Abstract
Background
Complementary feeding of infants in refugee settlements remains inadequate. Furthermore, there has been limited evaluation of interventions addressing these nutrition challenges.
Objective
This study examined the effects of a peer-led integrated nutrition education intervention on infant complementary feeding by South Sudanese refugee mothers in the West-Nile region in Uganda.
Methods
A community-based randomized trial enrolled 390 pregnant women (during third trimester) as the baseline. Two arms [mothers-only and parents-combined (both mothers and fathers)] comprised treatments with a control. Infant feeding was assessed using WHO and UNICEF guidelines. Data were collected at Midline-II and Endline. The medical outcomes study (MOS) social support index was used to measure social support. An overall mean score of >4 was considered optimal social support, a score of ≤2 was none or little support. Adjusted multivariable logistic regression models determined the effects of the intervention on infant complementary feeding.
Results
At the end of the study, infant complementary feeding improved significantly in both mothers-only and parents-combined arms. There was a positive effect on the introduction of solid, semisolid, and soft foods (ISSSF) in the mothers-only arm at both Midline-II {adjusted odds ratio (AOR) = 4.0]} and Endline (AOR = 3.8). Likewise, ISSSF was better for the parents-combined arm at both Midline-II (AOR = 4.5) and Endline (AOR = 3.4). Minimum dietary diversity (MDD) was significantly better at the Endline for the parents-combined arm (AOR = 3.0). Minimum acceptable diet (MAD) was significantly better at Endline for both mothers-only (AOR = 2.3) and parents-combined arms (AOR = 2.7). Infant consumption of eggs and flesh foods (EFF) was improved only in the parents-combined arm at both Midline-II (AOR = 3.3) and Endline (AOR = 2.4). Higher maternal social support was associated with better infant MDD (AOR = 3.3), MAD (AOR = 3.6), and EFF (AOR = 4.7).
Conclusion
Engaging both fathers and mothers in care groups benefited complementary feeding of infants. Overall, this peer-led integrated nutrition education intervention through care groups improved infant complementary feeding in the West-Nile postemergency settlements in Uganda.
This trial was registered at clinicaltrials.gov as NCT05584969.
Keywords: infant feeding, maternal social support, South Sudanese, refugee settlements, Uganda, postemergency
Introduction
The United Nations High Commissioner for Refugees (UNHCR) in 2020 reported the highest ever displacement of persons at 82.4 million [1,2]. Most refugee crises (86%) occurred in low-and-middle-income countries with 44.5% of the refugees within Africa [3]. Uganda was ranked third (jointly with Pakistan) among countries hosting refugees. Most (62%) refugees hosted in Uganda came from South Sudan due to the prolonged civil unrest [4]. The UN through its agencies, partner organizations, and the host country provide for the needs of the refugees including health, nutrition, and food security. Yet, as humanitarian aid is reduced after the emergency period [5,6], inadequate feeding practices and child undernutrition remain primary health concerns of refugees in protracted situations [7,8].
Optimal child feeding practices are critical in preventing undernutrition [[9], [10], [11]]. However, poor complementary feeding practices were reported in the West-Nile postemergency settlements in Uganda in 2020 [12]. Such suboptimal infant feeding practices are associated with an increased risk of undernutrition, disease, and mortality [13]. Hence, providing an integrated nutrition education intervention through maternal peer support may positively influence caregivers in adhering to feeding practices, thus improving child nutrition [10,[14], [15], [16], [17]]. Nutrition-specific interventions grounded in a social behavior change communication (SBCC) approach such as the care group model [[18], [19], [20], [21], [22], [23], [24]] may provide sustainable, cost effective strategies to improve child feeding practices and reduce malnutrition [25,26].
Understanding the role of such nutrition interventions delivered through maternal peer support on complementary feeding practices of infants may influence the implementation of sustainable programs on child nutrition in postemergency settlements. Yet, evidence of the effectiveness of such nutrition strategies remains limited [27]. Systematic reviews of health in humanitarian crises [5,28,29] indicated that few studies had been done to assess the efficacy of indirect nutrition-focused interventions on infant and young child feeding (IYCF) practices. Therefore, this study aimed to examine 1) the effect of a peer-led integrated nutrition education intervention delivered through care groups on complementary feeding practices of infants among refugees in the West-Nile region in Uganda and 2) the relation among the care group intervention, maternal social support, and complementary feeding of infants. To our knowledge, this is the first study to investigate the impact of a peer-led integrated nutrition education intervention using the care group model on IYCF practices among infants in postemergency settlements in Uganda. Further, this study uses the most recent WHO and UNICEF IYCF guidelines [30]. Postemergency settlements are defined as protracted politically stable environments in which the UNHCR and refugee host country continue to provide for the well-being of the refugees beyond the first 2 y of emergency [31,32]. The findings in this study may be used to design nutrition-sensitive programs and also inform policies targeting complementary feeding practices within postemergency settlements in Uganda.
Methods
Study setting
A community-based cluster randomized controlled trial (RCT) was conducted among refugee postemergency settlements in the West-Nile region in Uganda. The Adjumani district was randomly selected from among the 10 districts hosting refugees in the region. Four of the 19 settlements in the Adjumani district were randomly selected and assigned to three arms of the study. Each study arm had a total of 10 peer groups. Ayilo-I settlement was assigned as a mothers-only study arm, Pagirinya and Ayilo II settlements were the parents-combined (both mothers and fathers) study arm whereas Nyumanzi settlement was the control arm. These settlements were ≥6 km apart to reduce the possibility of spillover effects of the intervention. The intervention was conducted in the mothers-only and parents-combined arms. The village health team (VHT) members and health center midwife assistants supported the identification of pregnant women in their third trimester to be included in the study. Midwives and midwife assistants have formal educational training through a national curriculum licensed under the Ministry of Health of Uganda resulting in certification or a diploma in maternal health care practice [33,34]. VHTs are a network of community volunteers who link with the grassroots to promote primary health care, best hygiene, sanitation practices, nutrition, and health-seeking behavior for health center services [35]. VHTs are provided with basic training in health and nutrition education by personnel from the Ministry of Health and health partner agencies [36]. In this study, VHTs and midwives verified the pregnancy trimester of women using a copy of the Integrated Maternity Register (IMR) and each pregnant woman’s antenatal passport record.
Sample size
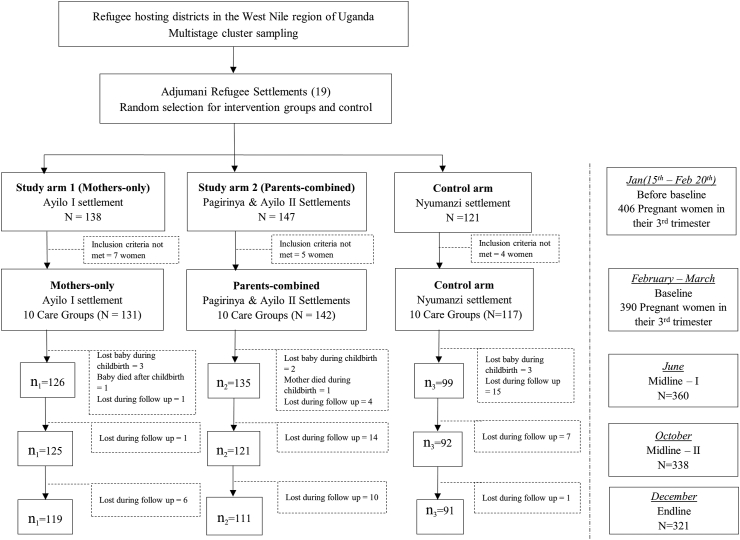
The introduction of complementary foods as recommended by WHO and UNICEF [30] was used as the primary outcome because of its reliability as an indicator of child feeding practices. The desired sample size of 317 pregnant women was calculated using GPower 3.1 software, a type I error of 0.05, a power of 0.90, and an effect size of 0.2 [14,17] to detect differences in the proportions of infants introduced to complementary foods at 6 to 8 mo [14,37,38] among the three study arms. A 23% loss during follow-up was estimated; thus, 390 women (aged 15–49 y) in their third trimester of pregnancy comprised the study sample and were enrolled at baseline. Husbands were eligible to participate with their wives in the parents-combined treatment arm. Eighty-two percent (n = 321) of the mother-infant dyads completed the study. The mother-infant dyads comprised the experimental unit for the assessment of the practices of complementary feeding of infants. By the end of the study, the mother-infant dyads were 119 for the mothers-only study arm, 111 for the parents-combined arm, and 91 for the control arm. A flow diagram of the study participants for the study was shown in Figure 1.
FIGURE 1.
Flow diagram of study design and participants in the study
Inclusion and exclusion criteria
Mothers whose antenatal records showed pregnancy complications were excluded from the study. Mothers who gave birth to premature infants, infants with congenital abnormalities, or whose infants died had the option of remaining in the study but were excluded from the final analyses.
Intervention
The study began in January 2020 and was completed in December 2020. A peer-led integrated nutrition education program was delivered using the care group model to the treatment arms. Ten groups each with 10–20 participants comprised the care groups (or peer groups) assigned to each of the two treatments. In one treatment, mothers-only participated in the intervention, whereas the other had a combination of parents (mothers and fathers) in the care groups. Through the care group model, peer leaders that served as community-based health and nutrition educators facilitated the trainings, peer supervision, and support of one another in the peer groups [22,[39], [40], [41]].
Two peer leaders were identified by each care group in the two treatment arms before the start of the intervention. These peer leaders participated in a 5-d comprehensive training using the prepared care group pamphlets facilitated by selected VHTs supervised by the district health and nutrition educator (DHE) and the researcher. Before the peer leader training, the selected VHTs for the intervention had been trained by the DHE supported by the researcher using the care group pamphlets and community workers training manuals [[42], [43], [44]]. The peer-led intervention, which began in March 2020 after the baseline, consisted of training on group dynamics, infant feeding guidelines [43], cooking demonstrations, and backyard farming demonstrations conducted over 10 mo (Supplementary Table 3). The selected VHTs and peer leaders had a monthly meeting for refresher training and to provide feedback to the researcher. The care group meetings lasted 60–90 min and were conducted every 2 wk.
