Abstract
Background
Medical Reserve Corps (MRC) in the U.S. provide an approach to organize and incorporate trained public health and medical professionals and supplement the current public health workforce. During the COVID-19 pandemic, MRCs provided immunizations, educated the general public, and assisted with community screening and testing. Reports of MRC activities are publicly available; however, their challenges are not well discussed. Therefore, this exploratory study aimed to identify some challenges that MRC units faced during the COVID-19 pandemic.
Methods
This cross-sectional pilot study aimed to address the composition, recruitment, and training of MRC volunteers and their responses during the pandemic. The survey consisted of 18 close-ended questions across 3 domains: (1) structure and designation of the MRC unit, (2) recruitment and training opportunities for volunteers; (3) demographics; and 2 open-ended questions.
Results
A total of 568 units across 23 states were invited to participate in this exploratory study with only 29 units completing the survey. Out of 29 respondents, 72% were female and 28% male, 45% were nurses, 10% were physicians, and 5% were pharmacists. Retired members were reported in 58% of MRC units, while 62% reported members being active professionals. Qualitative analysis revealed two themes - Obstacles faced by MRC units and Interdisciplinary Composition.
Conclusions
In this exploratory pilot study, we identified the challenges of MRC units during the COVID-19 pandemic. Our findings indicated variation in composition and type of volunteers at different MRC units that may be considered in planning for future disasters and emergencies.
Keywords: COVID-19 pandemic, Medical reserve corps (MRC), Public health, US
1. Introduction
Disasters and Emergencies have the potential to cause substantial losses in terms of human life, health, and the economy. Typically, in the U.S., when there are large-scale disasters – whether natural or human caused – the formal response consists of large deployments of ‘traditional’ first responders such as fire departments, emergency medical services providers, and law enforcement agencies [1]. For instance, following the September 2001 attacks, there were offers of help and support by civilians, many of whom were health and medical professionals [1]. It was apparent at the time that these offers could not be utilized since the identities, credentials, and licenses of these individuals could not be verified, and there was no mechanism to do so in a timely manner [1]. Questions about legal protections for volunteers, compensation or treatment in event of injury were yet to be addressed. As a result, even highly skilled professionals were not utilized in the aftermath of this disaster. Similarly, the anthrax mailings of October 2001, and subsequent mass medication dispensing responses highlighted the need for a system of volunteer medical and public health professionals [1].
The leaders of federal, state, and local response assets were fully engaged in providing prophylactic doses of antibiotics to thousands who may have been exposed to anthrax spores, were overwhelmed, and would be unable to mount an effective response if the proportion of exposed individuals exceeded response capacity [2]. Hence, the need for health worker identification to support the “point of distribution” or POD sites that serve local communities during disasters and emergencies. Subsequently, in response to harnessing civilian support during disasters and emergencies, the Medical Reserve Corps (MRC) was launched as a demonstration project in July 2002. Currently housed in the U.S. Department of Health and Human Services' Office of the Surgeon General, the MRCs mission is to ‘‘engage volunteers to strengthen public health, emergency response and community resiliency”. [2].
The U.S. has a history of volunteerism as evidenced by numerous local, regional, community, and other organizations that have developed naturally. The Medical Reserve Corps (MRC) provides an approach to organize and incorporate trained public health and medical professionals and addresses issues of pre-registration, credentialing, licensing, training, liability, and activation at local levels prior to a disaster or emergency event [3]. Since their creation, MRC units have participated in numerous disaster response efforts including, Hurricane Gustav, Hurricane Ike, Tropical Storm Hanna, 2015 papal visit, among others.
