PURPOSE:
As the largest integrated health care system in the United States, the Veterans Health Administration (VA) is a leader in telehealth-delivered care. All 10 million Veterans cared for within the VA are eligible for telehealth. The VA cares for approximately 46,000 Veteran patients with newly diagnosed cancer and an estimated 400,000 prevalent cases annually. With nearly 38% of VA health care system users residing in rural areas and only 44% of rural counties having an oncologist, many Veterans lack local access to specialized cancer services.
METHODS:
We describe the VA's National TeleOncology (NTO) Service. NTO was established to provide Veterans with the opportunity for specialized treatment regardless of geographical location. Designed as a hub-and-spoke model, VA oncologists from across the country can provide care to patients at spoke sites. Spoke sites are smaller and rural VA medical centers that are less able to independently provide the full range of services available at larger facilities. In addition to smaller rural spoke sites, NTO also provides subspecialized oncology care to Veterans located in larger VA medical facilities that do not have subspecialties available or that have limited capacity.
RESULTS:
As of fiscal year 2021, 23 clinics are served by or engaged in planning for delivery of NTO and there are 24 physicians providing care through the NTO virtual hub. Most NTO physicians continue to provide patient care in separate traditional in-person clinics. Approximately 4,300 unique Veterans have used NTO services. Approximately half (52%) of Veterans using NTO lived in rural areas. Most of these Veterans had more than one remote visit through NTO.
CONCLUSION:
NTO is a state-of-the-art model that has the potential to revolutionize the way cancer care is delivered, which should improve the experience of Veterans receiving cancer care.
INTRODUCTION
Telehealth, the use of digital technologies to remotely access health services, is ubiquitous. Since the peak of the COVID-19 pandemic, telehealth use has stabilized at levels that are 38 times higher than prepandemic levels.1 As the largest integrated health care system in the United States, the Veterans Health Administration (VA) is a leader in telehealth-delivered care. All 10 million Veterans cared for within the VA are eligible for telehealth-delivered services.
Telehealth use has increased from 10% of Veterans using the VA before the pandemic to 38%, currently, which represents a 390% increase.2 In fiscal year 2021, the last year with complete data, nearly 2.3 million unique Veterans had a telehealth visit.2 The VA has a robust history of sustained telehealth delivery for an array of services, including primary care, women's telehealth, mental health, weight management, stroke care, pathology, critical care unit, and dermatology, among others. This included some aspects of telehealth relevant for patients with cancer, such as a tele–intensive care unit that supported remote chemotherapy infusion.3 Until relatively recently, however, most VA patients sought oncology-related services by means of traditional, in-person office visits. Historically, telehealth for oncology services in the VA health care system was limited for several reasons. First, most VA medical centers (VAMCs) were able to meet oncology service demand using a traditional, in-person model. Second, the VA's national telehealth capabilities have matured in recent years such that establishing a multidisciplinary, national service became feasible.
The VA cares for approximately 46,000 Veteran patients with newly diagnosed cancer each year4 and an estimated 400,000 prevalent cases annually. With nearly 38% of VA health care system users residing in rural areas2 and only 44% of rural counties having an oncologist, many Veterans lack local access to specialized cancer services.5 Consequently, many Veterans have had to resort to a fragmented approach; for the most part, Veterans enrolled in VA health care seek their care from VA medical centers and clinics. However, when timely care is not accessible in the VA health care system (eg, because of long travel times to the VA), the VA purchases care for Veterans in their local community through the MISSION Act or one of their precursors.5 In fiscal year 2021, the estimated cost of hematology and oncology referrals on the basis of paid claims for outpatient care was $1,122,126,023 US dollars.2 Although this is a helpful benefit for many Veterans, it may be less applicable for Veterans in highly rural areas if specialized cancer services may also not be available in their local community. In addition, receiving treatment across multiple health care systems, particularly in patients with chronic disease states, jeopardizes the continuity of care and increases the necessity for ample coordination and communication among providers.6 In an attempt to abate this predicament, the VA's National TeleOncology (NTO) service was established to provide Veterans with the opportunity to seek specialized treatment regardless of their geographical location. Given the integrated nature of the VA, its history as a successful telehealth provider, and the prevalence of cancer among Veterans, the VA health care system is uniquely positioned to be a trailblazer in virtual oncology care.
