Abstract
Despite changes in the structure of contemporary families, little is known about extended family members—siblings, grandchildren, nieces/nephews, stepkin—who are primary caregivers for a relative living with dementia. Information about these caregivers is needed to help ensure their needs are understood by providers in health care and social service settings. The focus of this research was on the care situations of extended family caregivers and the impact of caregiving on their health and well-being. In Study 1, data from the National Study of Caregiving were used to describe the experiences of 107 extended family caregivers. In Study 2, case study techniques elicited additional information about the experiences of 10 extended family caregivers. Collectively, these caregivers provide care with little or no formal support and occasional help from a small informal network. Caregiving affected their physical and emotional health, depending on the strength of the relationship between the caregiver and the person living with dementia and the type of care provided. Findings contribute new knowledge about extended family caregivers and highlight the important role extended family dementia caregivers play and the challenges they face.
Keywords: Alzheimer’s disease, burden, home-care services, other caregivers
Nuclear family members (i.e., spouse/partners, adult children) provide most of the care for their relatives living with Alzheimer’s disease and other dementias (hereinafter referred to as dementia), but their availability as caregivers is shrinking. Societal trends, such as declining birthrates (Martin et al., 2021) and rising divorce rates among middle-aged and older adults (Mayol-García et al., 2021), raise questions about the sustainability of traditional approaches to family care. At the same time, greater longevity, and various social movements (e.g., civil rights, gender equity), legal and policy changes (e.g., marriage/divorce laws, social welfare), and social problems (e.g., incarceration trends) have led to a much broader array of family structures (Cohen, 2014; Roberto & Blieszner, 2015). Older adults are now likely to have expanded family boundaries beyond the level of the nuclear family. Their lives are embedded and closely linked to their extended family members including adult grandchildren (Geurts et al., 2012; Monserud, 2011), siblings (Bedford & Avioli, 2012), nieces/nephews (Milardo, 2010), as well as stepkin (Ganong & Coleman, 2012; Lin et al., 2018)—any of whom may become their primary caregiver. Knowledge about the experiences of extended family members who are the primary caregiver of a relative living with dementia is needed to help ensure that these families are not underserved or overlooked in health care and social service settings. Given the diversity in family experiences and potential generational differences in response to caregiving, understanding these family dynamics is critical today, and will only become more so as new family structures continue to emerge (Russell, 2020). The purpose of this preliminary research was to highlight structural diversity among dementia family caregivers, and more specifically, explore the experiences of extended family caregivers and how they manage their care responsibilities to meet the needs of their relative living with dementia.
Family Caregiving
For decades, reference to conventional nuclear families permeated the scholarly family gerontology literature (Allen et al., 2000; Brubaker, 1990; Silverstein & Giarrusso, 2010; Streib & Beck, 1980; Troll, 1971), even though such family patterns were statistically rare in the history of U.S. families (Coontz, 1992, 1997). Predicated on the Standard North American Family (Smith, 1993), the core assumptions of this model were based on normative beliefs about family life, that is, older adults reside in a conventional household with a living heterosexual spouse or children nearby to provide care. The model ignored unmarried persons and obscured the involvement of other family and nonfamily members in the care of older adults. It assumed universality in preferences for care given by spouses and adult children and gave peripheral acknowledgment to extended kin and others as members of older adults’ “latent kin networks” of support (Riley & Riley, 1993) who are enacted only in times of crisis. For example, adult grandchildren who typically provided periodic assistance to their grandparents to support their parents as primary caregivers (Hamill, 2012) only assumed the role of full-time caregiver if their parents were not able to maintain their caregiver role (Fruhauf et al., 2006; Piercy & Chapman, 2004). Whether serving in a primary or auxiliary caregiver role, grandchildren caregivers are a heterogeneous group with different priorities, demands, and roles (Venters & Jones, 2021) than family caregivers at other life stages. They experience unique caregiving-related strains, for example, limited career/family aspirations and decreased dating/social life (Dellmann-Jenkins et al., 2000; Fruhauf & Orel, 2008).
In recent years, greater recognition and attention has been given to the existence of multiple family structures that challenge and diverge from the ideal of who constitutes family and typical patterns of care (Brewster et al., 2020; Carr & Utz, 2020; Lin et al., 2018; Roberto & Blieszner, 2015). However, with few exceptions, most dementia family caregiving studies, regardless of sample size or design, include a relatively small number of extended family caregivers which has led investigators to exclusively focus on familial caregiving by either excluding other relatives from primary analyses or combining them into a single group of caregivers. For example, a retrospective study by Nichols and colleagues (2011) compared typical (spouse, children) and atypical (child-in-law, sibling, nephew/niece, grandchild) dementia family caregivers who participated in the Resources for Enhancing Alzheimer’s Caregivers Health (REACH I and II) national, multisite initiative. Among the 1,476 caregivers in their analytic sample, 125 (8.5%) were nonspouse or non-child caregivers. Across caregiver categories, persons living with dementia exhibited similar burdensome dementia-related behaviors and impairments in activities of daily living (ADL). Among African American caregivers there were higher percentages of grandchildren, siblings, and nieces/nephews compared with spouses; the opposite was true for White caregivers. Caregivers other than spouses were more likely to provide care for women and unmarried relatives living with dementia, leading the study authors to speculate that fewer care possibilities were available for them. In addition, atypical caregivers had fewer perceived competing family demands/commitments (i.e., unmarried, childless).
Wolff and colleagues (2016) used the National Health and Aging Trends Study’s (NHATS) National Study of Caregiving (NSOC) to develop a national profile of family and unpaid caregivers providing substantial help with health care activities (e.g., care coordination, medication management). Extended kin comprised 16.7% of the caregiver sample. Extended family and adult child caregivers were just as likely as spouse caregivers to report physical difficulties and reduced participation in valued activities because of caregiving. About 25% of the caregivers used supportive services to assist with the older persons’ care, but type of services used was not reported by caregiver type. More recently, an analysis of NHATS/NSOC data found that 50% of the older adults cared for by “other” caregivers reported having unmet daily care needs (Beach & Schulz, 2017).
