ABSTRACT
Preconception health is defined as the physical and psychological well-being of women and men throughout their reproductive life. It is a method that raises healthy fertility and focuses on activities that persons can take to minimize risks, raise healthy lifestyles, and increase preparation for pregnancy. The purpose of this systematic review study was to assess men’s knowledge of preconception health. Electronic databases, including Web of Science, PubMed, Scopus, Sciencedirect, ProQuest, Cochrane, SAGE, Springer, Google Scholar, were searched for published studies from 2000 to March 2021 to identify the studies carried out on men’s knowledge of preconception health. The quality assessment was done using the critical appraisal skills program tool for qualitative studies and the Newcastle-Ottawa scale for cross-sectional studies. Of the 1195 references identified in the initial search, 11 studies met the inclusion criteria. Because of the diversity in the study design and the data collection tools used in studies, meta-analysis was impossible. All the studies of the present systematic review found that men’s preconception health knowledge is poor. This systematic review showed that men’s preconception health knowledge is low. Due to the limited studies of men’s knowledge about the importance of optimizing their health before pregnancy, further study of the issue is still required.
Keywords: Health, knowledge, men, preconception
Background
Prepregnancy health refers to both the physical and psychological well-being of women and men throughout their reproductive life, without regard to sex, gender identity, sexual orientation, or pregnancy purpose. It is focused on actions that people can take to minimize risks, promote healthy habits, and increase preparation for conception.[1] Universally recognized scopes of women’s and men’s preconception health include sexual and reproductive health, genetics and family history, management of chronic diseases and infections, lifestyle behaviors, physical activity, nutrition, mental health, and hazards in the environment.[2] Research suggests that men’s health at conception influences pregnancy and neonatal outcomes over the spermatozoa quality and genetic effects[3] and by psycho-social determinants of health.[4] If men live a healthy lifestyle, they will have more chances to generate healthy sperm and better semen quality.[5] Evidence shows that men’s health conditions (e.g., obesity, diabetes) and risk behaviors (e.g., alcohol use, drug abuse, and smoking) impact not only their general health but also their reproductive ability.[6] Men know little about the factors that affect fertility.[5] Efforts to increase awareness of preconception health issues should not be limited to women.[7] The male’s genetics, medical history, reproductive history, and exposure to toxic substances are related to fertility and can affect the fetus’s environment directly or indirectly. Many occupational hazards can be brought into the home by men, including organic solvents, pesticides, and heavy metals. These hazards result in adverse reproductive effects such as infertility, miscarriage, low birth weight, and birth defects.[8,9] In addition, smoking men expose pregnant women to secondhand smoke. During pregnancy, passive smoke may have similar effects to active smoking by the mother and may increase the risk of adverse outcomes, such as low birth weight.[10]
Wholly, studies on preconception health awareness and men’s knowledge are rare. An acute barrier to the comprehensive use of preconception care seems to be a lack of knowledge about prevalent preconception risk factors. A first step toward reducing the risks associated with adverse pregnancy outcomes is understanding the sexual risk factors and unhealthy lifestyles associated with them before becoming pregnant. With increasing awareness of the risks associated with these factors, existing services are used more, and new services are developed. The purpose of this systematic review study was to examine men’s knowledge of preconception health.
Methods
Search strategies and study selection
Two independent authors (Z.R & A.GH) searched for published studies from 2000 to March 2021 by using the following key terms, “ men”, “male”, “father”, “preconception”, “pre-pregnancy”, “health”, “nutrition”, “lifestyle”, “exercise”, “weight”, “chronic disease”, “smoking”, “drinking”, “drug use”, “environmental toxins”, “immunizations”, “reproductive health-related behavior”, “reproductive life plan”, “prepare”, “knowledge”, and “awareness” in Electronic databases, including Scopus, Web of Science, PubMed, ProQuest, Sciencedirect, Cochrane, SAGE, Springer, and Google scholar.