Currently, the MRC network which consists of over 200,000 volunteers across 750+ community-based units, is a significant asset to the U.S. public health and emergency preparedness response [3]. While, there is no national-level mandatory training for MRC members, MRC units are encouraged to use the national core competencies grouped into four Learning Paths: Volunteer Preparedness, Volunteer Response, Volunteer Leadership, and Volunteer Support [4]. The existing literature on MRC suggests that training is focused primarily on natural disasters such as hurricanes, tornadoes, etc. with additional training for biological or chemical warfare such as anthrax through point-of-distribution (POD) simulations [2,5]. Additionally, volunteers are trained on responsiveness protocols. Yet, gaps remain in the literature regarding the actual participation of volunteers and their types (i.e., medical vs. non-medical) before, during, and after emergencies, and the differences by types of emergencies. Few studies have examined volunteers’ willingness to participate during certain emergencies.
Findings by Errett et al. to unearth MRC volunteers' willingness revealed that sensitivity to risk perception may influence volunteers’ willingness to respond [6]. Indeed, as the COVID-19 pandemic has continued to devastate the world, continual messaging and communications may lead to heightened risk perceptions, particularly for volunteers in high-risk areas with lower vaccination rates, thereby potentially reducing willingness and subsequent response. Another consideration is the fact that during emergencies such as the COVID-19 pandemic, healthcare workers may be deployed or work at their own organizations to address higher rates of hospitalizations, prevent infections, etc. Healthcare workers may be exhausted and overworked during emergencies (particularly, frontline workers) and this may lead to reduced participation in MRC activities.
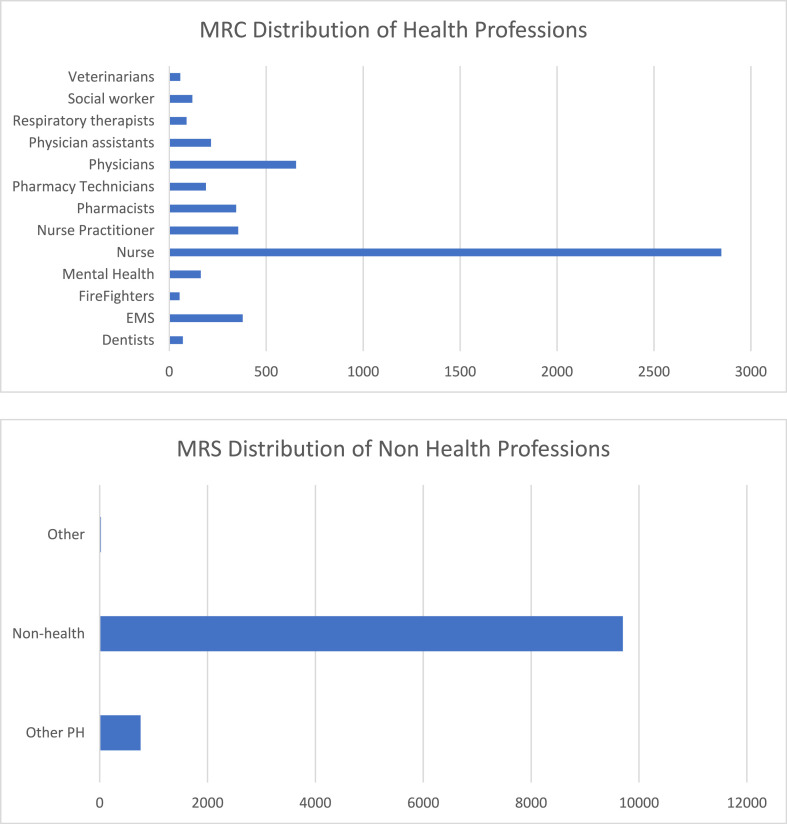