As in the national studies, extended family caregivers identified in smaller-scale studies of dementia care are often collectively categorized as “other relatives” and receive little attention within the context of the studies in which they appear (Gerstel, 2011). Among articles published in the past decade, we identified only three that included extended family caregivers in the analysis. A study of 55 U.S. caregivers of persons living with dementia, adult children reported needing more services, and specifically, more social services compared with spouses and other relatives (Ryan et al., 2010). Caregivers came mostly from clinics, so it is uncertain whether similar service needs would be found in community-based samples. A study of informal/formal care use by 560 persons living with dementia in Germany (Laporte Uribe et al., 2017) found spouses and adult children/children in-law provided most types of care, whereas more distant relatives were involved with peripheral tasks such as leisure activities and supervision/assistance with medical care (e.g., doctor’s visits). Other data about the specific caregiver categories were not provided. An analysis of 4,717 dyads of Dutch informal caregivers and their older care receivers (14% with dementia) from 21 research projects (Verbakel et al., 2016) included sibling (2.6%) and other family caregivers (2.2%). Other family caregivers reported spending significantly less time providing care than adult child caregivers. While the care relationship was used in the multilevel analysis and interesting trends reported, discussion of the study findings did not fully address the association between caregiver type and caregiver outcomes. Moreover, the analyses were not specific to dementia care.
The focus of the current research is on the care situations of extended family caregivers and the impact of caregiving on the caregivers’ health and well-being. Specifically, the purpose of this preliminary research was to analyze quantitative and qualitative data to explore the experiences of extended family caregivers and how they manage their care responsibilities to meet the needs of their relative living with dementia.
Method
We conducted independent analyses of two existing data sets to examine extended family members’ experiences as primary caregivers for a relative living with dementia, the type of care they provide, their use of informal support and services to help manage the care needs of their relative, and the ramification of caregiving on their health and well-being. In Study 1, we analyzed data from the NHATS’s NSOC (Spillman et al., 2014) to describe the care experiences of 107 extended family dementia caregivers. In Study 2, we used case study tools (Yin, 2014) to explore in more depth the experiences of and strategies used by 10 extended family dementia caregivers (Savla et al., 2022). Each study contributed unique (as well as similar) data that provided insight into extended family members experiences as caregivers.
Study 1: 2011 NHATS and the NSOC
Sample.
We linked data drawn from the 2011 NHATS and the 2011 NSOC, which constituted a nationally representative sample of Medicare beneficiaries aged 65 and above and their caregivers. Our analysis focused on NHATS participants identified as having dementia (criterion in NHATS technical paper 5, Kasper et al., 2013), needing help with mobility, self-care, or household activities, and who lived in the community (i.e., not in health care facility). For NSOC, telephone interviews were conducted with up to five family and unpaid individuals who were identified as helpers. Approximately 17% of caregivers for persons living with dementia in NSOC were extended family members. We focused our analyses on the subset of persons living with dementia (n = 89) who received care from at least one extended family caregiver (n = 107).
Excluding nuclear family caregivers (i.e., adult children, 59% and spouses, 17%), as well as non-kin caregivers (6%), four subgroups of extended family caregivers were created based on their relationship with sampled NHATS participants: siblings (2%; sister, brother, sister-in-law, brother-in-law), grandchild (10%; grandsons, granddaughters), niece/nephew (4%; nieces, nephews, cousins), and stepkin (1%; stepsons, stepdaughters, stepgrandchildren). Across groups, most caregivers were women (siblings, 68.7%; grandchildren, 71.7%; niece/nephews, 70.7%; stepkin, 77.1%). On average, grandchildren (Mage = 23.46, SE = 2.68) and stepkin (Mage = 49.72, SE = 0.00) were younger compared with nieces/nephews (Mage = 69.16, SE = 5.59) and sibling (Mage = 73.15, SE = 3.15) caregivers (p < .001).
Measures.
Sociodemographic characteristics included weighted sample size, sex, and age. Caregivers reported if they experienced caregiving-related difficulties in helping their relatives in three domains: physical, financial, and emotional. Responses were coded as (1) none or little, and (2) some or substantial difficulties. In addition, caregivers were also asked whether they used three types of supportive services to assist them with the care of their relative: respite care, participation in support group, and received caregiver training. Responses were coded (1) yes or (0) no.
Caregiver subjective well-being was measured using a 2-item depression (Physical Health Questionnaire [PHQ-2]) and 2-item anxiety (accessed by Generalized Anxiety Disorder-2 item [GAD-2] based on caregivers’ last month feeling) screening instrument (Kroenke et al., 2009). The PHQ-2 questions were “Over the last month, how often have you (a) had little interest or pleasure in doing things; (b) felt down, depressed, or hopeless.” The GAD-2 questions were “Over the last month, how often have you (a) felt nervous, anxious, or on edge; (b) been unable to stop or control worrying?” Caregivers rated these items on a 4-point rating scale (0 = not at all; 1 = several days; 2 = more than half the days; 3 = nearly every day). Total score for depression and anxiety was calculated by summing the responses for both items, with total scores ranging from 0 to 6 for each measure. The optimal cutoff for both scales, in terms of its ability to screen for their respective affective disorders, is a score ≥3 (Stahl et al., 2021). Caregivers who reported scores higher than 3 showed symptoms of depression and anxiety, respectively.
Persons living with dementia need for help with self-care (eating, dressing, bathing, toileting), mobility (indoor/outdoor mobility, transferring from bed), and household ADL (laundry, shopping, preparing meals, banking) were calculated using a binary variable (1 = received help from someone; 0 = did not receive help). Total number of unique informal caregivers who provided help with tasks in any of these three domains were summed.
Analysis.
Data subsets were created in R and all the other analyses were conducted in STATA. We first calculated the mean, standard deviation, and percentage under each subgroup of extended caregivers, adjusted for the survey weights. To test the differences of each variable across subgroups of extended family caregivers, chi-square tests were performed for categorical variables and adjusted Wald statistic tested against an F distribution was estimated for continuous variables. Analyses involving persons receiving care used NHATS analytical weights, whereas NSOC analytical weights were used for analysis involving caregivers.
Study 2: Families in Appalachia Caring for Elders With Alzheimer’s Disease (FACES-AD)
Sample.
As part of the FACES-AD multistage, mixed-methods study, we conducted structured telephone interviews and seven daily diaries with 124 primary family caregivers of community-dwelling (i.e., not living in a care facility) persons living with dementia in the rural Appalachia region of Virginia (for study details/approvals, see Savla et al., 2022). The overarching aim of the research was to learn from families in rural Appalachia about approaches to caregiving and influences on formal service use. Ten FACES-AD caregivers were extended family members: four siblings, three grandchildren, and three nieces (Table 1). They ranged in age from 26 to 81 (M = 57.5); nine caregivers identified as female and seven identified as White. Five caregivers (three sisters, the grandson, one niece) co-resided with their relative. Data used in the current analysis are from the initial interviews with these caregivers.
Table 1.
