Abstract
Introduction
Immune checkpoint inhibitors (ICI) such as anti-PD-L1 and anti-PD-1 agents have been proven to be effective in various cancers. However, the rate of non-responders is still high in all cancer entities. Therefore, the identification of biomarkers that could help to optimize therapeutic decision-making is of great clinical importance. Soluble PD-L1 (sPD-L1) and PD-1 (sPD-1) are emerging blood-based biomarkers and were previously shown to be prognostic in various clinical studies.
Objective
We aimed to evaluate the prognostic relevance of sPD-L1 and sPD-1 in patients with different tumor entities who underwent ICI therapy.
Methods
We searched for articles in PubMed via Medline, Embase, Scopus, and Cochrane databases. The primary outcome was overall survival (OS) and progression-free survival (PFS); furthermore, we analyzed on-treatment serum level changes of sPD-L1 and sPD-1 during ICI therapy.
Results
We synthesized the data of 1,054 patients with different cancer types from 15 articles. Pooled univariate analysis showed that elevated levels of sPD-L1 were significantly associated with inferior OS (HR = 1.67; CI:1.26–2.23, I2 = 79%, p < 0.001). The strongest association was found in non-small cell lung cancer, whereas weaker or no association was observed in melanoma as well as in renal cell and esophageal cancers. Pooled multivariate analysis also showed that elevated levels of sPD-L1 correlated with worse OS (HR = 1.62; CI: 1.00–2.62, I2 = 84%, p = 0.05) and PFS (HR = 1.71; CI:1.00–2.94, I2 = 82%, p = 0.051). Furthermore, we observed that one or three months of anti-PD-L1 treatment caused a strong (27.67-fold) elevation of sPD-L1 levels in malignant mesothelioma and urothelial cancer.
Conclusions
We found significantly inferior OS in ICI-treated cancer patients with elevated pre-treatment sPD-L1 levels, but this association seems to be tumor type dependent. In addition, sPD-L1 increases during anti-PD-L1 therapy seems to be therapy specific.
Supplementary Information
The online version contains supplementary material available at 10.1007/s00262-022-03328-9.
Introduction
Recently, growing evidence suggests that immune checkpoint inhibition with both programmed death protein-1 (PD-1) and programmed death protein ligand-1 (PD-L1) inhibitors is effective therapeutic options for several cancer types. Immune checkpoint inhibitors (ICI) revolutionized anti-cancer therapy, but the rate of non-responders is still high and varies significantly between various cancers [1–4]. Therefore, there is a great clinical need for prognostic and predictive biomarkers to identify patients who will respond to ICI therapy. Currently, ICIs are widely used in non-small cell lung cancer (NSCLC), melanoma, renal cell carcinoma (RCC), urothelial cancer, and breast cancer, but the list of indications is rapidly expanding [5].
PD-1 and PD-L1 are membrane-bound co-inhibitory immune checkpoint receptors expressed by various human immune and cancer cells. PD-1 is primarily located in T-cells, whereas PD-L1 is most abundantly expressed by cancer cells. Binding between PD-L1 and its receptor PD-1 leads to immune suppression, which helps cancer cells to escape from cytotoxic T-cell-mediated lysis [6]. PD-1 and PD-L1 are not only found on the surface of cells, but their soluble forms can be detected in blood circulation both in healthy individuals and cancer patients. Similar to its membrane-bond tissue expression, elevated serum PD-L1 (sPD-L1) and PD-1 (sPD-1) levels were generally associated with more advanced disease stages and worse survival, suggesting that these serum markers are prognostic in various tumors [7–11]. However, their predictive value regarding various systemic treatments remained largely contradictory.
There are only few available biomarkers for ICI therapy, such as tissue PD-L1 immunohistochemistry (IHC), tumor mutational burden, or microsatellite instability. However, their predictive ability is different among various tumor types.[12, 13]. For example, PD-L1 immunohistochemistry shows predictive value in NSCLC, head and neck squamous cell (HNSCC), and urothelial cancer [14–16], whereas in melanoma and RCC, PD-L1 IHC cannot be used for the prediction of ICI therapy [17, 18]. In addition, tissue-based IHC has further limitations related to the heterogeneity of PD-L1 expression, different characteristics of various diagnostic antibodies, and differences in evaluation methods [19]. Furthermore, as repeated biopsy for follow-up purposes is hardly feasible, tissue analysis is much less suitable for therapy monitoring than serum-based assays. Therefore, an unmet clinical need is the application of easily accessible, blood-based biomarkers determined by an easy-to-use and robust analytical method for pre-treatment prediction and monitoring of ICI therapy.
In the present study, we conducted a systematic review and meta-analysis of published literature data to assess the prognostic significance of circulating sPD-L1 and sPD-1 levels in pre-treatment and on-treatment samples of tumor patients who underwent ICI therapy.
Methods
The study was reported according to the Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA) 2020 recommendations [20], and the Cochrane Handbook was followed [21]. The protocol was registered on PROSPERO (Nr.:CRD42021283222).
Literature search
Electronic databases from PubMed, Scopus, Embase, and Cochrane library were screened to identify studies investigating the prognostic role of sPD-L1 and sPD-1 in various cancers treated with ICIs. Additionally, references of included studies were screened to identify further potentially eligible studies. Two independent authors (AS and TF) performed the systematic search and the selection process. References were screened using EndNote X9 (Clarivate Analytics, Philadelphia, PA, USA) and assessed by title, abstract, and full text.
Eligibility criteria
The PECO framework was applied to state our research question. We included original studies in the English language, which investigated (P) ICI-treated patients with various tumors, and (E and C) compared the hazard of high and low serum or plasma sPD-L1 and/or sPD-1 levels in regard to (O) overall survival (OS) or progression-free survival (PFS). There was no pre-defined cut-off value for the definition of high and low levels of biomarkers. If available, on-treatment sPD-L1 and sPD-1 concentrations (median or mean level, range, or interquartile range) were also considered as additionally assessed parameters.
The following exclusion criteria were used: study design: reviews, comments, letters, meta-analysis, systematic reviews, animal experiments, and conference abstracts. No restrictions were made regarding cohort size and study design.
Data extraction
Two independent authors (AS, TF) extracted data by reading full-text articles. Extracted parameters were the following: the first name of the author, year of publication, cancer type, ICI therapy type, country of sample/data collection, study type, cohort size, patient age, sex, cut-off values for sPD1/sPD-L1, cut-off definition method (e.g., median, receiver operating characteristic curve—ROC), assay method, follow-up time, OS, and PFS.
In eligible studies, either the article provided calculated hazard ratios (HR) with a 95% Confidence Interval (CI), or the overall HR and 95% CI were estimated from Kaplan–Meier curves by using the GetData Graph Digitizer software v2.26™. In addition, when available, data on changes of sPD-L1 and sPD-1 during ICI treatment were extracted.
