Abstract
Background:
A large portion of Iranian Working Population (IWP) is becoming at risk of Occupational Noise-Induced Hearing Loss (ONIHL). Several primary studies have evaluated the prevalence of ONIHL in Iran with a variety of prevalence rates. We aimed to estimate the prevalence of ONIHL in the IWP using data from relevant studies.
Methods:
The present study is a meta-analysis and systematic review of previously published studies on ONIHL in Iran. Accordingly, the relevant articles published until Sep 1, 2021 were searched through Pub-Med, Scopus, and Google Scholar, together with Iranian scientific electronic databases. Heterogeneity between among the studies and data analysis was assessed using the I2 test and Random-Effect Model (REM) respectively.
Results:
Having performed a quality assessment, the meta-analysis was performed on the data from twenty-six studies involving a total of 85685 participants. The prevalence of ONIHL was observed to range from 12.9% to 60.5% in the reviewed studies. Moreover, after combining the results from the primary research by the Random Effects Model (REM) approach, the prevalence of ONIHL among IWP was estimated to be 34.69% (95% CI: 29.10, 40.28).
Conclusion:
ONIHL is a significant concern with regard to public and occupational health in Iran. The results also highlighted the urgent need for taking appropriate preventive and control measures in the work-places; particularly by encouraging the employers and health-related policymakers to focus on preventive noise control techniques along with administrative and legislative approaches to mitigate the risk of developing ONIHL.
Keywords: Noise-induced hearing loss, Occupational diseases, Prevalence, Iran
Introduction
Recently, the progress of human societies towards industrialization as well as expanding industrial demands for various new products and resources, has made the exposure to excessive levels of noise particularly in the workplace unavoidable (1). According to the statistics released by the WHO, the daily health related harm caused by the noise exposure was around 4 million dollars (2).
In general, the major impacts of exposure to noise may be categorized into physiological and psychological effects. While more common physiological effects are considered as increased heart and respiratory rates, as well as the rise in blood pressure other general effects such as nausea, vomiting, and dizziness have been reported in the literature as well (3).
In terms of the psychological or mental health effects, industrial workers who are routinely exposed to high levels of occupational noise have reported experiencing symptoms such as headache, controversy, mood swings, and anxiety. Other reported effects include a loss of concentration and inability to concentrate. Thus, noise-induced hearing loss (NIHL) is only one of the many negative consequences that can result from prolonged exposure to louder levels of noise. Other adverse health effects may include disruption of communication and sleep, distraction, and a decline in overall workplace productivity (4, 5). Since NIHL is one of the most frequent types of sensory impairments, it is regarded as a significant public health issue all over the world (4). It is usually defined as a progressive sensorineural hearing loss caused by over-exposure to the noise.
As a subtype of NIHL, occupational noise-induced hearing loss (ONIHL) is a partial or total hearing loss which manifests itself in one or both ears, particularly due to continuous or intermittent noise exposure that often occurs gradually over several years (5–7). Typically, ONIHL is defined by an inner ear injury, is bilateral and symmetrical and affects the perception of upper range of frequencies at 4 kHz before being extended to 3 and 6 kHz.
In developing nations, a considerable proportion of adult hearing loss is attributable to exposure to occupational noise; hence, ONIHL is one of the most prevalent occupational illnesses globally which affects more than 10% of the working population worldwide (5–8).
ONIHL does not directly cause premature mortality, but does result in remarkable disability. Additionally, the impacts of occupational noise exposure inflict a tremendous financial and therapeutic burden on both the person and society as a whole.
According to reports, the annual compensation for the ONIHL in the United States is around 242.4 million dollars (5). Such economic burden on society is not only extremely high but also is rising continuously (9). ONIHL may also hinder interpersonal communication, resulting in increased social stress, low self-esteem, impaired self-identity, and strained interpersonal relationships (5).
Several variables, such as the type and intensity (i.e., the sound pressure level) of the noise in the workplace, the age range and work experience of the exposed workers, the duration of exposure and even workers’ personal habits (e.g., smoking and use of hearing protection equipment) may impact the incidence of occupational ONIHL (10, 11). There are several preventable risk factors for developing ONIHL; hence, its occurrence may be avoided by ensuring prompt diagnosis and treatment. In other words, although ONIHL is regarded as one of the ten most debilitating occupational disorders in the world, it is regarded as potentially preventable. Therefore, early-stage preventative measures along with identifying the type of hearing loss and its underlying causes, can mitigate the socio-economic problems associated with the ONIHL (12, 13).
To the best of knowledge, previous research on the prevalence of ONIHL among IWP has shown inconsistent results as well. For instance, while the prevalence of such hearing loss among heavy vehicle drivers (14), reported to be 14.6% in a study, another study, revealed a prevalence of 60.5% among the workers of automobile manufacturing companies (15). Neghab et al. also identified a 23.21% incidence of ONIHL among employees in the petrochemical industry. (16). The reported different prevalence of ONIHL in primary internal studies shows the diversity and information bombardment in this area, which this matter cannot be used due to wasted resources and dispersion. Accordingly, employers and health-related policy makers have thus found it challenging to implement comprehensive preventative interventions due to the great variance in the available epidemiological data and features of ONIHL prevalence reported in prior research. In light of this, we conducted the present study to systematically review and assess the prevalence of ONIHL among IWP based on the findings of all relevant studies.