METHODS
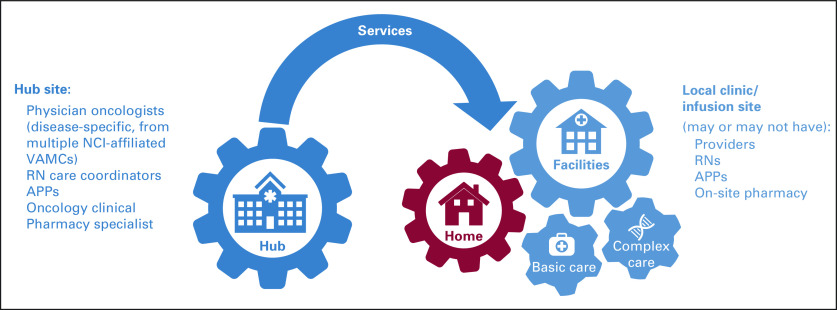
The NTO service was initiated in 2020 with one hub and three initial spoke sites (Fig 1). Designed as a hub-and-spoke model, from the health care system side, VA oncologists from across the country can provide care to patients at spoke sites. No Veterans ever physically travel to a hub site for care because it is a virtual hub. Spoke sites are typically smaller and rural VA medical centers that frequently are less able to independently provide the full range of services that are available at larger facilities.7 In addition to smaller rural spoke sites, NTO also provides subspecialized oncology care to Veterans located in larger VA medical facilities that do not have subspecialties available or that have limited capacity. The NTO hub was established with a physical hub located in Durham, NC, and rapidly evolved into a virtual hub that now includes medical oncologists and hematologists in Ann Arbor; San Francisco; San Diego; Washington, DC; Columbus; Puget Sound; West Haven; Salt Lake City; and Lexington. There are nearly 20 spoke sites served by NTO (Fig 2).
FIG 1.
National TeleOncology Service is a hub-and-spoke model. The services provided by the hub site and potential connection options. Two synchronous connection options are (1) clinical video telehealth (CVT), for Veterans who prefer or require a hybrid of in-person and virtual care (eg, consultation with a remote tele-medical oncologist plus an in-person laboratory draw or physical examination delivered by an in-person APP) or who lack telehealth self-efficacy or reliable internet at home and (2) Veterans Health Administration Video Connect (VVC), when a Veteran may connect directly from their own home or any other location. APP, advanced practice provider; NCI, National Cancer Institute; RN, registered nurse; VAMC, Veterans Affairs Medical Center.
FIG 2.
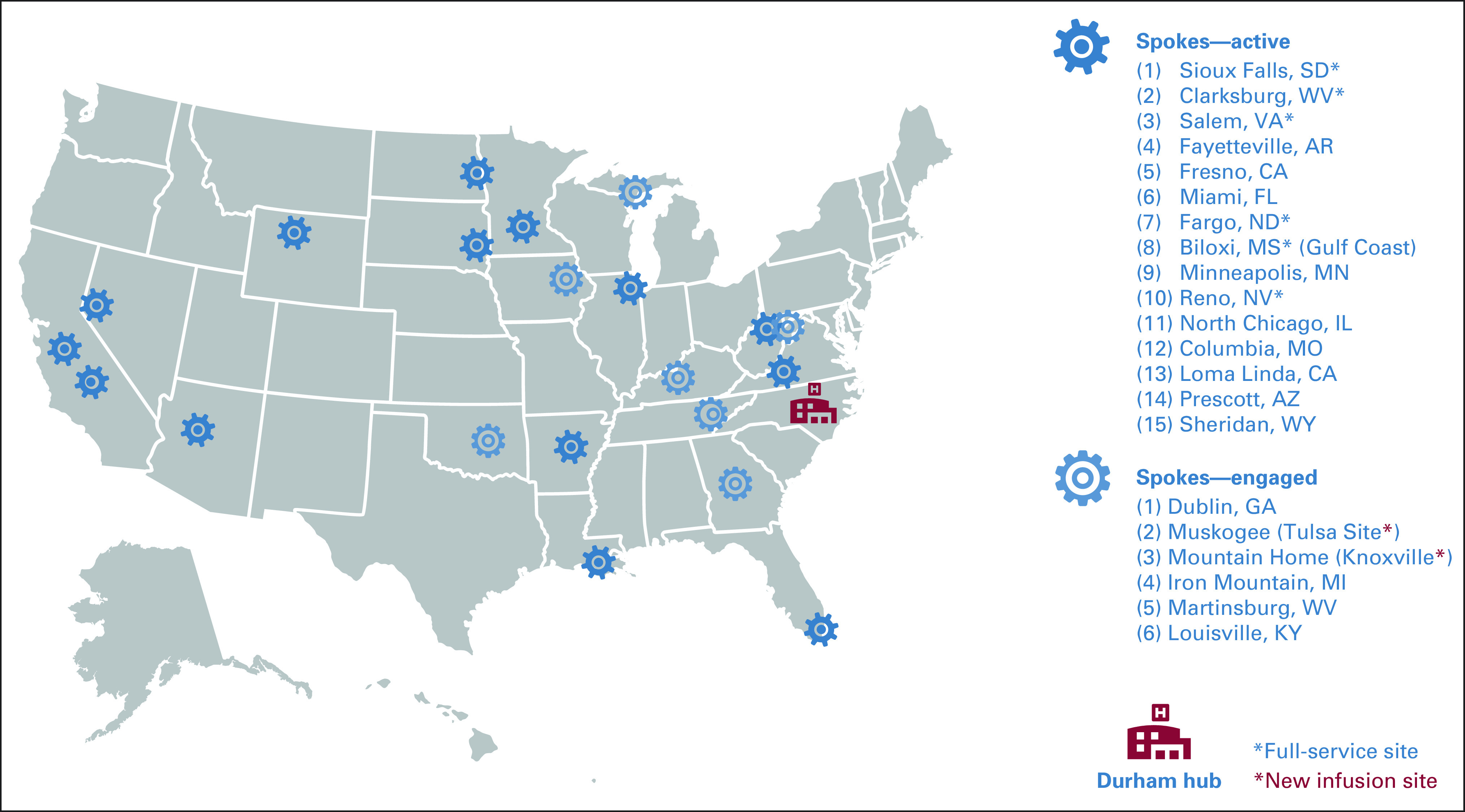
