Abstract
Background and aims
Gout, the most prevalent inflammatory arthritis, has undesirable effects on the quality of life. Omega-3 polyunsaturated fatty acids (n-3 PUFA) has a strong link with anti-inflammatory impacts. However, whether the harmful effects of seafood in relation to gout may vary owing to different levels of n-3 PUFA in seafood is still unclear. It was the goal of this study to examine the relationship between n-3 PUFA poor/rich seafood consumption and gout.
Methods
Between 2007 and 2016, five NHANES cycles were performed, with 12,505 subjects having complete data for gout and two 24-h dietary intake interviews. The 24-h dietary recalls were utilized to evaluate dietary habits. Gout was defined based on questionnaires. Weighted logistic regression models were conducted to investigate the association between n-3 PUFA poor/rich seafood consumption and gout. Moreover, subgroup analysis was utilized to estimate the stability of results. Covariates including age, gender, race/ethnicity, income, education, body mass index, chronic kidney disease, diabetes mellitus, hypertension, smoking status, and drinking status were stratified in different models.
Results
In the fully adjusted model, each unit of increase of n-3 PUFA poor seafood intake was associated with an 8.7% increased risk of gout (OR = 1.087, 95% CI: 1.039, 1.138, P < 0.001), whereas, no correlation was found between n-3 PUFA rich seafood consumption and gout. It also provided a proof-of-concept regarding the potential for n-3 PUFA rich seafood to counteract harmful effects of purines in relation to gout. A dose-response analysis showed that there was a non-linear relationship between n-3 PUFA rich seafood intake and the risk of gout in the female group.
Conclusion
Findings suggest that n-3 PUFA poor seafood consumption is associated with higher risk of gout, whereas n-3 PUFA rich seafood is not.
Keywords: n-3 PUFA poor/rich seafood consumption, gout, inflammation, National Health and Nutrition Examination Survey, nutrition
Introduction
Gout is an inflammatory crystal arthritis, the most important pathological characteristic of which is monosodium urate deposition in the joints. The incidence of gout has been stably increasing to 0.58–2.89 per 1,000 person-years worldwide with the development of the world economy and lifestyle changes (1). Additionally, gout episodes have undesirable effects on the quality of life (2).
Recent studies have revealed a strong link between omega-3 polyunsaturated fatty acids (n-3 PUFA) and anti-inflammatory impacts (3–5). Numerous systematic reviews and meta-analysis have noted that n-3 PUFAs exhibited anti-inflammatory effects on multiple non-communicable diseases, including systemic inflammatory response syndrome (3), colorectal cancer (4), type 2 diabetic mellitus (5), bipolar disorder (6), mental disorders (7), polycystic ovary syndrome (8), heart failure (9), hypertension (10), and rheumatoid arthritis (11). With respect to gout, experiments in vitro noted that n-3 PUFAs could inhibit the NLRP3 inflammasome in monocytes via downstream effects of a two-signal initiation system (12, 13), including suppression of nuclear factor kappa-B (NF-κB) via Toll-like receptor 4 and Toll-like receptor 2 (14) and assembly of the inflammasome and activation of caspase-1 (15). Clinically, a case control study showed that low serum n-3 PUFA levels were connected with frequent gout flares (16). Although it is well established that most seafood, which typically contains large quantities of purines, leads to increased risk of gout (17, 18), whether the harmful effects of seafood in relation to gout may vary owing to different levels of n-3 PUFA in seafood is still unclear. According to the US Department of Agriculture (USDA) Dietary Research Nutrition Database, the seafood component is divided into: seafood that are high in n-3 PUFA and seafood that are low in n-3 PUFA. Whether n-3 PUFA poor seafood or n-3 PUFA rich seafood can affect gout remained to be elucidated.
Hence, the preliminary aim of this study was to determine the relationship between n-3 PUFA poor/rich seafood consumption and gout in US adults using data from the National Health and Nutrition Examination Survey (NHANES). Our study was the first large-scale cross-sectional study evaluating n-3 PUFA poor/rich seafood consumption and gout, which could shed new light on gout management.
Materials and methods
Study population
Potential subjects in the present study were selected from 2007 to 2016 cycle of NHANES. NHANES is a periodic, nationally representative health study conducted by the Nation Center for Health Statistics (NCHS) at the Centers for Disease Control and Prevention (CDC) aimed at evaluating individuals’ health and nutritional status. NHANES was approved by the NCHS Ethics Review Board. All subjects provided written informed consent. All data in this study are publicly accessible at http://www.cdc.gov/nchs/nhanes/.
Participants aged <20 years old (n = 21,387), without complete information about dietary data (n = 6,489), missing data on gout (n = 1,131), or missing baseline condition (n = 9,076) were excluded, leaving a total of 12,505 subjects for the present analysis (Figure 1).
FIGURE 1.