Methods
This research was performed based on the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA). It has been registered in the international system of Prospective Register of Systematic Review (PROSPERO) with registration number CRD42021248143. Medical Ethics Committee of Mazandaran University of Medical Sciences (IR.MAZUMS.REC.1400.11883) approved the thesis proposal.
Search Strategy
The current investigation is both a systematic review and a meta-analysis of the papers found in electronic databases such as PubMed, Scopus, and Google Scholar. Persian databases, such as Scientific Information Database (SID), Magiran, IranMedex, Irandoc, Medlib, and all relevant published studies on ONIHL in Iran, were also investigated. Papers with the following keywords and their Persian equivalents were searched without time limitation until 1 Sep 2021:
“Hearing Loss” , “Noise-Induced” , “Acoustic Trauma” , “NIHL” , “Occupational noise-induced hearing loss” , “Occupational Exposure”, “Exposure, Occupational” , “Environmental Exposure” , “Occupational Diseases” , “Occupational exposure limit” , “Noise, Occupational” , “Occupational Noise” , “Noises, Occupational” , “Occupational Noises” , “Noise” , “Occupational Medicine” , “Iran”
Selection of Studies
English and Persian observational studies that have investigated the prevalence of ONIHL among IWP with respect to a history of occupational exposure and also in accordance with occupational health standards in Iran were included in this paper. There were no age or gender restrictions in selecting these studies.
The exclusion criteria were as follows: 1) Studies that have not reported the prevalence of ONIHL in IWP; 2) Review studies and studies with an unknown sample size; 3) Articles from international and local conferences without full-text; 4) Clinical trial studies that did not offer a reliable assessment of the prevalence; 5) Animal, cell, and genetic studies on NIHL in laboratory; 6) Studies related to the diagnosis and clinical treatment of NIHL; 7) Studies of hearing loss that were not related to occupational noise exposure.
No attempt was made to incorporate non-published or in-press research. Additionally, the reference list included in the pertinent papers was investigated as well. In summary, after formulating the relevant questions, the criteria for gathering and selecting literature data were determined based on the aim of the research. Then, the collected literature data were specified and classified. EndNote software was used to screen and extract the relevant literature. Research papers were filtered in three steps. In the first and second steps, irrelevant papers were removed and the titles and abstracts of the remaining papers were examined. In the third step, the full texts of all selected publications were retrieved to determine the relevant articles. The first and second steps were performed by two independent investigators (SE.S and A.SA). A third investigator (S.E) resolved any discrepancy between the other investigators.
Quality Assessment of studies and Data Extraction
The quality of the papers was assessed by two investigators (M.R and SE.S) using the Newcastle Ottawa Scale (NOS) checklist relevant to the cross-sectional studies. Based on this method, each paper could finally receive a total score of 9. In this meta-analysis, a score of 4 or above indicated a high-quality study, whereas a score of 4 or less indicated a low-quality research. Moreover, the agreement between the results from the quality assessment of the papers was reviewed by a third investigator (M.M). Eventually, 26 papers (12 Persian and 14 English) were included in the analysis stage. Information related to the socio-demographic characteristics of these studies such as age, gender, author name, language, type of study, type of industry, sample size, year of publication, work experience, hearing assessment tool, and ONIHL prevalence were extracted. The proportion of the participants detected with ONIHL was considered as the primary outcome.
Statistical Analysis
Stata software (ver. 16) was employed to analyse the obtained data. The heterogeneity index between studies was determined using Cochran (Q) and I-Squared tests. The standard error for the prevalence of ONIHL for each of the initial studies was estimated using a binomial distribution. Also, the prevalence of ONIHL was estimated with 95% confidence interval using methane command and Random Effect Model (REM). Sensitivity analysis was used to evaluate the effect of each study on the overall estimation. Egger test and Funnel plot chart were used to investigate publication bias. The effect of probable variables on the heterogeneity of the ONIHL prevalence was also investigated using Meta-regressions.
