Abstract
Background
The COVID‐19 pandemic affected outpatient care delivery and patients' access to health care. However, no prior studies have documented telehealth use among patients with cardiovascular disease.
Methods and Results
We documented the number of telehealth and in‐person outpatient encounters per 100 patients with cardiovascular disease and the percentage of telehealth encounters from January 2019 to June 2021, and the average payments per telehealth and in‐person encounters across a 12‐month period (July 2020–June 2021) using the MarketScan commercial database. From February 2020 to April 2020, the number of in‐person encounters per 100 patients with cardiovascular disease decreased from 304.2 to 147.7, whereas that of telehealth encounters increased from 0.29 to 25.3. The number of in‐person outpatient encounters then increased to 280.7 in June 2020, fluctuated between 268.1 and 346.4 afterward, and ended at 268.1 in June 2021, lower than the prepandemic levels. The number of telehealth encounters dropped to 16.8 in June 2020, fluctuated between 8.8 and 16.6 afterward, and ended at 8.8 in June 2021, higher than the prepandemic levels. Patients who were aged 18 to 35 years, women, and living in urban areas had higher percentages of telehealth encounters than those who were aged 35 to 64 years, men, and living in rural areas, respectively. The mean (95% CI) telehealth and in‐person outpatient encounter costs per visit were $112.8 (95% CI, $112.4–$113.2) and $161.4 (95% CI, $160.4– $162.4), respectively.
Conclusions
There were large fluctuations in telehealth and in‐person outpatient encounters during the pandemic. Our results provide insight into increased telehealth use among patients with cardiovascular disease after telehealth policy changes were implemented during the pandemic.
Keywords: cardiovascular disease, heart disease, stroke, telehealth, telehealth outpatient cost
Subject Categories: Health Services, Quality and Outcomes, Digital Health, Disparities
Nonstandard Abbreviations and Acronyms
- CCAE
Commercial Claims and Encounters
- OOP
out‐of‐pocket
Clinical Perspective.
What Is New?
Telehealth use increased significantly during the first 2 months of the pandemic among patients with cardiovascular disease and sub–cardiovascular diseases (eg, acute myocardial infarction, heart failure, ischemic heart disease, stroke, and atrial fibrillation).
In a subsample of a commercial claims database, telehealth and in‐person outpatient encounters among patients with cardiovascular disease changed significantly during the COVID‐19 pandemic periods compared with the prepandemic period.
Patients with cardiovascular disease who were younger, women, and living in urban areas had higher use of telehealth than those who were older, men, and living in rural areas, respectively, throughout the pandemic.
What Are the Clinical Implications?
Because the temporary telehealth provisions put in place during the COVID‐19 public health emergency remain, policymakers, health systems, health services researchers, and insurers may benefit from information about telehealth and in‐person use among patients with cardiovascular disease for decisions about drivers of telehealth use and sustainability.
Health care providers and health systems may attune the provision of care to the health needs of patients with cardiovascular disease–related diagnoses and continued interest in using telehealth services.
Policymakers, researchers, and insurers benefit from monitoring ongoing trends of use and cost of telehealth services when developing protocols for coverage and treatment, and tracking population health.
During the early COVID‐19 pandemic period, many states in the United States mandated stay‐at‐home orders, 1 and patients with COVID‐19 took priority for hospital beds and in‐person visits. 2 , 3 As a result, many patients who needed medical care either delayed their doctor visits 4 , 5 or sought telehealth. 6 Because of the emergency need for telehealth, the Centers for Medicare and Medicaid Services relaxed telehealth restrictions by expanding coverage of services starting March 6, 2020. 7 For example, expanded telehealth flexibilities allowed for broader use of telehealth during the public health emergency, such as waiving geographic limitations in service provision and expanding the list of services eligible for reimbursement. 8 The Centers for Medicare and Medicaid Services encouraged private health insurers to cover telehealth services, and the US Department of Health and Human Services Office for Civil Rights waived the Health Insurance Portability and Accountability Act rules to facilitate telehealth use during the pandemic. 9 Several studies have documented increased telehealth use associated with these COVID‐19–related policy changes. 10 , 11 , 12 , 13 , 14 However, no prior studies have documented telehealth use among patients diagnosed with cardiovascular disease (CVD).
CVD is prevalent and burdensome, with 931 558 deaths in 2020 attributed to CVD. 15 Nearly half of US adults (49.2%) have at least 1 type of CVD, 16 and 28% of all deaths of US adults are attributed to CVD. 15 Ideal care for chronic diseases often includes primary care, self‐management strategies, and multiple touchpoints with the health care system. 17 Heath care access, particularly the role of telehealth during the pandemic, was relevant for patients with cardiovascular conditions because of the potentially increased risk for developing serious illnesses from COVID‐19. 18 Although studies have examined overall trends in the use of telehealth at various time points throughout the pandemic, 19 , 20 , 21 no studies have documented telehealth use among patients diagnosed with CVD or those who have underlying and potentially undiagnosed CVD conditions. Documenting telehealth use among patients with cardiovascular conditions and the related costs could guide decisions about ongoing telehealth implementation among patients with CVD.
This study reports the trends in telehealth use and in‐person outpatient visits among patients with CVD before and during the COVID‐19 pandemic using commercial insurance claims data to examine health care use patterns that may have been associated with these policy changes (ie, mobility restrictions and expanded coverage of telehealth). Finally, we summarize the cost of telehealth and in‐person visits for patients with CVD.
