Abstract
Background
Breakfast skipping has previously been associated with worse diet quality among adolescents; the latter increases the risk of chronic disease. However, many studies do not consider diet quality as a function of calories, which is problematic as skippers tend to consume less energy than consumers. Additionally, due to the lack of one accepted definition of both breakfast skipping and diet quality, it is unclear how differences found may change when using varying definitions.
Objectives
We aimed to compare the Healthy Eating Index-2015 (HEI-2015) scores and nutrient intakes of teen breakfast skippers and consumers in Southwestern Ontario, Canada.
Methods
Cross-sectional, baseline data were used from SmartAPPetite, an ongoing nutrition intervention study. Singular 24-h dietary recalls and sociodemographic data from 512 adolescents aged 13–19 y were used to compare HEI-2015 scores and nutrient intakes via multivariable linear regression.
Results
Previous day breakfast skippers had significantly lower HEI-2015 scores (−4.4; 95% CI: −8.4, −0.4) and significantly lower intakes of calories, saturated fat, and vitamin C, as well as significantly higher intake of sodium and total fat.
Conclusions
Previous day breakfast consumers had significantly higher diet quality scores and better nutrient intakes than breakfast skippers, although, on average, both had poor diet quality. Consequently, it is unlikely that simply advising teens to consume breakfast will result in meaningful change in diet quality, and more effort should be placed on promoting nutritious breakfasts.
Keywords: adolescent, teen, diet quality, Healthy Eating Index, breakfast, nutrient, diet recall, epidemiology, pediatrics, nutrition
Introduction
Adolescence is a time of rapid change in the human life cycle associated with increased independence [1]. This independence, coupled with the fact that many teens have access to increased disposable income [2], can lead to increased control over food choices [3]. Unfortunately, this does not mean that teens are making healthy food choices, and evidence from the 2 most recent cycles of the Canadian Community Health Survey - Nutrition (CCHS; 2004 and 2015) suggest that Canadians aged 13–18 y have the worst diet quality among all age groups [4,5]. In a separate study by Minaker et al [6]. involving over 47,000 Canadian students of grades 6–12, only 10% met the 2007 Canada’s Food Guide vegetable and fruit recommendations. These poor dietary patterns are concerning since dietary habits formed during this life stage may persist into adulthood [7], which could then put them at risk of future disease.
Poor diet quality is a well-known risk factor for many chronic health conditions, including cardiovascular disease and various forms of cancer [8]. In a 2019 meta-analysis of studies from 195 countries, poor diet quality was responsible for more deaths than any other risks globally, and an improvement in diet quality could have prevented 20% of premature deaths [9]. Additionally, dietary risks affected people of all ages, suggesting that poor diet quality at any age is concerning. Poor diet quality during adolescence is especially problematic however, because this is an important period of growth, and in cases of certain nutrients such as calcium (which is important for bone growth), insufficient intake could have lifelong consequences [10,11]. Despite the importance of diet quality, there appears to be little congruence in terms of how to measure it, as evidenced by a 2020 systematic review that identified 19 unique dietary metrics commonly used to assess diet quality [12].
One common dietary habit among adolescents that is associated with poor diet quality is breakfast skipping [13], although there is little consistency on how to measure it. In a 2018 systematic review from the International Breakfast Research Initiative, the authors concluded that “there is no agreement as to how to define skippers, irregular and regular breakfast consumers and this contributes to variation in conclusions reached as to the impact of breakfast on overall nutrient intake” [14]. Despite this, research consistently shows that teens who consume breakfast tend to have better diet quality compared to their breakfast skipping counterparts [[15], [16], [17], [18], [19], [20]].
Prior research from Canada has found that the prevalence of breakfast skipping among teens (who have among the highest rates of skipping among all age groups) appears to be ∼12.1% on any given day [5]. One notable article from the International Breakfast Research Initiative showed that Canadian teens who skipped breakfast had lower intakes of fiber; dietary cholesterol; vitamins A, B1, B2, B6, B12, C, and D; calcium; iron; magnesium; and potassium and had lower total diet quality score [as measured via Nutrient-Rich Foods Index 9.3 (NRF 9.3) scores] [5]. Although this paper has added to our knowledge of diets of Canadian teens, it provides minimal context on the quality of foods consumed, as NRF 9.3 is based entirely on nutrient intake [21]. The same is true of a study by Barr et al. [15], which used nationally representative data from the 2004 cycle of the CCHS, finding largely similar results (i.e., inadequate nutrient intakes among breakfast skippers compared to consumers) as the International Breakfast Research Initiative. Although both food-based and nutrient-based measures of diet quality are valid measures of diet quality, they do not necessarily measure the same thing, and as such, assessment of differences in food intakes between skippers and consumers cannot be confidently made.
One explanation for lower diet quality among breakfast skippers is the belief that by skipping a meal, individuals may experience more intense hunger, may opt for poorer nutritional foods (i.e., leading to poorer diet quality), and end up consuming more calories than those they could have consumed from breakfast [22,23]. However, research supporting this notion is sparse, and conversely, there are numerous studies suggesting that skippers, on average, tend to consume less calories. For example, in a 2019 meta-analysis [24], breakfast skippers consumed 260 less calories per day (95% CI: 79, 441) than breakfast consumers. Consequently, when analyses exploring this association do not account for energy intake, the positive association between breakfast consumption and diet quality (measured by nutrient intake, food group consumption, etc.) could be due to the higher energy intake among breakfast consumers. A more thorough investigation of diet quality should consider differences in energy intake (i.e., calories) between breakfast consumers and skippers to determine if the former are truly making more nutritious choices, on a per-calorie basis.
Unfortunately, studies investigating diet quality and breakfast skipping habits among adolescents do not usually adjust for energy intake, and among those that do, differences in diet quality (e.g., nutrient intake and index scores) tend to be marginal [17,22,25]. Assessment of the magnitude of difference between breakfast skippers and consumers is also important to consider; however, even though differences may be statistically significant, it does not necessarily mean they are meaningful ones. Second, studies investigating breakfast habits and diet quality of Canadian teens tend to be even more sparse. Although research from other countries is beneficial to our understanding, to confidently assess breakfast’s impact on diet quality among Canadian teens, it is vital that research be conducted within this population. As such, this study seeks to examine and quantify the relationship between diet quality (measured via Healthy Eating Index-2015 scores and nutrient intake) and breakfast skipping (measured via habitual skipper status and previous day breakfast skipping) among Canadian adolescents while adjusting for energy intake between skippers and consumers.
Methods
This study is a cross-sectional analysis using baseline data from the first 2 years of the SmartAPPetite for Youth project (2018–2019), which received ethics approval from Western University’s Non-Medical Research Ethics Board, The Office of Research Ethics, University of Waterloo, and regional school boards. This project is an ongoing intervention study that seeks to improve diet quality, food knowledge, and food purchasing behavior of teens using a smartphone application, which sends daily messages on a variety of nutrition-related topics. The primary study population were adolescents aged 13–19 y who were enrolled in secondary schools in Southwestern Ontario from 2018 to 2019. All students from the first 8 participating schools were invited to participate in study, and some were included as controls (whereby students were not informed of the SmartAPPetite app). The response rate from the schools that were asked to participate was 100%.
Students were asked during class if they would be interested in participating, and if so, they were asked to take home a parental consent form and have it signed by their parent or guardian. Parents were informed of the purposes of the SmartAPPetite for Youth study via a letter of information, and gave consent that their data can be used in future research publications. Student participants were surveyed 3 times each during their enrollment in the study, and were given $10, $15, and $15 Amazon gift cards, respectively, upon completion of each round of surveys. Parents were only asked to complete a baseline survey and were given a $10 gift card for their participation. Student and parent names were removed from the dataset upon completion of enrollment, and each of them was given a unique ID number, which could only be traced back to individuals via a master list that is only accessible by the SmartAPPetite project coordinator. Finally, upon completion of the study, schools were provided with an online document summarizing the findings from the study, specifically from students from their schools.