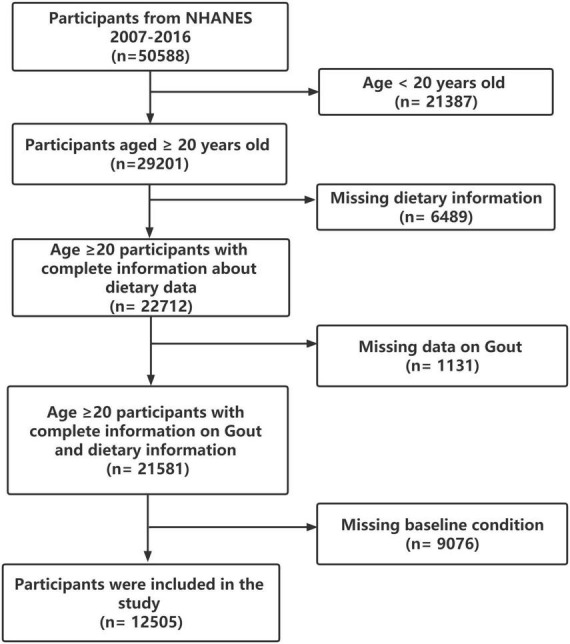
Study flowchart.
Measurements and covariation assessment
Dietary assessment
A total of 24-h dietary recalls were utilized to calculate individual dietary intakes, which have been examined by the Nutrition Methodology Working Group (19). To ensure precise food recall and alleviate the respondent burden, eligibility criteria included subjects who had both two valid 24-h dietary recalls.
Definition of seafood was founded on the USDA Dietary Research Nutrition Database. Seafood high in n-3 PUFA included anchovy, herring, mackerel, salmon, sardine, shark, trout, and bluefin and albacore tuna. Seafood low in n-3 PUFA included catfish, clams, cod, crabs, crayfish, croaker, eel, flounder, haddock, lobster, mussels, octopus, oyster, perch, pollock, scallop, shrimp, snapper, tilapia, tuna (other than bluefin and albacore), and turtle.
Gout
Similar to previous NHANES reports (20), all participants were asked “Has a doctor or other health professional ever told you that you had gout?” and then classified as non-gout participants and gout participants.
Covariables
Sociodemographic characteristics
According the current articles, the following variables were collected during the household interview, including age, gender, race/ethnicity, education level, and family poverty income ratio (PIR). Race/ethnicity was categorized into Mexican American, non-Hispanic Black, non-Hispanic White, other Hispanic, and other race (including multi-racial) based on NHANES classification (21). Education level was classified as less than high school, high school graduate/General Education Development (GED); some college/Associate of Arts (AA) degree and college graduate or more (22). PIR was utilized to evaluate family income. PIR was categorized into three strata (<1, 1–3, and ≥3) and defined as poor, near poor, and not poor, respectively (23).
Body mass index status
Body mass index (BMI) was calculated as the weight divided by the square of height (kg/m2). BMI <18.5 was considered as underweight, 18.5–24.9 as normal, 25–30 as overweight, and ≥30 as obese (24).
Smoking status
Smoking behavior was classified as never smoker, former smoker, and current smoker based on their answers to questionnaire about smoking more than 100 cigarettes in their life and whether they had quit smoking (25).
Drinking status
Drinking behavior was categorized as mild drinking (≤1 drink per day for women or ≤2 drinks per day for men on average over the past 12 months), moderate drinking (1–3 drinks per day for women or 2–4 drinks per day for men on average over the past 12 months), and heavy drinking (≥4 drinks per day for women or ≥5 drinks per day for men on average over the past 12 months) (26).
Chronic kidney disease
We used the Chronic Kidney Disease Epidemiology Collaboration formulate to assess estimated glomerular filtration rate (eGFR). Chronic kidney disease (CKD) was defined as eGFR <60 ml/min/1.73 m2 or urine albumin creatinine ratio (UACR) >30 mg/g (27).
Hypertension
Hypertension was defined as systolic blood pressure ≥140 mmHg and/or diastolic blood pressure ≥90 mmHg based on the average of three measurements of all subjects’ blood pressure (28).
Diabetes mellitus
Diabetes mellitus (DM) was defined as self-reported diabetes, the use of diabetes medication or insulin, glycohemoglobin (HbA1c) >6.5%, fasting glucose ≥7.0 mmol/L, random blood glucose ≥11.1 mmol/L, or 2-h oral glucose tolerance test (OGTT) blood glucose (mmol/L) ≥11.1 (29). Impaired fasting glucose (IFG) was defined as fasting plasma glucose concentration ≥5.6 and ≤6.9 mmol/L (30). Impaired glucose tolerance (IGT) was defined as a plasma glucose level ≥7.8 and ≤11.0 mmol/L at 2 h after OGTT (30).
Statistical analysis
All statistical analyses were performed following CDC guidelines for analysis of NHANES data. A suitable sample weight was utilized to calculate all statistical analyses in order that the data corresponded to the non-institutionalized civilian population. Continuous variables were represented by mean and standard deviation (SD), whereas categorical variables were expressed by counts and weighted percentages. One-way ANOVA test (for normally distributed continuous variables), Kruskal–Wallis H-test (for non-normally distributed continuous variables) and Chi-square test (for categorical variables) were utilized to measure differences among different groups.