Methods
Data
We used the IBM Watson Truven Health MarketScan Commercial Claims and Encounters (CCAE) database from January 1, 2019 to June 30, 2021. 22 MarketScan CCAE database are derived from administrative medical claims of a large subsample of enrollees and their dependents in employer‐sponsored health insurance plans provided by >300 large employers covering 30 health plans and >500 hospitals in the United States, with 24.9 million enrollees in 2017 and 16.4 million enrollees in 2020. The data include inpatient, emergency department, outpatient, and pharmacy claims, information about patients’ demographics such as age and sex, type of insurance plans (ie, capitated or noncapitated), and urban/rural status and Census region of patient residence, and allows tracking of patients over multiple periods. MarketScan data have been used in a wide range of studies, including those on health care use. 23 , 24 , 25 , 26 We accessed MarketScan data through Truven Health MarketScan Treatment Pathways, an online query tool that allows researchers to access data by identifying cohorts of patients based on the International Classification of Diseases, Tenth Revision, Clinical Modification (ICD‐10‐CM) diagnosis code, procedure modifiers, and place and date of service. All MarketScan patient data are deidentified and comply with the Health Insurance Portability and Accountability Act, so our study is not subject to institutional review board approval from the Centers for Disease Control and Prevention. The authors cannot make the MarketScan data publicly available because of the data use agreement. The program codes used for the study will be available upon request to the corresponding author.
Identification of Patients With CVD
Figure 1 shows the study sample selection to identify patients diagnosed with CVD. We first selected patients who appeared in 2017 to 2018 MarketScan commercial data, aged 18 to 64 years as of June 30, 2021, and continuously enrolled from January 2017 to June 2021. We excluded patients aged ≥65 years, because they might also have coverage through Medicare, which would not be captured in the CCAE database. We based our definition of patients with CVD on ICD‐10‐CM codes I00‐I09 and I16‐I78, defined after excluding hypertension diagnosis (ICD‐10‐CM code I10‐I15) from CVD diagnosis (ICD‐10‐CM code I00‐I78). We excluded patients with hypertension only because more than half of the patients with CVD diagnosis had only hypertension diagnosis, which we would like to study differently from other CVD diagnoses, as suggested by a subject matter expert in our institution. Patients with CVD were identifi ed if there was at least 1 CVD diagnosis (ICD‐10‐CM codes I00‐I09 and I16‐I78) from inpatient or emergency department encounters, or 2 diagnoses of CVD from outpatient encounters at least 30 days apart from January 2017 to December 2018. We used ICD‐10‐CM code Z3A to exclude patients with pregnancy diagnoses from January 2017 to June 2021.
Figure 1. Study sample selection of patients diagnosed with cardiovascular disease (CVD), MarketScan Commercial Claims and Encounters database, January 2017 to June 2021.
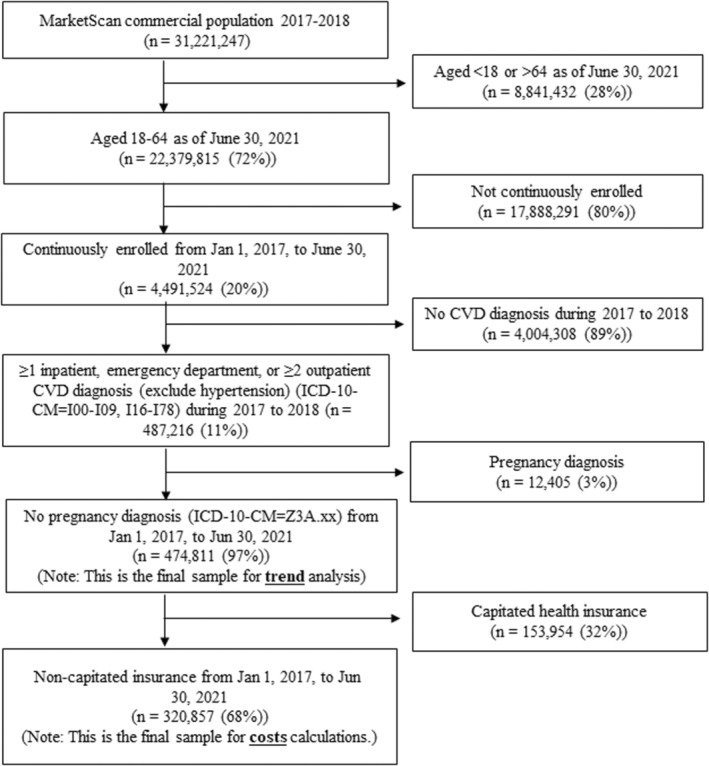
The MarketScan Commercial Claims and Encounters database from January 1, 2017 to June 30, 2021 was used. Inpatient, outpatient, and emergency department visits were identified using International Classification of Diseases, Tenth Revision, Clinical Modification (ICD‐10‐CM) codes. ICD‐10‐CM codes of I00–I09 and I16–I78 were used to define the diagnosis of cardiovascular disease (CVD) (ICD‐10‐CM codes I00–I09, I16–I78), defined after excluding hypertension diagnosis alone (ICD‐10‐CM codes I10–I15) from CVD (ICD‐10‐CM codes I00–I78). ICD‐10‐CM code Z3A was used to exclude patients with pregnancy diagnoses. Patients with CVD were identified if inpatient or emergency department encounters contained at least 1 diagnosis of CVD, or at least 2 outpatient encounters contained the diagnosis of CVD with at least a 30‐day interval during the 2 years of lookback periods from January 1, 2017 to December 31, 2018. For the patients with CVD with capitated and noncapitated health insurance, the trend analysis was performed from January 1, 2019 to June 30, 2021. Patients were restricted with noncapitated health insurance for the cost calculations because of inaccurate payment information in capitated health insurance.
Identification of Patients With Sub‐CVD Diseases
We used the same algorithms to identify patients with sub‐CVD diseases as we did to identify patients with CVD. We classified the following conditions as sub‐CVD diseases: acute myocardial infarction (ICD‐10‐CM codes I21–I22), heart failure (ICD‐10‐CM codes I09.81, I50.1–I50.4, I50.8–I50.9), ischemic heart disease (ICD‐10‐CM codes I20–I25), stroke (ICD‐10‐CM codes I60–I69), and atrial fibrillation (ICD‐10‐CM code I48). 27 The sub‐CVD diseases are particular subgroups of interest within the CVD sample population.
Identification of Telehealth Versus In‐Person Outpatient Encounters
We defined telehealth outpatient encounters as those in which the place of service was telehealth or the procedure modifiers were telehealth‐related (procedure modifiers 95, GO, GQ, and GT). 22 In‐person outpatient encounters were all the remaining outpatient encounters.
