Abstract
Background
We previously outlined the importance of considering acculturation within the context of older Latino adults' lived experience (ie, acculturation in context) to better capture contributors to cognitive aging. We now examine this conceptual framework as related to level of and change in cardiovascular health, and whether cardiovascular health modifies previously documented associations of acculturation in context with cognition.
Methods and Results
Acculturation in context data from 192 Latino participants without dementia at baseline (age ~70 years) were compiled into 3 separate composite scores: acculturation‐related (nativity, language‐, and social‐based preferences), contextually related socioenvironmental (experiences of discrimination, social isolation, social networks), and familism‐related (Latino‐centric family ethos). A modified American Heart Association's Life's Simple 7 (mLS7; ie, smoking, physical activity, body mass index, blood pressure, total cholesterol, blood glucose) was used to measure cardiovascular health. Mixed effects regressions simultaneously tested the association of all 3 composite scores with total mLS7 adjusting for confounders. Separate models tested whether mLS7 modified associations of the 3 composite scores and cognition. The contextually related socioenvironmental composite score reflecting higher discrimination, higher social isolation, and smaller social networks (estimate=0.22, SE=0.10, P=0.02) and the familism score (estimate=0.16, SE=0.07, P=0.02) both significantly associated with change in total mLS7. The acculturation‐related composite was not significantly associated with change in mLS7. No composite was significantly associated with level of mLS7. Total mLS7, however, significantly modified associations between the acculturation‐related composite and change in working memory (estimate=−0.02, SE=0.01, P=0.043).
Conclusions
Acculturation within the context of older Latino adults' lived experience is important for maintaining cardiovascular health, relationships that also affect domain‐specific cognitive decline.
Keywords: acculturation, cognition, Latino adults, Life's Simple 7, social determinants of health
Subject Categories: Aging, Race and Ethnicity, Risk Factors
Clinical Perspective.
What Is New?
To address prior mixed results of studies investigating acculturation (primarily based on nativity and language‐based metrics) and cardiovascular health in Latino adults, we examined the relationship between acculturation in the context of Latino adults' lived experience (eg, social support and experiences of discrimination) and level of as well as change in cardiovascular health (ie, Life's Simple 7).
Our results suggest that socioenvironmental and Latino‐centric aspects of acculturation contribute to change in (more so than level of) cardiovascular health, and, when taken together, affect cognitive decline in older Latino adults.
What Are the Clinical Implications?
Clinicians should query acculturation and lived experiences when evaluating cardiovascular health in older Latino adults.
Brain health is an important component of successful aging, as is cardiovascular health. In fact, declines in age‐specific incidence rates of Alzheimer's disease and related dementias in the United States may be due, in part, to improvements in cardiovascular health. 1 , 2 Cardiovascular health may be quantified using The American Heart Association's (AHA) Life's Simple 7 (LS7) 3 that considers ideal, intermediate (ie, average), or poor levels of AHA‐defined health behaviors (ie, smoking status, physical activity, and ranges of body mass index) as well as AHA‐defined biological factors (ie, blood pressure, blood glucose, and total cholesterol). LS7 has been cited as an ideal metric to study successful brain aging given the role of cardiovascular health in preserving cognition across the lifespan. 1 Multiple large‐scale epidemiological studies in primarily non‐Latino White older adults have reported that higher LS7 scores, indicative of better cardiovascular health, are independently associated with better cognitive functioning and lower risk of dementia. 4 , 5 , 6 , 7 Of the few predominantly or exclusively Latino cardiovascular health and cognition studies, results suggest that higher baseline LS7 scores were associated with higher baseline levels of 8 and fewer declines in 9 cognition. Although these studies are important, evidence suggests that culturally relevant factors are associated with Latino adults' cardiovascular health, 10 and this should be incorporated into research within this population.
Acculturation, that is, the process of adapting to a new environment and potentially adopting its values and practices, is a culturally relevant construct that has been associated with many cardiovascular health factors in the Latino population in both positive and negative ways; however, this acculturation‐related work has primarily been cross‐sectional and more consistently focused on AHA‐defined biological factors than AHA‐defined health behaviors. For example, some studies report that Latino adults with lower levels of acculturation to the United States—quantified by non‐US‐based nativity, shorter length of residence in the United States, later age at immigration, and/or Spanish language‐based preferences—have lower levels of cardiovascular risk when considering the presence/absence of hypertension, diabetes, hypercholesterolemia, obesity, and smoking 11 , 12 , 13 ; other studies report associations in the opposite direction, 14 , 15 and still others report no relationship. 16 , 17 Mixed results have also been reported for the associations of acculturation with dietary patterns, 13 , 18 with less work focused on acculturation and older Latino adults' physical activity levels. 19 Only 1 study directly assessed the relationship between acculturation and cardiovascular health using the AHA's LS7, reporting that, for a multiethnic cohort (22% Latino), higher levels of acculturation to the United States (ie, US nativity, longer length of residence in the United States, and speaking English in the home) were associated with lower odds of having average to ideal cardiovascular health. 20
Mixed results regarding the relationship between acculturation and cardiovascular health may be due, in part, to the fact that the acculturation‐related measures employed were often investigated in isolation, focused primarily on nativity and language‐based metrics, and did not take into consideration that acculturation is multifaceted and context dependent. 21 , 22 , 23 , 24 , 25 In fact, a relatively recent study reported that psychologically based measures of acculturation that pertain to an individual's lived experience were more robustly associated with a healthier diet than residence‐ or language‐based metrics of acculturation. 18 We recently described acculturation within the context of the lived experience of Latino adults living in the United States taking into consideration not only key social determinants of health like experiences of discrimination, but also key Latino‐centric considerations (eg, the importance of family) as they contributed to cognitive aging profiles of older Latino adults. 26 We did not, however, examine these factors as related to Latino adults' cardiovascular health.
In the current study, we examined the relationship between acculturation in the context of Latino adults' lived experience (ie, acculturation in context) and level of as well as change in cardiovascular health among older Latino adults without dementia at baseline participating in 1 of 2 Rush Alzheimer's Disease Center cohort studies. Previous studies in non‐Latino Black and White adults have reported that lower levels of self‐reported discrimination 27 and higher levels of social support/networks 28 were independently associated with more ideal (ie, better) AHA‐defined cardiovascular health. Work in a combined cohort of Latino, European, and East Asian Americans suggests that a greater emphasis on family and family ties (akin to Latino‐centric considerations regarding the importance of family, also known as “familism”) is related to higher health ratings. 29 Based on results of these studies and those discussed here, we hypothesized that acculturation‐related (ie, nativity, language‐, and social‐based metrics of acculturation), contextually related social determinants of health (ie, experiences of discrimination, social support, and social networks), and familism‐related aspects of our acculturation in context framework 26 would be differentially related to level of and change in cardiovascular health as measured by LS7. Furthermore, we explored whether LS7 modified previously documented 26 associations between these same aspects of our acculturation in context framework and cognition in older Latino adults.
METHODS
All data and materials can be found at the Rush Alzheimer's Disease Center Research Resource Sharing Hub (www.radc.rush.edu).