NTO service sites. Active sites are sites at which Veterans received care from NTO. Engaged sites are sites planning for care delivered by NTO. NTO, National TeleOncology service.
When a Veteran is identified as needing services through NTO, a referral is made to the service using an electronic queue. A nonphysician staff member reviews and triages Veterans who are in the queue, allocating the Veteran on the basis of their need in three ways to (1) relevant disease group (eg, genitourinary and malignant hematology), (2) needed level of care (eg, e-consult or appointment), and (3) needed and preferred modality of care delivery (eg, traditional in-person visit, telephone-based visit, clinical video telehealth, or VA Video Connect [VVC]). Veterans newly entering the NTO are typically seen by a remote physician provider. In instances when a Veteran requests in-person care, the Veteran may be seen by an on-site advanced practice provider (APP) who would then consult with a remote physician provider. After this initial appointment, follow-up appointments are scheduled with either an APP or a physician on the basis of both medical indication and the Veteran's preference. It should be noted that the focus of NTO is on medical oncology and hematology services. Therefore, radiation oncology, surgery, and radiopharmaceuticals are not provided through NTO; instead, they are provided either on-site at a VA facility or are purchased by the VA for the Veteran at a care site in the Veteran's local community.
Currently, NTO includes 24 hematology and medical oncology physicians. Physicians in NTO are based primarily at facilities with affiliation with National Cancer Institute–designated cancer centers and subspecialize in all common oncologic disease areas and many uncommon diseases, such as brain tumors, gynecologic malignancies, and sarcoma. Nonclinical staff and nonphysician clinical staff are widely distributed geographically.