Trends of Telehealth and In‐Person Outpatient Encounters
We calculated the number of telehealth and in‐person outpatient encounters per 100 patients with CVD and the percentage of telehealth encounters monthly during January 2019 to June 2021. The prepandemic period is defined from January 2019 to February 2020, and the pandemic period is determined to be from March 2020 to June 2021. We calculated the numbers of telehealth and in‐person outpatient encounters per 100 patients by dividing the total numbers of telehealth and in‐person outpatient encounters in a month by the total number of patients with CVD, respectively, then multiplying by 100. We calculated the percentage of telehealth outpatient encounters by dividing the total number of telehealth outpatient encounters in a month by the total number of all (both telehealth and in‐person) outpatient encounters for the month among patients with CVD, then multiplying by 100. Results were stratified by the subgroups of age group (aged 18–34 years versus 35–64 years), sex, urban/rural status of patient residence, Census region of patient residence, and sub‐CVD diseases. We compared the changes in the numbers of telehealth and in‐person encounters per 100 patients before and during the pandemic for all and for subgroups.
Statistical Analysis
The month‐to‐month changes in the numbers of telehealth and in‐person encounters per 100 patients from February 2020 (the month before the pandemic) to June 2020 and the differences in the monthly estimates between February 2020 and June 2021 were tested using a Welch 2‐tailed t test for all and the subgroups. For both telehealth and in‐person outpatient encounters, the differences in the monthly estimates of the numbers per 100 patients with CVD between subgroups of age group, sex, and urbanicity were tested using a Welch 2‐tailed t test, and the differences among subgroups of Census region and sub‐CVD diseases were tested using a 1‐way ANOVA by each month to test the differences in the monthly estimates by subgroups. A P value <0.05 indicates statistical significance.
Trends in the Proportion of Telehealth to Total Outpatient Encounters
We calculated the proportion of telehealth to total outpatient encounters among all patients with CVD and by subgroups (age group, sex, urbanicity, 4 Census regions, and sub‐CVD diseases). The proportions were calculated by dividing the total number of telehealth outpatient encounters by the total number of outpatient encounters. The month‐to‐month changes in the proportions from February 2020 (the month before the pandemic) to June 2020 and the differences in the monthly estimates between February 2020 and June 2021 were tested using a Welch 2‐tailed t test for all and the subgroups. The differences in the monthly estimates of the proportions of telehealth encounters between subgroups of age group, sex, and urbanicity were tested using a Welch 2‐tailed t test, and the differences among subgroups of Census region and sub‐CVD diseases were tested using 1‐way ANOVA. A P value <0.05 indicates statistical significance.
Costs Associated With Telehealth and In‐Person Outpatient Encounters
Cost calculations were restricted to patients with CVD who were covered by noncapitated health insurance plans, because capitated health insurance plans had incomplete payment information (Figure 1). We reported total payments per encounter, patient out‐of‐pocket (OOP) payments per encounter, and share of patient OOP payments to total payments per encounter among patients with CVD for both telehealth and in‐person outpatient encounters, respectively, during the 12‐month study period of July 1, 2020 to June 30, 2021. Total payments include insurer's payments, coordination of benefits, and patient OOP payments. Patient OOP payments include copayment, coinsurance, and deductible. We reported the values and the bias‐corrected and accelerated bootstrap 95% CI of the variables.
We used Stata MP statistical software version 14.2 (StataCorp, College Station, TX) for the trend and cost calculations. We performed the data analysis in 2021 to 2022.
Results
Trends in the Number of Telehealth and In‐Person Outpatient Encounters per 100 Patients With CVD
From January 1, 2017 to June 30, 2021, a total of 474 811 patients with CVD met the inclusion criteria (Figure 1). The number of telehealth encounters per 100 patients with CVD was 0.30 in February 2020 and peaked at 25.4 in April 2020, fluctuated between 9.0 and 16.8 afterward, and ended at 9.0 in June 2021, higher than the prepandemic levels (Figure 2A). The trend patterns were similar for all subgroups by age group, sex, urbanicity, and Census region, where the peak was in April 2020 (Figure 2 and Table S1). For both telehealth and in‐person outpatient encounters, the month‐to‐month changes in the numbers per 100 patients with CVD from February 2020 to June 2020 were statistically significant for all and the subgroups (age group, sex, urbanicity, and Census region) (Tables S1 and S2). Those with CVD who were aged 18 to 34 years (versus 35–64 years), women (versus men), and living in urban areas (versus rural areas) had statistically significantly higher numbers of telehealth outpatient encounters per 100 patients with CVD from March 2020 to June 2021, with peak differences observed in April 2020.
Figure 2. Numbers of telehealth and in‐person outpatient encounters per 100 patients with cardiovascular disease and by age, sex, urbanicity, and Census region, sub‐CVD disease, MarketScan Commercial Claims and Encounters database, January 2019 to June 2021.