Inclusion and exclusion criteria
Studies were eligible for inclusion if they were original articles, published full-text articles in English languages, and measured preconception health knowledge in men. We also included studies of men and women if data were presented separately for men. Studies were excluded if they (1) were a review of the literature, (2) were abstracts with incomplete findings and full text not available, or (3) were not published in the English language.
Data extraction and quality assessment
Two independent authors (Z.R & A.gh) extracted several characteristics from the included studies, such as author’s name, year of publication, objectives, study population, study province, sample size, study types, sampling method, and main results. Any disagreement between the two reviewers was resolved through discussion with the senior author (Z.M). Using tools appropriate to the type of study, two independent authors evaluated the quality of the studies. One of the most well-known scales for assessing the quality and risk of bias in observational studies is the Newcastle-Ottawa scale (NOS). The NOS checklist awards up to ten points in three domains, including a selection of study groups (five points), comparability of groups (two points), and ascertainment of exposure and outcome (three points). According to the NOS, the quality of the articles was rated in a range of 0–10. Total scores were categorized into four following groups:
Very good studies: 9–10 points
Good studies: 7–8 points
Satisfactory studies: 5–6 points
On the other hand, the critical appraisal skills program (CASP) tool is a universal tool for evaluating the strengths and limitations of any qualitative research method. The tool contains ten questions focusing on different aspects of qualitative research methodology.[13] In this study, the NOS was used to evaluate the quality of cross-sectional studies, and the CASP tool was used to evaluate the qualitative studies. Quality assessments are shown in Tables 1 and 2.
Table 1.
Assessing the quality of cross-sectional studies using the Newcastle-Ottawa scale
| Study (first author) | Study design | Selection | Comparability Basis of design or analysis |
Outcome | Final score | ||||
|---|---|---|---|---|---|---|---|---|---|
|
|
|
||||||||
| Representativeness of the sample | Sample size | Non respondents | Ascertainment of the exposure | Assessment of outcome | Statistical test | ||||
| Shaw, 2019[14] | Cross-sectional | * | * | ** | ** | * | 7 | ||
| Mitchell, 2012[15] | Cross-sectional | * | * | ** | ** | * | 7 | ||
| Temel, 2015[16] | Cross-sectional | * | * | * | ** | ** | * | 8 | |
| Frey, 2102[17] | Cross-sectional | * | * | * | ** | * | 6 | ||
| Al-Akour, 2015[18] | Cross-sectional | * | * | * | ** | ** | * | 8 | |
| Ishak, 2021[19] | Cross-sectional | * | * | ** | ** | * | 7 | ||
| Hammarberg, 2013[20] | Telephone survey | * | * | * | ** | * | 6 | ||
Table 2.
Assessing the quality of qualitative studies using the CASP tool
| Author | CASP question | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
|
| ||||||||||
| Was there a clear statement of the aims of the research? | Is a qualitative methodology appropriate? | Was the research design appropriate to address the aims of the research? | Are the study’s theoretical underpinnings clear, consistent and conceptually coherent? | Was the recruitment strategy appropriate to the aims of the research? | Was the data collected in a way that addressed the research issue? | Has the relationship between researcher and participants been adequately considered? | Have ethical issues been taken into consideration? | Was the data analysis sufficiently rigorous? | Is there a clear statement of findings? | |
| McGowan, 2020[21] | √ | √ | √ | √ | √ | √ | √ | √ | √ | |
| Hviid Malling, 2020[22] | √ | √ | √ | √ | √ | √ | √ | √ | √ | |
| Poels, 2017[23] | √ | √ | √ | √ | √ | √ | √ | √ | √ | √ |
| Hammarberg, 2017[24] | √ | √ | √ | √ | √ | √ | √ | √ | √ | |
Results
As illustrated in Figure 1, according to the PRISMA flowchart, 1195 studies were extracted through searching. Out of these 1195 studies, 1175 papers were excluded after reviewing the titles and abstracts, and then the full text of the remaining articles was assessed. Finally, 11 studies met the eligibility criteria and were included in the current systematic review. Seven studies were descriptive cross-sectional, and four were qualitative studies. All studies were published in English between 2012 and 2021. Descriptive studies include a total of 8401 participants, of whom 4746 were men, and qualitative studies include a total of 158 participants, of whom 73 were men. However, the analysis was only conducted on men participants. Two studies were conducted in the USA, two in the Netherlands, two in the UK, two in Australia, one in Sweden and Denmark, one in Jordan, and one in Malaysia. In descriptive studies, the sampling method was random, and a researcher-made questionnaire was used to assess preconception health knowledge. In qualitative studies, focus groups and semistructured interviews have been used to collect data. The summary of the study characteristics is shown in Table 3.