Extended Family Caregivers: Demographic, Care Tasks, Family Support, Service Use, and Well-Being Variables.
| Type of care | ||||||||
|---|---|---|---|---|---|---|---|---|
|
|
||||||||
| Caregiver | Age | Race | Proximity to PLWDa | IADL | ADL | Informal help | Formal services | Caregiver burden (M) |
|
| ||||||||
| Sadie (sister) | 71 | White | Same apt bldg | Chores, shopping, cooking, laundry, driving, money | Dressing | None | None | 2.83 |
| Sara (sister) | 81 | Black | Same household | Chores, shopping, cooking, laundry, driving | None | None | None | — |
| Sophie (sister) | 69 | Black | 5 miles | Shopping, cooking, laundry, driving, money, medications | None | Brother-in-law | Housekeeping, meal delivery, personal care | 0.75 |
| Stella (sister) | 79 | White | Same household | Chores, shopping, cooking, laundry, driving, money, medications | Eating, dressing, grooming, bathing, toileting, getting in/out bed | Sibling, cousin | None | 1 |
| Greg (grandson) | 26 | White | Same household | Chores, shopping, cooking, laundry, medications | Eating, getting in/ out bed | Sibling, spouse | Meal delivery, personal care, respite | 1.08 |
| Georgia (granddaughter) | 30 | Black | 5 miles | Chores, shopping, cooking, laundry, medications | Eating, getting in/ out bed | Adult son, sibling, nephew, PLWD boyfriend | Transportation service | 1.91 |
| Grace (granddaughter-in-law) | 51 | White | 40 miles | Chores, shopping, cooking, laundry, driving, money, medications | Bathing | Grandson, Neighbor | Meal delivery | 0.25 |
| Nancy (niece) | 53 | White | Same household | Chores, shopping, driving, money, medications | Grooming, bathing | Niece’s husband | None | 0.92 |
| Nelda (niece) | 63 | White | Same household | Chores, shopping, driving, money, medications | Grooming, bathing | Niece’s husband | Personal care, respite, transportation | 1.17 |
| Nora (niece) | 52 | White | 5 miles | Shopping, cooking, driving, medications | None | Siblings | None | 0.83 |
Note. IADL = instrumental activities of daily living; ADL = activities of daily living; M = mean.
PLWD = Person living with dementia.
Measures.
Caregivers responded to standard demographic questions about themselves and the person living with dementia. Functional abilities of the person living with dementia were based on the caregivers’ assessment of difficulties their relative had with eight instrumental ADL (IADL) and six personal ADL, respectively (see Savla et al., 2022).
The caregivers were asked a series of structured questions (with the opportunity to elaborate on their responses) about their care situation including personal duty and family expectations for providing care (Response: rarely true, somewhat true, mostly true), how well they got along with the person living with dementia (Response: very well, somewhat, fairly well, not very well), and feelings (i.e., guilty, angry, bad) about their interactions with their relative (Response: never, rarely, sometimes, often). Questions about assistance with managing the care needs of the person living with dementia focused on help from family members (i.e., who helped) and the use of five formal services (e.g., meal delivery, homemaker, transportation, personal care, respite; Responses: yes/no).
Caregivers were also asked several questions about their perceptions of caregiving in relationship to their personal health and well-being. Specifically, they were asked whether their health problems made caregiving difficult (Responses: yes/no) if their health was worse because of caregiving, and whether they felt exhausted at the end of the day (Responses: never, rarely, sometimes, often). Well-being measures included their assessment of time for themselves (Responses: never, rarely, sometimes, often) and their summed response to a 12-item caregiver burden scale (Bédard et al., 2001; Responses: 0 = never, 1 = rarely, 2 = sometimes, 4 = often).
Analysis.
Based on the responses to the structured interview and daily diary questions and measures, as well as the interviewers’ reflective memoing about the caregivers’ explanation of their responses, members of the authors’ research team prepared a brief written synopses for each of the FACES-AD caregivers that were subsequently discussed at weekly team meetings. The synopses, which were developed using a standardized one-page template that focused on care needs, relationship dynamics, informal help, and service use, provided integrated summaries about the care situation and the caregivers’ experiences. After the research team discussions, any needed revisions were made and final versions of the synopses were stored for future use.
Relying on descriptive statistics and qualitative techniques, we began the current analysis by first re-reading the synopses of the 10 extended family caregivers and creating bar graphs to explore patterns within and across caregivers (Schulz et al., 2021). We aggregated quantitative findings for each area of interest (e.g., caregiver perceptions, care needs, informal and formal assistance, caregiver health and well-being) and displayed each caregiver’s scores in a bar graph. This graphic representation of the data helped us to distill individual findings and identify similarities and differences across caregivers. We combined the visual data with the individual synopses to illustrate key findings.
Results
Study 1: 2011 NHATS and the NSOC
Compared with other extended caregivers, a large majority of grandchildren (68%) and sibling (59%) caregivers cared for a relative who had one or more self-care needs (p < .05; Table 2). The need to assist their relative living with dementia with household activities was common across all caregiver groups. Relatives of approximately one half of the grandchildren (53%), siblings (48%), and nieces/nephews (50%) also had mobility needs. In contrast, relatively fewer stepkin had a relative who needed help with self-care tasks (33%) or mobility needs (20%).
Table 2.
NHATS/NSOC 2011 Extended Family Caregivers: Response by Relationship Type.
| Variable | Sibling | Grandchild | Niece/nephew | Stepkin | p |
|---|---|---|---|---|---|
|
| |||||
| Weighted estimates, na | 104,697 | 492,243 | 194,973 | 50,055 | |
| Relationship to PLWD, % | 2.15 | 10.09 | 4.00 | 1.03 | |
| PLWD needs help, % | |||||
| W/self-care | 59.57 | 68.17 | 39.78 | 33.22 | .02 |
| W/mobility | 48.19 | 53.16 | 50.17 | 20.30 | .12 |
| W/household activities | 91.57 | 91.39 | 88.39 | 82.56 | .80 |
| Informal CG, M (SE) | 1.71 (0.08) | 3.15 (0.04) | 2.20 (0.28) | 2.26 (0.28) | .21 |
| CG difficulties w/care, % | |||||
| Emotional | |||||
| None/a little | 97.66 | 64.32 | 85.48 | 93.33 | .07 |
| Some/substantial | 2.34 | 35.68 | 14.52 | 6.67 | |
| Physical | |||||
| None/a little | 89.96 | 82.02 | 75.31 | 93.33 | .68 |
| Some/substantial | 10.04 | 17.98 | 24.69 | 6.67 | |
| Financial | |||||
| None/a little | 100.0 | 78.83 | 89.57 | 93.33 | .20 |
| Some/substantial | 0.0 | 21.17 | 10.43 | 6.67 | |
| Services used, % | |||||
| Respite care | 34.01 | 3.89 | 2.78 | 45.10 | .06 |
| Caregiver training | _b | 3.35 | 3.29 | 26.46 | .08 |
| Support group | 12.94 | 7.13 | _b | _b | .08 |
| CG well-being, % | |||||
| Depressive symptoms | 8.89 | 18.12 | 8.52 | 5.61 | .93 |
| Anxiety symptoms | _b | 11.79 | 15.25 | _b | .16 |
Note. NHATS/NSOC = National Health and Aging Trends Study/National Study of Caregiving; PLWD = person living with dementia; CG = caregiver.
