Background:
Chronic pain is common in cirrhosis; however, the mechanistic classifications are not well characterized. Nociplastic pain, for instance, is associated with comorbid nonpain symptoms and responds to different treatments than nociceptive pain.
Methods:
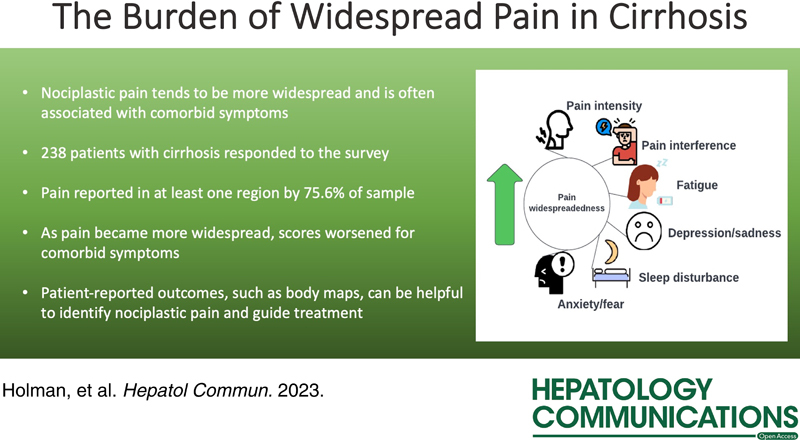
We conducted a survey study in February 2022 of adult patients with cirrhosis at the University of Michigan (N = 238) to evaluate pain widespreadedness, associated nociplastic symptoms, and pain intensity.
Findings:
Pain and pain widespreadedness were associated with mood and cognitive disturbance, fatigue, sleep difficulty, and physical and social functioning. Patient-reported Outcomes, such as body maps, can be useful to phenotype patients for pain mechanisms.
INTRODUCTION
Chronic pain is common in cirrhosis, reported by up to 79% of patients.1 Although not well characterized in cirrhosis, it is likely that multiple mechanistic classifications are represented: for example, nociceptive pain (pain from tissue damage), neuropathic pain (pain from nervous system damage), and nociplastic pain, which describes central augmentation of nociception which tends to be more widespread (eg, fibromyalgia and irritable bowel syndrome).2 In addition, nociplastic pain is often associated with comorbid nonpain symptoms, such as fatigue, memory or concentration problems, mood disturbances, and sleep difficulties, that can negatively impact patient well-being.2,3 The recognition of pain classifications can be important, given that responsivity to treatment differs between classifications. Nociceptive pain tends to respond to NSAIDs, acetaminophen, opioids, injections, and surgery, whereas nociplastic pain preferentially responds to centrally acting analgesics (eg, tricyclics, serotonin and norepinephrine reuptake inhibitors, and gabapentinoids) with aggressive use of nonpharmacologic therapies.2 Thus, our primary focus in this study was to characterize the impact of nociplastic pain in individuals with cirrhosis.
METHODS
Sample
Surveys were sent to 2000 adult (aged 18 y or above) patients through email in February 2022. Participants had an established diagnosis of cirrhosis and were followed by a hepatologist at the University of Michigan. We excluded patients with liver transplants. Participants were paid 10 dollars for completing the survey. The study was approved by the University of Michigan Institutional Review Board, and all respondents provided informed consent.
Measures
The widespreadedness of pain (a key feature of nociplastic pain), as well as associated nociplastic symptoms, was assessed using the American College of Rheumatology 2011 Fibromyalgia Survey Criteria.4 This survey includes the number of painful body regions (0–19; the Widespread Pain Index) and related symptoms such as problems with thinking, fatigue, and sleep difficulties (0–12; the Symptom Severity Index).4 This survey has been used to quantify centralized pain in other clinical populations,5 relates strongly to functional neuroimaging findings in nociplastic pain,6 and predicts pain and disability.7,8 Nonpain symptoms were assessed using the Patient-reported Outcome Measurement Information System 29-Item Profile, version 2 (PROMIS-29+2), which evaluates the following domains: Pain Interference, Physical Function, Fatigue, Anxiety, Depression, Sleep Disturbance, and Satisfaction with Participation in Social Roles, as well as cognitive function,9,10 and are scored using a T-score, where a score of 50 approximates the general population means with an SD of 10 points. Pain intensity was assessed with the PROMIS Pain Intensity 3a, a 3-item measure that assesses the worst and average pain in the past 7 days and the current pain.11 ANOVA was used to test the significance of the differences in each domain.
RESULTS
Sample characteristics
Overall, 238 patients responded to the survey (response rate 11.9%). Our study sample (N=238) was comprised of 40.8% of men with an average age of 58.8 years (Supplemental Table 1, http://links.lww.com/HC9/A245). Most (60%) had a college degree or more and were primarily White (89.5%). The commonest etiology of cirrhosis was NAFLD. Most were compensated, with 12.6% and 16% reporting ascites and HE, respectively. Overall, 21% were taking opioids. The most common pain region reported was the axial region (65.5%).
