Abstract
A case of infective endocarditis involving the vestigial eustachian valve is presented and the available English medical literature is reviewed. Only 5 prior cases have been reported: 4 of those required transesophageal echocardiography for diagnosis, and the other was found at autopsy. This clinical entity is routinely missed on transthoracic echocardiography. Injection drug use is a common predisposing factor, and Staphylococcus aureus is the most commonly identified organism.
This report broadens the differential diagnosis of endovascular infections in injection drug users and highlights the importance of transesophageal echocardiography for diagnosis in selected patients.
Key words: Echocardiography, transesophageal; endocarditis, bacterial/complications/etiology/ultra-sonography; heart valve diseases/etiology; predictive value of tests; staphylococcal infections/etiology/complications; substance abuse, intravenous/complications; tricuspid valve; vena cava, inferior/anatomy & histology
Infective endocarditis is a common complication of injection drug use. The most frequently involved valve is the tricuspid, although the reason for this tendency is not clear. 1 During development of the normal fetal cardiovascular system, there is a structure called the eustachian valve between the inferior vena cava and the right atrium. 2 This valve directs blood flow in the fetal circulation from the vena cava through the foramen ovale into the left atrium. The persistence of this valve in an adult is uncommon. Very rarely, however, this right-sided structure may persist and become infected, causing a clinical syndrome identical to that of tricuspid valve endocarditis. We report what we believe to be only the 6th reported case of infection causing endocarditis of the eustachian valve, and we present a review of the existing English medical literature.
Case Report
The patient was a 36-year-old woman. She was an injection drug user but was HIV negative. She presented in February 2000 with classic symptoms of endocarditis associated with left arm cellulitis. Blood cultures grew methicillin-sensitive Staphylococcus aureus. There was no clinical suggestion of local septic thrombophlebitis. On transthoracic echocardiography (TTE), several vegetations could be seen on the tricuspid valve, along with evidence of severe tricuspid regurgitation. No eustachian valve was seen. During the first 7 days of hospitalization, the patient's condition was complicated by the development of congestive heart failure, respiratory failure requiring mechanical ventilation, hemoptysis of unclear cause, and acute renal failure. Blood cultures were sterilized on day 5 of therapy with high-dose intravenous nafcillin.
Sixteen days later, the patient was in sufficiently stable condition to be extubated and transferred to a chronic care facility for continued antibiotic therapy. Three days later, she developed shortness of breath, peripheral edema, and recurrent hemoptysis, and was transferred back to the acute care setting. Two separate computed tomographic (CT) scans of the chest, obtained 3 days apart, revealed multiple septic emboli to the lungs. Transesophageal echocardiography (TEE) was performed and showed a 6-cm, mobile, echogenic mass attached to the eustachian valve (Fig. 1). Moreover, the tricuspid valve was noted to be nonmobile in the open position with no obvious vegetations attached. The right ventricle was diffusely hypokinetic; the echocardiogram showed no other notable findings.
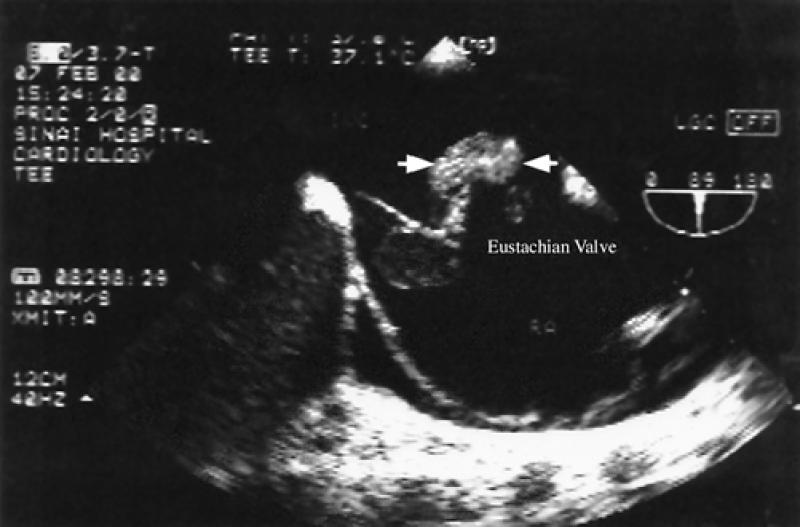
Fig. 1 A transesophageal echocardiographic view of the 6-cm vegetation attached to the eustachian valve (arrows). The tricuspid valve is free of vegetations.
Due to worsening right heart failure that was unresponsive to maximal medical treatment, the patient underwent removal of the eustachian valve and the attached vegetation. She continued to respond poorly and was taken back to surgery 2 days later for replacement of the failing tricuspid valve with a porcine valve. Subsequently, the patient's condition improved, and she was extubated and released from the hospital after a 6-week course of physical rehabilitation. When the patient was last seen in November 2000, she remained free of the use of illegal injection drugs.
