Abstract
Purpose
Suture anchors are commonly used to repair rotator cuff tendons in arthroscopy surgery, and several anchor materials have been created to maximize pull-out strength and minimize iatrogenic damage. We hypothesized that all-suture anchors have biomechanical properties equivalent to those of conventional anchors. Our purpose is to compare the biomechanical properties of different anchors used for rotator cuff repair.
Methods
The Embase, PubMed, Cochrane, and Scopus databases were searched for biomechanical studies on various suture anchors. The search keywords included rotator cuff tears and suture anchors, and two authors conducted study a selection, risk of bias assessment, and data extraction. The failure load, stiffness, and displacement were calculated using the mean differences with 95% confidence intervals (CIs). Failure modes were estimated using summary odds ratios with 95% CIs. The surface under the cumulative ranking curve was used for the relative ranking probabilities. A sensitivity analysis was performed by excluding studies using synthetic bones.
Results
The polyetheretherketone (PEEK) (p < 0.001) and all-suture anchors (p < 0.001) had higher failure loads than the biocomposite anchors, whereas no significant difference was observed in stiffness among the anchors. The all-suture (p = 0.006) and biocomposite anchors (p < 0.001) had displacements higher than the metal anchors. The relative ranking of the included anchors in failure loads and displacement changed in sensitivity analysis. The meta-analysis did not find significant differences, but the relative ranking probabilities suggested that all-suture anchor had a higher rate of anchor pull-out and a lower rate of eyelet or suture breakage. In contrast, the metal anchors were associated with a higher number of eyelet breakage episodes.
Conclusions
All-suture anchors showed significantly higher failure loads than the biocomposite anchors and similar cyclic displacements to the biocomposite and PEEK anchors. There were no significant differences in stiffness between all-suture and conventional suture anchors. The relative ranking of biomechanical properties changed in sensitivity analysis, suggesting the potential effect of bone marrow density.
Level of Evidence
Level IV.
Supplementary Information
The online version contains supplementary material available at 10.1186/s40634-023-00608-w.
Keywords: Rotator cuff injuries, Rotator cuff repair, Suture anchors, All-suture anchors, Biocomposite anchors, PEEK anchor, Metal anchors
Background
Arthroscopic rotator cuff repair has gained popularity for treating rotator cuff injuries, and suture anchors are commonly used to repair rotator cuff tendons in arthroscopic surgery [10]. Several anchor materials have been created to maximize pull-out strength and minimize iatrogenic damage. The anchor composition varied from metal to bioabsorbable to polyetheretherketone (PEEK) and all-suture anchors [7].
Metal anchors are simple to use and easy to visualize radiographically; however, they are associated with possible suture breakage because of sharp anchor eyelets, interference with magnetic resonance imaging, and difficulty in revision surgery [5]. Biocomposite anchors, composed of several materials such as polyglyconate, poly L-lactic acid (PLA), and calcium triphosphate, are associated with less suture damage but may cause inflammatory reactions and cyst formation [2]. The benefits of PEEK anchors include the fact that they appear to be radiolucent, non-absorbable, and non-metallic; however, their pull-out strengths are similar to those of metal anchors [6]. All-suture anchors use expanding intracortical sutures to fix the anchor, allowing for smaller drill holes with less bone disruption [25].
Several studies have compared the biomechanical properties of different materials of suture anchors in rotator cuff repair models [3, 23–25, 28, 31, 40]. However, there is a lack of systematic reviews and meta-analyses that draw a consensus on the optimal choice of suture anchors for rotator cuff repair in terms of biomechanical properties. Although the findings from biomechanical studies cannot be directly applied in clinical practice, precise suggestions from biomechanical studies would aid clinical decision-making in selecting suture anchors.
This network meta-analysis (NMA) aimed to compare the biomechanical properties of different suture anchors used in rotator cuff repair surgery. We hypothesized that all-suture anchors have biomechanical properties equivalent to those of conventional suture anchors.
Materials and methods
Search strategy and selection criteria
This NMA was performed following the preferred reporting items for systematic reviews and meta-analyses (PRISMA) extension guidelines [18] and was registered in PROSPERO (registration number: CRD42022337552). We conducted an electronic literature search using the following keywords and medical subject headings: population, rotator cuff tear, rotator cuff repair, rotator cuff injury, rotator cuff disease, and rotator cuff arthropathy. Interventions included all suture anchors, full suture anchors, soft anchors, suture anchors, Q-Fix, Iconix, JuggerKnot, and Y-knot for studies published from the inception of the databases (Embase, PubMed, Cochrane, and Scopus) to April 23, 2022. Additionally, we screened the reference lists of the extracted papers to identify potential studies that were not captured by the electronic database searches. The detailed syntax of the searches can be found in Appendix 3.2.
The inclusion criteria were as follows: (1) studies on rotator cuff repair models using human cadaveric or synthetic specimens; (2) studies that compared different suture anchor materials; (3) randomized controlled or comparative studies; (4) studies published in English; and (5) studies that used cadaver or osteoporotic bone models. The intervention arms included four suture anchor types: all-suture, biocomposite suture, PEEK, and metal anchors.
The exclusion criteria were as follows: (1) non-biomechanical studies, single-arm biomechanical studies, single-arm clinical studies, case series or reports, conference abstracts, or comments on other studies; (2) unknown target outcomes of interest; (3) rotator cuff repair models using pediatric, pathological, and animal specimens; and (4) comparisons without different suture anchor materials. In cases of duplicated data (e.g., different articles based on similar sources of participants), we included studies with more biomechanical outcomes.