Associated symptoms
As the number of positive pain regions increased from 0 to 4 or more, PROMIS29+2 scores increased for pain interference, depression/sadness, anxiety/fear, fatigue, and sleep disturbance, where higher scores reflect worse symptoms (Table 1). Likewise, as the number of pain regions increased from 0 to 4 or more, PROMIS29+2 scores decreased for cognitive function, physical function, and ability to participate in social roles/activities, where lower scores reflect worse functioning.
TABLE 1.
Relationship between widespread pain index and associated symptom scores
| No. pain regions present | ||||||
|---|---|---|---|---|---|---|
| PROMIS 29+2 category | 0 regions (24.3%, n=58) | 1 region (16.3%, n=39) | 2–3 regions (33.2%, n=79) | 4 or more regions (26.0%, n=62) | p | |
| Higher scores are worse | Symptoms | Mean + SD | ||||
| Pain Interference | 46.15±5.40 | 52.56±3.84 | 56.79±3.07 | 60.99±2.78 | <0.001 | |
| Depression/Sadness | 47.17±4.94 | 50.50±4.34 | 54.09±3.69 | 56.46±3.49 | <0.001 | |
| Anxiety/Fear | 49.08±4.74 | 52.25±4.15 | 54.86±3.79 | 58.23±3.37 | <0.001 | |
| Fatigue | 49.74±3.02 | 54.27±2.67 | 59.40±2.74 | 62.31±2.83 | <0.001 | |
| Sleep Disturbance | 49.31±3.61 | 52.00±3.56 | 54.64±3.37 | 56.70±3.44 | <0.001 | |
| Lower scores are worse | Functions | Mean + SD | ||||
| Cognitive Function | 54.49±6.32 | 51.69±5.85 | 50.09±5.76 | 47.58±5.82 | <0.001 | |
| Physical Function | 50.74±5.46 | 45.44±3.86 | 41.55±3.31 | 38.49±3.15 | <0.001 | |
| Ability to Participate in Social Roles/Activities | 55.86±4.01 | 51.12±2.98 | 46.32±2.78 | 44.98±2.80 | <0.001 | |
| Higher worse | PAIN Intensity PROMIS3a | 41.58±4.86 | 49.70±4.04 | 54.55±3.76 | 59.53±3.77 | <0.001 |
Abbreviation: PROMIS, Patient-reported Outcome Measurement Information System.
Pain intensity
As the number of pain regions present increased from 0 to 4 or more, Pain Intensity PROMIS3a scores increased, where higher scores reflect worse pain intensity (Table 1).
Pain region
There was no consistent association between pain region and associated symptoms or pain intensity (Supplemental Table 2, http://links.lww.com/HC9/A246).
DISCUSSION
Here, we find that pain and pain widespreadedness are associated with mood and cognitive disturbance, fatigue, sleep difficulty, and physical and social functioning. Pain in a specific region did not seem to affect any domain particularly. Overall, these results suggest that nociplastic pain may be a clinically significant contributor to the burden of chronic pain in patients with cirrhosis. Patient-reported Outcomes (PROs) like body maps can be useful to phenotype these patients for pain mechanism and help predict treatment responses.
Identifying patients with features of nociplastic pain is important because first-line treatment is nonpharmacologic, incorporating patient education, self-management strategies, lifestyle interventions (eg, exercise/diet optimization, healthy sleep habits, stress relief, and maintenance of occupational/social involvement), and psychological treatments (eg, cognitive behavioral therapy), which can be useful in patients with cirrhosis, for whom pharmacologic therapy is complex.2,12
In addition, PROs can identify patients with characteristics of nociplastic pain and help to predict the presence of nonpain symptoms that can guide therapy. For instance, in addition to nonpharmacologic therapy, low-dose tricyclic compounds can address multiple symptoms and are first-line for nociplastic pain.3 Serotonin-norepinephrine reuptake inhibitors can be used for accompanying depression or fatigue, and gabapentinoids can be used for anxiety or sleep disturbance.3
Similarly, PROs can predict treatment response. Conventional analgesics (eg, NSAIDs and acetaminophen) are not generally useful for nociplastic pain, and opioid use is strongly discouraged.2,3 In fact, higher fibromyalgia survey scores have been correlated with increased postoperative opioid consumption, suggesting decreased responsiveness to these medications.13 There is evidence that this type of pain might be worsened by opioids through opioid-induced hyperalgesia.14
Our study has various limitations, significantly the small sample size and primarily White, educated sample, which restricts the generalizability of our results.
Overall, nociplastic pain seems to be an important pain phenotype in patients with cirrhosis, for which treatment centers on nonpharmacologic therapies, as well as the improvement of nonpain symptoms and functioning.2,3 PROs, such as Fibromyalgia surveys and body maps, can be essential for identifying nociplastic pain and guiding treatment. One promising area of future research is to develop additional validated surveys tailored for use in patients with cirrhosis.