Figure 1.
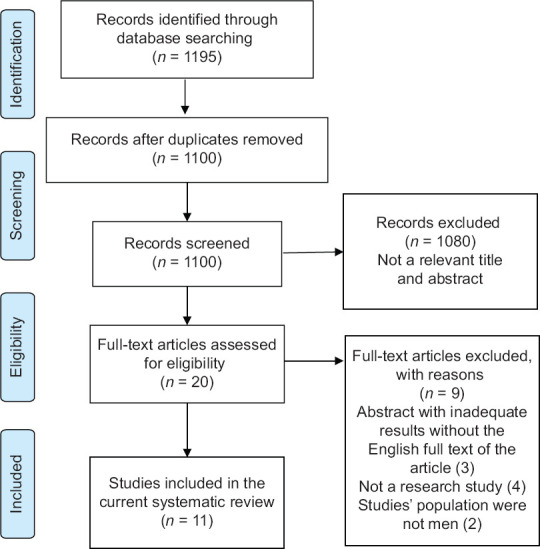
PRISMA flow diagram of the study
Table 3.
Main characteristics of the studies included in the present systematic review
| Author, year | Purpose of the study | Study population, country | Total sample size | Men sample size | Type of study | Sampling method | Main results |
|---|---|---|---|---|---|---|---|
| Shaw, 2019[14] | Examine men’s knowledge and health behaviors before fatherhood | Men attending antenatal care with their partners/England (London) | 573 | 573 | Cross-sectional | Convenience sampling | 19% of 565 men (n=108) said that they sought advice from a GP or health care professional about getting pregnant. A small percentage of respondents (2.3%, n=6) said that their GPs or health professionals gave them preconception health advice. In 24.5% of the cases (n=63), GPs or health professionals offered advice to both themselves and their partners. Only 21% of respondents (n=54) reported receiving information for their partner alone. |
| Mitchell, 2012[15] | Assessing men’s and women’s awareness of PCH exposure and knowledge of specific PCH behaviors | Women (18-44 yr) , Men (18-64yr)/united states | 2736 | 1796 | Healthstyle survey | Stratified random sampling | More than half of men (52%) were not aware of any exposure to PCH messages. Men perceived the most significant PCH behaviors for women, including avoiding cigarettes, illegal drugs, and alcohol use. |
| Temel, 2015[16] | Examine knowledge of preconception folic acid supplementation | Men and women aged between 16 and 85 years/Rotterdam, the Netherlands | 3500 | 1575 | Cross-sectional | Random sample | The correct answers to the preconception FA questions were 26% in men. |
| Frey, 2012[17] | To assess men’s knowledge level and beliefs about preconception healthcare. | Men aged between 16 and 45 years/united states (Arizona) | 132 | 132 | Survey study | Consecutive male patients presenting to primary care | Nearly all men in the study (93.2%) understood the importance of optimizing the mother’s health before pregnancy, but they showed a significant lack of knowledge about the factors that may threaten their health or the health of their fetuses. |
| Al-Akour, 2015[18] | Assess awareness of preconception care among Jordanian married women and men | Women and men who were married and aged >18 years/Jordan | 763 | 226 | Cross-sectional | Systematic random sampling (proportionate to size’) | Almost 50% of the men were aware that both the man’s and the woman’s family health history can affect their children’s health. More than 58% of men were aware that a woman’s health before pregnancy can have a serious impact on the health of her child, while 32.7% were aware that a man’s health can negatively affect the health of his child. |
| Ishak, 2021[19] | Assess the level of prepregnancy care knowledge among men | Married men aged more than 18 years old and less than 65 years old/Malaysia | 235 | 235 | Cross-sectional | Convenience Sampling. | Out of the respondents, 122 (51.9%) had poor knowledge of prepregnancy care, and 113 (48.1%) had a good knowledge of prepregnancy care. |
| Hammarberg, 2013[20] | To determine the knowledge of the effects of age, obesity, smoking, and timing of intercourse on fertility among Australians reproductive age | Men and women aged 18-45 years/Australia | 462 | 209 | Telephone survey | random sampling | About 20% of men realize that a woman’s fertility starts to decline before age 35. Approximately 52% of men stated that female fertility begins to decline after the age of 40, that age doesn’t matter, or that they don’t know. Only 36% of men are aware that a man’s fertility begins to decline at age 45. Overall, 58% of men indicated that male fertility declines after 50, “‘Age does not matter,”’ or “‘Don’t know.” |
| Hammarberg, 2017[24] | Explore fertility knowledge and information-seeking behaviors in people of reproductive age | Women and men aged 20-45 years, who were planning to have children in the future, or actively trying to conceive at the time of the research/Australia | 74 | 31 | Qualitative study/thematic analysis | Sampling with maximum diversity | Men generally reported “low” to “average” knowledge about fertility. Most of them overestimated women’s reproductive lifespans and had limited knowledge of the “fertile window” of the menstrual cycle. |