Standard of care
The control arm as well as the two treatment arms were expected to receive the standard of care which was the follow-up of mothers and their infants through the government health services system. The Government of Uganda implements a decentralized referral health system [45] where community VHTs provide the grassroots the first point of contact for health, sanitation, and nutrition promotion services, and for referrals [35]. Referrals to higher-level health center facilities depended on the complexity of services required by the patient. In this study, all the participants were served by VHTs in charge of their villages (≥two VHTs serving between 50–70 households). Additionally, the participants were able to freely access services at the health center III (three) facilities located within the refugee settlements (within 5 km of the households) [46]. All the study participants were expected to access health services including health-related training and follow-up through the standard health system facilities. Further referrals to higher-level facilities such as District Hospitals or Regional and National Referral Hospitals were more costly to access because of distant locations within urban centers but depended on the ability of a patient to meet the cost.
Measures
The independent variables for this study included the study arms, time, and maternal social support scores. All participants in the study were assigned by settlement to one of the three study arms, mothers-only, parents-combined, and the control. Complementary feeding practices of infants were assessed at the Midline-II and Endline study periods. However, maternal, household and other infant characteristics were collected during the four different study periods as illustrated in the study Gantt chart (Supplementary Figure 1).
Maternal social support was assessed with the medical outcomes study (MOS) social support scale [47]. A set of 19 questions (Supplementary Table 1) with a 5-point Likert scale was adapted from the MOS scale which has often been used in assessing social support. Recent studies in Uganda [48] and Zimbabwe [19] also adapted the MOS questions to assess maternal social support among local communities. In this study, participants expressed the level of perceived support with responses ranging from “none of the time” (score of “1”) to “all of the time” (score of “5”). The mother’s perceived social support based on their total mean score was categorized into optimal (>4 and ≤5); moderate (>3 and ≤4), low (>2 and ≤3), and none or very low support (≤2) [47].
Dependent variables
Infant complementary feeding practices
The dependent variables in this study were practices of complementary feeding as defined by the WHO IYCF Indicators [30]. These variables (specified in Supplementary Table 2) included the timely introduction of solid, semisolid, and soft foods (ISSSF) to infants, minimum dietary diversity (MDD), minimum meal frequency (MMF), minimum acceptable diet (MAD), and consumption of eggs and flesh foods (EFF). These complementary feeding practices assessed at both the Midline-II and Endline periods determined whether the infant “met” or “did not meet” the feeding practice.
Statistical analyses
Descriptive statistics for household, infant, and maternal characteristics, as well as practices of complementary feeding of infants were compiled. Differences in proportions of descriptive characteristics among the study arms’ were tested using chi-square and ANOVA. Bivariate logistic regression was used to examine the effects of the care group intervention on the complementary feeding of infants. Associations with P < 0.1 were included in the multivariable logistic regression models.
Confounding variables
This study controlled for potential confounders frequently reported as determinants of complementary feeding practices for infants [[49], [50], [51], [52], [53]]. The confounding maternal variables included the mother's current age, BMI, who supports the mother most, number of living children, and religion; household confounders included household food insecurity access scale (HFIAS) scores, family size, household head, ethnicity, wealth index, and years spent in refugee settlement, whereas infant confounders included birth weight and sex.
Exploratory analyses were performed to evaluate multicollinearity of the explanatory variables. The variance inflation factor (VIF) (<10) and the tolerance test (<0.2) were within acceptable limits. In this study, outcome variables that maintained a P value < 0.05 in the multivariable analyses were considered significant. Data analyses were performed using STATA/ SE v17.0 (Stata Corp LLC, Lakeway Drive, TX, USA).
Ethical approval
This study was approved by the Institutional Review Boards of the Uganda National Council of Science and Technology (SS 5038) in August 2019, Makerere University School of Health Science Research and Ethics Committee (SHSREC REF:2019-020) in May 2019, and Oklahoma State University (HS-19-2) in January 2019. Additional permission was acquired from the Office of the Prime Minister (OPM) Uganda (OPM/R/107). Informed consent was obtained from all the study participants by signature or thumbprint. At recruitment, consent was obtained to review the participants’ antenatal passports which also had medical records concerning their pregnancy. Further consent was obtained before each of the data collection for use in both current and future academic research. At each data collection period, the participants were provided with a 1kg bar of washing soap, 200mL of vitamin A fortified cooking oil, and 0.5 kg each of iodized salt and sugar, all worth 7600 Uganda shillings (1.5 USD) as compensation for participation in the study. This trial is registered at clinicaltrials.gov as NCT05584969 as of October 2022. In 2019, the researchers were unaware of the requirement for clinical trial registration for an educational-based intervention, which was completed upon notification during the manuscript submission process. Although the study was registered retrospectively, the clinical trial protocol was identical to the protocols used in the three approved IRBs which were acquired before the commencement of the study. All IRB protocols are available upon request to the corresponding author.
Results
Sociodemographic characteristics of the participants
Descriptive statistics included percentages and means of household, infant, and maternal characteristics reported in Table 1. Most respondents (52.7%) in this study were stay home spouses. The proportion of households headed by the mother in all study arms ranged from 46.5% to 58.8%. The mean ± SD for family size for all study arms was ∼8 people (8.3 ± 3.1). Based on the wealth index [54], less than half of the households in all arms were identified as poor, however, the parents-combined arm had the lowest proportion (25.2%) of poor households compared with the control (47.2%) and mothers-only (47.9%). Further, the HFIAS score was reported in the control (10.2 ± 5.3). The mothers in the control had stayed in the refugee settlements for a mean of 5 y. The highest proportions of male infants (62.4%) were observed in the parents-combined arm compared with the mothers-only arm (48.4%) and the control (43.4%). The overall mean infant birth weight was 3.1 ± 0.5 kg.
Table 1.
Sociodemographic characteristics of the respondents
| Variable | Control arm |
Mothers-only arm |
Parents-combined arm |
Total |
Sig.5 |
|---|---|---|---|---|---|
| Mean ± SD or % (n) | Mean ± SD or % (n) | Mean ± SD or % (n) | Mean ± SD or % (n) | ||
| Current working status2 | |||||
| Stay home spouse | 53.0 (61) | 51.2 (67) | 53.9 (76) | 52.7 (204) | 0.937 |
| Farmer | 19.1 (22) | 22.9 (30) | 19.9 (28) | 20.6 (80) | |
| Small business owner | 13.9 (16) | 15.3 (20) | 16.3 (23) | 15.3 (61) | |
| Other | 13.9 (16) | 10.7 (14) | 9.9 (14) | 11.4 (45) | |
| Household head1 | |||||
| Mother | 57.3 (67) | 58.8 (77) | 46.5 (66) | 53.9 (210) | 0.028 |
| Father | 27.4 (32) | 19.1 (25) | 35.9 (51) | 27.7 (108) | |
| Other adult relative | 15.4 (18) | 22.1 (29) | 17.6 (25) | 18.5 (72) | |
| Family size2,3 | 8.59 ± 3.63 | 8.38 ± 3.07 | 7.97 ± 3.36 | 8.30 ± 3.31 | 0.316 |
| Wealth index1 | |||||
| Poor and below | 47.2 (42) | 47.9 (57) | 25.2 (28) | 39.8 (127) | <0.001 |
| Middle | 27 (24) | 25.2 (30) | 13.5 (15) | 21.6 (69) | |
| Wealthy and above | 25.8 (23) | 26.9 (32) | 61.2 (68) | 38.6 (123) | |
| HFIAS4 | 10.2 ± 5.3 | 9.7 ± 6.0 | 8.0 ± 5.2 | 9.0 ± 5.7 | 0.011 |
| Years living in refugee area3 | 5.1 ± 1.8 | 4.8 ± 1.8 | 4.1 ± 1.3 | 4.7 ± 1.7 | <0.001 |
| Infant sex1 | |||||
| Male | 43.4 (43) | 48.4 (61) | 62.4 (83) | 52.2 (187) | 0.009 |
| Infant birthweight1,4 | 3.0 ± 0.4 | 3.0 ± 0.5 | 3.2 ± 0.5 | 3.1 ± 0.5 | <0.001 |
| Maternal education2 | |||||
| No formal education | 49.6 (58) | 45.8 (60) | 18.3 (26) | 36.9 (144) | <0.001 |
| Lower primary | 17.1 (20) | 22.9 (30) | 21.8 (31) | 20.8 (81) | |
| Upper primary | 26.5 (31) | 26.7 (35) | 38 (54) | 30.8 (120) | |
| Secondary and higher | 6.8 (8) | 4.6 (6) | 21.8 (31) | 11.5 (45) | |
| Ethnicity2 | |||||
| Dinka | 96.0 (95) | 88.8 (111) | 16.1 (20) | 65.0 (226) | <0.001 |
| Madi | 3.0 (3) | 11.2 (14) | 66.9 (83) | 28.7 (100) | |
| Other | 1.0 (1) | 0.0 (0) | 16.9 (21) | 6.3 (22) | |
| Religion2 | |||||
| Catholic | 2.6 (3) | 16.8 (22) | 50.6 (72) | 24.9 (97) | <0.001 |
| Anglican | 71.8 (84) | 71.0 (93) | 24.7 (35) | 54.4 (212) | |
| Other | 25.6 (30) | 12.2 (16) | 24.7 (35) | 20.8 (81) | |
| Mother’s current age4 | 27.5 ± 4.9 | 28.4 ± 5.0 | 27.3 ± 5.2 | 27.7 ± 5.1 | 0.185 |
| Infant delivery place1 | |||||
| Local health center | 68.7 (68) | 78.6 (99) | 70.5 (93) | 72.8 (260) | 0.022 |
| Private health center | 2.0 (2) | 0.8 (1) | 0.8 (1) | 1.2 (4) | |
| Hospital | 21.2 (21) | 19.8 (25) | 28.0 (37) | 23.2 (83) | |
| Home and other area | 8.1 (8) | 0.8 (1) | 0.8 (1) | 2.8 (10) | |
| ANC1 | |||||
| Optimal | 23.2 (23) | 22.2 (28) | 14.8 (20) | 19.7 (71) | 0.190 |
| PNC1 | |||||
| Optimal | 21.2 (21) | 22.2 (28) | 25.2 (34) | 23.1 (83) | 0.747 |
Abbreviations: ANC, antenatal care visit (≥routine 8 visits to a health center during pregnancy); HFIAS, Household Food Insecurity Access Scale; PNC, prenatal care visits (≥ routine 4 visits in < 6 wk after birth)
Variables collected at midline-I after the infant was born
Variables collected at Endline;
Mean scores and standard deviations respectively;
Study arm means differences performed with ANOVA;
Proportion differences among study arms tested using chi-square; Sig. statistical significance.