The MRCs allow for non-healthcare professionals to volunteer and provide assistance during emergencies. Their efforts may be typically directed towards administrative activities and there are limitations on medical or healthcare related activities that they may be permitted to carry out. Therefore, a healthy mix of healthcare and non-healthcare workers is important to effectively carry out the responsibilities of a MRC unit, particularly during emergencies and disasters. The National Association of City and County Health Officials (NACCHO) have published reports in 2013, 2015, 2017, and 2020 on MRC profiles [7]. Indeed, the 2020 report shows an increase of volunteers and the majority of volunteers were nurses (∼27%) and non-public health/non-medical (>30%) [7]. During emergencies, it is important to clearly identify the numbers of different types of healthcare professionals needed (doctors, nurses, pharmacists, etc.) depending upon the population size being served and the type of emergency or disaster (i.e., the necessary ratio of providers to population) in order to anticipate and adequately provide clinical services such as immunizations, treatments, testing, screenings, etc. that require professional licensures [8]. While overall numbers of volunteers have increased in the past several years, and also in 2020, these increases have been largely among non-healthcare providers [7]. Even among healthcare providers, the NACCHO report notes that in 2020, of the 444–454 total volunteers, there were 9% EMTs, 3% Mental Health Providers, 3% Nurse Practitioners, 28% Nurses, 2% Pharmacists, 5% Physicians, 2% Veterinarians, 12% Other Medical or Health Professionals. Thus, the professional diversity of a MRC unit throughout an emergency is an important consideration and needs to be explored in detail [8]. Additionally, each MRC is different in its approach to recruitment and retention, and such information is useful to identify best practices in successfully recruiting, training, and retaining volunteer groups over longer periods of time.
In this exploratory pilot study, we aimed to look at the COVID-19 response from the lens of professional diversity and to capture differences across responding MRC units.
2. Methods
Study aims and objectives: This cross-sectional pilot study aimed to identify the composition, recruitment, and training of MRC volunteers and their responses during the COVID-19 pandemic.
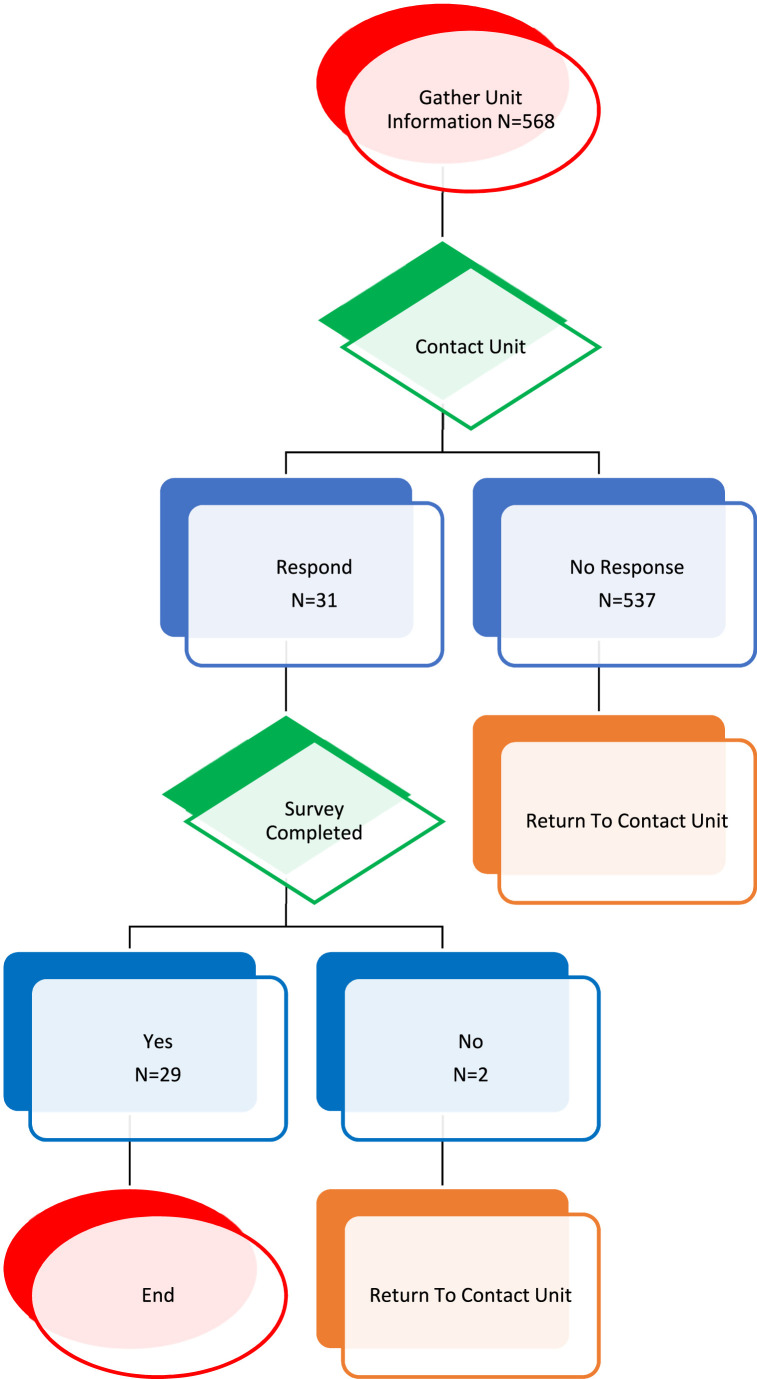
