Background.
Automation of deceased donor referrals with standardized clinical triggers allows organ procurement organizations to be rapidly aware of medically eligible potential donors without the need for manual reporting and subjective decision-making of otherwise very busy hospital staff. In October 2018, 3 Texas hospitals (pilot hospitals) began using an automated referral system; our goal was to evaluate the impact of this system on eligible donor referral.
Methods.
We studied ventilated referrals (n = 28 034) in a single organ procurement organization from January 2015 to March 2021. We estimated the change in referral rate in the 3 pilot hospitals due to the automated referral system using a difference-in-differences analysis with Poisson regression.
Results.
Ventilated referrals from the pilot hospitals increased from mean 11.7 per month pre-October 2018 to 26.7 per month post-October 2018. The difference-in-differences analysis estimated that automated referral was associated with a 45% increase in referrals (adjusted incidence rate ratio [aIRR] = 1.30 1.45 1.62), an 83% increase in approaches for authorization (aIRR = 1.34 1.83 2.48), a 73% increase in authorizations (aIRR = 1.18 1.73 2.55), and a 92% increase in organ donors (aIRR = 1.13 1.92 3.09).
Conclusions.
Following deployment of an automated referral system that did not require any actions by the referring hospital, referrals, authorizations, and organ donors increased substantially in the 3 pilot hospitals. Broader deployment of automated referral systems may lead to increases in the deceased donor pool.
Federal regulations mandate notification of imminent death to an organ procurement organization (OPO) in a timely manner1 to ensure that the maximum possible number of transplantable organs is available to those waiting for a transplant.2,3 Ideally, rapid referral allows the OPO sufficient time to determine eligibility for organ donation, communicate with family members about donation, and orchestrate organ recovery. Standard practice has relied on hospital staff to identify that a patient meets donor referral triggers and to communicate this information to the OPO.
However, there is heterogeneity in this process, because hospitals have individual agreements with OPOs that include a wide range of definitions of imminent and timely manner,1 and manual referrals rely on clinical decision-making from busy hospital staff with a wide range of training in donor identification and transplant science.4 As such, it is not surprising that OPOs are not consistently notified of all potential donors before key events, such as diagnosis of brain death or the withdrawal of all life-sustaining therapies. Delayed notification or failure to notify the OPO has been associated with attitudes, knowledge, and behaviors of healthcare personnel regarding donation,5 as well as their competing clinical duties.6 There are also reports of poorly trained hospital staff inappropriately screening families for receptivity to donation before making the referral call.6–8 In the United States, the OPO initiates a conversation about donation with legal next of kin regardless of registry status.
Automated donor referrals could reduce variation in timeliness as well as the subjective element and human interaction for the identification of potential organ donors.9 Automation obviates the reliance on manual initiation of contact with the OPO, by directly and electronically delivering donor referrals when triggered by predetermined clinical event data from the electronic medical record.
In October 2018, an automated referral system was piloted in 3 Texas hospitals within the donor service area of a single OPO. To better understand the impact of this automated referral system on referral patterns and timing, we studied all deceased donor referrals from these hospitals between January 2016 and March 2021. We compared temporal trends in the 3 pilot hospitals to trends at the rest of the OPOs during the study period to estimate changes in the total number of referrals, approaches for authorization, authorizations, and organ donors from the pilot hospitals associated with implementation of the pilot program.
MATERIALS AND METHODS
Automated Referrals
Automated electronic donor referrals generate from a hospital’s electronic health record (EHR), as defined by clinical triggers. In the United States, there are 3 currently implemented methods by which clinical triggers being met generate the automated delivery of a donor referral to the OPO. The first is defined by parameters indicative of organ donation potential, such as a combination of the patient (1) is on mechanical ventilation, (2) is admitted to the intensive care unit (ICU) because a neurocritical injury, and (3) has a Glasgow Coma Score of ≤5.1 The second method is a cardiac time of death being documented in the patient’s electronic medical record (this is to identify exclusively tissue donation opportunities). The third method is a send now button, which allows a provider nurse to electronically, although still somewhat manually, notify the OPO of a potential donor as they are arriving in the ICU. These clinical triggers are universally accepted as best practice and are consistent across many OPOs and hospital systems. Although this approach allows for referrals to be created automatically, the clinician retains the ability to proactively trigger a referral.