Participants
Participants were self‐identified Latino adults enrolled in either the Rush MAP (Memory and Aging Project) 30 or the Rush Alzheimer's Disease Center Latino Core. 31 These ongoing longitudinal cohort studies began in 1997 and 2015, respectively, as community‐based studies of aging recruiting from a variety of settings in and around Chicago. Both studies are identical in essential details (eg, overlapping and standardized evaluations of acculturation in context, cardiovascular health, and cognition). Specifically, they enroll older Latino adults free of known dementia at baseline who agree to annual, in‐home evaluations conducted by bilingual investigators with a single population studies team and trainer to ensure data can be efficiently merged and compared across cohorts. Both studies were approved by an institutional review board of Rush University Medical Center and participants gave written informed consent in accordance with the Declaration of Helsinki.
At the time of these analyses, 256 Latino participants had completed their baseline evaluation. We excluded 5 participants who received a diagnosis of dementia at the time of their baseline evaluation, which was determined via a uniform structured clinical evaluation 32 and National Institute of Neurological and Communicative Diseases and Stroke/Alzheimer's Disease and Related Disorders Association criteria. 33 We further excluded 7 participants missing data on key variables required for the LS7 calculation. An additional 52 participants who had not yet reached their first longitudinal follow‐up visit were also excluded. This left 192 individuals with a mean follow‐up of 3.3 years contributing to our analyses.
Acculturation in Context
As previously outlined, 26 we chose acculturation in context metrics that reflected acculturation‐ and contextually related factors outlined in the literature as important to the lived experience of Latino adults 21 , 22 , 23 , 24 , 25 and were aligned with the National Institute on Aging Health Disparities Research Framework. 34 Based on previously reported unrotated factor loadings, 26 we created 3 acculturation in context composite scores. The item‐level data that were included in each composite were as follows: the acculturation‐related composite included nativity status (based on country of origin documented separately for participants [United States or non‐United States] and their parents [neither parent, 1 parent, or both parents born outside mainland United States]), total and domain‐specific language‐ and social‐based acculturation scores from the Short Acculturation Scale for Hispanics, 35 and participants' language preference for testing (English or Spanish); the contextually related socioenvironmental composite included scores from the Williams Everyday Discrimination Scale, 36 a modified 5‐item version of the de Jong‐Gierveld Loneliness Scale assessing social isolation, 37 and an evaluation of social network size 38 ; and the familism composite was composed of only 1 item‐level data point: the total score of the 6‐item Sabogal Familism Measure. 39 Raw scores from these 10 metrics were converted to standard Z scores using the baseline mean (SD) of the entire sample. Select Z scores were multiplied by −1 to ensure that a higher score reflected higher levels of acculturation to the United States or higher exposure to an adverse contextually related socioenvironmental milieu. Higher familism scores reflected higher levels of identification and attachment of an individual to their family.
American Heart Association's Life's Simple 7
Information necessary to quantify a modified version of the AHA's LS7 score 3 was derived from the annual interview, self‐reported medical history and physical, as well as the annual visual inspection, identification, and coding of medications according to the Master Drug Data Base System (MediSpan). As outlined in Table 1, we derived a modified LS7 score (mLS7) comprising 3 of the 4 health behaviors (we did not have a measure of overall diet quality) and all 3 biological factors as delineated by the AHA.
Table 1.
Modified American Heart Association's Life's Simple 7 as Applied in This Study
| Ideal (2 points) | Intermediate/average (1 point) | Poor (0 points) | |
|---|---|---|---|
| Health behaviors | |||
| Smoking (self‐report) | Never or quit>12 mo | Former ≤12 mo | Current |
| Physical activity (self‐report) | ≥150 min/week moderate | 1 to 149 min/week moderate | None |
| Body mass index | 18.5 to <25 kg/m2 | 25 to <30 kg/m2 | ≥30 kg/m2 |
| Biological factors | |||
| Blood pressure (average of 3 readings) | <120/<80 mm Hg without medication | SBP 120 to 139 or DBP 80 to 89 or treated to <120/<80 mm Hg | SBP≥140 or DBP≥90 mm Hg |
| Total cholesterol | <200 mg/dL without medications | 200–239 or treated to <200 mg/dL | ≥240 mg/dL |
| Fasting blood glucose* | <100 mg/dL without medication | 100 to 125 mg/dL or treated <100 mg/dL | ≥126 mg/dL |
DBP indicates diastolic blood pressure; and SBP, systolic blood pressure.
Random levels accommodated for participants with nonfasting venipunctures.
Health behaviors were measured as follows: smoking status was defined via self‐report (0=never, 1=former, 2=current) 40 with additional questions probing the age a participant last smoked “regularly.” Physical activity was evaluated using questions adapted from the National Health Interview Survey and summed the hours per week (transposed into minutes for mLS7 derivation) that participants engaged in 5 categories of activities including walking, gardening, calisthenics, bicycle riding, and swimming/water exercises. 41 Body mass index was calculated using the formula kg/m2. Biological factors were measured either by a trained research assistant who measured systolic and diastolic blood pressure in participants' right arm using an Omron automated blood pressure machine (twice seated and once standing) 42 or by Quest Diagnostics who performed analyses of total glucose and cholesterol levels via venipuncture‐obtained blood draws; fasting status (yes/no) was documented at the time of blood draw. All relevant medication use for biological factors was documented using MediSpan. Each of the 6 items was scored based on the criteria outlined in Table 1 for ideal (2 points), intermediate/average (1 point), or poor (0 points) cardiovascular health. All item scores were summed to create the mLS7 total score (range: 0 to 12); health behaviors (range: 0 to 6) and biological factors (range: 0 to 6) were summed to create mLS7 subscores. Across all 3 variables of interest, a higher score reflected better cardiovascular health.
Cognition
All participants underwent a cognitive evaluation administered in an identical fashion at annual evaluations and conducted in the participant's preferred language, Spanish or English. 31 Nineteen tests assessed the following 5 cognitive domains: episodic memory, semantic memory, working memory, perceptual speed, and visuospatial ability. In addition to domain‐specific Z scores derived by converting all raw test scores to standard scores using the baseline mean and SD of the entire cohort and then averaging the Z scores of all tests for each domain, we created a global cognitive function score averaging an individual's standard scores across all 19 test scores. Psychometric properties of these summary scores have been deemed adequate, 43 and the list of individual test items included in each cognitive domain may be found in Table S1.
Covariates
In addition to age, sex, and education, we adjusted for depressive symptomatology given its potential to confound the association between acculturation in context and cardiovascular health. A 10‐item version of the Center for Epidemiologic Studies of Depression Scale 44 assessed depressive symptoms with a higher score reflecting a higher number of symptoms experienced (maximum=10).
Statistical Analysis
All analyses were conducted using SAS/STAT software, Version 9.4 of the SAS System for Linux (SAS Institute, Cary, NC), and statistical significance was set at P<0.05 unless otherwise noted.