Results
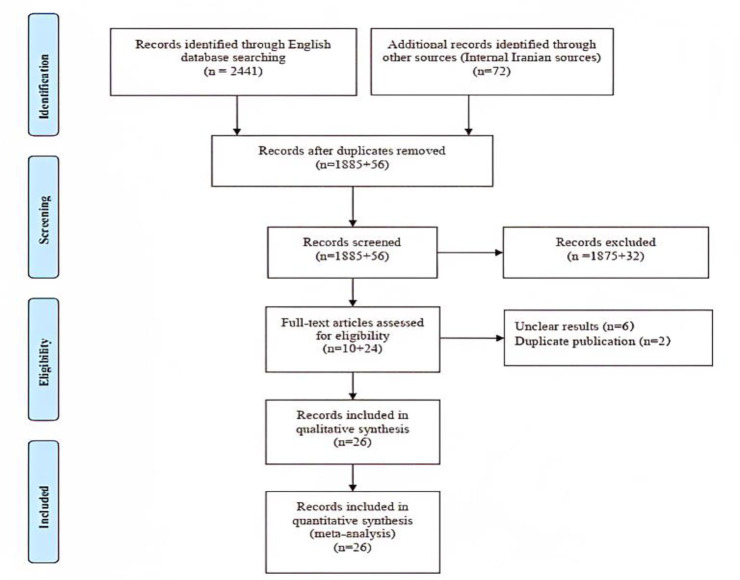
Overall, 2513 papers were retrieved by reviewing international and local electronic databases. After these papers were submitted to the reference management software, 572 duplicate entries were removed. We then screened the rest of 1941 papers, of which 1907 were excluded following the title or abstract evaluation performed based on exclusion criteria. Of 34 remaining papers, 8 papers were also excluded after reviewing the full text. All of the submitted publications were evaluated for quality using the NOS checklist, and all included studies attained the minimum score required for inclusion in this meta-analysis. Finally, 26 papers were systematically reviewed and meta-analysed (Fig. 1).
Fig. 1:
PRISMA flow diagram or the systematic and meta-analysis
In this paper, a summary of the characteristics of included studies is presented in Table 1. Totally, 26 papers met the requirements of the inclusion criteria. Publication dates of these papers ranged from 2004 to 2019 and all qualifying research were cross-sectional as well. Eleven papers were in Persian (17–27) and 15 were in English (14–16, 28–39). In terms of gender, all of the surveyed workers were male. In all of these studies, pure-tone audiometry (PTA) was employed for assessing the ONIHL.
Table 1:
Summary of characteristics of studies included in the systematic review
| Ref | Language | Type of factory | type of study | Sample size | ONIHL (%) | Gender | Age (mean ± SD) | Work experience (mean ± SD) |
|---|---|---|---|---|---|---|---|---|
| (28) | English | Driver | cross-sectional | 2283 | 41.8 | male | 39±10 | 14±9.3 |
| (15) | English | Automobile company | cross-sectional | 478 | 60.5 | male | 33.51±5.35 | - |
| (29) | English | Driver (long-distance) | cross-sectional | 4300 | 18.1 | male | 40.8±11 | 14.7±9.6 |
| (30) | English | Truck drivers | cross-sectional | 500 | 42 | male | 38±12.2 | 9.8±8.6 |
| (31) | English | Wagon manufacturing | cross-sectional | 504 | 39.5 | male | 42.25±6.56 | 18.14±6.5 |
| (14) | English | Heavy vehicle drivers | cross-sectional | 65533 | 14.6 | male | - | - |
| (32) | English | Food-producing factory | cross-sectional | 412 | 41.01 | male | - | - |
| (33) | English | Home appliances factory | cross-sectional | 371 | 55.25 | male | 32.17±4.92 | 6.65±2.74 |
| (34) | English | Tile and Ceramic Industry | cross-sectional | 853 | 17.4 | male | 32.95±7.15 | 5.95±4.62 |
| (35) | English | Drivers | cross-sectional | 1900 | 39.6 | male | 41.5±10.5 | - |
| (17) | Persian | Textile spinning | cross-sectional | 100 | 21 | male | - | - |
| (18) | Persian | Oil industry | cross-sectional | 110 | 49 | male | - | - |
| (19) | Persian | Airport | cross-sectional | 106 | 33 | male | 34.86±8.37 | 10.6±7.44 |
| (36) | English | Professional drivers | cross-sectional | 1901 | 49.65 | male | 41.56±10.57 | - |
| (20) | Persian | Car smoothing workshops | cross-sectional | 50 | 36 | male | 38.7±9.7 | 21.5±9.6 |
| (21) | Persian | Manufacturing industries | cross-sectional | 2004 | 22.5 | male | - | - |
| (37) | English | Fireclay mine | cross-sectional | 220 | 23.63 | male | 38±6.4 | - |
| (38) | English | Derivers | cross-sectional | 1000 | 42.6 | male | 34.02±13.9 | 8.21±7.84 |
| (22) | Persian | Tire manufacturing company | cross-sectional | 914 | 32.7 | male | 38.84±5.18 | 12.37±4.12 |