Quality assessment and evaluation of evidence
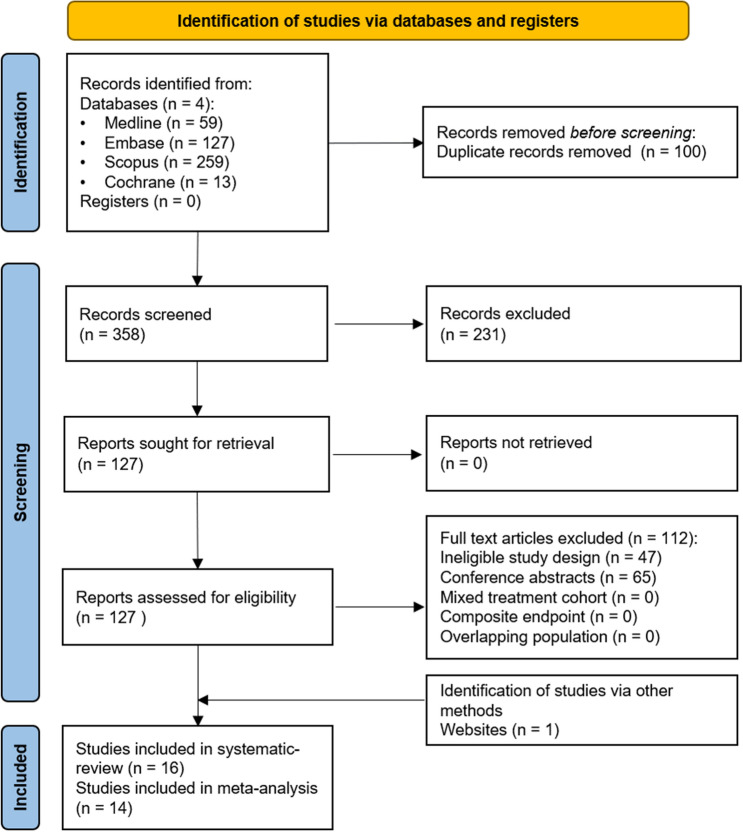
Two independent authors performed the risk of bias assessment using the Quality in Prognostic Studies (QUIPS) tool [22]. The study attrition domain was assessed only in the case of prospective studies. We used the RobVisR tool to summarize the results of the assessments [23]. (Supplementary Table 1, Fig. 1) For the level of evidence assessment, the GRADEpro™ program [24]. (Supplementary Table 2) was applied.
Fig. 1.
PRISMA 2020 flowchart representing the study selection process
Synthesis methods
Random-effects models with the inverse variance method were applied to pool hazard ratios (HR) with 95% confidence interval (CI) in the case of all outcomes. For the outcomes where the study number was over 5, a Hartung–Knapp adjustment [25, 26] was applied. The restricted maximum-likelihood method [27] was used to estimate variance measure 2τ2, and between-study heterogeneity was investigated with Cochrane Q test and the Higgins & Thompson’s I2I2 statistics [28]. The Q test was considered significant when the p value was less than 0.1. Forest plots were used to graphically summarize the results. Where applicable we reported the prediction intervals of results according to IntHout et al. [29]. Outlier and influence analyses were carried out following the recommendations of Harrer [27] and Viechtbauer and Cheung [30]. Small study effect was investigated on funnel plots, and if there had been at least 10 studies, it would have been assessed statistically using Egger’s test. Subgroup analysis was conducted based on the used ELISA assays and cancer types. In the case of subgroup analysis, a fixed-effects “plural” model was applied (aka. mixed-effects model). To assess the difference between the subgroups, Cochrane Q test was used [27]. The null hypothesis was rejected at a 5% significance level. All statistical analyses were performed with R [31] statistical environment and language, using the meta [32] and dmetar [33] packages. P < 0.05 was considered significant. Biomarker level changes were expressed as fold-changes, and a median fold-change was calculated separately for PD-1 and PD-L1 inhibitors (Table 2).
Table 2.
Dynamic changes of sPD-L1 and sPD-1 levels before and after 1–3 months of immune checkpoint inhibitor therapy
| Author (year) | Type of cancer | Type of treatment | No. of patients | Pre-treatment median sPD-L1 (pg/mL) | No. of patients | On-treatment (1–3 months) median sPD-L1 (pg/mL) | Fold change |
|---|---|---|---|---|---|---|---|
| Incorvaia et al. 2020 [38] | RCC | anti-PD-1 | 9 | 1090.0 (R 470.0–2410.0) | 9 | 730.0 (R 560.0–1390.0) | 0.67 |
| Meyo et al. 2020 [42] | NSCLC | anti-PD-1 | 50 | 160.0 (IQR 30.0–440.0) | 50 | 130.0 (IQR 30.0–380.0) | 0.81 |
| Mahoney et al. 2021 [40] | Melanoma | anti-PD-1 | 78 | 2312.0 | 78 | 2247.0 | 0.97 |
| Yang et al. 2021 [47] | NSCLC | anti-PD-1 | 19 | 37.7 (R 15.6–152.0) | 19 | 36.7 (R 15.6–109.0) | 0.97 |
| Mahoney et al. 2021 [40] | RCC | anti-PD-1 | 91 | 1978.0 | 91 | 2179.0 | 1.10 |
| Costantini et al. 2018 [37] | NSCLC | anti-PD-1 | 43 | 39.8 (IQR 29.8–59.2) | 43 | 51.6 (IQR 31.9–72.1) | 1.30 |
| Ando et al. 2019 [34] | mixed | anti-PD-1 | 21 | 347.4 (R 251.9–1491.1) | 9 | 468.8 (R 256.5–881.3) | 1.35 |
| Oh et al. 2021 [45] | Genitourinary | Mixed | 10 | 11.8 (R 5.9–21.5) | 10 | 17.1 (R 6.0–93.5) | 1.46 |
| Castello et al. 2020 [35] | NSCLC | anti-PD-1 | 20 | 27.2 (R 11.2–61.3) | 20 | 43.9 (R 19.6–77.8) | 1.61 |
| Oh et al. 2021 [45] | NSCLC | Mixed | 16 | 15.0 (R 3.8–51.9) | 10 | 58.4 (R 8.7–139.5) | 3.89 |
| Krafft et al. 2021 [10] | Urothelial | anti-PD-L1 | 19 | 71.2 (R 42.2–192.1) | 8 | 1946.5 (R 1694.0–1993.0) | 27.34 |
| Chiarucci et al. 2020 [36] | Mesothelioma | anti-PD-L1 | 29 | 70.0 (R 20.0–190.0) | 14 | 1960.0 (R 1330.0–2750.0) | 28.00 |
| Author (year) | Type of cancer | Type of treatment | No. of patients | Pre-treatment median sPD-1 (pg/mL) | No. of patients | On-treatment (1–3 months) median sPD-1 (pg/mL) | Fold change |
|---|---|---|---|---|---|---|---|
| Incorvaia et al. 2020 [38] | RCC | anti-PD-1 | 9 | 13,250.0 (R 1220.0- 25,000.0) | 9 | 1230.0 (R 1060.0–1930.0) | 0.09 |
| Meyo et al. 2020 [42] | NSCLC | anti-PD-1 | 50 | 70.0 (IQR 30.0–180.0) | 50 | 70.0 (IQR 30.0–200.0) | 1.0 |
Results
Search and selection
Using the above-defined search key, 458 articles were initially retrieved from the accessed databases (Fig. 1). After the selection process, 16 articles matched our eligibility criteria [10, 34–48]. However, the HR and 95% CI estimation in two articles were not possible [34, 35]. Therefore, these two articles were included only in the qualitative synthesis.
Baseline characteristics of included studies
Baseline characteristics of the included articles are summarized in Table 1. Cancer types included in this systematic review were the following: NSCLC, RCC, melanoma, esophageal squamous cell cancer (ESCC), urothelial cancer, and mesothelioma. Nine articles reported the results of prospectively performed studies, and seven articles were retrospective. Only three articles included data on sPD-1, and all the included publications reported on sPD-L1. Different studies used different strategies to set cut-off values; six studies used the median as cut-off, while eight used the ROC analysis to adjust the cut-off values. All but one study used the ELISA assay technique to determine sPD-1 or sPD-L1 concentrations. Nine studies applied ELISA assays by R&D Systems (Wiesbaden, Germany), and other studies used assays by Cloud-Clone (Dynabio, Marseille, France), Abcam (Cambridge, UK), Invitrogen (Thermo Fisher, Darmstadt, Germany), and SIMOA (Billerica, MA, USA). The remaining article used a multiplex immunoassay (14-ProcartaPlex Human Immuno-Oncology Checkpoint Panel by Invitrogen (Thermo Fisher, Darmstadt, Germany)). Ten articles reported on-treatment sPD-1/sPD-L1 levels in addition to baseline levels [10, 34–38, 40, 42, 45, 47].