Once the transmission of data from the hospital’s EHR to the OPO is complete, OPO staff are alerted of the new referral, and the OPO’s work to evaluate potential donors for suitability can begin. Those patients who do not die or have certain medical conditions or histories may not be eligible and are ruled out for donation. Of those potential donors who are suitable candidates for donation, the OPO approaches the family.
In the pilot hospitals, before the implementation of the automated referral system, the hospital would call the OPO to make the referral. At times, patients were determined to be not suitable for donation based on the information included in the initial referral alone. At times, the OPO would go on-site right away. At other times, the OPO would call the hospital nursing staff back for more information on the potential donor, enough to determine whether someone from the OPO should go on-site. Once on-site, the OPO staff would conduct a more thorough evaluation for preliminary suitability for donation.
Initially after implementation, the automated referral came in to the OPO, and the OPO would then call the nurse for enough clinical information to determine whether an on-site consult was needed. This quickly evolved so that when the automated referral was received by the OPO, staff would access the patient chart by logging into the hospital EHR remotely to determine whether an on-site consult was warranted. Then the nurse would receive a call advising whether someone from the OPO was on the way or whether the patient was not a candidate for donation.
The pilot hospitals had EHR developers on-site, which is uncommon. These developers wrote the automated referral as a customization that allowed the hospital EHR system to send the automated referral information to the OPO’s electronic donor record system using an Application Programming Interface. It was written using a coding software (mCODE), and the automation was accomplished using a function of the EHR where a new pop-up window appears for the user when certain conditions are met to advise of the best clinical practice.
Pilot Test of Automated Referral System
On October 9, 2018, the automated referral system described above was deployed in 3 of 137 hospitals served by the Southwest Transplant Alliance OPO (pilot hospitals). Starting on this date, referrals from the 3 pilot hospitals could occur either via the automated system (automated referrals) or from staff at the 3 pilot hospitals using the same process that existed before the existence of the automated system (manual referrals).
Study Population
We analyzed data on 28 034 ventilated referrals to a single OPO between January 1, 2015, and March 31, 2021. Data recorded included date and time of key events (hospital admission, referral, approach of the family for authorization, authorization, and cross-clamp) and demographics (age, sex, and race/ethnicity), whether the patient had registered as an organ donor, whether the patient was on a ventilator at time of referral, whether the referral was made through iReferral or called in to the OPO, and whether the patient became an organ donor. This study was exempt from institutional review board approval.
Statistical Analysis
All referrals during the study period were categorized as pre-October 2018 (before October 1, 2018), post-October 2018 automated (automatically generated referrals), or post-October 2018 manual (referred manually on or after October 1, 2018). October 1 was used as a boundary instead of October 9 because referral counts were analyzed by month; thus, all referrals (October 1–8, 2018; n = 121, of which 5 occurred at the pilot hospitals) were classified as post-October 2018 manual. For each step on the pathway to donation (referral, approach of the family for authorization, authorization for donation obtained, and actual recovery of at least 1 organ), we used Poisson regression to calculate the change in count per month associated with implementation of automated referrals. The Poisson regression was a difference-in-differences analysis comparing change at the 3 pilot hospitals to change in the other hospitals, adjusting for secular trend (linear proportional increase per month), era (pre-October 2018 versus post-October 2018), pilot versus nonpilot hospitals, and the pilot hospital/era interaction. Incidence rate ratios from the pilot hospital/era interaction represent the difference between rate change in the pilot hospitals versus rate change in the other hospitals following implementation of the pilot program. All analyses were performed using Stata 17 (StataCorp, College Station, TX). Confidence intervals are reported as per the method of Louis and Zeger.