This pilot study used a cross-sectional, exploratory survey to identify the composition, recruitment, and training of MRC volunteers at selected MRC units and their responses during the COVID-19 pandemic. The survey consisted of 18 close-ended questions across 3 domains: (1) structure and designation of the MRC unit, (2) recruitment and training opportunities for volunteers; (3) demographics; and 2 open-ended questions to qualitatively address strengths and challenges that respondent experienced during the current COVID-19 pandemic. This study was approved by the Institutional Review Board (IRB) of the University of Tennessee Health Science Center (UTHSC), (IRB# 20-07594-XM). A survey link was emailed to publicly available email addresses [9]. In the event that the MRC unit did not have a listed email, the study team contacted the unit via phone to request participation in the study. The survey was administered over nine months in 2020–2021, with a monthly reminder. (See Fig. 1 ).
Fig. 1.
Data collection procedure.
All continuous variables were evaluated for normality using the Kolmogorov-Smirnov test, Shapiro-wilk test, and visual inspection of histograms. Variables that met the assumption of normality are presented as mean and standard deviation. Those that violated the assumption of normality are presented as median and interquartile range. Categorical variables are presented as count and proportion of group. All quantitative statistical analysis was conducted with SAS (V. 9.4 [TSM1], SAS Corporation, Cary, NC, USA).
Open-ended responses were imported into Dedoose® (Manhattan Beach, CA), a qualitative analysis software to conduct inductive thematic analysis [10]. The purpose of the inductive analysis was to obtain direct information from the respondents without imposing defined categories or theories [10]. Two researchers (SS and AC) read the comments several times and extracted inductively the main codes. Both researchers (SS, AC) discussed the codes and categories and arbitrated any differences [10]. Main codes were then grouped based on similarities into categories, and resulting themes [10].
3. Results
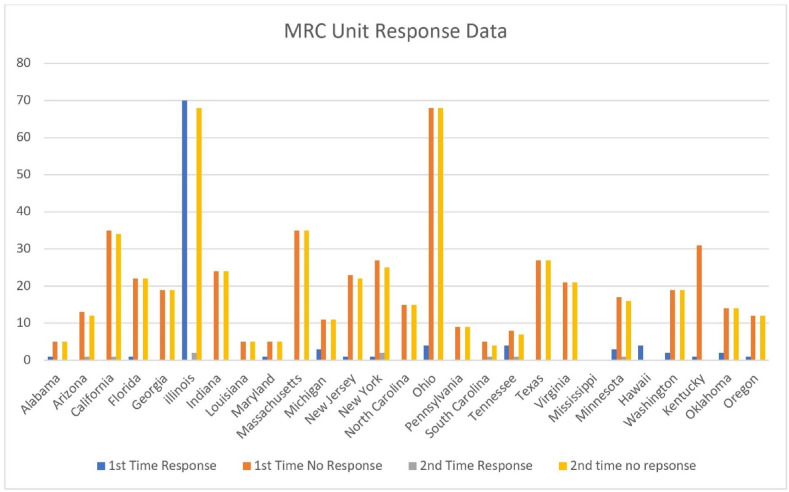
A total of 568 units across 23 states were invited to participate in this exploratory study with only 29 units completing the survey (Table 1 ). Response rates from the various MRCs are shown in Fig. 2 .