All analysis used sampling weights.
Data not reportable because unweighted cell sizes were too small to obtain valid estimates.
Although no significant differences were found among the different types of extended family caregivers and caregiving difficulties, a greater percentage of grandchildren reported substantial emotional (36%) and financial difficulties (21%) related to caregiving than the other caregivers. In addition, almost 18% of grandchildren and 25% of nieces/nephews reported physical difficulties related to providing care compared with just 10% of siblings and 7% of stepkin.
A small percentage of extended family members used supportive services; however, some marginal differences were found among the relationship groups. Stepkin were more likely to utilize respite care (p = .06) and receive caregivers training (p = .08) than the other extended family caregivers. Use of support groups was limited among extended caregivers (siblings, 13%; grandchildren, 7%).
No significant group differences were found among the extended family caregivers with respect to symptoms of depression and anxiety. A higher percentage of grandchildren (18%) reported depressive symptoms than other extended family caregivers. In addition, grandchildren (12%) and nieces/nephews (15%) reported symptoms of anxiety.
Study 2: FACES-AD
Care situation.
The caregivers helped their relative with four or more IADLs (M = 5.5; SD = 0.97; range = 4–7), with three sisters (Sadie, Sophie, and Stella) and the granddaughter-in-law (Grace) providing help in more areas than the other extended family caregivers (Table 1). Seven of the caregivers helped their relative with at least one ADL (M = 1.6; SD = 1.78; range = 0–6); Stella provided help to her sibling in all six areas assessed. Eight of the caregivers received help managing their care responsibilities from other family members. Five caregivers also relied on assistance from one or more formal services. Sadie and Sara (sister caregivers) did not receive assistance from either informal helpers or formal services. Both caregivers provided similar assistance with IADLs to their relatives as did the other extended family caregivers.
Care experiences.
Of the nine caregivers responding to the care expectations items, eight responded that it was somewhat or mostly true that it was an unspoken expectation within their family that they would care for their relative (see Figure 1). In addition, seven caregivers agreed that it was somewhat or mostly true that it was their duty to care for their family member.
Figure 1.
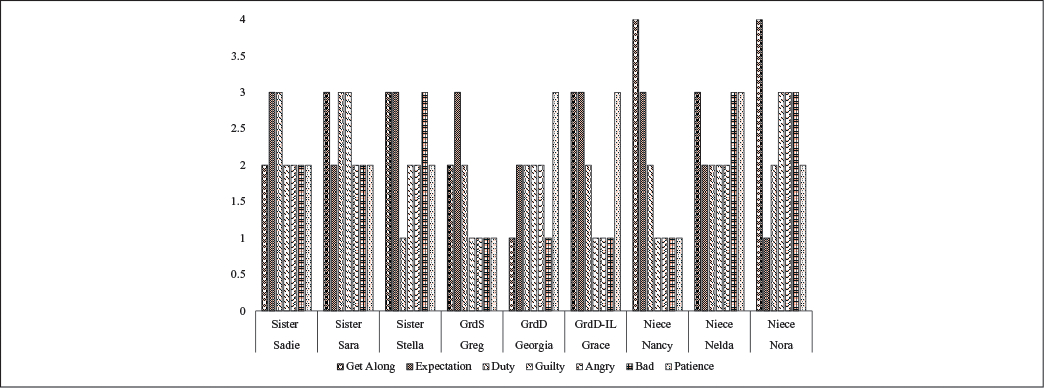
Caregiving experiences by relationship.
Seven of the caregivers indicated that they got along very well or fairly well with the person living with dementia (Figure 1). Only the granddaughter caregiver, Georgia, said she did not get along well with her grandmother. Regardless of how they got along, caregivers did not report consistent ill feelings about their interactions with their relative. The one exception was Nora, who reported that although she got along very well with her aunt, she sometimes felt guilty about the way she treated her aunt, felt bad about getting angry with her, and felt bad about not having more patience with her aunt.
Caregiver health and well-being.
Three caregivers, all sisters (Sadie, Sophie, Stella), reported having health problems that made it difficult to care for their sibling. Of these sisters, Sadie also reported that her health is often worse since she became a caregiver. Four caregivers (Sophie, Stella, Greg, Georgia) reported that because of their caregiving responsibilities, they were often exhausted at the end of the day. Five caregivers reported that they often (Sadie, Georgia) or sometimes (Stella, Greg, Nancy) did not have time for themselves. Caregivers reported an average burden score of 1.19 (SD = 0.75; range = 0.25–2.83), with Sadie and Georgia reporting higher than average burden scores (Table 1). These two caregivers also perceived their relationship with their relative more negatively than the other caregivers.
Common Themes Across Studies
Considering the findings across the two studies, we observed three themes common among the extended family caregivers that are also found among nuclear family dementia caregivers. First, many caregivers did not utilize formal assistance to help them manage their care responsibilities. Second, in some situations, caregiving was a family affair. And third, providing care took a toll on caregivers’ well-being.
Caregiving without services.
Reliance on formal services was rare among the extended family caregivers. Respite services, which provides caregivers some short-term relief from their care responsibilities, were used by less than 10% of the extended family caregivers in Study 1 and only two of the 10 caregivers (Greg, grandson; Nelda, niece) in Study 2. Three of the four sibling caregivers and two of the three niece caregivers in Study 2 (see Table 1) did not utilize any paid services and two of the grandchildren caregivers only used one service to supplement their care. For example, Grace (granddaughter-in-law) put in place Meals-on-Wheels for her grandfather who lived alone. She visited him daily unless there was some unforeseen circumstance, in which case she relied primarily on his neighbor to check in on him and provide any assistance needed.
Caregiving is a family affair.