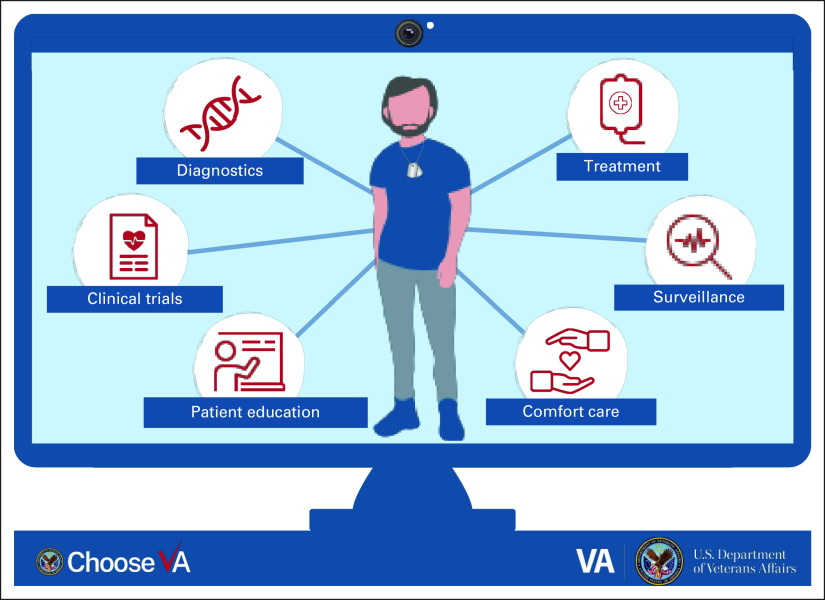
Each spoke site works with NTO leadership to assess the range of services that jointly can be provided for Veterans at that site. The array of services available via teleoncology are not limited to second opinions but span a broad segment of the cancer care continuum typically found in medical oncology practice, including diagnosis, staging and treatment planning in an initial consultation, administration and monitoring of oral and parenteral treatments, follow-up visits with surveillance, and palliative care. Infusion services are a major component of a medical oncology practice. The NTO model of infusional therapies is based on a model used at the Omaha VA Medical Center for more than 15 years and established at the Altoona and Fayetteville Arkansas VA Medical Centers in 2018.8,9 NTO was founded following these models because of their long-standing success within the VA health care system and the feasibility of implementing and scaling the model at other facilities. More specifically, a retrospective review of patients receiving first-line chemotherapy at three VA facilities associated with Omaha has been performed. The sample included patients (n = 108) who received their chemotherapy infusions in Omaha and those who received infusions at the remote sites (n = 43). The patient populations served were comparable regarding demographic and clinical characteristics. There were no significant differences in chemotherapy-related toxicities, missed cycles of treatment, emergency department visits, or hospitalizations.7 On-site staff, including an APP, oncology nurses, a clinical or staff pharmacist, and support staff, execute a treatment plan formulated by or in consultation with a hub-based virtual oncologist.
In 2021, the NTO virtual hub added nonphysician clinical staff including APPs, Clinical Pharmacy Practitioners, and oncology-certified registered nurses, who augment the capacity of the NTO service by providing triage of new consult results, completion of electronic consults, managing patients by telehealth (for APPs), performing medical management and on-treatment video telehealth assessments (for Clinical Pharmacy Practitioners), and conducting care coordination and patient education (for oncology registered nurses; Fig 3).
FIG 3.
Services provided by the National TeleOncology service. VA, Veterans Health Administration.
In addition to receiving traditional, in-person care, Veterans can synchronously access their NTO provider in three ways. Most commonly, Veterans travel to their usual VA facility (referred to as a spoke site) where they have access to that facility's physical infrastructure (eg, internet, video, and nurse to facilitate connection), infusional services, diagnostics, primary care, and other specialists as available. This approach is called clinical video telehealth and may be especially helpful for Veterans who prefer or require a hybrid of in-person and virtual care (eg, consultation with a remote telemedical oncologist plus an in-person laboratory draw or physical examination delivered by an in-person APP) or who lack telehealth self-efficacy or reliable internet at home. Second, Veterans may connect directly from their own home or any other location via VVC. This application-based service can be used on any internet-connected tablet, mobile device, or computer and allows for patients to receive care without the need for any transportation. For Veterans who prefer VVC but lack the resources, the VA has several programs that provide VVC-compatible devices to Veterans, including a national iPad provision program10 and initiatives such as Accessing Telehealth through Local Area Stations,11 which include a partnership with Walmart that provides Veterans with an opportunity to seek treatment closer to their home if there is not a nearby VA facility.12 Finally, Veterans may connect with their health care team over the telephone. Although NTO has adopted these connection modalities, they are available for many VA clinical services (not only oncology services). Thus, many Veterans might have familiarity with some of or all these care delivery modalities, especially Veterans living in rural areas and seeking specialty care.