More than half of the mothers in the parents-combined arm (59.8%) had an education of upper primary or higher than those in the mothers-only (31.3%) and the control (33.3%) study arms. The Dinka were the most prevalent ethnic group (65.0%) among all participants in the study. Additionally, most of the mothers in the control arm (71.8%) and the mothers-only arm (71.0%) were of the Anglican religion compared with the 24.7% in the parents-combined arm.
Most mothers (≥97.2%) in this study delivered at a health facility with skilled care. However, more than three-quarters (≥80.3%) of the mothers did not meet the WHO recommendations of a minimum of eight antenatal visits before infant delivery. Similarly, less than a quarter (23.1%) of all mothers attended the recommended minimum four postnatal care visits within the first 6 wk after giving birth.
Maternal social support
Results in Table 2a show that overall, spouses were the mothers’ best source of social support in all study arms during the two study periods when children began receiving complementary feeding. Further, mothers in the parents-combined arm had the highest spousal support at both the Midline-II (51.2%) and Endline (61.3%) periods. Likewise, the mothers in the parents-combined arm had the highest proportion of moderate to high social support at both Midline-II (84.3%) and the Endline period (94.6%). The lowest proportion of moderate to high social support was among the mothers in the control arm for both Midline-II (19.6%) and Endline (6.8%) periods. Furthermore, results in Table 2b indicated that there were significant differences in the mean social support scores among the three arms at Midline-II (F (2, 335) = 92.8, P < 0.001) and at Endline (F (2, 315) = 539.5, P < 0.001). The results in Table 2c showed that mothers in the parents-combined arm had higher mean social support scores than the mothers-only arm at both Midline-II [mean difference (MD) = 10.3, P < 0.001] and Endline (MD = 27.7, P < 0.001). Similarly, the parents-combined arm had higher social support scores than the control at Midline-II and the Endline periods (MD = 25.2, P < 0.001, and MD = 44.0, P < 0.001, respectively). The mothers-only treatment arm also had better maternal social support scores than the control at both Midline-II (MD = 15.0, P < 0.001) and the Endline period (MD = 16.3, P < 0.001).
TABLE 2a.
Maternal social support characteristics
| Variables | Midline-II |
Endline |
||||||
|---|---|---|---|---|---|---|---|---|
| C |
M |
M&F |
Total |
C |
M |
M and F |
Total |
|
| % (n) | % (n) | % (n) | % (n) | % (n) | % (n) | % (n) | % (n) | |
| Support the mother most | ||||||||
| Husband | 35.9 (33) | 45.6 (57) | 51.2 (62) | 45.0 (152) | 52.2 (46) | 40.3 (48) | 61.3 (68) | 50.9 (162) |
| Peers or Neighbors | 16.3 (15) | 13.6 (17) | 16.5 (20) | 15.4 (52) | 11.4 (10) | 10.9 (13) | 8.1 (9) | 10.1 (32) |
| Other relatives | 34.8 (32) | 25.6 (32) | 23.1 (28) | 27.2 (92) | 21.6 (19) | 30.3 (36) | 21.6 (24) | 24.8 (79) |
| Other | 1.0 (1) | 2.4 (3) | 0.9 (1) | 1.5 (5) | 6.8 (6) | 4.2 (5) | 4.5 (5) | 5.0 (16) |
| No one | 12.0 (11) | 12.8 (16) | 8.3 (10) | 10.9 (37) | 8.0 (7) | 14.3 (17) | 4.5 (5) | 9.2 (29) |
| Maternal Social support1 | ||||||||
| Very low or none | 6.5 (6) | 1.6 (2) | 1.7 (2) | 3.0 (10) | 17.0 (15) | 5.0 (6) | 1.8 (2) | 7.2 (23) |
| Low | 73.9 (68) | 36.0 (45) | 14.0 (17) | 38.5 (130) | 76.1 (67) | 33.6 (40) | 3.6 (4) | 34.9 (111) |
| Moderate | 17.4 (16) | 54.4 (68) | 49.6 (60) | 42.6 (144) | 4.5 (4) | 49.6 (59) | 21.6 (24) | 27.4 (87) |
| Optimal/high | 2.2 (2) | 8.0 (10) | 34.7 (42) | 16.0 (54) | 2.3 (2) | 11.8 (14) | 73.0 (81) | 30.5 (97) |
| Total social support score (%) | ||||||||
| Mean ± SD | 38.6 ± 9.7 | 53.5 ± 14.8 | 63.8 ± 14.3 | 53.2 ± 13.0 | 34.6 ± 9.5 | 51.0 ± 11.8 | 78.7 ± 6.7 | 56.0 ± 9.3 |
Abbreviations: C, control; M, mothers-only; M and F, parents-combined arms.
Maternal perceived social support mean score categorized into optimal (>4 and ≤5); moderate (>3 and ≤4), low (>2 and ≤3), and none or very low support (≤2) Sherbourne and Stewart (1991).
TABLE 2b.
Maternal social support among study arms in Adjumani postemergency settlements
| Midline-II | Endline | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Study arm | N | Mean ± SD | SE | F | P value | N | Mean ± SD | S. E | F | P value |
| Control | 92 | 38.5 ± 9.7 | 1.0 | 92.79 | <0.001 | 88 | 34.6 ± 9.4 | 1.0 | 539.5 | < 0.001 |
| Mothers-only | 125 | 53.5 ± 14.8 | 1.3 | 119 | 51.0 ± 11.8 | 1.1 | ||||
| Parents-combined | 121 | 63.8 ± 14.3 | 1.3 | 111 | 78.7 ± 6.7 | 0.6 | ||||
TABLE 2c.
Pairwise comparisons of maternal social support and study arms in Adjumani postemergency settlements
| Midline-II | Endline | ||||
|---|---|---|---|---|---|
| (I) Study arms | (J) Study arms | MD (I-J) | SE | MD (I-J) | SE |
| Mothers-only | Control | 15.0∗∗∗ | 1.9 | 16.3∗∗∗ | 1.3 |
| Parents-combined | −10.3∗∗∗ | 1.7 | −27.7∗∗∗ | 1.3 | |
| Parents-combined | Control | 25.2∗∗∗ | 1.9 | 44.0∗∗∗ | 1.4 |
| Mothers-only | 10.3∗∗∗ | 1.7 | 27.7∗∗∗ | 1.3 | |
MD-mean difference; Tukey HSD correction applied for unequal sample sizes; ∗P < 0.05, ∗∗ P < 0.01, ∗∗∗ P < 0.001
Complementary feeding practices of infants
The complementary feeding practices (IYCF) of mothers in the Adjumani district postemergency settlements are reported in Table 3. Most (≥87.4%) of the refugee mothers in both the mothers-only and parents-combined arms introduced their infants to solid and semisolid foods (ISSSF) during the 6 to 8 mo age period. In contrast, less than two-thirds of mothers in the control arm (66.2% at Midline-II and 65.6% at Endline) had ISSSF between 6 and 8 mo of age. By the end of the study, less than half of the infants (age range, 6–11 mo) in all arms met the MDD. In the parents-combined arm 47% of infants were reported to have consumed ≥5 of 8 food groups, followed by infants in the mothers-only (34.0%) and control (24.1%) arms. By the end of the study, >81.8% of infants in all arms met the MMF.
TABLE 3.
Complementary feeding of infants in the Adjumani postemergency settlements.
| Infant Complementary feeding indicators | Midline-II period |
Endline period |
||||||
|---|---|---|---|---|---|---|---|---|
| C |
M |
M and F |
C |
M |
M and F |
|||
| n (%) | n (%) | n (%) | Sig1 | n (%) | n (%) | n (%) | Sig1 | |
| Introduction of solid, semisolid, and soft foods2 | ||||||||
| No | 33.8 (23) | 12.0 (9) | 12.6 (11) | 0.001 | 34.4 (22) | 11.1 (9) | 11.5 (10) | <0.001 |
| Yes | 66.2 (45) | 88.0 (66) | 87.4 (76) | 65.6 (42) | 88.9 (72) | 88.5 (77) | ||
| Minimum ≥5 of 8 food groups3 | ||||||||
| Did Not Meet | 87.3 (62) | 81.1 (60) | 71.0 (66) | 0.037 | 75.9 (66) | 66.0 (66) | 52.8 (56) | 0.004 |
| Met | 12.7 (9) | 18.9 (14) | 29.0 (27) | 24.1 (21) | 34.0 (34) | 47.2 (50) | ||
| Minimum meal frequency3 | ||||||||
| Did Not Meet | 25.4 (18) | 14.9 (11) | 14.0 (13) | 0.125 | 18.2 (16) | 12.1 (12) | 13.3 (14) | 0.464 |
| Met | 74.6 (53) | 85.1 (63) | 86.0 (80) | 81.8 (72) | 87.9 (87) | 86.7 (91) | ||
| Minimum acceptable diet3 | ||||||||
| Did Not Meet | 87.3 (62) | 83.8 (62) | 74.2 (69) | 0.081 | 75.9 (66) | 62.0 (62) | 57.5 (61) | 0.025 |
| Met | 12.7 (9) | 16.2 (12) | 25.8 (24) | 24.1 (21) | 38.0 (38) | 42.5 (45) | ||
| Egg and/or flesh food consumption3 | ||||||||
| No | 91.5 (65) | 87.8 (65) | 73.1 (68) | 0.004 | 81.8 (72) | 71.0 (71) | 67.0 (71) | 0.055 |
| Yes | 8.5 (6) | 12.2 (9) | 26.9 (25) | 18.2 (16) | 29.0 (29) | 33.0 (35) | ||
Abbreviations: C, control study arm; M, mothers-only, M and F, parents-combined; Sig., statistical significance.