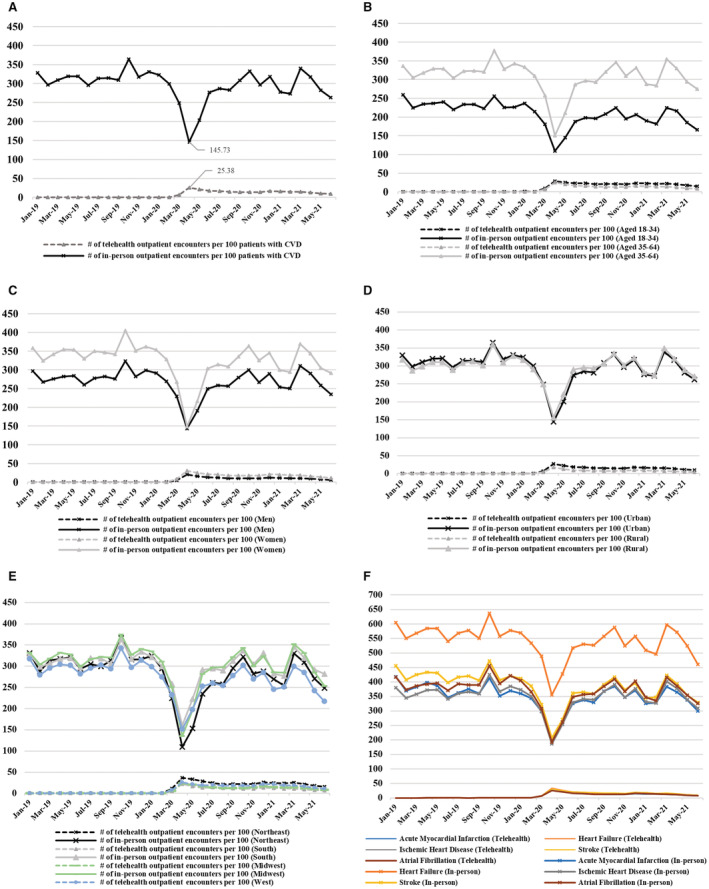
A, All samples. B, By age group. C, By sex. D, By urbanicity. E, By Census region. F, By sub‐CVD disease. On the y‐axis, we report the number of outpatient encounters per 100 patients diagnosed with CVD (ICD‐10‐CM code I00–I09, I16–I78) (A through E) and respective sub‐CVD diseases (F). Patients with CVD were defined if inpatient or emergency department encounters contained at least 1 diagnosis of CVD, or at least 2 outpatient encounters contained the diagnosis of CVD with at least a 30‐day interval during the 2 years of lookback periods from January 1, 2017 to December 31, 2018. CVD was defined after excluding hypertension alone (ICD‐10‐CM code I10‐I15) from CVD (ICD‐10‐CM code I00–I78). Out of 474 811 patients with CVD (Figure 1), 35 863 patients were aged 18 to 34 y, and 426 428 were aged 35 to 64 y; 234 107 patients were men, and 240 704 were women; 410 911 patients lived in urban regions, and 63 900 lived in rural regions; 72 859 patients lived in the Northeast; 244 384 patients lived in the South; 109 464 patients lived in the Midwest; and 47 176 patients lived in the West. There were 12 571 patients with acute myocardial infarction, 20 327 patients with heart failure, 81 082 patients with ischemic heart disease, 28 395 patients with strokes, and 32 599 patients with atrial fibrillation. For both telehealth and in‐person outpatient encounters, the differences in the monthly estimates of the numbers per 100 patients with CVD between subgroups of age group, sex, and urbanicity were tested using a Welch 2‐tailed t test, and the differences among subgroups of Census region and sub‐CVD diseases were tested using 1‐way ANOVA by each month to test the differences in the monthly estimates by subgroups. The corresponding numbers of telehealth and in‐person outpatient encounters per 100 patients with CVD and the test results are shown in Tables S1 and S2. CVD indicates cardiovascular disease; and ICD‐10‐CM, International Classification of Diseases, Tenth Revision, Clinical Modification.
The average number of in‐person outpatient encounters per 100 patients with CVD in February 2020 was 298.0.9, whereas the number was 145.7 in April 2020 (Figure 2A). The average numbers increased to 276.5 in June 2020, fluctuated between 263.2 and 340.0 afterward, and ended at 263.2 in June 2021, lower than the prepandemic levels (Table S2).
Trends in the Number of Telehealth and In‐Person Outpatient Encounters per 100 Patients With Sub‐CVD Diseases
Of the 474 811 patients with CVD (Figure 1), there were 12 571 patients with acute myocardial infarction, 20 327 patients with heart failure, 81 082 patients with ischemic heart disease, 28 395 patients with stroke, and 32 599 patients with atrial fibrillation. For both telehealth and in‐person outpatient encounters, the month‐to‐month changes in the numbers per 100 patients from February 2020 to June 2020 were statistically significant for each of the sub‐CVD diseases (acute myocardial infarction, heart failure, ischemic heart disease, stroke, and atrial fibrillation) (Tables S1 and S2). The differences between sub‐CVD diseases in the numbers of telehealth and in‐person outpatient encounters per 100 patients were statistically significantly different from March 2020 to June 2021 (Figure 2F and Tables S1 and S2).
Trends in the Proportion of Telehealth to Total Outpatient Encounters
The proportion of telehealth (to total outpatient) encounters among patients with CVD was 0.10% in February 2020 and peaked at 14.83% in April 2020 (Figure 3A and Table S3). The month‐to‐month changes in the proportions from February 2020 to June 2020 were statistically significant for all and the subgroups (by age group, sex, urbanicity, Census region, and sub‐CVD diseases) (Table S3). The proportions of telehealth encounters among patients with CVD peaked in April 2020 for all subgroups, where the proportion was statistically significantly higher for patients aged 18 to 34 years than for those aged 35 to 64 years (20.94% versus 14.24%, P<0.001), for women than men (17.09% versus 12.29%, P<0.001), and for those living in urban rather than in rural areas (15.61% versus 9.92%, P<0.001). The differences in the proportions by subgroups remained statistically different throughout the pandemic, from March 2020 to June 2021 (Table S3).
Figure 3. The proportion of telehealth outpatient encounters among patients with CVD by all subgroups: age, sex, urbanicity, Census region, and sub‐CVD disease during January 2019 to June 2021 using the MarketScan Commercial Claims and Encounters database.