Table 1.
Demographic characteristics of respondents.
| Respondents N = 29 | |
|---|---|
| Respondent Position/Role | |
| Non-Healthcare Professional | N = 0 (0%) |
| Nurse | N = 6 (20%) |
| Nurse Practitioner | N = 0 (0%) |
| Other | N = 23 (63%) |
| Other Public Health | N = 0 (0%) |
| Pharmacist | N = 2 (7%) |
| Physician | N = 0 (0%) |
| Physician Assistant | N = 0 (0%) |
| Respiratory Therapist | N = 0 (0%) |
| Social Worker | N = 1 (3%) |
| Veterinarian | N = 0 (0%) |
| MRC Coverage Area | |
| West | N = 9 (31%) |
| South | N = 9 (31%) |
| Midwest | N = 7 (24%) |
| Northeast | N = 4 (14%) |
| Total number of Volunteers | 16,021 |
| Number of Volunteers | Mean 616.19 (SD 911.54) |
| Composition of MRC Volunteer Base | |
| Dentists | N = 70 (0.44%) |
| EMS Professionals | N = 379 (2.38%) |
| Firefighters | N = 53 (0.33%) |
| Mental Health Professionals | N = 163 (1.02%) |
| Nurses | N = 2848 (17.85%) |
| Nurse Practitioners | N = 356 (2.23%) |
| Pharmacist | N = 345 (2.32%) |
| Pharmacy Technicians | N = 189 (1.18%) |
| Physicians | N = 654 (4.1%) |
| Physician Assistants | N = 215 (1.35%) |
| Respiratory Therapists | N = 89 (0.56%) |
| Social Workers | N = 119 (0.75%) |
| Veterinarians | N = 57 (0.36%) |
| Other Public Health/Medical | N = 759 (4.76%) |
| Non-Public Health/Non-Medical | N = 9701 (60.82%) |
| Other | N = 24 (0.15%) |
| Employment Status of MRC Volunteers | |
| Retired | N = 15 (26) (58%) |
| Furloughed | N = 16 (26) (62%) |
| Actively Working | N = 5 (26) (19%) |
| Where does the MRC Recruit | |
| University Student Organizations | N = 10 (35%) |
| Call/Reach Out to All Healthcare Professionals | N = 19 (65%) |
| Call/Reach Out to EMT/Firefighters and Other Emergency Management Personnel | N = 8 (27%) |
| Reach Out to Healthcare and Other Professional Organizations | N = 14 (47%) |
| Email Via List-Serv | N = 10 (34%) |
| Present at Continuing Education | N = 13 (42%) |
| How Often Does the MRC Recruit Volunteers | |
| Ongoing Year-Round Recruitment | N = 25 (86%) |
| Periodic Recruitment | N = 4 (14%) |
| Active License Required to Volunteer | N = 20 (80%) Who say yes |
| Format of Offering Training | |
| In-person Live Instruction | N = 25 (86%) |
| In-person Demonstrations | N = 23 (79%) |
| Online Live Instruction/Presentation | N = 24 (82%) |
| Online Demonstration/Presentation | N = 23 (79%) |
| Hoe Does the MRC Inform Volunteers About Specific Tasks | |
| N = 27 (92%) | |
| Webinar | N = 4 (14%) |
| Website | N (42%) |
| Other | N = 18 (62%) |
| The MRC Specific and/or Assigns a Task Checklist? | N = 15 (52%) Who say yes |
| The MRC Monitors and Evaluates a Volunteers Work | N = 21 (72%) Who say yes |
Fig. 2.