| (23) | Persian | Textile | cross-sectional | 100 | 23.25 | male | 38.98±10.43 | 13.83±6.1 |
| (39) | English | Automobile industry | cross-sectional | 441 | 49.88 | male | 33.07 | 8.06 |
| (16) | English | Petrochemical industry | cross-sectional | 280 | 23.21 | male | - | - |
| (24) | Persian | Agriculture factory | case-control | 131 | 36.69 | male | - | 19.6±8.4 |
| (25) | Persian | Metal workers | cross-sectional | 743 | 31.31 | male | - | - |
| (26) | Persian | Tile factory | cross-sectional | 342 | 12.9 | male | 37.3±8.1 | 10.6±6.9 |
| (27) | Persian | Small manufacturing industries | cross-sectional | 109 | 46.8 | male | - | - |
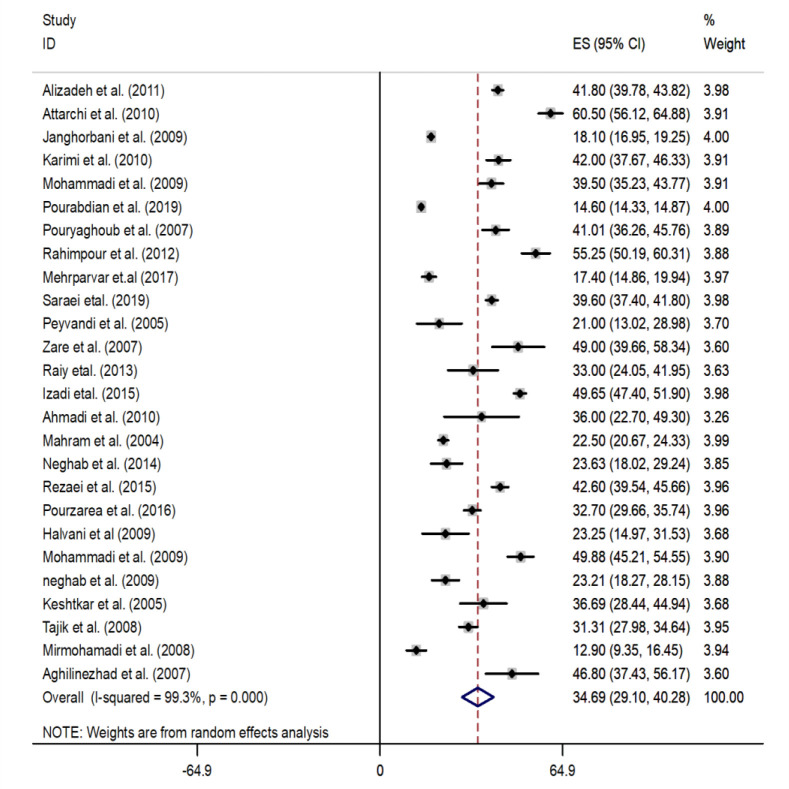
The results from 26 selected studies with 85,685 samples were included in the meta-analysis. The rate of ONIHL prevalence in eligible studies was varied, from 12.9% in the study of Mirmohamadi et al.(26) with a sample size of 342 people to 60.5% in the study of Attarchi et al.(15) with a sample size of 478 people. According to the findings, there was a wide range of variation in the main study findings. (I-squared: 99.3%, Q: 3841.1, P-value <0.001). The results from the eligible studies were combined using REM and the prevalence of ONIHL among IWP was estimated to be 34.69% (95% CI: 29.10, 40.28) (Fig. 2).
Fig. 2:
Forest Plot for estimation of pooled prevalence of ONIHL in Iranian workers
Due to the high heterogeneity among the results, subgroup analysis was performed based on the type of industry. Accordingly, individuals were divided into two groups: the transportation industry and the manufacturing industry. The findings of the subgroup analysis demonstrated that the industry type was also unable to identify the cause of heterogeneity (as supplementary data, the readers can contact authors if needed).
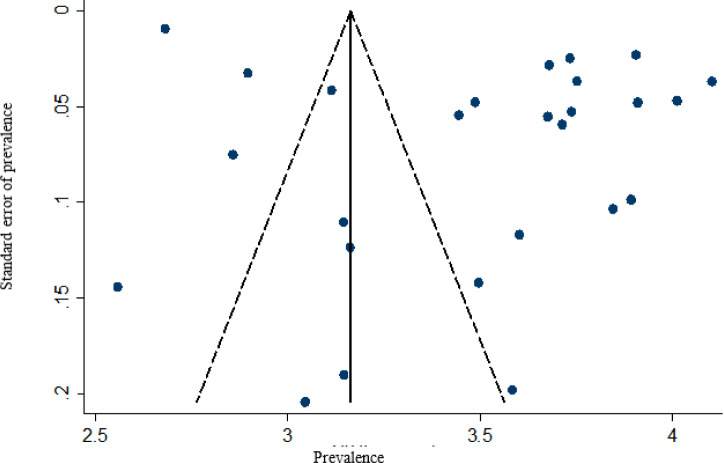
The funnel plot chart shows that there is publication bias in accessing the results of primary studies (Fig. 3). Publication bias was also evaluated by the Egger test which the results of this test also confirmed the existence of publication bias (β = 11.79, P: 0.008). Based on the results of sensitivity analysis, the effect of each primary study on the overall estimation was not different.
Fig. 3:
Funnel plot of ONIHL prevalence for a meta-analysis of eligible studies
The effects of variables such as year of publication (P: 0.859), age (P: 0.363), and work experience (P: 0.750) on the prevalence of ONIHL were investigated using meta-regression, which was not statistically significant.
Discussion
In this research, the previous studies conducted on ONIHL in Iran during 16 years (2004–2019) were reviewed and analysed. Our findings suggest that the majority of Iranian workers, who are suffering from ONIHL, were mainly from manufacturing industries such as automotive, ceramic, textile, steel, etc. These findings are also comparable with those of previous international studies, including those conducted in China and the United States; a high proportion of ONIHL cases occur among workers from conventional manufacturing sectors. According to the findings from the Asian research, the primary causes of noise pollution are the industrial, transportation, mining, and agricultural sectors. (8, 40).