On average, persons living with dementia in Study 1 relied on two to three family members for help with daily activities of living. In Study 2, at least one additional family member assisted 8 of the 10 caregivers (see Table 1). For example, Stella lived with a second sister and her sibling with dementia. Stella’s sister provided transportation and did mostly administrative tasks whereas she handled the practical, day-to-day care tasks. A cousin also provided care-related advice and emotional support to Stella. She did not use formal services. Although Stella felt that she generally had enough help, she wished she had a little respite care. Conversely, Georgia did not live with her grandmother and had multiple informal helpers, including her grandmother’s son, sister, nephew, and boyfriend. Although her grandmother used a transportation service, Georgia said she did not know where to go to find other types of services and was not sure what was available to her.
Caregiving takes its toll.
Across the two studies, caregivers who experienced a strained relationship with their relative with dementia and received little support from informal or formal sources found the role of caregiving emotionally and physically draining. In Study 1, more than half of the grandchildren’s grandparents needed assistance with self-care and mobility activities, and half of the niece/nephew’s relative required help with mobility. One third of the grandchildren (36%) reported some or substantial emotional issues because of caring for their relative and one fourth of the nieces/nephew caregivers (26%) reported substantial physical difficulties. In Study 2, Georgia (granddaughter) and Sadie (sister) provided help with self-care and household tasks and reported higher than average caregiver burden. They also reported feeling less close to their relative than most of the other caregivers.
Discussion
Changes in family structures present both opportunities and challenges for extended family caregivers who are responsible for the care of a relative living with dementia as well as for care professionals who attend to their health and service needs. Collectively, our findings suggest that like nuclear family caregivers, extended family caregivers provide care in multiple areas, with little or no assistance from formal services (Bieber et al., 2019; Potter, 2018). However, they periodically rely on a small informal network for emotional support and to assist with the care of the person living with dementia (Marcum et al., 2020; McCabe et al., 2016). The extended family caregivers in our studies also reported that caregiving impacted their physical and emotional well-being (Chiao et al., 2015). Recent research suggests that while care demands and not asking for help were associated with poor well-being for nuclear (i.e., spouse and adult children) and extended family caregivers, well-being differed between nuclear and extended family caregivers depending on the strength of relationship between the caregiver and the person living with dementia, the intensity of care provided, and whether they were part of a larger convoy of caregivers (Broese van Groenou et al., 2013). Variability in caregivers’ experiences and well-being also are driven by their social location and their life course trajectory (Eifert et al., 2016). For example, simultaneously raising their own family, working outside the home, coping with chronic illnesses and other health issues (i.e., their own or the person living with dementia), or caring for multiple family members influences the daily lives of family caregivers and how they manage their caregiving responsibilities. Our findings, particularly from Study 2, illuminate the mixed experiences of extended family caregivers and underscore the need for further understanding of within and across caregiver group situations and challenges.
Many siblings reciprocate practical and emotional support in early and mid-life, but changes in needs triggered by physical or mental illness and the absence of a spouse or adult child mobilize siblings to provide care in later life (Barnes, 2012). Studies comparing sibling caregivers with other family caregivers suggest that sibling caregivers fare better (Penning & Wu, 2015), which seemed to be the case for the siblings in our study. A lower percentage of sibling caregivers in our study reported emotional, financial, and physical difficulties than grandchildren or niece/nephew caregivers. Perhaps because of their life stage and own health challenges, sibling caregivers used paid services to help with ADL care tasks while they provided hands-on assistance with IADL-related duties. The less demanding nature of these latter care tasks may have contributed to lower feelings of caregiver strain and burden.
Caregiving roles among grandchildren evolve from the dynamics of intergenerational family relationships. Grandchildren in Study 2 assumed the caregiver role because of family expectations and physical proximity to their grandparents. They experienced stress as they managed their caregiving responsibilities while fulfilling career aspirations and addressing their personal needs (Dellmann-Jenkins et al., 2000; Fruhauf & Orel, 2008). However, unlike other studies (Celdrán et al., 2011), the grandchildren in Study 2 did not report strong emotional closeness to their grandparents. The age of the grandchild providing care may influence their relationship with their grandparent living with dementia. Our analyses included grandchildren who were 18 years and older, whereas Celdrán and colleagues included younger (14–18 years) and older (19–21 years) grandchildren. Grandchildren’s life stage and the care roles they are expected to play may have contributed to the differences in their appraisal of the caregiving experiences. In addition, grandchild caregivers in our study were often a member of a larger care network of other family members and paid workers who were also providing care to the person living with dementia. This denser “generalist” caregiving network of informal and formal care providers assisted with a variety of care needs, which may be protective for grandchildren caregivers (Perion et al., 2021; Spillman et al., 2020).
Our data on niece/nephew caregivers, albeit limited, provide some initial insights about the experiences of these caregivers. These middle-aged caregivers were involved in providing care with various ADL and IADL tasks, and relying on close family members (e.g., spouse, sibling) for assistance. Many of them also reported greater physical strain and higher anxiety symptoms, further paralleling the experiences of adult child caregivers. We speculate that life course influences on aunt/uncle–niece/nephew relationships, including emotional closeness, proximity, and frequency of contact (Milardo, 2010), may come into play when the need for dementia care arises.
Baby boomer divorce and remarriage rates (Raley & Sweeney, 2020) have resulted in the centrality of stepkin in family networks. Qualitative research suggests that roles in stepfamilies are idiosyncratic, which creates strain/conflict and increases social distance when support expectations are not in agreement (Chapman et al., 2016). Our analysis showed that a lesser percent of stepkin, compared with other extended family caregivers, expressed distress that is often associated with dementia caregiving. While our study data do not provide insight as to why this may be, national data showed that in late life, stepchildren/stepmothers were less likely to live together, to live nearby, or to move closer together than biological children/mothers (Seltzer et al., 2013). Older step-grandparents felt less emotionally close to their stepgrandchildren than older biological grandparents felt toward their biological grandchildren (Steinbach & Silverstein, 2019). Thus, when stepkin engage in dementia caregiving, demographic and relational variables may influence both their care practices and outcomes.
Future Research
Our findings shed light on the experiences of extended family caregivers, but they are limited by the available data. First, while the two data sets analyzed shared common elements conceptually, their sample and measures differed. The NSOC caregivers were not necessarily the primary caregivers, as data were collected on up to five caregivers who were willing to participate in the survey interview. Conversely, FACES-AD was limited to primary caregivers. Thus, disparities in the findings between these two studies can be related to these inclusion criteria. Second, NHATS/NSOC data do not provide in-depth information about the extent and circumstances of extended family care for persons living with dementia and nuances of service use, thereby limiting the ability to use these data to inform practice and policy. FACES-AD provided a more microlevel understanding of the caregivers’ experiences but did not gather information about why or how the family member assumed the caregiver role. It also was not focused specifically on extended family caregivers resulting in a small, nonrepresentative sample.