Data extraction and quality assessment
Two authors (Y-S Y and C-A S) initially screened titles and abstracts based on the inclusion and exclusion criteria and then independently evaluated the risk of bias for each domain described in the Cochrane risk-of-bias tool [16]. The tool includes five domains: the randomization process, intended intervention deviations, missing outcome data, outcome measurement, and reported result selection. Each study was identified as “high-risk,” “some concerns,” or “low-risk.” When a consensus could not be reached, a third author (C-K H) resolved any disagreements. The Quality Appraisal for Cadaveric Studies (QUACS) scale was used to assess the included studies [39].
One author (C-K H) extracted the following data and information: (1) first author’s name and publication year; (2) study nation or area; (3) study design; (4) specimen characteristics; (5) intervention and control protocols; and (6) primary biomechanical outcome measurement, including load-to-failure, stiffness, displacement, and failure modes.
Parameter selection
When several stiffness and cyclic displacement values were estimated in a study, the calculated load for stiffness and cyclic displacement (from 10 to 100 N) and the cycle for displacement were chosen for cyclic-to-failure as priorities, followed by the most common cycles (100 and 1000 cycles). These loads and cycles reflected the stiffness and displacement values most frequently measured in other biomechanical studies. Displacements from different studies with variations were calculated as a single outcome, “displacement.” All authors validated the accuracy of the extracted data. When necessary, the authors of the original article were contacted to retrieve any missing information or additional data.
Data synthesis and analysis
All statistical analyses were performed using the Stata 15.0 software (StataCorp. 2017. Stata Statistical Software: Release 15. College Station, TX: StataCorp LLC.). As only a few studies were included, various diameters and shapes of suture anchors were combined to calculate the results. For load-to-failure, stiffness, and displacement, mean differences (MDs) were calculated at 95% confidence intervals (CIs). For failure-mode data, we estimated summary odds ratios (ORs) with 95% CIs. An OR value of < 1 indicated a higher incidence of suture anchor failure. A pairwise meta-analysis was conducted for direct comparisons between trials, and an NMA was carried out to combine direct and indirect evidence [37]. The heterogeneity of the sample size and intervention protocols was evaluated using the estimated standard deviation of the effects across these studies. Statistical significance was defined as a two-tailed p-value < 0.05.
The relative ranking probabilities for the interventions and surface under the cumulative ranking curve (SUCRA) were calculated. The larger the SUCRA value [33], the higher the rank of the intervention [9, 29].
Publication bias in the NMA was examined using Egger regression. The potential inconsistency between the direct and indirect comparisons of all studies was determined using the loop-specific approach, local inconsistency with the node-splitting method, and the global inconsistency among the entire NMA with the design-by-treatment model [13, 38]. Finally, a sensitivity analysis was performed after excluding trials conducted using synthetic bone models. We also assessed the presence of small study effects on each outcome using a comparison-adjusted funnel plot. The funnel plot asymmetry indicated a small study effect bias [12, 17].
Results
Study selection, description, and quality
As shown in the PRISMA flow diagram in Fig. 1, 1601 studies were identified after searching the databases and other sources. We finally retrieved seven studies included in the NMA [3, 23–25, 28, 31, 40]. These studies included > 60 sawbones, 98 humeri, and 291 anchors. All seven studies compared load-to-failure, three compared stiffness [24, 25, 31], five compared anchor displacement [23–25, 28, 31], and six compared the incidence of failure modes [3, 23–25][28, 40]. The characteristics of all studies and specimens are summarized in Tables 1 and 2.
Fig. 1.
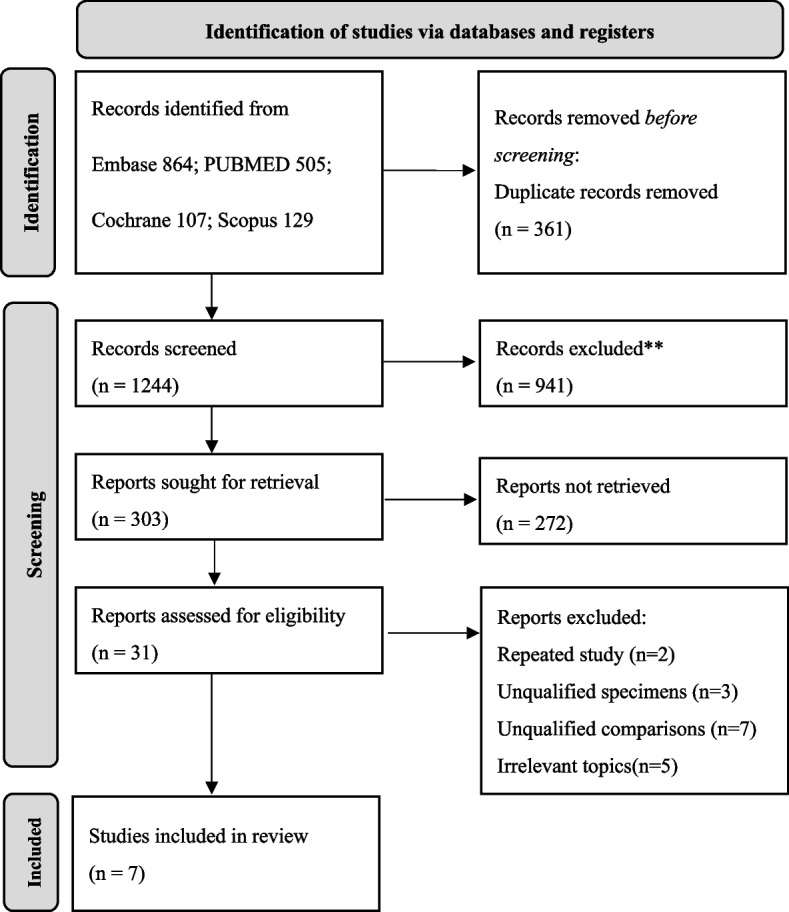
PRISMA Flow diagram for systematic reviews
Table 1.