Accordingly, the systematic and meta-analysis study performed on 71,865 workers (aged 33.5±8.7) found that most workers with ONIHL were employed in typical manufacturing industries (41). Our findings are consistent with the findings of other countries. In the United States, approximately 82% of ONIHL cases among workers were from industrial sectors such as construction, manufacturing, mining, agriculture, water and electricity utilities, transportation, etc (42). In this study, the prevalence of ONIHL was 34.69 based on the results of the reviewed studies conducted on IWP.
The frequency and prevalence of ONIHL in Iran was therefore found to be more than other countries, according to this research. In this respect, the total prevalence of ONIHL among Chinese employees was 21.3%; which was less than such prevalence among IWP (41). According to the Centres for Disease Control and Prevention (CDC), over 9 million workers are exposed to an average daily sound intensity of more than 85 dB(A), and about 26 million Americans have NIHL, which affects 15% of the population (43, 44). This high prevalence of ONIHL indicates the widespread distribution of noise in various industries as well as high levels of noise exposure in the workplaces. In Iran, for instance, exposure to high sound pressure levels of 90.29 dB (A) was recorded (45). According to the reviewed studies, exposure to this high level of noise and long-term noise exposure on the job might be regarded risk factors for the high prevalence of ONIHL in Iran (46, 47). In general, occupational noise exposure is likely to increase the incidence of NIHL. In addition, a dose-response association was discovered between NIHL and sound intensity among Danish employees, such that a greater noise level was related with a higher incidence of NIHL (48). The cumulative effects of noise level and exposure time can cause NIHL. Higher levels of noise may cause damage to the outer hair cells (OHCs), while chronic exposure to noise can be harmful to the inner hair cells (IHC), the cochlear supporting cells, spiral ganglion cells, and cochlear vessels (49).
According to the occupational permissible exposure level in Iran, a worker is allowed to be exposed to the noise pressure level of 85 dB for 8 h a day, 44 h a week for 30 years. The purpose of above standard is only to prevent hearing loss. Moreover, there is no standard for the non-auditory effects of chronic exposures to the noise in industrial settings and many IWP are exposed to high-level noise due to working with worn-out industrial equipment and machinery.
Currently, ONIHL is considered as an incurable and irreversible disease, and the best solution to reduce hearing loss is preventive measures to create a safe and healthy workplace in terms of noise exposure. The main purpose of these measures include investigating occupational exposures through periodic monitoring of the noise exposures; minimizing the noise exposure in the workplace via engineering, administrative controls and personal hearing protection equipment (PHPE); as well as early detection of the damage to the inner ear or auditory neural system before the establishment of the irreversible permanent hearing loss (5, 50–53).
For industrial noise, eliminating or reducing the noise levels in the workplace through engineering controls or administrative interventions is the most effective method for prevention of ONIHL. In that regard and according to the results from the available literature, if the noise level is minimized to less than 80 dB, the risk of developing ONIHL can be significantly reduced (13). Although the reduction of noise levels and exposure time through engineering or administrative controls may provide the workers with fairly adequate protection against ONIHL, such strategies are typically difficult to be implemented. In general, when it is impossible to lower the ambient noise levels to the acceptable levels, supplying the employees with the proper type of PHPE along with comprehensive training becomes a crucial alternative protection strategy. (54, 55). Nonetheless, adopting ONIHL control measures at the individual and organizational levels is fairly demanding as well as time-consuming. Control measures for ONIHL require evidence-based assessments that in turn would provide the policymakers with essentially reliable data and background records for implementing ONIHL prevention and control programs (5).
One of the factors that can affect the results as a factor of heterogeneity was the type of occupation that subgroup analysis could not identify the source of heterogeneity between studies. In this study, as it becomes clear, the prevalence of ONIH in workers active in the industry system is higher than in workers active in the transportation system related to differences in the nature of exposure to noise sources. Proposed reasons for this finding are that high levels of noise impede the ability to hear alarm signals, monitor equipment, respond to ambient noises, and coordinate with other workers. Hearing loss among workers who are exposed to noise depends on the industry and the job. In general, the industries that are most at risk for hearing loss are the mining, textile, construction, and wood products sectors (5, 56–58).
Finally, a number of limitations need to be considered. First, the number of primary studies in Iran focusing on Speech-frequency NIHL (SFNIHL) was limited, which led to inadequate evidence in these categories. Due to the absence of occupational prospective research on the noise exposure, assessing the prevalence of ONIHL among Iranian employees was also one of the limitations of this investigation. On the other hand, there was no cohort research among the qualifying studies, and all the primary evidence was cross-sectional; hence the correlation between occupational exposure variables and ONIHL was difficult to determine. The reviewed studies did not adequately address the epidemiological information and were mostly of low quality. Due to the considerable heterogeneity between the primary results, the subgroup analysis could not identify the source of heterogeneity between eligible studies; this can also be another limitation of this paper. The subgroup analysis due to the uniformity of study design, the age range of individuals, and other variables was performed only based on the type of industry, which as previously mentioned, could not identify the origin of the heterogeneity. In general, our findings indicate the need for conducting more accurate primary research in order to attain a more profound understanding about the etiology of ONIHL and its contributing factors.
