Abstract
Background
To identify important barriers to COVID-19 vaccination among African Americans living in the Black Belt region.
Methods
A cross-sectional, web-based questionnaire survey was conducted using best–worst scaling case 1 (the object case). Thirty-two potential barriers to COVID-19 vaccination were identified from the literature and confirmed by an expert. A nested balanced incomplete block design was used to generate 62 sets of 16 choice tasks. Each choice task included six barriers. Participants were asked to choose the most and least important barriers to their COVID-19 vaccination in each choice task of one set. The natural logarithm of the square root of best counts divided by the worst counts of each barrier was calculated to rank the importance of barriers.
Results
Responses from a total of 808 participants were included. Among 32 barriers to COVID-19 vaccination, the five most important barriers were “safety concern of COVID-19 vaccines,” “rapid mutation of COVID-19,” “ingredients of COVID-19 vaccines,” “Emergency Use Authorization (Fast-track approval) of COVID-19 vaccines,” and “inconsistent information of COVID-19 vaccines.” On the other hand, the five least important barriers were “religious reasons,” “lack of time to get COVID-19 vaccine,” “no support from my family and friends,” “political reasons,” and “fear of the needle.”
Conclusions
Important barriers to the COVID-19 vaccination for African Americans living in the Black Belt region centered around the issues that could be resolved by communication strategies.
Supplementary Information
The online version contains supplementary material available at 10.1007/s40615-023-01583-9.
Background
Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2 or COVID-19) has a tremendous ongoing impact on global health, economics, and human life [1, 2]. As of April 20, 2022, the death toll from COVID-19 passed six million globally [3] and was approximately one million in the United States (U.S.) [4]. However, COVID-19 hit the Black Belt Region (BBR), which is a string of counties in 11 states (i.e., Alabama, Arkansas, Florida, Georgia, Louisiana, Mississippi, North Carolina, South Carolina, Tennessee, Texas, and Virginia) harder than other regions of the country [5, 6]. While, historically, the BBR referred to the black soil of the cotton-producing areas in Alabama and Georgia [5], the region in this study includes counties characterized by the higher-than-average percentage of African Americans in the U.S. Most states (except North Carolina and Virginia) in the BBR had cumulative deaths due to COVID-19 higher than the national average rate (298 to 418 vs. 297 per 100,000) [6]. Among these reported deaths, the percentage of African Americans was higher than the average percentage of African Americans (13.5% vs. 12.5%) in the U.S. population [7].
Scientists promptly reacted to the COVID-19 pandemic by accelerating the development of vaccines. U.S. Food and Drug Administration (FDA) initially issued emergency use authorization and fully approved three COVID-19 vaccines [8, 9]. As of April 20, 2022, the percentage of fully vaccinated adults aged 18 and more in each state varied from 61.0% to 90.4%. African Americans were disproportionately impacted by COVID-19 [10, 11] and hold a lower share of being fully vaccinated than their population share among the U.S. population (10.1% vs. 12.5%) [12]. The full-dose COVID-19 vaccination rates among adults in the BBR states, except Florida and Virginia, were below the national rate (60.6% to 71.8% vs. 75.3%) [13]. The average first-dose COVID-19 vaccination rate of African Americans in 10 out of the 11 BBR states (no data for Arkansas) was 1.9% lower than Caucasian Americans [14].
A review study for COVID-19 vaccination hesitancy rates in the U.S. found that 26.3% of American adults were vaccine-hesitant while the number for African Americans was 41.6% [15]. A literature review identified structural and attitudinal barriers to COVID-19 vaccination from long-term experience in the U.S. [16]. The structural barriers included systemic issues that limited one’s ability to access a service (e.g., time, transportation, cost, and clinic or outlet location). In contrast, the attitudinal barriers comprised individual issues (e.g., complacency about the disease being prevented, perceived risks of vaccines, lack of trust toward pharmaceutical companies, health care systems, clinical trials, government agents, misinformation, and misconceptions) [16]. These barriers and their importance could vary among people from different sociodemographic characteristics, including race and ethnicity [17, 18]. A qualitative study found mistrust stemmed from systemic racism and historical mistreatment of African Americans were evident in this population [19]. Other factors, including exposure to myths and misinformation, perceived risk of COVID-19 infection, concerns about the safety, efficacy, and side effects of the COVID-19 vaccines, were identified as major barriers to COVID-19 vaccination among African Americans [15].
Numerous efforts were made to promote COVID-19 vaccination at the population level, such as financial incentives, mandatory vaccination, and social media advertising campaigns [20, 21]. However, the outcomes of these interventions were mixed [20, 22]. A report from the National Institutes of Health recommended that effective and equitable intervention strategies should base on the specific concerns of targeted populations [23]. Since African Americans living in the BBR were hit by COVID-19 harder than other regions due to multiple barriers to the COVID-19 vaccination [4, 17–19], one of the research gaps was which barriers were important to them. Therefore, the objective of this study was to determine important barriers to COVID-19 vaccination for African Americans living in the BBR. This study also examined the important barriers for these African Americans with different COVID-19 vaccine statuses and sociodemographic characteristics (age, gender, education level, and income level) [18, 24]. These important barriers could be used to inform policy decisions and strategies at the broad levels (e.g., state and county levels) to improve the COVID-19 vaccination rate in this specific population.
Methods
This study used a cross-sectional design. Auburn University Institution Review Board (IRB) approved this study and was exempted from human subject review.