Weighted logistic regression analysis was set up to estimate the relationship between n-3 PUFA poor/rich seafood consumption and gout. To further examine the covariable effect on this correlation, we employed Model 1 (unadjusted), Model 2 (age, gender, and race/ethnicity were adjusted), and Model 3 (all covariates in Table 1 were adjusted). In addition, restricted cubic spline models were utilized to investigated their dose-response relationship in Model 3. Finally, we further explored the heterogenicity in different groups with interaction terms. P < 0.05 with effective confidence interval (CI) was of statistical significance. All analyses were constructed with R version 4.0.41 (The R foundation).
TABLE 1.
Characteristics among adults with/without gout.
| Variable | Overall | Individuals without gout | Individuals with gout | P-value |
| Age, years, mean (SD) | 46.29 (0.31) | 45.80 (0.30) | 59.50 (0.70) | <0.001 |
| n-3 PUFA rich seafood intake, oz/day, mean (SD) | 0.19 (0.01) | 0.19 (0.01) | 0.29 (0.06) | 0.100 |
| n-3 PUFA poor seafood intake, oz/day, mean (SD) | 0.48 (0.02) | 0.46 (0.02) | 0.78 (0.13) | 0.020 |
| Gender, n (%) | <0.001 | |||
| Female | 5,894 (48.83) | 5,777 (49.69) | 117 (25.57) | |
| Male | 6,611 (51.17) | 6,189 (50.31) | 422 (74.43) | |
| Race/ethnicity, n (%) | <0.001 | |||
| Mexican American | 1,718 (7.21) | 1,687 (7.37) | 31 (2.71) | |
| Non-Hispanic Black | 2,370 (9.18) | 2,240 (9.13) | 130 (10.52) | |
| Non-Hispanic White | 6,071 (73.18) | 5,771 (72.95) | 300 (79.17) | |
| Other Hispanic | 1,202 (4.71) | 1,169 (4.81) | 33 (2.13) | |
| Other race (including multi-racial) | 1,144 (5.73) | 1,099 (5.74) | 45 (5.47) | |
| Income, n (%) | 0.570 | |||
| Poor | 2,275 (11.75) | 2,178 (11.74) | 97 (12.22) | |
| Near poor | 4,841 (32.48) | 4,631 (32.58) | 210 (29.86) | |
| Not poor | 5,389 (55.76) | 5,157 (55.68) | 232 (57.91) | |
| Education, n (%) | 0.790 | |||
| Less than high school | 2,259 (11.64) | 2,162 (11.63) | 97 (11.73) | |
| High school graduate/GED | 2,737 (20.39) | 2,602 (20.34) | 135 (21.88) | |
| Some college or AA degree | 3,951 (32.94) | 3,784 (32.90) | 167 (33.96) | |
| College graduate or more | 3,558 (35.03) | 3,418 (35.12) | 140 (32.43) | |
| BMI, n (%) | <0.001 | |||
| Underweight (<18.5) | 168 (35.14) | 164 (1.31) | 4 (0.40) | |
| Normal (≥18.5 and ≤24.9) | 3,530 (1.28) | 3,442 (30.08) | 88 (13.97) | |
| Overweight (>24.9 and <30) | 4,247 (34.08) | 4,074 (34.14) | 173 (32.48) | |
| Obese (≥30) | 4,560 (29.5) | 4,286 (34.47) | 274 (53.15) | |
| CKD, n (%) | <0.001 | |||
| No | 10,706 (88.19) | 10,372 (88.92) | 334 (68.65) | |
| Yes | 1,799 (11.81) | 1,594 (11.08) | 205 (31.35) | |
| DM, n (%) | <0.001 | |||
| DM | 1,858 (11.5) | 1,660 (10.76) | 198 (31.50) | |
| IFG | 540 (4.5) | 503 (4.31) | 37 (9.47) | |
| IGT | 507 (3.75) | 478 (3.75) | 29 (3.89) | |
| No | 9,600 (80.25) | 9,325 (81.18) | 275 (55.13) | |
| Hypertension, n (%) | <0.001 | |||
| No | 7,622 (64.65) | 7,514 (66.21) | 108 (22.76) | |
| Yes | 4,883 (35.35) | 4,452 (33.79) | 431 (77.24) | |
| Smoking status, n (%) | <0.001 | |||
| Former | 3,219 (26.35) | 2,990 (25.70) | 229 (43.73) | |
| Never | 6,417 (52.71) | 6,204 (53.13) | 213 (41.34) | |
| Current | 2,869 (20.95) | 2,772 (21.17) | 97 (14.92) | |
| Drinking status, n (%) | <0.001 | |||
| Mild | 6,166 (49.48) | 5,844 (49.10) | 322 (59.51) | |
| Moderate | 2,797 (23.3) | 2,710 (23.61) | 87 (14.97) | |
| Heavy | 3,542 (27.22) | 3,412 (27.28) | 130 (25.53) |
SD, standard deviation; n-3 PUFA, omega-3 polyunsaturated fatty acid; oz, ounce; GED, General Education Development; AA degree, Associate of Arts; BMI, body mass index; HUA, hyperuricemia; CKD, chronic kidney disease; DM, diabetes mellitus; IFG, impaired fasting glucose; IGT, impaired glucose tolerance.