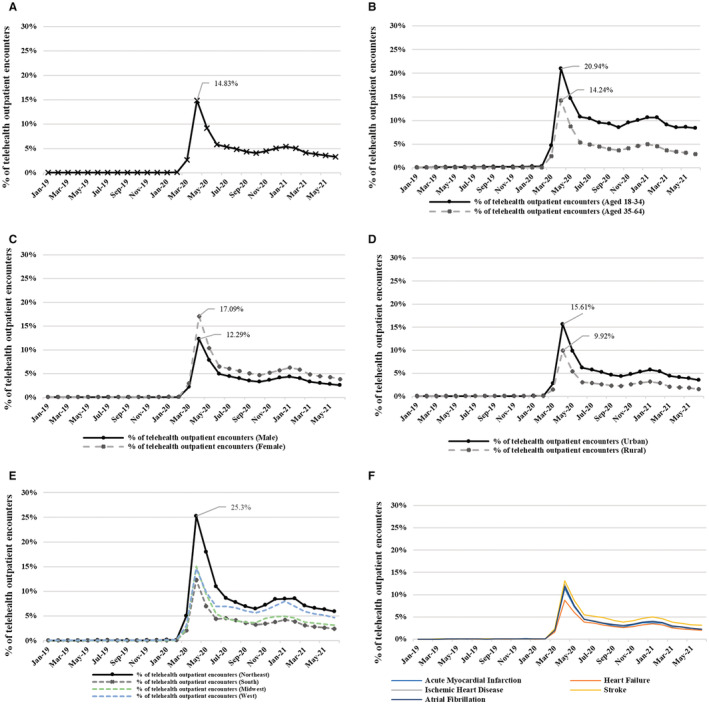
A, All samples. B, By age group. C, By sex. D, By urbanicity. E, By Census region. F, By sub‐CVD disease. On the y‐axis, we report the percent of telehealth outpatient encounters among patients with CVD (ie, the total number of telehealth outpatient encounters divided by the total number of outpatient encounters, then multiplied by 100). Out of 474 811 patients with CVD (Figure 1), 35 863 patients were aged 18 to 34 y, and 426 428 were aged 35 to 64 y; 234 107 patients were men, and 240 704 were women; 410 911 patients lived in urban regions, and 63 900 lived in rural regions; 72 859 patients lived in the Northeast; 244 384 patients lived in the South; 109 464 patients lived in the Midwest; and 47 176 patients lived in the West. There were 12 571 patients with acute myocardial infarction, 20 327 patients with heart failure, 81 082 patients with ischemic heart disease, 28 395 patients with all strokes, and 32 599 patients with atrial fibrillation. For both telehealth and in‐person outpatient encounters, the differences in the monthly estimates of the numbers per 100 patients with CVD between subgroups of age, sex, and urbanicity were tested using a Welch 2‐tailed t test, and the differences among subgroups of Census region and sub‐CVD diseases were tested using 1‐way ANOVA by each month to test the differences in the monthly estimates by subgroups. The test results are shown in Table S3. CVD indicates cardiovascular disease.
Costs of Telehealth and In‐Person Outpatient Encounters
A total of 320 857 out of 474 811 patients with CVD had noncapitated insurance from January 1, 2017 to June 30, 2021, and were included for cost calculations (Figure 1). Of the 320 857 patients, 119 689 patients had at least 1 telehealth outpatient encounter, and 308 130 patients had at least 1 in‐person encounter from July 2020 to June 2021 (TableTable).
Table 1.
Outpatient Visits and Payments for Telehealth and In‐Person Outpatient Encounters Among Patients With Cardiovascular Disease, MarketScan Commercial Claims and Encounters Database, July 2020 to June 2021
| Encounters | Mean (95% CI) |
|---|---|
| Telehealth encounters | |
| No. of telehealth encounters per patient | 4.2 (4.16–4.25) |
| Total payments per encounter | $113.1 ($112.8–$113.5) |
| Patient OOP payments per encounter | $23.8 ($23.6–$24.0) |
| Share of patient OOP payments to total payments per encounter | 23.2 (23.1–23.4) |
| Sample size, n | 119 689 |
| In‐person encounters | |
| No. of in‐person encounters per patient | 37.5 (37.3–37.7) |
| Total payments per encounter | $160.9 ($159.8–$161.8) |
| Patient OOP payments per encounter | $32.7 ($32.5–$32.8) |
| Share of patient OOP payments to total payments per encounter | 27.6 (27.5–27.7) |
| Sample size, n | 308 130 |
Cardiovascular disease (CVD) was defined after excluding hypertension diagnosis alone (ICD‐10‐CM codes I10–I15) from CVD (ICD‐10‐CM codes I00‐I78). Patients with CVD (ICD‐10‐CM codes I00–I09, I16–I78) were defined if inpatient or emergency department encounters contained at least 1 diagnosis of CVD, or at least 2 outpatient encounters contained the diagnosis of CVD with at least a 30‐day interval during the 2 years of lookback periods from January 1, 2017 to December 31, 2018. Of the 320 857 patients with CVD (Figure 1), 308 130 (or 96.0%) patients had at least 1 in‐person outpatient encounter, 119 689 (or 37.3%) patients had at least 1 telehealth encounter, 309 590 (or 96.5%) patients had at least 1 in‐person or telehealth encounter, 118 229 (or 36.8%) patients had both an in‐person and telehealth encounter, 1460 (or 0.5%) patients had only a telehealth outpatient encounter, 189 901 (or 59.2%) patients had only an in‐person outpatient encounter, and 11 267 (or 3.5%) patients did not have any in‐person or telehealth outpatient encounters during July 1, 2020 to June 30, 2021. Patients with telehealth outpatient encounters were defined in the following way: the place of service is equal to 2 in MarketScan data for telehealth; and procedure modifiers are equal to 95 for synchronous telemedicine service rendered via real‐time interactive audio and visual telecommunication system; equal to GO for telehealth services for diagnosis, evaluation, or treatment of symptoms of acute stroke; equal to GQ for telehealth service rendered via an asynchronous telecommunications system; and equal to GT for telehealth service rendered via interactive audio and video telecommunication systems. If outpatient encounters contained any of the above telehealth places of service or procedure modifiers from July 1, 2020 to June 30, 2021, we defined them as telehealth outpatient encounters. The cost calculation for in‐person outpatient encounters was defined by taking differences between total outpatient costs and total telehealth outpatient costs. Outpatient encounters were defined if settings contained nonphysician office visits, other outpatient office visits, specialty office visits, primary care physician office visits, or other outpatient (ie, all encounters excluding inpatient, emergency department, laboratory test, and pharmacy). Total payments for in‐person and telehealth were defined by the average payment per outpatient encounter for in‐person and telehealth encounters, respectively. The OOP payment share was the ratio of patients' OOP payments and total payments. The 95% CIs are the bias‐corrected and accelerated bootstrap 95% CIs with 1000 replications. ICD‐10‐CM indicates International Classification of Diseases, Tenth Revision, Clinical Modification; and OOP, out‐of‐pocket.