Future research is needed to systematically examine and more deeply assess the experiences of extended family caregivers and heterogeneity across relationship groups than what can be ascertained from archived databases. The use of rigorous mixed-methods and qualitative investigations that go beyond descriptive presentations of extended family caregivers’ experiences will provide researchers and practitioners a better understanding of the dynamics of family caregiving in the context of the structural diversity of contemporary families. This knowledge is essential for family nurses and other practitioners for enhancing the coordination of care for persons living with dementia as well as developing tailored education and intervention programs to address the needs of extended family caregivers and promote caregiver health and well-being.
Implications for Family Nursing Practice
Much of the literature on caregiving has concentrated on spouses and adult child caregivers, frequently disregarding the true complexity of caregiving in contemporary families where norms of selected kin and complex and changing care networks are more common (Brewster et al., 2020; Russell, 2020). Acquiring a deeper and more nuanced understanding of the characteristics that distinguish extended carers from nuclear caregivers can provide crucial information for program development and implementation. Because extended family caregivers are so diverse, regular needs assessment by nurses and other health professionals will be a critical component of supportive care programming for these families. For instance, younger caregivers may be more comfortable with digital technologies and may seek support through social media platforms, whereas these domains may be seen as unacceptable to older caregivers who may be less technologically savvy. However, with some coaching and practice, older caregivers may become more skilled and open to using digital technologies (Mitzner et al., 2019).
Because persons living with dementia often have other chronic conditions, family caregivers are increasingly assisting in the management of complex medical and nursing tasks (Ploeg et al., 2020) as well as their own health concerns. Health care providers need to consider both the person living with dementia and their extended family caregivers when developing, implementing, and assessing plans for care. In addition, younger extended family caregivers may require additional assistance balancing work and family obligations, whereas older caregivers may benefit from advice on maintaining their own and their relative’s physical and mental health.
Finally, extended family caregivers may be part of a wider care network and may require assistance and support in negotiating and navigating care obligations with other members of the care network. It is critical for nurses and other professionals to take cultural norms and values into account (Brewster et al., 2020) while offering such coaching to extended family caregivers. Thus, contemporary caregivers will benefit from health professionals and program developers who recognize their individual needs and prioritize the adaptability, appropriateness, accessibility, and acceptability of programs and policies to their unique care setting, as one size does not fit all.
Conclusion
The dementia caregiving literature has largely ignored extended family caregivers who play a vital role in sustaining community living for older adults living with dementia. In light of changing family structures, more now than ever before, a greater understanding is needed about how extended family caregiving relationships work, the strengths and weaknesses of these care conventions, and the needs of and barriers faced by these frequently invisible caregivers. Because most health and community services are predicated upon the availability and willingness of families to care for their older members living with dementia, it is important that health care and service providers as well as policymakers recognize the multiple configurations of families and support distal kin who assume the role of primary caregiver and provide important sources of daily care for their relative living with dementia.
Funding
The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This work was supported by the National Institute on Aging at the National Institutes of Health (R21AG054682, R01AG069818).
Biographies
Karen A. Roberto, PhD, is a university distinguished professor, executive director of the Institute for Society, Culture and Environment, and senior fellow at the Center for Gerontology, Virginia Tech, USA. She holds secondary appointments in the Departments of Internal Medicine and Psychiatry and Behavioral Medicine at the Virginia Tech Carilion School of Medicine. Her research focuses on health and social support in late life and includes studies of the health of rural older women, dementia family caregiving, and elder abuse. Recent publications include “Dementia Family Caregiving in Rural Appalachia: A Sociocultural Model of Care Decisions and Service Use” in The Journals of Gerontology, Series B (2022, with J. Savla, B. R. McCann, R. Blieszner, & A. L. Knight), “Elder Abuse and the Opioid Epidemic. Evidence From APS Cases in Central Appalachia” in Journal of Rural Mental Health (2022, with B. R. McCann, P. B. Teaster, & E. Hoyt), and “A Long and Winding Road: Dementia Caregiving With Grit and Grace” in Innovation in Aging (2019, with B. R. Mccann, R. Blieszner, & J. Savla).
Jyoti Savla, PhD, is professor of human development and family science and research methodologist at the Center for Gerontology at Virginia Tech. She holds a secondary appointment in the Department of Psychiatry and Behavioral Medicine at the Virginia Tech Carilion School of Medicine. Her research is positioned at the nexus of gerontology, daily stress and coping, and health psychology. A primary focus of her research is identifying and enhancing support structures for caregivers and their relative living with dementia as they cope with the daily challenges of chronic illness. Recent publications include “Family Caregivers in Rural Appalachia Caring for Older Relatives With Dementia: Predictors of Service Use” in Innovations in Aging (2022, with K. A. Roberto, R. Blieszner, & A. L. Knight), “Dementia Caregiving During the “Stay-at-Home” Phase of COVID-19 Pandemic” in The Journals of Gerontology, Series B (2021, with K. A. Roberto et al.), and “Where You Age Matters: Individual- and County-Level Predictors of Formal and Informal Care in Rural Appalachia” in Journal of Aging and Health (2019, with L. R. Bivens, K. A. Roberto, & R. Blieszner).