Descriptive summaries of all variables of interest including covariates were conducted for the analytic sample. Linear mixed effects regressions were used to test the association of all 3 acculturation in context composite scores (acculturation‐related, contextually related, and familism) with baseline level and longitudinal change in cardiovascular health (mLS7 total score). Models included terms for the 3 acculturation in context composite scores, age, sex, education, and Center for Epidemiologic Studies of Depression Scale‐10, as well as time‐in‐study and interactions of each variable with time. Given that the familism scale was introduced after the other acculturation in context measures, it was missing in 53 participants; thus, the sample size for analyses including this variable were reduced.
Where relevant, we followed these analyses with an investigation of mLS7 health behaviors and biological factors subscores as separate outcomes. Given that the distributions of these 2 subscores reflected sparse observations at the end of the ordinal distribution, we combined lower scores and recalibrated all remaining scores. 45 Thus, scores of 0, 1, or 2 for health behaviors were combined and the subscore recalibrated to a range of 0 to 4 (higher=more ideal); scores of 0 or 1 for biological factors were combined and the subscore recalibrated to a range of 0 to 5 (higher=more ideal). Ordinal mixed effects models assuming proportionality of odds 46 were then used to assess the association of all 3 acculturation in context composite scores with the odds of having higher level of and slower change in each of the recalibrated subscores separately adjusting for the same confounders noted previously.
Finally, to explore whether mLS7 modified the effect of previously documented associations between acculturation in context composite scores and cognition, the original mixed effects regression model outlined previously was augmented with terms for mLS7 total, its interaction with time, and its 3‐way interaction with each of the 3 acculturation in context composite scores; global cognition and the 5 domain‐specific cognitive composite scores became the separate outcome variables of interest.
RESULTS
Participants (N=192) were on average 70 years of age, primarily female, with an average education of nearly 11 years. Participants' mLS7 total scores were approximately 7 out of a possible 12 suggesting intermediate or average levels of cardiovascular health. Additional baseline characteristics are outlined in Table 2. There were no significant differences in key participant characteristics (ie, age, sex, education, or depressive symptomatology) between Latino participants with and without familism scores (P≥0.06; Table S2).
Table 2.
Participant Characteristics at Baseline
| N=192 | |
|---|---|
| Age, y | 69.7 (6.6) |
| Sex, male:female ratio | 37:155 |
| Education, y | 10.9 (4.7) |
| Center for Epidemiologic Studies of Depression Scale 10‐item version | 1.7 (2.1) |
| Acculturation in context | |
| Acculturation‐related composite | 0.08 (0.87) |
| Contextually related socioenvironmental composite | −0.006 (0.69) |
| Familism | −0.01 (1.0) |
| Modified Life's Simple 7 (mLS7) | |
| mLS7 total score (max=12) | 7.37 (1.81) |
| Health behaviors subscore (max=6) | 3.95 (1.27) |
| Biological factors subscore (max=6) | 3.42 (1.22) |
All values are mean (SD) unless otherwise noted.
Acculturation in Context and mLS7
The mixed effects regression simultaneously testing the association of all 3 acculturation in context composite scores with level of and change in total mLS7 adjusting for age, sex, education, and depressive symptomatology as well as their interactions with time resulted in significant associations of higher contextually related socioenvironmental composite scores and higher levels of familism with faster increases in mLS7 scores over time (P≤0.024; Table 3 and Figure 1). Follow‐up analyses investigating mLS7 health behavior and biological factor subscores as separate outcomes did not enlighten the seemingly paradoxical positive association between the contextually related socioenvironmental composite representing higher self‐reported experiences of discrimination, social isolation, and smaller social networks together as a composite score and improvement over time in overall cardiovascular health; however, they did reveal that the relationship between higher levels of self‐reported identification/attachment to family (ie, familism) and improvement over time in overall cardiovascular health was driven by faster increases in the health behavior subscore reflecting smoking status, physical activity levels, and body mass index profiles (estimate=0.31, SE=0.14, P=0.029). The acculturation‐related composite score was not significantly associated with change in total mLS7 (Table 3). None of the acculturation in context variables significantly associated with baseline level of mLS7.
Table 3.
Associations of Acculturation in Context Composite Scores With Cardiovascular Health as Measured by Modified Life's Simple 7 (mLS7)
| Composite scores | mLS7 total score | mLS7 subscores | |
|---|---|---|---|
| Health behaviors | Biological factors | ||
| Acculturation‐related factors |
0.12 (0.22) P=0.56 |
0.05 (0.44) P=0.90 |
0.65 (0.43) P=0.13 |
| Socioenvironmental factors |
0.02 (0.22) P=0.91 |
−0.32 (0.43) P=0.45 |
0.34 (0.42) P=0.41 |
| Familism |
−0.10 (0.16) P=0.50 |
0.01 (0.30) P=0.97 |
−0.16 (0.30) P=0.59 |
| Acculturation‐related factors×time |
−0.08 (0.11) P=0.45 |
−0.20 (0.20) P=0.32 |
−0.18 (0.21) P=0.38 |
| Socioenvironmental factors×time |
0.22 (0.10) P=0.024* |
0.20 (0.19) P=0.27 |
0.25 (0.18) P=0.19 |
| Familism×time |
0.16 (0.07) P=0.020* |
0.31 (0.14) P=0.029* |
0.18 (0.13) P=0.16 |
Values are unstandardized coefficient (SE), P value from fully adjusted linear (mLS7 total) or ordinal (mLS7 health behaviors and biological factors subscores) mixed effects models (3 models in total represented by the 3 columns) including additional terms for time (in study) as well as age, sex, education, depressive symptomatology, and interactions of these variables with time.
Denotes significance at P<0.05.
Figure 1. Representation of the associations of acculturation in context composite scores of the contextually related socioenvironment (left panel), and familism (right panel) with level of the modified Life's Simple 7 (mLS7) total score (represented as the point of each composite score at 0.0 on the x axis) as well as change in mLS7 total score (represented by the entirety of the lines) in fully adjusted models accounting for age, sex, education, time‐in‐study, CESD‐10, and interactions of each variable with time.
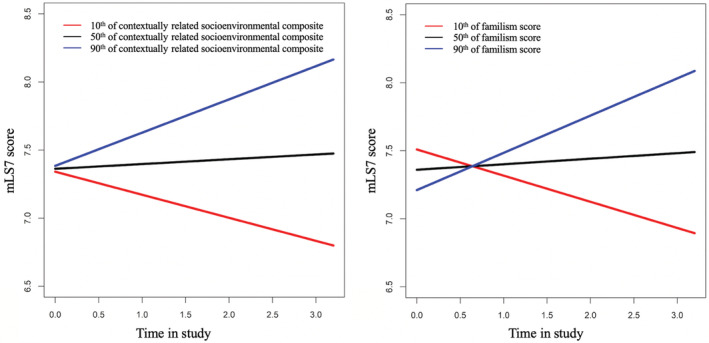
Figures display the estimated mean composite mLS7 total scores for participants in 3 percentiles, that is, 10th (red line), 50th (black line), and 90th (blue line), with all other terms in the model held constant (ie, continuous variables were centered, and sex was female) for ease of interpretation. The acculturation‐related composite score is not represented as it was not associated with level of or change in mLS7 total score. CESD‐10 indicates 10‐item Center for Epidemiologic Studies of Depression Scale.