| Hviid Malling, 2020[22] | Explore young childless Danish and Swedish men’s perspectives on fertility and infertility. | Young childless men aged between 20 and 30 years/Denmark and Sweden | 29 | 29 | Qualitative content analysis | Snow-ball methods | The young men had limited knowledge about factors that can impair male and female fertility. |
| Poels, 2017[23] | Assess how PCC should be provided from the perspective of parents. | Couples who received antenatal care at a Dutch community midwifery practice/Netherlands | 34 | 5 | Thematic analysis | Purpose-based | Men were generally unaware of preconception care. |
| McGowan, 2020[21] | Explore beliefs, knowledge, and attitudes on preconception health amongst adults of reproductive age | Females and males of childbearing age (aged 18-45 years)/UK | 21 | 8 | Descriptive qualitative | Purpose-based | Lack of comprehensive knowledge about preconception health |
Discussion
The purpose of this systematic review was to assess men’s knowledge of preconception health. The articles reviewed in this study provided only a poor overview of men’s knowledge of preconception health. It is because the number of studies done in this field is limited. Not to mention, due to the diversity in the study design and the data collection tools used in studies, meta-analysis was not possible.
The preconception period is fundamental and vital. The preconception period is fundamental and vital. It determines the future health of the mother, her child, and her family.[15] At pregnancy, 50% of DNA comes from male spermatozoa. Numerous factors, including environmental factors and lifestyle, appear to cause DNA damage through oxidative stress, consequently reducing sperm quality and successful pregnancies.[25] Moreover, from an ethical perspective, men have a moral responsibility to change their preconception lifestyles and habits to create a healthy, safe environment for raising children.[26] Furthermore, fathers are in a strong position to positively influence maternal behaviors, such as drug use and early use of prenatal care, each of which can have a significant impact on pregnancy outcomes.[27] Studies show that men’s preconception health is increasingly considered a factor in improving reproductive health, pregnancy, and neonatal outcomes.[6,28] To improve pregnancy outcomes by maintaining or enhancing position of men’s preconception health, two key points should be considered: first, providing motivational information to men, and second, encouraging men to correct behaviors based on new knowledge.[26]
In this systematic review, studies examined topics such as men’s awareness of the importance of their preconception health and its effect on infant health, men’s awareness of the importance of women’s preconception health, men’s awareness of specific preconception behaviors in women (such as avoiding smoking, alcohol, and illicit drugs), men’s awareness of preconception folic acid supplementation by women, men’s awareness of women’s preconception care, and men’s knowledge of the effects of age, obesity, smoking, and sexual intercourse time on fertility. Al-Akour et al.[18] (2015) showed that almost 50% of men were aware of the serious consequences of a father’s family history on the health of his child, and more than 58% of men knew that woman’s health before conception could have a significant impact on the health of her child. On the other hand, 32.7% of men were aware of the serious consequences of man’s health before conception on the health of his infant. Frey et al.[17] (2012) reported that 93.2% of men were aware of the importance of optimizing maternal health before pregnancy. Also, they were highly aware of key risk factors before pregnancy in women (e.g., alcohol use, illicit drug use, and domestic violence), which may affect pregnancy outcomes, while only 8.3% of men mentioned that they had received information and advice from their doctor about their prepregnancy health. Mitchell et al.[15] (2012) showed that 52% of men were unaware of any exposure to preconception health messages, while they were aware of specific preconception health behaviors for women. However, Ishak et al.[19] (2021) reported that 51.9% of men (n = 122) had poor knowledge about preconception care for women.
