Abstract
Vestibular rehabilitation therapy (VRT) mainly comprises physical therapies that encourage head, eye, and truncal movements, accelerating the recovery of patients with acute peripheral labyrinthine dysfunction. VRT aims to improve vestibular hypofunction by reinforcing vestibulo-ocular, vestibulospinal, and vestibulocollic reflexes. An asymmetry in peripheral vestibular inputs from the pair of membranous labyrinths to the central nervous system frequently results from vestibular lithiasis, causing benign paroxysmal positional vertigo (BPPV). The article discusses the pathophysiology, subtypes, and diagnostic oculomotor patterns generated during positional tests in each subtype of BPPV. Accurate identification of the pathophysiology (canalolithiasis versus cupulolithiasis) as well as the involved semicircular canal (localization and lateralization) is crucial for the unerring VRT of BPPV by physical therapies and/or repositioning maneuvers. The article elaborates the currently known variants of BPPV, the anatomico-physiological correlation between otoconial location and oculomotor patterns generated during the diagnostic positional tests in terms of the direction, latency, and duration of the elicited positional nystagmus [Figures 1 and 2; Table 2]. A detailed description of the treatment of different BPPV subtypes with repositioning maneuvers and/or physical therapy is given [Figures 3-8; Table 3].
Keywords: BPPV, canalolithiasis, cupulolithiasis, semicircular canal, VRT
INTRODUCTION
Many of the commonly occurring peripheral vestibular lesions are known to have a benign etiology, and a self-limiting course due to central compensation, which is accomplished mainly by the cerebellum, vestibular nuclear complex, visual-proprioceptive interactions, and motor efference.[1] The sensory conflicts resulting from peripheral vestibular pathology are repaired by the active neuronal changes in the cerebellum and brainstem.[2] The composite signals thus generated with these structures after a peripheral vestibular loss are used to estimate the body motion and stabilize eye and body movements. Poor compensation and acquisition of maladaptive postural control strategies occasionally occur even in the absence of an ongoing vestibular lesion, highlighting the need for initiating the vestibular rehabilitation at an appropriate time.[1]
Cawthorne and Cooksey were the first to innovate the exercises (that now bear their name) to treat patients with labyrinthine damage resulting from surgery or head injury, and they can be aptly termed as the earliest vestibular rehabilitation therapy (VRT), which have stood the test of time.[3,4] These exercises, which were designed to encourage head, eye, and truncal movements, accelerated the patient's recovery by reinforcing the vestibulo-ocular, vestibulospinal, and vestibulocollic reflexes. The VRT can be categorized into two main types: (1) physical therapy for vestibular hypofunction and (2) physical therapy and canalith repositioning maneuvers for the benign paroxysmal positional vertigo (BPPV). This paper focuses on physical therapy and therapeutic maneuvers for the correction of BPPV.
BPPV is a mechanical disorder of the membranous labyrinth and is the most common cause of vertigo worldwide. It results from vestibular lithiasis, which exists in two forms.
A. Canalolithiasis: It is a condition in which the degenerative otoconial debris gets parted from the utricular matrix and imprudently enters one of the three semicircular canals, namely, posterior, horizontal, and anterior in that order of frequency.[5]
B. Cupulolithiasis: It is the condition where the otoconial debris inappropriately annexes to the cupula, making it heavy and gravity sensitive.[6] Cupulolithiasis occurs in two forms, with the otoconial debris getting attached to either canal (Cup-C) or utricular (Cup-U) side of the cupula.[7]
The major symptom of BPPV is severe rotatory vertigo provoked by changes in the position of the head relative to gravity. Situations during which attacks typically occur include lying recumbent, getting up from supine to sitting, taking lateral recumbent positions, inclining forward (e.g., to pick up an object from the floor), and tilting the head up (e.g., keeping an object on the top shelf). The attendant autonomic symptoms like nausea, vomiting, and diaphoresis are more common in the horizontal semicircular canal benign paroxysmal positional vertigo (HSC-BPPV).[8] The head motion normally moves endolymph in the pertinent semicircular canal, bending the cupula to produce the nerve impulse in the vestibular nerve: the latter apprizes the brain (via the vestibulo-ocular reflex) in which plane and at what angle the head has moved. Brain reflexively generates corrective eye movements equal in angle but in the opposite direction so that the point of fixation invariably falls on the fovea centralis. If otoconial particles inappropriately go into any of the semicircular canals, they continue to drag endolymph for a few seconds (maximum 30 s in canalolithiasis[9] and longer in cupulolithiasis[10]) even after the head movement has stopped, thus causing a sudden severe asymmetry in the resting vestibular tone and a paroxysm of short-lived severe vertigo. By a similar mechanism, the sudden severe asymmetry of the resting vestibular tone results from a cupula, the adhering mass of the otoconial debris on which has rendered it abnormally heavy and gravity-sensitive, resulting in positionally triggered vertigo.
Table 1 shows the relative frequency of all patients diagnosed with BPPV at any specialty clinic.[11,12,13,14,15,16,17,18,19,20,21] Owing to its distinct anatomy, which assists the sequestered degenerative otoconial debris to gravitate into the canal, the posterior semicircular canal BPPV (PSC-BPPV) is the most preponderant subtype. The relatively higher disposition of the anterior semicircular canal (ASC) within the bony labyrinth restrains the upward movement of the otoconial debris as well as enables self-clearance of any debris through its non-ampullary arm, which inadvertently enters it. For these reasons, the anterior semicircular canal BPPV (ASC-BPPV) is the least prevalent variant of the disorder.[21] In the upright position, the horizontal semicircular canal (HSC) inclines 30-degrees posteriorly relative to the horizontal plane, its cupular barrier is at a relatively rostral location, and it becomes vertical in the supine position. On that account, any free-floating debris' that enters the HSC leaves the canal through the utricular exit in its non-ampullary long posterior arm during lateral recumbent positions. The spontaneous remission of HSC-BPPV reported in a few studies is possibly responsible for its modest frequency.[15,22]
Table 1.