RESULTS
Since its initiation, NTO has reached a substantial number of Veterans with cancer. As of fiscal year 2021, 23 clinics are served by or engaged in planning for delivery of services by NTO and there are 24 physicians providing care through the NTO virtual hub. Most NTO physicians also continue to provide patient care in separate traditional in-person clinics. In addition, approximately 4,300 unique Veterans have used NTO services. Approximately half (52%) of Veterans using NTO lived in rural areas. Most of these Veterans had more than one remote visit through NTO.2 In fiscal year 2021, the most common reasons for Veterans receiving care in the NTO were because of distance to VA health care (55.5%), because a service was unavailable at the VA nearest to the Veteran (19.1%), or because it was deemed to be in the best medical interest of the Veteran (13.4%). Although the volume of teleoncology care is increasing, less is known about how the quality of teleoncology compares with in-person care. A report from the Ann Arbor VAMC showed that implementing a teleoncology care decreased travel time and costs for Veterans.13
Although NTO predated the COVID-19 pandemic era, the program has enabled delivery of cancer care in novel ways during the pandemic.13,14 Interestingly, evidence collected in a single-site study of Veterans accessing teleoncology care during the pandemic demonstrated that most Veterans were satisfied with their teleoncology-delivered care (83% agree or strongly agree) and approximately half were equally or more satisfied with teleoncology-delivered care compared with traditional in-person oncology visits (47%). Veterans who used teleoncology services also reported a decrease in travel-related expenses, cutting costs by an average of $497 US dollars per patient across a 4-month span.13 One novel aspect of this work is that NTO was operational before the pandemic. All VA sites of care implemented local COVID precautions, such as masking, which necessitated adaptation of NTO's core model to continue operations. The pandemic accelerated NTO expansion, likely because of an increased acceptance of telehealth.
ADDITIONAL ANTICIPATED BENEFITS
Broadly, NTO increases access to care by providing access to expert oncologists/hematologists in areas where these specialists may not be readily available, abating transportation barriers, and decreasing health care costs for patients. The comprehensive program provides resources that can be used throughout the cancer journey, including remote chemotherapy infusions, symptom management, survivorship care, and heightened access to clinical trial enrollment, among others. ASCO recently published guidelines, standards, and recommendations for providing virtual cancer care.15 These standards are largely based on the consensus of an expert panel, and they endorse the American Medical Association's Telehealth Implementation Playbook16 and American Telemedicine Association Quick-Start Guide,17 both of which provide guidance on the implementation of telehealth for organizations. NTO implementation and delivery are consistent with these ASCO standards. The VA has historically provided high-quality, in-person cancer care to its Veterans18,19 and strives to deliver the same level of care virtually. The NTO is conducting an ongoing program evaluation to ensure that the same standards are paralleled throughout the NTO.
DISCUSSION
As the population of Veterans with cancer seeking VA health care grows, especially for Veterans living in rural areas, we anticipate further expansion of NTO. In addition to ensuring that high-quality care is delivered throughout the service, the VA is dedicated to securing health equity for its patients. This is consistent with President Biden's reignition of the Cancer Moonshot, one focus of which is to improve the experience of people and their families living with and surviving cancer.20 The Veterans' Health Administration has been a leader in providing quality cancer care to Veterans across the country and is dedicated to continuing this standard virtually. NTO is a contemporary model that has the potential to revolutionize the way cancer care is delivered, which should improve the experience of Veterans receiving cancer care. Importantly, there is a focus on continuous assurance of equity in access to care. Most services are equally accessible across hub and spoke sites. Hematopoietic stem-cell transplantation and CAR T-cell therapy are notable exceptions, which are only available in three and one VA health care system sites, respectively; however, Veterans also have access through care purchased by the VA in their local communities.