The results of the present systematic review show that men’s preconception health knowledge is poor, while studies on women’s knowledge of preconception health and care have reported a better level of knowledge. To that end, in Iraq, Mirkhan Ahmed et al.[29] (2017) reported that most women (76.7%) of childbearing age had sufficient knowledge about preconception care. Similarly, Coonrod et al.[30] (2009) in the United States reported that the average score of women’s knowledge of preconception care was 76%. In Iran, a study by Firouzi et al. (2017) on married women showed that women have a good level of knowledge about preconception care.[31] However, the results of studies conducted on women indicate that they are more aware of preconception care than men; maybe this difference is due to the different tools of knowledge measuring in studies, the existence of specific guidelines for women’s preconception health, more women’s access to health care and preconception health education, lack of regular visits in health centers for men, and insufficient attention of developing countries to preconception health in men.
Strengths and limitations
The novelty of this study was the first systematic review of men’s preconception health knowledge.
The present systematic review study has limitations. First, the use of various tools to measure knowledge within the studies can affect the level of knowledge of preconception health. Because of this, it is not possible to generalize the results. Few studies have been conducted on men’s knowledge of preconception health. This problem was solved by including studies consisting of men and women. However, this review study analyzed only men’s data.
Conclusion
This systematic review showed that men’s preconception health knowledge is low. Men should be aware of behaviors and habits that may be harmful or helpful to their reproductive health. Efforts to strengthen preconception healthcare in men have so far been few, and knowledge about their impact on men’s reproductive and lifelong health is limited. Due to the limited studies of men’s knowledge about the importance of optimizing their health before pregnancy, further study of the issue is still required.
Key points
Men were generally unfamiliar with preconception health. However, men perceived avoiding high-risk behaviors to be the most important for women.
The previous finding showed a significant lack of men’s knowledge about the factors that may threaten their health or the health of their fetuses
The results of the present systematic review show that men’s preconception health knowledge is poor.
Men should be aware of behaviors and habits that may be harmful or helpful for their reproductive health.
Authors’ contributions
All authors contributed to the study’s conception and design. Material preparation, data collection, and analysis were performed by [ZR], [AGh], [RT], [NM], and [M Sh]. The first draft of the manuscript was written by [ZR] and [ZM], and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgement
The present study was part of the results of the Ph.D. thesis approved by Shahroud University of Medical Sciences (Thesis code: 907). We sincerely want to thank our colleagues who provided advice and knowledge that helped us significantly in writing the paper.