Relative frequencies of the different BPPV subtypes presenting to a specialty clinic
| Authors | No. of patients | PSC-BPPV | HSC-BPPV | ASC-BPPV | Multiple canals |
|---|---|---|---|---|---|
| De la Meilleure et al.,[11] 1996 | 287 | 78.05 percent | 16.38 percent | - | 5.57 percent |
| Honrubia et al.,[12] 1999 | 292 | 85.62 percent | 5.14 percent | 1.37 percent | 7.87 percent |
| Macias et al.,[13] 2000 | 259 | 93.02 percent | 1.94 percent | - | 5.04 percent |
| Korres et al.,[21] 2002 | 122 | 90.16 percent | 8.2 percent | 1.64 percent | - |
| Sakaida et al.,[14] 2003 | 50 | 56 percent | 38 percent | 6 percent | |
| Imai et al.,[15] 2005 | 108 | 64.82 percent | 33.33 percent | - | 1.85 percent |
| Nakayama & Epley JM.,[16] 2005 | 833 | 66.39 percent | 10.08 percent | 2.28 percent | 21.25 percent |
| Cakir et al.,[17] 2006 | 169 | 85.21 percent | 11.83 percent | 1.18 percent | 1.78 percent |
| Moon et al.,[18] 2006 | 1692 | 60.9 percent | 31.9 percent | 2.2 percent | 5.0 percent |
| Jackson et al.,[19] 2007 | 260 | 66.9 percent | 11.9 percent | 21.2 percent | - |
| Chung et al.,[20] 2009 | 589 | 61.8 percent | 35.3 percent | 2.9 percent | - |
PSC-BPPV – Posterior semicircular canal benign paroxysmal positional vertigo HSC-BPPV – Horizontal semicircular canal benign paroxysmal positional vertigo ASC-BPPV – Anterior semicircular canal benign paroxysmal positional vertigo
Classification of BPPV
BPPV can be classified as under –
Monocanalicular
-
Posterior semicircular canal BPPV (PSC-BPPV)
-
Geotropic variant (geo-PSC-BPPV)
- Otoconia free-floating in the ampullary arm in the juxtacupular location.
- Otoconia adherent to the cupula (heavy cupula).
- Apogeotropic (apo-PSC-BPPV) – due to free-floating otoconia in the non-ampullary arm.
-
-
Horizontal semicircular canal BPPV (HSC-BPPV)
- Geotropic variant (geo-HSC-BPPV) – due to free-floating otoconia in the long non-ampullary posterior arm (long posterior arm horizontal semicircular canalolithiasis).
-
Apogeotropic variant (apo-HSC-BPPV)
- Free-floating otoconia in the short ampullary anterior arm of the HSC (short anterior arm horizontal semicircular canalolithiasis).
-
Cupulolithiasis (heavy cupula)
- Otoconial debris adherent to canal side of cupula (Cup-C variant).
- Otoconial debris adherent to utricular side of cupula (Cup-U variant).
Anterior semicircular canal BPPV (ASC-BPPV) – ASC-BPPV is due to canalolithiasis, as per the consensus statement of the committee for the classification of vestibular disorders of the Bárány Society.[23] The otoconial debris in the ampullary arm of ASC results in positional downbeating nystagmus during the provocative positional tests. The cupulolithiasis of the ASC and the non-ampullary arm ASC canalolithiasis are not convincingly known to exist.
Multicanalicular
Single-canal bilateral involving the same semicircular canal in either of the labyrinths.
Multicanal unilateral involving at least two different semicircular canals (posterior, lateral, or anterior) in one of the labyrinths.
Multicanal bilateral involving two or more different semicircular canals in both labyrinths.
Diagnosis
The clinical features of the BPPV are summed up in the introduction section of the article and it is impossible to localize and lateralize the involved semicircular canal solitarily based on symptoms. Two additional salient considerations about BPPV symptoms are
Vertigo in the HSC-BPPV appears during the lateral movements of the patient's head in the supine position and is uncommon during extension or flexion of the neck.[8]
A striking sense of continuous dizziness, rather than rotatory vertigo, still amplifying with the changes in the position of the head relative to gravity but, overall, continuous is the hallmark of apo-PSC-BPPV.[24]
The experiments of Julius Ewald (1855–1921) in pigeons framed the three laws that bear his name, and these are essential for understanding the pathophysiology of the diagnostic positional tests, namely, Dix-Hallpike test (DHT), supine roll test (SRT), and straight head-hanging test (SHHT) which produce the diagnostic oculomotor patterns for localizing and lateralizing the semicircular canals affected by the vestibular lithiasis.[25] Ewald (1892) cannulated each of the three semicircular canals and applied negative and positive pressures to observe the intensity and direction of the generated nystagmus. The two main investigative findings of Ewald's experiments are:
The generated nystagmus is always directed parallel to the plane of the stimulated canal (Ewald's first law).
The generated nystagmus is stronger when the endolymph moves toward the ampulla (ampullopetal) in the case of the HSC (Ewald's second law), and away from the ampulla (ampullofugal) in case of vertical semicircular canals (PSC and ASC) (Ewald's third law). With this knowledge framework of the physiology of semicircular canals, the positional tests are discussed below.
Dix-Hallpike test (DHT)[26]
The positional nystagmus generated during DHT is invariably directed parallel to the plane of the stimulated canal as per the Ewald's first law. Lowering the 45-degrees inclined head in the yaw plane to a 20-degree head-hanging position during the Dix-Hallpike positioning aligns the PSC with the sagittal plane and places its ampullary end to the rostral most position. As a result, there is an ampullofugal shift of the otoconial debris in the ampullary arm of the PSC, leading to an excitatory cupular deflection (Ewald's third law) and this generates the oculomotor patterns characterized by an upbeating ipsitorsional positional nystagmus. For carrying out DHT, position the patient in long-sitting on the examination table, such that the distance between his bottoms and the head end of the examination table allows his head to hang during the test. Hold the patient's head with both hands and incline 45-degrees to one side (e.g., left) in the yaw plane. After that, position him supine such that his 45-degree left inclined head extends 20-degree on the support of the therapist's hands representing the left Dix-Hallpike position [Figure 1]. Maintain the left Dix-Hallpike positioning for at least 60 s or until the elicited nystagmus lasts. A similar sequence of positioning is done in the right head-hanging position if it elicits no nystagmus on the initially tested side. Deciphering DHT results as under –
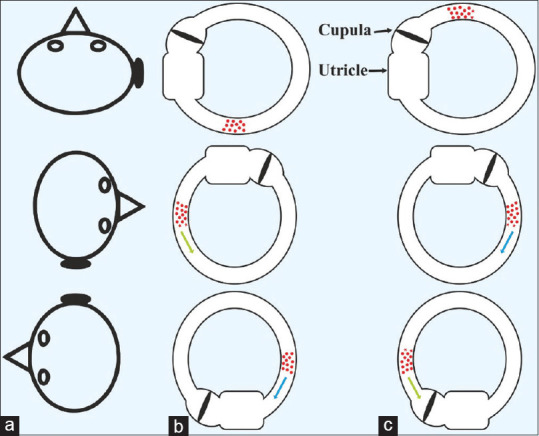
Figure 1.