Table 1.
Basic characteristics of included studies
| Author (year) | Type of cancer treatment | Study site/type | No. of patients (female %) |
Age (year) | Biomarker/Cut-off(pg/mL)/type of cut-off | Follow-up period (months) | Type of ELISA | Outcome |
|---|---|---|---|---|---|---|---|---|
| Ando et al. 2019† [34] |
NSCLC—Nivo/ Pembro Gastric—Nivo/ Pembro Bladder—Pembro |
Japan/R | 21 (29) | NA | sPD-L1/347/median | 6.0 (1.0–27.0) | R&D | OS |
| Castello et al. 2020† [35] | NSCLC—mixed | Italy/P | 20 (35) | 77 (51–86) | sPD-L1/27.2/median | 10.3 (2.0–29.0) | R&D | OS/PFS |
| Chiarucci et al. 2020 [36] | Mesothelioma—Durva/Termeli | Italy/P | 40 (34) | 66 (42–83) | sPD-L1/70/median | 19.2 (13.8 – 20.5) * | R&D | OS |
| Costantini et al. 2018 [37] | NSCLC—Nivo | France/R | 43 (33) | 68 (62–72) | sPD-L1/34/ROC | 16.3 (11.7–21.1) * | Abcam | OS/PFS |
| Incorvaia et al. 2020 [38] | RCC—Nivo | Italy/P | 21 (10) | 61 (36–70) |
sPD-L1/660/ROC sPD-1/2110/ROC |
NA | DYNABIO | PFS |
| Ji et al. 2020 [39] |
ESCC—anti-PD-1 Mixed–mixed |
China/R |
21 (5) 61 (39) |
57 (46–70) 43 (21–64) |
sPD-L1/NA/ROC | NA | Multiplex immunoassay kit | OS/PFS |
| Krafft et al. 2021# [10] | Urothelial—Atezo/Pembro | Hungary/P | 19 (26) | 66 (43 – 77) | sPD-L1/76/median | 17.0 (6.0–31.0) | R&D | OS/PFS |
| Mahoney et al. 2021 [40] |
RCC—Nivo Melanoma—Nivo |
USA/P |
91 (33) 78 (44) |
NA | sPD-L1/NA/NA | NA | SIMOA | OS/PFS |
| Mazzaschi et al. 2020 [41] | NSCLC—Nivo/Pembro/Atezo | Italy/P | 109 (33) | 72 (41–85) | sPD-L1/113/CART tree | 17.3 | R&D | OS/PFS |
| Meyo et al. 2020 [42] | NSCLC—Nivo | France/P | 51 (43) | 66 (60 – 69) |
sPD-L1/160/median sPD-1/70/median |
26.4 (18.1 – 36.5) | Cloud-Clone | OS/PFS |
| Murakami et al. 2020 [43] | NSCLC—Pembro/Nivo | Japan/R | 233 (35) | 63 (30–84) | sPD-L1/90/mean + 2sd | NA | R&D | OS/PFS |
| Okuma et al. 2018 [44] | NSCLC—Nivo | Japan/P | 39 (26) | 69 (50–88) | sPD-L1/3357/ROC | NA | Cloud-Clone | OS |
| Oh et al. 2021 [45] | Mixed–mixed | Korea/R | 128 (31) | 62 (21–82) | sPD-L1/11/ROC | NA | Invitrogen | OS/PFS |
| Ugurel et al. 2019 [46] | Melanoma—anti-PD-1 | Germany/R | 85 (41) | 62** |
sPD-L1/10/ROC sPD-1/500/ROC |
12.1 | R&D | OS/PFS |
| Yang et al. 2021 [47] | NSCLC—mixed | China/P | 21 (NA) | NA | sPD-L1/0.95##/fold change | NA | R&D | OS/PFS |
| Zhou et al. 2017 [48] | Melanoma—Pembro | USA/NA | 35 (NA) | NA | sPD-L1/1400/NA | NA | R&D | OS |
Nivo—nivolumab, Pembro—pembrolizumab, Termeli—tremelimumab, Durva—durvalumab, Atezo—atezolizumab, NSCLC—non-small cell lung cancer, RCC—renal cell carcinoma, ESCC—esophageal squamous cell carcinoma, R—retrospective, P—prospective, ROC—receiver operating curve, CART—Classification and Regression Trees, sd—standard deviation, OS—overall survival, PFS—progression-free survival *IQR, **mean, † included only in systematic review, # cohort data are supplemented with unpublished data, ## Fold change
Elevated pre-treatment sPD-L1 predicts OS in NSCLC and melanoma
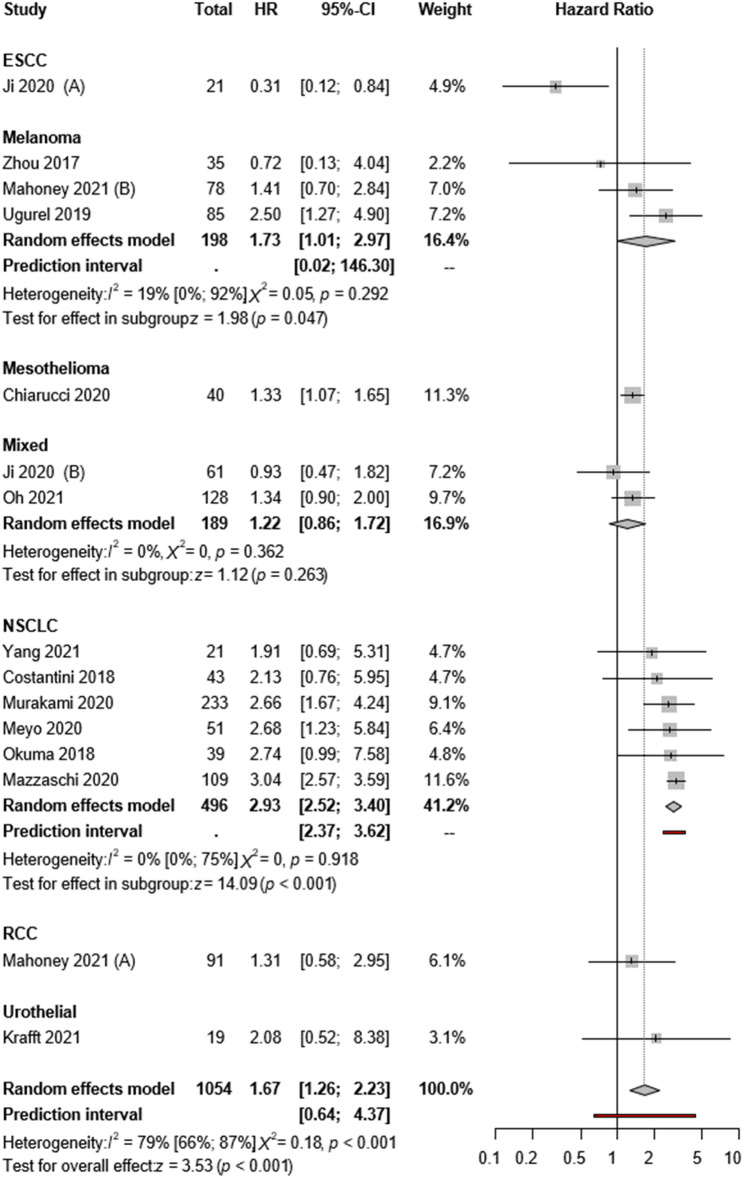
Thirteen articles reported univariate OS as a primary outcome. The pooled overall estimate showed that patients with high sPD-L1 levels had worse OS (HR:1.67; CI:1.26–2.23, I2 = 79%, p < 0.001; Fig. 2). As for publication bias, the funnel plot seems asymmetric; however, Egger’s test shows no publication bias (p = 0.177)(Supplementary Figs. 5 and 7).