Descriptive characteristics of the included studies
| Study and Year | Nation | Specimen, n | Age | Gender | Bone Mineral Density | Insertion Angle | Intervention | Outcomes | Level of Evidence | Risk of Bias |
|---|---|---|---|---|---|---|---|---|---|---|
| Yamauchi et al., 2022 [40] | Japan | Sawbone model, 160 | N/A | N/A |
1. 10-pounds/cubic foot (160 mg/cm3) 2. 5-pounds/cubic foot (80 mg/cm3) |
90 degrees | Corkscrew FT Ti 4.5 mm, HEALICOIL PK 4.5 mm, Corkscrew Bio 4.75 mm | LTF, Failure mode | IV | High risk |
| Rosso et al., 2020 [31] | Switzerland | Sawbone model, 60 | N/A | N/A |
1. Physiological group: 120 mg/cm3 2. Osteoporotic group: 90 mg/cm3 |
45 degrees | TwinFix Ti 4.5 mm, Healix BR 4.5 mm, Iconix 2.3 mm | LTF, STF, DIS | IV | Low risk |
| Ntalos et al., 2019 [24] | Germany | Human humerus, 10 | 50-73y | N/A |
1. All-suture anchor: 126 ± 25 mg/cm3 2. Conventional anchor: 127 ± 30 mg/cm3 |
90 degrees |
Y-knot 2.8 mm, CrossFT 4.5 mm |
LTF, STF, DIS, Failure mode | IV | Some concerns |
| Ntalos et al., 2019 [25] | Germany | Human humerus, 36 |
22-76y (61.4 ± 11y) |
N/A |
1. 126 ± 18 mg /cm3 2. 126 ± 26 mg /cm3 3. 127 ± 16 mg /cm3 |
45, 90, 110 degrees |
Y-knot 2.8 mm, CrossFT 4.5 mm |
LTF, STF, DIS, Failure mode | IV | Low risk |
| Nagra et al., 2017 [23] | United Kingdom | Human humerus, 24 | 58-96y | 16 M, 8F | N/A | N/A |
Y-knot 2.8 mm, TwinFix ultra PK 6.5 mm |
LTF, DIS, Failure mode | IV | Some concerns |
| Barber et al., 2010 [3] | United States | Human humerus, 16 | 70-96y | 7 M, 1F | N/A | N/A |
Bio-Corkscrew FT 5.5 mm, CrossFT PK 5.5 mm |
LTF, DIS, Failure mode | IV | Some concerns |
| Pietschmann et al., 2009 [28] | Germany | Human humerus, 12 | 27-93y | 8 M, 4F |
1. Non-osteopenic: 109 ± 26 mg/cm3 2. Osteoporotic bones: 41 ± 20 g/cm3 |
45 degrees | SPIRALOK BC 5.0 mm, Super Revo 5.0 mm | LTF, DIS, Failure mode | IV | Some concerns |
LEGEND: Characteristics included author names, publication year, sources of country, specimen type, specimen numbers, age, gender and bone mineral densities of human cadaver, anchor insertion anchor, interventions, outcomes, level of evidence and risk of bias of each study. LTF Load to failure, STF Stiffness, DIS Displacement
Table 2.
Descriptive characteristics of the included suture anchors
| Anchor Name | Study | Material | Suture | Loaded | Diameter | n | |
|---|---|---|---|---|---|---|---|
| All-suture anchor | Iconix | Rosso et al | Braided UHMWP | No. 2 Force Fiber | Single | 2.3 mm | 10 |
| Y-knot |
Ntalos et al Ntalos et al Nagra et al |
Braided UHMWP | No. 2 HiFi | Single | 2.8 mm | 24 | |
| Biocomposite suture anchor | Bio Corkscrew | Yamauchi et al | Poly-L-lactic acid | No. 2 FiberWire | Single | 4.75 mm | 5 |
| Bio Corkscrew FT | Barber et al | Poly-L-lactic acid | No. 2 FiberWire | Single | 5.5 mm | 12 | |
| Healix BR | Rosso et al | 30% b-TCP/ 70% PLGA | No. 2 Orthocord | Single | 4.5 mm | 10 | |
| SPIRALOK BC | Pietschmann et al | Poly-L-lactic acid | USP 2 | Single | 5.0 mm | 6 | |
| PEEK suture anchor | CrossFT PK |
Ntalos et al Ntalos et al |
PEEK | No. 2 HiFi | Single | 4.5 mm | 19 |
| CrossFT PK | Barber et al | PEEK | No. 2 HiFi | Single | 5.5 mm | 12 | |
| HEALICOIL PK | Yamauchi et al | PEEK | No. 2 Ultrabraid | Single | 4.5 mm | 5 | |
| TwinFix ultra PK | Nagra et al | PEEK | No. 2 white/Cobraid blue | Single | 6.5 mm | 4 | |