Dix-Hallpike test (DHT) involves moving the patient from a long-sitting position on the examination table with the head turned 45-degrees to one side (left in the figure) to the 20-degree below horizontal head-hanging supine position. An upbeating or downbeating nystagmus with a torsional component indicates PSC-BPPV and ASC-BPPV, respectively. The direction of torsion is toward the involved side
An upbeating ipsitorsional positional nystagmus suggests the most prevalent geotropic subtype of the PSC-BPPV (geo-PSC-BPPV). The lateralization is to the side toward which the torsional component of the elicited upbeating positional nystagmus is directed in the 20-degrees head-hanging position during the DHT. https://youtu.be/MBsbJeYRF7s
A downbeating torsional nystagmus suggests either ASC-BPPV or the apo-PSC-BPPV. The direction of the torsional component, which is often too small or inconspicuous, suggests lateralization of the ASC-BPPV. DHT in the ASC-BPPV evokes positional downbeating nystagmus in the head-hanging position to either side and in the deep or enhanced straight head-hanging positions. The positional downbeating nystagmus of apo-PSC-BPPV is not typically crescendo-decrescendo, often lasts longer, and is contratorsional. Nonetheless, initially, not infrequently it is almost impossible to differentiate between an ASC-BPPV and apo-PSC-BPPV based on findings of the DHT alone. https://youtu.be/Ubwsqx9J75c.
Supine roll test (Head Yaw Test or Pagnini-McClure Maneuver)[26]
Place a pillow of about 4-inch thickness at the head end of the examination table and position the patient in long-sitting. In succession, position the patient supine flexing the head 30-degrees as the occiput lands on the pillow. Roll the patient's head laterally from neutral to one side while the patient is supine. After waiting for any nystagmus or vertigo to subside, perform the test on the opposite side [Figure 2]. The positive test elicits horizontal positional nystagmus, which may be –
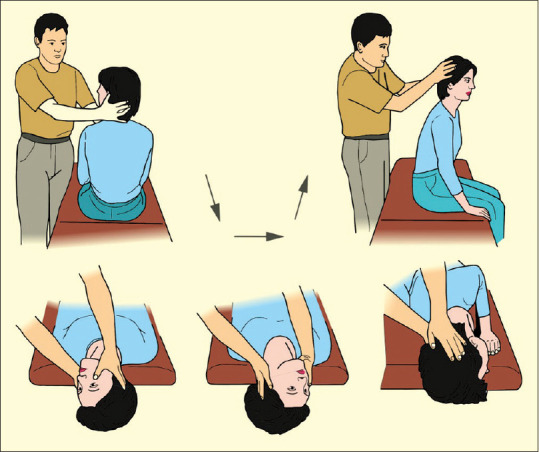
Figure 2.
Supine roll test: From long-sitting on the examination table, shift the patient supine with the head landing on 4-inch-thick pillow and anteflexing it 30-degrees. In the horizontal canal BPPV, lateral head roll to either side elicits geotropic (in long posterior arm canalolithiasis) or apogeotropic (in short anterior arm canalolithiasis and cupulolithiasis) horizontal positional nystagmus
Geotropic: which connotes that the quick component of the nystagmus is directed toward the lowermost ear. The geotropic positional nystagmus is elicited on the lateral head roll to either side and is attributed to the long posterior non-ampullary arm horizontal semicircular canalolithiasis. The side to which the lateral head roll elicits stronger geotropic nystagmus is the affected side as per the Ewald's second law. https://youtu.be/-gp7Dol6_jk
Apogeotropic: be interpreted as meaning that the quick component of the nystagmus is directed away from the lowermost ear. The apogeotropic positional nystagmus is elicited on the lateral head roll to either side and is attributed to the short anterior ampullary arm horizontal semicircular canalolithiasis or cupulolithiasis. The side to which the lateral head roll elicits the weaker apogeotropic nystagmus is the affected side as per the Ewald's second law. https://youtu.be/t_Ie7LGcCXQ
The geotropic variant of HSC-BPPV (geo-HSC-BPPV), has the otoconial debris free-floating in the long posterior non-ampullary arm of the HSC, and an ipsilesional lateral head roll in the yaw-axis, during SRT, produces an excitatory hydrodynamic drag of the endolymph toward the ampulla. This very reason in the variant, during SRT, elicits stronger geotropic nystagmus to the side of the lesion than to the opposite side [Figure 3a and b] (https://youtu.be/-gp7Dol6_jk). In the apogeotropic variant of HSC-BPPV (apo-HSC-BPPV), in which the otoconial debris is either free-floating in the short anterior ampullary arm of the HSC or is adherent to the cupula, thus making it heavier, the excitatory hydrodynamic drag of the endolymph toward the ampulla occurs when there is contralesional lateral head roll in the yaw axis during SRT. For this reason, in the apo-HSC-BPPV during the SRT, stronger apogeotropic nystagmus is elicited when the head is yawed to the contralesional side [Figure 3a and c] (https://youtu.be/v6vmGAJaRDs).
Figure 3.
Ewald's second law: Ampullopetal cupular deflection eliciting a stronger positional nystagmus on ipsilateral head roll (compared to contralateral head roll) in the right long posterior arm horizontal semicircular canalolithiasis (geotropic variant; column B and 2nd and 3rd rows); and for the same reason, a contralateral head roll does so in cupulolithiasis and the right short anterior arm horizontal semicircular canalolithiasis (apogeotropic variant; column C and 3rd and 2nd rows)
The duration of the positional nystagmus is up to 1 min in the canalolithiasis and more than 1 min in the cupulolithiasis. The HSC-BPPV caused by short anterior ampullary arm canalolithiasis presents with apogeotropic positional nystagmus that may last longer than 1 min. However, if the SRT elicits persistent apogeotropic positional nystagmus lasting > 1 min and there are no changes in the direction of nystagmus even after repetitive head roll tests, it is explicable by the horizontal canal cupulolithiasis either on canal-side (Cup-C) or on the utricular-side (Cup-U)[23] https://youtu.be/glT9HtAwaFc
Straight head-hanging test[27]
To conduct the SHHT, position the patient in long-sitting on the examination table such that the distance of the patient's bottom from the head end of the table allows the head to hang during supine positioning. Hold the patient's head firmly and position supine neutral with the head 30-degrees or maximally extended (beyond the short edge of the examination table). Hold the patient in the enhanced straight head-hanging position until positional nystagmus appears and lasts, or at least 60 s, if it does not elicit positional nystagmus. Instruct the patient to keep eyes open, even when experiencing vertigo in the head-hanging position to observe the pattern of induced positional nystagmus. A straight head-hanging test is positive if elicits a downbeating nystagmus with or without a torsional component. https://youtu.be/Ubwsqx9J75c.