Students from the control and intervention groups were combined for the purposes of this study, as only baseline information was used. Data were collected in the fall during school time at their respective schools.
Three measurement tools were used to obtain self-reported information from participants:
Youth survey
Participants completed the youth survey using Qualtrics survey software [26], which gathered information on demographics; self-reported health; nutritional knowledge; and various dietary behaviors, including breakfast consumption. Students were asked, “During the last week, on which days did you eat Breakfast and where?” for each day from Monday to Sunday.
Parent survey
Parents of adolescent participants were asked to complete a survey that included questions regarding the parents’ (if more than one) age, sex, employment status, and family meal habits. Parents of students with consent to participate were invited to complete the parent survey online using Qualtrics survey software [26].
24-h dietary recall
Adolescents completed a 24-h recall via the Automated Self-Administered 24-Hour Dietary Assessment Tool (ASA24) [27] immediately after completing the youth survey. ASA24 is a web-based tool that allows respondents to complete a 24-h recall without the requirement of an interviewer. Developed by the National Cancer Institute, ASA24 uses an Automated Multiple-Pass Method approach and is used in epidemiologic studies, such as those conducted by NHANES [28], as well as the CCHS – Nutrition [29]. Nutrient intakes and diet quality scores were derived from 24-h dietary recalls of participants. Specific nutrients to assess were based upon the availability of data provided by ASA24 and nutrients of public health concern among this population [30].
Breakfast skipping
Two definitions were used for breakfast skipping: 1) Habitual breakfast skipper status, as assessed via the youth survey, and 2) previous day breakfast skipping, as assessed by ASA24 dietary recalls. Teens who skipped breakfast for ≥4 d per week were classified as “habitual skippers,” whereas those who skipped breakfast for ≤3 d were considered “habitual consumers.” This cutoff was decided on because individuals who skip ≥4 d per week skip breakfast more often than they consume it, and this definition has also been used in a similar study [31].
The second independent variable used was whether an individual reported a breakfast meal for the day they reported on their 24-h dietary recall (hereafter referred to as “previous day skippers” and “previous day consumers”). This definition was used in addition to habitual skipper status, since it was thought that skipping breakfast might have its largest effects on diet quality for the day that it was skipped, as opposed to whether an individual usually skips breakfast or not. Second, it was done to compare estimates of the relationship of breakfast skipping with diet quality between the 2 definitions. Individuals who reported consuming a breakfast ≥50 kcal were classified as previous day consumers, whereas those who did not report a breakfast or one <50 kcal were considered previous day skippers. A cutoff of 50 calories was chosen for energy restriction, as any food/beverage consumed that is less than this amount would have a negligible impact on one’s nutrient intake and was not deemed enough food to constitute eating breakfast. This cutoff has been used in a similar study by Drewnowski et al. [18].
Diet quality
Diet quality was assessed via Healthy Eating Index 2015 (HEI-2015) scores and daily nutrient intakes. The Healthy Eating Index was developed in 1995 by the United States Department of Agriculture, and after revisions to its scoring in 2005, has been a joint effort with the National Cancer Institute [32]. The HEI-2015 scores individuals’ diets based on consumption of total fruits, whole fruits, total vegetables, greens and beans, whole grains, dairy, total protein foods, seafood and plant proteins, fatty acids, refined grains, sodium, added sugars, and saturated fats per 1000 calories [32]. Because HEI-2015 scores are measured based on nutrient density, it allows for the important distinction between diet quality and diet quantity. Although there has been a reliable Canadian variation developed (Canadian Healthy Eating Index; HEI-C) [33], this index does not adjust for energy intake, nor is it able to be calculated from the output provided by ASA24; as such, it was not used. HEI-2015 scores were calculated in SAS 9.3 [34] using the source code provided by NIH [35].
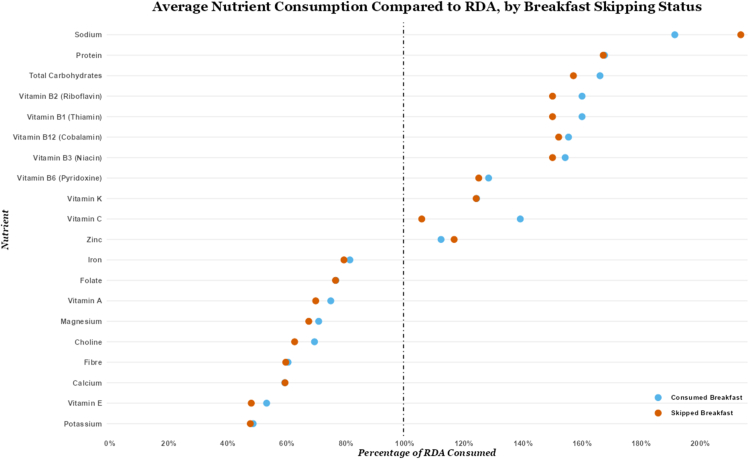
The second outcome assessed was daily nutrient intake of previous day consumers compared to previous day skippers. Pertinent total daily nutrients assessed included calories, protein, fat, carbohydrates, total sugar, fiber, calcium, iron, magnesium, potassium, sodium, zinc, vitamin C, vitamin B1, vitamin B2, vitamin B3, vitamin B6, folate, vitamin B12, vitamin A, vitamin E, vitamin K, saturated fat, monounsaturated fat, polyunsaturated fat, eicosapentaenoic acid, docosahexaenoic acid, choline, and added sugars. Daily nutrient intakes were investigated in addition to index scores to further examine the differences between those who consumed breakfast and those who did not. Furthermore, adjusted daily nutrient intakes were compared against RDA or AI for a 14–18-y-old woman. This was chosen because the majority of the participants identified as female, and a singular reference standard was necessary for comparison. AIs were used as a goal intake for fiber, potassium, vitamin K, choline, and sodium, as no RDA has yet been established. Nutrients with no RDA/AI were not compared against, as no reference standard could be established. Moreover, the difference between previous day skippers and consumers was quantified and compared against the RDA (as a percentage) to illustrate how much the difference between skippers and consumers represents in reference to the RDA. This was done to signify how meaningful the difference is. The comparison of adjusted nutrient intakes to the RDA/AI was subsequently displayed in a Cleveland dot plot, stratified by previous day breakfast status, using RStudio [36].
Covariates
Additional variables were included in models as covariates. The median household income was obtained from Statistics Canada’s 2016 census [37]. Information on age, sex, ethnicity, vegetarian status, importance of healthy eating, physical health rating, mental health rating, physical activity, and nutritional knowledge were obtained from the youth survey, and information on parent’s highest education was obtained from the parent survey.
The age information was obtained by asking “What is your current age?,” with responses being limited to ages 13–19.
Information on sex was obtained by asking participants to respond to the statement, “I am a (insert response),” where responses included: “Male,” “Female,” and “I identify as (please specify).” No participant who identified as neither male nor female had complete data, and therefore, sex was treated as a binary variable.
For analytic purposes, ethnicity was classified as either White/Caucasian or non-White/mixed due to limited numbers of those identifying as alternative ethnicities. This method of controlling for ethnicity was chosen because research has shown that certain ethnic minority groups may be more likely to have lower diet quality compared to Whites/Caucasians [38].
Vegetarian status was obtained by asking participants to respond to the statement, “I eat the following way (select all that apply).” Responses included “Gluten-free,” “Lactose-free,” “Kosher,” “Halal,” “Vegetarian,” “Vegan,” “Other (please specify),” and “None of the above.” Research has demonstrated that vegetarians tend to have better diet quality than nonvegetarians [39], and as such, it was included in all models.
For the importance of healthy eating, participants were asked to respond via a 5-point Likert scale to the following statement: “Eating healthy is important to me,” with 5 being the highest importance and 1 being the lowest. This was important to consider as those who put more emphasis on eating healthy may also be less likely to skip breakfast, as it has been heralded as the “most important meal of the day” [14], representing a potential confounder in the relationship between breakfast consumption and diet quality.