| Metal suture anchor | TwinFix Ti | Rosso et al | Titanium | No. 2 white/Cobraid blue | Single | 4.5 mm | 10 |
| Corkscrew FT | Yamauchi et al | Titanium | No. 2 FiberWire | Single | 4.5 mm | 5 | |
| Super Revo | Pietschmann et al | Titanium | No. 2 HiFi | Single | 5.0 mm | 6 |
LEGEND: Characteristics included each anchor name, study resource, anchor material, suture material, repair construction (all single loaded), anchor diameter and numbers. UHMWP Ultra-high-molecular-weight polyethylene, PEEK Polyetheretherketone, β-TCP β-tricalcium phosphate, PLGA Poly lactic-co-glycolic acid
Network meta-analysis
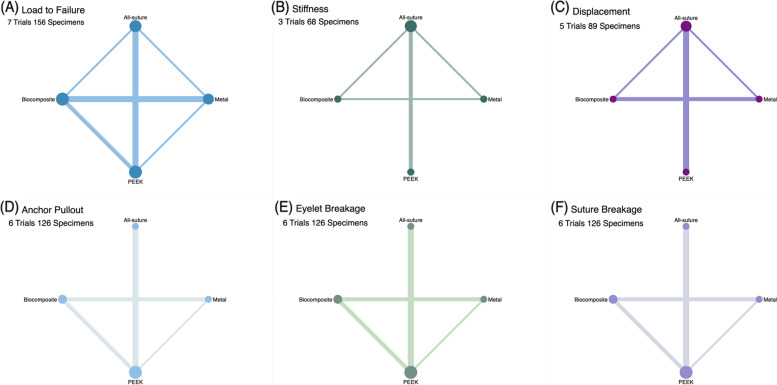
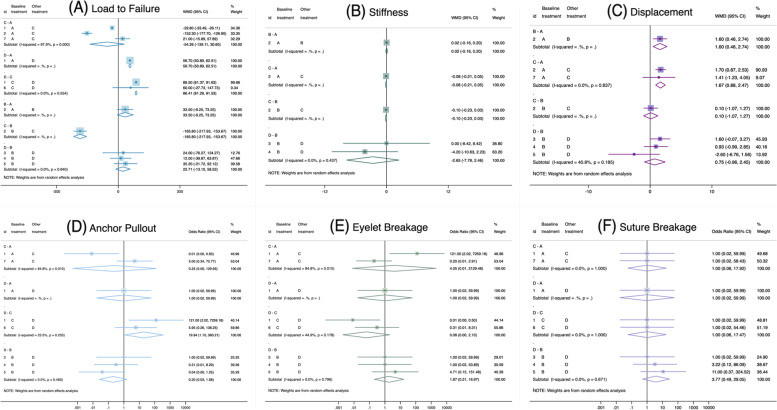
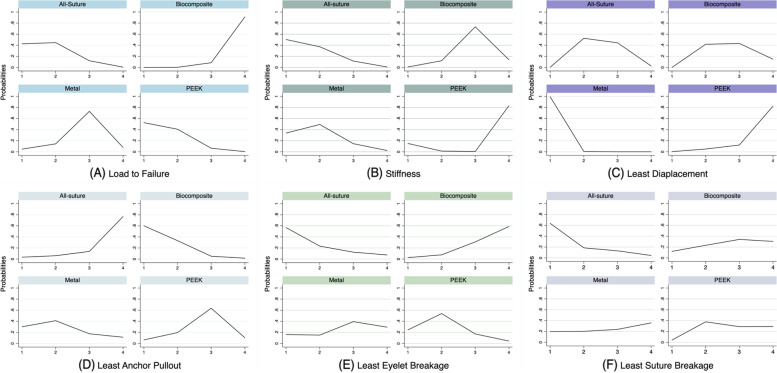
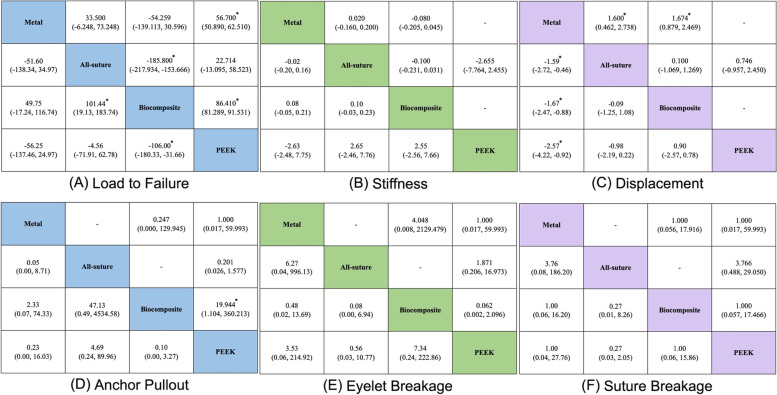
The network geometry for each outcome is shown in Fig. 2. The forest plots and rank probabilities are shown in Figs. 3 and 4. The league table and pairwise plots of MD and OR with 95% CIs are shown in Fig. 5.
Fig. 2.
Summary of Network Geometry of Each Biomechanical Property. The size of straight lines is proportional to the number of studies, and the size of round nodes is proportional to the number of interventions. Direct and indirect evidence were combined for multiple treatment comparisons. A All included studies reported failure load values; therefore, all anchors had connections with each other. B Three studies had stiffness values, and (C) five studies had displacement values and a lack of direct connections from PEEK to the biocomposite and metal anchors. (D–F) Six studies reported failure mode rates and a lack of direct connections from all-suture anchors to biocomposites and metal anchors
Fig. 3.
Forest Plots of Each Biomechanical Property. Forest plots demonstrate (A–C) weighted mean differences and (D–F) odds ratios
Fig. 4.
Probability Rankings of Each Biomechanical Property. In (A) and (B), higher values indicate a superior ranking. C-F smaller values indicate superior ranking
Fig. 5.
League Table and Pairwise of Each Biomechanical Property. The results of the network meta-analysis are presented in the lower-left half, whereas those of the pairwise meta-analysis are presented in the upper-right half. In (A-C), the weighted mean differences with 95% confidence intervals (CIs) are presented. If the 95% CIs crossed 0, the differences are not statistically significant. In (D-F), odds ratios (ORs) with 95% CIs are presented, and the column-defining treatment is favored if the odds ratio is < 1. If the 95% CIs crossed 1, there are no significant difference between groups. The stars marked in the figure refer to significant differences
Load to failure
In total, 128 anchors were evaluated. The PEEK anchor showed significantly higher strength than the metal and biocomposite anchors, while the biocomposite anchor showed significantly lower strength than the all-suture anchor. The PEEK anchor (SUCRA: 81.9%) ranked first ahead of the all-suture anchor (76.5%), followed by the metal anchor (38.7%) and the biocomposite anchor (3.0%) (Fig. 5A). In the sensitivity analysis, the PEEK anchor ranked first (SUCRA: 91.5%), followed by the all-suture (58.0%), biocomposite (39.7%), and metal (10.8%) anchors. However, no significant difference was observed in the sensitivity analysis.