Post Hoc Analyses
Given the somewhat paradoxical finding that higher levels of the contextually related socioenvironmental composite score, reflecting greater self‐reported experiences of discrimination and social isolation as well as smaller social networks, were associated with improvements in overall cardiovascular health over time, we investigated the individual items that comprised the contextually related socioenvironmental composite to determine which component(s) may have been driving the aforementioned result (Table 4). Although no one item was significantly associated with level of or change in the total mLS7 (P≥0.32), individuals reporting a smaller network size (higher score=smaller network; raw score multiplied by −1 to ensure that a higher score reflected higher exposure to an adverse socioenvironmental milieu) tended to have higher baseline biological health subscores (estimate=0.08, SE=0.04, P=0.043), and faster increases in health behavior subscores (estimate=0.02, SE=0.01, P=0.04); however, these post hoc associations did not reach threshold for significance after correcting for multiple comparisons given the unplanned nature of these analyses (0.05/2 terms of interest=P<0.025).
Table 4.
Post Hoc Associations of Individual Contextually Related Socioenvironmental Items With Ideal Cardiovascular Health as Measured by Modified Life's Simple 7
| mLS7 total score | mLS7 subscores | ||
|---|---|---|---|
| Health behaviors | Biological factors | ||
| Social isolation | 0.11 (0.21) P=0.59 | 0.09 (0.32) P=0.77 | 0.007 (0.35) P=0.98 |
| Social isolation×time | 0.01 (0.04) P=0.72 | 0.01 (0.06) P=0.79 | 0.03 (0.07) P=0.59 |
| Discrimination | 0.02 (0.06) P=0.67 | 0.02 (0.10) P=0.85 | 0.08 (0.11) P=0.47 |
| Discrimination×time | 0.01 (0.01) P=0.48 | −0.01 (0.02) P=0.59 | 0.03 (0.02) P=0.20 |
| Network size | 0.02 (0.02) P=0.32 | −0.04 (0.03) P=0.31 | 0.08 (0.04) P=0.04* |
| Network size×time | −0.002 (0.007) P=0.72 | 0.02 (0.01) P=0.041* | −0.01 (0.01) P=0.13 |
Values are unstandardized coefficient (SE), P value from fully adjusted linear (mLS7 total) or ordinal (mLS7 health behaviors and biological factors subscores) mixed effects models with individual contextually related socioenvironmental items as separate predictors in each model that also included additional terms for time (in study) as well as age, sex, education, depressive symptomatology, and interactions of these variables with time. mLS7 indicates Modified Life's Simple 7.
Denotes significance at P<0.05, although these associations did not meet the threshold for significance after correction for multiple comparisons (0.05/2 terms of interest in each model=P<0.025).
Exploratory Analyses: mLS7 as Effect Modifier of Acculturation in Context and Cognition
The mLS7 total score did not significantly modify (P≥0.86) previously documented 26 (and currently confirmed; Table S3) associations of the acculturation‐related and contextually related socioenvironmental composite scores with level of global cognition. Familism neither significantly associated with (Table S3) nor showed significant effect modification by mLS7 (P >0.29) when considering global cognition.
We next investigated previously documented associations between acculturation in context and cognitive domain scores for effect modification by mLS7. The mLS7 total score did not significantly modify (P≥0.53) the previously documented 26 (and currently confirmed; Table S3) association between the acculturation‐related composite score and level of semantic memory or the previously documented 26 (and currently confirmed; Table S3) associations of the acculturation‐related and contextually related socioenvironmental composite scores with levels of perceptual speed. The mLS7 did unmask a novel association not previously documented between higher acculturation‐related composite scores and faster rates of decline in perceptual speed performance (estimate=−0.07, SE=0.03, P=0.033). Because this indirect effect modification was not a planned term of interest, we applied the same correction for multiple comparisons used in our prior work (0.05/5 cognitive domains=P<0.01) 26 after which, the association no longer reached threshold for significance. Familism neither significantly associated with (Table S3) nor showed significant effect modification by mLS7 (P≥0.73) when considering these 2 cognitive domains.
The mLS7 score modified the association between the acculturation‐related composite score and change in working memory over time (estimate=−0.02, SE=0.01, P=0.043) such that better cardiovascular health in the face of lower levels of acculturation to the United States resulted in slower rates of decline in working memory (Figure 2). As earlier, the incorporation of mLS7 also unmasked other previously undocumented associations. Specifically, higher levels of the contextually related socioenvironmental composite score (ie, higher self‐reported experiences of discrimination and social isolation as well as smaller social networks) were associated with lower levels of working (estimate=−0.16, SE=0.07, P=0.027) and episodic (estimate=−0.16, SE=0.07, P=0.022) memory. The indirect effect modification by cardiovascular health evidenced by these unmasked associations did not, however, reach threshold for significance after correction for multiple comparison. No effect modification interaction terms (direct or indirect) were significant for the visuospatial domain score (P≥0.44).
Figure 2. Representation of the effect modification of cardiovascular health quantified using the modified Life's Simple 7 score (mLS7) on the association between the acculturation‐related composite score and change in working memory in fully adjusted models accounting for age, sex, education, time‐in‐study, CESD‐10, and interactions of each variable with time.
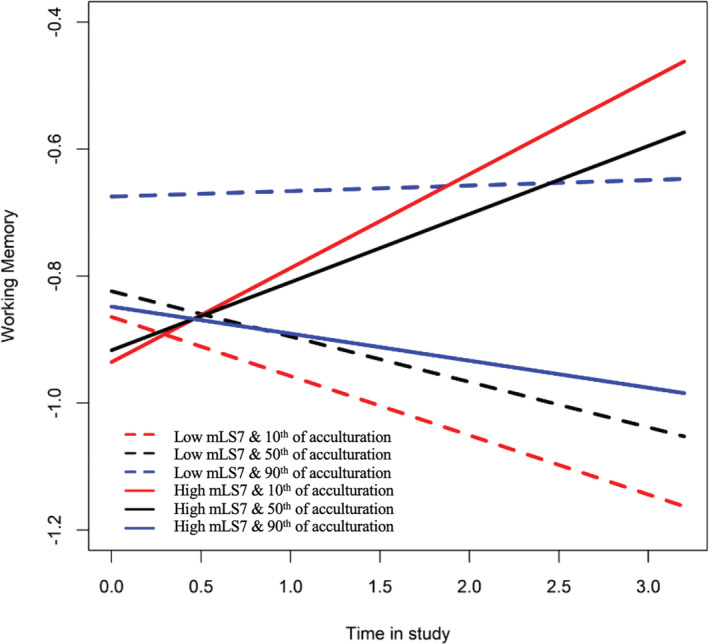
The figure displays the estimated mean mLS7 score in 2 percentiles, that is, low/10th percentile (dotted lines) and high/90th percentile (solid lines) as related to the estimated mean acculturation‐related composite displayed in 3 percentiles, that is, 10th (red line), 50th (black line), and 90th (blue line) percentiles, with all other terms in the model held constant (ie, continuous variables were centered, and sex was female) for ease of interpretation. CESD‐10 indicates 10‐item Center for Epidemiologic Studies of Depression Scale.