Supplementary Material
FUNDING INFORMATION
Effort on this publication was partially supported by the National Institute of Arthritis and Musculoskeletal and Skin Diseases of the National Institutes of Health (T32-AR07080 to Alexis Holman) and NIDDK to Elliot B. Tapper and Neehar D. Parikh (U01-DK130113).
CONFLICTS OF INTEREST
Daniel J. Clauw consults for Pfizer, Lilly, Virios, Scirex, and Tonic. The remaining authors have no conflicts to report.
Footnotes
Abbreviations: PROs, Patient-reported Outcomes; PROMIS, Patient-reported Outcome Measurement Information System.
Supplemental Digital Content is available for this article. Direct URL citations are provided in the HTML and PDF versions of this article on the journal’s website, www.hepcommjournal.com.
Contributor Information
Alexis Holman, Email: aaholman@med.umich.edu.
Neehar D. Parikh, Email: ndparikh@med.umich.edu.
Zhe Zhao, Email: zzhaozhe@umich.edu.
Samantha Nikirk, Email: samjwalk@med.umich.edu.
Daniel J. Clauw, Email: dclauw@med.umich.edu.
David A. Williams, Email: daveawms@med.umich.edu.
Elliot B. Tapper, Email: etapper@umich.edu.
REFERENCES
- 1.Rogal SS, Bielefeldt K, Wasan AD, Lotrich FE, Zickmund S, Szigethy E, et al. Inflammation, psychiatric symptoms, and opioid use are associated with pain and disability in patients with cirrhosis. Clin Gastroenterol Hepatol. 2015;13:1009–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Fitzcharles MA, Cohen SP, Clauw DJ, Littlejohn G, Usui C, Hauser W. Nociplastic pain: towards an understanding of prevalent pain conditions. Lancet. 2021;397:2098–110. [DOI] [PubMed] [Google Scholar]
- 3.Clauw DJ. Fibromyalgia: a clinical review. JAMA. 2014;311:1547–55. [DOI] [PubMed] [Google Scholar]
- 4.Wolfe F, Clauw DJ, Fitzcharles MA, Goldenberg DL, Hauser W, Katz RS, et al. Fibromyalgia criteria and severity scales for clinical and epidemiological studies: a modification of the ACR Preliminary Diagnostic Criteria for Fibromyalgia. J Rheumatol. 2011;38:1113–22. [DOI] [PubMed] [Google Scholar]
- 5.Janda AM, As-Sanie S, Rajala B, Tsodikov A, Moser SE, Clauw DJ, et al. Fibromyalgia survey criteria are associated with increased postoperative opioid consumption in women undergoing hysterectomy. Anesthesiology. 2015;122:1103–1111. [DOI] [PubMed] [Google Scholar]
- 6.Kutch JJ, Ichesco E, Hampson JP, Labus JS, Farmer MA, Martucci KT, et al. Brain signature and functional impact of centralized pain: a multidisciplinary approach to the study of chronic pelvic pain (MAPP) network study. Pain. 2017;158:1979. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wolfe F. Pain extent and diagnosis: development and validation of the regional pain scale in 12,799 patients with rheumatic disease. J Rheumatol. 2003;30:369–78. [PubMed] [Google Scholar]
- 8.Wolfe F, Häuser W, Hassett AL, Katz RS, Walitt BT. The development of fibromyalgia–I: examination of rates and predictors in patients with rheumatoid arthritis (RA). Pain. 2011;152:291–9. [DOI] [PubMed] [Google Scholar]
- 9.Rose AJ, Bayliss E, Huang W, Baseman L, Butcher E, García R-E, et al. Evaluating the PROMIS-29 v2. 0 for use among older adults with multiple chronic conditions. Qual Life Res. 2018;27:2935–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Verma M, Stites S, Navarro V. Bringing assessment of patient-reported outcomes to hepatology practice. Clin Gastroenterol Hepatol. 2018;16:447–8. [DOI] [PubMed] [Google Scholar]
- 11.Cella D, Riley W, Stone A, Rothrock N, Reeve B, Yount S, et al. The Patient-Reported Outcomes Measurement Information System (PROMIS) developed and tested its first wave of adult self-reported health outcome item banks: 2005–2008. J Clin Epidemiol. 2010;63:1179–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Holman A, Parikh N, Clauw DJ, Williams DA, Tapper EB. Rethinking the management of pain in cirrhosis: toward precision therapy for pain. Hepatology. 2022;77:290–304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Brummett CM, Janda AM, Schueller CM, Tsodikov A, Morris M, Williams DA, et al. Survey criteria for fibromyalgia independently predict increased postoperative opioid consumption after lower-extremity joint arthroplasty: a prospective, observational cohort study. Anesthesiology. 2013;119:1434–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Schrepf A, Harper DE, Harte SE, Wang H, Ichesco E, Hampson JP, et al. Endogenous opioidergic dysregulation of pain in fibromyalgia: a PET and fMRI study. Pain. 2016;157:2217–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