Stiffness
A total of 68 anchors were evaluated, and no significant differences in stiffness were observed. The all-suture and metal anchors ranked first (SUCRA: 79.1% and 71.5%, respectively), followed by the biocomposite (33.3%) and PEEK (16.1%) anchors (Fig. 5B). However, metal anchors (83.6%) ranked much higher than all-suture anchors (16.4%) in the sensitivity analysis, in which only cadaveric bone models were included.
Displacement
In total, 89 anchors were evaluated. The all-suture and biocomposite anchors exhibited significantly greater displacements than the metal anchor. The metal anchor ranked first in terms of the least anchor displacement (SUCRA: 99.8%), followed by the all-suture (50.2%), biocomposite (42.3%), and PEEK (7.7%) anchors (Fig. 5C). In the sensitivity analysis, the all-suture anchor ranked first (66.3%) in displacement with the lowest values, followed by the metal (61.0%), biocomposite, and PEEK (35.5%; 37.3%) anchors. However, no significant difference was observed in the sensitivity analysis.
Failure mode
A total of 98 anchors were evaluated. The PEEK anchor was significantly more likely to be pulled out than the biocomposite anchor. No other significant differences were observed in the three failure modes among the different suture anchors. The all-suture anchors were most probably pulled out, followed by the PEEK, metal, and biocomposite anchors (Fig. 5D). The biocomposite anchors were more likely to cause the eyelet breakage than the other three suture anchors (Fig. 5E). Finally, suture breakage was less likely to occur in all suture anchors (Fig. 5F). However, the differences in three failure modes among four anchors did not reach statistical significances. In the sensitivity analysis, eyelet or suture failure was the least likely to occur with the all-suture anchor. The metal anchor still had the highest possibility of eyelet breakage and the least anchor pull-out.
Publication Bias, Inconsistency, and Heterogeneity
The funnel and Egger regression plots were mostly symmetric. Significant global and local inconsistencies were observed in the design-by-treatment interaction, side-splitting inconsistency, and loop-inconsistency models. (Additional file: Appendices 10, 11).
Risk of Bias, CINeMA Assessment, and the QUACS Scale
The overall bias was low risk, and some concerns are listed in an additional file (Appendix 7). The confidence ratings of CINEMA were generally very low (Additional file: Appendix 13). The QUACS ranged from 8–10 out of 13 points (Additional file: Appendix 15).
Discussion
The most significant finding of this study was that PEEK anchors had the greatest ultimate failure loads, whereas biocomposite anchors had the least; all-suture anchors had the highest stiffness, whereas PEEK anchors had the least. Regarding the displacement ranking, the metal anchor had the least displacement, followed by the all-suture anchor. We also found that the ranking of the anchors included in the ultimate failure load and displacement changed in the sensitivity analysis, which excluded synthetic bone models and included osteoporotic cadaveric models alone.
An ideal suture anchor should have a high failure load, high stiffness, and small cyclic displacement. Theoretically, a suture anchor with a high failure load reduces the possibility of surgical failure. The structural design and materials of anchors may affect the ultimate failure load [4, 5, 8, 19]. PEEK anchors, made of crystalline thermoplastic, are sufficiently solid to build a stable anchor-bone construct [8]. Biocomposite anchors made of PLA or calcium triphosphate can be absorbed into the bone, raising concerns regarding the preservation of the pull-out strength [4, 5]. Because only small drill tunnels are required for all-suture anchors, their surface area-to-anchor volume ratio is significantly higher than that of conventional anchors, providing sufficient stability without extensive bone damage [19].
In addition to the ultimate failure load, stiffness is an important feature when evaluating the biomechanical properties of suture anchors because it represents the capability of a suture anchor to stabilize the repair structure [23]. A repaired structure with greater stiffness improves surgical success and shortens recovery periods [23]. This NMA compared the stiffness of the constructs in rotator cuff repair models and revealed that all-suture anchors had comparable stiffness to other suture anchors. Based on the ultimate failure load and stiffness findings, an all-suture anchor can be an attractive option owing to its superior biomechanical properties. However, care should be taken when interpreting the results, as the sensitivity analysis indicated a high risk of bias because of the small number of studies included.
All-suture anchors have shown a clinical performance equivalent to that of hard-body anchors for rotator cuff repair [27]. Van der Bracht et al. reported a series of 20 patients who underwent double-row cuff repairs using all-suture anchors for both the medial and lateral rows [36]. They found that only one patient sustained a retear and that there was no difference in the contralateral supraspinatus strength at mean postoperative 1.58 years [36]. Dhinsa et al. analyzed 31 patients who underwent double-row repair and reported one retear at a mean follow-up of 10.2 months with a mean Constant score of 77.1 [11]. Ro et al. retrospectively compared 213 patients who underwent single-row rotator cuff repair using all-suture (n = 137), bioabsorbable (n = 36) or PEEK anchors (n = 40). They reported that 71% of the repaired tendons were healed irrespective of the anchor type [30]. Since promising clinical outcomes have been reported [11, 30, 36], the superior biomechanical properties of the current NMA provide further support for using all-suture anchors in rotator cuff repair.
