Lung cancer (LC) is the second most common cancer in the United States and the leading cause of cancer deaths in men and women (1). Previous studies have shown disparities in LC mortality between sexes and races (2–5). Our primary aim was to assess changing disparities in LC mortality in the United States over the past 2 decades.
We extracted LC mortality data (International Classification of Diseases-Tenth Revision, C34) from 1999 to 2019 from the CDC WONDER (Centers for Disease Control and Prevention’s Wide-ranging ONline Data for Epidemiologic Research) database, a comprehensive online public health information system developed and owned by the CDC and its collaborating partners to serve public health practice and research (6). Age-standardized mortality rates (ASMRs) were reported yearly on the basis of race and sex per 100,000 population. Research ethics approval was unnecessary as the data used in this analysis is publicly available. We assessed and compared the four groups' absolute and relative changes in LC mortality and used Joinpoint regression analysis to assess trends in LC mortality (Command Line Version 4.5.0.1) (7). Joinpoint regression tests for changes in the model with the sequential addition of Joinpoints in which there is a significant change in the slope of the line and computes an estimated annual percentage change (EAPC) for each trend by fitting a regression line to the natural logarithm of the mortality rates.
Over 20 years, 3,244,746 LC deaths were reported. For White patients, ASMR data were available for all 50 states from 1999 to 2019, plus Washington, DC from 2015. For Black patients, ASMR data were available for 38 states for men and 37 states for women, with varying start and end years. Nationally, ASMR for women decreased from 40.2 (95% confidence interval [CI], 39.9–40.5) to 28.2 (95% CI, 28.0–28.4) (PC, −29.9%), for men from 76.8 (95% CI, 76.3–77.3) to 40.1 (95% CI, 39.8–40.3) (−47.8%), for White population from 55.4 (95% CI, 55.1–55.7) to 34.2 (95% CI, 34.0–34.4) (−38.3%), and Black population from 64.7 (95% CI, 63.7–65.8) to 34.5 (95% CI, 34.0–35.1) (−46.7%). Even though the rate of decline from 1999 to 2019 was steeper in the Black population as compared with the White population, with the steepest for Black men (−54.2%) by 2019, the order of