Results
Population characteristics between groups
As illustrated in Figure 1, a total of 12,505 subjects were enrolled in this study. Table 1 summarized the population characteristics overall and between two groups (adults with/without gout). In the whole research population, the median age at baseline was 46.29 years, 48.33% were females and 51.17% were males. The overall prevalence of gout among US adults was 4.31%. Participants with gout were more likely be older, male, non-Hispanic White, obese, alcoholic, former smokers (P < 0.01). Additionally, they suffered from CKD, DM, hypertension, and had higher n-3 PUFA poor seafood intake (P < 0.05). There was no difference in income and education levels (P > 0.05).
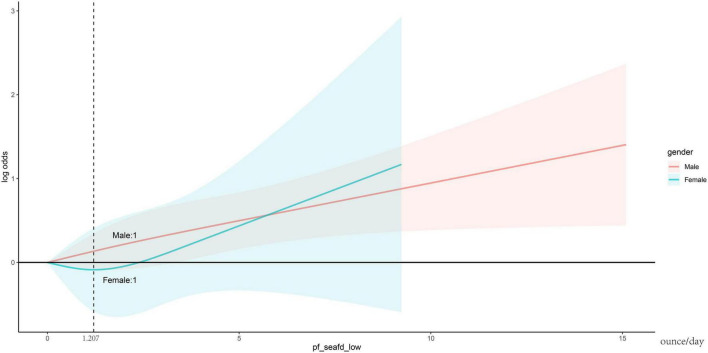
n-3 PUFA poor seafood intake is associated with higher risk of gout
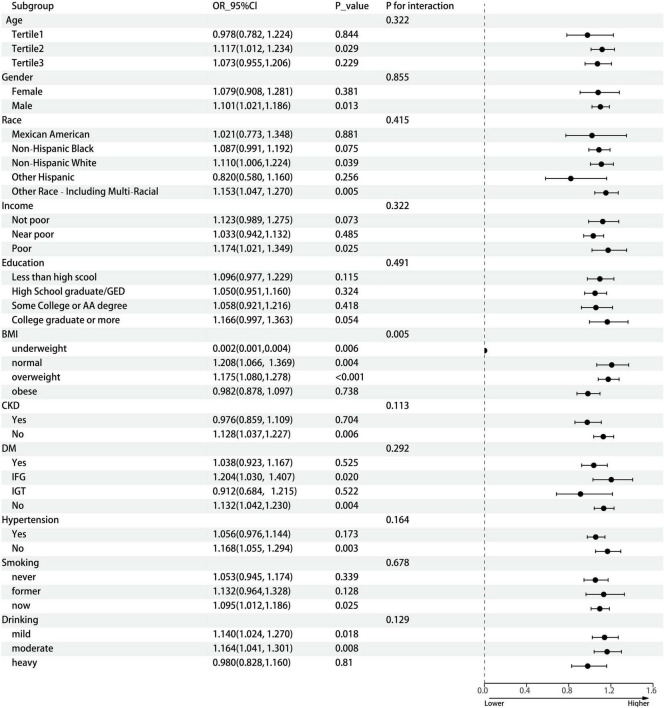
Results of weighted logistic regression analysis for the association between n-3 PUFA poor/rich seafood consumption and gout are shown in Table 2. Weighted logistic regression analysis confirmed that higher n-3 PUFA poor seafood intake was associated with an increased risk of gout (Model 1, OR = 1.098, 95% CI: 1.053, 1.145, P < 0.001; Model 2, OR = 1.096, 95% CI: 1.048, 1.146, P < 0.001; Model 3, OR = 1.087, 95% CI: 1.039, 1.138, P < 0.001). In model 3, which adjusted for all confounding variables, the results still revealed that each unit of increase of n-3 PUFA poor seafood intake was associated with an 8.7% increased risk of gout. With respect to n-3 PUFA rich seafood intake, the connection with gout was only significant in model 1(OR = 1.112, 95% CI: 1.017, 1.216, P = 0.019), but become non-significant after stepwise adjusting for confounding variables (Models 2 and 3). In dose-response relationships, n-3 PUFA rich seafood consumption was non-linearly related with gout in the female group. We found an inverted L-shaped association. The prevalence of gout reached a plateau when the n-3 PUFA poor seafood intake was lower than 1.207 ounce/day in the female group. Figure 2 depicts the dose response relationship. We also conducted subgroup analyses stratified by age, gender, race/ethnicity, income, education, BMI, CKD, DM, hypertension, smoking, and drinking status to evaluate the association between n-3 PUFA rich seafood intake and gout (Figure 3). This association was similar among participants aged >37 and <56 years old. Relatively stronger relationships were also observed among male, non-Hispanic White, other race and patients with underweight, normal weight, overweight, IFG, non-DM, mild drinking, and moderate drinking. Additionally, statistically significant ORs were only present in people without CKD, hypertension and with a lower household PIR and current smoking. Besides, we also explored the heterogenicity among each subgroup with interaction terms and no significant difference was revealed among age, gender, race/ethnicity, income, education, CKD, DM, hypertension, smoking status, and drinking status (P for interaction >0.05 for all), revealing that the magnitude of this relationship was the same for the subjects separated into different subgroups.
TABLE 2.