References
- 1.Ontario Public Health Association. Shift–Enhancing the Health of Ontarians: A Call to Action for Preconception Health Promotion and Care. Toronto, ON: Ontario Public Health Association; 2019. [Google Scholar]
- 2.Robbins CL, Zapata LB, Farr SL, Kroelinger CD, Morrow B, Ahluwalia I, et al. Core state preconception health indicators—pregnancy risk assessment monitoring system and behavioral risk factor surveillance system, 2009. MMWR Surveill Summ. 2014;63:1–62. [PubMed] [Google Scholar]
- 3.Moss JL, Harris KM. Impact of maternal and paternal preconception health on birth outcomes using prospective couples'data in Add Health. Arch Gynecol Obstet. 2015;291:287–98. doi: 10.1007/s00404-014-3521-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kotelchuck M, Lu M. Father's role in preconception health. Matern Child Health J. 2017;21:2025–39. doi: 10.1007/s10995-017-2370-4. [DOI] [PubMed] [Google Scholar]
- 5.Barron ML. Fertility literacy for men in primary care settings. J Nurse Pract. 2013;9:155–60. [Google Scholar]
- 6.Gavin L, Pazol K, Ahrens K. Providing quality family planning services:Recommendations of CDC and the US Office of Population Affairs. MMWR Morb Mortal Wkly Rep. 2017;66:1383–5. doi: 10.15585/mmwr.mm6650a4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Johnson K, Posner SF, Biermann J, Cordero JF, Atrash HK, Parker CS, et al. Recommendations to improve preconception health and Health Care—United States:Report of the CDC/ATSDR preconception care work group and the select panel on preconception care. MMWR Recomm Rep. 2006;55:1–23. [PubMed] [Google Scholar]
- 8.Burdorf A, Figà-Talamanca I, Jensen TK, Thulstrup AM. Effects of occupational exposure on the reproductive system:Core evidence and practical implications. Occup Med. 2006;56:516–20. doi: 10.1093/occmed/kql113. [DOI] [PubMed] [Google Scholar]
- 9.Ojifinni OO, Ibisomi L. Preconception care practices in Nigeria:A descriptive qualitative study. Reprod Health. 2020;17:1–13. doi: 10.1186/s12978-020-01030-6. doi:10.1186/s12978-020-01030-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Grant SG. Qualitatively and quantitatively similar effects of active and passive maternal tobacco smoke exposure on in utero mutagenesis at the HPRT locus. BMC Pediatr. 2005;5:1–8. doi: 10.1186/1471-2431-5-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Herzog R, Álvarez-Pasquin MJ, Díaz C, Del Barrio JL, Estrada JM, Gil Á. Are healthcare workers'intentions to vaccinate related to their knowledge, beliefs and attitudes?A systematic review. BMC Public Health. 2013;13:1–17. doi: 10.1186/1471-2458-13-154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lo CK-L, Mertz D, Loeb M. Newcastle-Ottawa Scale:Comparing reviewers'to authors'assessments. BMC Med Res Methodol. 2014;14:1–5. doi: 10.1186/1471-2288-14-45. doi:10.1186/1471-2288-14-45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Long HA, French DP, Brooks JM. Optimising the value of the critical appraisal skills programme (CASP) tool for quality appraisal in qualitative evidence synthesis. Res Methods in Med Health Sci. 2020;1:31–42. [Google Scholar]
- 14.Shawe J, Patel D, Joy M, Howden B, Barrett G, Stephenson J. Preparation for fatherhood:A survey of men's preconception health knowledge and behaviour in England. PLoS One. 2019;14:e0213897. doi: 10.1371/journal.pone.0213897. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Mitchell EW, Levis DM, Prue CE. Preconception health:Awareness, planning, and communication among a sample of US men and women. Matern Child Health J. 2012;16:31–9. doi: 10.1007/s10995-010-0663-y. [DOI] [PubMed] [Google Scholar]