Conclusion
Based on the previous studies conducted among IWP, the prevalence of ONIHL was estimated to be 34.69%. This high prevalence of ONIHL in Iran is therefore indicative of widespread exposure to excessive noise levels in a variety of industries and workplaces. Under light of the fact that the therapeutic approaches for the treatment of the hearing loss are still in development, the most effective strategy for limiting the occurrence of ONIHL is to establish a noise-free and thus healthy work environment. Our findings not only highlight the need for immediate implementation of preventative and control measures in this context, but also may encourage the employers and health and safety policymakers to focus on taking more appropriate preventive approaches, initiating preliminary noise control and hearing conservation programmes, as well as establishing legislative and regulatory frameworks to minimize the risk of the developing ONIHL.
Journalism Ethics considerations
Ethical issues (Including plagiarism, informed consent, misconduct, data fabrication and/or falsification, double publication and/or submission, redundancy, etc.) have been completely observed by the authors.
Acknowledgements
This study was supported financially by Mazandaran University of Medical Scienses, Iran. Mazandaran University of Medical Sciences supported this work under Grant number 11883.
Footnotes
Conflict of interest
No potential conflict of interest was reported by the author.
References
- 1.Fiedler PEK, Zannin PHT. (2015). Evaluation of noise pollution in urban traffic hubs—Noise maps and measurements. Environ Impact Assess Rev, 51:1–9. [Google Scholar]
- 2.Nelson DI, Nelson RY, Concha-Barrientos M, Fingerhut M. (2005). The global burden of occupational noise-induced hearing loss. Am J Ind Med, 48(6):446–58. [DOI] [PubMed] [Google Scholar]
- 3.EtemadiNezhad S, Taban E, Naghavi Konjin Z, et al. (2022). Investigating the effect of urban traffic noise pollution on university students' cognitive performance: a simulated study. J Mazandaran Uni Med Sci, 31(204):133–45. [Google Scholar]
- 4.Le TN, Straatman LV, Lea J, Westerberg B. (2017). Current insights in noise-induced hearing loss: a literature review of the underlying mechanism, pathophysiology, asymmetry, and management options. J Otolaryngol Head Neck Surg, 46(1):41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Chen K-H, Su S-B, Chen K-T. (2020). An overview of occupational noise-induced hearing loss among workers: epidemiology, pathogenesis, and preventive measures. Environ Health Prev Med, 25(1):65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Leensen M, Van Duivenbooden J, Dreschler W. (2011). A retrospective analysis of noise-induced hearing loss in the dutch construction industry. Int Arch Occup Environ Health, 84(5): 577–590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Śliwińska-Kowalska M. (2020). New trends in the prevention of occupational noise-induced hearing loss. Int J Occup Med Environ Health, 33(6):841–848. [DOI] [PubMed] [Google Scholar]
- 8.Fuente A, Hickson L. (2011). Noise-induced hearing loss in Asia. Int J Audiol, 50 Suppl 1:S3–10. [DOI] [PubMed] [Google Scholar]
- 9.Zhou H, Zhou Y, Zhang H, et al. (2021). Socioeconomic disparity in the global burden of occupational noise-induced hearing loss: an analysis for 2017 and the trend since 1990. Occup Environ Med, 78(2):125–128. [DOI] [PubMed] [Google Scholar]
- 10.Aliabadi M, Farhadian M, Darvishi E. (2015). Prediction of hearing loss among the noise-exposed workers in a steel factory using artificial intelligence approach. Int Arch Occup Environ Health, 88(6):779–787. [DOI] [PubMed] [Google Scholar]
- 11.Li W, Yi G, Chen Z, Wu J, Lu Z, Liang J. (2021). Association of occupational noise exposure, bilateral hearing loss with hypertension among chinese workers. J Hypertens, 39(4):643–650. [DOI] [PubMed] [Google Scholar]
- 12.Sulkowski WJ, Szymczak W, Kowalska S, Sward-Matyja M. (2004). Epidemiology of occupational noise-induced hearing loss (onihl) in poland. Otolaryngol Pol, 58(1):233–6. [PubMed] [Google Scholar]
- 13.Hong O, Kerr MJ, Poling GL, Dhar S. (2013). Understanding and preventing noise-induced hearing loss. Dis Mon, 59(4):110–8. [DOI] [PubMed] [Google Scholar]
- 14.Pourabdian S, Yazdanirad S, Lotfi S, Golshiri P, Mahaki B. (2019). Prevalence hearing loss of truck and bus drivers in a cross-sectional study of 65533 subjects. Environ Health Prev Med, 24(1):78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Attarchi MS, Labbafinejad Y, Mohammadi S. (2009). Contemporary exposure to cigarette smoke and noise of automobile manufacturing company workers. J Public Health, 18(3):245–9. [Google Scholar]