Table 2 summarizes the currently known variants of BPPV, the anatomico-physiological correlation between otoconial location and oculomotor patterns generated by the diagnostic positional tests in terms of the direction, latency, and duration of the elicited positional nystagmus. Column 7 of Table 2 shows the YouTube links to access the videos of the oculomotor patterns of the generated nystagmi during the positional tests in different variants of BPPV. Because the management of BPPV solitarily depends on the repositioning maneuvers and/or physical therapy, it is imperative to localize as well as lateralize the involved semicircular canal by meticulous execution of the provocative positional tests and observing the patterns of the elicited positional nystagmus thereon.
Table 2.
Synopsis of otoconial location, diagnostic positional test, elicited nystagmus characteristics, and YouTube links in different BPPV subtypes
| BPPV variant | Otoconial location in upright position | Positional test | Nystagmus direction | Nystagmus latency | Nystagmus duration | YouTube link |
|---|---|---|---|---|---|---|
| geo-PSC-BPPV | Juxta-cupular in the ampullary arm of PSC | DHT | Upbeating and ipsitorsional | Brief latency (rarely up to 40 s) | <1 min | https://youtu.be/MBsbJeYRF7s |
| apo-PSC-BPPV | Non-ampullary arm of PSC near common crus | DHT and SHHT | Downbeating and contratorsional | No latency | >2 min | https://youtu.be/Ubwsqx9J75c |
| PSC-BPPV cupulolithiasis | Adherent to cupula of PSC | Half-DHT* | Upbeating and ipsitorsional | Brief or no latency | >1 min | - |
| ASC-BPPV | Juxta-cupular in ampullary arm of ASC | DHT and SHHT | Downbeating and ipsitorsional; torsion often too little or absent | Brief or no latency (rarely up to 30 s) | <1 min | https://youtu.be/_f87fHMFuVI |
| Long posterior-arm HSC-canalolithiasis | Long posterior-arm of HSC | SRT | Horizontal geotropic | Brief or no latency | <1 min (rarely up to 2 min) | https://youtube/-gp7Dol6_jk. |
| Short anterior arm HSC-canalolithiasis | Short anterior arm of HSC | SRT | Horizontal apogeotropic | Brief or no latency | <1 min | https://youtu.be/v6vmGAJaRDs |
| HSC cupulolithiasis | Adherent to cupula of HSC (Cup-C or Cup-U) | SRT | Horizontal apogeotropic | Brief or no latency | >1 min | https://youtu.be/glT9HtAwaFc |
* The patient’s head is turned 45° toward the side to be tested: the patient is then inclined 60° backwards to one side, instead of 110° so that the cupula of PSC is earth horizontal. Rolling the head 180° to the other side (release position) should reveal a less intense nystagmus beating in the opposite direction, due to ampullopetal deflection of the cupula. Abbreviations: PSC-BPPV – Posterior semicircular canal benign paroxysmal positional vertigo; HSC-BPPV – Horizontal semicircular canal benign paroxysmal positional vertigo; ASC-BPPV – Anterior semicircular canal benign paroxysmal positional vertigo; geo – Geotropic; apo – Apogeotropic; Cup-C – Cupulolithiasis canal side; Cup-U – Cupulolithiasis utricular side; DHT – Dix-Hallpike test; SHHT – Straight head-hanging test; SRT – Supine roll test
Management
The treatment of BPPV with drugs is neither indicated nor successful. In selected patients who develop severe nausea and/or vomiting during repositioning maneuvers and/or physical therapy, oral promethazine is given. Once there is accurate lateralization of the side and localization of the involved canal, it is treated with an appropriate repositioning maneuver and/or physical therapy. Generally, canalolithiasis is more yielding to treatment with repositioning maneuvers compared to cupulolithiasis. It is essential to review the patient at short intervals at least twice, at 1 h, and 24 h after the repositioning maneuver and/or physical therapy. Improvement is assessed in terms of elimination of the positional nystagmus and the associated vertigo. The treatment of different BPPV variants with repositioning maneuvers and/or physical therapy is summarized in Table 3. Figures 4 to 8 are schematic representations of the different maneuvers used to treat the common variants of BPPV. Column 4 of Table 3 shows YouTube links to access videos of therapeutic repositioning maneuvers and/or physical therapy. After the repositioning maneuver, otoconial debris occasionally refluxes into a canal different from the one originally affected. This phenomenon is known as canal-switch and occurs in 6–8% of patients.[28,29,30] The appearance of a different oculomotor pattern on a verifying positional test than the one initially observed, after the patient has been subjected to a seemingly successful repositioning maneuver, is a harbinger of canal-switch. Patients undergoing canal-switch require treatment according to the protocol of the canal involved with the switch phenomenon. The appearance of persistent spontaneous nystagmus following a repositioning maneuver in HSC-BPPV may result from jamming of the otoconia within a canal or between the cupula and the adjacent ampulla wall. Canal jam results in partial or complete obstruction within the canal, resulting in spontaneous nystagmus that persists irrespective of a change in head position.[31] Physicians involved in the physical treatment of patients with BPPV should be aware of these two potential complications of physical therapy, namely the canal-switch and canal jam.
Table 3.