Anchor characteristics are closely related to failure modes [8, 15, 22, 26]. This study showed that all-suture anchors were much more likely to fail owing to anchor pull-out, biocomposite anchors had more eyelet breakage, and that metal anchors easily caused suture breakage. The edge of the metal anchor is sharp enough to easily cut the suture, leading to frequent suture breakage [15, 22, 26]. The eyelet design of biocomposite anchors commonly uses a distal crossbar structurally weaker than the screw threads, resulting in crossbar breaking as the predominant anchor failure type [8]. PEEK anchors are chemically resistant without sharp edges, decreasing suture or eyelet breakage rates [8]. Thus, the PEEK anchors are more likely to be pulled out by the entire repair structure. Instead of the eyelet or suture breakage, anchor pull-out is the most common failure mode for all-suture anchors.
Bone mineral density affects the healing of the rotator cuff tendon [1] and suture anchor fixation strength [14, 21, 32, 34]. Placing anchors at areas with good cortical density provides higher resistance to pulling strength, thereby preventing suture anchor loosening and ensuring successful repair [14, 34]. Although previous studies have reported decreased load-to-failure in specimens with lower bone mineral density [20, 34, 35], there is a lack of comparison of the fixation strengths of different anchor types with respect to bone marrow density. This study conducted a sensitivity analysis, representing findings obtained from osteoporotic cadaveric models alone. The results showed that the ranking of the included anchors in terms of ultimate failure load and displacement changed after sensitivity analysis, suggesting that the biomechanical performance of different suture anchors is affected by bone marrow density to varying degrees. Further studies must analyze the effect of bone marrow density on the fixation strength of different anchor types.
Limitations
This study had several limitations. First, some studies that used human cadavers and synthetic bone models were included in the NMA. Because the number of human cadaver studies that met the inclusion criteria was limited [3, 23–25, 28], we also included studies that used synthetic bone models [31, 40]. The inconsistent bone mineral densities observed in different studies may have affected the results. Although this study conducted a sensitivity analysis, thereby providing results from cadaveric studies only, diversity in bone mineral density was observed in these studies, potentially influencing the study results. The detailed mean and standard deviations of bone mineral density in each groups can be found in Appendix 6.4. Second, the anchors were classified according to the materials of which they were made, and their size and shape could not be controlled. Thus, inter-anchor variability within the same group may have caused these inconsistencies. Finally, the absorbability of the suture anchors was not considered in the time-zero biomechanical studies. Therefore, care should be taken when applying our biomechanical findings to clinical practice, as fixation strength may change after surgery. Despite these limitations, the NMA compared the most common biomechanical outcomes of different suture anchors, which may predict the possible clinical outcomes of patients.
Conclusions
All-suture anchors showed significantly higher failure loads than the biocomposite anchors and similar cyclic displacements to the biocomposite and PEEK anchors. There were no significant differences in stiffness between all-suture and conventional suture anchors. The relative ranking of biomechanical properties changed in sensitivity analysis, suggesting the potential effect of bone marrow density.
Supplementary Information
Acknowledgements
We thank Skeleton Materials and Bio-compatibility Core Lab, Research Center of Clinical Medicine, National Cheng Kung University Hospital for the assistance of this project.
Informed consent
Not applicable.
Abbreviations
- NMA
Network meta-analysis
- MD
Mean difference
- CI
Confidence interval
- OR
Odds ratio
- SUCRA
The surface under the cumulative ranking curve
- PEEK
Polyetheretherketone
- PLA
Poly L-lactic acid
Authors’ contributions
Y-S Y and T-T H conducted the systematic review and collected the data. C-A S and C-J F contributed to the methodology. W-R S contributed to the concept. Y-S Y, C-A S, and C-K H analyzed the data. Y-S Y draft the manuscript. K-L H, F–C K, and C-K H revised the manuscript. C-K H supervised the study. The author(s) read and approved the final manuscript.
Funding
The study was supported by research grants from the Ministry of Science and Technology, Taiwan (MOST 110–2314-B-006–021) and National Cheng Kung University Hospital, Tainan, Taiwan (NCKUH-11204010).
Declarations
Ethics approval and consent to participate
Not applicable.
Competing interests
The authors have no relevant financial or non-financial interests to disclose.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Abtahi AM, Granger EK, Tashjian RZ. Factors affecting healing after arthroscopic rotator cuff repair. World J Orthop. 2015;6(2):211–220. doi: 10.5312/wjo.v6.i2.211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Barber FA, Dockery WD, Cowden CH., 3rd The degradation outcome of biocomposite suture anchors made from poly L-lactide-co-glycolide and β-tricalcium phosphate. Arthroscopy. 2013;29(11):1834–1839. doi: 10.1016/j.arthro.2013.08.004. [DOI] [PubMed] [Google Scholar]