Fig. 2.
Forest plots representing hazard ratios of OS for sPD-L1 in different tumor types
Four of the included articles reported a multivariate Cox proportional hazard model. The pooled multivariate analysis confirmed that patients with high sPD-L1 levels had shorter OS (HR:1.62; CI:1.00–2.62, I2 = 84%, p = 0.05; Supplementary Fig. 2).
A subgroup analysis was performed according to cancer type. Based on six studies with NSCLC patients, high sPD-L1 levels were consequently associated with poor OS (HR:2.93; CI:2.52–3.40, I2 = 0%, p < 0.001). According to three publications, poorer OS was found for malignant melanoma (HR:1.73; CI:1.01–2.97, I2 = 19% p = 0.047). No difference was found between high and low sPD-L1 levels in OS in the subgroup of mixed tumor types (HR:1.22; CI:0.86–1.72, I2 = 0%, p = 0.263), but in this case, various studies showed rather heterogeneous results (Fig. 2).
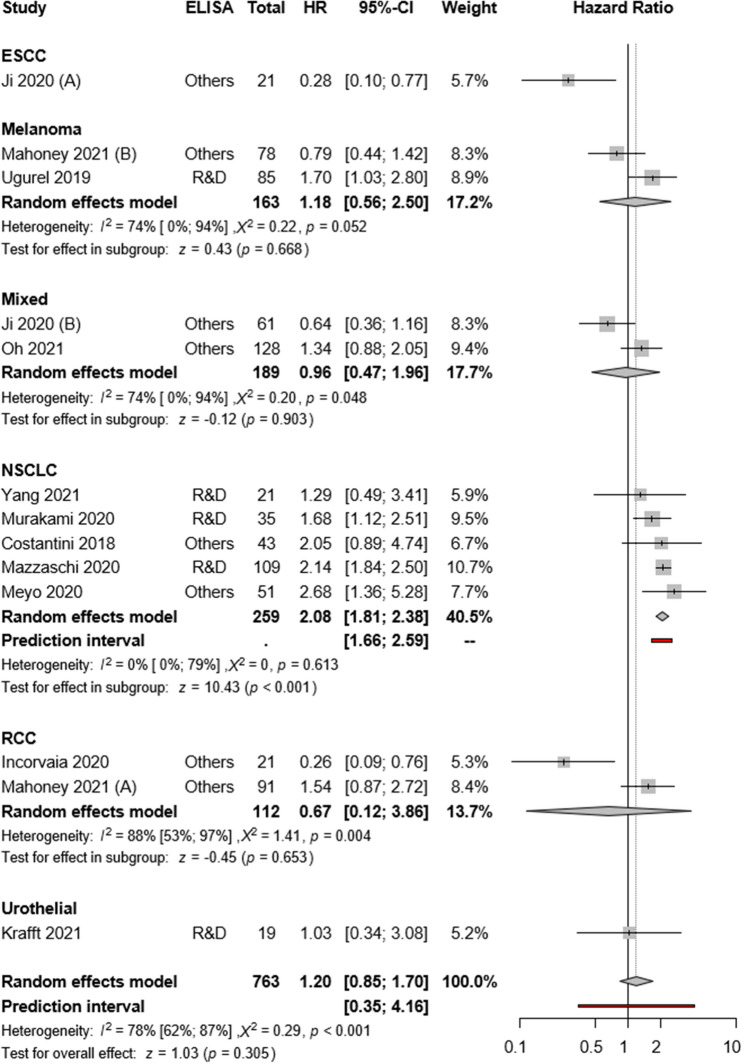
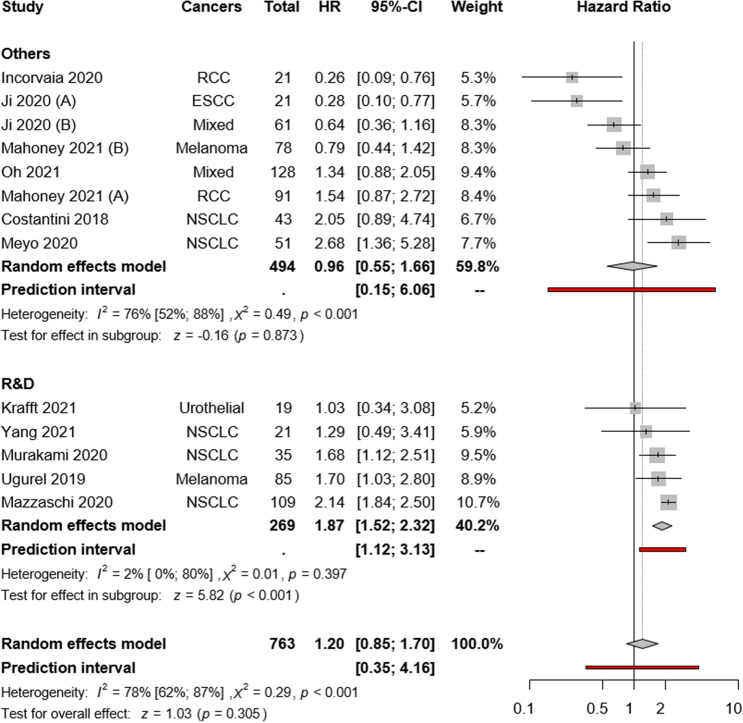
Elevated pre-treatment sPD-L1 predicts poor PFS in NSCLC
Eleven articles reported univariate PFS as the primary outcome. The pooled overall estimate found no PFS difference between high and low sPD-L1 groups (HR:1.20; CI:0.85–1.70, I2 = 78%, p = 0.305; Fig. 3). The visual presentation of the Funnel plot and Egger’s test suggested publication bias (p = 0.007) (Supplementary Figs. 6 and 8).
Fig. 3.
Forest plots representing hazard ratios of PFS for sPD-L1 in different tumor types
Four of the included articles reported a multivariate Cox proportional hazard model. The pooled multivariate analysis showed that patients with high sPD-L1 levels tended to have inferior PFS (HR:1.71; CI:1.00–2.94, I2 = 82%, p = 0.051; Supplementary Fig. 3).
The subgroup analysis of cancer types revealed high pre-treatment sPD-L1 as a strong risk factor in the NSCLC subgroup (HR:2.08; CI:1.81–2.38, I2 = 0% p < 0.001), whereas rather heterogeneous results were observed in RCC (HR:0.67; CI:0.12–3.86, I2 = 88% p = 0.653), melanoma (HR:1.18; CI: 0.56–2.50, I2 = 74%, p = 0.668) and mixed cohorts (HR:0.96; CI:0.47–1.96, I2 = 74%, p = 0.903) (Fig. 3).