mortality burden was unchanged, with the highest ASMR being in Black men (47.1), followed by White men (40.3), White women (29.4), and Black women (25.9). This indicates even though disparities have decreased with curves almost meeting each other, the disparities certainly still exist. At the same time, at the state level, ASMR decreased in all states except South Dakota (+13.0%) for White women, Kansas (+22.5%) for Black women, and Nebraska (+14.4%) for Black men.
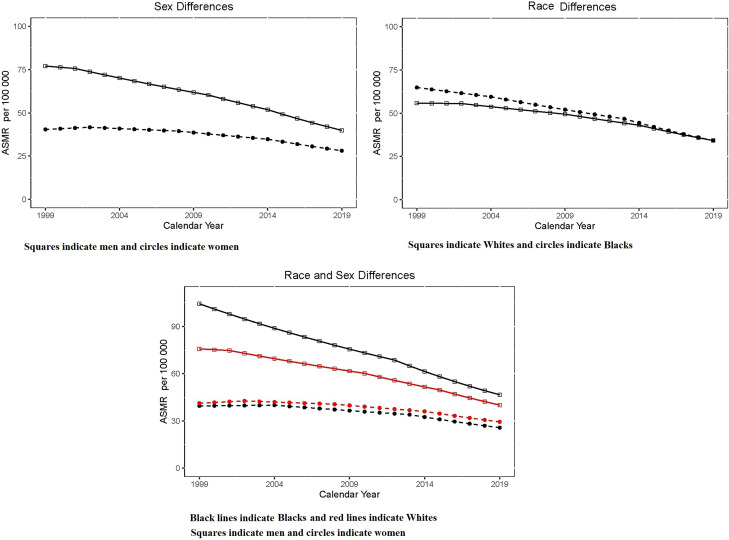
Joinpoint regression demonstrated significant changes in trends over the study period. ASMR for men including both races decreased throughout the study period, whereas women from both races had an initial increase followed by a later decline (Figures 1 and 2 and Table 1), indicating a delay in the peak of ASMR for women. For men, the initial trend seen was between 1999 and 2001 (EAPC, −0.9%), followed by a steeper negative trend between 2001 and 2010 (EAPC, −2.5%), 2010 and 2014 (EAPC, −3.7%), and the last and most noticeable change was seen between 2014 and 2019 (EAPC, −5.1%). At the same time, women had an initial positive trend (EAPC, 1.0% [1999–2002]) followed by declining trends (EAPC, −0.9% [2002–2008] and EAPC, −2.1% [2008–2014]). Like men, the most noticeable change was seen in the fourth trend (2014–2019), with a trend of EAPC −4.2%. At the same time, for racial groups, there was a steady decline for Whites, with the highest decline observed from 2009 to 2014 (EAPC, −4.5%). Similarly, Blacks also observed a similar decline, with the highest decline in the last years of the study between 2013 and 2019 (EAPC, −5.1%). Interestingly, all subgroups showed the highest decline in recent years. White men’s most notable change was between 2015 and 2019 (EAPC, −5.2%). For Black men, the most notable change was between 2012 and 2019 (EAPC, −5.4%). Women from both races had an initial positive trend followed by negative trends (White women, EAPC, +1.1% between 1999 and 2002 and Black women, EAPC, +0.2% between 1999 and 2004). The most notable change for White and Black women was EAPC, −4.0% (2014–2019) and EAPC, −4.5% (2013–2019), respectively.
Figure 1.