Instrument Development
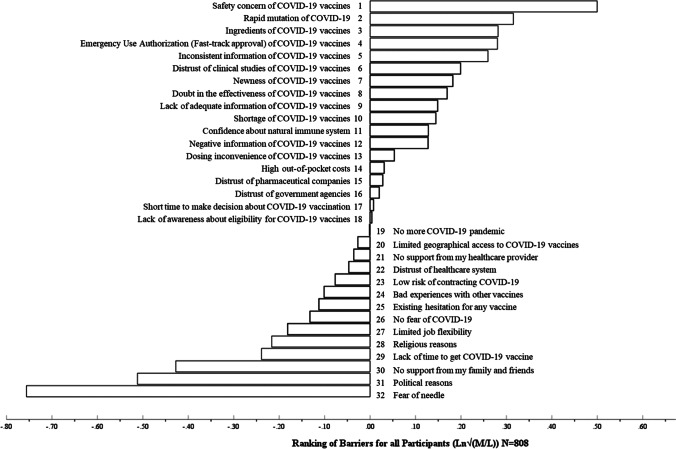
A self-administered, web-based questionnaire survey was developed from September to December 2021. First, 32 barriers to COVID-19 vaccination were obtained from the most recent literature review about attitudes and acceptance among the worldwide general population to receive COVID-19 vaccines at the time of instrument development and confirmed by an expert who has studied the uptake of vaccines for almost two decades [25]. The complete list of barriers and their explanation can be found in Table S1. To reduce the cognitive burden on respondents and increase the discrimination ability to rank barriers, a best–worst scaling (BWS) Case 1 (Object case) was used [26]. A nested balanced incomplete block design (BIBD) generated 62 sets of 16 choice tasks. Each choice task included six barriers with brief description statements. This design ensured that each barrier was compared with other barriers for the same number of times. Each participant was asked to choose the most and least important barriers from six barriers in each choice task, as the example shown in Fig. 1, and to complete 16 choice tasks from only one out of the 62 sets. Questions about participants’ characteristics and their COVID-19 and COVID-19 vaccine experience were also included in the survey. Two experts in social science with extensive experience in survey research were asked to examine any overlapping barriers and the content validity of the survey. The survey was then piloted with 30 participants from the online QualtricsXM panel. No major problem was found.
Fig. 1.
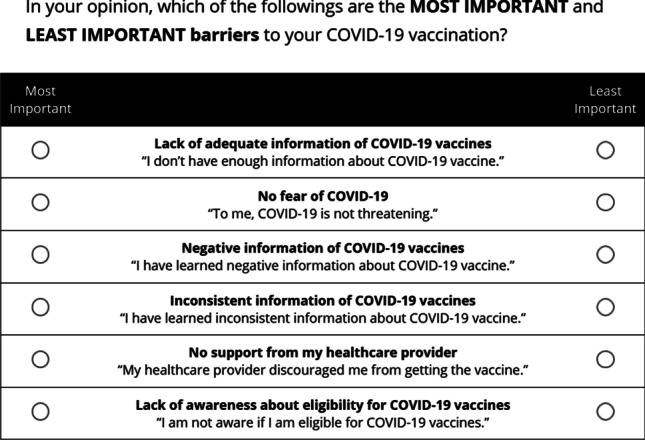
Example of a choice task
Data Collection
There was no specific method to calculate the sample size for BWS [26]. A systematic review of the use of BWS in health care reported the sample size of BWS ranged from 25 to 803 [27]. This survey was administered between January 4 and 27, 2022. A total of 1,000 African American adults living in the BBR were recruited by third parties for a national, online QualtricsXM panel [28]. QualtricsXM indicated that the third parties used the zip codes to identify the target regions and recorded demographics to select the eligible participants. An information letter was provided at the beginning of the survey. Participants who agreed to participate in this study were directed to screening questions to start the survey. Participants were asked to select their state and fill in their zip codes. Only African American participants selected one of the eleven BBR states, and their zip codes matched the zip codes in BBR counties were included in the data analysis.
Data Analysis
Participants’ characteristics and their COVID-19 and COVID-19 vaccine experience were descriptively analyzed via IBM® SPSS® Statistics 28.0. The numbers of times each barrier being chosen as the most (M) and least (L) important were counted through Microsoft 365 Excel®. The natural logarithm of the square root of M counts divided by L counts (Ln√(M/L)) of each barrier was calculated to rank the importance of barriers [29]. All analyses were done for the whole participants. The importance rankings of these barriers among participants by vaccination status (fully vaccinated vs. non-fully vaccinated), gender (female vs. male), age (30 years old or younger vs. older than 30 years old), education (high school or lower vs. college or higher, and income (less than $50,000 per year vs. $50,000 per year or higher) were also examined.
Results
Only 808 respondents with complete responses were included in the data analyses. Table 1 shows the characteristics of the study participants. More than half (55.2%) of them received a full dose of COVID-19 vaccination, which included two doses of the Pfizer or Moderna vaccine and one dose of the Johnson & Johnson vaccine. The percentage of respondents from the 11 states of the BBR ranged from 1.2% (Alabama) to 21.2% (Georgia). The mean age of the participants was 36.1 (SD = 15.4) years old. The majority were single (59.2%), female (71.4%), and had an annual household income of less than $50,000 (63.3%). All of them were non-Hispanic. Approximately 42.6% of the participants were full-time employed, and 46.3% had high school or less education. Their political leaning included conservative (15.0%), liberal (27.7%), and moderate (44.2%). More than half (53.6%) of participants had at least one chronic health condition, and 81.2% had good and better health status.
Table 1.