Pre-treatment sPD-1 and PFS and OS
Three articles reported PFS for sPD-1 (HR:1.16; CI:0.23–5.75, I2 = 89%, p = 0.858) (Supplementary Fig. 4) with heterogeneous results. Meyo et al. in NSCLC and Ugurel et al. found in melanoma that higher sPD-1 level patients had shorter PFS, whereas Incorvaia et al. found the opposite result in metastatic RCC [38, 42, 46].
Meyo et al. (HR:2.28; CI:1.11–4.68; p = 0.025) and Ugurel et al. (HR:2.70; CI:1.10–6.25; p = 0.055) reported sPD-1 and OS [42, 46].
sPD-L1 levels strongly increase during anti-PD-L1 therapy
Ten articles reported both pre-treatment and on-treatment sPD-L1 levels in 12 tumor entities. Serum sPD-L1 levels remained unchanged under anti-PD-1 therapy, whereas anti-PD-L1 therapy caused a remarkable (27.67-fold) elevation of sPD-L1 levels (Table 2). Two articles reported both pre-treatment and on-treatment sPD-1 levels during anti-PD-1 (nivolumab) therapy [38, 42] (Table 2).
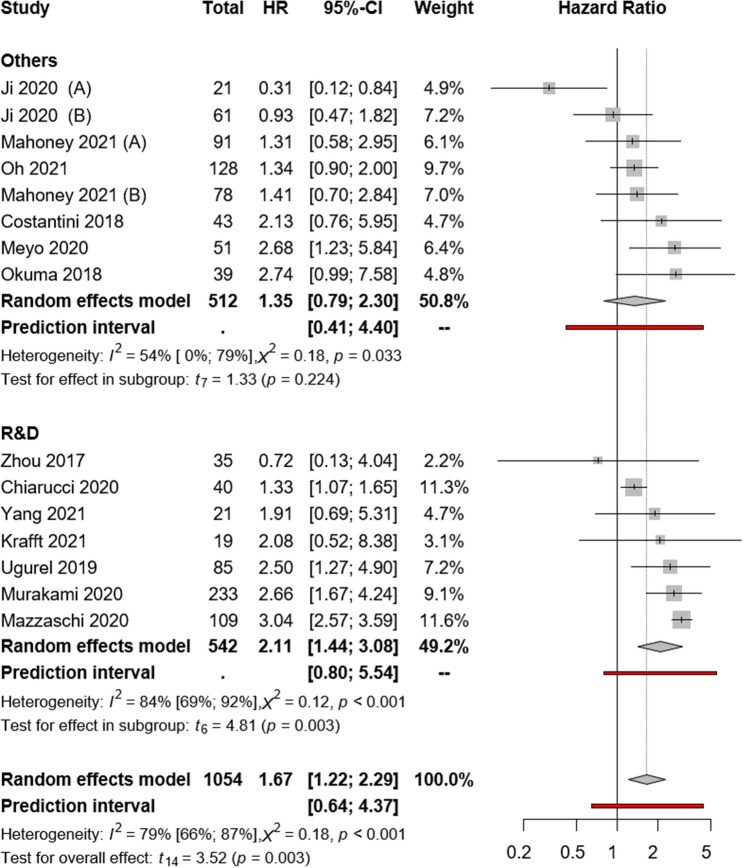
The assay method does not seem to influence the correlations between sPD-L1 and OS
Our subgroup analysis according to the used assay methods suggested that the sPD-L1 assay method had no major influence on the OS (R&D: HR:2.11; CI:1.44–3.08, I2 = 84%, p = 0.003 vs. “others”: HR:1.35; CI:0.79–2.30, I2 = 54%, p = 0.224; Fig. 4). The same subgroup analysis was further evaluated based on PFS. Our subgroup analysis suggested that the sPD-L1 assay method might influence PFS. (R&D: HR:1.87; CI:1.52–2.32, I2 = 2%, p = 0.025 vs. “others”: HR:0.96; CI:0.55–1.66, I2 = 76%, p = 0.873; Fig. 5). Because of the low number of studies with sPD-1, no comparison was possible between various assay methods.
Fig. 4.
Forest plots representing hazard ratios of OS for sPD-L1 for different ELISA kits
Fig. 5.
Forest plots representing hazard ratios of PFS for sPD-L1 for different ELISA kits
Risk of bias assessment and level of evidence
Based on author judgment, 12 out of 16 articles had a low risk of bias, while four carried a moderate risk (Supplementary Fig. 1, Supplementary Table 1).
Grading
On the basis of GRADEpro™, moderate certainty of the evidence was found for the two primary endpoints (Supplementary Table 2).
Discussion
This meta-analysis aimed to summarize the data of currently available literature on the prognostic significance of sPD-L1 and sPD-1 in various cancers in the aspect of ICI therapy. Serum sPD-1 and sPD-L1 are easily accessible biomarkers that may help in pre-treatment prognostication and in therapy monitoring of patients who underwent ICI therapy.
In the past few years, several studies assessed the association between sPD-L1 and prognosis in various cancers and treatment settings. Huang et al. constructed a meta-analysis in 2021 to assess the correlation between sPD-L1 and survival in a wide range of human malignancies [49]. The pooled overall estimate showed sPD-L1 as a significant indicator of shorter OS in various cancers. However, the article contained only three ICI therapy-related articles that did not allow to draw firm conclusions. Recently, a significant number of research articles have been published focusing on sPD-L1 (or sPD-1) levels in the context of ICI therapy, and these articles provided contradictory results concerning the prognostic role of sPD-L1. For example, Incorvaia et al. found that nivolumab-treated metastatic RCC patients with high sPD-L1, sPD-1, and BTN3A1 levels had better PFS [38]. In contrast, Mahoney et al. in the Checkmate 009 trial found no significant survival benefits for RCC patients with high sPD-L1 levels [40]. In addition, Ji et al. also found significantly higher disease control in ICI-treated ESCC patients as well as better survival rates for patients with high sPD-L1 levels [39]. In contrast, in NSCLC studies, high sPD-L1 levels consequently tended to be associated with shorter patient survival in ICI-treated patients. This finding is in line with the previous meta-analysis by Liao et al., suggesting that low rather than high sPD-L1 levels might have predictive values for ICI treatment [50].
In the present meta-analysis, summarizing data from 16 publications including more than six cancer types and an overall number of 1,054 ICI-treated patients, a 67% higher risk of death was found in patients with high sPD-L1 levels. Similarly, patients with high sPD-L1 levels had a 20% higher risk of disease progression. Interestingly, our subgroup analyses for different tumor entities revealed a heterogeneous pattern. For melanoma, we found three eligible publications with 198 ICI-treated patients, and the observed hazard ratios for OS and PFS revealed a rather heterogeneous picture regarding the prognostic value of sPD-L1 in melanoma. In contrast, for NSCLC, the pooled analysis of six studies with an overall number of 457 ICI-treated patients provided a much more consistent results for both OS and PFS across various studies. Overall, our summary suggests an association between higher sPD-L1 levels and poor prognosis. However, this effect may be different in distinct tumor types. On the basis of these, a tumor type-specific interpretation is suggested for the prognostic value of sPD-L1 in ICI-treated patients. The prognostic value of sPD-L1 is not sufficiently confirmed in melanoma patients, whereas several independent studies confirmed it in NSCLC. Therefore, in NSCLC, pre-treatment sPD-L1 may be a potential biomarker to predict OS and PFS before ICI therapy. On the other hand, in NSCLC, sPD-L1 levels were associated with shorter survival in other therapy settings, suggesting that sPD-L1 might be rather a prognostic than a predictive factor. Further prospective studies are necessary to address this question.