For physical health scores, participants were asked to respond to the following statement: “In general, how do you rate your own physical health?,” with responses including “Excellent,” “Very Good, “Good,” “Fair,” and “Poor.” Physical health is important as it can potentially impact the diet quality (e.g., those who place more importance on physical health may place more importance on eating a higher quality diet [40,41]), while also being superior (on average) among those who consume breakfast [42], thereby representing a potential confounder. Mental health scores were also obtained in a similar fashion, where participants were asked, “In general, how do you rate your own mental health?,” with the same possible responses as above. Mental health is important because individuals with poorer mental health may be less inclined to consume a high-quality diet [43]. Second, mental health has strong ties with breakfast skipping and eating disorders [44], and has been shown to be lower among those who skip breakfast [45], thereby operating as a potential confounder.
Physical activity information was obtained by asking participants, “Over the past 7 days, how many days were you physically active for a total of at least 60 minutes per day?” Responses were limited to 0–7 d, and participants were told that physical activity includes activities that increase their heart rate and cause them to be out of breath some of the time.
Nutritional knowledge was assessed in a series of 51 questions based on a previously validated nutritional survey [46,47]. Participants were scored out of a total of 51 points relating to a variety of questions regarding nutrients, foods that should or should not be consumed as often, and their ability to correctly read a nutrition facts table. Nutritional knowledge is important to consider, since individuals who know more about nutrition tend to have higher diet quality [48] while also being more likely to consume breakfast [49], thereby indirectly inflating the positive effect of breakfast consumption on diet quality.
Neighborhood-level median household income obtained via the Statistics Canada 2016 census was used as a measure of household socioeconomic status [37]. As identified in previous studies [[50], [51], [52]], dissemination areas were used to represent neighborhoods. They are an ideal proxy for neighborhoods given their size, and they are the smallest geographic units for which Statistics Canada releases information on median household income. For analytic purposes, although median household income is a continuous variable, it is presented in models as per a $10,000 increment to improve interpretability.
Finally, parents of participants were asked to list the highest level of education (attained by them) as follows: 1) high school or less; 2) some postsecondary, but less than bachelor’s degree; 3) bachelor’s degree, and 4) greater than bachelor’s degree. Parental education has been shown to be a strong indicator of socioeconomic status [53], which in turn has been associated with both breakfast consumption and diet quality [54,55], thereby acting as a potential confounder in the relationship between the latter 2 factors.
Validity of diet recalls
The validity of diet recalls was determined via an individual’s reported intake of food on their diet recall. Specifically, validity was determined by one’s total daily intake of calories, protein, fat, vitamin C, and beta-carotene. The cut-offs for these nutrients were provided by ASA24 [56], and are based on the 5th and 95th percentile of individuals’ intakes for these specific nutrients from NHANES data. Any diet recall that had an intake for any of these 5 nutrients outside of these ranges were deemed implausible, and while their other data were retained, their dietary recall information was changed to missing data. To examine differences between those who provided a plausible diet recall (n = 672) and those who did not (n = 442), the 2 groups were compared for a variety of socioeconomic status and demographic characteristics, which were largely found with very little differences (see Supplemental Table 1).
Missing data
Missing data were considered to be Missing at Random (MAR [57]). Using a multiple imputation by chained equations (MICE) approach [58], nutrient intake and HEI-2015 scores were determined via multiple linear regression; parental highest education was determined via ordinal logistic regression; number of days the students were physically active was determined using Poisson regression; and vegetarian status was determined via logistic regression. Multiple imputed results (see Supplemental Tables 2, 3, and 4) were largely consistent with our listwise deletion approach, and therefore, only listwise deletion results are shown.
Sample size justification
For multiple regression, there should be at least 10 participants for every predictor variable of interest [59]. As our models had 12–13 predictors per regression, this would require 120–130 participants for the respective models.
Statistical analyses
All regression analyses were performed using STATA IC version 15 [60] and were completed via multivariable linear regression, with either HEI-2015 scores as the outcome (models 1 and 2) or individual nutrient intakes (model 3). The habitual breakfast skipper status was used as the primary exposure variable for model 1, and the previous day breakfast status was used as the primary exposure variable for models 2 and 3. This was done to assess differences between the definitions of breakfast skipping and their relationships with diet quality. The previous day breakfast status was chosen as the primary exposure variable for models 2 and 3 as breakfast skipping would be thought to enact its impact on diet quality for the day it was skipped, rather than whether individuals habitually skipped breakfast or not. Beta-coefficients (unadjusted and adjusted) and their corresponding 95% CIs are presented for each variable in the following tables, along with constants for each model, and R2 (unadjusted and adjusted). A P value of ≤0.05 was considered statistically significant.
Results
A total of 512/1114 (46.0%) adolescent participants (who have completed the SmartAPPetite study so far) had complete case information and valid diet recalls for the variables under study. Descriptive statistics of these participants are shown in Table 1.
TABLE 1.
Descriptive statistics of the sample
| Total sample (N = 512)1 | Previous day consumer (n = 448)2 | Previous day skipper (n = 64)3 | |
|---|---|---|---|
| Descriptive Characteristic | Mean ± SD, median (min, max), or n (%) 4 | ||
| Calories (kcal) | 1740 ± 706 | 1785 ± 705 | 1407 ± 637 |
| Sex (% female) | 317 (61.9%) | 272 (60.7%) | 45 (70.3%) |
| Age (y) | 15.6 ± 1.2 | 15.6 ± 1.2 | 15.5 ± 1.2 |
| Ethnicity (%White) | 357 (69.9%) | 316 (70.5%) | 41 (64.1%) |
| Physical health rating | 3 (1, 5) | 3 (1, 5) | 3 (1, 5) |
| Mental health rating | 3 (1, 5) | 3 (1, 5) | 3 (1, 5) |
| Physically active days | 4.0 ± 1.9 | 4.1 ± 1.9 | 3.5 ± 2.0 |
| Nutritional knowledge score | 32.0 ± 7.0 | 32.0 ± 7.0 | 32.4 ± 7.0 |
| Following vegetarian diet | 28 (5.5%) | 23 (5.1%) | 5 (7.8%) |
| HEI-2015 total score | 55.3 ± 14.7 | 56.0 ± 15.0 | 50.4 ± 12.0 |
| Median household income (CAD $) | $94,369 ± $27,491 | $95,297 ± $27,679 | $87,709 ± $25,149 |
| Habitual skippers | 104 (20.3%) | 63 (14.1%) | 41 (64.1%) |
| Eating healthy importance rating | 4 (2, 5) | 4 (2, 5) | 4 (2, 5) |
| Parental highest education | |||
| High school or less | 69 (13.5%) | 60 (13.4%) | 9 (14.1%) |
| Some postsecondary, less than bachelor’s degree | 191 (37.3%) | 159 (35.5%) | 32 (50.0%) |
| Bachelor’s degree | 139 (27.1%) | 126 (28.1%) | 13 (20.3%) |
| More than bachelor’s degree | 113 (22.1%) | 103 (23.0%) | 10 (15.6%) |
Descriptive statistics for the entire sample included in analysis.
Descriptive statistics for those who reported a breakfast on their 24-h dietary recall.
Descriptive statistics for those who did not report a breakfast on their 24-h dietary recall.
Mean + SD, median (minimum value, maximum value), or number of participants and what percent of participants in the column they represent.
Model 1 (Table 2) sought to compare the overall diet quality of individuals who skipped breakfast for more than 4 d in the previous week to that of those who had breakfast for >4 d. Habitual breakfast skippers did not have significantly different HEI-2015 scores compared to habitual consumers (−1.9; 95% CI: −5.0, 1.1). Significantly higher diet quality scores were associated with being female, vegetarian, higher rating of healthy eating importance, higher nutritional knowledge scores, higher median household income, and having a parent with higher education.
TABLE 2.