There are early signals that the NTO approach provides services that are feasible and beneficial for both the health care system and patients with cancer by reducing many traditional barriers that lead to a lapse in care (eg, transportation and cost). There may be potential challenges in expanding the program for several reasons. First, it may be challenging for both Veterans and their care teams to transition from a well-known model of in-person care to a less familiar model of remotely delivered care. Despite this barrier, the demand currently exceeds NTO's capacity and hiring staff, particularly those needed for elements of on-site care delivery, is challenging. There are a few related challenges with delivering NTO. For example, having a group of remote oncologists, some of whom cover multiple remote sites, may not lend itself to building strong relationships with on-side staff members; however, with intentional effort, this may be overcome. One approach that NTO has launched is a program called NTOpics to educate and connect primary and specialty care to bolster rapport building. Furthermore, given the scarcity of oncologists, particularly in rural areas, and the shift in the means through which patients receive care after the COVID-19 pandemic, NTO plays an important role in reaching Veterans who might otherwise miss opportunities to access quality cancer care.
ACKNOWLEDGMENT
We thank the Center of Innovation to Accelerate Discovery and Practice Transformation (ADAPT) at the Durham Veterans Affairs Health Care System for their support (CIN 13-410).
Leah L. Zullig
Consulting or Advisory Role: Novartis
Scott E. Sherman
Consulting or Advisory Role: OAR Health
Heather A. King
Research Funding: Merck (Inst)
Michael J. Kelley
Research Funding: Novartis (Inst), AstraZeneca (Inst), Bristol Myers Squibb (Inst), Regeneron (Inst), Genentech (Inst)
Other Relationship: IBM (Inst)
Open Payments Link: https://openpaymentsdata.cms.gov/physician/827136
No other potential conflicts of interest were reported.
DISCLAIMER
The content is solely the responsibility of the authors and does not necessarily reflect the position or policy of Duke University, the US Department of Veterans Affairs, or the US government.
SUPPORT
Supported in part by a grant from the Bristol Myers Squibb Foundation (to M.J.K.). D.B. was supported by the HSR&D Career Development Award (HX002808-01).
AUTHOR CONTRIBUTIONS
Conception and design: Leah L. Zullig, Gina McWhirter, Daniel Becker, Susanne Danus, Vida Passero, Michael J. Kelley
Financial support: Leah L. Zullig, Michael J. Kelley
Administrative support: Leah L. Zullig
Provision of study materials or patients: Michael J. Kelley
Collection and assembly of data: Leah L. Zullig, Gina McWhirter, Daniel Becker, John Pura, Amy S. Jeffreys, Susanne Danus, Vida Passero, Michael J. Kelley
Data analysis and interpretation: Leah L. Zullig, Whitney Raska, Gina McWhirter, Scott E. Sherman, Danil Makarov, Daniel Becker, Heather A. King, John Pura, Vida Passero, Karen M. Goldstein, Michael J. Kelley
Manuscript writing: All authors
Final approval of manuscript: All authors
Accountable for all aspects of the work: All authors
AUTHORS' DISCLOSURES OF POTENTIAL CONFLICTS OF INTEREST
Veterans Health Administration National TeleOncology Service
The following represents disclosure information provided by authors of this manuscript. All relationships are considered compensated unless otherwise noted. Relationships are self-held unless noted. I = Immediate Family Member, Inst = My Institution. Relationships may not relate to the subject matter of this manuscript. For more information about ASCO's conflict of interest policy, please refer to www.asco.org/rwc or ascopubs.org/op/authors/author-center.
Open Payments is a public database containing information reported by companies about payments made to US-licensed physicians (Open Payments).
Leah L. Zullig
Consulting or Advisory Role: Novartis
Scott E. Sherman
Consulting or Advisory Role: OAR Health
Heather A. King
Research Funding: Merck (Inst)
Michael J. Kelley
Research Funding: Novartis (Inst), AstraZeneca (Inst), Bristol Myers Squibb (Inst), Regeneron (Inst), Genentech (Inst)
Other Relationship: IBM (Inst)
Open Payments Link: https://openpaymentsdata.cms.gov/physician/827136
No other potential conflicts of interest were reported.