Footnotes
Declaration of Conflicting Interests
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
References
- Allen K, Blieszner R, & Roberto KA (2000). Families in the middle and later years: A review and critique of research in the 1990s. Journal of Marriage and Family, 62(4), 911–926. 10.1111/j.1741-3737.2000.00911.x [DOI] [Google Scholar]
- Barnes M (2012). An ethic of care and sibling care in older age. Families, Relationships and Societies, 1(1), 7–23. 10.1332/204674312X633135 [DOI] [Google Scholar]
- Beach SR, & Schulz R (2017). Family caregiver factors associated with unmet needs for care of older adults. Journal of the American Geriatrics Society, 65(3), 560–566. 10.1111/jgs.14547 [DOI] [PubMed] [Google Scholar]
- Bédard M, Molloy DW, Squire L, Dubois S, Lever JA, & O’Donnell M (2001). The Zarit Burden Interview: A new short version and screening version. The Gerontologist, 41(5), 652–657. 10.1093/geront/41.5.652 [DOI] [PubMed] [Google Scholar]
- Bedford VH, & Avioli PS (2012). Sibling relationships from midlife to old age. In Blieszner R & Bedford VH (Eds.), Handbook of families and aging (2nd ed., pp. 125–152). Praeger/ABC-CLIO. [Google Scholar]
- Bieber A, Nguyen N, Meyer G, & Stephan A (2019). Influences on the access to and use of formal community care by people with dementia and their informal caregivers: A scoping review. BMC Health Services Research, 19(1), 1–21. 10.1186/s12913-018-3825-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brewster GS, Bonds K, McLennon S, Moss KO, Epps F, & Lopez RP (2020). Missing the mark: The complexity of African American dementia family caregiving. Journal of Family Nursing, 26(4), 294–301. 10.1177/1074840720945329 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Broese van Groenou MI, de Boer A, & Iedema J (2013). Positive and negative evaluation of caregiving among three different types of informal care relationships. European Journal of Ageing, 10(4), 301–311. 10.1007/s10433-013-0276-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brubaker TH (1990). Families in later life: A burgeoning research area. Journal of Marriage and Family, 52(4), 959–981. 10.2307/353313 [DOI] [Google Scholar]
- Carr D, & Utz RL (2020). Families in later life: A decade in review. Journal of Marriage and Family, 82(1), 346–363. 10.1111/jomf.12609 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Celdrán M, Triadó C, & Villar F (2011). My grandparent has dementia: How adolescents perceive their relationship with grandparents with a cognitive impairment. Journal of Applied Gerontology, 30(3), 332–352. 10.1177/0733464810368402 [DOI] [Google Scholar]
- Chapman A, Sanner C, Ganong LH, Coleman M, Russell L, Kang Y, & Mitchell S (2016). Exploring the complexity of stepgrandparent-stepgrandchild relationships. In Gianesini G & Blair SL (Eds.), Divorce, separation, and remarriage: The transformation of family (pp. 101–130). Emerald Group. [Google Scholar]
- Chiao CY, Wu HS, & Hsiao CY (2015). Caregiver burden for informal caregivers of patients with dementia: A systematic review. International Nursing Review, 62(3), 340–350. 10.1111/inr.12194 [DOI] [PubMed] [Google Scholar]
- Cohen PN (2014). The family: Diversity, inequality, and social change. W.W. Norton. [Google Scholar]
- Coontz S (1992). The way we never were. Basic Books. [Google Scholar]
- Coontz S (1997). The way we really are. Basic Books. [Google Scholar]
- Dellmann-Jenkins M, Blankemeyer M, & Pinkard O (2000). Young adult children and grandchildren in primary caregiver roles to older relatives and their service needs. Family Relations, 49(2), 177–186. 10.1111/j.1741-3729.2000.00177.x [DOI] [Google Scholar]
- Eifert EK, Adams R, Morrison S, & Strack R (2016). Emerging trends in family caregiving using the life course perspective: Preparing health educators for an aging society. American Journal of Health Education, 47(3), 176–197. 10.1080/19325037.2016.1158674 [DOI] [Google Scholar]
- Fruhauf CA, Jarrott SE, & Allen KR (2006). Grandchildren’s perceptions of caring for grandparents. Journal of Family Issues, 27(7), 887–911. 10.1177/0192513X05286019 [DOI] [Google Scholar]
- Fruhauf CA, & Orel NA (2008). Developmental issues of grandchildren who provide care to grandparents. The International Journal of Aging and Human Development, 67(3), 209–230. 10.2190/AG.67.3.b [DOI] [PubMed] [Google Scholar]
- Ganong L, & Coleman M (2012). Relationships with older stepfamilies. In Blieszner R & Bedford VH (Eds.), Handbook of families and aging (2nd ed., pp. 213–242). Praeger/ABC-CLIO. [Google Scholar]
- Gerstel N (2011). Rethinking families and community: The color, class, and centrality of extended kin ties. Sociological Forum, 26(1), 1–20. 10.1111/j.1573-7861.2010.01222.x [DOI] [Google Scholar]
- Geurts T, Van Tilburg TG, & Poortman AR (2012). The grandparent–grandchild relationship in childhood and adulthood: A matter of continuation? Personal Relationships, 19(2), 267–278. 10.1111/j.1475-6811.2011.01354.x [DOI] [Google Scholar]
- Hamill SB (2012). Caring for grandparents with Alzheimer’s disease: Help from the “forgotten” generation. Journal of Family Issues, 33(9), 1195–1217. 10.1177/0192513X12444858 [DOI] [Google Scholar]
- Kasper JD, Freedman VA, & Spillman B (2013). Classification of persons by dementia status in the National Health and Aging Trends Study (Technical Paper #5). Johns Hopkins University School of Public Health. https://nhats.org/sites/default/files/2021-12/Dementia_Classification_with_Programming_Statements.zip [Google Scholar]
- Kroenke K, Spitzer RL, Williams JBW, & Lowe B (2009). An ultra-brief screening scale for anxiety and depression: The PHQ-4. Psychosomatics, 50(6), 613–621. 10.1176/appi.psy.50.6.613 [DOI] [PubMed] [Google Scholar]
- Laporte Uribe F, Heinrich S, Wolf-Ostermann K, Schmidt S, Thyrian JR, Schäfer-Walkmann S, & Holle B (2017). Caregiver burden assessed in dementia care networks in Germany: Findings from the DemNet-D study baseline. Aging and Mental Health, 21(9), 926–937. 10.1080/13607863.2016.1181713 [DOI] [PubMed] [Google Scholar]
- Lin I-F, Brown SL, & Cupka CJ (2018). A national portrait of stepfamilies in later life. The Journals of Gerontology: Series B, 73(6), 1043–1054. 10.1093/geronb/gbx150 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marcum CS, Ashida S, & Koehly LM (2020). Primary caregivers in a network context. The Journals of Gerontology: Series B, 75(1), 125–136. 10.1093/geronb/gbx165 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martin JA, Hamilton BE, Osterman MJK, & Driscoll AK (2021). Births: Final data for 2019. National Vital Statistics Reports, 70(2), 1–50. 10.15620/cdc:100472 [DOI] [PubMed] [Google Scholar]
- Mayol-García Y, Gurrentz B, & Kreider RM (2021). Number, timing, and duration of marriages and divorces: 2016 [Current population reports]. https://www.census.gov/content/dam/Census/library/publications/2021/demo/p70-167.pdf