HEI-2015 scores by habitual breakfast skipper status (N = 512)
| Model 1 | |||
|---|---|---|---|
| Variable1 | Unadjusted β (95% CI)2 |
R2: 0.16 Adjusted R2: 0.14 |
|
| Adjusted β (95% CI)3 | P value4 | ||
| Constant | 26.2 | ||
| Habitual breakfast skipper status | |||
| Consumer | Reference | -- | |
| Skipper | −3.1 (−6.3, 0.1) | −1.9 (−5.0, 1.1) | 0.21 |
| Sex | |||
| Female | Reference | -- | |
| Male | −3.5 (−6.1, −0.9) | −3.1 (−5.6, −0.5) | 0.025 |
| Age | −0.1 (−1.1, 1.0) | −0.4 (−1.5, 0.6) | 0.38 |
| Ethnicity | |||
| Non-White | Reference | ||
| White | 0.1 (−2.7, 2.9) | −1.3 (−4.1, 1.5) | 0.35 |
| Importance of eating healthy rating | 5.5 (3.5, 7.4) | 4.2 (2.1, 6.2) | <0.015 |
| Physical health rating | 1.8 (0.5, 3.1) | 1.4 (−0.1, 2.9) | 0.07 |
| Mental health rating | 0.0 (−1.1, 1.2) | −0.2 (−1.5, 1.0) | 0.72 |
| Usual number of days physically active | 0.1 (−0.5, 0.8) | −0.6 (−1.4, 0.1) | 0.11 |
| Nutritional knowledge score | 0.3 (0.1, 0.5) | 0.2 (0.1, 0.4) | 0.015 |
| Vegetarian status | |||
| Nonvegetarian | Reference | -- | |
| Vegetarian | 10.6 (5.0, 16.1) | 9.8 (4.5, 15.1) | <0.015 |
| Parental highest education | 2.9 (1.7, 4.2) | 2.4 (1.1, 3.6) | <0.015 |
| Neighborhood income (per $10,000) | 0.8 (0.4, 1.3) | 0.5 (0.1, 1.0) | 0.025 |
Model was adjusted for habitual skipper status (skipped ≥4 d in previous week), sex (male/female), age (continuous), ethnicity (White/non-White), importance of healthy eating rating (continuous), physical health rating (continuous), mental health rating (continuous), usual number of days physically active (continuous), nutritional knowledge score (continuous), vegetarian status (yes/no), parental highest education (continuous), and neighborhood income (per $10,000; continuous)
Variable used in the analysis of the multivariable linear regression.
Beta-coefficient value for unadjusted linear regression with HEI-2015 score as the outcome.
Beta-coefficient value for multivariable linear regression with HEI-2015 score as the outcome.
P value for the adjusted regression analysis for each variable.
P < 0.05.
Model 2 (Table 3) compared the diet qualities of previous day skippers and previous day consumers. Previous day skippers had significantly lower diet quality (−4.4; 95% CI: −8.4, −0.4) than previous day consumers. Significantly higher diet quality scores were associated with being female, vegetarian, higher rating of healthy eating importance, higher nutritional knowledge scores, higher median household income, and having a parent with higher education.
TABLE 3.
Skipping breakfast and its association with the day’s HEI-2015 scores (N = 512)
| Model 2 | |||
|---|---|---|---|
| Variable1 | Unadjusted β (95% CI)2 |
R2: 0.16 Adjusted R2: 0.14 |
|
| Adjusted β (95% CI)3 | P value4 | ||
| Constant | 28.3 | ||
| Previous day breakfast status | |||
| Previous day consumer | Reference | -- | |
| Previous day skipper | -5.6 (-9.4, -1.7) | -4.4 (-8.4, -0.4) | 0.035 |
| Habitual breakfast skipper status | |||
| Consumer | Reference | -- | |
| Skipper | -3.1 (-6.3, 0.1) | -0.5 (-3.8, 2.7) | 0.74 |
| Sex | |||
| Female | Reference | -- | |
| Male | -3.5 (-6.1, -0.9) | -2.9 (-5.5, -0.4) | 0.015 |
| Age | -0.1 (-1.1, 1.0) | -0.5 (-1.5, 0.5) | 0.36 |
| Ethnicity | |||
| Non-White | Reference | ||
| White | 0.1 (-2.7, 2.9) | -1.6 (-4.4, 1.2) | 0.27 |
| Importance of eating healthy rating | 5.5 (3.5, 7.4) | 4.0 (2.0, 6.0) | <0.015 |
| Physical health rating | 1.8 (0.5, 3.1) | 1.5 (-0.1, 3.0) | 0.05 |
| Mental health rating | 0.0 (-1.1, 1.2) | -0.3 (-1.6, 0.9) | 0.60 |
| Usual number of days physically active | 0.1 (-0.5, 0.8) | -0.7 (-1.4, 0.1) | 0.09 |
| Nutritional knowledge score | 0.3 (0.1, 0.5) | 0.2 (0.1, 0.4) | 0.015 |
| Vegetarian status | |||
| Nonvegetarian | Reference | -- | |
| Vegetarian | 10.6 (5.0, 16.1) | 9.8 (4.5, 15.1) | <0.015 |
| Parental highest education | 2.9 (1.7, 4.2) | 2.3 (1.0, 3.6) | <0.015 |
| Neighborhood income (per $10,000) | 0.8 (0.4, 1.3) | 0.5 (0.1, 1.0) | 0.035 |
Model was adjusted for previous day breakfast skipper status (yes/no), habitual skipper status (skipped for ≥4 d in previous week), sex (male/female), age (continuous), ethnicity (White/non-White), importance of healthy eating rating (continuous), physical health rating (continuous), mental health rating (continuous), usual number of days physically active (continuous), nutritional knowledge score (continuous), vegetarian status (yes/no), parental highest education (continuous), and neighborhood income (per $10,000; continuous).
Variable used in analysis of the multivariable linear regression.
Beta-coefficient value for unadjusted linear regression with HEI-2015 score as the outcome.
Beta-coefficient value for multivariable linear regression with HEI-2015 score as the outcome.
P value for the adjusted regression analysis for each variable.
P < 0.05
Model 3 (Table 4) includes a series of multivariable linear regressions to assess nutrient intake based on whether an individual was a previous day skipper or consumer. Disregarding calories, all other nutrients were analyzed while holding caloric intake constant to better assess the differences in diet quality. Previous day breakfast skippers had significantly less intake of calories, vitamin C, and saturated fat, whereas they consumed significantly higher total fat and sodium.
TABLE 4.