MRC unit response data by state.
3.1. MRC structure
Of the 29 respondents from the 29 MRC units, 72% were female and 28% male. 45% of the respondents were nurses while physicians represented 10% of respondents, and pharmacists 5% of respondents (Fig. 3 ). From the eligible respondents, retired members were reported in 58% of MRC units, while 62% reported members being active professionals. Only 19% of the units reported furlough members. Nurses were well represented compared to physicians, pharmacists, and other health professionals. The smaller units had fewer health professional volunteers comprising mostly of physicians and nurses. Most respondents were not health professionals (22); however, of those respondents that were health professionals, nurses (5) were the prominent responders to the survey, the other two were a pharmacist and a physician, whereas the remaining 22 had a mix of advanced degrees such as MBA, MPH, etc., and administrative titles such as Executive Director.
Fig. 3.
MRC unit distribution by profession.
3.2. MRC recruitment
Per the responses, less than half of the units indicated no outreach to universities for recruitment; however, the same proportion of units (65%) did reach out to healthcare professionals. The majority of units (73%) did not reach out to recruit EMT/Fire Fighters and over half the units (53%) did not reach out to other health organizations. Of the units, only 34% recruited through email and 65% of units indicated they recruited by other means such as word of mouth. Less than half the units (42%) reported being present at continuing education. Year-round recruiting was reported by 88% of units. A professional license was reported to not be a requirement to join by 80% of the units.
3.3. MRC volunteer training
For unit training, in-person live instruction was reported by 88% with in-person live demonstration being 77%. Online live instruction/presentation was reported by 81% with online demonstration being 77% of units. The majority of units inform volunteers through email (92%) while lower percentages were noted for webinar (15%), website (42%), and other (62%). Documented special tasks list were documented by 53% of units while 73% said they had clear evaluations of volunteers’ work. Of the units reporting, submission and/or shared annual reports to the state and/or public was indicated by 69% of units. Both Chi Square and Fisher tests showed that there was no statistical significance.
3.4. Results of qualitative data analysis
3.4.1. Theme 1: Obstacles faced by MRC units
During the COVID-19 pandemic, MRCs response to the challenge of providing vaccinations, staffing call centers, community screening and testing operations, wellness check calls, food distribution, PPE distribution, among other activities [11]. In this study, a common theme emergent from the data analysis was the barrier faced by responding MRC units regarding the decreasing numbers of volunteers in the current pandemic. Respondents emphasized their difficulties in recruiting volunteers to perform tasks, particularly since volunteers such as professional healthcare workers are already engaged during the pandemic and would not be reimbursed. Respondents further stated that volunteers were concerned about potential COVID infections thereby rendering then unwilling to participate in various tasks.
Furthermore, most respondents noted funding as one of the major obstacles faced by MRC.
| “COVID-19 has taken a toll on our ability to do much at the moment. We do not have as many volunteers to help with the services we provide and are not having as much of a community impact as we had hoped for this past year.” |
| “Getting volunteers to respond. Recruiting volunteers ….” |
| “… Keeping them engaged, reliable individuals since work is not compensated.” |
| “Time commitment – limited availability due to working status, and fears –afraid of potential exposures, and disinterest – want to pick and choose when and/or what is the task or need.” |
| “Lack of volunteers, lack of training opportunities ….” |
| “Funding is our major challenge …” |
| “Recruitment, retention, funding, opportunities to source …” |
| “Promotion and advertisement are really the biggest challenge because they don't have any money, just word of mouth.” |
3.4.2. Theme 2: Interdisciplinary Composition
The second theme centered on the importance of an interdisciplinary MRC unit that could provide the appropriate knowledge and support in emergency situations such as the current pandemic. Frequently, respondents emphasized the interdisciplinary structure of the MRC units that adequately equips the team members to face challenges situations and respond to them.