Discussion
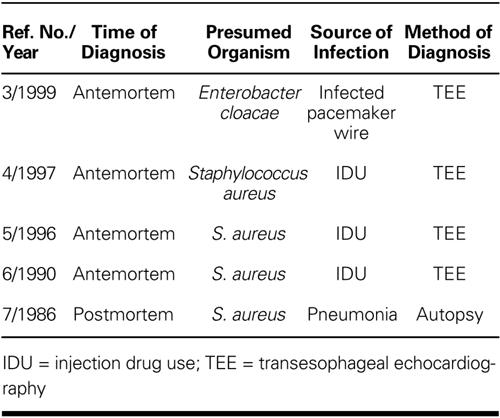
A review of the English literature using Medline from 1966 to the present revealed only 5 cases of eustachian valve endocarditis, 3–7 which are summarized in Table I. In our opinion, this case is important because it broadens the differential diagnosis of the types of right heart infection to be considered in injection drug users. It is of interest, given the large size of the vegetation in this patient (>6 cm), that the initial TTE failed to reveal it, while TEE did. However, the eustachian valve vegetation may have enlarged during the 2 weeks between the performance of the 2 types of echocardiograms, making its presence more readily apparent when TEE was performed. It is also possible that the tricuspid valve vegetations seen on TTE embolized to the lung or that they were evidence of eustachian valve infection but not identified as such. The latter possibility is most likely the case, since the appearance of the septic emboli on the chest CT scans did not change from the 1st echocardiogram to the next. These results suggest that no major septic pulmonary emboli developed during that time.
TABLE I. Previously Reported Cases of Eustachian Valve Endocarditis
After diagnosis, eustachian valve endocarditis is treated in the same way as is tricuspid valve endocarditis, and does not appear to require surgery any more often. The discrepancy between the capabilities of TEE and TTE to detect infection of the eustachian valve occurs in 4 of the 5 reported cases of eustachian valve endocarditis, 3–6 all of which were seen on TEE but missed on TTE. The remaining case was diagnosed at autopsy at a time when TEE was not readily available. 7 This further emphasizes the importance of the use of TEE in the evaluation of difficult-to-manage infections. Moreover, a recent statistical analysis of the cost-effectiveness of TEE showed substantial cost savings with the use of TEE for initial diagnostic imaging in patients with a 4% to 60% prior likelihood of having infective endocarditis. 8
Other indications for the use of TEE in febrile injection drug users include
Clinical endocarditis without an audible cardiac murmur
“Culture-negative” endocarditis
Blood that that cannot be sterilized with pathogen-specific antibiotic therapy
A tricuspid valve that is apparently “frozen” in the open position (as occurred in the case presented)
Antimicrobial management is not altered by the recognition of eustachian valve infection (as it is by a diagnosis of tricuspid valve infection); however, surgical management is different for patients who have eustachian valve infections. Therefore, we recommend that TEE be chosen over TTE for an accurate preoperative diagnosis in selected patients.
Footnotes
Address for reprints: Reprints will not be available.
References
- 1.Frontera JA, Gradon JD. Right-side endocarditis in injection drug users: a review of proposed mechanisms of pathogenesis. Clin Infect Dis 2000;30:374–9. [DOI] [PubMed]
- 2.Limacher MC, Gutgesell HP, Vick GW, Cohen MH, Huhta JH. Echocardiographic anatomy of the eustachian valve. Am J Cardiol 1986;57:363–5. [DOI] [PubMed]
- 3.James PR, Dawson D, Hardman SM. Eustachian valve endocarditis diagnosed by transesophageal echocardiography. Heart 1999;81:91. [DOI] [PMC free article] [PubMed]
- 4.Palakodeti V, Keen WD Jr, Rickman LS, Blanchard DG. Eustachian valve endocarditis: detection with multiplane transesophageal echocardiography. Clin Cardiol 1997;20: 579–80. [DOI] [PMC free article] [PubMed]
- 5.Georgeson R, Liu M, Bansal RC. Transesophageal echocardiographic diagnosis of eustachian valve endocarditis. J Am Soc Echocardiogr 1996;9:206–8. [DOI] [PubMed]
- 6.Vilacosta I, San Roman JA, Roca V. Eustachian valve endocarditis. Br Heart J 1990;64:340–1. [DOI] [PMC free article] [PubMed]
- 7.Edwards AD, Vickers MA, Morgan CJ. Infective endocarditis affecting the eustachian valve. Br Heart J 1986;56:561–2. [DOI] [PMC free article] [PubMed]
- 8.Heidenreich PA, Masoudi FA, Maini B, Chou TM, Foster E, Schiller NB, Owens DK. Echocardiography in patients with suspected endocarditis: a cost-effectiveness analysis. Am J Med 1999;107:198–208. [DOI] [PubMed]