Daily nutrient intakes by previous day breakfast status (N = 512)
| Model 3 | ||||||
|---|---|---|---|---|---|---|
| Nutrient1 | Previous day skipper2 | Previous day consumer3 | Difference, (95% CI)4 | RDA/AI5 | % of RDA/AI6 | |
| Calories (kcal)7,8 | 1461 | 1775 | −314 (−503, −126) | N/A | ||
| Protein (g) | 76.9 | 77.1 | −0.2 (−8.2, 7.7) | 46 g | 0.4% | |
| Total fat (g)7 | 69.7 | 64.7 | 5.0 (0.5, 9.3) | N/A | ||
| Saturated fat (mg)7 | 21.5 | 24.4 | −2.9 (−5.2, −0.6) | N/A | ||
| Total monounsaturated fats (g) | 25.2 | 23.6 | 1.6 (−0.5, 3.7) | N/A | ||
| Total polyunsaturated fats (g) | 14.0 | 13.8 | 0.3 (−1.6, 2.2) | N/A | ||
| Eicosapentaenoic acid (mg) | 30.4 | 39.2 | −8.8 (−67.0, 49.4) | N/A | ||
| Docosahexaenoic acid (mg) | 61.8 | 80.4 | −18.6, (−111.4, 74.2) | N/A | ||
| Total carbohydrates (g) | 204.2 | 215.9 | −11.8 (−25.8, 2.3) | 130 g | 9.1% | |
| Total sugar (g) | 73.3 | 85.4 | −12.2 (−24.5, 0.1) | N/A | ||
| Add sugars (tsp equivalents) | 9.4 | 10.9 | −1.4 (−4.1, 1.2) | N/A | ||
| Fiber (g) | 15.5 | 15.7 | −0.2 (−2.1., 1.8) | 26 g | 0.8% | |
| Calcium (mg) | 771.7 | 770.7 | 1.1 (−101.6, 103.7) | 1300 mg | 0.1% | |
| Iron (mg) | 11.9 | 12.2 | −0.3(−1.4, 0.8) | 15 mg | 2.0% | |
| Magnesium (mg) | 242.7 | 254.8 | −12.2 (−36.2, 11.9) | 360 mg | 3.4% | |
| Potassium (mg) | 2237.9 | 2282.5 | −44.6 (−245.3, 156.2) | 4700 mg | 0.9% | |
| Sodium (mg)7 | 3206.7 | 2871.2 | 335.6 (48.5, 622.7) | 1500 mg | 22.4% | |
| Zinc (mg) | 10.5 | 10.1 | 0.4 (−1.0, 1.8) | 9 mg | 4.4% | |
| Vitamin C (mg)7 | 68.7 | 90.4 | −21.7 (−43.2, −0.2) | 65 mg | 33.4% | |
| Vitamin B1 (Thiamin) (mg) | 1.5 | 1.6 | −0.1(−0.3, 0.1) | 1.0 mg | 10.0% | |
| Vitamin B2 (riboflavin) (mg) | 1.5 | 1.6 | −0.1 (−0.2, 0.1) | 1.0 mg | 10.0% | |
| Vitamin B3 (Niacin) (mg) | 21.0 | 21.6 | −0.6 (−3.4, 2.1) | 14 mg | 4.3% | |
| Vitamin B6 (pyridoxine) (mg) | 1.50 | 1.54 | −0.04 (−0.24, 0.15) | 1.2 mg | 3.3% | |
| Folate (mcg) | 305.9 | 306.3 | −0.4 (−34.7, 33.9) | 400 mcg | 0.1% | |
| Vitamin B12 (mcg) | 3.65 | 3.73 | −0.07 (−0.90, 0.76) | 2.4 mcg | 2.9% | |
| Vitamin A (mcg, RAE) | 488.3 | 524.1 | −36.6 (−110.1, 36.9) | 700 mcg | 5.2% | |
| Vitamin E (mg) | 7.19 | 7.97 | −0.78 (−1.9, 0.34) | 15 mg | 5.2% | |
| Vitamin K (mg) | 93.1 | 93.2 | −0.1 (−27.9, 27.7) | 75 mcg | 0.1% | |
| Choline (mg) | 250.5 | 277.4 | −26.9 (−66.0, 12.1) | 400 mg | 6.7% | |
Models were adjusted for calories (continuous), previous day breakfast skipper status (yes/no), habitual skipper status (skipped ≥4 d in previous week), sex (male/female), age (continuous), ethnicity (White/non-White), importance of healthy eating rating (continuous), physical health rating (continuous), mental health rating (continuous), usual number of days physically active (continuous), nutritional knowledge score (continuous), vegetarian status (yes/no), parental highest education (continuous), and neighborhood income (per $10,000; continuous).
Nutrient for which its intake was being assessed via multivariable linear regression.
Mean intake of nutrients for those who did not report a breakfast on their 24-h recall, as assessed via multivariable linear regression.
Mean intake of nutrients for those who reported a breakfast on their 24-h recall, as assessed via multivariable linear regression.
Difference in nutrient intake amounts for skippers versus consumers and the corresponding 95% confidence intervals.
Reference daily intake for each nutrient or, when not yet established, the recommended dietary allowance for a female aged 14–18 y. If neither, N/A is written.
Absolute difference of each nutrient’s intake between skippers and consumers, divided by the recommendations (RDA or AI), expressed in percentage.
P < 0.05.
Not adjusted for calories.
Figure 1 is a visual representation of model 3’s findings. Overall, both previous day breakfast consumers and skippers, on average, appear to be either meeting or exceeding the recommendations for vitamins B1, B2, B3, B6, B12, C, and K; sodium; total carbohydrates; zinc; and protein, whereas they appear to fall short of recommendations for iron, folate, vitamin A, magnesium, choline, fiber, calcium, vitamin E, and potassium. Vitamin C intakes represented the largest difference (33.4%) between those who ate breakfast and those who did not.
FIGURE 1.
Nutrient intake profiles comparison by previous day breakfast consumption status.
Discussion
Overall, diet quality was significantly higher among previous day breakfast consumers, yet even among breakfast consumers, diet quality was poor on average. This is intriguing, as it is possible that participants were susceptible to both volunteer and social desirability bias in the current study [61,62]. This may have occurred because those who signed up for the study may have had a prior interest in nutrition and/or improving their diet, whereas individuals completing 24-h dietary recalls have been known to overestimate the consumption of “healthy” foods while simultaneously underestimating the consumption of “unhealthy” foods [61]. Despite the possibility of these biases influencing results, both groups still did not meet the recommendations for several nutrients, which may indicate that teens’ “true” diet quality may be even worse than what was found in the current study. It should also be noted that although these biases may have affected the estimates of the population’s true diet quality, because they would be expected to affect skippers and consumers equally, it should not have affected the estimates of the difference in diet quality between the 2 groups.
This study also found that habitual skippers did not have significantly different diet quality scores comparison to habitual consumers. These contrasting findings (compared to the findings of previous day breakfast consumers vs. skippers) illustrate the importance of a standardized definition for breakfast skipping, as these 2 definitions may lead readers to differing results, despite both definitions being valid measures of breakfast skipping. Although random measurement error cannot be ruled out as the sole reason for the contrasting findings, one alternative reason may be attributed in part to the fact that most habitual skippers reported a breakfast on their diet recall (from which the diet quality scores were obtained from). Nuances such as these are important to consider when determining which definition(s) to use for classifying skippers and consumers.
It is important to note that while previous day breakfast consumers had significantly better diet quality scores than previous day skippers, the magnitude of the difference in HEI-2015 scores (∼4.4 points) is rather small. To put this difference into perspective, 5 points on the HEI-2015 score represents the following difference for a 2000-cal diet (any one of the following) [32]: half of a large apple, 1 banana, 1 orange, 1 cup of milk, or 2 slices of whole grain bread. Although all these foods represent important contributions to one’s daily diet, they could be considered relatively minor differences, and according to the grading approach by Krebs-Smith et al [63]. for HEI-2015 scores, both skippers and consumers would be given an “F,” suggesting that there is much room for improvement. Potential reasons for the minor differences could be attributed to the plethora of ultra-processed breakfast food options, including frozen waffles, products made from refined grains (e.g., many ready-to-eat cereals), and even take-out from fast-food outlets [64], which teens have access to. Indeed, although breakfast may represent an opportunity for a healthy meal, it does not necessarily mean youth are doing so, which might explain why those consuming breakfast had only slightly higher diet quality scores than those who did not. As such, although a minimally clinically important difference has yet to be established for the Healthy Eating Index [65], it can be argued that 5 points may not represent a meaningful difference.
Daily nutrient intakes revealed that previous day breakfast skippers had significantly lower intakes of calories, vitamin C, and saturated fat, but had significantly higher intakes of total fat and sodium, compared to previous day breakfast consumers. These differences are largely in line with previous research [15,16,22,24,25,[66], [67], [68], [69], [70]], with the exception of skippers consuming less saturated fat, on a per-calorie basis. This finding is somewhat novel (especially considering that total fat was higher in skippers), and inconsistent with most studies showing that saturated fat intake is generally higher among teens who skip breakfast [15,68,70]. However, it is possible that individuals who consumed breakfast may have been more likely to choose popular breakfast foods that are high in saturated fat, such as bacon or other processed meats, butter, and/or other high-fat dairy products (e.g., cream cheese) [71], leading to this finding.