The mean (95% CI) number of telehealth encounters per patient with CVD was 4.2 (95% CI, 4.16–4.25) during the 12‐month study period, whereas the mean (95% CI) number of in‐person encounters per patient with CVD was 37.5 (95% CI, 37.3–37.7). The mean (95% CI) of total payments per telehealth encounter was $113.1 (95% CI, $112.8–$113.5), whereas the mean (95% CI) of total payments per in‐person encounter was $160.9 (95% CI, $159.8–$161.8). The mean (95% CI) of patient OOP payments per telehealth encounter was $23.8 (95% CI, $23.6–$24.0), whereas the mean (95% CI) of patient OOP payments per in‐person encounter was $32.7 (95% CI, $32.5–$32.8). The mean share of patient OOP payments to total payments per telehealth encounter was 23.2% (95% CI, 23.1%–23.4%), whereas the mean share of patient OOP payments to total payments per in‐person encounter was 27.6% (95% CI, 27.5%–27.7%).
Discussion
We documented the trends of telehealth use among patients with CVD before and during the pandemic from January 2019 to June 2021 using the MarketScan CCAE database. The number of telehealth encounters increased by >80 times from February 2020 to April 2020, whereas the number of in‐person outpatient encounters decreased by about half during the same time 2‐month period. During the same time period, the proportion of telehealth to total outpatient encounters increased from 0.1% to 14.8%. The increased number of telehealth encounters only partially offset the reduction in in‐person outpatient encounters. By June 2020, 3 months after after the pandemic was declared a national emergency, the number of in‐person outpatient encounters quickly rebounded afterward, although it was still about 6% lower than the prepandemic levels, and the proportion of telehealth to total outpatient encounters went down to 5.8% in June 2020 and fluctuated 3% to 5.4% afterward. Patients who were younger, women, and living in urban areas had higher use of telehealth than those who were older, men, and living in rural areas, respectively, throughout the pandemic. Overall, surveillance of telehealth use since the start of the COVID‐19 pandemic shows higher rates in urban areas, 19 , 20 and the findings from our study affirm a similar trend for patients with CVD. Additionally, our study shows that women and younger patients with CVD tended to use telehealth more frequently, which is consistent with trends for non–disease‐specific telehealth use. 21 The cost of outpatient encounters and patient OOP payments were higher for in‐person encounters than telehealth encounters, whereas the number of in‐person encounters was higher than the number of telehealth encounters. The findings of higher costs of in‐person than telehealth were consistent with a prior study on a different disease. 28 Costs of telehealth may be moderated by the expanded provisions and reimbursement for telehealth allowed by the Coronavirus Aid, Relief, and Economic Security Act. 29
Telehealth use trends for patients with CVD described in this study correspond with broader trends in telehealth during the same period 20 , 21 and align with timing of the initial community spread of COVID‐19 in the United States, the Centers for Medicare and Medicaid Services waivers for the use of telehealth, 30 and implementation of the Coronavirus Aid, Relief, and Economic Security Act. 21 , 29 Fluctuations in the use of telehealth among patients with CVD during the COVID‐19 pandemic may reflect patients adjusting their need for health care access and clinical care, and health systems adapting to patients' changing needs for care and using enhanced policy provisions for telehealth.
The Community Preventive Services Task Force recommends the use of telehealth to help address the needs of patients with CVD. 31 Furthermore, a 2017 policy statement from the American Heart Association recommended leveraging the use of evidence‐based strategies, such as remote patient monitoring and telestroke, to support the needs of patients with CVD. 32 As a result of these recommendations and the widespread use of telehealth during the COVID‐19 pandemic, more patients with CVD are receiving their care virtually than ever before. More work is required to understand the role and impact of telehealth on the nation's leading causes of morbidity and mortality; this study is a first step. Future studies may focus on either inpatient or outpatient settings, because the use and delivery of telehealth may differ substantially in each setting. Additional next steps include assessing the costs and use of telehealth services for condition‐specific and actionable cardiovascular issues, for example, hypertension, which is prevalent, costly, and manageable in an outpatient setting. 33 , 34 Further studies may also examine disparities in telehealth use by race and ethnicity, income, and other characteristics to better understand the equitability of access, use, cost, and outcomes related to telehealth. Finally, future work may examine health system, payer, or patient costs to document the economic impact of expanded telehealth use.
This study has 5 limitations. First, the MarketScan CCAE is a large convenient subsample of the employees and their dependents with employer‐sponsored private health insurance and is not representative of the privately insured population, while also excluding both those with public insurance (eg, through Medicare or Medicaid) and the uninsured. Second, recording errors may occur in claims data. If providers are less familiar with telehealth‐related coding, telehealth outpatient encounters might be over‐ or underestimated. Third, the study sample is limited to patients who had any outpatient, emergency department, or inpatient claim (regardless of reason for the encounter) and who reported having a CVD‐related diagnosis. Therefore, the outpatient encounters included in the analysis may not be to address CVD but to treat/manage entirely unrelated conditions. Fourth, the period of our cost calculations (July 1, 2020–June 30, 2021) occurred during the time in the pandemic when the Centers for Medicare and Medicaid Services telehealth waivers 30 and Coronavirus Aid, Relief, and Economic Security Act 29 temporarily institutionalized flexibilities for billing of telehealth visits and for copays and other costs incurred by patients. As a result, this analysis reflects the costs of telehealth services only during the public health emergency and does not summarize historical costs or project future costs for telehealth visits for patients with CVD. Fifth, we restricted our analysis to patients who have been continuously covered by insurance before and during the pandemic. Consequently, our results do not capture those who lost coverage because of disruptions in their jobs, stay‐at‐home orders, or other causes. Future studies may address these limitations by exploring trends and use among publicly insured patients or by examining trends and use of telehealth for patients with CVD for encounters related to managing their condition.