Sensitivity Analysis
Because the COVID-19 epidemic may have had unexpected effects on donor referral, we performed a sensitivity analysis restricting the post-October 2018 period to October 1, 2018, to February 28, 2020, ending before widespread COVID-19 incidence in the United States.
RESULTS
Study Population
Of 28 034 referrals to the OPO during the study period, 1328 were made to the pilot hospitals, of which 802 (60.4%) were made during the post-October 2018 period. The age of referrals increased slightly from pre-October 2018 to post-October 2018, both in nonpilot hospitals (from median [interquartile range], 58 [44–68] to 62 [49–73] y) and pilot hospitals (from median [interquartile range], 63 [51–72] to 65 [53–76] y; Table 1). The proportion of referrals that were female was 41.7% in nonpilot hospitals both pre- and post-2018; the proportion of referrals that were female in pilot hospitals was 41.5% pre-October 2018 and 40.8% post-October 2018. Referrals from the pilot hospitals were substantially more likely to be White (73.6% pre-October 2018 and 70.9% post-October 2018) than referrals from nonpilot hospitals (48.5% pre-October 2018 and 50.1% post-October 2018). The proportion of referrals that were registered organ donors increased from 18.9% to 24.1% in the nonpilot hospitals and from 19.0% to 20.9% in the pilot hospitals.
Table 1.
Demographics of referrals for deceased donation
| Pre-October 2018 | Post-October 2018 | Pre-October 2018 | Post-October 2018 | |
|---|---|---|---|---|
| Nonpilot | Nonpilot | Pilot | Pilot | |
| n = 13 015 | n = 13 691 | n = 526 | n = 802 | |
| Median age, y (IQR) | 58 (44–68) | 62 (49–73) | 63 (51–72) | 65 (53–76) |
| Female, % | 41.7 | 41.7 | 41.5 | 40.8 |
| Non-Hispanic White, % | 48.5 | 50.1 | 73.6 | 70.9 |
| Hispanic, % | 26.6 | 27.3 | 8.2 | 5.6 |
| Black, % | 21.6 | 19.6 | 17.3 | 21.9 |
| Other/missing, % | 3.3 | 3.0 | 1.0 | 1.5 |
| Registered organ donors, % | 18.9 | 24.1 | 19.0 | 20.9 |
Pilot hospitals are those that were selected for the pilot deployment of the automated referral system, which began in October 2018.
IQR, interquartile range.
Of the 802 post-October 2018 referrals in the pilot hospitals, 586 (73.1%) were automated referrals, whereas the rest were manual referrals. Post-October 2018 automated referrals and manual referrals were comparable at the pilot hospital with regard to age, sex, race, and organ donor status (Table S1, SDC, http://links.lww.com/TXD/A431).
Referrals pre- and post-October 2018
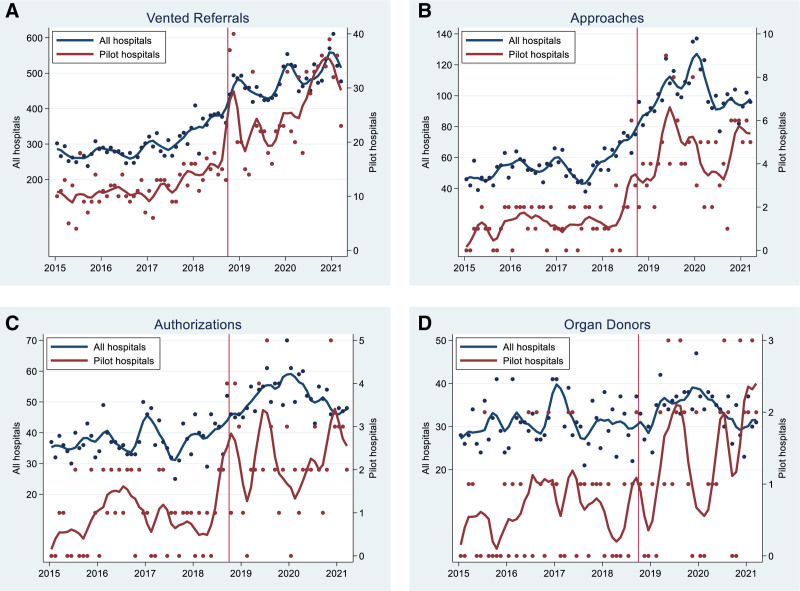
During the pre-October 2018 period, there were 13 541 total referrals (mean, 300.9 per month), of which 526 (mean, 11.7 per month) came from pilot hospitals (Figure 1A). During the post-October 2018 period, there were 14 493 total referrals (483.1 per month), of which 802 (26.7 per month) came from pilot hospitals. Of the 26.7 per month from the pilot hospitals during the post-October 2018 period, 7.1 per month were manual referrals, and 19.7 per month were automated referrals (Table 2). The difference-in-differences analysis yielded an estimated 45% increase in monthly referrals at the pilot hospitals associated with implementation of the automated referral system (adjusted incidence rate ratio [aIRR] = 1.30 1.45 1.62; < 0.001; Table 3).