As there are several commercially available sPD-L1 assay kits, we assessed the potential influence of the assay method on study results. Overall, in the 16 included studies, seven different assay kits were applied, with the R&D kit as the most commonly used. However, slightly worse survival rates were found in studies that used the R&D assay, but the visual interpretation of the plot (Figs. 4 and 5) revealed a similar distribution of the articles around the line of no effect. Therefore, we conclude that the ELISA method may not significantly influence the outcomes.
Four articles presented the multivariate analysis of OS and PFS, and the pooled estimate showed high sPD-L1 as an independent risk factor for ICI therapy. However, these articles presented different factors as independent determinators of both OS and PFS. In these four articles, ECOG performance status was consequently found to be a significant independent predictor of survival, whereas tissue expression of PD-L1 was independently associated with poor OS in three articles. Furthermore, two articles showed high neutrophil-to-lymphocyte ratio as an independent predictor of poor OS in a multivariate analysis, suggesting that inflammation status has an inevitable impact on ICI-sensitivity.
Comparison between baseline and on-treatment sPD-L1 levels was possible in 12 studies. Based on our previous observation in urothelial cancer, we hypothesized that anti-PD-L1 therapy leads to an elevation in sPD-L1 levels [10]. Accordingly, in the two studies with presenting patients who received anti-PD-L1 therapy a strong (27- and 28-fold) increase in sPD-L1 levels could be observed [10, 36], whereas no such difference was detected in anti-PD-1-treated patients [34, 35, 37, 38, 40, 42, 45, 47]. Furthermore, sPD-1 levels did not increase after anti-PD-1 (nivolumab) therapy [38, 42]. In contrast, Music et al. observed that sPD-1 elevated after the administration of anti-PD-1 pembrolizumab therapy [51]. Therefore, it appears that anti-PD-L1 rather than anti-PD-1 therapy induces a significant increase in sPD-L1 levels. However, one possible explanation could be that ICIs—especially atezolizumab—can trigger a strong anti-drug-antibody (ADA) production, which may form antibody complexes that can enhance the measured ELISA signal [52]. On the basis of these, the on-treatment flare-up of sPD-L1 seems to be therapy specific for anti-PD-L1 therapy, but the biological and clinical relevance of this elevation needs to be further evaluated.
Our study has some limitations mainly related to the heterogeneity of the included studies regarding their cohort sizes, tumor types, applied ICI drugs, and cut-off values. A further limitation is the unavailability of radiographic response data.
The strength of our study is that it is the first meta-analysis focusing on the prognostic values of sPD-L1 and sPD-1 in a particular group of ICI-treated cancer patients. Furthermore, we evaluated 16 eligible studies with > 1,000 cases using both OS and PFS as endpoints and evaluated results in the context of tumor type, assay method, and marker level changes.
Conclusion
In conclusion, we found significantly worse OS in ICI-treated cancer patients with high baseline sPD-L1 levels, but this association seems to be tumor type dependent. Therefore, we suggest that sPD-L1 as a pre-treatment prognostic biomarker for ICI therapy, which should be interpreted in a tumor type-specific context. In addition, we found a remarkably strong increase in sPD-L1 during anti-PD-L1 treatment. The biological background and clinical significance of this sPD-L1 flare need to be evaluated in future studies. A further prospectively designed biomarker-based randomized clinical trial is of great need to reveal the therapy predictive role of sPD-L1.
Supplementary Information
Below is the link to the electronic supplementary material.
Acknowledgements
This study was supported by the K139059 grant of the Ministry for Innovation and Technology from the source of the National Research Development and Innovation Fund. T.S. was supported by a János Bolyai Research Scholarship of the Hungarian Academy of Sciences (BO/00451/20/5) and by the New National Excellence Program (ÚNKP-21-5-SE-3). A.C. was supported by the New National Excellence Program (ÚNKP-21-3-II-SE-13).
Author contribution
Conceptualization was contributed by AS, FT, and SV; project administration was contributed by SV, PH, PN, and TS; methodology was contributed by SV, BH, AC, MV, and AV; formal analysis was contributed by AV, BH, AC, and PTK; writing—original draft, was contributed by AS, AV, SV, and ST; visualization was contributed by PTK, UK, VG, UH, and AV; data curation was contributed by UK, VG, UH, and VG; writing—review and editing, was contributed by AS, FT, SV, BH, AC, PTK, BH, TS, VG, and NP; supervision was contributed by PH, NP, TS, and BH; funding acquisition was contributed by PH, NP, and TS. All authors certify that they have participated sufficiently in the work to take public responsibility for the content, including participation in the concept, design, analysis, writing, or revision of the manuscript.
Funding
Open access funding provided by Semmelweis University. Sponsors had no role in the design, data collection, analysis, interpretation, and manuscript preparation.
Declarations
Conflict of interest
BH reports personal fees from AAA/Novartis, ABX, Bayer, LightPoint Medical, Inc., Janssen R&D, Bristol–Myers Squibb, and Astellas; research funding from Profound Medical, German Cancer Aid, German Research Foundation, Janssen R&D, Bristol–Myers Squibb, MSD, Pfizer, and Astellas; and travel fees from AstraZeneca, Janssen R&D, and Astellas; all outside the current manuscript. The other authors report none to declare.
Ethical approval
No ethical approval was required for this systematic review with meta-analysis, as all data were already published in peer-reviewed journals. Furthermore, no patients were involved in the design, conduct, or interpretation of our study. The datasets used in this study can be found in the full-text articles included in the systematic review and meta-analysis.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Péter Nyirády and Tibor Szarvas authors have contributed equally to this work.