Trends in lung cancer mortality stratified by (A) sex (squares indicate men and circles indicate women), (B) race (squares indicate White patients and circles indicate Black patients), and (C) both sex and race (black lines indicate Black individuals and red lines indicate White individuals; squares indicate men and circles indicate women). ASMR = age-standardized mortality rates.
Figure 2.
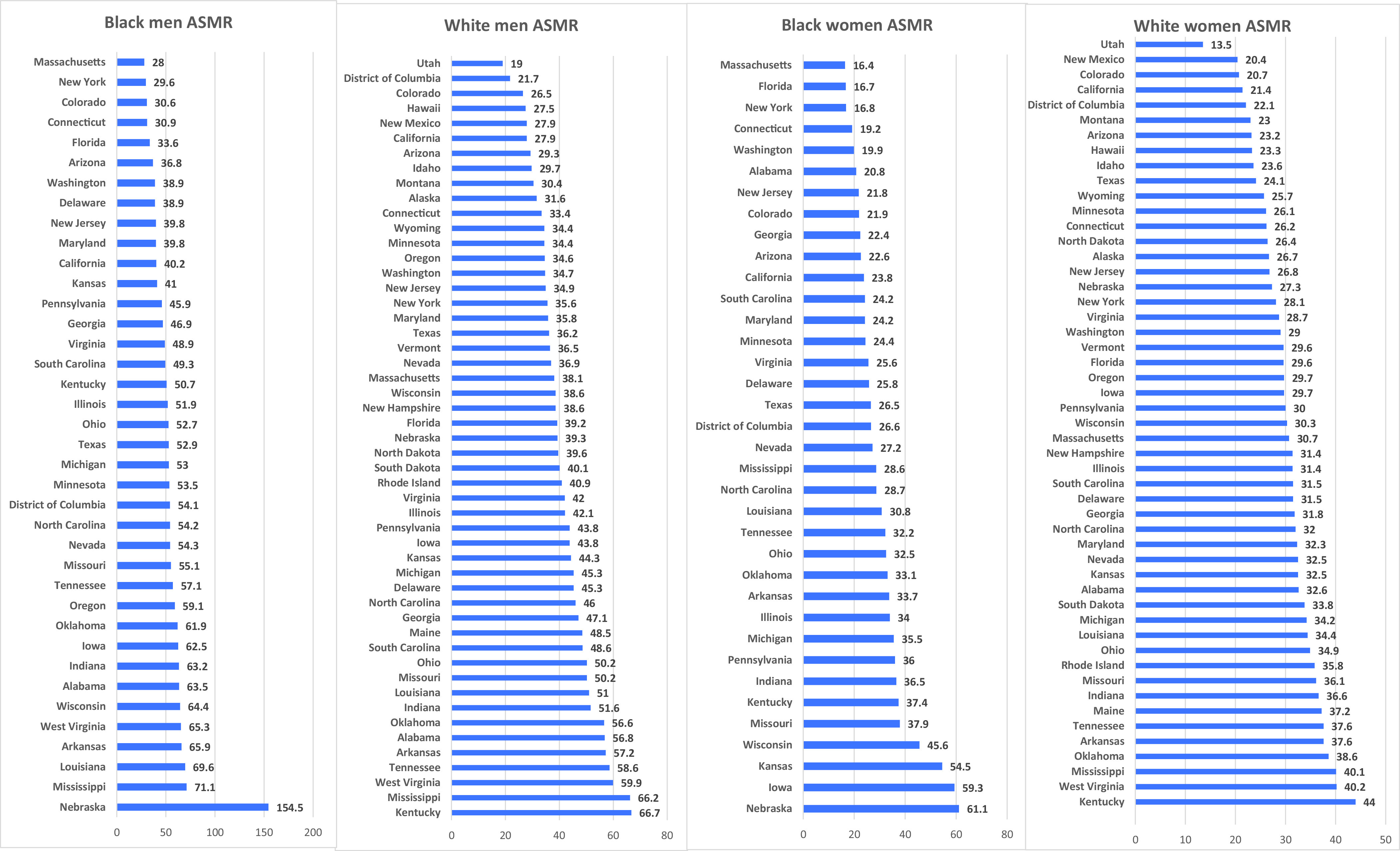
Lung cancer related age-standardized mortality rates (ASMRs) in Black men, White men, Black women, and White women in different states in the United States (2019). All indices are per 100,000 population.
Table 1.
Trends in lung cancer mortality stratified by sex, race, and both sex and race
| Trend 1 |
Trend 2 |
Trend 3 |
Trend 4 |
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Years | EAPC (95% CI) | P Value | Years | EAPC (95% CI) | P Value | Years | EAPC (95% CI) | P Value | Years | EAPC (95% CI) | P Value | |
| Sex | ||||||||||||
| Women | 1999–2002 | 1 (0.1 to 1.9) | 0.026 | 2002–2008 | −0.9 (−1.3 to −0.5) | <0.001 | 2008–2014 | −2.1 (−2.4 to −1.7) | <0.001 | 2014–2019 | −4.2 (−4.5 to −3.8) | <0.001 |
| Men | 1999–2001 | −0.9 (−2.8 to 1) | 0.313 | 2001–2010 | −2.5 (−2.7 to −2.3) | <0.001 | 2010–2014 | −3.7 (−4.6 to −2.8) | <0.001 | 2014–2019 | −5.1 (−5.5 to −4.7) | <0.001 |
| Race | ||||||||||||
| Black | 1999–2004 | −1.7 (−2.2 to −1.2) | <0.001 | 2004–2013 | −2.6 (−2.9 to −2.4) | <0.001 | 2013–2019 | −5.1 (−5.5 to −4.7) | <0.001 | — | — | — |
| White | 1999–2002 | −0.1 (−0.9 to 0.6) | 0.739 | 2002–2009 | −1.7 (−1.9 to −1.4) | <0.001 | 2009–2014 | −2.7 (−3.2 to −2.3) | <0.001 | 2014–2019 | −4.5 (−4.8 to −4.2) | <0.001 |
| Race and sex combined | ||||||||||||
| Black women | 1999–2004 | 0.2 (−0.7 to 1.2) | 0.575 | 2004–2013 | −1.8 (−2.2 to −1.4) | <0.001 | 2013–2019 | −4.5 (−5.2 to −3.9) | <0.001 | — | — | — |
| Black men | 1999–2012 | −3.2 (−3.3 to −3) | <0.001 | 2012–2019 | −5.4 (−5.7 to −5) | <0.001 | — | — | — | — | — | — |
| White women | 1999–2002 | 1.1 (0.2 to 2.1) | 0.027 | 2002–2008 | −0.8 (−1.2 to −0.4) | 0.002 | 2008–2014 | −2 (−2.4 to −1.6) | <0.001 | 2014–2019 | −4 (−4.4 to −3.6) | <0.001 |
| White men | 1999–2001 | −0.7 (−2.5 to 1.1) | 0.416 | 2001–2010 | −2.4 (−2.6 to −2.2) | <0.001 | 2010–2015 | −3.8 (−4.3 to −3.2) | <0.001 | 2015–2019 | −5.2 (−5.8 to −4.7) | <0.001 |
Definition of abbreviations: CI = confidence interval; EAPC = estimated annual percentage change.