The current study has some limitations. First, it is likely that there was some underreporting with respect to food intake by the teens, as average energy intakes were lower than what has been found in previous Canadian studies [5,15,40,72]. Although it is unclear why teens had lower averages, it may be due in part to the method chosen to gather dietary information. Indeed, in a similar study of youth using ASA24 as a diet recall tool, estimates of food intake were shown to be somewhat inaccurate, with some items being overreported and others being underreported [73], which may have also occurred in this present study. However, our results suggest that the relative difference in diet quality scores between breakfast skippers and consumers is comparable to what has been found in similar research [17,19], and both diet quality scores and daily nutrient intakes were measured as a function of calories, negating the impact that underreporting would potentially have had on the findings.
Second, the present study has treated breakfast skipping as if it were a choice for all individuals. Unfortunately, neither food insecurity nor food availability was assessed. It is possible that some breakfast skippers may be abstaining from consuming breakfast simply because the resources are not available. Although all attempts were made to consider socioeconomic factors, it is possible that food insecurity, which has previously been linked with poorer diet quality [74], may have impacted the present study’s findings. Future research should take into consideration of how food insecurity might affect the relationship between breakfast consumption and diet quality.
Third, the present study only investigated food intake and did not assess the impact supplementation may have had on dietary intake. Although ASA24 does provide users an option to input information about supplementation usage, insufficient data were provided by the teen participants to be used for analysis purposes. Additionally, as the purpose of our study was to assess diet quality, equating supplement intake with nutrient intake from food may be problematic to accurately assess whether one was consuming a healthy diet or whether it was largely aided through the usage of supplements. As such, although it is possible that the diet recalls did not capture the entirety of nutrient intake, they have captured intake from food, which was the primary purpose of this study.
Finally, this study only used one dietary recall to assess the dietary intakes of skippers and consumers. Although more recalls would be ideal to get a more accurate estimation of usual dietary intake, our method of classifying teens as skippers and consumers based on a single recall is accepted and has been used in previous studies [15,16,72,75]. Importantly, the intention of the current study was to classify the average intake of 2 groups of teens, and while individual intakes may vary day-to-day, the group averages ideally would not. A major strength of the current study is that it assessed both previous day breakfast skipping and habitual skipping to account for the aforementioned day-to-day variations.
In conclusion, although breakfast represents a meal that could potentially improve diets of teens, it is likely that simply advising teens to consume one will not result in major improvements in diet quality. If breakfast truly is the most important meal of the day, then teens, on average, are not making the most of it. This study demonstrated that although breakfast consumers have slightly better diet quality than skippers, on average, the diet quality of all teens was lacking. Further research should address barriers to eating healthy breakfasts, rather than focusing solely on breakfast consumption or not. In doing so, improvement in diet quality and, by extension, reduced risk of chronic disease among those consuming higher quality diets would be expected.
Author disclosures
The authors report no conflicts of interest.
Data Availability
Data described in the manuscript, code book, and analytic code will not be made available due to requirements of the participating school board research committee.
Acknowledgements
The authors’ responsibilities were as follows – JS, JH, SS, LM, CO, SD, JG: designed research; NW: conducted research and analyzed data; NW, JS, JH, SS, LM, CO, SD, JG: wrote paper; NW: had primary responsibility for final content; and all authors: read and approved the final manuscript.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.cdnut.2022.100003.
Funding
This study was supported by Children’s Health Research Institute, Heart & Stroke Foundation of Canada, and the Canadian Institute of Health Research, who funded the SmartAPPetite project, from which this data is based upon. The funders were not involved in design, analysis, or interpretation of the data and have no publication restrictions.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- 1.Das JK, Salam RA, Thornburg KL, Prentice AM, Campisi S, Lassi ZS, et al. Nutrition in adolescents: physiology, metabolism, and nutritional needs. Ann N Y Acad Sci. 20171;1393(1):21–33. [DOI] [PubMed]
- 2.Statistics Canada . 2018 May. Canadian youth and full-time work: A slower transition. Ottawa, ON. [Google Scholar]
- 3.Bassett R., Chapman G.E., Beagan B.L. Autonomy and control: the co-construction of adolescent food choice. Appetite. 2008;50(2–3):325–332. doi: 10.1016/j.appet.2007.08.009. [DOI] [PubMed] [Google Scholar]
- 4.Garriguet D. Diet quality in Canada. Health Rep. 2009;20(3):41–52. [PubMed] [Google Scholar]
- 5.Barr S.I., Vatanparast H., Smith J. Breakfast in Canada: Prevalence of consumption, contribution to nutrient and food group intakes, and variability across tertiles of daily diet quality. A study from the international breakfast research initiative. Nutrients. 2018;10(8):985. doi: 10.3390/nu10080985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Minaker L., Hammond D. Low frequency of fruit and vegetable consumption among Canadian youth: findings from the 2012/2013 youth smoking survey. J Sch Health. 2016;86(2):135–142. doi: 10.1111/josh.12359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Movassagh E.Z., Baxter-Jones A.D.G., Kontulainen S., Whiting S.J., Vatanparast H. Tracking dietary patterns over 20 years from childhood through adolescence into young adulthood: The saskatchewan pediatric bone mineral accrual study. Nutrients. 2017;9(9):1–14. doi: 10.3390/nu9090990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.McCullough M.L., Feskanich D., Stampfer M.J., Giovannucci E.L., Rimm E.B., Hu F.B., et al. Diet quality and major chronic disease risk in men and women: Moving toward improved dietary guidance. Am J Clin Nutr. 2002;76(6):1261–1271. doi: 10.1093/ajcn/76.6.1261. [DOI] [PubMed] [Google Scholar]
- 9.Afshin A., Sur P.J., Fay K.A., Cornaby L., Ferrara G., Salama J.S., et al. Health effects of dietary risks in 195 countries, 1990–2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet. 2019;393(10184):1958–1972. doi: 10.1016/S0140-6736(19)30041-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Cromer B., Harel Z. Adolescents: at increased risk for osteoporosis? Clin Pediatr (Phila). 2000 Oct;39(10):565–574. doi: 10.1177/000992280003901001. [DOI] [PubMed] [Google Scholar]
- 11.Gordon C.M., Leonard M.B., Zemel B.S. pediatric position development conference: EXECUTIVE summary and reflections. J Clin Densitom. 2013;17(2):219–224. doi: 10.1016/j.jocd.2014.01.007. 2014. [DOI] [PubMed] [Google Scholar]
- 12.Miller V., Webb P., Micha R., Mozaffarian D. The Lancet Planetary Health. Vol. 4. Elsevier B.V.; 2020. Defining diet quality: a synthesis of dietary quality metrics and their validity for the double burden of malnutrition; pp. 352–370. 8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lillico H.G., Hammond D., Manske S., Murnaghan D. The prevalence of eating behaviors among Canadian youth using cross-sectional school-based surveys. BMC Public Health. 2014;14(1):323. doi: 10.1186/1471-2458-14-323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Gibney M.J., Barr S.I., Bellisle F., Drewnowski A., Fagt S., Livingstone B., et al. Breakfast in human nutrition: The International Breakfast Research Initiative. Nutrients. 2018;10(5):559. doi: 10.3390/nu10050559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Barr S.I., DiFrancesco L., Fulgoni V.L. Breakfast consumption is positively associated with nutrient adequacy in Canadian children and adolescents. Br J Nutr. 2014;112(8):1373–1383. doi: 10.1017/S0007114514002190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Affenito S.G., Thompson D., Dorazio A., Albertson A.M., Loew A., Holschuh N.M. Ready-to-eat cereal consumption and the school breakfast program: relationship to nutrient intake and weight. J Sch Health. 2013;83(1):28–35. doi: 10.1111/j.1746-1561.2012.00744.x. [DOI] [PubMed] [Google Scholar]
