of this manuscript do not necessarily represent the policy of NIDILRR, ACL, HHS, and you should not assume endorsement by the Federal Government
All financial disclosures and CME information related to this article can be found on the mē® site (http://me.aapmr.org/) prior to accessing the activity.
Footnotes
Supporting Information
Additional supporting information may be found online in the Supporting Information section at the end of the article.
Contributor Information
Conan So, Department of Physical Medicine and Rehabilitation, Spaulding Rehabilitation Hospital, Boston, MA; University of Maryland School of Medicine, Baltimore, MD.
Daniel E. Lage, Department of Medicine, Massachusetts General Hospital, Boston, MA; Harvard Medical School, Boston, MA.
Chloe S. Slocum, Department of Physical Medicine and Rehabilitation, Spaulding Rehabilitation Hospital, Boston, MA; Harvard Medical School, Boston, MA.
Ross D. Zafonte, Department of Physical Medicine and Rehabilitation, Spaulding Rehabilitation Hospital, Boston, MA; Department of Medicine, Massachusetts General Hospital, Boston, MA; Harvard Medical School, Boston, MA.
Jeffrey C. Schneider, Department of Physical Medicine and Rehabilitation, Spaulding Rehabilitation Hospital, Boston, MA; Harvard Medical School, Boston, MA..
References
- 1.Fingar K, Washington R. Trendsin Hospital Readmissions for Four High-Volume Conditions, 2009–2013. Healthcare Cost and Utilization Project (HCUP); 2015. https://www.hcup-us.ahrq.gov/reports/statbriefs/sb196-Readmissions-Trends-High-Volume-Conditions.jsp. Accessed October 31, 2017. [Google Scholar]
- 2.Menendez ME, Ring D, Harris MB, Cha TD. Predicting in-hospital mortality in elderly patients with cervical spine fractures: a comparison of the Charlson and Elixhauser comorbidity measures. Spine (Phila Pa 1976). 2015;40(11):809–815. [DOI] [PubMed] [Google Scholar]
- 3.Karres J, Heesakkers NA, Ultee JM, Vrouenraets BC. Predicting 30-day mortality following hip fracture surgery: evaluation of six risk prediction models. Injury. 2015;46(2):371–377. [DOI] [PubMed] [Google Scholar]
- 4.Kansagara D, Englander H, Salanitro A, et al. Risk prediction models for hospital readmission: a systematic review. JAMA. 2011;306(15):1688–1698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Holman CD, Preen DB, Baynham NJ, Finn JC, Semmens JB. A multipurpose comorbidity scoring system performed better than the Charlson index. J Clin Epidemiol. 2005;58(10):1006–1014. [DOI] [PubMed] [Google Scholar]
- 6.Knaus WA, Wagner DP, Draper EA, et al. The APACHE III prognostic system. Risk prediction of hospital mortality for critically ill hospitalized adults. Chest. 1991;100(6):1619–1636. [DOI] [PubMed] [Google Scholar]
- 7.Heinemann AW, Kirk P, Hastie BA, et al. Relationships between disability measures and nursing effort during medical rehabilitation for patients with traumatic brain and spinal cord injury. Arch Phys Med Rehabil. 1997;78(2):143–149. [DOI] [PubMed] [Google Scholar]
- 8.Ottenbacher KJ, Karmarkar A, Graham JE, et al. Thirty-day hospital readmission following discharge from postacute rehabilitation in fee-for-service Medicare patients. JAMA. 2014;311(6):604–614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kumar A, Karmarkar AM, Graham JE, et al. Comorbidity indices versus function as potential predictors of 30-day readmission in older patients following Postacute rehabilitation. J Gerontol A Biol Sci Med Sci. 2017;72(2):223–228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Shih SL, Zafonte R, Bates DW, et al. Functional status outperforms comorbidities as a predictor of 30-day acute care readmissions in the inpatient rehabilitation population. J Am Med Dir Assoc. 2016;17(10):921–926. [DOI] [PubMed] [Google Scholar]