Chi-square test for differences in proportions of feeding practices between groups within the study period
Calculated for children between 6 and 8 mo.
Calculated for infants aged 6–23 mo.
Additionally, by the end of the study, more than one-third (≥38.0%) of the infants in the mothers-only and parents-combined arms met the MAD compared with infants in the control arm (24.1%). By the end of the study, the highest proportion of infants who consumed eggs and or flesh foods (EFF) was in the parents-combined arm (33.0%), followed by the mothers-only arm (29.0%) and the control arm (18.2%) but these results were not significantly different (P = 0.055). However, significantly more infants in the parents-combined arm had begun EFF consumption (26.9%) by Midline-II, whereas EFF consumption among infants was low in the mothers-only (12.2%) and control (8.5%) arms.
Effect of the care group intervention on complementary feeding of infants
Significant associations were observed between mothers’ involvement in the care groups and the complementary feeding practices of infants (Table 4 and Supplementary Figure 2).
TABLE 4.
Association between infant complementary feeding practices and the care group intervention
| Midline-II Period |
Endline period |
|||||||
|---|---|---|---|---|---|---|---|---|
| Unadjusted |
P value | Adjusted |
P value | Unadjusted |
P value | Adjusted |
P value | |
| OR (95% CI) | AOR1 (95% CI) | OR (95% CI) | AOR1 (95% CI) | |||||
| Introduction of solid, semisolid, and soft foods | ||||||||
| Mothers-only | 3.7 (1.59, 8.85) | 0.003 | 4.0 (1.47, 10.69) | 0.007 | 4.2 (1.77, 9.94) | 0.001 | 3.8 (1.41, 10.34) | 0.008 |
| Parents-combined | 3.1 (1.57, 7.92) | 0.002 | 4.5 (1.46, 14.13) | 0.009 | 4.0 (1.75, 9.31) | 0.001 | 3.4 (1.01, 11.33) | 0.048 |
| Minimum dietary diversity | ||||||||
| Mothers-only | 1.6 (0.65, 3.99) | 0.306 | 1.6 (0.56, 4.34) | 0.330 | 1.6 (0.85, 3.08) | 0.141 | 1.8 (0.89, 3.70) | 0.099 |
| Parents-combined | 2.8 (1.22, 6.46) | 0.014 | 1.6 (0.53, 4.90) | 0.387 | 2.8 (1.5, 5.23) | 0.001 | 3.0 (1.33, 6.64) | 0.014 |
| Minimum meal frequency | ||||||||
| Mothers-only | 1.9 (0.84, 4.48) | 0.118 | 2.7 (1.03, 7.23) | 0.043 | 1.6 (0.72, 3.63) | 0.246 | 2.7 (0.99, 7.28) | 0.055 |
| Parents-combined | 2.1 (0.95, 4.62) | 0.069 | 3.4 (1.14, 10.10) | 0.028 | 1.4 (0.66, 3.15) | 0.356 | 2.3 (0.77, 7.18) | 0.134 |
| Minimum acceptable diet | ||||||||
| Mothers-only | 1.3 (0.52, 3.39) | 0.546 | 1.1 (0.40, 3.25) | 0.845 | 1.9 (1.02, 3.64) | 0.043 | 2.3 (1.13, 4.63) | 0.021 |
| Parents-combined | 2.4 (1.04, 5.55) | 0.041 | 1.4 (0.43, 4.37) | 0.586 | 2.3 (1.24, 4.33) | 0.008 | 2.7 (1.20, 6.00) | 0.016 |
| Egg and/or flesh food consumption | ||||||||
| Mothers-only | 1.5 (0.50, 4.46) | 0.723 | 1.3 (0.34, 4.42) | 0.532 | 1.8 (0.92, 3.67) | 0.085 | 2.1 (0.99, 4.50) | 0.055 |
| Parents-combined | 4.0 (1.53, 10.34) | 0.043 | 3.3 (1.03, 10.36) | 0.036 | 2.2 (1.12, 4.36) | 0.021 | 2.4 (1.01, 5.14) | 0.031 |
Abbreviations: AOR, adjusted odds ratios; OR, crude odds ratios. Control arm – reference category
Results adjusted for the household head, food insecurity, wealth index, years spent in refugee settlement, maternal education, who supports the mother most, ethnicity, body mass index, religion, child sex, birthweight
ISSSF
There were significant associations between the care group intervention and ISSSF among mothers in the Adjumani postemergency settlements (Table 4). Infants of mothers in the mothers-only arm were more likely to receive ISSSF at both the Midline-II [adjusted odds ratio (AOR) = 4.0, 95% CI: 1.47, 10.69, P = 0.007] and the Endline (AOR = 3.8, CI: 1.41, 10.34, P = 0.008) study periods compared with the control arm. Similarly, infants in the parents-combined arm were more likely to receive ISSSF at both the Midline-II (AOR = 4.5, CI: 1.46, 14.13, P = 0.009) and Endline (AOR = 3.4, CI: 1.01, 11.33, P = 0.048). In this study, infants of mothers in the care groups were associated with better infant ISSSF than the infants in the control arm.
Infant MDD
A significant association between participation in the parents-combined arm and infant MDD was reported by the end of the study (Table 4). Infant MDD was better for infants in the parents-combined arm (AOR = 3.0, CI: 1.33, 6.64, P = 0.014) when compared with the control arm.
Infant MMF
Infants in the parents-combined arm were more likely to have met MMF at the Midline-II (AOR = 3.4, CI: 1.14, 10.10, P = 0.028) but were not significantly better than the control arm at the end of the study. In the mothers-only arm, infants showed significantly improved odds of meeting MMF at Midline-II (AOR = 2.7, CI: 1.03, 7.23, P = 0.043) but were only marginally improved by Endline (AOR = 2.7, CI: 0.99, 7.28, P = 0.055) compared with the control.
Infant MAD
Significant associations between infant MAD and parent participation in the care group intervention were observed by the end of our study. Infants of mothers who participated in either the mothers-only (AOR = 2.3, CI: 1.13, 4.63, P = 0.021) or parents-combined (AOR = 2.7, CI: 1.20, 6.00, P = 0.016) arms were more likely to have met MAD.
Infant consumption of EFF
Our findings showed that infants whose parents were in the parents-combined arm were more likely to consume EFF earlier (at Midline-II; AOR = 3.3, CI: 1.03, 10.36, P = 0.036) and at Endline (AOR = 2.4, CI: 1.01, 5.14, P = 0.031). The infants in the mothers-only arm showed marginal improvements in consumption of EFF by the end of the study (AOR = 2.1, CI: 0.99, 4.50, P = 0.055)
In summary, over the study period, mothers in the care group intervention arms were more likely to follow complementary feeding guidelines than mothers in the control arm. By the end of the study, infants in both treatment arms had significantly better ISSSF and MAD. Infant MDD and EFF were significantly improved in the parents-combined study arm. Infant MMF and EFF were marginally improved for infants whose mothers participated in the mothers-only study arm.
Maternal social support and complementary feeding of infants
Associations between complementary feeding indicators and the extent of maternal social support were not significant during the Midline-II period (Table 5). However, by Endline, infants of mothers with higher social support were more likely to have met the MDD, MAD, and EFF. Mothers with optimal social support had infants that were three times more likely to meet MDD (AOR = 3.3, CI: 1.02, 10.63, P = 0.046) and MAD (AOR = 3.6, CI: 1.12, 11.69, P = 0.032), and >4 times more likely to feed eggs or flesh food to their infant (AOR = 4.7, CI: 1.18, 18.87, P = 0.028) in the Adjumani district postemergency settlements.
Table 5.
Association of maternal social support1 on complementary feeding of infants.