Synopsis of BPPV variants, otoconial location, therapeutic repositioning maneuvers and/or physical therapy, and YouTube links
| BPPV variant | Otoconial location in upright position | Therapeutic repositioning maneuver and/or physical therapy | YouTube link |
|---|---|---|---|
| geo-PSC-BPPV | Juxta-cupular in the ampullary arm of PSC | Epley maneuver[26] [Figure 4] | https://youtu.be/JSwRvT453M8 |
| apo-PSC-BPPV | Non-ampullary arm of PSC near common crus | Demi Semont maneuver[24] | https://youtu.be/cPOmsx68nfl |
| PSC-BPPV cupulolithiasis | Adherent to cupula of PSC | Epley maneuver[26] [Figure 4] (more sessions required compared to geo-PSC-BPPV[32]) | https://youtu.be/JSwRvT453M8 |
| ASC-BPPV | Juxta-cupular in ampullary arm of ASC | Yacovino maneuver[33] [Figure 8] | https://youtu.be/frQ98anQTtk |
| Long posterior-arm HSC-canalolithiasis |
Long non-ampullary posterior-arm of HSC | Gufoni maneuver[34] [Figure 6], Lempert’s 360-degrees Barbecue Roll maneuver[35,36] [Figure 5], forced prolonged positioning (FPP[37,38]) |
https://youtu.be/u_WNOpsxG30 (Gufoni Maneuver) https://youtu.be/ZEG-rKEYnZw (Lempert’s 360-degrees Barbecue Roll Maneuver) |
| Short anterior arm HSC-canalolithiasis |
Short ampullary anterior-arm of HSC | Appiani maneuver[39] [Figure 7] | https://youtu.be/EUW4GVhlPdl |
| HSC cupulolithiasis | Adherent to cupula of HSC (Cup-C or Cup-U) | Head-shaking maneuver (HSM),[40] Cupulolith repositioning maneuver[41] | https://youtu.be/pOK0OFAqtul (HSM) |
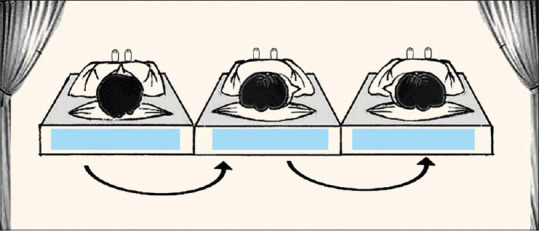
Figure 4.
Epley maneuver (for left PSC-BPPV): From long-sitting on the examination table, with the head rotated 45-degrees to left, the patient is positioned to 20-degree head-hanging position for a minute. After this, two sequent positionings each of a minute duration are carried out inclining the head 90-degrees to right and the right lateral recumbent with nose down towards the horizon. Thereafter the patient is uprighted to short-sitting position
Figure 8.
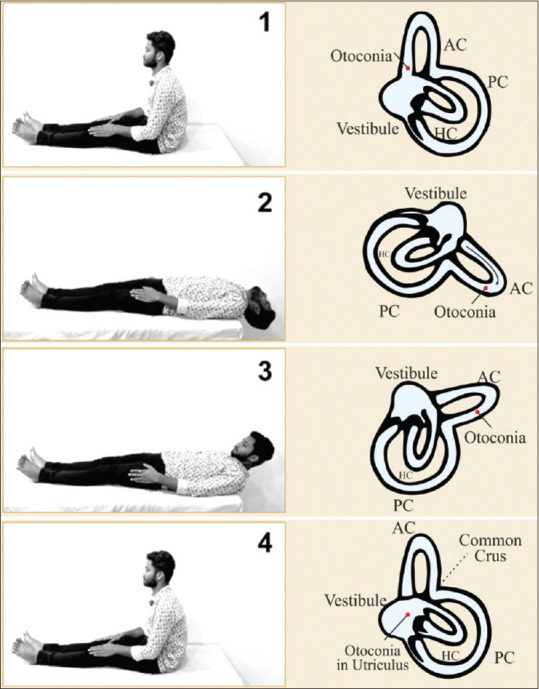
Yakovino maneuver: comprises four sequent steps of each 30 seconds duration of shifting patient from long-sitting on the examination table (1) to more than 30-degree head-hanging position; (2) flexing the head 30-degrees or more relative to horizon chin-to-chest position; and (3) finally uprighting to long-sitting position (4)
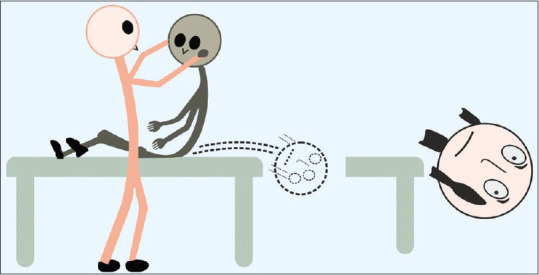
Figure 5.
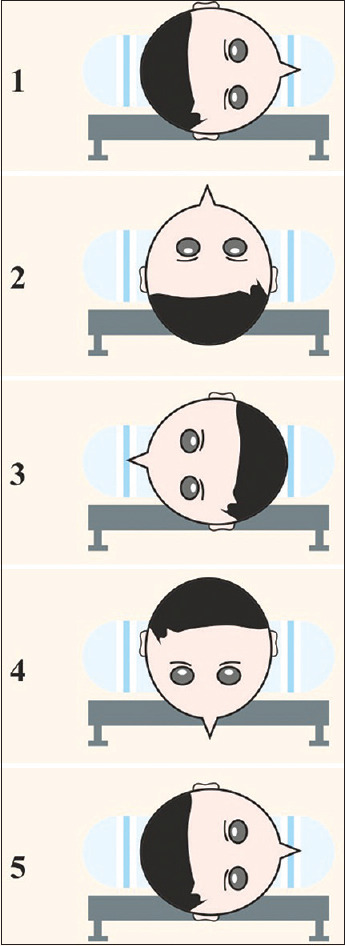
Lempert's 360-degrees Barbecue Roll Maneuver for right long posterior arm horizontal semicircular canalolithiasis: comprises sequent rolling of the patient and/or his head and maintaining each of the five positions for 30 seconds from right lateral recumbent, supine with nose pointing upwards, left lateral recumbent, supine with nose pointing downwards and right lateral recumbent, and after this patient is uprighted to short sitting position
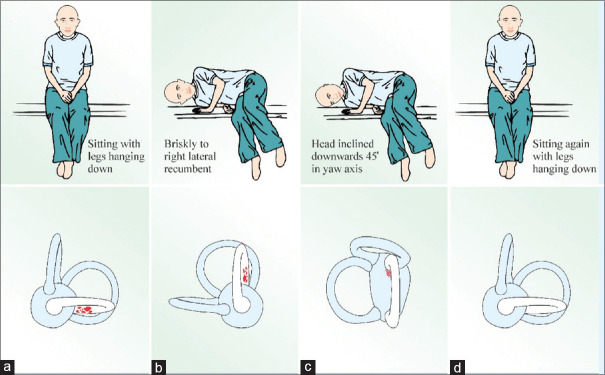
Figure 6.