- 11.Fisher SR, Graham JE, Krishnan S, Ottenbacher KJ. Predictors of 30-day readmission following inpatient rehabilitation for patients at high risk for hospital readmission. Phys Ther. 2016;96(1):62–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Zaslavsky O, Zisberg A, Shadmi E. Impact of functional change before and during hospitalization on functional recovery 1 month following hospitalization. J Gerontol A Biol Sci Med Sci. 2015;70(3):381–386. [DOI] [PubMed] [Google Scholar]
- 13.Valiani V, Chen Z, Lipori G, Pahor M, Sabba C, Manini TM. Prognostic value of Braden activity subscale for mobility status in hospitalized older adults. J Hosp Med. 2017;12(6):396–401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Fisher SR, Graham JE, Ottenbacher KJ, Deer R, Ostir GV. Inpatient walking activity to predict readmission in older adults. Arch Phys Med Rehabil. 2016;97(suppl 9):S226–S231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Prescott HC, Angus DC. Enhancing recovery from sepsis: a review. JAMA. 2018;319(1):62–75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Volpato S, Cavalieri M, Guerra G, et al. Performance-based functional assessment in older hospitalized patients: feasibility and clinical correlates. J Gerontol A Biol Sci Med Sci. 2008;63(12):1393–1398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Torres OH, Munoz J, Ruiz D, et al. Outcome predictors of pneumonia in elderly patients: importance of functional assessment. J Am Geriatr Soc. 2004;52(10):1603–1609. [DOI] [PubMed] [Google Scholar]
- 18.Tonkikh O, Shadmi E, Flaks-Manov N, Hoshen M, Balicer RD, Zisberg A. Functional status before and during acute hospitalization and readmission risk identification. J Hosp Med. 2016;11(9):636–641. [DOI] [PubMed] [Google Scholar]
- 19.Stein J, Bettger JP, Sicklick A, Hedeman R, Magdon-Ismail Z, Schwamm LH. Use of a standardized assessment to predict rehabilitation care after acute stroke. Arch Phys Med Rehabil. 2015;96(2):210–217. [DOI] [PubMed] [Google Scholar]
- 20.Sood MM, Rigatto C, Bueti J, et al. The role of functional status in discharge to assisted care facilities and in-hospital death among dialysis patients. Am J Kidney Dis. 2011;58(5):804–812. [DOI] [PubMed] [Google Scholar]
- 21.Socorro Garcia A, de la Puente M, Perdomo B, Lopez Pardo P, Baztan JJ. Functional status and mortality at month and year in nonagenarians hospitalized due to acute medical illness. Eur J Intern Med. 2015;26(9):705–708. [DOI] [PubMed] [Google Scholar]
- 22.Rozzini R, Sabatini T, Cassinadri A, et al. Relationship between functional loss before hospital admission and mortality in elderly persons with medical illness. J Gerontol A Biol Sci Med Sci. 2005;60(9):1180–1183. [DOI] [PubMed] [Google Scholar]
- 23.Roberts PS, Mix J, Rupp K, et al. Using functional status in the acute hospital to predict discharge destination for stroke patients. Am J Phys Med Rehabil. 2016;95(6):416–424. [DOI] [PubMed] [Google Scholar]
- 24.Ostir GV, Berges IM, Kuo YF, Goodwin JS, Fisher SR, Guralnik JM. Mobility activity and its value as a prognostic indicator of survival in hospitalized older adults. J Am Geriatr Soc. 2013;61(4):551–557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Narain P, Rubenstein LZ, Wieland GD, et al. Predictors of immediate and 6-month outcomes in hospitalized elderly patients. The importance of functional status. J Am Geriatr Soc. 1988;36(9):775–783. [DOI] [PubMed] [Google Scholar]
- 26.Mauthe RW, Haaf DC, Hayn P, Krall JM. Predicting discharge destination of stroke patients using a mathematical model based on six items from the Functional Independence Measure. Arch Phys Med Rehabil. 1996;77(1):10–13. [DOI] [PubMed] [Google Scholar]