FIGURE 1.
Month-to-month event counts in all hospitals in the organ procurement organization (navy) and pilot hospitals (maroon). Dots represent individual months; thick lines are a linear smooth. The vertical line at October 2018 represents implementation of the automated referral system. A, An estimated 45% increase in monthly referrals at the pilot hospitals associated with implementation of the automated referral system. B, An 83% increase in monthly approaches at the pilot hospitals associated with implementation of the automated referral system. C, An estimated 73% increase in monthly authorizations at the pilot hospitals associated with implementation of the automated referral system. D, An estimated 92% increase in monthly donors from the pilot hospitals associated with implementation of the automated referral system. 1 It should be noted that these criteria are based on the US framework of potential donor referrals. In the United States, donor referrals occur independently of a patient’s treatment futility. To this end, OPOs in the United States are exempt from the data sharing requirements typically imposed on hospitals that govern the sharing of PHI with other healthcare providers. As such, the conditions for sharing patient data in the United States may not be applicable in other countries. OPO, organ procurement organization; PHI, Protected Health Information.
Table 2.
Disposition of referrals at pilot hospitals pre-October 2018, manual referrals post-October 2018, and automated referrals post-October 2018
| Event | n (rate) pre-October 2018 | n (rate) post-October 2018 | n (rate) post, manual | n (rate) post, automated |
|---|---|---|---|---|
| Referrals | 526 (11.7) | 802 (26.7) | 212 (7.1) | 590 (19.7) |
| Approaches | 61 (1.4) | 136 (4.5) | 57 (1.9) | 79 (2.6) |
| Authorizations | 44 (1.0) | 68 (2.3) | 29 (1.0) | 39 (1.3) |
| Organ donors | 30 (0.7) | 41 (1.4) | 21 (0.7) | 20 (0.7) |
Rate is the average number per month. There were 45 mo in the pre-2018 period and 30 mo in the post-2018 period.
Table 3.
Difference-in-differences analysis of the change in events per month associated with implementation of the automated referral system
| Event | aIRR | P |
|---|---|---|
| Referrals | 1.30 1.45 1.62 | <0.001 |
| Approaches | 1.34 1.83 2.48 | <0.001 |
| Authorizations | 1.18 1.73 2.55 | <0.01 |
| Organ donors | 1.19 1.92 3.09 | <0.01 |
IRRs were calculated by Poisson regression adjusting for secular trend (linear increase per month) and represent the difference between the change at pilot hospitals vs the change at other hospitals.
aIRR, adjusted incidence rate ratio; IRR, incidence rate ratio.