Association between n-3 PUFA rich/poor seafood intake and gout.
| Variable | OR (95% CI), P-value | ||
| Model 1 | Model 2 | Model 3 | |
| n-3 PUFA rich seafood intake | 1.112 (1.017, 1.216), 0.019 | 1.045 (0.947, 1.153), 0.380 | 1.070 (0.969, 1.183), 0.180 |
| n-3 PUFA poor seafood intake | 1.098 (1.053, 1.145), <0.001 | 1.096 (1.048, 1.146), <0.001 | 1.087 (1.039, 1.138), <0.001 |
Model 1: no adjustment.
Model 2: adjusted for age, gender, and race/ethnicity.
Model 3: adjusted for age, gender, race/ethnicity, income, education, BMI, CKD, DM, hypertension, smoking status, and drinking status.
OR, odds ratio; CI, confidence interval; n-3 PUFA, omega-3 polyunsaturated fatty acid; BMI, body mass index; CKD, chronic kidney disease; DM, diabetes mellitus.
FIGURE 2.
The dose-response relationship between n-3 PUFA poor seafood intake and gout. Adjusted for age, gender, race/ethnicity, income, education, BMI, CKD, DM, hypertension, smoking status, and drinking status. Solid lines hazard ratio, blue or pink area 95% confidence interval. n-3 PUFA, omega-3 polyunsaturated fatty acid; BMI, body mass index; CKD, chronic kidney disease; DM, diabetes mellitus.
FIGURE 3.
Subgroup analysis between n-3 PUFA poor seafood intake and gout. The subgroup analysis was adjusted for age, gender, race/ethnicity, income, education, BMI, CKD, DM, hypertension, smoking status, and drinking status. Age (years old), Tertile 1, 20–37, Tertile 2, 37–56, Tertile 3, 56–80; n-3 PUFA, omega-3 polyunsaturated fatty acid; OR, odds ratio; CI, confidence interval; GED, General Education Development; AA degree, Associate of Arts; BMI, body mass index; CKD, chronic kidney disease; DM, diabetes mellitus; IFG, impaired fasting glucose; IGT, impaired glucose tolerance.
Discussion
In this nationwide cross-sectional study with 12,505 adults, a significant positive connection of n-3 PUFA poor seafood intake with gout was uncovered, revealing that higher consumption of n-3 PUFA poor seafood may contribute to an increased risk of gout. This connection remained statistically significant after we adjusted for all confounders, including age, gender, race/ethnicity, income, education, BMI, CKD, DM, hypertension, smoking status, and drinking status. Correlated subgroup analyses stratified by different variables revealed that this positive connection was not influenced, suggesting that this connection could be appropriated for different population.
It was worth noting that there was a lack of research on the effect of n-3 PUFA poor/rich seafood consumption on gout. It is well established that purine-rich foods consumption, which comprised most seafood, brings about an increased risk of gout (17). Interestingly, our study demonstrated that only n-3 PUFA poor seafood consumption was associated with increased risk of gout with statistical significance. The results of our study also provided a proof-of-concept regarding the potential for n-3 PUFA rich seafood to counteract harmful effects of purines in relation to gout. Emerging evidence has shown that n-3 PUFAs could exert protective anti-inflammatory effects. A meta-analysis revealed that supplementation of n-3 PUFAs in adults can improve inflammatory biomarkers, such as serum C-reactive protein, tumor necrosis factor α (TNF-α), and interleukin 6 (IL-6) (31).
Several hypotheses could be put forward to explain the anti-inflammatory effects of n-3 PUFAs. First, n-3 PUFAs may involve in the regulation of immunological and inflammatory responses via the gut microbiome (32–34). Gut microbiota can influence the metabolism and absorption of n-3 PUFAs, in the meantime, n-3 PUFAs can also affect the diversity and abundance of the gut microbiome. For example, n-3 PUFAs possibly suppressed the Firmicutes/Bacteroidetes ratio and the levels of Coprococcus and Faecalibacterium and increased the abundance of butyrate-producing bacterial genera, thus further reducing the inflammatory processes (35–37).
Second, n-3 PUFAs are important mediators in membrane phospholipid fatty acid composition of inflammatory cells (38). n-3 PUFAs could vary the composition of membrane phospholipid fatty acid via a variety of general mechanisms, resulting in affecting inflammatory cell function. To begin with, the physical properties of the membrane, such as membrane fluidity and raft structure could be altered by n-3 PUFAs (38). Then, n-3 PUFAs could exert influences on cell signaling pathways. Certain n-3 PUFAs have been shown to have anti-inflammatory effects through inhibition of the principal inflammatory cytokine via extracellular inflammatory stimuli (39) and G-protein coupled receptors (40). An in vivo experiment revealed that peroxisome proliferator-activated receptor γ, an anti-inflammatory factor, was induced by n-3 PUFAs in dendritic cells (41). Furthermore, n-3 PUFAs could alter the production in the pattern of the lipid mediators. Animal studies have shown that n-3 PUFAs may modify the fatty acid of eicosanoid, a key mediators of inflammation, resulting in producing several anti-inflammatory and inflammation resolving mediators, such as resolvins and protectins (39). Finally, with respect to T cell signaling, n-3 PUFAs were found to disturb membrane-cytoskeletal structure and function in CD4+ T lymphocytes (33).