- 17.Hopkins L.C., Sattler M., Steeves E.A., Jones-Smith J.C., Gittelsohn J. Breakfast consumption frequency and its relationships to overall diet quality, using healthy eating index 2010, and body mass index among adolescents in a low-income urban setting. Ecol Food Nutr. 2017;56(4):297–311. doi: 10.1080/03670244.2017.1327855. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Drewnowski A., Rehm C.D., Vieux F. Breakfast in the United States: Food and nutrient intakes in relation to diet quality in National Health And Examination Survey 2011-2014. a study from the International Breakfast Research Initiative. Nutrients. 2018;10(9):1200. doi: 10.3390/nu10091200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Woodruff S.J., Hanning R.M., Lambraki I., Storey K.E., McCargar L. Healthy Eating Index-C is compromised among adolescents with body weight concerns, weight loss dieting, and meal skipping. Body Image. 2008;5(4):404–408. doi: 10.1016/j.bodyim.2008.04.006. [DOI] [PubMed] [Google Scholar]
- 20.Rampersaud G.C., Pereira M.A., Girard B.L., Adams J., Metzl J.D. Breakfast habits, nutritional status, body weight, and academic performance in children and adolescents. J Am Diet Assoc. 2005;105(5):742–743. doi: 10.1016/j.jada.2005.02.007. [DOI] [PubMed] [Google Scholar]
- 21.Fulgoni V.L., Keast D.R., Drewnowski A. Development and validation of the nutrient-rich foods index: a tool to measure nutritional quality of foods. J Nutr. 2009;139(8):1549–1554. doi: 10.3945/jn.108.101360. [DOI] [PubMed] [Google Scholar]
- 22.Pereira J.L., Castro MA de, Hopkins S., Gugger C., Fisberg R.M., Fisberg M. Prevalence of consumption and nutritional content of breakfast meal among adolescents from the Brazilian National Dietary Survey. J Pediatr (Rio J). 2018;94(6):630–641. doi: 10.1016/j.jped.2017.10.004. [DOI] [PubMed] [Google Scholar]
- 23.Kant A.K., Graubard B.I. Within-person comparison of eating behaviors, time of eating, and dietary intake on days with and without breakfast: NHANES 2005-2010. Am J Clin Nutr. 2015;102(3):661–670. doi: 10.3945/ajcn.115.110262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Sievert K., Hussain S.M., Page M.J., Wang Y., Hughes H.J., Malek M., et al. Effect of breakfast on weight and energy intake: Systematic review and meta-analysis of randomised controlled trials. BMJ. 2019:364. doi: 10.1136/bmj.l42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Coulthard J.D., Palla L., Pot G.K. Breakfast consumption and nutrient intakes in 4-18-year-olds: UK National Diet and Nutrition Survey Rolling Programme (2008-2012) Br J Nutr. 2017;118(4):280–290. doi: 10.1017/S0007114517001714. [DOI] [PubMed] [Google Scholar]
- 26.Qualtrics X.M. 2020. https://www.qualtrics.com/ [software]. 2020 [cited 2021 Mar 3]. Available from:
- 27.National Cancer Institute ASA24® Dietary Assessment Tool [software] 2020. https://epi.grants.cancer.gov/asa24/ [cited 2020 Apr 20]. Available from:
- 28.Zimmerman T.P., Hull S.G., McNutt S., Mittl B., Islam N., Guenther P.M., et al. Challenges in converting an interviewer-administered food probe database to self-administration in the National Cancer Institute automated self-administered 24-hour recall (ASA24) J Food Compos Anal. 2009;22(Supplement 1):S48–51. doi: 10.1016/j.jfca.2009.02.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Health Canada . 2015. Canadian Community Health Survey - Nutrition. Ottawa, ON: 2015. [Google Scholar]
- 30.Health Canada . 2012. Do Canadian adolescents meet their nutrient requirements through food intake alone? Ottawa, ON. Cat. No.: H164-112/2-2012E-PDF. [Google Scholar]
- 31.Wadolowska L., Hamulka J., Kowalkowska J., Ulewicz N., Gornicka M., Jeruszka-Bielak M., et al. Skipping breakfast and a meal at school: its correlates in adiposity context. Report from the ABC of healthy eating study of polish teenagers. Nutrients. 2019;11(7) doi: 10.3390/nu11071563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.National Cancer Institute. Developing the Healthy Eating Index [Internet]. Bethesda: National Institute of Health; c2020 [cited 2020 Feb 5]. Available from: https://epi.grants.cancer.gov/hei/developing.html#2010.
- 33.Jessri M., Ng A.P., L’Abbé M.R. Adapting the healthy eating Index 2010 for the canadian population: Evidence from the Canadian national nutrition survey. Nutrients. 2017;9(8) doi: 10.3390/nu9080910. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.SAS Institute. Version 9.3. 2020. https://www.sas.com/en_ca/software/stat.html [cited 2022 Jul 15]. Available from:
- 35.Healthy Eating Index SAS Code [Internet]. Bethesda: National Institute of Health; c2020 [cited 2022 Mar 8]. Available from: https://epi.grants.cancer.gov/hei/sas-code.html.
- 36.RStudio. Version 4.1. 2022. https://www.rstudio.com/ [cited 2022 Jul 14]. Available from:
- 37.Statistics Canada. 2016 Census of Population. 2016. Ottawa, ON. [Google Scholar]
- 38.Satia J.A. Diet-related disparities: understanding the problem and accelerating solutions. J Am Diet Assoc. 2009;109(4):610–615. doi: 10.1016/j.jada.2008.12.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Parker H.W., Vadiveloo M.K. Diet quality of vegetarian diets compared with nonvegetarian diets: a systematic review. Nutr Rev. 2019;77(3):144–160. doi: 10.1093/nutrit/nuy067. [DOI] [PubMed] [Google Scholar]
- 40.Storey K.E., Forbes L.E., Fraser S.N., Spence J.C., Plotnikoff R.C., Raine K.D., et al. Diet quality, nutrition and physical activity among adolescents: the Web-SPAN (Web-Survey of Physical Activity and Nutrition) project. Public Health Nutr. 2009;12(11):2009–2017. doi: 10.1017/S1368980009990292. [DOI] [PubMed] [Google Scholar]
- 41.Wu X.Y., Ohinmaa A., Veugelers P.J. Diet quality, physical activity, body weight and health-related quality of life among grade 5 students in Canada. Public Health Nutr. 2012;15(1):75–81. doi: 10.1017/S1368980011002412. [DOI] [PubMed] [Google Scholar]
- 42.Corder K., van Sluijs E.M.F.F., Ridgway C.L., Steele R.M., Prynne C.J., Stephen A.M., et al. Breakfast consumption and physical activity in adolescents: daily associations and hourly patterns. Am J Clin Nutr. 2014;99(2):361–368. doi: 10.3945/ajcn.111.027607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Stranges S., Samaraweera P.C., Taggart F., Kandala N.B., Stewart-Brown S. Major health-related behaviours and mental well-being in the general population: The health survey for England. BMJ Open. 2014;4(9) doi: 10.1136/bmjopen-2014-005878. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Charbonneau K.D., Seabrook J.A. Adverse birth outcomes associated with types of eating disorders: a review. Can J Diet Practice Res. 2019;80(3):131–136. doi: 10.3148/cjdpr-2018-044. [DOI] [PubMed] [Google Scholar]
- 45.Sawa S., Hashizume K., Abe T., Kusaka Y., Fukazawa Y., Hiraku Y., et al. Pathway linking physical activity, sleep duration, and breakfast consumption with the physical/psychosocial health of schoolchildren. J Child Heal Care. 2021;25(1):5–17. doi: 10.1177/1367493519891019. [DOI] [PubMed] [Google Scholar]
- 46.Vereecken C.A., Keukelier E., Maes L. Influence of mother’s educational level on food parenting practices and food habits of young children. Appetite. 2004;43(1):93–103. doi: 10.1016/j.appet.2004.04.002. [DOI] [PubMed] [Google Scholar]
- 47.Anderson A., Bell A., Adamson A., Moynihan P. A questionnaire assessment of nutrition knowledge – validity and reliability issues. Public Health Nutr. 2002;5(3):497–503. doi: 10.1079/PHNPHN2001307. [DOI] [PubMed] [Google Scholar]
- 48.Spronk I., Kullen C., Burdon C., O’Connor H. Relationship between nutrition knowledge and dietary intake. Br J Nutr. 2014;111(10):1713–1726. doi: 10.1017/S0007114514000087. [DOI] [PubMed] [Google Scholar]
- 49.Matsumoto M., Ishige N., Sakamoto A., Saito A., Ikemoto S. Nutrition knowledge related to breakfast skipping among Japanese adults aged 18-64 years: A cross-sectional study. Public Health Nutr. 2019;22(6):1029–1036. doi: 10.1017/S1368980018003014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Hollands S., Campbell M.K., Gilliland J., Sarma S. Association between neighbourhood fast-food and full-service restaurant density and body mass index: A cross-sectional study of Canadian adults. Can J Public Health. 2014;105(3) doi: 10.17269/cjph.105.4287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.McInerney M., Csizmadi I., Friedenreich C.M., Uribe F.A., Nettel-Aguirre A., McLaren L., et al. Associations between the neighbourhood food environment, neighbourhood socioeconomic status, and diet quality: An observational study. BMC Public Health. 2016;16(1):1–15. doi: 10.1186/s12889-016-3631-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Gilham K., Gu Q., Dummer T.J.B., Spinelli J.J., Murphy R.A. Diet quality and neighborhood environment in the atlantic partnership for tomorrow’s health project. Nutrients. 2020;12(10):1–13. doi: 10.3390/nu12103217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.American Psychological Association . 2016. Children, Youth, Families and Socioeconomic Status. Washington (DC) [Google Scholar]
- 54.Vereecken C., Dupuy M., Rasmussen M., Kelly C., Nansel T.R., Al Sabbah H., et al. Breakfast consumption and its socio-demographic and lifestyle correlates in schoolchildren in 41 countries participating in the HBSC study. Int J Public Health. 2009;54(Suppl 2):180–190. doi: 10.1007/s00038-009-5409-5. Suppl 2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Darmon N., Drewnowski A. Does social class predict diet quality? Am J Clin Nutr. 2008;87(5):1107–1117. doi: 10.1093/ajcn/87.5.1107. [DOI] [PubMed] [Google Scholar]
- 56.Reviewing & Cleaning ASA24® Data. Bethesda: National Institute of Health [cited 2020 Apr 21]. Available from: https://epi.grants.cancer.gov/asa24/resources/cleaning.html#guidelines.