Conclusions
Telehealth use among a large sample of privately insured patients diagnosed with CVD increased rapidly during the first 2 months of the COVID‐19 pandemic, increasing from <0.1% to 14.8% of all outpatient encounters between February 2020 and April 2020. However, the share of telehealth use dropped as rapidly to 5.8% by June 2020 and fluctuated in a range of 3% to 5.4% over the remaining 12 months, which is slightly higher compared with the prepandemic period. Telehealth encounters had a lower average cost compared with in‐person encounters in July 2020 to June 2021. The temporary telehealth provisions put in place during the COVID‐19 public health emergency remain, and policymakers, health systems, health services researchers, and insurers may benefit from information about telehealth use and costs among patients with CVD for decisions about drivers of telehealth use and sustainability.
Sources of Funding
None.
Disclosures
None.
Supporting information
Tables S1–S3
Acknowledgments
The authors are genuinely grateful to F. Loustalot, X. Tong, Q. Yang, and S. L. Jackson (Centers for Disease Control and Prevention) for their guidance, suggestions, and article review. The authors appreciate F. Coronado, K. Roy, K. E. MacLeod, and R. Schwartz (Centers for Disease Control and Prevention) for their thorough review and meaningful advice to improve the quality of the article. Thank you K. Miller (Merative) for your technical guidance and support. The findings and conclusions in this article are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention. Use of trade names and commercial sources is for identification only and does not imply endorsement by the US Department of Health and Human Services.
Supplemental Material is available at https://www.ahajournals.org/doi/suppl/10.1161/JAHA.122.028713
For Sources of Funding and Disclosures, see page 10.
REFERENCES
- 1. Moreland A, Herlihy C, Tynan MA, Sunshine G, McCord RF, Hilton C, Poovey J, Werner AK, Jones CD, Fulmer EB, et al. Timing of state and territorial COVID‐19 stay‐at‐home orders and changes in population movement ‐ United States, March 1–May 31, 2020. MMWR Morb Mortal Wkly Rep. 2020;69:1198–1203. doi: 10.15585/mmwr.mm6935a2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. NHS England. Operating framework for urgent and planned services in hospital settings during COVID‐19, 2020 . Accessed October 16, 2021. https://covidlawlab.org/wp‐content/uploads/2020/06/Operating‐framework‐for‐urgent‐and‐planned‐services‐within‐hospitals.pdf
- 3. D'Aeth JC, Ghosal S, Grimm F, Haw D, Koca E, Lau K, Moret S, Rizmie D, Deeny SR, Perez‐Guzman PN. Optimal national prioritization policies for hospital care during the SARS‐CoV‐2 pandemic. Nat Comput Sci. 2021;1:521–531. doi: 10.1038/s43588-021-00111-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Czeisler MÉ, Marynak K, Clarke KE, Salah Z, Shakya I, Thierry JM, Ali N, McMillan H, Wiley JF, Weaver MD. Delay or avoidance of medical care because of COVID‐19–related concerns—United States, June 2020. Morb Mortal Wkly Rep. 2020;69:1250–1257. doi: 10.15585/mmwr.mm6936a4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Riera R, Bagattini ÂM, Pacheco RL, Pachito DV, Roitberg F, Ilbawi A. Delays and disruptions in cancer health care due to COVID‐19 pandemic: systematic review. JCO Glob Oncol. 2021;7:311–323. doi: 10.1200/GO.20.00639 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Wong MYZ, Gunasekeran DV, Nusinovici S, Sabanayagam C, Yeo KK, Cheng C‐Y, Tham Y‐C. Telehealth demand trends during the COVID‐19 pandemic in the top 50 most affected countries: infodemiological evaluation. JMIR Public Health Surveill. 2021;7:e24445. doi: 10.2196/24445 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Centers for Medicare & Medicaid Services . Current emergencies. Accessed October 16, 2021. https://www.cms.gov/About‐CMS/Agency‐Information/Emergency/EPRO/Current‐Emergencies/Current‐Emergencies‐page
- 8. US Department of Health and Human Services . New HHS Study shows 63‐fold increase in Medicare telehealth utilization during the pandemic. Accessed January 13, 2022. https://www.hhs.gov/about/news/2021/12/03/new‐hhs‐study‐shows‐63‐fold‐increase‐in‐medicare‐telehealth‐utilization‐during‐pandemic.html
- 9. Centers for Medicare & Medicaid Services . FAQs on availability and usage of telehealth services through private health insurance coverage in response to coronavirus disease 2019 (COVID‐19). Accessed October 16, 2021. https://www.cms.gov/files/document/faqs‐telehealth‐covid‐19.pdf
- 10. Parisien RL, Shin M, Constant M, Saltzman BM, Li X, Levine WN, Trofa DP. Telehealth utilization in response to the novel coronavirus (COVID‐19) pandemic in orthopaedic surgery. J Am Acad Orthop Surg. 2020;28:e487–e492. doi: 10.5435/JAAOS-D-20-00339 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Chao GF, Li KY, Zhu Z, McCullough J, Thompson M, Claflin J, Fliegner M, Steppe E, Ryan A, Ellimoottil C. Use of telehealth by surgical specialties during the COVID‐19 pandemic. JAMA Surg. 2021;156:620–626. doi: 10.1001/jamasurg.2021.0979 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Der‐Martirosian C, Wyte‐Lake T, Balut M, Chu K, Heyworth L, Leung L, Ziaeian B, Tubbesing S, Mullur R, Dobalian A. Implementation of telehealth services at the US Department of Veterans Affairs during the COVID‐19 pandemic: mixed methods study. JMIR Form Res. 2021;5:e29429. doi: 10.2196/29429 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Lonergan PE, Washington Iii SL, Branagan L, Gleason N, Pruthi RS, Carroll PR, Odisho AY. Rapid utilization of telehealth in a comprehensive cancer center as a response to COVID‐19: cross‐sectional analysis. J Med Internet Res. 2020;22:e19322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Cantor JH, McBain RK, Pera MF, Bravata DM, Whaley CM. Who is (and is not) receiving telemedicine care during the COVID‐19 pandemic. Am J Prev Med. 2021;61:434–438. doi: 10.1016/j.amepre.2021.01.030 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. National Center for Health Statistics . Multiple cause of death 1999–2020 on CDC WONDER Online Database website. Accessed February 21, 2022. https://wonder.cdc.gov/mcd‐icd10.html
- 16. Tsao CW, Aday AW, Almarzooq ZI, Alonso A, Beaton AZ, Bittencourt MS, Boehme AK, Buxton AE, Carson AP, Commodore‐Mensah Y. Heart disease and stroke statistics—2022 update: a report from the American Heart Association. Circulation. 2022;145:e153–e639. doi: 10.1161/CIR.0000000000001052 [DOI] [PubMed] [Google Scholar]
- 17. Reynolds R, Dennis S, Hasan I, Slewa J, Chen W, Tian D, Bobba S, Zwar N. A systematic review of chronic disease management interventions in primary care. BMC Fam Pract. 2018;19:1–13. doi: 10.1186/s12875-017-0692-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Centers for Disease Control and Prevention . People with Certain Medical Conditions. Accessed November 15, 2021. https://www.cdc.gov/coronavirus/2019‐ncov/need‐extra‐precautions/people‐with‐medical‐conditions.html.