Third, n-3 PUFAs may exert anti-inflammatory effects in macrophages. The balance between pro- and anti-inflammation is coordinated by macrophages. Previous animal studies have demonstrated that adding n-3 PUFA to the diet induced a decrease in macrophages (40, 42). In studies of mechanisms, the anti-inflammatory function by n-3 PUFAs has been proved through the free fatty acid receptor 4 protein in macrophages resulting in suppressing activity of the NF-κB complex (42). Otherwise, in vivo findings have been supported that n-3 PUFAs regulated inflammatory signaling in macrophages via the autophagic receptor SQSTM1/p62-bodies and NFE2L2 (43).
The major strengths of this population-based study are using a nationally representative sample, which facilitates the finding to be universal to a broader population. Nevertheless, several limitations cannot be ignored. First, there were only two 24-h dietary recalls in NHANES rather than three 24-h dietary recalls (two weekdays and one Friday), where recall bias is inevitable.
To minimize the influence of two-time recall bias, the NHANES design utilized sampling weight and multiple-pass method to ensure precise of dietary intake and subjects who had both two valid 24-h dietary recalls were included in this study. Second, we were unable to consider more purine-rich foods except alcohol consumption, which may lead to confounding bias. Third, cross-section design cannot draw causal relationship.
Conclusion
In summary, our results suggest that n-3 PUFA poor seafood consumption is associated with higher risk of gout, whereas n-3 PUFA rich seafood is not and also provide a proof-of-concept regarding the potential for n-3 PUFA rich seafood to counteract harmful effects of purines in relation to gout. A dose-response analysis showed that there was a non-linear relationship between n-3 PUFA rich seafood intake and the risk of gout in the female group. Given this cross-section design, more well-designed prospective studies are warranted to validate the causal relationship between n-3 PUFA poor/rich seafood and gout.
Data availability statement
The original contributions presented in this study are included in the article/supplementary material, further inquiries can be directed to the corresponding author.
Author contributions
GZ and JW: conceptualization. GZ and DY: methodology. GZ, DY, and JW: software. GZ, LY, and JW: formal analysis. GZ, DY, LY, HS, JL, YW, and ZJ: data collection. GZ: writing—original draft preparation. JW: writing—review and editing and supervision. All authors read and agreed to the published version of the manuscript.
Acknowledgments
We thank the NHANES participants and staff for their contributions. We also thank Zhang Jing (Shanghai Tongren Hospital) for his work on the NHANES database. His outstanding work, nhanesR package, and webpage, makes it easier for us to explore NHANES database.
Footnotes
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
- 1.Dehlin M, Jacobsson L, Roddy E. Global epidemiology of gout: prevalence, incidence, treatment patterns and risk factors. Nat Rev Rheumatol. (2020) 16:380–90. 10.1038/s41584-020-0441-1 [DOI] [PubMed] [Google Scholar]
- 2.Smith E, Hoy D, Cross M, Merriman T, Vos T, Buchbinder R, et al. The global burden of gout: estimates from the global burden of disease 2010 study. Ann Rheum Dis. (2014) 73:1470–6. 10.1136/annrheumdis-2013-204647 [DOI] [PubMed] [Google Scholar]
- 3.Wan X, Gao X, Bi J, Tian F, Wang X. Use of N-3 PUFAs can decrease the mortality in patients with systemic inflammatory response syndrome: a systematic review and meta-analysis. Lipids Health Dis. (2015) 14:23. 10.1186/s12944-015-0022-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Mocellin M, Camargo C, Nunes E, Fiates G, Trindade EA. Systematic review and meta-analysis of the N-3 polyunsaturated fatty acids effects on inflammatory markers in colorectal cancer. Clin Nutr. (2016) 35:359–69. 10.1016/j.clnu.2015.04.013 [DOI] [PubMed] [Google Scholar]
- 5.Lin N, Shi J, Li Y, Zhang X, Chen Y, Calder P, et al. What is the impact of N-3 PUFAs on inflammation markers in type 2 diabetic mellitus populations?: a systematic review and meta-analysis of randomized controlled trials. Lipids Health Dis. (2016) 15:133. 10.1186/s12944-016-0303-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Saunders E, Ramsden C, Sherazy M, Gelenberg A, Davis J, Rapoport S. Omega-3 and omega-6 polyunsaturated fatty acids in bipolar disorder: a review of biomarker and treatment studies. J Clin Psychiatry. (2016) 77:e1301–8. 10.4088/JCP.15r09925 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Gao X, Su X, Han X, Wen H, Cheng C, Zhang S, et al. Unsaturated fatty acids in mental disorders: an umbrella review of meta-analyses. Adv Nutr. (2022) 13:2217–36. 10.1093/advances/nmac084 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Yuan J, Wen X, Jia M. Efficacy of Omega-3 polyunsaturated fatty acids on hormones, oxidative stress, and inflammatory parameters among polycystic ovary syndrome: a systematic review and meta-analysis. Ann Palliat Med. (2021) 10:8991–9001. 10.21037/apm-21-2018 [DOI] [PubMed] [Google Scholar]