| Midline-II Period |
Endline period |
|||||||
|---|---|---|---|---|---|---|---|---|
| Unadjusted |
P value | Adjusted |
P value | Unadjusted |
P value | Adjusted |
P value | |
| OR (95% CI) | AOR2 (95% CI) | OR (95% CI) | AOR2 (95% CI) | |||||
| Introduction of solid, semisolid, and soft foods | ||||||||
| Low social support | 1.9 (0.42, 8.79) | 0.392 | 1.3 (0.19, 8.39) | 0.677 | 1.1 (0.31, 3.69) | 0.919 | 1.0 (0.27, 3.49) | 0.962 |
| Moderate social support | 3.3 (0.71, 15.4) | 0.126 | 2.2 (0.31, 15.67) | 0.387 | 2.4 (0.61, 9.68) | 0.209 | 2.1 (0.48, 8.89) | 0.325 |
| Optimal social support | 5.6 (0.87, 16.19) | 0.070 | 6.5 (0.55, 19.46) | 0.138 | 2.1 (0.57, 7.95) | 0.259 | 1.7 (0.18, 3.05) | 0.681 |
| Minimum dietary diversity | ||||||||
| Low social support | 1.6 (0.18, 14.21) | 0.655 | 2.4 (0.26, 15.26) | 0.443 | 1.1 (0.40, 3.10) | 0.836 | 1.4 (0.46, 4.48) | 0.531 |
| Moderate social support | 2.1 (0.24, 17.97) | 0.502 | 2.5 (0.27, 15.54) | 0.413 | 1.2 (0.44, 3.71) | 0.656 | 1.7 (0.52, 5.41) | 0.384 |
| Optimal social support | 2.2 (0.23, 20.33) | 0.503 | 2.8 (0.28, 21.26) | 0.380 | 2.4 (0.88, 6.81) | 0.088 | 3.3 (1.02, 10.63) | 0.046 |
| Minimum meal frequency | ||||||||
| Low social support | 0.6 (0.07, 4.95) | 0.611 | 0.6 (0.04, 8.39) | 0.698 | 0.8 (0.21, 2.91) | 0.713 | 0.8 (0.19, 3.38) | 0.771 |
| Moderate social support | 0.7 (0.08, 6.07) | 0.744 | 0.8 (0.06, 10.89) | 0.852 | 1.0 (0.25, 4.16) | 0.981 | 1.5 (0.32, 6.99) | 0.612 |
| Optimal social support | 0.8 (0.08, 8.31) | 0.873 | 0.9 (0.06, 12.58) | 0.913 | 1.1 (0.29, 4.53) | 0.844 | 1.7 (0.36, 8.12) | 0.499 |
| Minimum acceptable diet | ||||||||
| Low social support | 1.5 (0.18, 13.29) | 0.702 | 2.4 (0.29, 20.33) | 0.416 | 1.5 (0.53, 4.53) | 0.428 | 1.9 (0.60, 5.94) | 0.273 |
| Moderate social support | 1.9 (0.22, 16.04) | 0.572 | 2.2 (0.26, 18.08) | 0.479 | 1.7 (0.57, 5.32) | 0.330 | 2.3 (0.71, 7.30) | 0.169 |
| Optimal social support | 1.5 (0.15, 14.64) | 0.727 | 2.0 (0.19, 19.77) | 0.568 | 2.7 (0.93, 8.05) | 0.068 | 3.6 (1.12, 11.69) | 0.032 |
| Egg and flesh food consumption | ||||||||
| Low social support | 1.2 (0.14, 10.79) | 0.855 | 0.9 (0.05, 13.98) | 0.923 | 1.7 (0.46, 6.20) | 0.430 | 2.0 (0.50, 7.99) | 0.333 |
| Moderate social support | 1.5 (0.17, 13.18) | 0.705 | 0.9 (0.06, 13.50) | 0.944 | 2.9 (0.77, 10.88) | 0.116 | 3.3 (0.80, 13.61) | 0.098 |
| Optimal social support | 1.8 (0.19, 17.37) | 0.605 | 0.7 (0.04, 12.30) | 0.779 | 3.4 (0.93, 12.31) | 0.065 | 4.7 (1.18, 18.87) | 0.028 |
Abbreviations: OR-crude odds ratios; AOR-adjusted odds ratios; ISSSF- Introduction of solid, semi-solid, and soft foods; MDD-Minimum dietary diversity; MFF- Minimum meal frequency; MAD-Minimum acceptable diet; EFF-Egg and flesh food consumption.
Maternal social support mean score categorized into optimal (>4 and ≤5); moderate (>3 and ≤4), low (>2 and ≤3), and none or very low support (≤2) Sherbourne and Stewart (1991); none or very low support – reference category; C – control, M- Moms-only, M&D-Moms & Dads combined study arms
Results adjusted for the household head, food insecurity, years spent in refugee settlement, who supports the mother most, maternal occupation, age, education, ethnicity, religion, number of living children
Discussion
To our knowledge, this was the first RCT to examine the effects of a peer-led integrated nutrition education intervention using the care group model on complementary feeding practices of infants among refugee settlements in Uganda. We hypothesized that 1) maternal participation in the care group intervention would improve complementary feeding practices of infants in refugee settlements, and 2) the care group intervention would improve maternal social support concerning complementary feeding of infants.
In our study, the care group model supported peer-to-peer nutritional training on the complementary feeding of infants using visual aids with key messages [43]. Short questions included in each module facilitated discussion among members and promoted dialog and understanding of the concepts of recommended practices in the treatment arms. Further, activities such as vegetable gardening and cooking demonstrations in the care groups encouraged more nutrient-dense recipes for infants. Peer-to-peer home visits and peer support emphasized accountability on feeding and infant care practices within the care groups [55].
This study demonstrated that appropriate ISSSF was more likely for infants whose mothers had participated in the care group interventions compared with infants of mothers in the control arm. A study from Malawi [56] highlighted the value of local food preparation demonstrations as a means for mothers to taste and examine the consistency of appropriate foods for infants. Thus, building the capacity of mothers improved the timing of ISSSF, as well as the quality of infant food. Our findings also supported a systematic review of multiple trials [14] on complementary feeding which reported that nutrition education interventions reduced the practice of untimely ISSSF for infants. Additionally, caretakers learning and observing peers performing desired behaviors normalized the behaviors and enhanced diffusion of improved preparation of infant complementary foods to maximize nutrient retention for the child’s growth and development [57]. Our findings emphasize the importance of the care group model among postemergency refugee communities as a caregiver-centered behavior change communication strategy for timely infant ISSSF.
By the study’s end, infants of mothers in the parents-combined care groups had significantly better MDD than those in the control. RCTs from Kenya [17] and Uganda [58] likewise reported that caretakers who participated in integrated nutrition training provided their children (aged 6–48 mo) with more food groups including flesh foods and vegetables than those without training. The training modules in our intervention on healthy nutrition emphasized eating a variety of foods categorized under proteins, vitamins, minerals, and carbohydrate-rich foods demonstrated under the grow, glow, and go themes for easier comprehension among the caretakers. Similarly, a joint program evaluation in Bangladesh, Malawi, Peru, and Zambia [59] and a study from Malawi [56] reported that mothers’ groups were effective in improving dietary quality and quantity due to participatory nutritional counseling and simultaneous cooking demonstrations.
Our care group cooking demonstrations showed participants options for nutritious meals for infants, such as a sorghum or millet porridge blended with peanut paste or an egg. Such a combination would provide carbohydrates, protein, lipids, and important micronutrients beneficial for infant growth while using locally available foods [60]. Likewise, studies in Ethiopia [61,62] demonstrated that mothers who participated in SBCC interventions such as meal preparation demonstrations had children with better MDD than the children of caretakers in the control arms. Our findings provide additional evidence for the impact of the care group model as an integrative SBCC approach in improving the consumption of a variety of food groups among infants at 6 mo and beyond. The lack of significance at the Midline-II yet better MDD observed at the Endline period may be explained by the need for a relatively longer period for the care group intervention to positively influence the MDD practices. Additionally, the time variability of ISSSF for infants even at the 6–8 mo of age recommended by WHO and UNICEF guidelines [30] may have affected the infant’s consumption of a variety of foods.
At Midline-II, significant beneficial effects of the care group interventions on infant MMF were observed in both mothers-only and parents-combined arms. Meal frequency is important in these younger infants because of the very rapid rate of growth during early infancy [63,64]; furthermore, smaller consumption capacity means that frequency of meal consumption is especially important for optimal growth in younger infants. Our significant findings during this study period were consistent with RCTs in Ethiopia [37], and rural China [65] that reported improved MMF among infants (<12 mo of age) of mothers participating in SBCC-centered interventions in their communities. Similarly, a recent systematic review [66] and a meta-analysis [67] of peer group nutrition interventions reported an increase in the likelihood of MMF. Child–caregiver engagement in a cooking demonstration together with educational counseling created positive changes in child feeding practices concerning the frequency of meals. However, our study findings showed that by Endline, infants of mothers in the treatment arms no longer showed significantly higher odds for better MMF scores. Studies in Ethiopia [68,69] which examined children ≤24 mo of age compared with those aged <12 mo in our study reported 2 or more times better odds of meeting infant MMF in their treatment groups than that for the control group. These studies suggested that the longer exposure of child caregivers to SBCC nutrition messages created improved and lasting practices of child feeding including the number of child meals.
Despite the coronavirus disease 2019 (COVID-19) pandemic, our findings revealed that by the end of our study, both mothers-only and parents-combined arms had significantly better infant MAD when compared with the control arm. Our findings were consistent with the reports from Ethiopia [37] and Kenya [17] of better MAD, MDD, and MMF among children whose caretakers participated in complementary feeding behavior change communication interventions. In our care group intervention, in addition to peer-led dialog, emphasis on the value of local foods together with the cooking demonstrations provided an understanding of both optimal quality and quantities of meals thus likely improving MAD for infants in the intervention groups. In addition to the food demonstrations, the nutrition training materials had pictures of nutritious foods that were informative both during the care group meetings and the peer-to-peer home visits. These materials were easily understandable with limited literacy.
EFF remained low throughout the study. An RCT in Western Uganda [58] attributed the low consumption of EFF to the high cost of these foods. Further, findings from 11 countries [70], explained that the limited availability of eggs and their low shelf life reduced the purchase of EFF for consumption by infants. However, by the end of our study, infants of mothers in the care group interventions were 2 times more likely to consume EFF when compared with the control arm. Studies in Kenya [17,71] also emphasized the importance of integrated education, nutrition, and agricultural programs in addressing barriers like myths related to delayed speech and prohibitive notions about the consumption of EFF. Based on our findings we suggest that programs targeting the improvement of EFF in postemergency settlements should consider integrating nutrition-sensitive agricultural activities such as poultry rearing to increase sources of EFF. For example, recent studies in Ghana [72] and Ethiopia [73,74] showed that providing mothers with local chickens to rear in addition to nutritional education training [75] increased infant consumption of eggs.
The positive effect of the care group intervention on the complementary feeding of infants by the end of our study suggested that the intervention may be beneficial within the refugee postemergency context. The marginal improvements, especially in the mothers-only study arm, emphasize that the behavioral change approach among communities requires adherence to the treatment over a sufficient time for the desired change to take effect [76] and to provide significantly better infant practices. The infants of mothers in the care groups in our study received better complementary feeding than those in the control. These results were consistent with the findings of a comparative analysis study of five countries in Africa and Asia [20] which determined that countries that implemented the care group model through organizations demonstrated better infant and young child complementary feeding. Additionally, the parents-combined arm had better complementary feeding practices indicating that including fathers in the care group intervention provided additional support and motivation to the mothers.