- 27.Matzen LE, Jepsen DB, Ryg J, Masud T. Functional level at admissionis a predictor of survival in older patients admitted to an acute geriatric unit. BMC Geriatr. 2012;12:32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Kane RL, Chen Q, Finch M, Blewett L, Burns R, Moskowitz M. Functional outcomes of posthospital care for stroke and hip fracture patients under medicare. J AmGeriatrSoc.1998;46(12):1525–1533. [DOI] [PubMed] [Google Scholar]
- 29.Justice AC, Aiken LH, Smith HL, Turner BJ. The role of functional status in predicting inpatient mortality with AIDS: a comparison with current predictors. J Clin Epidemiol. 1996;49(2):193–201. [DOI] [PubMed] [Google Scholar]
- 30.Inouye SK, Peduzzi PN, Robison JT, Hughes JS, Horwitz RI, Concato J. Importance of functional measures in predicting mortality among older hospitalized patients. JAMA. 1998;279(15):1187–1193. [DOI] [PubMed] [Google Scholar]
- 31.Gabbe BJ, Simpson PM, Sutherland AM, et al. Functional measures at discharge: are they useful predictors of longer term outcomes for trauma registries? Ann Surg. 2008;247(5):854–859. [DOI] [PubMed] [Google Scholar]
- 32.Fortinsky RH, Covinsky KE, Palmer RM, Landefeld CS. Effects of functional status changes before and during hospitalization on nursing home admission of older adults. J Gerontol A Biol Sci Med Sci. 1999;54(10):M521–M526. [DOI] [PubMed] [Google Scholar]
- 33.Farrell RT, Gamelli RL, Sinacore J. Analysis of functional outcomes in patients discharged from an acute burn center. J Burn Care Res. 2006;27(2):189–194. [DOI] [PubMed] [Google Scholar]
- 34.Emhoff TA, McCarthy M, Cushman M, Garb JL, Valenziano C. Functional scoring of multi-trauma patients: who ends up where? J Trauma. 1991;31(9):1227–1232. [DOI] [PubMed] [Google Scholar]
- 35.Davis RB, Iezzoni LI, Phillips RS, Reiley P, Coffman GA, Safran C. Predicting in-hospital mortality. The importance of functional status information. Med Care. 1995;33(9):906–921. [DOI] [PubMed] [Google Scholar]
- 36.Covinsky KE, Palmer RM, Counsell SR, Pine ZM, Walter LC, Chren MM. Functional status before hospitalization in acutely ill older adults: validity and clinical importance of retrospective reports. J Am Geriatr Soc. 2000;48(2):164–169. [DOI] [PubMed] [Google Scholar]
- 37.Covinsky KE, Justice AC, Rosenthal GE, Palmer RM, Landefeld CS. Measuring prognosis and case mix in hospitalized elders. The importance of functional status. J Gen Intern Med. 1997;12(4):203–208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Corsonello A, Lattanzio F, Pedone C, et al. Prognostic significance of the short physical performance battery in older patients discharged from acute care hospitals. Rejuvenation Res. 2012;15(1):41–48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Choo B, Umraw N, Gomez M, Cartotto R, Fish JS. The utility of the functional independence measure (FIM) in discharge planning for burn patients. Burns. 2006;32(1):20–23. [DOI] [PubMed] [Google Scholar]
- 40.Bohannon RW, Lee N, Maljanian R. Postadmission function best predicts acute hospital outcomes after stroke. Am J Phys Med Rehabil. 2002;81(10):726–730. [DOI] [PubMed] [Google Scholar]
- 41.Bohannon RW, Lee N. Association of physical functioning with same-hospital readmission after stroke. Am J Phys Med Rehabil. 2004;83(6):434–438. [DOI] [PubMed] [Google Scholar]
- 42.Barnes DE, Mehta KM, Boscardin WJ, et al. Prediction of recovery, dependence or death in elders who become disabled during hospitalization. J Gen Intern Med. 2013;28(2):261–268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Higgins J, Green S. Cochrane Handbook for Systematic Reviews of Interventions, Version 5.1; 2011. http://training.cochrane.org/handbook. Accessed January 13, 2018.