- 9.Zheng S, Qiu M, Wu J, Pan X, Liu X, Sun L, et al. Long-chain Omega-3 polyunsaturated fatty acids and the risk of heart failure. Ther Adv Chronic Dis. (2022) 13:20406223221081616. 10.1177/20406223221081616 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Musazadeh V, Kavyani Z, Naghshbandi B, Dehghan P, Vajdi M. The beneficial effects of Omega-3 polyunsaturated fatty acids on controlling blood pressure: an umbrella meta-analysis. Front Nutr. (2022) 9:985451. 10.3389/fnut.2022.985451 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Goldberg R, Katz JA. Meta-analysis of the analgesic effects of Omega-3 polyunsaturated fatty acid supplementation for inflammatory joint pain. Pain. (2007) 129:210–23. 10.1016/j.pain.2007.01.020 [DOI] [PubMed] [Google Scholar]
- 12.Martinon F, Pétrilli V, Mayor A, Tardivel A, Tschopp J. Gout-associated uric acid crystals activate the NALP3 inflammasome. Nature. (2006) 440:237–41. 10.1038/nature04516 [DOI] [PubMed] [Google Scholar]
- 13.Novak T, Babcock T, Jho D, Helton W, Espat N. NF-Kappa B inhibition by Omega -3 fatty acids modulates Lps-stimulated macrophage TNF-alpha transcription. Am J Physiol Lung Cell Mol Physiol. (2003) 284:L84–9. 10.1152/ajplung.00077.2002 [DOI] [PubMed] [Google Scholar]
- 14.Zhao Y, Joshi-Barve S, Barve S, Chen L. Eicosapentaenoic acid prevents LPS-induced TNF-alpha expression by preventing NF-kappab activation. J Am Coll Nutr. (2004) 23:71–8. 10.1080/07315724.2004.10719345 [DOI] [PubMed] [Google Scholar]
- 15.Weatherill A, Lee J, Zhao L, Lemay D, Youn H, Hwang D. Saturated and polyunsaturated fatty acids reciprocally modulate dendritic cell functions mediated through TLR4. J Immunol. (2005) 174:5390–7. 10.4049/jimmunol.174.9.5390 [DOI] [PubMed] [Google Scholar]
- 16.Abhishek A, Valdes A, Doherty M. Low Omega-3 fatty acid levels associate with frequent gout attacks: a case control study. Ann Rheum Dis. (2016) 75:784–5. 10.1136/annrheumdis-2015-208767 [DOI] [PubMed] [Google Scholar]
- 17.Choi H, Atkinson K, Karlson E, Willett W, Curhan G. Purine-rich foods, dairy and protein intake, and the risk of gout in men. N Engl J Med. (2004) 350:1093–103. 10.1056/NEJMoa035700 [DOI] [PubMed] [Google Scholar]
- 18.Villegas R, Xiang Y, Elasy T, Xu W, Cai H, Cai Q, et al. Purine-rich foods, protein intake, and the prevalence of hyperuricemia: the shanghai men’s health study. Nutr Metab Cardiovasc Dis. (2012) 22:409–16. 10.1016/j.numecd.2010.07.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.National Center for Health Statistics. Plan and operation of the third national health and nutrition examination survey, 1988-94. Series 1: programs and collection procedures. Vital Health Stat 1. (1994) 32:1–407. [PubMed] [Google Scholar]
- 20.Nie J, Deng M, Wang K, Liu F, Xu H, Feng Q, et al. Higher HEI-2015 scores are associated with lower risk of gout and hyperuricemia: results from the national health and nutrition examination survey 2007-2016. Front Nutr. (2022) 9:921550. 10.3389/fnut.2022.921550 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Tsai J, Homa D, Gentzke A, Mahoney M, Sharapova S, Sosnoff C, et al. Exposure to secondhand smoke among nonsmokers - United States, 1988-2014. MMWR Morb Mortal Wkly Rep. (2018) 67:1342–6. 10.15585/mmwr.mm6748a3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Scholes S, Bann D. Education-related disparities in reported physical activity during leisure-time, active transportation, and work among us adults: repeated cross-sectional analysis from the national health and nutrition examination surveys, 2007 to 2016. BMC Public Health. (2018) 18:926. 10.1186/s12889-018-5857-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Liu Y. The relationship between lifestyle and self-reported oral health among American adults. Int Dent J. (2014) 64:46–51. 10.1111/idj.12061 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Lu N, Dubreuil M, Zhang Y, Neogi T, Rai S, Ascherio A, et al. Gout and the risk of Alzheimer’s disease: a population-based, BMI-matched cohort study. Ann Rheum Dis. (2016) 75:547–51. 10.1136/annrheumdis-2014-206917 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ssy A, Natto Z, Midle J, Gyurko R, O’Neill R, Steffensen B. Association between time since quitting smoking and periodontitis in former smokers in the national health and nutrition examination surveys (NHANES) 2009 to 2012. J Periodontol. (2019) 90:16–25. 10.1002/jper.18-0183 [DOI] [PubMed] [Google Scholar]