Participants’ Characteristics
| All participants N = 808 | Fully Vaccinated N = 446 | Not Fully Vaccinated N = 333 | |
|---|---|---|---|
| Average age in years, mean (SD) | 36.12(15.42) | 39.99(16.80) | 31.86(11.97) |
| Current state of residence, n (%) | |||
| Alabama | 10(1.2) | 7(1.6) | 2(0.6) |
| Arkansas | 27(3.3) | 11(2.5) | 15(4.5) |
| Florida | 90(11.1) | 46(10.3) | 42(12.6) |
| Georgia | 171(21.2) | 90(20.2) | 74(22.2) |
| Louisiana | 67(8.3) | 39(8.7) | 24(7.2) |
| Mississippi | 54(6.7) | 37(8.3) | 16(4.8) |
| North Carolina | 88(10.9) | 48(10.8) | 39(11.7) |
| South Carolina | 49(6.1) | 32(7.2) | 15(4.5) |
| Tennessee | 42(5.2) | 22(4.9) | 19(5.7) |
| Texas | 126(15.6) | 65(14.6) | 55(16.5) |
| Virginia | 84(10.4) | 49(11.0) | 32(9.6) |
| Gender, n (%) | |||
| Female | 577(71.4) | 308(69.1) | 249(74.8) |
| Male | 228(28.2) | 137(30.7) | 82(24.6) |
| Others | 3(0.4) | 1(0.2) | 2(0.6) |
| Marital status, n (%) | |||
| Married | 195(24.1) | 127(28.5) | 64(19.2) |
| Single | 478(59.2) | 233(52.2) | 221(66.4) |
| Divorced or separated/ Widowed or surviving partner/Others | 135(16.7) | 86(19.3) | 48(14.4) |
| Insurance, n (%) | |||
| Private health | 228(35.6) | 162(36.3) | 122(36.6) |
| Medicaid/Medicare | 344(42.6) | 178(39.9) | 156(46.8) |
| Tricare/Veterans Health Insurance | 31(3.8) | 21(4.7) | 10(3.0) |
| Others | 28(3.5) | 11(2.5) | 13(3.9) |
| I do not have health insurance | 117(14.5) | 74(16.6) | 32(9.6) |
| Average annual household income, n (%) | |||
| Less than $25,000 per year | 258(31.9) | 116(26.0) | 132(39.6) |
| $25,000 to $49,999 per year | 254(31.4) | 140(31.4) | 108(32.4) |
| $50,000 to $99,999 per year | 187(23.1) | 125(28.0) | 57(17.1) |
| $100,000 to $149,999 per year | 43(5.3) | 28(6.3) | 15(4.5) |
| $150,000 to $199,999 per year | 12(1.5) | 6(1.3) | 5(1.5) |
| $200,000 and more per year | 15(1.9) | 13(2.9) | 1(0.3) |
| Prefer not to say | 39(4.8) | 18(4.0) | 15(4.5) |
| Education background, n (%) | |||
| High school or less than high school | 374(46.3) | 170(38.1) | 190(57.0) |
| Technical school | 70(8.7) | 40(9.0) | 29(8.7) |
| 2-year college degree (Associate’s degree) | 156(19.3) | 88(19.7) | 59(17.7) |
| 4-year college degree (e.g., BA, BS) | 146(18.1) | 103(23.1) | 41(12.3) |
| Graduate or professional degree (e.g., MBA, MS, MD, PhD) | 62(7.7) | 45(10.1) | 14(4.2) |
| Employment status, n (%) | |||
| Full-time employed | 344(42.6) | 207(46.4) | 128(38.4) |
| Part-time employed | 105(13.0) | 57(12.8) | 46(13.8) |
| Self-employed | 69(8.5) | 29(6.5) | 35(10.5) |
| Student | 50(6.2) | 21(4.7) | 23(6.9) |
| Retired/ Stay-at-home spouse/ Unemployed | 220(27.3) | 123(27.5) | 91(27.3) |
| Others | 20(2.5) | 9(2.0) | 10(3.0) |
| Politic leaning, n (%) | |||
| Conservative | 121(15.0) | 54(12.1) | 64(19.2) |
| Liberal | 224(27.7) | 155(34.8) | 65(19.5) |
| Moderate | 357(44.2) | 201(45.1) | 150(45.0) |
| Prefer not to say | 106(13.1) | 36(8.1) | 54(16.2) |
| Chronic disease, n(%) | |||
| Yes | 433(53.6) | 276(61.9) | 148(44.4) |
| No | 375(46.4) | 170(38.1) | 185(55.6) |
| General Health, n(%) | |||
| Excellent | 171(21.2) | 96(21.5) | 66(19.8) |
| Very good | 234(29.0) | 126(28.3) | 100(30.0) |
| Good | 256(31.7) | 150(33.6) | 98(29.4) |
| Fair | 130(16.1) | 65(14.6) | 62(18.6) |
| Poor | 17(2.1) | 9(2.0) | 7(2.1) |
Table 2 shows the COVID-19 related experiences of the study participants. About two-thirds of participants (60.1%) had COVID-19 test experience, and 34.8% had positive COVID-19 results at least once. Almost half of the participants (43.5%) experienced beyond moderate difficulty due to COVID-19. Similarly, about half of the participants reported that it was acceptable that the government (49.8%) and employers (50.6%) asked them to receive COVID-19 vaccination.
Table 2.
Participants’ COVID-19 Related Experiences
| COVID-19 test experience, n(%) | All participants, N = 808 | Fully Vaccinated, N = 446 | Not Fully Vaccinated, N = 333 |
| Yes | 486(60.1) | 301(67.5) | 174(52.3) |
| No | 306(37.9) | 141(31.6) | 156(46.8) |
| Prefer not to say | 16(2.0) | 4(0.9) | 3(0.9) |
| COVID-19 test result, n(%) | N = 486* | N = 301* | N = 174* |
| Positive result at least once | 169(34.8) | 93(30.9) | 73(42.0) |
| Always negative result | 310(63.8) | 204(67.8) | 100(57.5) |
| Prefer not to say | 7(1.4) | 4(1.3) | 1(0.6) |
| Experienced difficulty due to COVID-19, n(%) | N = 808 | N = 446 | N = 333 |
| Extremely | 159(19.7) | 83(18.6) | 70(21.0) |
| Very | 192(23.8) | 91(20.4) | 94(28.4) |