Approaches pre- and post-October 2018
During the pre-October 2018 period, there were 2456 total approaches (mean, 54.6 per month; 18.1% of referrals), of which 61 (mean, 1.4 per month) came from pilot hospitals (Figure 1B). During the post-October 2018 period, there were 3058 total approaches (33.8 per month; 21.1% of referrals), of which 136 (4.5 per month) came from pilot hospitals. Of the 4.5 per month from the pilot hospitals during the post-October 2018 period, 1.9 per month were from manual referrals, and 2.6 per month were from automated referrals (Table 2). The difference-in-differences analysis yielded an estimated 83% increase in monthly approaches at the pilot hospitals associated with implementation of the automated referral system (aIRR = 1.34 1.83 2.48; P < 0.001; Table 3).
Authorizations pre- and post-October 2018
During the pre-October 2018 period, there were 1705 total authorizations (mean, 37.9 per month; 69.4% of approaches), of which 44 (mean, 1.0 per month) came from pilot hospitals (Figure 1C). During the post-October 2018 period, there were 1550 total authorizations (51.7 per month; 50.7% of approaches), of which 68 (2.3 per month) came from pilot hospitals. Of the 2.3 per month from the pilot hospitals during the post-October 2018 period, 1.0 per month were from manual referrals, and 1.3 per month were from automated referrals (Table 2). The difference-in-differences analysis yielded an estimated 73% increase in monthly authorizations at the pilot hospitals associated with implementation of the automated referral system (aIRR = 1.18 1.73 2.55; P < 0.01; Table 3).
Organ Donors pre- and post-October 2018
During the pre-October 2018 period, there were 1396 total organ donors (mean, 31.0 per month; 89.9% of authorizations), of which 30 (mean, 0.7 per month) came from pilot hospitals (Figure 1D). During the post-October 2018 period, there were 1015 total donors (33.8 per month; 65.5% of authorizations), of which 41 (1.4 per month) came from pilot hospitals. Of the 1.4 per month from the pilot hospitals during the post-October 2018 period, 0.7 per month were from manual referrals, whereas 0.7 per month were from automated referrals (Table 2). The difference-in-differences analysis yielded an estimated 92% increase in monthly organ donors from the pilot hospitals associated with implementation of the automated referral system (aIRR = 1.19 1.92 3.09; P < 0.01; Table 3).
Sensitivity Analysis
In sensitivity analysis restricting the post-October 2018 period to time before widespread COVID incidence in the United States, the proportional increase in the number of referrals per month, approaches, authorizations, and organ donors was comparable to findings from our main analysis (Table S2, SDC, http://links.lww.com/TXD/A431). However, confidence intervals were wider, particularly for the change in rates of authorizations and organ donors, and the increase in number of organ donors was no longer statistically significant (aIRR = 0.84 1.50 2.69; P = 0.17).
DISCUSSION
In this study of 28 034 referrals to a single OPO over a 4-y period, implementation of a pilot automated referral program in 3 hospitals was associated with a 45% increase in referrals, an 83% increase in approaches for authorization, a 73% increase in authorizations, and a 92% increase in deceased donation compared to trends at other hospitals in the OPO during the same time. Taken as a whole, our data suggest that a broader implementation of automated donor referrals has the potential to increase deceased organ donation in the United States, ultimately reducing the severe shortage of lifesaving donor organs.
Initially, many frontline clinicians at the 3 pilot hospitals resisted the shift to automated referrals because it meant they had less control over making approaches. Over time, more clinicians have come to understand that the automation is intended to overcome some of the limitations of manual referrals and increase the number of patients approached for authorization; however, there are still some who believe that it interferes in their decision-making process regarding end-of-life care and treatment futility.