- 26.Hicks C, Wang D, Matsushita K, Windham B, Selvin E. Peripheral neuropathy and all-cause and cardiovascular mortality in U.S. Adults: a prospective cohort study. Ann Intern Med. (2021) 174:167–74. 10.7326/m20-1340 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kidney Disease: Improving Global Outcomes (KDIGO) Glomerular Diseases Work Group. KDIGO 2021 clinical practice guideline for the management of glomerular diseases. Kidney Int. (2021) 100:S1–276. 10.1016/j.kint.2021.05.021 [DOI] [PubMed] [Google Scholar]
- 28.Elliott W. Systemic hypertension. Curr Probl Cardiol. (2007) 32:201–59. 10.1016/j.cpcardiol.2007.01.002 [DOI] [PubMed] [Google Scholar]
- 29.Qin Z, Zhao J, Li J, Yang Q, Geng J, Liao R, et al. Low lean mass is associated with lower urinary tract symptoms in us men from the 2005-2006 national health and nutrition examination survey dataset. Aging. (2021) 13:21421–34. 10.18632/aging.203480 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.American Diabetes Association [ADA]. Diagnosis and classification of diabetes mellitus. Diabetes Care. (2010) 33(Suppl. 1):S62–9. 10.2337/dc10-S062 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Kavyani Z, Musazadeh V, Fathi S, Hossein Faghfouri A, Dehghan P, Sarmadi B. Efficacy of the Omega-3 fatty acids supplementation on inflammatory biomarkers: an umbrella meta-analysis. Int Immunopharmacol. (2022) 111:109104. 10.1016/j.intimp.2022.109104 [DOI] [PubMed] [Google Scholar]
- 32.Bäck M, Hansson G. Omega-3 fatty acids, cardiovascular risk, and the resolution of inflammation. FASEB J. (2019) 33:1536–9. 10.1096/fj.201802445R [DOI] [PubMed] [Google Scholar]
- 33.Hou T, McMurray D, Chapkin R. Omega-3 fatty acids, lipid rafts, and T cell signaling. Eur J Pharmacol. (2016) 785:2–9. 10.1016/j.ejphar.2015.03.091 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Kim M, Qie Y, Park J, Kim C. Gut microbial metabolites fuel host antibody responses. Cell Host Microbe. (2016) 20:202–14. 10.1016/j.chom.2016.07.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Balfegó M, Canivell S, Hanzu F, Sala-Vila A, Martínez-Medina M, Murillo S, et al. Effects of sardine-enriched diet on metabolic control, inflammation and gut microbiota in drug-naïve patients with type 2 diabetes: a pilot randomized trial. Lipids Health Dis. (2016) 15:78. 10.1186/s12944-016-0245-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Andersen A, Mølbak L, Michaelsen K, Lauritzen L. Molecular fingerprints of the human fecal microbiota from 9 to 18 months old and the effect of fish oil supplementation. J Pediatr Gastroenterol Nutr. (2011) 53:303–9. 10.1097/MPG.0b013e31821d298f [DOI] [PubMed] [Google Scholar]
- 37.Watson H, Mitra S, Croden F, Taylor M, Wood H, Perry S, et al. A randomised trial of the effect of omega-3 polyunsaturated fatty acid supplements on the human intestinal microbiota. Gut. (2018) 67:1974–83. 10.1136/gutjnl-2017-314968 [DOI] [PubMed] [Google Scholar]
- 38.Yaqoob P. The nutritional significance of lipid rafts. Annu Rev Nutr. (2009) 29:257–82. 10.1146/annurev-nutr-080508-141205 [DOI] [PubMed] [Google Scholar]
- 39.Calder P. Fatty acids and inflammation: the cutting edge between food and pharma. Eur J Pharmacol. (2011) 668(Suppl. 1):S50–8. 10.1016/j.ejphar.2011.05.085 [DOI] [PubMed] [Google Scholar]
- 40.Oh D, Talukdar S, Bae E, Imamura T, Morinaga H, Fan W, et al. Gpr120 is an Omega-3 fatty acid receptor mediating potent anti-inflammatory and insulin-sensitizing effects. Cell. (2010) 142:687–98. 10.1016/j.cell.2010.07.041 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Kong W, Yen J, Vassiliou E, Adhikary S, Toscano M, Ganea D. Docosahexaenoic acid prevents dendritic cell maturation and in vitro and in vivo expression of the Il-12 cytokine family. Lipids Health Dis. (2010) 9:12. 10.1186/1476-511x-9-12 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Im D. Functions of Omega-3 fatty acids and FFA4 (Gpr120) in macrophages. Eur J Pharmacol. (2016) 785:36–43. 10.1016/j.ejphar.2015.03.094 [DOI] [PubMed] [Google Scholar]
- 43.Mildenberger J, Johansson I, Sergin I, Kjøbli E, Damås J, Razani B, et al. N-3 PUFAs induce inflammatory tolerance by formation of KEAP1-containing SQSTM1/P62-bodies and activation of NFE2L2. Autophagy. (2017) 13:1664–78. 10.1080/15548627.2017.1345411 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The original contributions presented in this study are included in the article/supplementary material, further inquiries can be directed to the corresponding author.