REFERENCES
- 1.Bestsennyy O, Gilbert G, Harris A, et al. : Telehealth: A Quarter-Trillion-Dollar Post-COVID-19 Reality. Washington DC, McKinsey and Company, 2020 [Google Scholar]
- 2.United States Department of Veterans Affairs, Veterans Health Administration, VHA Support Service Center : Telehealth Workload. Washington DC, Organization's Secure Intranet, 2022 [Google Scholar]
- 3.Arnold A, Asif S, Shostrom V, et al. : Outcomes following off-site remote chemotherapy administration. J Clin Oncol 2022;40 (suppl 16; abstr 1516) [Google Scholar]
- 4.Zullig LL, Sims KJ, McNeil R, et al. : Cancer incidence among patients of the U.S. Veterans Affairs Health Care System: 2010 update. Mil Med 182:e1883-e1891, 2017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Zullig LL, Goldstein KM, Bosworth HB: Changes in the delivery of Veterans Affairs Cancer Care: Ensuring delivery of coordinated, quality cancer care in a time of uncertainty. J Oncol Pract 13:709-711, 2017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Liu CF, Chapko M, Bryson CL, et al. : Use of outpatient care in Veterans Health Administration and Medicare among veterans receiving primary care in community-based and hospital outpatient clinics. Health Serv Res 45:1268-1286, 2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Franchio C: Expanding access to specialty cancer care through TeleOncology. 2021. US Veterans Affairs News. https://news.va.gov/90397/expanding-access-specialty-cancer-care-teleoncology/ [Google Scholar]
- 8.Arnold A, Asif S, Shostrom V, et al. : Outcomes Following Off-Site Remote Chemotherapy Administration, Chicago, IL. Alexandria, VA, American Society of Clinical Oncology, 2022 [Google Scholar]
- 9.Passero VA, Liman AD, Rai H, et al. : Development of a Virtual Cancer Care Network for Distance Oncology Treatment, Chicago, IL. Alexandria, VA, American Society of Clinical Oncology, 2018 [Google Scholar]
- 10.US Department of Veterans Affairs Office of Public and Intergovernmental Affairs : VA expands Veteran access to telehealth with iPad services. 2020. https://www.va.gov/opa/pressrel/pressrelease.cfm?id=5521 [Google Scholar]
- 11.US Department of Veterans Affairs Office of Connected Care : VA and atlas. https://connectedcare.va.gov/partners/atlas
- 12.US Department of Veterans Affars VAntage Point : Walmart open telehealth locations to serve Veterans in rural areas. 2019. https://www.va.gov/opa/pressrel/pressrelease.cfm?id=5374
- 13.Jiang CY, Strohbehn GW, Dedinsky RM, et al. : Teleoncology for veterans: High patient satisfaction coupled with positive financial and environmental impacts. JCO Oncol Pract 17:e1362-e1374, 2021 [DOI] [PubMed] [Google Scholar]
- 14.Jiang CY, El-Kouri NT, Elliot D, et al. : Telehealth for cancer care in veterans: Opportunities and challenges revealed by COVID. JCO Oncol Pract 17:22-29, 2021 [DOI] [PubMed] [Google Scholar]
- 15.Zon RT, Kennedy EB, Adelson K, et al. : Telehealth in oncology: ASCO standards and practice recommendations. JCO Oncol Pract 17:546-564, 2021 [DOI] [PubMed] [Google Scholar]
- 16.American Medical Association : Telehealth implementation Playbook. Digital Health Implementation Playbook Series. 2020. https://www.ama-assn.org/system/files/ama-telehealth-playbook.pdf [Google Scholar]
- 17.American Telemedicine Association : COVID-19 Rapid Response: ATA'S Quick-Start Guide to Telehealth During a Health Crisis https://info.americantelemed.org/covid-19-resources-quickstart-guide-landing
- 18.Jackson GL, Melton LD, Abbott DH, et al. : Quality of nonmetastatic colorectal cancer care in the Department of Veterans Affairs. J Clin Oncol 28:3176-3181, 2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Keating NL, Landrum MB, Lamont EB, et al. : Quality of care for older patients with cancer in the Veterans Health Administration versus the private sector: A cohort study. Ann Intern Med 154:727-736, 2011 [DOI] [PubMed] [Google Scholar]
- 20.National Cancer Institute : Cancer Moonshot℠. https://www.cancer.gov/research/key-initiatives/moonshot-cancer-initiative