The automated referrals from the hospital to the OPO described in this study overcome limitations of current manual referrals, whether telephone or electronic, to increase donor referrals and increase the number of patients approached for authorization. Automated referrals address issues associated with the timeliness of the donor referral process and the subjective element of identifying potential organ donors. Donation attitudes, knowledge, and behaviors of healthcare personnel have been identified as a significant barrier to timely referral and impact the referral process.6,10,11 End-of-life care can be a particularly stressful period associated with strong emotional reactions for healthcare personnel, patients, and families. Research has highlighted that some healthcare providers screen families for receptivity to donation, which leads to particular families not being presented with donation as an option.6 Nonreferral, untimely referral, and suboptimal request for donation or de-escalation of care may be impacted by clinician bias. Automatically initiating the referral process when predetermined clinical parameters are documented in the hospital EHR removes bias and clinician error in the identification of clinical triggers. This makes an automated referral system distinct from an electronic referral system, which automates some data entry but is still entirely dependent on the clinician to start the process. A fully automated referral saves clinicians time; allows OPO staff direct access to data, beginning the donation process; supports patient safety; and provides better data quality. That said, the automated referrals being currently generated result in minimal data being transmitted to the OPO, and much of the donor chart is still transcribed either through human-to-human communication or a search of the hospital EHR. Further efficiencies, including reduced costs, could be achieved by a greater number of data points being transmitted automatically to the OPO for evaluation of donor suitability and for the efficient deployment of OPO resources for which the opportunity for donation is greatest.
Electronic clinical decision support tools that leverage the hospital EHR improve notifications requiring clinical intervention and reduce unnecessary diagnostics.12–18 A retrospective study on OPO notification timeliness and number of donations found an increase in donors and donor conversions (which is defined as the percentage of eligible donors for whom procurement is actually performed) and a decrease in mean time to OPO notification using electronic referral systems.19 In that study, the electronic referral system in place was a clinical decision support system that was designed to identify individuals who meet OPO notification criteria for impending brain death. Programs designed to increase timely notification and donor conversions but require the ongoing manual participation of healthcare personnel have been found not to be sustainable long term.11
We previously determined that automated referrals would reduce the need for donation knowledge and decision-making by hospital staff while also providing the opportunity for manual referral for exceptional cases, such as early family mention of donation.5,9 Automation of referrals may also improve patient safety, by reducing the likelihood of timeliness issues and ensuring that no opportunities to recover organs from eligible donors are overlooked, and standardization, by removing much of the subjectivity in identifying potential organ donors.
Seventy-four percent of referrals in the post-October 2018 era were made through the automated referral system. As with any study comparing 2 different eras, however, we cannot fully account for other changes to the potential donor pool, healthcare practices, or other trends that might affect our inference, such as COVID-19. However, the difference-in-differences framework compared changes in the 3 pilot hospitals to changes at other hospitals within the OPO; observed increases in referrals, authorizations, and donations were in excess of trends at other hospitals within the OPO during the same time.
For the impact of COVID-19, we conducted a sensitivity analysis using only data from before March 1, 2021. Data were not originally collected for research and, in principle, may be subject to measurement error. However, operation of the OPO requires accurate counts of referrals, authorizations, and donations.
Our findings should be interpreted with several limitations in mind. First, the automated referral system was implemented in only 3 hospitals, all located within the same geographic region. As such, our findings may not be generalizable to all hospitals in differing regions of the United States or internationally. In the international context, different methods of timely referral, based on triggers, have been tested on hospital and ICU admission or during ICU management. Most European countries have already adopted an in-hospital organ procurement team model; however, an automated, 24/7 referral on hospital admission could be used to optimize possible donor detection. Second, the implementation in this study required considerable custom code development by programming staff at the hospital. To replicate the approach used here, a hospital would likely need an EHR developer, or equivalent, which is something most hospitals do not have. Future iterations will be aimed at implementing the automation at a larger number of hospitals across the United States, thereby increasing and diversifying the sample size. Third, some OPO staff members have expressed concern that an automated referral system based only on ventilation, neurocritical injury, and a Glasgow Coma Scale <5 could overburden or overwork the OPO. Those staff members have resisted adopting the automated referral system because of claims that they already receive too many referrals; however, it is incumbent on the OPO to manage its workload to ensure that opportunities are not lost. Fourth, possible differences in clinical data (aside from age) between automated (590) and manual referrals (212) in the pilot hospitals after October 2018 were not explored. Subsequent studies should consider possible differences in etiology, imaging, brainstem reflexes, timing of referral, timing of death, donation after brain death, donation after circulatory death, etc. Lastly, no secondary alerts are made after the key event has occurred. As a result, OPO personnel are responsible for following up independently to ensure they do not overlook any potential opportunities. This requires OPO personnel to check the patients’ charts at least once a day.