References
- 1.Doroshow DB, Sanmamed MF, Hastings K, Politi K, Rimm DL, Chen L, Melero I, Schalper KA, Herbst RS. Immunotherapy in non-small cell lung cancer: facts and hopes. Clin Cancer Res. 2019;25:4592–4602. doi: 10.1158/1078-0432.CCR-18-1538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Gide TN, Wilmott JS, Scolyer RA, Long GV. Primary and Acquired resistance to immune checkpoint inhibitors in metastatic melanoma. Clin Cancer Res. 2018;24:1260–1270. doi: 10.1158/1078-0432.CCR-17-2267. [DOI] [PubMed] [Google Scholar]
- 3.Raimondi A, Randon G, Sepe P, Claps M, Verzoni E, de Braud F, Procopio G. The evaluation of response to immunotherapy in metastatic renal cell carcinoma: open challenges in the clinical practice. Int J Mol Sci. 2019 doi: 10.3390/ijms20174263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ramos JD, Yu EY. Making urothelial carcinomas less immune to immunotherapy. Urol Oncol. 2016;34:534–537. doi: 10.1016/j.urolonc.2016.10.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Jacob JB, Jacob MK, Parajuli P. Review of immune checkpoint inhibitors in immuno-oncology. Adv Pharmacol. 2021;91:111–139. doi: 10.1016/bs.apha.2021.01.002. [DOI] [PubMed] [Google Scholar]
- 6.Sun C, Mezzadra R, Schumacher TN. Regulation and function of the PD-L1 checkpoint. Immunity. 2018;48:434–452. doi: 10.1016/j.immuni.2018.03.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Chang B, Huang T, Wei H, Shen L, Zhu D, He W, Chen Q, Zhang H, Li Y, Huang R, et al. The correlation and prognostic value of serum levels of soluble programmed death protein 1 (sPD-1) and soluble programmed death-ligand 1 (sPD-L1) in patients with hepatocellular carcinoma. Cancer Immunol Immunother. 2019;68:353–363. doi: 10.1007/s00262-018-2271-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Abu Hejleh T, Furqan M, Ballas Z, Clamon G. The clinical significance of soluble PD-1 and PD-L1 in lung cancer. Crit Rev Oncol Hematol. 2019;143:148–152. doi: 10.1016/j.critrevonc.2019.08.009. [DOI] [PubMed] [Google Scholar]
- 9.Hassen G, Kasar A, Jain N, Berry S, Dave J, Zouetr M, Priyanka Ganapathiraju VLN, Kurapati T, Oshai S, Saad M, et al. Programmed death-ligand 1 (PD-L1) positivity and factors associated with poor prognosis in patients with gastric cancer: an umbrella meta-analysis. Cureus. 2022;14:e23845. doi: 10.7759/cureus.23845. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Krafft U, Olah C, Reis H, Kesch C, Darr C, Grunwald V, Tschirdewahn S, Hadaschik B, Horvath O, Kenessey I, et al. High serum PD-L1 levels are associated with poor survival in urothelial cancer patients treated with chemotherapy and immune checkpoint inhibitor therapy. Cancers (Basel) 2021 doi: 10.3390/cancers13112548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bian B, Fanale D, Dusetti N, Roque J, Pastor S, Chretien AS, Incorvaia L, Russo A, Olive D, Iovanna J. Prognostic significance of circulating PD-1, PD-L1, pan-BTN3As, BTN3A1 and BTLA in patients with pancreatic adenocarcinoma. Oncoimmunology. 2019;8:e1561120. doi: 10.1080/2162402X.2018.1561120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Palmeri M, Mehnert J, Silk AW, Jabbour SK, Ganesan S, Popli P, Riedlinger G, Stephenson R, de Meritens AB, Leiser A, et al. Real-world application of tumor mutational burden-high (TMB-high) and microsatellite instability (MSI) confirms their utility as immunotherapy biomarkers. ESMO Open. 2022;7:100336. doi: 10.1016/j.esmoop.2021.100336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Patel SP, Kurzrock R. PD-L1 Expression as a predictive biomarker in cancer immunotherapy. Mol Cancer Ther. 2015;14:847–856. doi: 10.1158/1535-7163.MCT-14-0983. [DOI] [PubMed] [Google Scholar]
- 14.Burtness B, Harrington KJ, Greil R, Soulières D, Tahara M, de Castro G, Psyrri A, Basté N, Neupane P, Bratland Å, et al. Pembrolizumab alone or with chemotherapy versus cetuximab with chemotherapy for recurrent or metastatic squamous cell carcinoma of the head and neck (KEYNOTE-048): a randomised, open-label, phase 3 study. Lancet. 2019;394:1915–1928. doi: 10.1016/s0140-6736(19)32591-7. [DOI] [PubMed] [Google Scholar]
- 15.Lantuejoul S, Sound-Tsao M, Cooper WA, Girard N, Hirsch FR, Roden AC, Lopez-Rios F, Jain D, Chou TY, Motoi N, et al. PD-L1 testing for lung cancer in 2019: perspective from the IASLC pathology committee. J Thorac Oncol. 2020;15:499–519. doi: 10.1016/j.jtho.2019.12.107. [DOI] [PubMed] [Google Scholar]
- 16.Eckstein M, Cimadamore A, Hartmann A, Lopez-Beltran A, Cheng L, Scarpelli M, Montironi R, Gevaert T. PD-L1 assessment in urothelial carcinoma: a practical approach. Ann Transl Med. 2019;7:690. doi: 10.21037/atm.2019.10.24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Motzer RJ, Escudier B, McDermott DF, George S, Hammers HJ, Srinivas S, Tykodi SS, Sosman JA, Procopio G, Plimack ER, et al. Nivolumab versus everolimus in advanced renal-cell carcinoma. N Engl J Med. 2015;373:1803–1813. doi: 10.1056/NEJMoa1510665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Madore J, Vilain RE, Menzies AM, Kakavand H, Wilmott JS, Hyman J, Yearley JH, Kefford RF, Thompson JF, Long GV, et al. PD-L1 expression in melanoma shows marked heterogeneity within and between patients: implications for anti-PD-1/PD-L1 clinical trials. Pigment Cell Melanoma Res. 2015;28:245–253. doi: 10.1111/pcmr.12340. [DOI] [PubMed] [Google Scholar]
- 19.Paver EC, Cooper WA, Colebatch AJ, Ferguson PM, Hill SK, Lum T, Shin JS, O'Toole S, Anderson L, Scolyer RA, et al. Programmed death ligand-1 (PD-L1) as a predictive marker for immunotherapy in solid tumours: a guide to immunohistochemistry implementation and interpretation. Pathology. 2021;53:141–156. doi: 10.1016/j.pathol.2020.10.007. [DOI] [PubMed] [Google Scholar]
- 20.Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, Shamseer L, Tetzlaff JM, Akl EA, Brennan SE, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372:n71. doi: 10.1136/bmj.n71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Higgins JP, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, Welch VA. Cochrane handbook for systematic reviews of interventions. Hoboken: John Wiley & Sons; 2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Hayden JA, van der Windt DA, Cartwright JL, Côté P, Bombardier C. Assessing Bias in Studies of Prognostic Factors. Ann Intern Med. 2013;158:280–286. doi: 10.7326/0003-4819-158-4-201302190-00009. [DOI] [PubMed] [Google Scholar]
- 23.McGuinness LA, Higgins JPT. Risk-of-bias VISualization (robvis): an R package and Shiny web app for visualizing risk-of-bias assessments. Res Synth Methods. 2021;12:55–61. doi: 10.1002/jrsm.1411. [DOI] [PubMed] [Google Scholar]
- 24.Guyatt G, Oxman AD, Akl EA, Kunz R, Vist G, Brozek J, Norris S, Falck-Ytter Y, Glasziou P, DeBeer H, et al. GRADE guidelines: 1. Introduction-GRADE evidence profiles and summary of findings tables. J Clin Epidemiol. 2011;64:383–394. doi: 10.1016/j.jclinepi.2010.04.026. [DOI] [PubMed] [Google Scholar]
- 25.Knapp G, Hartung J. Improved tests for a random effects meta-regression with a single covariate. Stat Med. 2003;22:2693–2710. doi: 10.1002/sim.1482. [DOI] [PubMed] [Google Scholar]
- 26.IntHout J, Ioannidis JP, Borm GF. The Hartung-Knapp-Sidik-Jonkman method for random effects meta-analysis is straightforward and considerably outperforms the standard DerSimonian-Laird method. BMC Med Res Methodol. 2014;14:25. doi: 10.1186/1471-2288-14-25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Harrer, M., Pim Cuijpers, Furukawa Toshi A, and David D Ebert (2021) Doing Meta-Analysis With R: A Hands-On Guide. Boca Raton, FL; London: Chapman & Hall/CRC Press.1st ed.