Consistent with previous community-based studies [[77], [78], [79]] which reported that targeting fathers in behavior change nutrition programs increased the participation of fathers in child feeding beyond the traditional role of provision of food for the household, our findings suggest that future nutrition-sensitive programs should consider having more care groups with both mothers and fathers for even better maternal social support and complementary feeding of infants. For example, an Alive and Thrive technical brief [60] reported that adult males being prioritized for meats and flesh foods while infants were left to be fed porridges was a barrier in developing strategies for adequate complementary infant feeding. Therefore, engaging fathers in the care groups and similar social behavioral change interventions may positively impact child feeding practices.
This study reported that the mothers in the care group intervention had higher maternal social support than those in the control arm. Further, the parents-combined arm had significantly better mean social support scores compared with the mothers-only and control arms. Increased peer and spousal support may have been encouraged by our care group intervention because the role of fathers in infant feeding and childcare practices was emphasized through visual aids and key messages. A qualitative study from Tanzania [79] noted that fathers who received nutrition counseling improved spousal communication and engagement in household chores including feeding the children. Our study findings also revealed that the mothers who had higher social support scores were more likely to have infants that met MDD, MAD, and EFF. Likewise, studies in Zimbabwe [19] and Uganda [48] reported that children of mothers with greater social support were more likely to achieve MDD. Additionally, a study from western Kenya [71] showed that social support to mothers by fathers and grandmothers improved infants’ MDD, and a cross-sectional study in Uganda [48], reported that increased maternal social support was positively associated with infant MAD.
Our study found that the mothers in the parents-combined arm had higher social support and better complementary feeding practices for their infants. Studies in Kenya [80,81] also reported that fathers who participated in peer dialogs on nutrition-sensitive topics through intervention programs demonstrated positive behavioral change. The behavioral transformation among fathers led to increased acquisition and provision of nutritionally diverse diets to their children evidenced by both improved MDD and MAD. Fathers’ involvement in nutrition-sensitive farming like vegetable growing or keeping chickens for eggs as well as prioritization of flesh foods for children’s meals improved the complementary feeding of infants.
Our study provided evidence for the positive effects on infant complementary feeding practices by a peer-led integrated nutrition-sensitive intervention using care groups within refugee communities. Based on findings from this study, agencies supporting refugees in postemergencies may consider engaging more fathers and other caretakers in care group interventions to increase maternal social support and enhance complementary feeding practices for infants.
One challenge for our study was that the standard operating procedures implemented for safety to combat the spread of COVID-19 beginning in March 2020 [82] may have mitigated the potential of the care group model, a strategy built on enhanced peer support. In response to the COVID-19 threat, preventive measures [43] were integrated into the care group activities. Although no participants or research team members reported contracting COVID-19, we acknowledge that smaller peer support groups and fewer contacts may have minimized the potential impacts of the intervention [83]. Nevertheless, the findings in this study were consistent with previous trials conducted in rural community settings, and support recommendations for continued nutrition-sensitive interventions amidst pandemics such as COVID-19 to mitigate adverse effects on nutrition among vulnerable groups such as young children as well as pregnant and lactating women [84]. Another limitation was that recall bias may have affected the assessment of infant feeding practices based on the caregiver’s 24-h memory. Further, the assessment of perceived maternal social support may have been influenced by social desirability bias if mothers overstated or understated their perceived support. A strength of our study was the use of the randomized control study design which allowed the establishment of a causal association between the care group intervention and complementary feeding practices of infants. Further, the training of the care group leaders and routine monitoring of the activities of the care groups by the VHTs that worked with the researcher and district health and nutrition educators support the effectiveness and sustainability of the intervention and are a key strength of the study.
Our study intervention involved fathers in one of the study arms which showed significant improvements in the complementary feeding of infants. Future research may assess the experiences of maternal social support from other caretakers such as grandparents and older relatives within households having children under 2 y of age in postemergency settlements. Engaging older relatives in households having young children in a similar intervention may increase social support to a mother and improve infant and young child care, thus enhancing child nutrition.
Conclusion
A peer-led integrated nutrition education intervention through care groups improved complementary feeding practices of infants in postemergency settlements in Uganda. Our study illustrated that engaging fathers in the care group intervention had stronger effects on complementary feeding of infants than targeting mothers alone, although improvements in infant feeding practices were observed in both treatments. Humanitarian partners and refugee host countries may find integrative nutrition-focused programming using indirect strategies such as the care groups to be a cost effective, sustainable approach for the improvement of infant feeding practices among postemergency settlements in similar local contexts.
Funding
This research was funded by a grant from the Nestlé Foundation for the Study of Problems of Nutrition in the World, Switzerland, supplemented by the Marilynn Thoma Chair in Human Sciences, the Esther Winterfeldt Fellowship, and administrative funds from Oklahoma State University. The funders had no role in the design, implementation, analysis, or interpretation of the data.
Author disclosures
The authors report no conflicts of interest.
Data availability
The data described in the manuscript, code book, and analytic code will be made available upon request from the corresponding author.
Acknowledgments
We thank Dr. Ivan Muzira Mukisa, the Department Head of the School of Food Technology, Nutrition & Bio-Engineering at Makerere University Kampala for supporting this research. We would also like to thank Andrew Masaba, Deputy Program Coordinator at the Lutheran World Federation (LWF), Uganda for supporting this study. We also appreciate the support from the refugee settlement leadership including personnel from UNHCR, OPM settlement commandants of Pagirinya, Nyumanzi, Ayilo, and Refugee Welfare Councils. The authors’ responsibilities were as follows: JJK, CNW, HR, and BJS: designed the study; JJK conducted statistical analysis; KLC, HR, and BJS: advised on data analysis; JK developed the first draft of the manuscript; SRE, KLC, CNW, HR, MK, DH, BJS critically reviewed and revised manuscript; all authors read and approved the final manuscript.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.cdnut.2023.100042.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- 1.UNHCR, Figures at a Glance: UNHCR, Geneva, Switzerland; 2020. [Internet]. Available from: https://www.unhcr.org/en-us/figures-at-a-glance.html, Accessed January, 2022.
- 2.UNHCR, Global trends in forced displacement Geneva, Switzerland: UNHCR; 2020. [Internet]. Available from: https://www.unhcr.org/60b638e37/unhcr-global-trends-2020. Accessed January 2022.
- 3.UNHCR . UNHCR; Switzerland: 2020. Global report Geneva.https://reporting.unhcr.org/sites/default/files/gr2020/pdf/GR2020_English_Full_lowres.pdf#_ga=2.40980326.530398663.1646028267-223738670.1642515446 [Internet]. Available from: February 2022. [Google Scholar]
- 4.UNHCR, Government of Uganda . UNHCR; Switzerland: 2021. Refugees and Asylum-Seekers in Uganda - Uganda Refugee Response Geneva.https://data2.unhcr.org/en/documents/details/90182 [Internet] Available from: February 2022. [Google Scholar]
- 5.Blanchet K., Ramesh A., Frison S., Warren E., Hossain M., Smith J., et al. Evidence on public health interventions in humanitarian crises. Lancet. 2017;390:2287–2296. doi: 10.1016/S0140-6736(16)30768-1. [DOI] [PubMed] [Google Scholar]
- 6.Gee S., Vargas J., Foster A.M. We need good nutrition but we have no money to buy food": sociocultural context, care experiences, and newborn health in two UNHCR-supported camps in South Sudan. B.M.C. Int. Health. Hum. Rights. 2018;18:40. doi: 10.1186/s12914-018-0181-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Corbett M., Oman A. UNHCR/WFP; Geneva, Switzerland: 2006. Acute malnutrition in protracted refugee situations: a global strategy.https://www.unhcr.org/en-us/publications/operations/45fe62642/malnutrition-protracted-refugee-situations-global-strategy-joint-unhcr.html Accessed December 2021. [Google Scholar]
- 8.Buscher D. New approaches to urban refugee livelihoods, Refuge. Can.S J. Refugees. 2011;28:17–29. doi: 10.25071/1920-7336.36473. [DOI] [Google Scholar]
- 9.Black R.E., Allen L.H., Bhutta Z.A., Caulfield L.E., De Onis M., Ezzati M., et al. Maternal and child undernutrition: global and regional exposures and health consequences. Lancet. 2008;371:243–260. doi: 10.1016/S0140-6736(07)61690-0. [DOI] [PubMed] [Google Scholar]