- 19. Demeke HB, Pao LZ, Clark H, Romero L, Neri A, Shah R, McDow KB, Tindall E, Iqbal NJ, Hatfield‐Timajchy K. Telehealth practice among health centers during the COVID‐19 pandemic—United States, July 11–17, 2020. Morb Mortal Wkly Rep. 2020;69:1902–1905. doi: 10.15585/mmwr.mm6950a4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Demeke HB, Merali S, Marks S, Pao LZ, Romero L, Sandhu P, Clark H, Clara A, McDow KB, Tindall E. Trends in use of telehealth among health centers during the COVID‐19 pandemic—United States, June 26–November 6, 2020. Morb Mortal Wkly Rep. 2021;70:240–244. doi: 10.15585/mmwr.mm7007a3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Koonin LM, Hoots B, Tsang CA, Leroy Z, Farris K, Jolly B, Antall P, McCabe B, Zelis CB, Tong I. Trends in the use of telehealth during the emergence of the COVID‐19 pandemic—United States, January–March 2020. Morb Mortal Wkly Rep. 2020;69:1595–1599. doi: 10.15585/mmwr.mm6943a3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Truven Health MarketScan® Research Databases . Accessed November 9, 2022. https://marketscan.truvenhealth.com/marketscanportal
- 23. Gold JA, Kiernan E, Yeh M, Jackson BR, Benedict K. Health care utilization and outcomes associated with accidental poisonous mushroom ingestions—United States, 2016–2018. Morb Mortal Wkly Rep. 2021;70:337–341. doi: 10.15585/mmwr.mm7010a1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Lee J, Joo H, Maskery BA, Alpern JD, Park C, Weinberg M, Stauffer WM. Increases in anti‐infective drug prices, subsequent prescribing, and outpatient costs. JAMA Netw Open. 2021;4:e2113963. doi: 10.1001/jamanetworkopen.2021.13963 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Joo H, Lee J, Maskery BA, Park C, Alpern JD, Phares CR, Weinberg M, Stauffer WM. The effect of drug pricing on outpatient payments and treatment for three soil‐transmitted helminth infections in the United States, 2010–2017. Am J Trop Med Hyg. 2021;104:1851–1857. doi: 10.4269/ajtmh.20-1452 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Meyers J, Hoog M, Mody R, Yu M, Davis K. The health care resource utilization and costs among patients with type 2 diabetes and either cardiovascular disease or cardiovascular risk factors an analysis of a US health insurance database. Clin Ther. 2021;43:1827–1842. doi: 10.1016/j.clinthera.2021.09.003 [DOI] [PubMed] [Google Scholar]
- 27. Division for Heart Disease and Stroke Prevention . Data Sources ‐ Heart Disease and Stroke Data. Accessed March 3, 2022. https://www.cdc.gov/dhdsp/maps/atlas/data‐sources.html
- 28. Ashwood JS, Mehrotra A, Cowling D, Uscher‐Pines L. Direct‐to‐consumer telehealth may increase access to care but does not decrease spending. Health Aff (Millwood). 2017;36:485–491. doi: 10.1377/hlthaff.2016.1130 [DOI] [PubMed] [Google Scholar]
- 29. Coronavirus Aid, Relief, and Economic Security (CARES) Act, Pub. L. 116‐36, 134 Stat. 2811 (Mar. 27, 2020) . Accessed January 20, 2022. https://www.congress.gov/bill/116th‐congress/house‐bill/748/text
- 30. US Department of Health and Human Services . COVID‐19 emergency declaration blanket waivers for health care providers. Accessed January 20, 2022. https://www.cms.gov/files/document/covid19‐emergency‐declaration‐health‐care‐providers‐fact‐sheet.pdf
- 31. Guide to Community Preventive Services . TFFRS ‐ cardiovascular disease prevention: interactive digital interventions for blood pressure self‐management. Accessed September 14, 2020. https://www.thecommunityguide.org/content/tffrs‐cardiovascular‐disease‐prevention‐interactive‐digital‐interventions‐blood‐pressure
- 32. Schwamm LH, Chumbler N, Brown E, Fonarow GC, Berube D, Nystrom K, Suter R, Zavala M, Polsky D, Radhakrishnan K. Recommendations for the implementation of telehealth in cardiovascular and stroke care: a policy statement from the American Heart Association. Circulation. 2017;135:e24–e44. doi: 10.1161/CIR.0000000000000475 [DOI] [PubMed] [Google Scholar]
- 33. Centers for Disease Control and Prevention . Hypertension cascade: hypertension prevalence, treatment and control estimates among U.S. Adults aged 18 years and older applying the criteria from the American College of Cardiology and American Heart Association's 2017 hypertension guideline—NHANES 2015–2018. U.S. Department of Health and Human Services; 2021. [Google Scholar]
- 34. Kirkland EB, Heincelman M, Bishu KG, Schumann SO, Schreiner A, Axon RN, Mauldin PD, Moran WP. Trends in healthcare expenditures among US adults with hypertension: national estimates, 2003–2014. J Am Heart Assoc. 2018;7:e008731. doi: 10.1161/JAHA.118.008731 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Tables S1–S3