- 28.Higgins JP, Thompson SG. Quantifying heterogeneity in a meta-analysis. Stat Med. 2002;21:1539–1558. doi: 10.1002/sim.1186. [DOI] [PubMed] [Google Scholar]
- 29.IntHout J, Ioannidis JP, Rovers MM, Goeman JJ. Plea for routinely presenting prediction intervals in meta-analysis. BMJ Open. 2016;6:e010247. doi: 10.1136/bmjopen-2015-010247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Viechtbauer W, Cheung MW. Outlier and influence diagnostics for meta-analysis. Res Synth Methods. 2010;1:112–125. doi: 10.1002/jrsm.11. [DOI] [PubMed] [Google Scholar]
- 31.R Core Team (2022). R: A language and environment for statistical computing. R Foundation for Statistical Computing, Vienna, Austria. https://www.R-project.org/
- 32.Schwarzer, G (2022) Meta‐Analysis in R. Systematic Reviews in Health Research: Meta‐Analysis in Context :510–534
- 33.Harrer, M., Cuijpers, P., Furukawa, T.A., & Ebert, D.D. (2021). Doing Meta-Analysis with R: A Hands-On Guide. Boca Raton, FL and London: Chapman & Hall/CRC Press. ISBN 978-0-367-61007-4. http://dmetar.protectlab.org
- 34.Ando K, Hamada K, Watanabe M, Ohkuma R, Shida M, Onoue R, Kubota Y, Matsui H, Ishiguro T, Hirasawa Y, et al. Plasma levels of soluble PD-L1 correlate With tumor regression in patients with lung and gastric cancer treated with immune checkpoint inhibitors. Anticancer Res. 2019;39:5195–5201. doi: 10.21873/anticanres.13716. [DOI] [PubMed] [Google Scholar]
- 35.Castello A, Rossi S, Toschi L, Mansi L, Lopci E. Soluble PD-L1 in NSCLC patients treated with checkpoint inhibitors and its correlation with metabolic parameters. Cancers (Basel) 2020 doi: 10.3390/cancers12061373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Chiarucci C, Cannito S, Daffina MG, Amato G, Giacobini G, Cutaia O, Lofiego MF, Fazio C, Giannarelli D, Danielli R, et al. Circulating levels of PD-L1 in mesothelioma patients from the NIBIT-MESO-1 study: correlation with survival. Cancers (Basel) 2020 doi: 10.3390/cancers12020361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Costantini A, Julie C, Dumenil C, Helias-Rodzewicz Z, Tisserand J, Dumoulin J, Giraud V, Labrune S, Chinet T, Emile JF, et al. Predictive role of plasmatic biomarkers in advanced non-small cell lung cancer treated by nivolumab. Oncoimmunology. 2018;7:e1452581. doi: 10.1080/2162402X.2018.1452581. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Incorvaia L, Fanale D, Badalamenti G, Porta C, Olive D, De Luca I, Brando C, Rizzo M, Messina C, Rediti M, et al. Baseline plasma levels of soluble PD-1, PD-L1, and BTN3A1 predict response to nivolumab treatment in patients with metastatic renal cell carcinoma: a step toward a biomarker for therapeutic decisions. Oncoimmunology. 2020;9:1832348. doi: 10.1080/2162402X.2020.1832348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Ji S, Chen H, Yang K, Zhang G, Mao B, Hu Y, Zhang H, Xu J. Peripheral cytokine levels as predictive biomarkers of benefit from immune checkpoint inhibitors in cancer therapy. Biomed Pharmacother. 2020;129:110457. doi: 10.1016/j.biopha.2020.110457. [DOI] [PubMed] [Google Scholar]
- 40.Mahoney KM, Ross-Macdonald P, Yuan L, Song L, Veras E, Wind-Rotolo M, McDermott DF, Stephen Hodi F, Choueiri TK, Freeman GJ. Soluble PD-L1 as an early marker of progressive disease on nivolumab. J Immunother Cancer. 2022 doi: 10.1136/jitc-2021-003527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Mazzaschi G, Minari R, Zecca A, Cavazzoni A, Ferri V, Mori C, Squadrilli A, Bordi P, Buti S, Bersanelli M, et al. Soluble PD-L1 and Circulating CD8+PD-1+ and NK cells enclose a prognostic and predictive immune effector score in immunotherapy treated NSCLC patients. Lung Cancer. 2020;148:1–11. doi: 10.1016/j.lungcan.2020.07.028. [DOI] [PubMed] [Google Scholar]
- 42.Tiako Meyo M, Jouinot A, Giroux-Leprieur E, Fabre E, Wislez M, Alifano M, Leroy K, Boudou-Rouquette P, Tlemsani C, Khoudour N, et al. Predictive value of soluble PD-1, PD-L1, VEGFA, CD40 ligand and CD44 for nivolumab therapy in advanced non-small cell lung cancer: a case-control study. Cancers (Basel) 2020 doi: 10.3390/cancers12020473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Murakami S, Shibaki R, Matsumoto Y, Yoshida T, Goto Y, Kanda S, Horinouchi H, Fujiwara Y, Yamamoto N, Ohe Y. Association between serum level soluble programmed cell death ligand 1 and prognosis in patients with non-small cell lung cancer treated with anti-PD-1 antibody. Thorac Cancer. 2020;11:3585–3595. doi: 10.1111/1759-7714.13721. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Okuma Y, Wakui H, Utsumi H, Sagawa Y, Hosomi Y, Kuwano K, Homma S. Soluble Programmed cell death ligand 1 as a novel biomarker for nivolumab therapy for non-small-cell lung cancer. Clin Lung Cancer. 2018;19:410–417. doi: 10.1016/j.cllc.2018.04.014. [DOI] [PubMed] [Google Scholar]
- 45.Oh SY, Kim S, Keam B, Kim TM, Kim DW, Heo DS. Soluble PD-L1 is a predictive and prognostic biomarker in advanced cancer patients who receive immune checkpoint blockade treatment. Sci Rep. 2021;11:19712. doi: 10.1038/s41598-021-99311-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Ugurel S, Schadendorf D, Horny K, Sucker A, Schramm S, Utikal J, Pfohler C, Herbst R, Schilling B, Blank C, et al. Elevated baseline serum PD-1 or PD-L1 predicts poor outcome of PD-1 inhibition therapy in metastatic melanoma. Ann Oncol. 2020;31:144–152. doi: 10.1016/j.annonc.2019.09.005. [DOI] [PubMed] [Google Scholar]
- 47.Yang Q, Chen M, Gu J, Niu K, Zhao X, Zheng L, Xu Z, Yu Y, Li F, Meng L, et al. Novel biomarkers of dynamic blood PD-L1 expression for immune checkpoint inhibitors in advanced non-small-cell lung cancer patients. Front Immunol. 2021;12:665133. doi: 10.3389/fimmu.2021.665133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Zhou J, Mahoney KM, Giobbie-Hurder A, Zhao F, Lee S, Liao X, Rodig S, Li J, Wu X, Butterfield LH, et al. Soluble PD-L1 as a biomarker in malignant melanoma treated with checkpoint blockade. Cancer Immunol Res. 2017;5:480–492. doi: 10.1158/2326-6066.CIR-16-0329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Huang P, Hu W, Zhu Y, Wu Y, Lin H. The Prognostic Value of Circulating Soluble Programmed Death Ligand-1 in Cancers: A Meta-Analysis. Front Oncol. 2020;10:626932. doi: 10.3389/fonc.2020.626932. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Liao G, Zhao Z, Qian Y, Ling X, Chen S, Li X, Kong FS. Prognostic Role of Soluble Programmed Death Ligand 1 in Non-Small Cell Lung Cancer: A Systematic Review and Meta-Analysis. Front Oncol. 2021;11:774131. doi: 10.3389/fonc.2021.774131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Music M, Iafolla MAJ, Ren AH, Soosaipillai A, Prassas I, Diamandis EP. Serum PD-1 Is Elevated after Pembrolizumab Treatment but Has No Predictive Value. Mol Cancer Ther. 2019;18:1844–1851. doi: 10.1158/1535-7163.MCT-19-0132. [DOI] [PubMed] [Google Scholar]
- 52.Wu B, Sternheim N, Agarwal P, Suchomel J, Vadhavkar S, Bruno R, Ballinger M, Bernaards CA, Chan P, Ruppel J, et al. Evaluation of atezolizumab immunogenicity: Clinical pharmacology (part 1) Clin Transl Sci. 2022;15:130–140. doi: 10.1111/cts.13127. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.