- 10.Lassi Z.S., Das J.K., Zahid G., Imdad A., Bhutta Z.A. Impact of education and provision of complementary feeding on growth and morbidity in children less than 2 years of age in developing countries: a systematic review. B.M.C. Public. Health. 2013;13:1–10. doi: 10.1186/1471-2458-13-S3-S13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Rabbani A., Padhani Z.A., Siddiqui F.A., Das J.K., Bhutta Z. Systematic review of infant and young child feeding practices in conflict areas: what the evidence advocates. B.M.J. Open. 2020;10 doi: 10.1136/bmjopen-2020-036757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ministry of Health Uganda, Uganda Bureau of Statistics . 2020. Office of the Prime Minister Uganda, UNHCR. Food Security and Nutrition Assessment in Refugee Settlements and Kampala. Kampala: MOH and UNHCR Representation Office in Uganda.https://reliefweb.int/sites/reliefweb.int/files/resources/Refugee%20FSNA_Report_Final_Dec%202020_Aug%202021.pdf Accessed February 2022. [Google Scholar]
- 13.Style S., Tondeur M., Wilkinson C., Oman A., Spiegel P., Kassim I.A., et al. Operational guidance on the use of special nutritional products in refugee populations. Food. Nutr. Bull. 2013;34:420–428. doi: 10.1177/156482651303400407. [DOI] [PubMed] [Google Scholar]
- 14.Arikpo D., Edet E.S., Chibuzor M.T., Odey F., Caldwell D.M. Educational interventions for improving primary caregiver complementary feeding practices for children aged 24 months and under. Cochrane. Database. Syst. Rev. 2018;5:CD011768. doi: 10.1002/14651858.CD011768.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Majamanda J., Maureen D., Munkhondia T.M., Carrier J. The effectiveness of community-based nutrition education on the nutrition status of under-five children in developing countries. A systematic review. Malawi. Med. J. 2014;26:115–118. [PMC free article] [PubMed] [Google Scholar]
- 16.Perry H.B., Sacks E., Schleiff M., Kumapley R., Gupta S., Rassekh B.M., et al. Comprehensive review of the evidence regarding the effectiveness of community-based primary health care in improving maternal, neonatal and child health: 6. strategies used by effective projects. J. Glob. Health. 2017;7 doi: 10.7189/jogh.07.010906. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Waswa L.M., Jordan I., Herrmann J., Krawinkel M.B., Keding G.B. Community-based educational intervention improved the diversity of complementary diets in western Kenya: results from a randomized controlled trial. Public. Health. Nutr. 2015;18:3406–3419. doi: 10.1017/S1368980015000920. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Davis T.P., Wetzel C., Hernandez Avilan E., de Mendoza Lopes C., Chase R.P., Winch P.J., et al. Reducing child global undernutrition at scale in Sofala Province, Mozambique, using Care Group Volunteers to communicate health messages to mothers. Glob. Health. Sci. Pract. 2013;1:35–51. doi: 10.9745/GHSP-D-12-00045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Matare C.R., Mbuya M.N.N., Dickin K.L., Constas M.A., Pelto G., Chasekwa B., et al. Maternal capabilities are associated with child caregiving behaviors among women in rural Zimbabwe. J. Nutr. 2021;151:685–694. doi: 10.1093/jn/nxaa255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.George C.M., Vignola E., Ricca J., Davis T., Perin J., Tam Y., et al. Evaluation of the effectiveness of care groups in expanding population coverage of Key child survival interventions and reducing under-5 mortality: a comparative analysis using the lives saved tool (LiST) B.M.C. Public. Health. 2015;15:835. doi: 10.1186/s12889-015-2187-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Pieterse P., Matthews A., Walsh A., Chirwa E. Exploring how and why Care Groups work to improve infant feeding practices in low- and middle-income countries: a realist review protocol. Syst Rev. 2021;9:237. doi: 10.1186/s13643-020-01497-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Perry H., Morrow M., Borger S., Weiss J., DeCoster M., Davis T., et al. Care Groups I: an innovative community-based strategy for improving maternal, neonatal, and child health in resource-constrained settings. Glob. Health. Sci. Pract. 2015;3:358–369. doi: 10.9745/GHSP-D-15-00051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Perry H., Morrow M., Davis T., Borger S., Weiss J., DeCoster M., et al. Care Groups II: a summary of the maternal, neonatal and child health outcomes achieved in high-mortality, resource-constrained settings. Glob. Health. Sci. Pract. 2015;3:370–381. doi: 10.9745/GHSP-D-15-00052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Dall’Oglio I., Marchetti F., Mascolo R., Amadio P., Gawronski O., Clemente M., et al. Breastfeeding protection, promotion, and support in humanitarian emergencies: a systematic review of literature. J. Hum. Lact. 2020;36:687–698. doi: 10.1177/0890334419900151. [DOI] [PubMed] [Google Scholar]
- 25.Bhutta Z.A., Akseer N., Keats E.C., Vaivada T., Baker S., Horton S.E., et al. How countries can reduce child stunting at scale: lessons from exemplar countries. Am. J. Clin. Nutr. 2020;112 doi: 10.1093/ajcn/nqaa153. 894S–904S. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Wills T.A., Ainette M.C. In: Handbook of health psychology. Baum A., Revenson T.A., Singer J., editors. Psychology Press; New York: 2012. Social networks and social support; pp. 465–492. [Google Scholar]
- 27.World Health Organization . WHO; Geneva, Switzerland: 2008. Closing the gap in a generation: health equity through action on the social determinants of health; final report of the Commission on Social Determinants of Health.http://www.who.int/social_determinants/thecommission/finalreport/en/ Accessed February 2022. [Google Scholar]
- 28.Prudhon C., Benelli P., Maclaine A., Harrigan P., Frize J. Informing infant and young child feeding programming in humanitarian emergencies: an evidence map of reviews including low-and middle-income countries. Matern. Child. Nutr. 2018;14 doi: 10.1111/mcn.12457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Carroll G.J., Lama S.D., Martinez-Brockman J.L., Pérez-Escamilla R. Evaluation of nutrition interventions in children in conflict zones: a narrative review. Adv. Nutr. 2017;8:770–779. doi: 10.3945/an.117.016121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.WHO, UNICEF . World Health Organization, UNICEF; Geneva: 2021. Indicators for assessing infant and young child feeding practices: definitions and measurement methods.https://www.who.int/publications/i/item/9789240018389 Licence: CC BYNC- SA 3.0 IGO. Accessed February 2022. [Google Scholar]
- 31.Government of Uganda, United Nations, World Bank . In: Office of the Prime Minister. Uganda O.P.M., editor. 2017. The Refugee and Host Population Empowerment (ReHoPE) Strategic Framework, Uganda. Kampala, Uganda. [Google Scholar]
- 32.Crisp J. No solutions in sight: the problem of protracted refugee situations in Africa. Refug. Surv. Q. 2003;22:114–150. doi: 10.1093/rsq/22.4.114. [DOI] [Google Scholar]
- 33.Edwards G., Hellen K., Brownie S. Developing a work/study programme for midwifery education in East Africa. Midwifery. 2018;59:74–77. doi: 10.1016/j.midw.2018.01.007. [DOI] [PubMed] [Google Scholar]
- 34.Telfer M., Zaslow R., Chalo Nabirye R., Nalugo Mbalinda S. Review of midwifery education in Uganda: toward a framework for integrated learning and midwifery model of care. Midwifery. 2021;103 doi: 10.1016/j.midw.2021.103145. [DOI] [PubMed] [Google Scholar]
- 35.World Health Organization . World Health Organization; 2017. Primary Health Care Systems (PRIMASYS): case study from Uganda.https://apps.who.int/iris/handle/10665/341064 Accessed March 2022. [Google Scholar]
- 36.Turinawe E.B., Rwemisisi J.T., Musinguzi L.K., de Groot M., Muhangi D., de Vries D.H., et al. Selection and performance of village health teams (VHTs) in Uganda: lessons from the natural helper model of health promotion. Hum. Resour. Health. 2015;13:73. doi: 10.1186/s12960-015-0074-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Abiyu C., Belachew T. Effect of complementary feeding behavior change communication delivered through community-level actors on dietary adequacy of infants in rural communities of West Gojjam Zone, Northwest Ethiopia: a cluster-randomized controlled trial. PLoS One. 2020;15 doi: 10.1371/journal.pone.0238355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Fegan S., Bassett E., Peng Y., Steel O’Connor K. Adherence to complementary feeding recommendations for infants and implications for public health. Public. Health. Nutr. 2016;19:638–649. doi: 10.1017/S1368980015001433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Hanold M., Wetzel C., Davis T. technical and operational performance support program; Washington DC: 2014. Care-groups, A training manual for program design and implementation. [Google Scholar]
- 40.Food Security & Nutrition Network Social & Behavioral Change Task Force . Technical and Operational Performance Support Program; Washington D.C: 2014. Care groups: a training manual for program design and implementation. [Google Scholar]
- 41.Perry H., Morrow M., Davis T., Borger S., Weiss J., DeCoster M., et al. Care groups – an effective community-based delivery strategy for improving reproductive, maternal, neonatal, and child health in high-mortality. resource-constrained settings. 2014 doi: 10.9745/GHSP-D-15-00051. https://www.fsnnetwork.org/sites/default/files/resource_uploads/care_group_policy_guide_final_8_2014_0.pdf [Internet] Available from: June 2022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.UNICEF . United Nations Children’s Fund and University Research Co., LLC; New York: 2020. The community IYCF counselling cards for community workers. UNICEF. [Google Scholar]
- 43.UNICEF . UNICEF; New York: 2022. The community infant and young child feeding counselling package.https://www.unicef.org/documents/community-iycf-package [Internet]. Available from: March 2019. [Google Scholar]
- 44.Government of Uganda . Ministry of Health. Ministry of Health; Uganda: 2002. Village health team: participant manual for village health team members. Kampala, Uganda. [Google Scholar]
- 45.Ministry of Health Uganda . The Republic of Uganda Ministry of Health. Ministry of Health; Kampala: 2014. Uganda hospital and health centre IV census survey. [Google Scholar]
- 46.Ministry of Health Uganda . In: Kampala: The Republic of Uganda Ministry of Health. MOH, editor. 2015. Health Sector Development Plan 2015/16–2019/20. [Google Scholar]
- 47.Sherbourne C.D., Stewart A.L. The MOS social support survey. Soc. Sci. Med. 1991;32:705–714. doi: 10.1016/0277-9536(91)90150-b. [DOI] [PubMed] [Google Scholar]