- 3.Barber FA, Hapa O, Bynum JA. Comparative testing by cyclic loading of rotator cuff suture anchors containing multiple high-strength sutures. Arthroscopy. 2010;26(9 Suppl):S134–S141. doi: 10.1016/j.arthro.2010.03.007. [DOI] [PubMed] [Google Scholar]
- 4.Barber FA, Herbert MA. All-Suture Anchors: Biomechanical Analysis of Pull-out Strength, Displacement, and Failure Mode. Arthroscopy. 2017;33(6):1113–1121. doi: 10.1016/j.arthro.2016.09.031. [DOI] [PubMed] [Google Scholar]
- 5.Barber FA, Herbert MA. Cyclic loading biomechanical analysis of the pull-out strengths of rotator cuff and glenoid anchors: 2013 update. Arthroscopy. 2013;29(5):832–844. doi: 10.1016/j.arthro.2013.01.028. [DOI] [PubMed] [Google Scholar]
- 6.Barber FA, Herbert MA, Beavis RC, Barrera Oro F. Suture anchor materials, eyelets, and designs: update 2008. Arthroscopy. 2008;24(8):859–867. doi: 10.1016/j.arthro.2008.03.006. [DOI] [PubMed] [Google Scholar]
- 7.Barber FA, Herbert MA, Coons DA, Boothby MH. Sutures and suture anchors–update 2006. Arthroscopy. 2006;22(10):1063.e1–1063.e10639. doi: 10.1016/j.arthro.2006.04.106. [DOI] [PubMed] [Google Scholar]
- 8.Barber FA, Herbert MA, Hapa O, Rapley JH, Barber CA, Bynum JA, Hrnack SA. Biomechanical analysis of pull-out strengths of rotator cuff and glenoid anchors: 2011 update. Arthroscopy. 2011;27(7):895–905. doi: 10.1016/j.arthro.2011.02.016. [DOI] [PubMed] [Google Scholar]
- 9.Bax L, Ikeda N, Fukui N, Yaju Y, Tsuruta H, Moons KG. More than numbers: the power of graphs in meta-analysis. Am J Epidemiol. 2009;169(2):249–255. doi: 10.1093/aje/kwn340. [DOI] [PubMed] [Google Scholar]
- 10.Burkhart SS. The Burden of Craft in Arthroscopic Rotator Cuff Repair: Where Have We Been and Where We Are Going. Am J Orthop (Belle Mead NJ) 2015;44(8):353–358. [PubMed] [Google Scholar]
- 11.Dhinsa BS, Bhamra JS, Aramberri-Gutierrez M, Kochhar T. Mid-term clinical outcome following rotator cuff repair using all-suture anchors. J Clin Orthop Trauma. 2019;10(2):241–243. doi: 10.1016/j.jcot.2018.02.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Dias S, Welton NJ, Caldwell DM, Ades AE. Checking consistency in mixed treatment comparison meta-analysis. Stat Med. 2010;29(7–8):932–944. doi: 10.1002/sim.3767. [DOI] [PubMed] [Google Scholar]
- 13.Dias S, Welton NJ, Sutton AJ, Caldwell DM, Lu G, Ades AE. Evidence synthesis for decision making 4: inconsistency in networks of evidence based on randomized controlled trials. Med Decis Making. 2013;33(5):641–656. doi: 10.1177/0272989X12455847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ergün S, Akgün U, Barber FA, Karahan M. The Clinical and Biomechanical Performance of All-Suture Anchors: A Systematic Review. Arthrosc Sports Med Rehabil. 2020;2(3):e263–e275. doi: 10.1016/j.asmr.2020.02.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Goschka AM, Hafer JS, Reynolds KA, Aberle NS, 2nd, Baldini TH, Hawkins MJ, McCarty EC. Biomechanical comparison of traditional anchors to all-suture anchors in a double-row rotator cuff repair cadaver model. Clin Biomech (Bristol, Avon) 2015;30(8):808–813. doi: 10.1016/j.clinbiomech.2015.06.009. [DOI] [PubMed] [Google Scholar]
- 16.Higgins JPT, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, Welch VA [2017]. Cochrane Handbook for Systematic Reviews of Interventions version 5.2 (updated February 2017). Cochrane, 2017. Available from www.training.cochrane.org/handbook.
- 17.Higgins JP, Jackson D, Barrett JK, Lu G, Ades AE, White IR. Consistency and inconsistency in network meta-analysis: concepts and models for multi-arm studies. Res Synth methods. 2012;3(2):98–110. doi: 10.1002/jrsm.1044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hutton B, Salanti G, Caldwell DM, Chaimani A, Schmid CH, Cameron C, Ioannidis JP, Straus S, Thorlund K, Jansen JP, Mulrow C, Catalá-López F, Gøtzsche PC, Dickersin K, Boutron I, Altman DG, Moher D. The PRISMA extension statement for reporting of systematic reviews incorporating network meta-analyses of health care interventions: checklist and explanations. Ann Intern Med. 2015;162(11):777–784. doi: 10.7326/M14-2385. [DOI] [PubMed] [Google Scholar]
- 19.Jost, P. W., Khair, M. M., Chen, D. X., Wright, T. M., Kelly, A. M., & Rodeo, S. A. [2012]. Suture number determines strength of rotator cuff repair. The Journal of bone and joint surgery. American volume, 94(14), e100. 10.2106/JBJS.K.00117 [DOI] [PubMed]
- 20.Kirchhoff C, Braunstein V, Milz S, Sprecher CM, Fischer F, Tami A, Ahrens P, Imhoff AB, Hinterwimmer S. Assessment of bone quality within the tuberosities of the osteoporotic humeral head: relevance for anchor positioning in rotator cuff repair. Am J Sports Med. 2010;38(3):564–569. doi: 10.1177/0363546509354989. [DOI] [PubMed] [Google Scholar]
- 21.Kirchhoff C, Braunstein V, Milz S, Sprecher CM, Kirchhoff S, Graw M, Imhoff AB, Hinterwimmer S. Age and gender as determinants of the bone quality of the greater tuberosity: a HR-pQCT cadaver study. BMC Musculoskelet Disord. 2012;13:221. doi: 10.1186/1471-2474-13-221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Meyer DC, Nyffeler RW, Fucentese SF, Gerber C. Failure of suture material at suture anchor eyelets. Arthroscopy. 2002;18(9):1013–1019. doi: 10.1053/jars.2002.36115. [DOI] [PubMed] [Google Scholar]