DISCUSSION
In this cohort study of nearly 200 older Latino adults without dementia at baseline, we investigated the association of acculturation in context with level of and change in cardiovascular health and explored whether cardiovascular health modified associations of acculturation in context with cognition and cognitive decline. Consistent with our hypothesis, acculturation in context differentially related to overall cardiovascular health. Specifically, higher contextually related socioenvironmental composite scores and higher familism scores were both associated with increases in overall cardiovascular. Although the acculturation‐related composite score did not significantly associate with level of, or change in cardiovascular health, exploratory analyses suggested that cardiovascular health modified associations between this acculturation in context factor and changes in domain‐specific cognitive (ie, working memory) functioning. Taken together, results suggest that socioenvironmental and Latino‐centric aspects of acculturation in context contribute to change in (more so than level of) cardiovascular health, and that combinations of cardiovascular health and acculturation‐related aspects of acculturation in context may further impact cognitive decline in older Latino adults.
A closer investigation of the seemingly paradoxical association between the contextually related socioenvironmental composite and changes in cardiovascular health revealed a nuanced profile that helps to belie any notion that higher exposure to an adverse socioenvironmental milieu is good for cardiovascular health. First, some AHA‐derived criteria for ideal cardiovascular health could, paradoxically, be less than “ideal” for older adults. For example, current clinical guidelines recommend blood pressure targets lower than 130/80 mm Hg instead of the LS7 ideal of 120/70 mm Hg, which might place (and keep) many of our participants in the intermediate or “average” range of this LS7 item. Thus, changes noted in the face of higher contextually derived socioenvironmental factors when taken as a composite may, in part, reflect a move from poor to intermediary levels of blood pressure in pursuit of current clinical guidelines rather than an increase of ideal health. Furthermore, perceptions of discrimination may vary based on generational status 47 and time in the United States. 22 Our older Latino participants reported an average of 40 years of residence in the United States, which may have tempered their reports of discrimination. Moreover, when our contextually related socioenvironmental composite reflecting higher levels of discrimination and social isolation and smaller social networks was broken down into its constituent parts, only smaller social network size significantly associated with cardiovascular health. Older Latino adults often live in multigenerational homes 48 ; this smaller, presumably familial‐based social network may provide opportunities for in‐home support of a participant's medication adherence and other health‐related behaviors. 49 Thus, although a smaller social network size was the only constituent composite score part significantly associated with cardiovascular health in our older Latino participants, further exploration of whether this network is family‐based through a more formal assessment of where older Latino adults live and who they live with may be warranted. Such an assessment may also provide a more robust association with cardiovascular health than that seen in the current study for social network size more generally. In keeping with the idea of the importance of family, familism was related to longitudinal change in overall cardiovascular health, driven primarily by increases in health behaviors. This suggests that family as referent and perceived familial obligations may further support a participant's positive health‐related behaviors (eg, 96% of our participants met ideal criteria for smoking behaviors), or maintenance of healthy physical and/or dietary patterns that promote an age‐appropriate body mass index. Some, 50 but not all, 51 studies support this interpretation, however, more work is needed.
Although the acculturation‐related composite score did not significantly associate with level of or change in overall or domain‐specific cardiovascular health, exploratory analyses found that levels of cardiovascular health directly modified the association between acculturation‐related factors and cognitive change. Specifically, higher levels of cardiovascular health in individuals with lower levels of acculturation to the United States resulted in slower rates of working memory decline. This may provide a more nuanced, longitudinal counterpoint to previous cross‐sectional findings that demonstrated high (not low) levels of acculturation were associated with better working memory performance more generally. 52 Thus, maintaining higher levels of cardiovascular health may protect against working memory declines in older Latino adults reporting lower levels of US‐based acculturation‐related behaviors. This may be due, in part, to the fact that the acculturation‐relatedbehaviors queried in this study may predispose one toward lived experience that bolsters health more generally 53 yet requires the combination with cardiovascular health to exert an effect on a cardiovascular‐reliant cognitive domain like working memory. 54 Additionally, levels of cardiovascular health indirectly modified other relationships between acculturation in context and domain‐specific cognitive performance, unmasking associations between select composite scores and levels of as well as changes in cognition not previously reported. 26 Although exploratory analyses suggest cardiovascular health may be important in the face of acculturation in context experiences when considering cognitive aging in older Latino adults, directed study in larger samples are necessary.
CONCLUSIONS
This study contributes to the literature on acculturation and cardiovascular health in several important ways. First, our results continue to support the acculturation in context framework as a multifaceted concept that differentially contributes to cognitive health in the older Latino population 26 and extends this work to include cardiovascular health. Second, although aspects of our acculturation in context framework have been examined in isolation, 11 , 12 , 13 , 19 we are among the first to employ composite scores of acculturation and extend this work to include broader socioenvironmental determinants as related to cardiovascular health in Latino adults. Third, our work also demonstrates that Latino‐centric constructs, for example, familism, may differentially contribute to general and domain‐specific cardiovascular health, extending previous cross‐sectional studies into a longitudinal framework, and answering calls in the literature for such investigations. 53 Additionally, whereas studies in older Latino adults have reported relationships between LS7 and cognition 8 , 9 or acculturation in context and cognition, 26 the current study investigated all 3 over a mean follow‐up of 3.3 years. Although these results require replication and longer follow‐up, they nonetheless suggest the importance of considering acculturation in context and cardiovascular health when assessing cognitive aging in older Latino adults and further support the assertion 1 that LS7 may be a useful metric to monitor successful brain aging.
This study has several strengths. The comprehensive nature of our conceptualization of acculturation in context allowed us to discuss the effect of socioenvironmental and culturally‐relevant factors on cardiovascular health in older Latino adults. Thus, we studied acculturation in the older Latino population in a way that has not been extensively examined as related to cardiovascular health and LS7 more specifically. Additionally, this study represents one of only a few studies to investigate, within a single study, acculturation in context as it relates to cardiovascular health, and the role of cardiovascular health on the relationship between acculturation and cognition. It suggests that cardiovascular health may directly and indirectly modify relationships between acculturation in context and level of as well as change in cognition.