Gufoni maneuver for the left long posterior arm horizontal semicircular canalolithiasis: From short-sitting on examination table (a) the patient is positioned to right lateral recumbent for a minute; (b) after which the head is inclined downwards 45-degrees in yaw axis; and (c) maintained for 2 min. After this, the patient is uprighted to short-sitting position (d). The lower row (a, b, c, and d) depicts the movement of otoconial debris
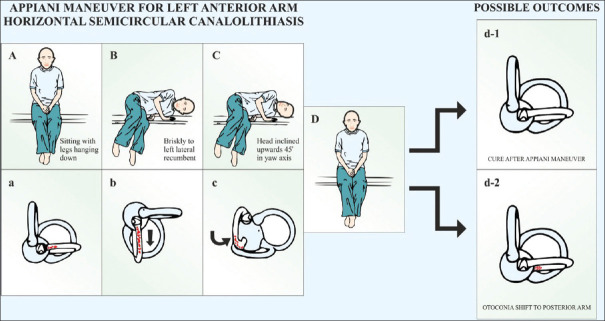
Figure 7.
Appiani maneuver for the left anterior arm horizontal semicircular canalolithiasis: From short-sitting on examination table (a) patient is positioned to left lateral recumbent for a minute; (b) after which head is inclined upwards 45-degrees in yaw axis; and (c) maintained for 2 min. After this, patient is uprighted to short-sitting position (d). The end result is either a direct cure (d-1) or transformation to left long posterior arm horizontal semicircular canalolithiasis (d-2)
Multicanal BPPV
The otoconia within the semicircular canals comprises calcite crystals (in canalolithiasis and cupulolithiasis) composed of calcium carbonate derived as broken-off fragments from the degenerative utricular macula. Usually, BPPV affects only one semicircular canal, and the monocanalicular posterior semicircular canalolithiasis is by far the most frequently encountered variant.[11,12,13,14,15,16,17,18,19,20,21] The vestibular rehabilitation of patients having multicanal BPPV requires special considerations regarding the chronological sequencing of treatment with repositioning maneuvers. The multicanalicular BPPV is unilateral in two-thirds of the cases, bilateral in the other one-third of the cases and roughly 80–90% of these patients have simultaneous involvement of posterior and horizontal semicircular canals of the same or opposite side.[42,43] In the most common variant of unilateral multicanalicular vestibular lithiasis of posterior and horizontal semicircular canals, possibly the otoconia enter both the canals simultaneously. In the second most frequent variant of bilateral multicanalicular vestibular lithiasis of posterior and horizontal semicircular canals, it is reasonable to think that the PSC-BPPV develops first on one side; this probably alters the habitual sleeping position of the sufferer to the unaffected lateral recumbent that sequentially leads to contralateral horizontal semicircular canalolithiasis.
The chronological sequencing of treatment with repositioning maneuvers and/or physical therapy, for the multicanalicular BPPV depends on the severity of symptoms attributed to the involved semicircular canal. As the horizontal semicircular canal is more frequently associated with autonomic symptoms like, nausea, vomiting, and diaphoresis,[8] in cases of multicanalicular canalolithiasis involving posterior and horizontal semicircular canals, a reasonable strategy would be to treat the horizontal semicircular canalolithiasis first and posterior semicircular canalolithiasis subsequently. It may take the spatial orientation of the involved semicircular canals into consideration for deciding the preferential sequencing for the treatment with repositioning maneuver and/or physical therapy. The posterior semicircular canal slopes inferiorly and has its cupular barrier at a relatively more dependent end; any otoconial debris that sequestrates in the ampullary arm of the posterior semicircular canal is liable to remain trapped for a long time. The cupular barrier of the horizontal semicircular canal is relatively higher in a location and this allows the free-floating debris to drift back to the utricle under the effect of gravity. It is, for this reason, some may prefer to treat posterior semicircular canalolithiasis first, considering this to be the reservoir of otoconia.
In the multicanal BPPV, it is imperative to perform all three positional tests, namely, DHT, SRT, and SHHT. The positioning may need to be repeated several times to unveil multiple nystagmi, each with different localizing and lateralizing values. The clinicians involved in the care of multicanalicular vestibular lithiasis need to realize that the pattern of nystagmus elicited during positioning in the positional test by stimulation of more than one semicircular canal is the net effect of force vectors generated by the otoconial movement in the concurrently affected semicircular canals.[44] If the repositioning maneuver cannot clear the semicircular canal, an alternative maneuver may need to be executed. A developing country like India requires clinicians involved in the care of patients with multicanalicular vestibular lithiasis to well verse all back-up maneuvers for clearing each of the three semicircular canals.
CONCLUSIONS
Successful treatment of BPPV with repositioning maneuvers and physical therapy has been one of the greatest conquests in the field of otoneurology. This has been possible due to several factors like in vivo demonstration of otoconia in the SCC, the application of physical laws to precisely lateralize as well as localize the otoconial debris within the SCC, and conceptualizing the movement of otoconia in the SCC during head movements in the physical models of the labyrinth to develop specific canal clearing maneuvers. A trained vestibular physician's role in medical fraternity is to obviate the unnecessary and often expensive neuroimaging studies which patients of BPPV often undergo due to ignorance of physicians at large to identify and treat this truly benign peripheral vestibular disorder by repositioning maneuvers and physical therapy.
Copyrights information
The educational videos in the YouTube links mentioned in column 7 of the Table 2 and column 4 of the Table 3 are protected by the copyrights of the author. The author has obtained the permission of the persons displayed in these educational videos. However, other than educational purposes in a limited audience, the reproduction of these videos on social media would be illegal and liable for civil prosecution.
Financial support and sponsorship
Nil.
Conflicts of interest
The authors whose names are listed above certify that they have NO affiliations with or involvement in any organization or entity with any financial interest (such as honoraria; educational grants; participation in speakers' bureaus; membership, employment, consultancies, stock ownership, or other equity interest; and expert testimony or patent-licensing arrangements), or non-financial interest (such as personal or professional relationships, affiliations, knowledge, or beliefs) in the subject matter or materials discussed in this manuscript.