- 44.Nyunt MSZ, Soh CY, Gao Q, et al. Characterisation of physical frailty and associated physical and functional impairments in mild cognitive impairment. Front Med (Lausanne). 2017;4:230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Pacala JT, Boult C, Boult L. Predictive validity of a questionnaire that identifies older persons at risk for hospital admission. J Am Geriatr Soc. 1995;43(4):374–377. [DOI] [PubMed] [Google Scholar]
- 46.Pfeiffer E A short portable mental status questionnaire for the assessment of organic brain deficit in elderly patients. J Am Geriatr Soc. 1975;23(10):433–441. [DOI] [PubMed] [Google Scholar]
- 47.Malhotra C, Chan A, Matchar D, Seow D, Chuo A, Do YK. Diagnostic performance of short portable mental status questionnaire for screening dementia among patients attending cognitive assessment clinics in Singapore. Ann Acad Med Singapore. 2013;42(7):315–319. [PubMed] [Google Scholar]
- 48.Gori D, Dulal R, Blayney DW, et al. Utilization of prostate cancer quality metrics for research and quality improvement: a structured review. Jt Comm J Qual Patient Saf. 2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Young Y, Xiong K, Pruzek RM. Longitudinal functional recovery after postacute rehabilitation in older hip fracture patients: the role of cognitive impairment and implications for long-term care. J Am Med Dir Assoc. 2011;12(6):431–438. [DOI] [PubMed] [Google Scholar]
- 50.Seematter-Bagnoud L, Lecureux E, Rochat S, Monod S, Lenoble-Hoskovec C, Bula CJ. Predictors of functional recovery in patients admitted to geriatric postacute rehabilitation. Arch Phys Med Rehabil. 2013;94(12):2373–2380. [DOI] [PubMed] [Google Scholar]
- 51.Sainsbury A, Seebass G, Bansal A, Young JB. Reliability of the Barthel Index when used with older people. Age Ageing. 2005;34(3):228–232. [DOI] [PubMed] [Google Scholar]
- 52.CFMM Services. 2018 CAHPS Survey for Accountable Care Organizations Participating in Medicare Initiatives; 2018. http://acocahps.cms.gov/globalassets/aco—epi-2-new-site/pdfs-for-aco/survey-instruments/2018-aco-survey/english/2018-cahps-for-acos-mail-survey—june-2018.pdf. Accessed October 10, 2018.
- 53.Centers for Medicare and Medicaid Services. Accountable Care Organization (ACO) 2018 Quality Measures: Narrative Specifications Document; 2018. https://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/sharedsavingsprogram/Downloads/2018-reporting-year-narrative-specifications.pdf. Accessed July 11, 2018.
- 54.Hall KM, Mann N, High WMJ, Wright J, Kreutzer JS, Wood D. Functional measures after traumatic brain injury: ceiling effects of FIM, FIM+FAM, DRS, and CIQ. J Head Trauma Rehabil. 1996;11(5):27–39. [Google Scholar]
- 55.Anderson K, Aito S, Atkins M, et al. Functional recovery measures for spinal cord injury: an evidence-based review for clinical practice and research. J Spinal Cord Med. 2008;31(2):133–144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Jette DU, Stilphen M, Ranganathan VK, Passek SD, Frost FS, Jette AM. Validity of the AM-PAC “6-Clicks” inpatient daily activity and basic mobility short forms. Phys Ther. 2014;94(3):379–391. [DOI] [PubMed] [Google Scholar]
- 57.Lu M, Sajobi T, Lucyk K, Lorenzetti D, Quan H. Systematic review of risk adjustment models of hospital length of stay (LOS). Med Care. 2015;53(4):355–365. [DOI] [PubMed] [Google Scholar]
- 58.Harrison JK, Walesby KE, Hamilton L, et al. Predicting discharge to institutional long-term care following acute hospitalisation: a systematic review and meta-analysis. Age Ageing. 2017;46(4):547–558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Soley-Bori M, Soria-Saucedo R, Ryan CM, et al. Functional status and hospital readmissions using the medical expenditure panel survey. J Gen Intern Med. 2015;30(7):965–972. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Jette DU, Stilphen M, Ranganathan VK, Passek SD, Frost FS, Jette AM.AM-PAC “6-Clicks” functional assessment scores predict acute care hospital discharge destination. Phys Ther. 2014;94(9):1252–1261. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