This study also has limitations. Definitions of ideal cardiovascular health have changed since LS7's inception in 2010. 3 As previously stated, guidelines for those over 60 years of age no longer target blood pressure at the LS7 ideal of 120/70 mm Hg. We are currently compiling all guideline changes to LS7 factors since 2010 to determine if and how evolving guidelines may affect reported relationships. We are also collecting dietary and sleep information to more fully capture the latest AHA guidelines for cardiovascular health. 55 Our current measure of physical activity encompassed some (eg, walking), 56 but not all (eg, dancing) 56 of the most reported types of physical activities for older Latino adults, which may have led to lower reports of physical activity as applied to the mLS7 used in this study. Additionally, although we adjusted for demographic and affective variables, other variables such as acculturation‐related stress and neighborhood‐level environmental factors were not accounted for and may help to explain our results given their importance in explaining health disparities in LS7 between non‐Latino Black and White adults of other cohort studies. 57 Furthermore, although our cohort was relatively diverse, composed of self‐identified Mexican, Puerto Rican, Cuban, and Central and South American participants, we did not have adequate representation across these backgrounds to investigate background differences as has been done in other epidemiologic studies of cardiovascular health. 11 , 58 Moreover, our overall sample size was relatively small. Lastly, work in other cohorts suggests that familism may be a multifaceted construct reflecting distinct aspects of familial obligations, perceived family support, and family as referents. 59 We are actively exploring these distinctions to determine if they are a better reflection of familism in our Latino cohort. Thus, future larger‐scale studies are needed that incorporate additional factors for acculturation in context as they relate to cardiovascular health and how cardiovascular health may interact with acculturation in context to influence cognition over time.
Sources of Funding
This work was supported by National Institute on Aging (grant numbers R01 AG062711, R01 AG17917, P30 AG010161, and P30 AG72975). Funding for Dr Estrella was provided by NIA K01‐AG075353.
Disclosures
Nothing to disclose.
Supporting information
Tables S1–S3
Acknowledgments
We thank all the participants in the Memory and Aging Project and the Rush Alzheimer's Disease Center's Latino Core as well as the research assistants, Outreach and Recruitment staff, and the Statistics and Data Management Core of the center.
Supplemental Material is available at https://www.ahajournals.org/doi/suppl/10.1161/JAHA.122.027620
For Sources of Funding and Disclosures, see page 10.
References
- 1. Gorelick PB, Furie KL, Iadecola C, Smith EE, Waddy SP, Lloyd‐Jones DM, Bae HJ, Bauman MA, Dichgans M, Duncan PW, et al. Defining optimal brain health in adults: a presidential advisory from the American Heart Association/American Stroke Association. Stroke. 2017;48:e284–e303. doi: 10.1161/STR.0000000000000148 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Langa KM, Larson EB, Crimmins EM, Faul JD, Levine DA, Kabeto MU, Weir DR. A comparison of the prevalence of dementia in the United States in 2000 and 2012. JAMA Intern Med. 2017;177:51–58. doi: 10.1001/jamainternmed.2016.6807 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Lloyd‐Jones DM, Hong Y, Labarthe D, Mozaffarian D, Appel LJ, Van Horn L, Greenlund K, Daniels S, Nichol G, Tomaselli GF, et al. Defining and setting national goals for cardiovascular health promotion and disease reduction: the American Heart Association's strategic impact goal through 2020 and beyond. Circulation. 2010;121:586–613. doi: 10.1161/CIRCULATIONAHA.109.192703 [DOI] [PubMed] [Google Scholar]
- 4. Samieri C, Perier MC, Gaye B, Proust‐Lima C, Helmer C, Dartigues JF, Berr C, Tzourio C, Empana JP. Association of Cardiovascular Health Level in older age with cognitive decline and incident dementia. JAMA. 2018;320:657–664. doi: 10.1001/jama.2018.11499 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Crichton GE, Elias MF, Davey A, Alkerwi A. Cardiovascular health and cognitive function: the Maine‐Syracuse Longitudinal Study. PLoS One. 2014;9:e89317. doi: 10.1371/journal.pone.0089317 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Pase MP, Beiser A, Enserro D, Xanthakis V, Aparicio H, Satizabal CL, Himali JJ, Kase CS, Vasan RS, DeCarli C, et al. Association of ideal cardiovascular health with vascular brain injury and incident dementia. Stroke. 2016;47:1201–1206. doi: 10.1161/STROKEAHA.115.012608 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Wei J, Wang L, Kulshreshtha A, Xu H. Adherence to Life's Simple 7 and cognitive function among older adults: the National Health and Nutrition Examination Survey 2011 to 2014. J Am Heart Assoc. 2022;11:e022959. doi: 10.1161/JAHA.121.022959 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Gonzalez HM, Tarraf W, Gouskova N, Rodriguez CJ, Rundek T, Grober E, Pirzada A, Gonzalez P, Lutsey PL, Camacho A, et al. Life's Simple 7's cardiovascular health metrics are associated with Hispanic/Latino neurocognitive function: HCHS/SOL results. J Alzheimers Dis. 2016;53:955–965. doi: 10.3233/JAD-151125 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Gardener H, Wright CB, Dong C, Cheung K, DeRosa J, Nannery M, Stern Y, Elkind MS, Sacco RL. Ideal cardiovascular health and cognitive aging in the Northern Manhattan Study. J Am Heart Assoc. 2016;5:e002731. doi: 10.1161/JAHA.115.002731 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Butte NF, Gregorich SE, Tschann JM, Penilla C, Pasch LA, De Groat CL, Flores E, Deardorff J, Greenspan LC, Martinez SM. Longitudinal effects of parental, child and neighborhood factors on moderate‐vigorous physical activity and sedentary time in Latino children. Int J Behav Nutr Phys Act. 2014;11:108. doi: 10.1186/s12966-014-0108-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Daviglus ML, Pirzada A, Durazo‐Arvizu R, Chen J, Allison M, Aviles‐Santa L, Cai J, Gonzalez HM, Kaplan RC, Schneiderman N, et al. Prevalence of low cardiovascular risk profile among diverse Hispanic/Latino adults in the United States by age, sex, and level of acculturation: the Hispanic Community Health Study/Study of Latinos. J Am Heart Assoc. 