- 16.Neghab M, Madahi M, Rajaeifard A. (2009). Hearing impairment and hypertension associated with long term occupational exposure to noise. Iran Red Crescent Med J, 11(2):160–5. [Google Scholar]
- 17.Peyvandy AA, Mahdavi ME. (2005). Investigation of sound intensity and hearing loss in a textile factory. Iran J Forensic Med, 37(11):7–11. [Google Scholar]
- 18.Zare M, Nasiri P, Shahtaheri S, Golbabaei F, Aghamolaei T. (2007). Noise pollution and hearing loss in one of the oil industries. Hormozgan Med J, 11(2):121–6. [Google Scholar]
- 19.Raiy A, Farzampour S, Mehrparvar A. (2013). Assessment of noise-induced hearing loss in the staff of Yazd Airport, 2010–2011. Ebnesina J, 15(1):1–11. [Google Scholar]
- 20.Ahmadi S, Karboro A, Einanlo M, Aubi ZH, Zarei M. (2011). Occupational noise exposure and hearing loss among car smoothers in qazvin. Iranian J of Health and Environ, 4(1):85–92. [Google Scholar]
- 21.Mahram M, Soghli A, Niknam M. (2004). Survey of Hearing Loss at Workers of Highly Noised Industrial Units, Zanjan. J Zanjan Uni Med Sci, 12(49):44–9. [Google Scholar]
- 22.Pourzarea G, Attarchi M, Valirad F, Mohammadi S. (2016). The effect of simultaneous exposure to organic solvents and noise on high frequency hearing loss in tire manufacturing company workers. Occup Med Quar J, 8(2):72–80. [Google Scholar]
- 23.Halvani GH, Zare M, Barkhordari A. (2008). Noise induced hearing loss among textile workers of Taban factories in Yazd. J Birjand Uni Med Sci, 15(4):69–74. [Google Scholar]
- 24.Keshtkar AA, Kabir MJ. (2005). The relationship between hearing loss and noise exposure among cultivated plants workers. Iranian J Epidemiology, 1(2):59–64. [Google Scholar]
- 25.Tajik R, Ghadami A, Ghamari F. (2009). The effects of noise pollution and hearing of metal workers in Arak. Zahedan J Res Med Sci, 10(4):293–301. [Google Scholar]
- 26.Mirmohammadi S, Baba haji meibodi F, Noorani F. (2007). Assessment of hearing threshold at meibod tile workers. J Yazd Uni Med Sci, 16(1):8–13. [Google Scholar]
- 27.Aghilinezhad M, Ali MI, Mohammadi S, Falahi M. (2007). Assessment of the effect of occupational noise on workers hearing in small scale industries in Tehran. Annals of Military and Health Sciences Research, 5(1):1305–10. [Google Scholar]
- 28.Alizadeh A, Etemadinezhad S, Charati JY, Mohamadiyan M. (2016). Noise-induced hearing loss in bus and truck drivers in mazandaran province, 2011. Int J Occup Saf Ergon, 22(2):193–198. [DOI] [PubMed] [Google Scholar]
- 29.Janghorbani M, Sheykhi A, Pourabdian S. (2009). The prevalence and correlates of hearing loss in drivers in isfahan, iran. Arch Iran Med,12(2):128–34. [PubMed] [Google Scholar]
- 30.Karimi A, Nasiri S, Kazerooni FK, Oliaei M. (2010). Noise induced hearing loss risk assessment in truck drivers. Noise Health,12(46):49–55. [DOI] [PubMed] [Google Scholar]
- 31.Mohammadi S, Mazhari MM, Mehrparvar AH, Attarchi MS. (2010). Cigarette smoking and occupational noise-induced hearing loss. Eur J Public Health, 20(4):452–455. [DOI] [PubMed] [Google Scholar]
- 32.Pouryaghoub G, Mehrdad R, Mohammadi S. (2007). Interaction of smoking and occupational noise exposure on hearing loss: a cross-sectional study. BMC Public Health, 7:137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Rahimpour F, Mirzamohammadi E, Attarchi M, Mohammadi S. (2012). Association between cigarette smoking and occupational noise exposure on hearing loss and hearing impairment. J Babol Uni Med Sci, 14(1):56–63. [Google Scholar]
- 34.Mehrparvar AH, Heidari F, Mostaghaci M, Sharifabadi MS, Zaresakhvidi MJ. (2017). Prevalence and pattern of noise-induced hearing loss in tile and ceramic industry. Int J Occup Hyg, 9(2):60–65. [Google Scholar]
- 35.Saraei M, Izadi N, Eftekhari S. (2019). Investigating the relationship between lipid profile as well as blood groups and noise-induced hearing loss in professional drivers. Int J Occup Hyg, 11(2):91–97. [Google Scholar]
- 36.Izadi N, Sadeghi M, Saraie M. (2015). Survey of noise-induced hearing loss and health in professional drivers. Health Scope, 4(3): e25296. [Google Scholar]
- 37.Neghab M, Karimi H, Tabatabaei SH, Soleimani E, Kasayee NA. (2014). Effects of occupational noise exposure on hearing status, blood lipid and hypertension levels in workers of a fireclay mine. J Health Sci Surv Sys, 2(3):107–12. [Google Scholar]