| Moderately | 228(28.2) | 142(31.8) | 81(24.3) |
| Slightly | 96(11.9) | 57(12.8) | 38(11.4) |
| Not at all | 133(16.5) | 73(16.4) | 50(15.0) |
| Government request taking vaccine, n(%) | |||
| Very acceptable | 239(29.6) | 189(42.4) | 48(14.4) |
| Acceptable | 163(20.2) | 112(25.1) | 49(14.7) |
| Neutral | 191(23.6) | 90(20.2) | 93(27.9) |
| Unacceptable | 81(10.0) | 26(5.8) | 50(15.0) |
| Very unacceptable | 100(12.4) | 21(4.7) | 77(23.1) |
| Prefer not to say | 34(4.2) | 8(1.8) | 16(4.8) |
| Employer request taking vaccine, n(%) | |||
| Very acceptable | 224(27.7) | 176(39.5) | 46(13.8) |
| Acceptable | 185(22.9) | 126(28.3) | 59(17.7) |
| Neutral | 203(25.1) | 95(21.3) | 96(28.8) |
| Unacceptable | 65(8.0) | 22(4.9) | 40(12.0) |
| Very unacceptable | 82(10.1) | 16(3.6) | 64(19.2) |
| Prefer not to say | 26(3.2) | 7(1.6) | 14(4.2) |
| Not applicable | 23(2.8) | 4(0.9) | 14(4.2) |
*486 participants had tested COVID-19
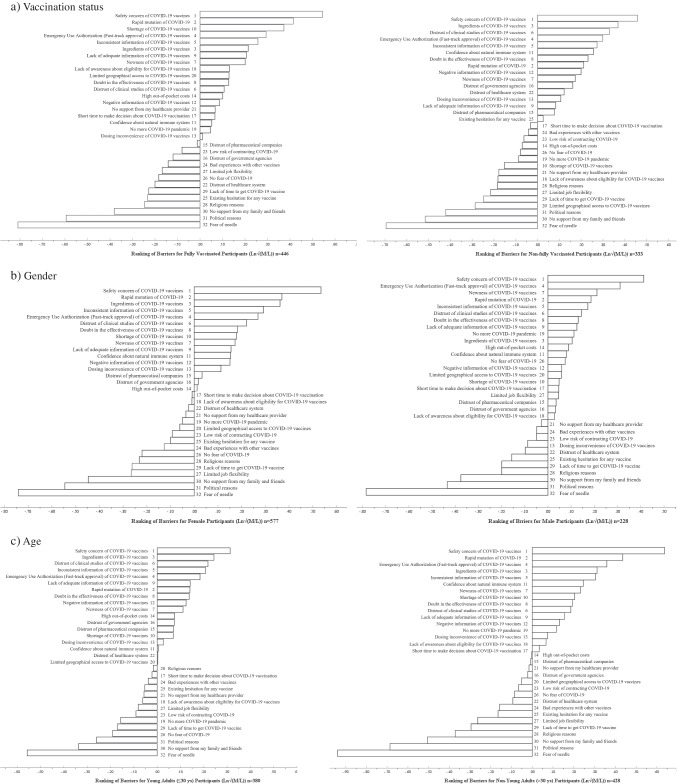
Figure 2 shows the ranks of barriers to COVID-19 vaccination among Africa Americans in BBR. Among 32 barriers to COVID-19 vaccination, the five most important barriers for all participants were “safety concern of COVID-19 vaccines,” (Ln√(M/L) = 0.50); “rapid mutation of COVID-19,” (Ln√(M/L) = 0.36); “ingredients of COVID-19 vaccines,” (Ln√(M/L) = 0.28); “Emergency Use Authorization (Fast-track approval) of COVID-19 vaccines,” (Ln√(M/L) = 0.28); and “inconsistent information of COVID-19 vaccines,” (Ln√(M/L) = 0.26). On the other hand, the five least important barriers were “religious reasons,” (Ln√(M/L) = -0.21); “lack of time to get COVID-19 vaccine,” (Ln√(M/L) = -0.23); “no support from my family and friends,” (Ln√(M/L) = -0.42); “political reasons,” (Ln√(M/L) = -0.51); and “fear of the needle” (Ln√(M/L) = -0.77).
Fig. 2.
Rank of barriers to COVID-19 vaccination among Africa Americans in Black Belt Region (From high to low). Ln√(M/L): The natural logarithm of the square root of most (M) counts divided by least (L) counts of each barrier
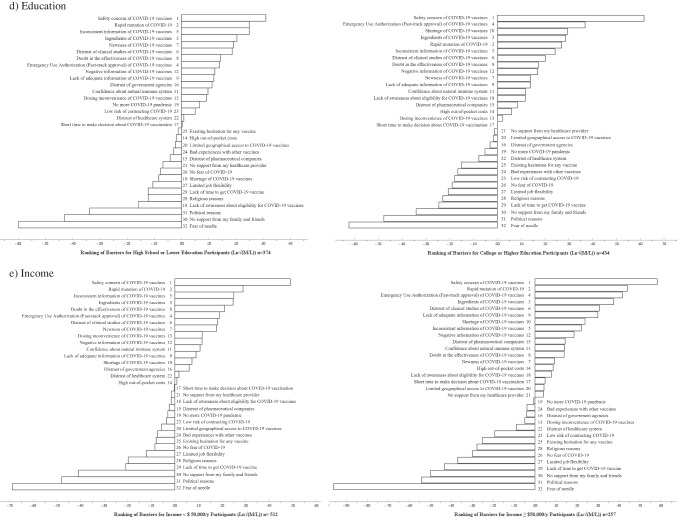
Figure 3 shows the ranks of barriers to COVID-19 vaccination among African Americans in BBR by vaccination status, gender, age, education, and income. For the fully COVID-19 vaccinated participants, the five most important barriers were “Safety concern of COVID-19 vaccines”, “Rapid mutation of COVID-19”, “Shortage of COVID-19 vaccines”, “Emergency Use Authorization (Fast-track approval) of COVID-19 vaccines”, and “Inconsistent information of COVID-19 vaccines”. The “Ingredients of COVID-19 vaccines” and “Distrust of clinical studies of COVID-19 vaccines” became the top five most important barriers to the participants who were not fully vaccinated, instead of “Rapid mutation of COVID-19” and “Shortage of COVID-19 vaccines”. Interestingly, the “Shortage of COVID-19 vaccines” and “Limited geographical access to COVID-19 vaccines” barriers were ranked higher by the fully vaccinated participants than those who were not fully vaccinated. Female participants had the five most important barriers, the same as all participants. The “Newness of COVID-19 vaccines” became the third important barrier among male participants, while it was not among the five most important barriers for all participants. The five most important barriers for different age groups were similar to those for all participants. However, the “Distrust of clinical studies of COVID-19 vaccines” became one of the five most important barriers for young adults or participants 30 years old or under. While most of the five most important barriers for the participants with different education levels were similar to those for all participants, the “Shortage of COVID-19 vaccines” barrier became the third most important barrier for the participants with a college education or higher. Also, the “Doubt in the effectiveness of COVID-19 vaccines” became one of the top five most important barriers for the participants with lower income levels.
Fig. 3.
Ranks of barriers to COVID-19 vaccination among Africa Americans in BBR by vaccination status, gender, age, education, and income (From high to low). a) Vaccination status, b) Gender, c) Age, d) Education, e) Income. 1. Ln√(M/L): The natural logarithm of the square root of most (M) counts divided by least (L) counts of each barrier. 2. The numbers showed in Fig. 3 was the ranking number of barriers in all participants in Fig. 2. (Number 1 is the most important and number 32 is the least important.)