2016;5:e003929. doi: 10.1161/JAHA.116.003929 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Kershaw KN, Giacinto RE, Gonzalez F, Isasi CR, Salgado H, Stamler J, Talavera GA, Tarraf W, Van Horn L, Wu D, et al. Relationships of nativity and length of residence in the U.S. with favorable cardiovascular health among Hispanics/Latinos: the Hispanic Community Health Study/Study of Latinos (HCHS/SOL). Prev Med. 2016;89:84–89. doi: 10.1016/j.ypmed.2016.05.013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Ortega AN, Pintor JK, Langellier BA, Bustamante AV, Young MT, Prelip ML, Alberto CK, Wallace SP. Cardiovascular disease behavioral risk factors among Latinos by citizenship and documentation status. BMC Public Health. 2020;20:629. doi: 10.1186/s12889-020-08783-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Lopez L, Peralta CA, Lee A, Zeki Al Hazzouri A, Haan MN. Impact of acculturation on cardiovascular risk factors among elderly Mexican Americans. Ann Epidemiol. 2014;24:714–719. doi: 10.1016/j.annepidem.2014.07.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Kandula NR, Diez‐Roux AV, Chan C, Daviglus ML, Jackson SA, Ni H, Schreiner PJ. Association of acculturation levels and prevalence of diabetes in the Multi‐Ethnic Study of Atherosclerosis (MESA). Diabetes Care. 2008;31:1621–1628. doi: 10.2337/dc07-2182 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Padilla R, Steiner JF, Havranek EP, Beaty B, Davidson AJ, Bull S. A comparison of different measures of acculturation with cardiovascular risk factors in Latinos with hypertension. J Immigr Minor Health. 2011;13:284–292. doi: 10.1007/s10903-010-9434-5 [DOI] [PubMed] [Google Scholar]
- 17. Chang A, Kenya S, Ilangovan K, Li H, Koru‐Sengul T, Alonzo Y, Carrasquillo O. Is greater acculturation associated with an increased prevalence of cardiovascular risk factors among Latinos in South Florida? Med Care. 2015;53:417–422. doi: 10.1097/MLR.0000000000000337 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Mattei J, McClain AC, Falcon LM, Noel SE, Tucker KL. Dietary acculturation among Puerto Rican adults varies by acculturation construct and dietary measure. J Nutr. 2018;148:1804–1813. doi: 10.1093/jn/nxy174 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. van Rompay MI, McKeown NM, Castaneda‐Sceppa C, Falcon LM, Ordovas JM, Tucker KL. Acculturation and sociocultural influences on dietary intake and health status among Puerto Rican adults in Massachusetts. J Acad Nutr Diet. 2012;112:64–74. doi: 10.1016/j.jada.2011.08.049 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Osibogun O, Ogunmoroti O, Mathews L, Okunrintemi V, Tibuakuu M, Michos ED. Greater acculturation is associated with poorer cardiovascular health in the Multi‐Ethnic Study of Atherosclerosis. J Am Heart Assoc. 2021;10:e019828. doi: 10.1161/JAHA.120.019828 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Abraido‐Lanza AF, Armbrister AN, Florez KR, Aguirre AN. Toward a theory‐driven model of acculturation in public health research. Am J Public Health. 2006;96:1342–1346. doi: 10.2105/AJPH.2005.064980 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Abraido‐Lanza AF, Echeverria SE, Florez KR. Latino immigrants, acculturation, and health: promising new directions in research. Annu Rev Public Health. 2016;37:219–236. doi: 10.1146/annurev-publhealth-032315-021545 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Lara M, Gamboa C, Kahramanian MI, Morales LS, Bautista DE. Acculturation and Latino health in the United States: a review of the literature and its sociopolitical context. Annu Rev Public Health. 2005;26:367–397. doi: 10.1146/annurev.publhealth.26.021304.144615 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Lopez‐Class M, Castro FG, Ramirez AG. Conceptions of acculturation: a review and statement of critical issues. Soc Sci Med. 2011;72:1555–1562. doi: 10.1016/j.socscimed.2011.03.011 [DOI] [PubMed] [Google Scholar]
- 25. Schwartz SJ, Unger JB, Zamboanga BL, Szapocznik J. Rethinking the concept of acculturation: implications for theory and research. Am Psychol. 2010;65:237–251. doi: 10.1037/a0019330 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Lamar M, Barnes LL, Leurgans SE, Fleischman DA, Farfel JM, Bennett DA, Marquez DX. Acculturation in context: the relationship between acculturation and socioenvironmental factors with level of and change in cognition in older Latinos. J Gerontol B Psychol Sci Soc Sci. 2021;76:e129–e139. doi: 10.1093/geronb/gbaa156 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Bey GS, Person SD, Kiefe C. Gendered race and setting matter: sources of complexity in the relationships between reported interpersonal discrimination and cardiovascular health in the CARDIA study. J Racial Ethn Health Disparities. 2020;7:687–697. doi: 10.1007/s40615-020-00699-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Islam SJ, Kim JH, Baltrus P, Topel ML, Liu C, Ko YA, Mujahid MS, Vaccarino V, Sims M, Mubasher M, et al. Neighborhood characteristics and ideal cardiovascular health among Black adults: results from the Morehouse‐Emory Cardiovascular (MECA) Center for Health Equity. Ann Epidemiol. 2022;65:120.e1–120.e10. doi: 10.1016/j.annepidem.2020.11.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Corona K, Campos B, Chen C. Familism is associated with psychological well‐being and physical health: main effects and stress‐buffering effects. Hispanic J Behavioral Sci. 2017;39:46–65. doi: 10.1177/0739986316671297 [DOI] [Google Scholar]
- 30. Bennett DA, Launer LJ. Longitudinal epidemiologic clinical‐pathologic studies of aging and Alzheimer's disease. Curr Alzheimer Res. 2012;9:617–620. doi: 10.2174/156720512801322645 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Marquez DX, Glover CM, Lamar M, Leurgans SE, Shah RC, Barnes LL, Aggarwal NT, Buchman AS, Bennett DA. Representation of older Latinxs in cohort studies at the Rush Alzheimer's Disease Center. Neuroepidemiol. 2020;54:404–418. doi: 10.1159/000509626 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Bennett DA, Schneider JA, Aggarwal NT, Arvanitakis Z, Shah RC, Kelly JF, Fox JH, Cochran EJ, Arends D, Treinkman AD, et al. Decision rules guiding the clinical diagnosis of Alzheimer's disease in two community‐based cohort studies compared to standard practice in a clinic‐based cohort study. Neuroepidemiol. 2006;27:169–176. doi: 10.1159/000096129 [DOI] [PubMed] [Google Scholar]
- 33. McKhann G, Drachman D, Folstein M, Katzman R, Price D, Stadlan EM. Clinical diagnosis of Alzheimer's disease: report of the NINCDS‐ADRDA work group under the auspices of Department of Health and Human Services Task Force on Alzheimer's Disease. Neurology. 1984;34:939–944. doi: 10.1212/WNL.34.7.939 [DOI] [PubMed] [Google Scholar]
- 34. Hill CV, Perez‐Stable EJ, Anderson NA, Bernard MA. The National Institute on Aging health disparities research framework. Ethn Dis. 2015;25:245–254. doi: 10.18865/ed.25.3.245 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Marín G, Sabogal F, VanOss MB, Otero‐Sabogal F, Pérez‐Stable EJ. Development of a short acculturation scale for Hispanics. Hispanic J Behavioral Sci. 1987;9:183–205. doi: 10.1177/07399863870092005 [DOI] [Google Scholar]