Acknowledgements
The author is grateful to Professor Thomas Lempert, Professor of Neurology, Chief Physician of the Neurology Department at the Schlosspark Clinic in Berlin, Germany, for his kindness in providing his illustration [Figure 4] for this article. To Mr. Renith Kurian, who video recorded the diagnostic and therapeutic maneuvers (shown in the YouTube links) and precisely captured the nystagmus during the entire diagnostic and treatment period and to Mr. Ashraf for drawing the Figures 1 to 8 on CorelDRAW Graphics Suite 2019.
REFERENCES
- 1.Shepard NT, Telian SA, Smith-Wheelock M. Habituation and balance retraining therapy. A retrospective review. Neurol Clin. 1990;8:459–75. [PubMed] [Google Scholar]
- 2.Shepard NT, Telian SA. Programmatic vestibular rehabilitation. Otolaryngol Head Neck Surg. 1995;112:173–82. doi: 10.1016/S0194-59989570317-9. [DOI] [PubMed] [Google Scholar]
- 3.Cawthorne T. Vestibular injuries. Proc R Soc Med. 1946;39:270–3. [PMC free article] [PubMed] [Google Scholar]
- 4.Cooksey FS. Rehabilitation in vestibular injuries. Proc R Soc Med. 1946;39:273–8. [PMC free article] [PubMed] [Google Scholar]
- 5.Hall SF, Ruby RR, McClure JA. The mechanics of benign paroxysmal vertigo. J Otolaryngol. 1979;8:151–8. [PubMed] [Google Scholar]
- 6.Schuknecht HF. Cupulolithiasis. Arch Otolaryngol. 1969;90:765–78. doi: 10.1001/archotol.1969.00770030767020. [DOI] [PubMed] [Google Scholar]
- 7.Bruintjes TD, Masius-Olthof S, Kingma H. Benign paroxysmal positional vertigo of the horizontal canal. Otorhinolaryngol Clin. 2017;1(007):1–4. [Google Scholar]
- 8.Pagnini P, Nuti D, Vannucchi P. Benign paroxysmal vertigo of the horizontal canal. ORL J Otorhinolaryngol Relat Spec. 1989;51:161–70. doi: 10.1159/000276052. [DOI] [PubMed] [Google Scholar]
- 9.Parnes LS, Agrawal SK, Atlas J. Diagnosis and management of benign paroxysmal positional vertigo (BPPV) CMAJ. 2003;169:681–93. [PMC free article] [PubMed] [Google Scholar]
- 10.Ichijo H. Cupulolithiasis of the posterior semicircular canal. Am J Otolaryngol. 2013;34:458–63. doi: 10.1016/j.amjoto.2013.04.001. [DOI] [PubMed] [Google Scholar]
- 11.De la Meilleure G, Dehaene I, Depondt M, Damman W, Crevits L, Vanhooren G. Benign paroxysmal positional vertigo of the horizontal canal. J Neurol Neurosurg Psychiatry. 1996;60:68–71. doi: 10.1136/jnnp.60.1.68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Honrubia V, Baloh RW, Harris MR, Jacobson KM. Paroxysmal positional vertigo syndrome. Am J Otol. 1999;20:465–70. [PubMed] [Google Scholar]
- 13.Macias JD, Lambert KM, Massingale S, Ellensohn A, Fritz JA. Variables affecting treatment in benign paroxysmal positional vertigo. Laryngoscope. 2000;110:1921–4. doi: 10.1097/00005537-200011000-00029. [DOI] [PubMed] [Google Scholar]
- 14.Sakaida M, Takeuchi K, Ishinaga H, Adachi M, Majima Y. Long-term outcome of benign paroxysmal positional vertigo. Neurology. 2003;60:1532–4. doi: 10.1212/01.wnl.0000061477.03862.4d. [DOI] [PubMed] [Google Scholar]
- 15.Imai T, Ito M, Takeda N, Uno A, Matsunaga T, Sekine K, et al. Natural course of the remission of vertigo in patients with benign paroxysmal positional vertigo. Neurology. 2005;64:920–1. doi: 10.1212/01.WNL.0000152890.00170.DA. [DOI] [PubMed] [Google Scholar]
- 16.Nakayama M, Epley JM. BPPV and variants: Improved treatment results with automated, nystagmus-based repositioning. Otolaryngol Head Neck Surg. 2005;133:107–12. doi: 10.1016/j.otohns.2005.03.027. [DOI] [PubMed] [Google Scholar]
- 17.Cakir BO, Ercan I, Cakir ZA, Civelek S, Sayin I, Turgut S. What is the true incidence of horizontal semicircular canal benign paroxysmal positional vertigo. Otolaryngol Head Neck Surg. 2006;134:451–4. doi: 10.1016/j.otohns.2005.07.045. [DOI] [PubMed] [Google Scholar]
- 18.Moon SY, Kim JS, Kim BK, Kim JI, Lee H, Son SI, et al. Clinical characteristics of benign paroxysmal positional vertigo in Korea: A multicenter study. J Korean Med Sci. 2006;21:539–43. doi: 10.3346/jkms.2006.21.3.539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Jackson LE, Morgan B, Fletcher JC, Krueger WW. Anterior canal benign paroxysmal positional vertigo: An underappreciated entity. Otol Neurotol. 2007;28:218–22. doi: 10.1097/01.mao.0000247825.90774.6b. [DOI] [PubMed] [Google Scholar]
- 20.Chung KW, Park KN, Ko MH, Jeon HK, Choi JY, Cho YS, et al. Incidence of horizontal canal benign paroxysmal positional vertigo as a function of the duration of symptoms. Otol Neurotol. 2009;30:202–5. doi: 10.1097/mao.0b013e31818f57da. [DOI] [PubMed] [Google Scholar]
- 21.Korres S, Balatsouras DG, Kaberos A, Economou C, Kandiloros D, Ferekidis E. Occurrence of semicircular canal involvement in benign paroxysmal positional vertigo. Otol Neurotol. 2002;23:926–32. doi: 10.1097/00129492-200211000-00019. [DOI] [PubMed] [Google Scholar]
- 22.Shim DB, Ko KM, Lee JH, Park HJ, Song MH. Natural history of horizontal canal benign paroxysmal positional vertigo is truly short. J Neurol. 2015;262:74–80. doi: 10.1007/s00415-014-7519-0. [DOI] [PubMed] [Google Scholar]
- 23.von Brevern M, Bertholon P, Brandt T, Fife T, Imai T, Nuti D, et al. Benign paroxysmal positional vertigo: Diagnostic criteria. J Vestib Res. 2015;25:105–17. doi: 10.3233/VES-150553. [DOI] [PubMed] [Google Scholar]