| “The main strength that could be identified is that the small group does include health-care professionals who could provide appropriate care in emergencies.” |
| “Wide variety of volunteer skills and backgrounds, and strong mental health component, and strong relationships within the MRC and with community partners.” |
| “Strong medical background, experience, most members have been loyal …” |
4. Discussion
To our knowledge, this exploratory study was the first to focus exclusively on the role, composition, and training of MRC volunteers during the COVID-19 pandemic. Study results suggested areas of potential improvement, training, and interventions in order to better understand barriers and challenges during emergencies. The study focused on responses across states that were heavily affected by the pandemic, and based on study results, it appeared that robust collaboration between units and their communities would be needed to better address the needs of the communities.
As documented in previous studies regarding the nature of MRC reliance on volunteers, respondents in our study also emphasized the decreasing number of volunteers as one of the main obstacles to function as a unit [12]. In the same vein, due to the limited number of volunteers, the study team reached out to MRC unit in a multitude of ways. For example, our team contacted 568 units; however, approximately 70% of the time, the emails bounced back, and the phone number provided on the website was not functional. Additional efforts are needed to raise awareness among public health professionals and communities to recruit volunteers trained to respond to crises and update the contact information on their respective websites. Furthermore, most units indicated that they required a professional license in order to respond; however professional license was not required at the time of volunteer registration. This presents a logistical challenge that may be addressed by requiring licenses at the time of registration. Moreover, during the COVID-19 pandemic, many states modified licensing requirements and MRC units may need to adapt rapidly to incorporate and communicate modified requirements to their volunteer base.
Challenges to MRC volunteer recruitment and responses during the COVID-19 pandemic have included funding, volunteer willingness, and role specification. Several respondents mentioned that volunteers may perceive heightened risk to themselves or their family members for contracting the SARS Cov-2 virus that may impact their willingness to respond. These findings are consistent with earlier observations of the unwillingness of some health workers to respond to HIV/AIDS in the early 1980s, and to the 2003 SARS epidemic if they perceived risk of exposure to themselves or family members [13].
A novel aspect of MRC units that is not adequately addressed includes their role in building community resiliency, and the challenges thereof resulting from myriad jurisdiction barriers since most of the response is dependent upon the capacity of the federal government to act as a first responding partner in emergencies. Interestingly, an indicator of community disaster resilience lies in the ability of a local community to cope with events without excessively relying on outside resources. This is not always possible, nor facile. In fact, there is no national strategy for building community disaster resilience [14]. A ‘bottom-up’ approach employing public-private collaboration may support existing efforts and experiences in local communities [14]. In its 2006 report “Facing Hazards and Disasters: Understanding Human Dimensions”, the National Research Council linked disaster resilience to the concept of social capital and emphasized the importance of both horizontal integration (within the community) and vertical integration (across different scales) among entities participating in loss-reduction activities [15]. Regarding the importance of strong horizontal ties, this report noted that a community with a high degree of active civic engagement program fosters tightly knit social networks among citizens and local organizations [15].
5. Conclusion
In this study, we identified the challenges of MRC units during the COVID-19 pandemic. Our findings indicated variation in composition and type of volunteers at different MRC units during the peak phases of COVID-19 in 2020–21. Among healthcare professionals at responding MRC units, pharmacists had low participation and their potential during disasters and emergencies as well as during periods of normalcy remains untapped. While MRC units are unique and build upon the volunteer spirit of Americans, more work is needed for their long-term sustainability and viability, including exploring new avenues of partnership such as public-private partnerships, expanding MRC work beyond disaster management and recovery towards social cohesion and resilience building.
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Data availability
Data will be made available on request.