- 57.Jakobsen J.C., Gluud C., Wetterslev J., Winkel P. When and how should multiple imputation be used for handling missing data in randomised clinical trials - A practical guide with flowcharts. BMC Med Res Methodol. 2017;17(1):162. doi: 10.1186/s12874-017-0442-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Azur M.J., Stuart E.A., Frangakis C., Leaf P.J. Multiple imputation by chained equations: What is it and how does it work? Int J Methods Psychiatr Res. 2011;20(1):40–49. doi: 10.1002/mpr.329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Schaafsma H., Laasanen H., Twynstra J., Seabrook J.A. A review of statistical reporting in dietetics research (2010-2019): How is a Canadian journal doing? Can J Diet Pract Res. 2021;82(2):59–67. doi: 10.3148/cjdpr-2021-005. [DOI] [PubMed] [Google Scholar]
- 60.StataCorp. Stata Statistical Software. Version 15. 2020. https://www.stata.com/ [cited 2022 Jul 15]. Available from:
- 61.Hebert J.R., Clemow L., Pbert L., Ockene I.S., Ockene J.K. Social desirability bias in dietary self-report may compromise the validity of dietary intake measures. Int J Epidemiol. 1995;24(2):389–398. doi: 10.1093/ije/24.2.389. [DOI] [PubMed] [Google Scholar]
- 62.Cheung K.L., Ten Klooster P.M., Smit C., De Vries H., Pieterse M.E. The impact of non-response bias due to sampling in public health studies: A comparison of voluntary versus mandatory recruitment in a Dutch national survey on adolescent health. BMC Public Health. 2017;17(1):1–10. doi: 10.1186/s12889-017-4189-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Krebs-Smith S.M., Pannucci T.R.E., Subar A.F., Kirkpatrick S.I., Lerman J.L., Tooze J.A., et al. Update of the Healthy Eating Index: HEI-2015. J Acad Nutr Diet. 2018;118(9):1591–1602. doi: 10.1016/j.jand.2018.05.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Monteiro C.A., Cannon G., Levy R.B., Moubarac J.C., Louzada M.L.C., Rauber F., et al. Ultra-processed foods: what they are and how to identify them. Public Health Nutr. 2019;22(5):936–941. doi: 10.1017/S1368980018003762. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Liu J., Rehm C.D., Onopa J., Mozaffarian D. Trends in diet quality among youth in the United States, 1999-2016. JAMA. 2020;323(12):1161–1174. doi: 10.1001/jama.2020.0878. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Deshmukh-Taskar P.R., Nicklas T.A., O’Neil C.E., Keast D.R., Radcliffe J.D., Cho S. The relationship of breakfast skipping and type of breakfast consumption with nutrient intake and weight status in children and adolescents: the National Health and Nutrition Examination Survey 1999-2006. J Am Diet Assoc. 2010;110(6):869–878. doi: 10.1016/j.jada.2010.03.023. [DOI] [PubMed] [Google Scholar]
- 67.Williams P. Breakfast and the diets of Australian children and adolescents: an analysis of data from the 1995 National Nutrition Survey. Int J Food Sci Nutr. 2007;58(3):201–216. doi: 10.1080/09637480701198075. [DOI] [PubMed] [Google Scholar]
- 68.Fayet-Moore F., McConnell A., Tuck K., Petocz P. Breakfast and breakfast cereal choice and its impact on nutrient and sugar intakes and anthropometric measures among a nationally representative sample of Australian children and adolescents. Nutrients. 2017;9(10):1045. doi: 10.3390/nu9101045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Fayet-Moore F., Kim J., Sritharan N., Petocz P. Impact of breakfast skipping and breakfast choice on the nutrient intake and body mass index of Australian children. Nutrients. 2016;8(8):487. doi: 10.3390/nu8080487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Grieger J.A., Cobiac L. Comparison of dietary intakes according to breakfast choice in Australian boys. Eur J Clin Nutr. 2012;66(6):667–672. doi: 10.1038/ejcn.2011.220. [DOI] [PubMed] [Google Scholar]
- 71.Choose foods with healthy fats – Canada’s Food Guide [Internet]. Ottawa: Canada's Food Guide; c2020 [cited 2020 Jul 10]. Available from: https://food-guide.canada.ca/en/healthy-eating-recommendations/make-it-a-habit-to-eat-vegetables-fruit-whole-grains-and-protein-foods/choosing-foods-with-healthy-fats/.
- 72.Storey K.E., Hanning R.M., Lambraki I.A., Driezen P., Fraser S.N., McCargar L.J. Determinants of diet quality among Canadian adolescents. Can J Diet Pract Res. 2009;70(2):58–65. doi: 10.3148/70.2.2009.58. [DOI] [PubMed] [Google Scholar]
- 73.Raffoul A., Hobin E.P., Sacco J.E., Lee K.M., Haines J., Robson P.J., et al. School-age children can recall some foods and beverages consumed the prior day using the automated self-administered 24-Hour Dietary Assessment Tool (ASA24) without assistance. J Nutr. 2019;149(6):1019–1026. doi: 10.1093/jn/nxz013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Bocquier A., Vieux F., Lioret S., Dubuisson C., Caillavet F., Darmon N. Socio-economic characteristics, living conditions and diet quality are associated with food insecurity in France. Public Health Nutr. 2015;18(16):2952–2961. doi: 10.1017/S1368980014002912. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Nicklas T.A., Reger C., Myers L., O’Neil C., TA N., Reger C., et al. Breakfast consumption with and without vitamin-mineral supplement use favorably impacts daily nutrient intake of ninth-grade students. J Adolesc Health. 2000;27(5):314–321. doi: 10.1016/s1054-139x(00)00113-0. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Data described in the manuscript, code book, and analytic code will not be made available due to requirements of the participating school board research committee.