- McCabe M, You E, & Tatangelo G (2016). Hearing their voice: A systematic review of dementia family caregivers’ needs. The Gerontologist, 56(5), e70–e88. 10.1093/geront/gnw078 [DOI] [PubMed] [Google Scholar]
- Milardo RM (2010). The forgotten kin: Aunts and uncles. Cambridge University Press. [Google Scholar]
- Mitzner TL, Savla J, Boot WR, Sharit J, Charness N, Czaja SJ, & Rogers WA (2019). Technology adoption by older adults: Findings from the PRISM trial. The Gerontologist, 59(1), 34–44. 10.1093/geront/gny113 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Monserud MA (2011). Changes in grandchildren’s adult role statuses and their relationships with grandparents. Journal of Family Issues, 32(4), 425–451. 10.1177/0192513X10384466 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nichols LO, Martindale-Adams J, Burns R, Graney MJ, & Zuber J (2011). Typical and atypical dementia family caregivers: Systematic and objective comparisons. The International Journal of Aging and Human Development, 72(1), 27–43. 10.2190/AG.72.1.b [DOI] [PubMed] [Google Scholar]
- Penning MJ, & Wu Z (2015). Caregiver stress and mental health: Impact of caregiving relationship and gender. The Gerontologist, 56, 1102–1113. 10.1093/geront/gnv03 [DOI] [PubMed] [Google Scholar]
- Perion J, Steiner V, & Ames A (2021). “It makes me feel like good inside because I helped him do stuff”–Perceptions of psychological well-being in adolescents providing dementia care. Journal of Aging Studies, 56, Article 100908. 10.1016/j.jaging.2020.100908 [DOI] [PubMed] [Google Scholar]
- Piercy KW, & Chapman JG (2004). Adopting the caregiver role: A family legacy. Family Relations, 50(4), 386–393. 10.1111/j.1741-3729.2001.00386.x [DOI] [Google Scholar]
- Ploeg J, Northwood M, Duggleby W, McAiney CA, Chambers T, Peacock S, Fisher K, Ghosh S, Markle-Reid M, Swindle J, Williams A, & Triscott JAC (2020). Caregivers of older adults with dementia and multiple chronic conditions: Exploring their experiences with significant changes. Dementia, 19(8), 2601–2620. 10.1177/1471301219834423 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Potter AJ (2018). Factors associated with caregivers’ use of support services and caregivers’ nonuse of services sought. Journal of Aging & Social Policy, 30(2), 155–172. 10.1080/08959420.2017.1414539 [DOI] [PubMed] [Google Scholar]
- Raley RK, & Sweeney MM (2020). Divorce, repartnering, and stepfamilies: A decade in review. Journal of Marriage and Family, 82(1), 81–99. 10.1111/jomf.12651 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Riley MW, & Riley JW (1993). Connections: Kin and cohort. In Bengtson VL & Achenbaum WA (Eds.), The changing contract across generations (pp. 169–190). Aldine de Gruyter. [Google Scholar]
- Roberto KA, & Blieszner R (2015). Diverse family structures and the care of older persons. Canadian Journal on Aging, 34(3), 305–320. 10.1017/S0714980815000288 [DOI] [PubMed] [Google Scholar]
- Russell LT (2020). Capturing family complexity in family nursing research and practice. Journal of Family Nursing, 26(4), 287–293. 10.1177/1074840720965396 [DOI] [PubMed] [Google Scholar]
- Ryan KA, Weldon A, Huby NM, Persad C, Bhaumik AK, Heidebrink JL, & Giordani B (2010). Caregiver support service needs for patients with mild cognitive impairment and Alzheimer’s disease. Alzheimer Disease and Associated Disorders, 24(2), 171–176. 10.1097/WAD.0b013e3181aba90d [DOI] [PMC free article] [PubMed] [Google Scholar]
- Savla J, Roberto KA, Blieszner R, & Knight A (2022). Family caregivers in rural Appalachia caring for older relatives with dementia: Predictors of service use. Innovations in Aging, 6(1), 1–12. 10.1093/geroni/igab055 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schulz GL, Patterson Kelly K, Armer J, & Ganong L (2021). Uncovering family treatment decision-making processes: The value and application of case study methods to family research. Journal of Family Nursing, 27(3), 191–198. 10.1177/1074840720987223 [DOI] [PubMed] [Google Scholar]
- Seltzer JA, Yahirun JJ, & Bianchi SM (2013). Coresidence and geographic proximity of mothers and adult children in stepfamilies. Journal of Marriage and Family, 75(5), 1164–1180. 10.1111/jomf.12058 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Silverstein M, & Giarrusso R (2010). Aging and family life: A decade review. Journal of Marriage and Family, 72(5), 1039–1058. 10.1111/j.1741-3737.2010.00749.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith DE (1993). The Standard North American Family: SNAF as an ideological code. Journal of Family Issues, 14(1), 50–65. 10.1177/0192513X93014001005 [DOI] [Google Scholar]
- Spillman BC, Freedman VA, Kasper JD, & Wolff JL (2020). Change over time in caregiving networks for older adults with and without dementia. The Journals of Gerontology: Series B, 75(7), 1563–1572. 10.1093/geronb/gbz105 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spillman BC, Wolff J, Freedman VA, & Kasper JD (2014). Informal caregiving for older Americans: An analysis of the 2011 National Study of Caregiving. U.S. Department of Health and Human Services. https://aspe.hhs.gov/reports/informal-caregiving-older-americans-analysis-2011-national-study-caregiving [Google Scholar]
- Stahl ST, Rodakowski J, & Smagula SF (2021). Timing of daily activities over a 24-hour period and affective status among a national cohort of older dementia caregivers. Journal of Aging and Health, 33(1–2), 125–132. 10.1177/0898264320962363 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Steinbach A, & Silverstein M (2019). Step-grandparent–step-grandchild relationships: Is there a “Grand Step-Gap” in emotional closeness and contact? Journal of Family Issues, 41(8), 1137–1160. 10.1177/0192513X19886638 [DOI] [Google Scholar]
- Streib GF, & Beck RW (1980). Older families: A decade review. Journal of Marriage and Family, 42(4), 937–956. 10.2307/351834 [DOI] [Google Scholar]
- Troll LE (1971). The family of later life: A decade review. Journal of Marriage and Family, 33(2), 263–290. 10.2307/349414 [DOI] [Google Scholar]
- Venters S, & Jones CJ (2021). The experiences of grandchildren who provide care for a grandparent with dementia: A systematic review. Dementia, 20(6), 2205–2230. 10.1177/1471301220980243 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Verbakel E, Metzelthin SF, & Kempen GI (2016). Caregiving to older adults: Determinants of informal caregivers’ subjective well-being and formal and informal support as alleviating conditions. The Journals of Gerontology, Series B, 73(6), 1099–1111. 10.1093/geronb/gbw047 [DOI] [PubMed] [Google Scholar]
- Wolff JL, Spillman BC, Freedman VA, & Kasper JD (2016). A national profile of family and unpaid caregivers who assist older adults with health care activities. JAMA Internal Medicine, 176(3), 372–379. 10.1001/jamainternmed.2015.7664 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yin RK (2014). Case study research: Design and methods (5th ed.). SAGE. [Google Scholar]