- 24.Vannucchi P, Pecci R, Giannoni B, Di Giustino F, Santimone R, Mengucci A. Apogeotropic posterior semicircular canal benign paroxysmal positional vertigo: Some clinical and therapeutic considerations. Audiol Res. 2015;5:130. doi: 10.4081/audiores.2015.130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ewald JR. Wiesbaden, Germany: Bergmann JF Publishers; 1892. Physiologische Untersuchungen Ueber das Endorgan de Nervus Octavus. [Google Scholar]
- 26.Bhattacharyya N, Gubbels SP, Schwartz SR, Edlow JA, El-Kashlan H, Fife T, et al. Clinical practice guideline: Benign paroxysmal positional vertigo (Update) Otolaryngol Head Neck Surg. 2017;156(3 Suppl):S1–47. doi: 10.1177/0194599816689667. [DOI] [PubMed] [Google Scholar]
- 27.Helminski JO. Differential diagnosis and treatment of anterior canal paroxysmal positional vertigo. Vestibular Rehabilitation Special Interest Group Newsletter: BPPV Special Edition, American Physical Therapy Association/Neurology Section. 2012:17–21. [Google Scholar]
- 28.Yimtae K, Srirompotong S, Srirompotong S, Sae-Seaw P. A randomized trial of the canalith repositioning procedure. Laryngoscope. 2003;113:828–32. doi: 10.1097/00005537-200305000-00011. [DOI] [PubMed] [Google Scholar]
- 29.Anagnostou E, Stamboulis E, Kararizou E. Canal conversion after repositioning procedures: Comparison of Semont and Epley maneuver. J Neurol. 2014;261:866–9. doi: 10.1007/s00415-014-7290-2. [DOI] [PubMed] [Google Scholar]
- 30.Nuti D, Agus G, Barbieri MT, Passali D. The management of horizontal-canal paroxysmal positional vertigo. Acta Otolaryngol. 1998;118:455–60. doi: 10.1080/00016489850154559. [DOI] [PubMed] [Google Scholar]
- 31.Ko KM, Song MH, Kim JH, Shim DB. Persistent spontaneous nystagmus following a canalith repositioning procedure in horizontal semicircular canal benign paroxysmal positional vertigo. JAMA Otolaryngol Head Neck Surg. 2014;140:250–2. doi: 10.1001/jamaoto.2013.6207. [DOI] [PubMed] [Google Scholar]
- 32.Dorigueto RS, Ganança MM, Ganança FF. The number of procedures required to eliminate positioning nystagmus in benign paroxysmal positional vertigo. Braz J Otorhinolaryngol. 2005;71:769–75. doi: 10.1016/S1808-8694(15)31247-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Yacovino DA, Hain TC, Gualtieri F. New therapeutic maneuver for anterior canal benign paroxysmal positional vertigo. J Neurol. 2009;256:1851–5. doi: 10.1007/s00415-009-5208-1. [DOI] [PubMed] [Google Scholar]
- 34.Asprella GL, Gufoni M. Vertigine parossistica da CSL: Manovre di barbecue ed altre varianti. In: Nuti D, Pagnini P, Vicini C, editors. Atti della XIX Giornata di Nistagmografia Clinica. Milano: Formenti; 1999. pp. 321–36. [Google Scholar]
- 35.Lempert T, Tiel-Wilck K. A positional maneuver for treatment of horizontal-canal benign positional vertigo. Laryngoscope. 1996;106:476–8. doi: 10.1097/00005537-199604000-00015. [DOI] [PubMed] [Google Scholar]
- 36.Tusa RJ. Vertigo. Neurol Clin. 2001;19:23–55. doi: 10.1016/s0733-8619(05)70004-9. [DOI] [PubMed] [Google Scholar]
- 37.Vannucchi P, Giannoni B, Pagnini P. Treatment of horizontal semicircular canal benign paroxysmal positional vertigo. J Vestib Res. 1997;7:1–6. [PubMed] [Google Scholar]
- 38.Mandalà M, Califano L, Casani AP, Faralli M, Marcelli V, Neri G, et al. Double-blind randomized trial on the efficacy of the forced prolonged position for treatment of lateral canal benign paroxysmal positional vertigo. Laryngoscope. 2021;131:E1296–300. doi: 10.1002/lary.28981. [DOI] [PubMed] [Google Scholar]
- 39.Ciniglio Appiani G, Catania G, Gagliardi M, Cuiuli G. Repositioning maneuver for the treatment of the apogeotropic variant of horizontal canal benign paroxysmal positional vertigo. Otol Neurotol. 2005;26:257–60. doi: 10.1097/00129492-200503000-00022. [DOI] [PubMed] [Google Scholar]
- 40.Kim JS, Oh SY, Lee SH, Kang JH, Kim DU, Jeong SH, et al. Randomized clinical trial for apogeotropic horizontal canal benign paroxysmal positional vertigo. Neurology. 2012;78:159–66. doi: 10.1212/WNL.0b013e31823fcd26. [DOI] [PubMed] [Google Scholar]
- 41.Kim SH, Jo SW, Chung WK, Byeon HK, Lee WS. A cupulolith repositioning maneuver in the treatment of horizontal canal cupulolithiasis. Auris Nasus Larynx. 2012;39:163–8. doi: 10.1016/j.anl.2011.03.008. [DOI] [PubMed] [Google Scholar]
- 42.Tomaz A, Ganança MM, Ganança CF, Ganança FF, Caovilla HH, Harker L. Benign paroxysmal positional vertigo: Concomitant involvement of different semicircular canals. Ann Otol Rhinol Laryngol. 2009;118:113–7. doi: 10.1177/000348940911800206. [DOI] [PubMed] [Google Scholar]
- 43.Leopardi G, Chiarella G, Serafini G, Pennacchi A, Bruschini L, Brizi S, et al. Paroxysmal positional vertigo: Short- and long-term clinical and methodological analyses of 794 patients. Acta Otorhinolaryngol Ital. 2003;23:155–60. [PubMed] [Google Scholar]
- 44.Vats AK. Unilateral multicanalicular vestibular lithiasis of right horizontal and posterior semicircular canals: An unusual case. Ann Otol Neurotol. 2021 doi: 10.1055/s-0041-1735989. [DOI] [Google Scholar]