- 36. Williams DR, Yu Y, Jackson JS, Anderson NB. Racial differences and mental health: socioeconomic status, stress, and discrimination. J Health Psychol. 1997;2:335–351. doi: 10.1177/135910539700200305 [DOI] [PubMed] [Google Scholar]
- 37. Wilson RS, Krueger KR, Arnold SE, Schneider JA, Kelly JF, Barnes LL, Tang Y, Bennett DA. Loneliness and risk of Alzheimer disease. Arch Gen Psychiatry. 2007;64:234–240. doi: 10.1001/archpsyc.64.2.234 [DOI] [PubMed] [Google Scholar]
- 38. Bennett DA, Schneider JA, Tang Y, Arnold SE, Wilson RS. The effect of social networks on the relation between Alzheimer's disease pathology and level of cognitive function in old people: a longitudinal cohort study. Lancet Neurol. 2006;5:406–412. doi: 10.1016/S1474-4422(06)70417-3 [DOI] [PubMed] [Google Scholar]
- 39. Sabogal F, Marin G, Otero‐Sabogal R. Hispanic familism and acculturation: what changes and what doesn't? Hispanic J Behavioral Sci. 1987;9:397–412. doi: 10.1177/07399863870094003 [DOI] [Google Scholar]
- 40. Aggarwal NT, Bienias JL, Bennett DA, Wilson RS, Morris MC, Schneider JA, Shah RC, Evans DA. The relation of cigarette smoking to incident Alzheimer's disease in a biracial urban community population. Neuroepidemiology. 2006;26:140–146. doi: 10.1159/000091654 [DOI] [PubMed] [Google Scholar]
- 41. Buchman AS, Boyle PA, Wilson RS, Bienias JL, Bennett DA. Physical activity and motor decline in older persons. Muscle Nerve. 2007;35:354–362. doi: 10.1002/mus.20702 [DOI] [PubMed] [Google Scholar]
- 42. Lamar M, Fleischman DA, Leurgans SE, Aggarwal N, Yu L, Kim N, Poole V, Han SD, Arfanakis K, Barnes LL. Relationship of blood pressure and white matter hyperintensity burden with level of and change in cognition in older Black adults. Psychosom Med. 2022;84:437–445. doi: 10.1097/PSY.0000000000001059 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Wilson RS, Beckett LA, Barnes LL, Schneider JA, Bach J, Evans DA, Bennett DA. Individual differences in rates of change in cognitive abilities of older persons. Psychol Aging. 2002;17:179–193. doi: 10.1037/0882-7974.17.2.179 [DOI] [PubMed] [Google Scholar]
- 44. Wilson RS, Barnes LL, Mendes de Leon CF, Aggarwal NT, Schneider JS, Bach J, Pilat J, Beckett LA, Arnold SE, Evans DA, et al. Depressive symptoms, cognitive decline, and risk of AD in older persons. Neurology. 2002;59:364–370. doi: 10.1212/WNL.59.3.364 [DOI] [PubMed] [Google Scholar]
- 45. Agresti A. Analysis of Ordinal Categorical Data. Wiley & Sons, Inc; 2010. [Google Scholar]
- 46. McCullagh P. Regression models for ordinal data. J Royal Stat Soc: Series B (Methodological). 1980;42:109–127. doi: 10.1111/j.2517-6161.1980.tb01109.x [DOI] [Google Scholar]
- 47. Viruell‐Fuentes EA. Beyond acculturation: immigration, discrimination, and health research among Mexicans in the United States. Soc Sci Med. 2007;65:1524–1535. doi: 10.1016/j.socscimed.2007.05.010 [DOI] [PubMed] [Google Scholar]
- 48. Cohn D, Passel JS. A record 64 million Americans live in multigenerational households. Household Structure and Family Roles. Pew Research Center. 2018. https://www.pewresearch.org/fact‐tank/2018/04/05/a‐record‐64‐million‐americans‐live‐in‐multigenerational‐households/ [Google Scholar]
- 49. Warren‐Findlow J, Prohaska TR. Families, social support, and self‐care among older African‐American women with chronic illness. Am J Health Promot. 2008;22:342–349. doi: 10.4278/ajhp.22.5.342 [DOI] [PubMed] [Google Scholar]
- 50. Abraido‐Lanza AF, Shelton RC, Martins MC, Crookes DM. Social norms, acculturation, and physical activity among Latina women. J Immigr Minor Health. 2017;19:285–293. doi: 10.1007/s10903-016-0519-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Juarbe T, Turok XP, Perez‐Stable EJ. Perceived benefits and barriers to physical activity among older Latina women. West J Nurs Res. 2002;24:868–886. doi: 10.1177/019394502237699 [DOI] [PubMed] [Google Scholar]
- 52. Mendoza L, Garcia P, Duara R, Rosselli M, Loewenstein D, Greig‐Custo MT, Barker W, Dahlin P, Rodriguez MJ. The effect of acculturation on cognitive performance among older Hispanics in the United States. Appl Neuropsychol Adult. 2022;29:163–171. doi: 10.1080/23279095.2020.1725888 [DOI] [PubMed] [Google Scholar]
- 53. Gallo LC, Penedo FJ, Espinosa de los Monteros K, Arguelles W. Resiliency in the face of disadvantage: do Hispanic cultural characteristics protect health outcomes? J Pers. 2009;77:1707–1746. doi: 10.1111/j.1467-6494.2009.00598.x [DOI] [PubMed] [Google Scholar]
- 54. Foret JT, Dekhtyar M, Birdsill AC, Tanaka H, Haley AP. Metabolic syndrome components moderate the association between executive function and functional connectivity in the default mode network. Brain Imaging Behav. 2021;15:2139–2148. doi: 10.1007/s11682-020-00409-0 [DOI] [PubMed] [Google Scholar]
- 55. Lloyd‐Jones DM, Allen NB, Anderson CAM, Black T, Brewer LC, Foraker RE, Grandner MA, Lavretsky H, Perak AM, Sharma G, et al. Life's Essential 8: updating and enhancing the American Heart Association's construct of cardiovascular health: a presidential advisory from the American Heart Association. Circulation. 2022;146:e18–e43. doi: 10.1161/CIR.0000000000001078 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Marquez DX, Hoyem R, Fogg L, Bustamante EE, Staffileno B, Wilbur J. Physical activity of urban community‐dwelling older Latino adults. J Phys Act Health. 2011;8(suppl 2):S161–S170. doi: 10.1123/jpah.8.s2.s161 [DOI] [PubMed] [Google Scholar]
- 57. Tabb LP, Roux AVD, Barber S, Judd S, Lovasi G, Lawson A, McClure LA. Spatially varying racial inequities in cardiovascular health and the contribution of individual‐ and neighborhood‐level characteristics across the United States: the REasons for geographic and racial differences in stroke (REGARDS) study. Spat Spatiotemporal Epidemiol. 2022;40:100473. doi: 10.1016/j.sste.2021.100473 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Lamar M, Durazo‐Arvizu RA, Sachdeva S, Pirzada A, Perreira KM, Rundek T, Gallo LC, Grober E, DeCarli C, Lipton RB, et al. Cardiovascular disease risk factor burden and cognition: implications of ethnic diversity within the Hispanic Community Health Study/Study of Latinos. PLoS One. 2019;14:e0215378. doi: 10.1371/journal.pone.0215378 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Campos B, Roesch SC, Gonzalez P, Hooker ED, Castaneda SF, Giachello AL, Perreira KM, Gallo LC. Measurement properties of Sabogal's Familism Scale: findings from the Hispanic Community Health Study/Study of Latinos (HCHS/SOL) Sociocultural Ancillary Study. J Lat Psychol. 2019;7:257–272. doi: 10.1037/lat0000126 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Tables S1–S3