All states showed a decrease in ASMR throughout the study period except New York (EAPC, 1.5% [2008–2011]), Missouri (EAPC, 3.2% [2009–2014]), and Indiana (EAPC, 6.9% [2017–2019]) for Black men, and Illinois for White men (EAPC, 0.0% [1999–2001]). For White women, even though ASMR increased initially in many different states (25/51 [49.0%]), there was a decline in all states in recent years. In contrast, only a few states (6/51 [17.1%]) showed an increase in ASMR during the initial years for Black women, with a decline in recent years except for Kansas (34.0% [2017–2019]). Overall, there was a significant variation in state-by-state ASMR for lung cancer (Figure 2), indicating existing disparities within different states.
Compared with White population, we observed that Black population had higher LC mortality rates for 2 decades, which seems to be multifactorial (5). It is found that Black men and women have a twofold likelihood of developing LC between 40 and 54, with a higher smoking-adjusted risk of developing LC (8–10). However, over the past 20 years, there has been a greater proportional decrease in tobacco smoking among the Black population compared with the rest of the United States population (11, 12). It is also observed that Black patients are less likely to undergo standard-of-care interventions, including surgery, systemic therapy, and radiation, compared with White patients (13–16). Interestingly, it has been demonstrated that Black and White patients experience no difference in lung cancer survival after controlling for stage and socioeconomic factors (17, 18). Studies have also shown that Black patients have better survival with the recent incorporation of biomarker-driven therapies and checkpoint inhibitors (15, 19, 20). A recent study by Howlader and colleagues showed that the decrease in mortality was associated with a substantial improvement in survival over time, which corresponded to the timing of approval of targeted therapy. Similar to our study, they saw a sharp decline in recent years, and survival after diagnosis has improved significantly (21). A 2-year survival improvement related to non small cell lung cancer was noted among all races and ethnic groups (21). The above findings can be contributed to our observation of improvement in LC mortality with proportional improvement in Black patients.
During the same period, there has been an increasing awareness of lung cancer screening (LCS) (22–24). A recent study showed that non-Hispanic White people and people living in the highest income and educational areas showed a significant shift to an earlier stage of diagnosis coinciding with the introduction of LCS, highlighting the need for efforts to increase LCS access to non-White patients and in underserved areas (25). Recently, the United States Preventive Services Taskforce guidelines lowered the threshold as the lower pack-year smoking history found among Black individuals with LC resulted in many Black individuals falling behind with the older LCS guidelines (26, 27). There are still concerns that these guidelines might result in many Black individuals falling below the limit of 20 pack-years (28). Future studies like ours showing mortality trends will help us evaluate the effects of the newer guidelines.
Strengths and Limitations
The strengths of this investigation include using annual mortality data collected from national surveillance statistics from the CDC. These data have made it possible to assess racial and sex disparities in population-level trends over an extended observation period, allowing comparisons in trends rather than absolute annual mortality rates. Using longitudinal data has also helped comment on overall trends within individual states after standardization and reporting these differences between state health systems. There were a few limitations of our study. We could not assess the prevalence or incidence of LC. However, previous reports have suggested an accelerating decrease in lung cancer incidence, with the absolute number of new LC cases in 2022 projected to be higher in females than males for the first time in the United States (24). Also, although the risk for mortality can vary on the basis of the stage and grade as well as different pathological subtypes, this data is not available in the CDC WONDER database, and we are unable to further characterize trends on the basis of these factors. Furthermore, ASMR data was available for only 38 and 37 states for Black men and women, respectively. All the missing states had under 6% of Black population, decreasing the chances of bias in national trends (29). Also, as with any observational study, causal statements could not be made.
Conclusions
In the past 20 years, there has been a significant decrease in LC mortality for men and women and White and Black patients. Although there appears to be a decrease in the disparity in LC mortality between sexes and races, significant disparities remain, with Black men having the highest mortality and men consistently having higher mortality than women. Decreasing the disparities in LC screening and smoking rates might have helped reduce the gaps. Future studies are required to evaluate potential causes of racial and sex disparities in LC mortality and help formulate appropriate strategies to eliminate inequalities.
Footnotes
Supported by National Institutes of Health/National Heart, Lung, and Blood Institute (T32HL007633-36; J.D.S.).