A second implementation with a larger healthcare system has since been accomplished using a much different approach that also captures missed donor referrals. The scalability of the solution is ultimately a function of the combination of resources available to each hospital/OPO combination. OPOs can choose to support the implementation of automated referrals using multiple different approaches. Nearly all OPOs are working with an EHR that is capable of receiving the information and are providing some support to the hospital for their side of the development. If this technology is applied to the broader concept of automating referrals, then it is 100% scalable using the same technologies that support the Health Information Exchanges with which hospitals are already required to interface.
With increasing referrals, the OPO was in fact much busier, responded to more referrals, approached more families, managed more donors, and ultimately recovered more organs for transplant. The process generated the biggest impact in terms of patients referred to the OPO, with decreasing impact at each stage thereafter due to the natural falloff from referral to following for donation to approach for authorization to donation. Every year, thousands of individuals die on the deceased donor waitlist in the United States while waiting for a deceased donor organ. The problem of supply of deceased donor organs has proven to be stubbornly durable, and no single intervention is likely to solve it. For the foreseeable future, healthcare providers, OPOs, and policymakers will have to continue to seek creative new solutions to the problem. However, our results suggest that even a basic automated referral system may have the potential to increase organ recovery and improve access to deceased donor transplantation.
ACKNOWLEDGMENTS
This work was funded by the Southwest Transplant Alliance under a research collaboration with the Epidemiology Research Group in Organ Transplantation at the Johns Hopkins University (Principal Investigator: M.L.L.). The Johns Hopkins investigators are also supported by training grant numbers F32DK124941 (Boyarsky), K01DK101677 (A.B.M.), and K01 DK114388 (Levan [Henderson]) from the National Institute of Diabetes and Digestive and Kidney Diseases and K24AI144954 (D.L.S.) from the National Institute of Allergy and Infectious Diseases.
Supplementary Material
Footnotes
Co-first and co-senior authors.
Substantial contributions to the conception or design of the work or the acquisition, analysis, or interpretation of data for the work: M.L.L., C.T., J.H., T.S., M.A.L., A.B.M., P.N., and D.L.S.; drafting the work or revising it critically for important intellectual content: M.L.L., C.T., M.A.L., B.L.A., K.B.V., S.B.K., P.N., and D.L.S.; final approval of the version to be published: M.L.L., C.T., J.H., T.S., M.A.L., K.B.V., S.B.K., D.L.S., A.B.M., and P.N.; agreement to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved: M.L.L., C.T., J.H., T.S., M.A.L., K.B.V., D.L.S., A.B.M., and P.N.
Funding or a product for the study described in this publication was provided by Southwest Transplant Alliance. Spouse of M.A.L. is also a paid consultant to Southwest Transplant Alliance. This arrangement has been reviewed and approved by Johns Hopkins University in accordance with its conflict of interest policies. D.L.S. reports consulting and speaking honoraria from Sanofi, Novartis, CLS Behring, Jazz Pharmaceuticals, Veloxis, Mallinckrodt, and Thermo Fisher Scientific. The other authors declare no conflicts of interest.
Supplemental digital content (SDC) is available for this article. Direct URL citations appear in the printed text, and links to the digital files are provided in the HTML text of this article on the journal’s Web site (www.transplantationdirect.com).
REFERENCES
- 1.Relationships with hospitals, critical access hospitals, and tissue banks. 42 CFR §486.322. 2014. Available at https://advance-lexis-com.ezproxy.med.nyu.edu/api/document?collection=administrative-codes&id=urn:contentItem:6065-P2X1-DYB7-W0YS-00000-00&context=1516831. Accessed April 18, 2022. [Google Scholar]
- 2.Centers for Medicare & Medicaid Services. Medicare and Medicaid programs; organ procurement organizations conditions for coverage: revisions to the outcome measure requirements for organ procurement organizations. 2020. Available at https://www.federalregister.gov/documents/2020/12/02/2020-26329/medicare-and-medicaid-programs-organ-procurement-organizations-conditions-for-coverage-revisions-to. Accessed September 15, 2021.