- 38.Rezaei L, Alipour V. (2015). Prevalence of noise induced hearing loss among vehicle drivers at bandar abbas freight terminal, south of iran. Environ Health Eng Manag, 2(3):135–9. [Google Scholar]
- 39.Mohammadi S, Labbafinejad Y, Attarachi M. (2010). Combined effects of ototoxic solvents and noise on hearing in automobile plant workers in iran. Arh Hig Rada Toksikol, 61(3):267–74. [DOI] [PubMed] [Google Scholar]
- 40.Stucken EZ, Hong RS. (2014). Noise-induced hearing loss: an occupational medicine perspective. Curr Opin Otolaryngol Head Neck Surg, 22(5):388–393. [DOI] [PubMed] [Google Scholar]
- 41.Zhou J, Shi Z, Zhou L, Hu Y, Zhang M. (2020). Occupational noise-induced hearing loss in china: a systematic review and meta-analysis. BMJ Open, 10(9): e039576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Tak S, Davis RR, Calvert GM. (2009). Exposure to hazardous workplace noise and use of hearing protection devices among US workers—nhanes, 1999–2004. Am J Ind Med, 52(5):358–371. [DOI] [PubMed] [Google Scholar]
- 43.Masterson EA, Deddens JA, Themann CL, Bertke S, Calvert GM. (2015). Trends in worker hearing loss by industry sector, 1981–2010. Am J Ind Med, 58(4):392–401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Shargorodsky J, Curhan SG, Curhan GC, Eavey R. (2010). Change in prevalence of hearing loss in US adolescents. JAMA, 304(7):772–778. [DOI] [PubMed] [Google Scholar]
- 45.Soltanzadeh A, Ebrahimi H, Fallahi M, Kamalinia M, Ghassemi S. (2014). Noise induced hearing loss in iran:(1997–2012): systematic review article. Iran J Public Health, 43(12):1605–1615. [PMC free article] [PubMed] [Google Scholar]
- 46.Jabbari K, Nassiri P, Monazzam MR, Faridan M. (2016). The relationship between occupational noise exposure and noise induced hearing loss (nihl) in small-scale industries: a case study in the city of damavand, iran. Biotech Health Sci, 3(4): e40735. [Google Scholar]
- 47.Ketabi D, Barkhordari A. (2010). Noise induced hearing loss among workers of an iranian axial parts factory, 2009. Int J Occup Hyg, 2(2):69–73. [Google Scholar]
- 48.Rubak T, Kock SA, Koefoed-Nielsen B, Bonde JP, Kolstad HA. (2006). The risk of noise-induced hearing loss in the danish workforce. Noise Health, 8(31):80–87. [DOI] [PubMed] [Google Scholar]
- 49.Zhu W, Ding B, Sheng H, Zhu B. (2015). Occupational noise-induced deafuess diaqnosis analysis in Jiangsu from 2006 to 2009. Zhonghua Lao Dong Wei Sheng Zhi Ye Bing Za Zhi, 33(9):671–3. [PubMed] [Google Scholar]
- 50.Leensen MC, Dreschler WA. (2015). Longitudinal changes in hearing threshold levels of noise-exposed construction workers. Int Arch Occup Environ Health, 88(1):45–60. [DOI] [PubMed] [Google Scholar]
- 51.Ebrahimzadeh M, Halvani G, Foroughinasab F, Jafari Nodoushan R. (2011). Evaluation of the hearing state of workers of a uranium mine in central region of iran. Occup Med, 3(3):32–38. [Google Scholar]
- 52.Swanepoel DW, Strauss S, Becker P, Grobler LM, Eloff Z. (2020). Occupational noise and age: a longitudinal study of hearing sensitivity as a function of noise exposure and age in south african gold mine workers. S Afr J Commun Disord, 67(2):e1–e7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Buqammaz M, Gasana J, Alahmad B, Shebl M, Albloushi D. (2021). Occupational noise-induced hearing loss among migrant workers in Kuwait. Int J Environ Res Public Health, 18(10):5295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Campo P, Venet T, Rumeau C, Thomas A, Rieger B. (2011). Impact of noise or styrene exposure on the kinetics of presbycusis. Hear Res, 280(1–2):122–132. [DOI] [PubMed] [Google Scholar]
- 55.Rabinowitz PM, Galusha D, Kirsche SR, Cullen MR. (2011). Effect of daily noise exposure monitoring on annual rates of hearing loss in industrial workers. Occup Environ Med, 68(6):414–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Girard S-A, Leroux T, Courteau M, Picard M, Turcotte F, Richer O. (2015). Occupational noise exposure and noise-induced hearing loss are associated with work-related injuries leading to admission to hospital. Inj Prev, 21(e1):e88–92. [DOI] [PubMed] [Google Scholar]
- 57.Chen J-D, Tsai J-Y. (2003). Hearing loss among workers at an oil refinery in taiwan. Arch Environ Health, 58(1):55–8. [DOI] [PubMed] [Google Scholar]
- 58.Lesage F-X, Jovenin N, Deschamps F, Vincent S. (2009). Noise-induced hearing loss in french police officers. Occup Med (Lond), 59(7):483–6. [DOI] [PubMed] [Google Scholar]