Author Contributions: Each of the authors significantly contributed to this manuscript. O.A.O., C.J., J.D.S., C.C.T., and U.T. made significant contributions to the concept and design of this paper. J.D.S., D.C.M., and C.J. were significantly involved in the statistical analysis. O.A.O., C.J., A.A., D.C.M., H.S., P.B., A.W., L.A., A.R., R.G., J.S., J.D.S., and C.C.T. extensively drafted the manuscript. U.T., J.D.S., A.R., C.J., and C.C.T. were involved in the critical revision of the manuscript and contributed important intellectual content. C.J. (corresponding author, guarantor) takes responsibility for the manuscript's content, including the data and analysis.
Author disclosures are available with the text of this letter at www.atsjournals.org.
References
- 1.Centers for Disease Control and Prevention. 2022. https://www.cdc.gov/cancer/lung/statistics/
- 2. Hunt B, Balachandran B. Black:White disparities in lung cancer mortality in the 50 largest cities in the United States. Cancer Epidemiol . 2015;39:908–916. doi: 10.1016/j.canep.2015.10.003. [DOI] [PubMed] [Google Scholar]
- 3. Cook MB, McGlynn KA, Devesa SS, Freedman ND, Anderson WF. Sex disparities in cancer mortality and survival. Cancer Epidemiol Biomarkers Prev . 2011;20:1629–1637. doi: 10.1158/1055-9965.EPI-11-0246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Sagerup CM, Småstuen M, Johannesen TB, Helland Å, Brustugun OT. Sex-specific trends in lung cancer incidence and survival: a population study of 40,118 cases. Thorax . 2011;66:301–307. doi: 10.1136/thx.2010.151621. [DOI] [PubMed] [Google Scholar]
- 5. Gallagher CM, Goovaerts P, Jacquez GM, Hao Y, Jemal A, Meliker JR. Racial disparities in lung cancer mortality in U.S. congressional districts, 1990-2001. Spat Spatio-Temporal Epidemiol . 2009;1:41–47. doi: 10.1016/j.sste.2009.07.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Friede A, Reid JA, Ory HW. CDC WONDER: a comprehensive on-line public health information system of the Centers for Disease Control and Prevention. Am J Public Health . 1993;83:1289–1294. doi: 10.2105/ajph.83.9.1289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Kim HJ, Fay MP, Feuer EJ, Midthune DN. Permutation tests for joinpoint regression with applications to cancer rates. Stat Med . 2000;19:335–351. doi: 10.1002/(sici)1097-0258(20000215)19:3<335::aid-sim336>3.0.co;2-z. [DOI] [PubMed] [Google Scholar]
- 8. Robbins HA, Landy R, Ahluwalia JS. Achieving equity in lung cancer screening for Black individuals requires innovation to move beyond “equal” guidelines. JAMA Oncol . 2022;8:1–2. doi: 10.1001/jamaoncol.2021.7252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Stram DO, Park SL, Haiman CA, Murphy SE, Patel Y, Hecht SS, et al. Racial/ethnic differences in lung cancer incidence in the multiethnic cohort study: an update. J Natl Cancer Inst . 2019;111:811–819. doi: 10.1093/jnci/djy206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Schwartz AG, Swanson GM. Lung carcinoma in African Americans and Whites. A population-based study in metropolitan Detroit, Michigan. Cancer . 1997;79:45–52. doi: 10.1002/(sici)1097-0142(19970101)79:1<45::aid-cncr7>3.0.co;2-l. [DOI] [PubMed] [Google Scholar]
- 11. Jani C, Marshall DC, Singh H, Goodall R, Shalhoub J, Al Omari O, et al. Lung cancer mortality in Europe and the USA between 2000 and 2017: an observational analysis. ERJ Open Res . 2021;7:00311-2021. doi: 10.1183/23120541.00311-2021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Centers for Disease Control and Prevention. 2019. https://www.cdc.gov/media/releases/2019/p1114-smoking-low.html
- 13. Bach PB, Cramer LD, Warren JL, Begg CB. Racial differences in the treatment of early-stage lung cancer. N Engl J Med . 1999;341:1198–1205. doi: 10.1056/NEJM199910143411606. [DOI] [PubMed] [Google Scholar]