- 48.Ickes S.B., Wu M., Mandel M.P., Roberts A.C. Associations between social support, psychological well-being, decision making, empowerment, infant and young child feeding, and nutritional status in Ugandan children ages 0 to 24 months. Matern. Child. Nutr. 2018;14 doi: 10.1111/mcn.12483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Walters C.N., Rakotomanana H., Komakech J.J., Stoecker B.J. Maternal determinants of optimal breastfeeding and complementary feeding and their association with child undernutrition in Malawi (2015-2016) B.M.C. Public. Health. 2019;19:1503. doi: 10.1186/s12889-019-7877-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Rakotomanana H., Gates G.E., Hildebrand D., Stoecker B.J. Situation and determinants of the infant and young child feeding (IYCF) indicators in Madagascar: analysis of the 2009 Demographic and Health Survey. B.M.C. Public. Health. 2017;17:812. doi: 10.1186/s12889-017-4835-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Kassa T., Meshesha B., Haji Y., Ebrahim J. Appropriate complementary feeding practices and associated factors among mothers of children age 6-23 months in Southern Ethiopia. B.M.C. Pediatr. 2015;16:131. doi: 10.1186/s12887-016-0675-x. 2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Kimani-Murage E.W., Madise N.J., Fotso J.C., Kyobutungi C., Mutua M.K., Gitau T.M., et al. Patterns and determinants of breastfeeding and complementary feeding practices in urban informal settlements, Nairobi Kenya. B.M.C. Public. Health. 2011;11:396. doi: 10.1186/1471-2458-11-396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Komakech J.J., Walters C.N., Rakotomanana H., Hildebrand D.A., Stoecker B.J. The associations between women's empowerment measures, child growth and dietary diversity: Findings from an analysis of demographic and health surveys of seven countries in Eastern Africa. Matern. Child. Nutr. 2022;18 doi: 10.1111/mcn.13421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Hjelm L., Mathiassen A., Miller D., Wadhwa A. World Food Programme; Rome, Italy: 2017. VAM guidance paper: creation of a wealth index. [Google Scholar]
- 55.Lowery C.M., Craig H.C., Litvin K., Dickin K.L., Stein M., Worku B., et al. Experiences engaging family members in maternal, child, and adolescent nutrition: a survey of global health professionals. Curr. Dev. Nutr. 2022;6 doi: 10.1093/cdn/nzac003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Hotz C., Gibson R.S. Participatory nutrition education and adoption of new feeding practices are associated with improved adequacy of complementary diets among rural Malawian children: a pilot study. Eur. J. Clin. Nutr. 2005;59:226–237. doi: 10.1038/sj.ejcn.1602063. [DOI] [PubMed] [Google Scholar]
- 57.Shi L., Zhang J. Recent evidence of the effectiveness of educational interventions for improving complementary feeding practices in developing countries. J. Trop. Pediatr. 2011;57:91–98. doi: 10.1093/tropej/fmq053. [DOI] [PubMed] [Google Scholar]
- 58.Kabahenda M., Mullis R., Erhardt J., Northrop-Clewes C., Nickols S. Nutrition education to improve dietary intake and micronutrient nutriture among children in less-resourced areas: a randomised controlled intervention in Kabarole district, western Uganda. S. Afr. J. Clin. Nutr. 2011;24:83–88. doi: 10.1080/16070658.2011.11734355. [DOI] [Google Scholar]
- 59.Sanghvi T., Seidel R., Baker J., Jimerson A. Using behavior change approaches to improve complementary feeding practices. Matern. Child. Nutr. 2017;13 doi: 10.1111/mcn.12406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Dewey K.G., Vitta B.S. Vol. 7. Alive & Thrive; Washington: 2017. (Strategies for ensuring adequate nutrient intake for infants and young children during the period of complementary feeding). [Google Scholar]
- 61.Dangura D., Gebremedhin S. Dietary diversity and associated factors among children 6-23 months of age in Gorche district, Southern Ethiopia: Cross-sectional study. B.M.C. Pediatr. 2017;17:6. doi: 10.1186/s12887-016-0764-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Kim S.S., Nguyen P.H., Yohannes Y., Abebe Y., Tharaney M., Drummond E., et al. Behavior change interventions delivered through interpersonal communication, agricultural activities, community mobilization, and mass media increase complementary feeding practices and reduce child stunting in Ethiopia. J. Nutr. 2019;149:1470–1481. doi: 10.1093/jn/nxz087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Roba K.T., O’Connor T.P., Belachew T., O’Brien N.M. Variations between post- and pre-harvest seasons in stunting, wasting, and Infant and Young Child Feeding (IYCF) practices among children 6-23 months of age in lowland and midland agro-ecological zones of rural Ethiopia. Pan. Afr. Med. J. 2016;24:163. doi: 10.11604/pamj.2016.24.163.9387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Dewey K.G., Begum K. Long-term consequences of stunting in early life. Matern. Child. Nutr. 2011;7:5–18. doi: 10.1111/j.1740-8709.2011.00349.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Shi L., Zhang J., Wang Y., Caulfield L.E., Guyer B. Effectiveness of an educational intervention on complementary feeding practices and growth in rural China: a cluster randomised controlled trial. Public. Health. Nutr. 2010;13:556–565. doi: 10.1017/S1368980009991364. [DOI] [PubMed] [Google Scholar]
- 66.Ahmed K.Y., Agho K.E., Page A., Arora A., Ogbo F.A. the Global Maternal and Child Health Research collaboration (GloMACH), Interventions to improve infant and young child feeding practices in Ethiopia: a systematic review. B.M.J. Open. 2021;11 doi: 10.1136/bmjopen-2021-048700. [DOI] [Google Scholar]
- 67.Janmohamed A., Sohani N., Lassi Z.S., Bhutta Z.A. The effects of community home visit and peer group nutrition intervention delivery platforms on nutrition outcomes in low and middle-income countries: a systematic review and meta-analysis. Nutrients. 2020;12 doi: 10.3390/nu12020440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Kim S.S., Rawat R., Mwangi E.M., Tesfaye R., Abebe Y., Baker J., et al. Exposure to large-scale social and behavior change communication interventions is associated with improvements in infant and young child feeding practices in Ethiopia. PLoS. One. 2016;11 doi: 10.1371/journal.pone.0164800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Kang Y., Kim S., Sinamo S., Christian P. Effectiveness of a community-based nutrition programme to improve child growth in rural Ethiopia: a cluster randomized trial. Matern. Child. Nutr. 2017;13 doi: 10.1111/mcn.12349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Headey D., Hirvonen K., Hoddinott J. Animal sourced foods and child stunting. Am. J. Agric. Econ. 2018;100:1302–1319. doi: 10.1093/ajae/aay053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Mukuria A.G., Martin S.L., Egondi T., Bingham A., Thuita F.M. Role of social support in improving infant feeding practices in Western Kenya: a quasi-experimental study. Glob. Health. Sci. Pract. 2016;4:55–72. doi: 10.9745/GHSP-D-15-00197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Dallmann D., Marquis G.S., Colecraft E.K., Kanlisi R., Aidam B.A. Maternal participation level in a nutrition-sensitive agriculture intervention matters for child diet and growth outcomes in rural Ghana. Curr. Dev. Nutr. 2022;6 doi: 10.1093/cdn/nzac017. nzac017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Alderman H., Gilligan D.O., Leight J., Mulford M., Tambet H. The role of poultry transfers in diet diversity: a cluster randomized intent to treat analysis. Food Policy. 2022;107 doi: 10.1016/j.foodpol.2021.102212. [DOI] [Google Scholar]
- 74.Passarelli S., Ambikapathi R., Gunaratna N.S., Madzorera I., Canavan C.R., Noor A.R., et al. A chicken production intervention and additional nutrition behavior change component increased child growth in Ethiopia: a cluster-randomized trial. J. Nutr. 2020;150:2806–2817. doi: 10.1093/jn/nxaa181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Kim S.S., Nguyen P.H., Tran L.M., Alayon S., Menon P., Frongillo E.A. Different combinations of behavior change interventions and frequencies of interpersonal contacts are associated with infant and young child feeding practices in Bangladesh, Ethiopia, and Vietnam. Curr. Dev. Nutr. 2019;4 doi: 10.1093/cdn/nzz140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Bellg A.J., Borrelli B., Resnick B., Hecht J., Minicucci D.S., Ory M., et al. Enhancing treatment fidelity in health behavior change studies: best practices and recommendations from the NIH Behavior Change Consortium, Health. Psychol. 2004;23:443. doi: 10.1037/0278-6133.23.5.443. [DOI] [PubMed] [Google Scholar]
- 77.Aoko L., Kiage B.N., Kyallo F.M. The participation of fathers in breastfeeding process: knowledge, beliefs, and practices in Kisumu, Kenya. Afr. J. Food Agric. Nutr. 2018:13634–13645. doi: 10.18697/ajfand.83.17120. [DOI] [Google Scholar]
- 78.Rakotomanana H., Walters C.N., Komakech J.J., Hildebrand D., Gates G.E., Thomas D.G., et al. Fathers’ involvement in child care activities: qualitative findings from the highlands of Madagascar. PLoS. One. 2021;16 doi: 10.1371/journal.pone.0247112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Martin S.L., Matare C.R., Kayanda R.A., Owoputi I., Kazoba A., Bezner Kerr R., et al. Engaging fathers to improve complementary feeding is acceptable and feasible in the Lake Zone, Tanzania. Matern. Child. Nutr. 2021;17 doi: 10.1111/mcn.13144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.DeLorme A.L., Gavenus E.R., Salmen C.R., Benard G.O., Mattah B., Bukusi E., et al. Nourishing networks: a social-ecological analysis of a network intervention for improving household nutrition in Western Kenya. Soc. Sci. Med. 2018;197:95–103. doi: 10.1016/j.socscimed.2017.11.023. [DOI] [PubMed] [Google Scholar]
- 81.Thuita F., Mukuria A., Muhomah T., Locklear K., Grounds S., Martin S.L. Fathers and grandmothers experiences participating in nutrition peer dialogue groups in Vihiga County, Kenya. Matern. Child. Nutr. 2021;17 doi: 10.1111/mcn.13184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Tumwesigye N.M., Denis O., Kaakyo M., Biribawa C. Center for Global Development Washington; Washington: 2021. Effects of the COVID-19 pandemic on health services and mitigation measures in Uganda. [Google Scholar]
- 83.Lai C.C., Shih T.P., Ko W.C., Tang H.J., Hsueh P.R. Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) and coronavirus disease-2019 (COVID-19): the epidemic and the challenges. Int. J. Antimicrob. Agents. 2020;55 doi: 10.1016/j.ijantimicag.2020.105924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Pérez-Escamilla R., Cunningham K., Moran V.H. COVID-19 and maternal and child food and nutrition insecurity: a complex syndemic. Matern. Child. Nutr. 2020;16 doi: 10.1111/mcn.13036. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data described in the manuscript, code book, and analytic code will be made available upon request from the corresponding author.