References
- 1.Watson M., Selck F., Rambhia K., Morhard R., Franco C., Toner E. Medical reserve corps volunteers in disasters: a survey of their roles, experiences, and challenges. Biosecur. Bioterrorism Biodefense Strategy, Pract. Sci. 2014;12(2):85–93. doi: 10.1089/bsp.2013.0091. [DOI] [PubMed] [Google Scholar]
- 2.Hoard M.L., Tosatto R.J. Medical reserve corps: strengthening public health and improving preparedness. Disaster Manag. Response. 2005;3(2):48–52. doi: 10.1016/j.dmr.2005.02.002. [DOI] [PubMed] [Google Scholar]
- 3.(MRC) MRC A national network of local groups of volunteers engaging local communities to strengthen public health, reduce vulnerability, build resilience, and improve preparedness, response, and recovery capabilities. 2021. https://mrc.hhs.gov/FindMRC Accessed June 22.
- 4.Sonneman A. 2017. Updated Mrc Core Competencies: Streamlining Training Standards for All Public Health Preparedness Roles. Naccho.https://www.naccho.org/blog/articles/updated-mrc-core-competencies-streamlining-training-standards-for-all-public-health-preparedness-roles Updated. Accessed. [Google Scholar]
- 5.Raja K. The medical reserve corps: volunteers augmenting local public health preparedness and response. J. Publ. Health Manag. Pract. 2019;25(1):95–97. doi: 10.1097/PHH.0000000000000945. [DOI] [PubMed] [Google Scholar]
- 6.Errett N.A., Barnett D.J., Thompson C.B., et al. Assessment of medical reserve corps volunteers' emergency response willingness using a threat-and efficacy-based model. Biosecur. Bioterrorism Biodefense Strategy, Pract. Sci. 2013;11(1):29–40. doi: 10.1089/bsp.2012.0047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.NACCHO. Network Profile of the medical reserve corps. National association of city and county health Officials. Network profile of the medical reserve corps. https://www.naccho.org/programs/public-health-preparedness/medical-reserve-corps/mrc-network-profile Accessed.
- 8.NACCHO. Network Profile of the medical reserve corps. National association of city and county health Officials. Rising to the challenge: mrc answers the call in unprecedented times. https://www.naccho.org/uploads/header-images/public-health-preparedness/NACCHO-Network-Profile-MRC-2020.pdf Accessed.
- 9.Dillman D.A., Smyth J.D., Christian L.M. John Wiley & Sons; 2014. Internet, Phone, Mail, and Mixed-Mode Surveys: the Tailored Design Method. [Google Scholar]
- 10.Hsieh H.-F., Shannon S.E. Three approaches to qualitative content analysis. Qual. Health Res. 2005;15(9):1277–1288. doi: 10.1177/1049732305276687. [DOI] [PubMed] [Google Scholar]
- 11.Assistant Secretary for Preparedness and Response. Department of Health and Human Services. A network created for this moment: How the medical reserve corps has met the challenges of the covid-19 pandemic; 2023. https://aspr.hhs.gov/MRC/Shared%20Documents/MRC-COVID19-Report-12Apr2021-508.pdf Accessed February 19. [Google Scholar]
- 12.Ye J., Stanford S., Gousse T., Tosatto R.J. Developing strong response capacity: training volunteers in the medical reserve corps. Disaster Med. Public Health Prep. 2014;8(6):527–532. doi: 10.1017/dmp.2014.128. [DOI] [PubMed] [Google Scholar]
- 13.Stein B.D., Tanielian T.L., Eisenman D.P., Keyser D.J., Burnam M.A., Pincus H.A. Emotional and behavioral consequences of bioterrorism: planning a public health response. Milbank Q. 2004;82(3):413–455. doi: 10.1111/j.0887-378X.2004.00317.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Council N.R., Committee G.S. National Academies Press; 2011. Building Community Disaster Resilience through Private-Public Collaboration. [Google Scholar]
- 15.Council N.R. National Academies Press; 2006. Facing Hazards and Disasters: Understanding Human Dimensions. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data will be made available on request.