- 3.Doby BL, Ross-Driscoll K, Shuck M, et al. Public discourse and policy change: absence of harm from increased oversight and transparency in OPO performance. Am J Transplant. 2021;21:2646–2652. [DOI] [PubMed] [Google Scholar]
- 4.Witjes M, Jansen NE, van der Hoeven JG, et al. Interventions aimed at healthcare professionals to increase the number of organ donors: a systematic review. Crit Care. 2019;23:227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Traino HM, Alolod GP, Shafer T, et al. Interim results of a national test of the rapid assessment of hospital procurement barriers in donation (RAPiD). Am J Transplant. 2012;12:3094–3103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Zier JL, Spaulding AB, Finch M, et al. Improved time to notification of impending brain death and increased organ donation using an electronic clinical decision support system. Am J Transplant. 2017;17:2186–2191. [DOI] [PubMed] [Google Scholar]
- 7.Siminoff LA, Gordon N, Hewlett J, et al. Factors influencing families’ consent for donation of solid organs for transplantation. JAMA. 2001;286:71–77. [DOI] [PubMed] [Google Scholar]
- 8.Meyer K, Bjørk IT. Change of focus: from intensive care towards organ donation. Transpl Int. 2008;21:133–139. [DOI] [PubMed] [Google Scholar]
- 9.Niles P, Hewlett J, Liu W, et al. Automated electronic referrals are changing donation. Transplant. 2020;104:259. [Google Scholar]
- 10.Akkas M, Demir MC. Barriers to brain death notifications from emergency departments. Transplant Proc. 2019;51:2171–2175. [DOI] [PubMed] [Google Scholar]
- 11.Koh HK, Jacobson MD, Lyddy AM, et al. A statewide public health approach to improving organ donation: the Massachusetts Organ Donation Initiative. Am J Public Health. 2007;97:30–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Colpaert K, Hoste EA, Steurbaut K, et al. Impact of real-time electronic alerting of acute kidney injury on therapeutic intervention and progression of RIFLE class. Crit Care Med. 2012;40:1164–1170. [DOI] [PubMed] [Google Scholar]
- 13.Amland RC, Lyons JJ, Greene TL, et al. A two-stage clinical decision support system for early recognition and stratification of patients with sepsis: an observational cohort study. JRSM Open. 2015;6:2054270415609004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Okumura LM, Veroneze I, Burgardt CI, et al. Effects of a computerized provider order entry and a clinical decision support system to improve cefazolin use in surgical prophylaxis: a cost saving analysis. Pharm Pract (Granada). 2016;14:717. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Amland RC, Dean BB, Yu H, et al. Computerized clinical decision support to prevent venous thromboembolism among hospitalized patients: proximal outcomes from a multiyear quality improvement project. J Healthc Qual. 2015;37:221–231. [DOI] [PubMed] [Google Scholar]
- 16.Kharbanda AB, Madhok M, Krause E, et al. Implementation of electronic clinical decision support for pediatric appendicitis. Pediatrics. 2016;137:e20151745. [DOI] [PubMed] [Google Scholar]
- 17.Henry NR, Russian CJ, Nespral J. Identifying potential ventilator auto-triggering among organ procurement organization referrals. Prog Transplant. 2016;26:129–134. [DOI] [PubMed] [Google Scholar]
- 18.Squires JE, Coughlin M, Dorrance K, et al. Criteria to identify a potential deceased organ donor: a systematic review. Crit Care Med. 2018;46:1318–1327. [DOI] [PubMed] [Google Scholar]
- 19.Alban RF, Gibbons BL, Bershad VL. Improving donor conversion rates at a level one trauma center: impact of best practice guidelines. Cureus. 2016;8:e891. [DOI] [PMC free article] [PubMed] [Google Scholar]