Discussion
This study employed a rigorous study design, including the nested BIBD and BWS, to rank the importance of the barriers to COVID-19 vaccination among overall African Americans in the BBR and subgroups based on their vaccination status, gender, age, education, and income. The study intended to include specific contexts of the barriers. For instance, the distrusts of the clinical trial of the COVID-19 vaccine, pharmaceutical companies, and government agencies were three separate barriers. Researchers and policymakers could then generate and implement strategies to specifically target these barriers.
Among the five most important barriers to all participants, four barriers were related to the COVID-19 vaccine, including the safety, the ingredients, the fast-track approval, and inconsistent information about the vaccine. Another barrier was the rapid mutation of COVID-19. The barriers related to the COVID-19 vaccine were consistent with the results from previous studies suggesting that the safety and effectiveness of the vaccine were the top reasons for COVID-19 vaccine hesitancy [30, 31]. A qualitative study also reported that African Americans would like to wait and see the short-term and long-term safety of the COVID-19 vaccine [19]. On the other hand, the barrier from the rapid mutation of COVID-19 was a relatively recent reason since the survey was administered in January 2022, when the country was experiencing new variants, including Delta and Omicron, at the time of the study [32]. The participants might be concerned about the uncertain effectiveness of vaccines to new variants.
It is noteworthy that although the distrust of the clinical trial of the COVID-19 vaccine was ranked sixth among all participants, it reflected that historical mistreatment in clinical trials was still an important barrier among African Americans living in the BBR. Also, this barrier made the third place of importance among the participants who were not fully vaccinated. These results were consistent with previous studies highlighting the Black community's historical mistreatment and associated distrust as barriers to the COVID-19 vaccination [33–35].
Our study also showed that “religious reasons,” “lack of time to get COVID-19 vaccine,” “no support from my family and friends,” “political reasons,” and “fear of the needle” were the five least important barriers to COVID-19 vaccination among African Americans living in the BBR. The least important barrier, “fear of the needle,” was consistent with a nationwide study suggesting that fear of the needle was a less frequently endorsed reason to decline the COVID-19 vaccine [30]. Various studies reported mixed results for other lower-ranked barriers [31, 36–38]. For instance, a previous study showed that Christian nationalism and political conservatives were more likely to hold anti-vaccine attitudes [38]. On the other hand, studies indicated that political ideology had no relationship with attitude toward the COVID-19 vaccine among the U.S. population, and faith-based institutions worked with a social worker to promote vaccination among African American community [31, 39]. Also, a previous study suggested that the opinion of family members and friends was associated with persons’ willingness to take vaccines, and this opinion could be a facilitator or barrier to vaccination [40]. Family members could persuade people previously hesitant or resistant to receiving the vaccine to take the COVID-19 vaccine [41]. It is noteworthy that these lower-ranking barriers might become more important to the participants if other higher-ranking barriers were overcome.
This study also ranked the importance of the barriers among the fully and non-fully vaccinated participants separately to reflect the opinions of those individuals who could and could not overcome the barriers to getting vaccinated at the survey time. Among the participants who were fully vaccinated and not fully vaccinated, some barriers remained in the same ranks as in the overall analyses, while the others changed. For example, the safety concern of the COVID-19 vaccine was ranked the first most important regardless of vaccination status. The fast-track approval and inconsistent information on COVID-19 vaccines remained the fourth and fifth most important barriers, respectively. These results reinforced that the safety concern, fast-track approval, and inconsistent information about COVID-19 vaccines must be addressed to increase the vaccination rate of the African Americans living in the BBR. On the other hand, other barriers (e.g., the distrust of clinical studies and concerns about the ingredients of the vaccine) were ranked higher among the individuals who were not fully vaccinated. They should be emphasized or scrutinized because they might make African Americans living in the BBR, who were not yet vaccinated, decide to get COVID-19 vaccines.
The barriers of “Shortage of COVID-19 vaccines” and “Limited geographical access to COVID-19 vaccines” were ranked higher in the fully vaccinated group than the not-fully vaccinated group. This finding suggested that these logistical barriers to COVID-19 vaccination were more important barriers to the vaccinated participants than the participants who were not fully vaccinated. It was possible that the vaccinated participants were early vaccine adopters who experienced these logistical barriers when COVID-19 vaccines were just available. A previous study found counties with a higher number of non-Hispanic African American were disadvantaged by the disparity of COVID-19 vaccine distribution at the early roll-out stage [42]. While these logistical barriers became less important since the COVID-19 vaccine roll-out effort might be more effective in BBR at the time of the survey, some participants, who were not fully vaccinated, still experienced other barriers and did not get the vaccines.
The ranks of some barriers slightly varied for the participants with different genders, ages, education levels, and income levels. The “Newness of COVID-19 vaccines” was the third most important barrier among male participants. The finding aligned with a previous study that male participants were more likely to mistrust medical research [43]. One possible reason was that male participants were less likely to have a positive attitude toward the future COVID-19 vaccine than female participants [44]. Therefore, they were more concerned about the newly developed COVID-19 vaccine. For the younger African Americans or the African Americans who were 30 years old or less living in BBR, this study indicated that the “Distrust of clinical studies of COVID-19 vaccines” was an important barrier to them. One meta-analysis found that the effectiveness of COVID-19 vaccines was better among younger people than older people, but the incidence of adverse events was higher among younger people [45]. It was possible that the information on the higher incidence of adverse events among younger people found in clinical trials was not widespread. The lack of this evidence contradicted the real-life observation of younger people, which led to more distrust of clinical studies among younger African American in BBR. This study found that the “Shortage of COVID-19 vaccines” barrier became the third most important barrier for the participants with college or higher education, which was also an important barrier to fully vaccinated participants. Previous studies showed that higher education was associated with higher acceptance of the COVID-19 vaccine in the U.S [46, 47]. and college or higher education participants tended to be earlier adopters of COVID-19 vaccines [48]. Therefore, it was possible that the shortage of COVID-19 vaccine in the early vaccine rollout stage was an important barrier for them. The “Doubt in the effectiveness of COVID-19 vaccines” barrier became a top five most important barrier for the participants with lower income levels. At the same time, it ranked as the 12th most important barrier for participants with higher income levels. This finding echoed a previous study that people with lower incomes were more likely to mistrust the benefit of vaccines [49].