- 16.Temel S, Erdem Ö, Voorham TA, Bonsel GJ, Steegers EA, DenktaşS Knowledge on preconceptional folic acid supplementation and intention to seek for preconception care among men and women in an urban city:A population-based cross-sectional study. BMC Pregnancy Childbirth. 2015;15:1–11. doi: 10.1186/s12884-015-0774-y. doi:10.1186/s12884-015-0774-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Frey KA, Engle R, Noble B. Preconception healthcare:What do men know and believe? J Mens Health. 2012;9:25–35. [Google Scholar]
- 18.Al-Akour N, Sou'Ub R, Mohammad K, Zayed F. Awareness of preconception care among women and men:A study from Jordan. J Obstet Gynaecol. 2015;35:246–50. doi: 10.3109/01443615.2014.958145. [DOI] [PubMed] [Google Scholar]
- 19.Ishak SH, Yaacob LH, Ishak A. Knowledge of pre-pregnancy care among men attending the outpatient clinics of Hospital Universiti Sains Malaysia. T Malays J Med Sci. 2021;28:119–27. doi: 10.21315/mjms2021.28.2.11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hammarberg K, Setter T, Norman RJ, Holden CA, Michelmore J, Johnson L. Knowledge about factors that influence fertility among Australians of reproductive age:A population-based survey. Fertil Steril. 2013;99:502–7. doi: 10.1016/j.fertnstert.2012.10.031. [DOI] [PubMed] [Google Scholar]
- 21.McGowan L, Lennon-Caughey E, Chun C, McKinley MC, Woodside JV. Exploring preconception health beliefs amongst adults of childbearing age in the UK:A qualitative analysis. BMC Pregnancy Childbirth. 2020;20:1–13. doi: 10.1186/s12884-020-2733-5. doi:10.1186/s12884-020-2733-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Hviid Malling GM, Schmidt L, Pitsillos T, Hammarberg K, Tydén T, Friberg B, et al. Taking fertility for granted–a qualitative exploration of fertility awareness among young, childless men in Denmark and Sweden. Hum Fertil. 2020:1–12. doi: 10.1080/14647273.2020.1798516. doi: 10.1080/14647273.2020.1798516. [DOI] [PubMed] [Google Scholar]
- 23.Poels M, Koster M, Franx A, Van Stel H. Parental perspectives on the awareness and delivery of preconception care. BMC Pregnancy Childbirth. 2017;17:1–9. doi: 10.1186/s12884-017-1531-1. doi:10.1186/s12884-017-1531-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Hammarberg K, Zosel R, Comoy C, Robertson S, Holden C, Deeks M, et al. Fertility-related knowledge and information-seeking behaviour among people of reproductive age:A qualitative study. Hum Fertil. 2017;20:88–95. doi: 10.1080/14647273.2016.1245447. [DOI] [PubMed] [Google Scholar]
- 25.Wright C, Milne S, Leeson H. Sperm DNA damage caused by oxidative stress:Modifiable clinical, lifestyle and nutritional factors in male infertility. Reprod Biomed Online. 2014;28:684–703. doi: 10.1016/j.rbmo.2014.02.004. [DOI] [PubMed] [Google Scholar]
- 26.O'Brien AP, Hurley J, Linsley P, McNeil KA, Fletcher R, Aitken JR. Men's preconception health:A primary health-care viewpoint. Am J Mens Health. 2018;12:1575–81. doi: 10.1177/1557988318776513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Misra DP, Caldwell C, Young AA, Abelson S. Do fathers matter?Paternal contributions to birth outcomes and racial disparities. Am J Obstet Gynecol. 2010;202:99–100. doi: 10.1016/j.ajog.2009.11.031. [DOI] [PubMed] [Google Scholar]
- 28.Frey KA, Navarro SM, Kotelchuck M, Lu MC. The clinical content of preconception care:Preconception care for men. Am J Obstet Gynecol. 2008;199:S389–95. doi: 10.1016/j.ajog.2008.10.024. [DOI] [PubMed] [Google Scholar]
- 29.Mirkhan Ahmed H, Jamil Piro T. Knowledge, practice, and attitude of married women about preconception care. J Client- Centered Nurs Care. 2017;3:37–44. [Google Scholar]
- 30.Coonrod DV, Bruce NC, Malcolm TD, Drachman D, Frey KA. Knowledge and attitudes regarding preconception care in a predominantly low-income Mexican American population. Am J Obstet Gynecol. 2009;200:686.e1–7. doi: 10.1016/j.ajog.2009.02.036. [DOI] [PubMed] [Google Scholar]
- 31.Firouzi M, Ebrahimi A. Knowledge and attitudes of women about preconception care. Qom Univ Med Sci J. 2017;10:62–8. [Google Scholar]