- 23.Nagra NS, Zargar N, Smith RD, Carr AJ. Mechanical properties of all-suture anchors for rotator cuff repair. Bone & joint research. 2017;6(2):82–89. doi: 10.1302/2046-3758.62.BJR-2016-0225.R1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ntalos D, Huber G, Sellenschloh K, Briem D, Püschel K, Morlock MM, Frosch KH, Thiesen DM, Klatte TO. Biomechanical analysis of conventional anchor revision after all-suture anchor pull-out: a human cadaveric shoulder model. J Shoulder Elbow Surg. 2019;28(12):2433–2437. doi: 10.1016/j.jse.2019.04.053. [DOI] [PubMed] [Google Scholar]
- 25.Ntalos, D., Sellenschloh, K., Huber, G., Briem, D., Püschel, K., Morlock, M. M., Frosch, K. H., Fensky, F., & Klatte, T. O. [2019]. Conventional rotator cuff versus all-suture anchors-A biomechanical study focusing on the insertion angle in an unlimited cyclic model. PloS one, 14(11), e0225648. 10.1371/journal.pone.0225648 [DOI] [PMC free article] [PubMed]
- 26.Ozbaydar M, Elhassan B, Warner JJ. The use of anchors in shoulder surgery: a shift from metallic to bioabsorbable anchors. Arthroscopy. 2007;23(10):1124–1126. doi: 10.1016/j.arthro.2007.05.011. [DOI] [PubMed] [Google Scholar]
- 27.Pak, T., Menendez, M. E., Hwang, S., Ardebol, J., Ghayyad, K., & Denard, P. J. [2023]. Soft Anchors for Rotator Cuff Repair: A Review. JBJS reviews, 11(2), 10.2106/JBJS.RVW.22.00207 [DOI] [PubMed]
- 28.Pietschmann MF, Fröhlich V, Ficklscherer A, Gülecyüz MF, Wegener B, Jansson V, Müller PE. Suture anchor fixation strength in osteopenic versus non-osteopenic bone for rotator cuff repair. Arch Orthop Trauma Surg. 2009;129(3):373–379. doi: 10.1007/s00402-008-0689-4. [DOI] [PubMed] [Google Scholar]
- 29.Riley, R. D., Jackson, D., Salanti, G., Burke, D. L., Price, M., Kirkham, J., & White, I. R. [2017]. Multivariate and network meta-analysis of multiple outcomes and multiple treatments: rationale, concepts, and examples. BMJ (Clinical research ed.), 358, j3932. 10.1136/bmj.j3932 [DOI] [PMC free article] [PubMed]
- 30.Ro K, Pancholi S, Son HS, Rhee YG. Perianchor Cyst Formation After Arthroscopic Rotator Cuff Repair Using All-Suture-Type, Bioabsorbable-Type, and PEEK-Type Anchors. Arthroscopy. 2019;35(8):2284–2292. doi: 10.1016/j.arthro.2019.03.032. [DOI] [PubMed] [Google Scholar]
- 31.Rosso C, Weber T, Dietschy A, de Wild M, Müller S. Three anchor concepts for rotator cuff repair in standardized physiological and osteoporotic bone: a biomechanical study. J Shoulder Elbow Surg. 2020;29(2):e52–e59. doi: 10.1016/j.jse.2019.07.032. [DOI] [PubMed] [Google Scholar]
- 32.Sakamoto Y, Kido A, Inoue K, Sakurai G, Hashiuchi T, Munemoto M, Tanaka Y. In vivo microstructural analysis of the humeral greater tuberosity in patients with rotator cuff tears using multidetector row computed tomography. BMC Musculoskelet Disord. 2014;15:351. doi: 10.1186/1471-2474-15-351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Salanti G, Ades AE, Ioannidis JP. Graphical methods and numerical summaries for presenting results from multiple-treatment meta-analysis: an overview and tutorial. J Clin Epidemiol. 2011;64(2):163–171. doi: 10.1016/j.jclinepi.2010.03.016. [DOI] [PubMed] [Google Scholar]
- 34.Tingart MJ, Apreleva M, Lehtinen J, Zurakowski D, Warner JJ. Anchor design and bone mineral density affect the pull-out strength of suture anchors in rotator cuff repair: which anchors are best to use in patients with low bone quality? Am J Sports Med. 2004;32(6):1466–1473. doi: 10.1177/0363546503262644. [DOI] [PubMed] [Google Scholar]
- 35.Tingart, M. J., Apreleva, M., Zurakowski, D., & Warner, J. J. [2003]. Pull-out strength of suture anchors used in rotator cuff repair. The Journal of bone and joint surgery. American volume, 85(11), 2190–2198. 10.2106/00004623-200311000-00021 [DOI] [PubMed]
- 36.Van der Bracht H, Van den Langenbergh T, Pouillon M, Verhasselt S, Verniers P, Stoffelen D. Rotator cuff repair with all-suture anchors: a midterm magnetic resonance imaging evaluation of repair integrity and cyst formation. J Shoulder Elbow Surg. 2018;27(11):2006–2012. doi: 10.1016/j.jse.2018.03.006. [DOI] [PubMed] [Google Scholar]
- 37.White IR. Network meta-analysis. The Stata Journal: Promoting Communications on Statistics and Stata. 2015;15(4):951–985. doi: 10.1177/1536867x1501500403. [DOI] [Google Scholar]
- 38.White IR, Barrett JK, Jackson D, Higgins JP. Consistency and inconsistency in network meta-analysis: model estimation using multivariate meta-regression. Res Synth Methods. 2012;3(2):111–125. doi: 10.1002/jrsm.1045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Wilke J, Krause F, Niederer D, Engeroff T, Nürnberger F, Vogt L, Banzer W. Appraising the methodological quality of cadaveric studies: validation of the QUACS scale. J Anat. 2015;226(5):440–446. doi: 10.1111/joa.12292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Yamauchi S, Tsukada H, Sasaki E, Sasaki S, Kimura Y, Yamamoto Y, Tsuda E, Ishibashi Y. Biomechanical analysis of bioabsorbable suture anchors for rotator cuff repair using osteoporotic and normal bone models. J Orthop Sci. 2022;27(1):115–121. doi: 10.1016/j.jos.2020.11.017. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.