Interestingly, most of the important barriers in this study, such as concerns related to safety, fast-track approval, inconsistent information of the COVID-19 vaccine, the distrust of clinical studies, concerns about the ingredients of the vaccine, and being confident about the natural immune system, could be overcome by communicating with effective and trusted channels, messengers, and contents [50]. A detailed communication plan, such as addressing the concerns about the rapid mutation of COVID-19 through social marketing [51], and tailoring messages to segmented audiences, would promote COVID-19 vaccination among African Americans living in the BBR [52]. Consistent messages communicating the safety of COVID-19 vaccination in this population should be accompanied by an explanation of the COVID-19 vaccine approval process and the subsequent safety and effectiveness monitoring steps conducted by the U.S. FDA [23]. It is critical to incorporate components to acknowledge the historical mistreatment of African Americans, provide a fact about the vaccine ingredients [53] and generate social norms about vaccination when designing the communication messages to target African Americans in BBR who were not yet fully vaccinated [23]. This ranked importance of barriers in the participants with different genders, ages, and income levels could inform the strategies to improve the uptake of the COVID-19 vaccine in these respective segmented populations. For instance, post-marketing surveillance information should be provided to reassure the safety and effectiveness of COVID-19 vaccines to address the “Newness of COVID-19 vaccines” barrier if the targeted population was male African Americans living in BBR [54]. To improve the COVID-19 vaccine uptake among younger African Americans in BBR, the information about the adverse events in clinical trials among them should be acknowledged [45]. Similarly, the effectiveness of the COVID-19 vaccine should be highlighted if the targeted population were African Americans with lower incomes in BBR. Also, it should be noted that the important barriers to COVID-19 vaccination among African Americans in BBR in this study could be barriers among other populations, including Caucasian Americans and African Americans in different regions of the U.S., but the importance of each barrier might differ.
To our knowledge, this study was the first to identify the important barriers to African Americans living in the BBR. However, this study suffered from four major limitations. First, this cross-sectional study could not capture the participants’ opinions about barriers to COVID-19 vaccination over time [55]. Second, the barriers in this study might not be mutually exclusive (e.g., emergency use authorization and political reasons). However, this study intended to include specific barriers to inform strategies to address these content-specific concerns to targeted populations. Third, the participants in this study might not represent the overall population of African Americans living in the BBR. Especially, 71.4% of all participants were female, which was higher than the national average of female African Americans (53.3%) [56]. The results from this study should be cautiously interpreted. Another limitation was that some barriers had similar Ln√(M/L) results (e.g., “ingredients of COVID-19 vaccines,” (Ln√(M/L) = 0.28); “Emergency Use Authorization (Fast-track approval) of COVID-19 vaccines,” (Ln√(M/L) = 0.28) and “inconsistent information of COVID-19 vaccines” (Ln√(M/L) = 0.26)). Their rankings might be subject to change.
Conclusions
The important barriers to COVID-19 vaccination for African Americans living in the BBR centered around issues (e.g., the safety concern, ingredients, emergency use authorization, inconsistent information about COVID-19 vaccines, and the rapid mutation of COVID-19), which could be overcome by tailored communication interventions. Future research should focus on generating, testing, and implementing communication strategies to promote COVID-19 vaccination for this population.
Supplementary Information
Below is the link to the electronic supplementary material.
Acknowledgements
We acknowledge that Dr. Salisa Westrick helped review the list of barriers to COVID-19 vaccination.
Author Contributions
All authors contributed to the study's conception and design. Material preparation, data collection, and analysis were performed by Surachat Ngorsuraches, Heqin Yang, Nabin Poudel, and Savanah Simpson. The first draft of the manuscript was written by Heqin Yang, and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Funding
This study was funded by PhRMA Collaborative Actions to Reach Equity (CAREs).
Data availability
Raw data of this study is available upon request to the corresponding author.
Declarations
Ethics Approval
The Auburn University Institutional Review Board reviewed and determined the study as exempt.
Consent to Participate
Informed consent was obtained from all individual participants included in the study.
Conflict of Interest
The authors declare no competing interests.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Mofijur M, et al. Impact of COVID-19 on the social, economic, environmental and energy domains: Lessons learnt from a global pandemic. Sustain Prod Consum. 2021;26:343–359. doi: 10.1016/j.spc.2020.10.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Xu Z, et al. Impacts of COVID-19 on Global Supply Chains: Facts and Perspectives. IEEE Eng Manage Rev. 2020;48(3):153–166. doi: 10.1109/EMR.2020.3018420. [DOI] [Google Scholar]
- 3.WHO Coronavirus (COVID-19) Dashboard. 2022 April 20, 2022. Accessed 21 Apr 2022. Available from: https://covid19.who.int/.
- 4.COVID Data Tracker: daily update for the United States. 2022. Accessed 21 Apr 2022. Available from: https://covid.cdc.gov/covid-data-tracker/#datatracker-home.
- 5.Chi G, et al. Lost in the Black Belt South: health outcomes and transportation infrastructure. Environ Monit Assess. 2019;191(Suppl 2):297. doi: 10.1007/s10661-019-7416-1. [DOI] [PubMed] [Google Scholar]
- 6.COVID Data Tracker: compare trends in COVID-19 cases and deaths in the US. 2022. Accessed 21 Apr 2022. Available from: https://covid.cdc.gov/covid-data-tracker/#compare-trends_comptrends-deaths-cum-rate-log.
- 7.COVID Data Tracker: demographic trends of COVID-19 cases and deaths in the US reported to CDC. 2022. Accessed 8 May 2022. Available from: https://covid.cdc.gov/covid-data-tracker/#demographics.
- 8.FDA News Release: FDA approves first COVID-19 vaccine. 2021. Accessed 26 Mar 2022. Available from: https://www.fda.gov/news-events/press-announcements/fda-approves-first-covid-19-vaccine.
- 9.COVID-19 Vaccines. 2022. Accessed 8 May 2022. Available from: https://www.fda.gov/emergency-preparedness-and-response/coronavirus-disease-2019-covid-19/covid-19-vaccines.