- 14. Ryan BM. Lung cancer health disparities. Carcinogenesis . 2018;39:741–751. doi: 10.1093/carcin/bgy047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Tapan U, Furtado VF, Qureshi MM, Everett P, Suzuki K, Mak KS. Racial and other healthcare disparities in patients with extensive-stage SCLC. JTO Clin Res Rep . 2020;2:100109. doi: 10.1016/j.jtocrr.2020.100109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Blom EF, Ten Haaf K, Arenberg DA, de Koning HJ. Disparities in receiving guideline-concordant treatment for lung cancer in the United States. Ann Am Thorac Soc . 2020;17:186–194. doi: 10.1513/AnnalsATS.201901-094OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Hua X, Ward KC, Gillespie TW, Lipscomb J, Goodman M. Non-small cell lung cancer treatment receipt and survival among African-Americans and Whites in a rural area. J Community Health . 2014;39:696–705. doi: 10.1007/s10900-013-9813-7. [DOI] [PubMed] [Google Scholar]
- 18. Aldrich MC, Grogan EL, Munro HM, Signorello LB, Blot WJ. Stage-adjusted lung cancer survival does not differ between low-income Blacks and Whites. J Thorac Oncol . 2013;8:1248–1254. doi: 10.1097/JTO.0b013e3182a406f6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Zhou K, Shi H, Chen R, Cochuyt JJ, Hodge DO, Manochakian R, et al. Association of race, socioeconomic factors, and treatment characteristics with overall survival in patients with limited-stage small cell lung cancer. JAMA Netw Open . 2021;4:e2032276. doi: 10.1001/jamanetworkopen.2020.32276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Gupta A, Zhang D, Braithwaite D, Karanth SD, Tailor TD, Clarke JM, et al. Racial differences in survival among advanced-stage non-small-cell lung cancer patients who received immunotherapy: an analysis of the US National Cancer Database (NCDB) J Immunother . 2022;45:132–137. doi: 10.1097/CJI.0000000000000400. [DOI] [PubMed] [Google Scholar]
- 21. Howlader N, Forjaz G, Mooradian MJ, Meza R, Kong CY, Cronin KA, et al. The effect of advances in lung-cancer treatment on population mortality. N Engl J Med . 2020;383:640–649. doi: 10.1056/NEJMoa1916623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Kowall B, Jöckel KH, Stang A. [Lung cancer screening: current trends] Bundesgesundheitsblatt Gesundheitsforschung Gesundheitsschutz . 2018;61:1551–1558. doi: 10.1007/s00103-018-2834-8. [DOI] [PubMed] [Google Scholar]
- 23. de Koning HJ, van der Aalst CM, de Jong PA, Scholten ET, Nackaerts K, Heuvelmans MA, et al. Reduced lung-cancer mortality with volume CT screening in a randomized trial. N Engl J Med . 2020;382:503–513. doi: 10.1056/NEJMoa1911793. [DOI] [PubMed] [Google Scholar]
- 24.U.S. Preventive Services Task Force. 2021. https://uspreventiveservicestaskforce.org/uspstf/recommendation/lung-cancer-screening
- 25. Potter AL, Rosenstein AL, Kiang MV, Shah SA, Gaissert HA, Chang DC, et al. Association of computed tomography screening with lung cancer stage shift and survival in the United States: quasi-experimental study. BMJ . 2022;376:e069008. doi: 10.1136/bmj-2021-069008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Colson YL, Shepard JO, Lennes IT. New USPSTF guidelines for lung cancer screening: better but not enough. JAMA Surg . 2021;156:513–514. doi: 10.1001/jamasurg.2021.0242. [DOI] [PubMed] [Google Scholar]
- 27. Japuntich SJ, Krieger NH, Salvas AL, Carey MP. Racial disparities in lung cancer screening: an exploratory investigation. J Natl Med Assoc . 2018;110:424–427. doi: 10.1016/j.jnma.2017.09.003. [DOI] [PubMed] [Google Scholar]
- 28. Jones CC, Mercaldo SF, Blume JD, Wenzlaff AS, Schwartz AG, Chen H, et al. Racial disparities in lung cancer survival: the contribution of stage, treatment, and ancestry. J Thorac Oncol . 2018;13:1464–1473. doi: 10.1016/j.jtho.2018.05.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.https://data.census.gov/