- 10.Cyrus E, et al. The Impact of COVID-19 on African American Communities in the United States. Health Equity. 2020;4(1):476–483. doi: 10.1089/heq.2020.0030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Tai DBG, et al. The Disproportionate Impact of COVID-19 on Racial and Ethnic Minorities in the United States. Clin Infect Dis. 2021;72(4):703–706. doi: 10.1093/cid/ciaa815. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.COVID Data Tracker: demographic characteristics of people receiving COVID-19 vaccinations in the United States. 2022. Accessed 21 Apr 2022. Available from: https://covid.cdc.gov/covid-data-tracker/#vaccination-demographic.
- 13.COVID Data Tracker: COVID-19 vaccinations in the United States. 2022. Accessed 21 Apr 2022. Available from: https://covid.cdc.gov/covid-data-tracker/#vaccinations_vacc-total-admin-rate-total.
- 14.Latest Data on COVID-19 vaccinations by race/ethnicity. 2022. Accessed 15 Apr 2022. Available from: https://www.kff.org/coronavirus-covid-19/issue-brief/latest-data-on-covid-19-vaccinations-by-race-ethnicity/.
- 15.Khubchandani J, Macias Y. COVID-19 vaccination hesitancy in Hispanics and African-Americans: A review and recommendations for practice. Brain Behav Immun Health. 2021;15:100277. doi: 10.1016/j.bbih.2021.100277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Zhang Y, Fisk RJ. Barriers to vaccination for coronavirus disease 2019 (COVID-19) control: experience from the United States. Glob Health J. 2021;5(1):51–55. doi: 10.1016/j.glohj.2021.02.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Bunch L. A Tale of Two Crises: Addressing Covid-19 Vaccine Hesitancy as Promoting Racial Justice. HEC Forum. 2021;33(1–2):143–154. doi: 10.1007/s10730-021-09440-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Szilagyi PG, et al. The role of trust in the likelihood of receiving a COVID-19 vaccine: Results from a national survey. Prev Med. 2021;153:106727. doi: 10.1016/j.ypmed.2021.106727. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Bateman LB, et al. Exploring COVID-19 Vaccine Hesitancy Among Stakeholders in African American and Latinx Communities in the Deep South Through the Lens of the Health Belief Model. Am J Health Promot. 2022;36(2):288–295. doi: 10.1177/08901171211045038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Athey S, et al. Digital public health interventions at scale: The impact of social media advertising on beliefs and outcomes related to COVID vaccines. Proc Natl Acad Sci U S A. 2023;120(5):e2208110120. doi: 10.1073/pnas.2208110120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Andreas M, et al. Interventions to increase COVID-19 vaccine uptake: a scoping review. Cochrane Database Syst Rev. 2022;8(8):CD015270. doi: 10.1002/14651858.CD015270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Batteux E, et al. The effectiveness of interventions for increasing COVID-19 vaccine uptake: a systematic review. Vaccines (Basel). 2022;10(3):386. 10.3390/vaccines10030386. [DOI] [PMC free article] [PubMed]
- 23.Chou WY, Burgdorf CE, Gaysynsky A, Hunter CM. COVID-19 vaccination communication: applying behavioral and social science to address vaccine hesitancy and foster vaccine confidence. 2021. Accessed 3 May 2022. Available from: https://obssr.od.nih.gov/sites/obssr/files/inline-files/OBSSR_VaccineWhitePaper_FINAL_508.pdf?ceid=4112502&emci=712687ce-1e60-eb11-a607-00155d43c992&emdi=e4597073-8d64-eb11-9889-00155d43c992.
- 24.van den Broek-Altenburg EM AA, Hess S, Benson J. The effect of unobserved preferences and race on vaccination hesitancy for COVID-19 vaccines: implications for health disparities. 2021;27(9-a Suppl):S4-S13. 10.18553/jmcp.2021.27.9-a.s4. [DOI] [PubMed]
- 25.Cascini F, et al. Attitudes, acceptance and hesitancy among the general population worldwide to receive the COVID-19 vaccines and their contributing factors: A systematic review. E Clin Med. 2021;40:101113. doi: 10.1016/j.eclinm.2021.101113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Louviere J, et al. An introduction to the application of (case 1) best–worst scaling in marketing research. Int J Res Mark. 2013;30(3):292–303. doi: 10.1016/j.ijresmar.2012.10.002. [DOI] [Google Scholar]
- 27.Cheung KL, et al. Using Best-Worst Scaling to Investigate Preferences in Health Care. Pharmacoeconomics. 2016;34(12):1195–1209. doi: 10.1007/s40273-016-0429-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Miller CA, et al. A Tale of Two Diverse Qualtrics Samples: Information for Online Survey Researchers. Cancer Epidemiol Biomarkers Prev. 2020;29(4):731–735. doi: 10.1158/1055-9965.EPI-19-0846. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Cheung KL, et al. Comparison of statistical analysis methods for object case best-worst scaling. J Med Econ. 2019;22(6):509–515. doi: 10.1080/13696998.2018.1553781. [DOI] [PubMed] [Google Scholar]
- 30.Ruiz JB, Bell RA. Predictors of intention to vaccinate against COVID-19: Results of a nationwide survey. Vaccine. 2021;39(7):1080–1086. doi: 10.1016/j.vaccine.2021.01.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Pogue K, et al. Influences on attitudes regarding potential COVID-19 vaccination in the United States. Vaccines (Basel). 2020;8(4):582. 10.3390/vaccines8040582. [DOI] [PMC free article] [PubMed]
- 32.Variant proportions: monitoring variant proportions 2022. Accessed 21 Apr 2022. Available from: https://covid.cdc.gov/covid-data-tracker/#variant-proportions.
- 33.Balasuriya L, et al. COVID-19 Vaccine Acceptance and Access Among Black and Latinx Communities. JAMA Netw Open. 2021;4(10):e2128575. doi: 10.1001/jamanetworkopen.2021.28575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Ferdinand KC, Nedunchezhian S, Reddy TK. The COVID-19 and Influenza "Twindemic": Barriers to Influenza Vaccination and Potential Acceptance of SARS-CoV2 Vaccination in African Americans. J Natl Med Assoc. 2020;112(6):681–687. doi: 10.1016/j.jnma.2020.11.001. [DOI] [PubMed] [Google Scholar]
- 35.Thompson HS, et al. Factors Associated With Racial/Ethnic Group-Based Medical Mistrust and Perspectives on COVID-19 Vaccine Trial Participation and Vaccine Uptake in the US. JAMA Netw Open. 2021;4(5):e2111629. doi: 10.1001/jamanetworkopen.2021.11629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Fridman A, Gershon R, Gneezy A. COVID-19 and vaccine hesitancy: A longitudinal study. PLoS ONE. 2021;16(4):e0250123. doi: 10.1371/journal.pone.0250123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Corpuz JCG. Multisectoral Approach on COVID-19 vaccination: a proposed solution on vaccine hesitancy. J Public Health (Oxf) 2021;43(2):e370–e371. doi: 10.1093/pubmed/fdab085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Corcoran KE, Scheitle CP, DiGregorio BD. Christian nationalism and COVID-19 vaccine hesitancy and uptake. Vaccine. 2021;39(45):6614–6621. doi: 10.1016/j.vaccine.2021.09.074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Shelton RL, et al. Telehealth in a Washington, DC African American Religious Community at the Onset of COVID-19: Showcasing a Virtual Health Ministry Project. Soc Work Health Care. 2021;60(2):208–223. doi: 10.1080/00981389.2021.1904322. [DOI] [PubMed] [Google Scholar]
- 40.Cordina M, Lauri MA, Lauri J. Attitudes towards COVID-19 vaccination, vaccine hesitancy and intention to take the vaccine. Pharm Pract (Granada) 2021;19(1):2317. doi: 10.18549/PharmPract.2021.1.2317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Ashley Kirzinger GS, Mollyann B. COVID-19 vaccine monitor: in their own words, six months later. 2021. Accessed 29 Apr 2022. Available from: https://www.kff.org/coronavirus-covid-19/poll-finding/kff-covid-19-vaccine-monitor-in-their-own-words-six-months-later/.
- 42.Hernandez I, et al. Disparities in distribution of COVID-19 vaccines across US counties: A geographic information system-based cross-sectional study. PLoS Med. 2022;19(7):e1004069. doi: 10.1371/journal.pmed.1004069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Ding ELPN, Manson JE, Sherber NS, Braunstein JB. Sex Differences in Perceived Risks, Distrust, and Willingness to Participate in Clinical Trials: A Randomized Study of Cardiovascular Prevention Trials. Arch Intern Med. 2007;167(9):905–912. doi: 10.1001/archinte.167.9.905. [DOI] [PubMed] [Google Scholar]
- 44.Seale H, et al. Examining Australian public perceptions and behaviors towards a future COVID-19 vaccine. BMC Infect Dis. 2021;21(1):120. doi: 10.1186/s12879-021-05833-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Wang J, Tong Y, Li D, Li J, Li Y. The impact of age difference on the efficacy and safety of COVID-19 vaccines: a systematic review and meta-analysis. Front Immunol. 2021;12:758294. 10.3389/fimmu.2021.758294. [DOI] [PMC free article] [PubMed]
- 46.Lazarus JV, et al. Hesitant or Not? The Association of Age, Gender, and Education with Potential Acceptance of a COVID-19 Vaccine: A Country-level Analysis. J Health Commun. 2020;25(10):799–807. doi: 10.1080/10810730.2020.1868630. [DOI] [PubMed] [Google Scholar]
- 47.Boyle J, et al. Understanding the impact of general vaccine attitudes on the intent for early COVID-19 vaccination. Vaccines (Basel). 2023;11(2):235. 10.3390/vaccines11020235. [DOI] [PMC free article] [PubMed]
- 48.Hunter-Mullis K, et al. Perceived COVID-19 vaccine attributes associated with early adoption among adults in rural Indiana. Health Educ Res. 2022;37(6):466–475. doi: 10.1093/her/cyac029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Paul E, Steptoe A, Fancourt D. Attitudes towards vaccines and intention to vaccinate against COVID-19: Implications for public health communications. Lancet Reg Health Eur. 2021;1:100012. doi: 10.1016/j.lanepe.2020.100012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Kerrigan D, et al. Context and considerations for the development of community-informed health communication messaging to support equitable uptake of COVID-19 vaccines among communities of color in Washington, DC. J Racial Ethn Health Disparities. 2022;10(1):395–409. 10.1007/s40615-022-01231-8. [DOI] [PMC free article] [PubMed]
- 51.French J, et al. Key Guidelines in Developing a Pre-Emptive COVID-19 Vaccination Uptake Promotion Strategy. Int J Environ Res Public Health. 2020;17(16). [DOI] [PMC free article] [PubMed]
- 52.Washburn KJ, et al. Orange County, California COVID-19 Vaccine Equity Best Practices Checklist: A Community-Centered Call to Action for Equitable Vaccination Practices. Health Equity. 2022;6(1):3–12. doi: 10.1089/heq.2021.0048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Peteet B, et al. Faith, Fear, and Facts: A COVID-19 Vaccination Hesitancy Intervention for Black Church Congregations. Vaccines (Basel). 2022;10(7). [DOI] [PMC free article] [PubMed]
- 54.Dhanda SOV, Lynn E, Saad S. Postmarketing studies: can they provide a safety net for COVID-19 vaccines in the UK? BMJ Evidence-Based Med. 2022;27:1–6. doi: 10.1136/bmjebm-2020-111507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Nguyen KH, et al. Changes in COVID-19 vaccination receipt and intention to vaccinate by socioeconomic characteristics and geographic area, United States, January 6 - March 29, 2021. Ann Med. 2021;53(1):1419–1428. doi: 10.1080/07853890.2021.1957998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.S0201: Selected Population Profile in the United States. 2019: ACS 1-Year estimates selected population profiles 2019. Accessed 12 Aug 2022. Available from: https://data.census.gov/cedsci/table?q=S0201%3A%20SELECTED%20POPULATION%20PROFILE%20IN%20THE%20UNITED%20STATES&t=004%20-%20Black%20or%20African%20American%20alone&tid=ACSSPP1Y2019.S0201&hidePreview=true.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Raw data of this study is available upon request to the corresponding author.