Abstract
Background
The aim of the present study is to evaluate the most common reasons for replacing posterior amalgam and resin composite restorations in patients attending the university dental restorative clinics.
Methods
A total of 318 restorations which needed to be replaced were clinically and radiographically evaluated in a period of nine months. The frequencies of reasons for replacing posterior amalgam and resin composite restorations were calculated; secondary caries, restoration/tooth fracture, marginal discoloration/ditching, proximal overhang/open margin, loss of anatomy, pain/sensitivity, and esthetics.
Results
The sample population comprised of 191 females and 106 males. The majority of the sample population fell in the age group of 40–50 years (n = 110). 318 restorations (n = 318) were examined in this study. 82% of examined teeth were restored with amalgam (n = 261), while posterior composite restorations comprised 18% of the examined teeth (n = 57). Among all restorations demanded to be replaced by the patients (n = 318), aesthetic need was the most common reason (n = 98), followed by Ditching or discoloration (n = 64), secondary caries (n = 57), and fracture (n = 44). Loss of anatomy was the least common cause to replace both amalgam and resin composite restorations (n = 5). The different reasons of failure were all significant between amalgam and resin composite restorations as shown in (Fig. 1) (p < 0.005). The most common reason for amalgam replacement was aesthetic. The most common reason for composite replacement was secondary caries and marginal ditching.
Conclusion
Both amalgam and composite had different reasons for replacement. Amalgam had lesser risk of developing secondary caries and higher longevity than composite.
Keywords: Resin composite, Amalgam, Recurrent caries, Fracture, Aesthetics
1. Introduction
For centuries dental amalgam was considered material of choice for restoring carious cavities in posterior teeth (Talabani, 2015). However, the advent of adhesive dental materials since 1955 by Buonocore has led to a giant leap in restorative dentistry (Mendiratta et al., 2021). Thus, minimal invasive philosophy was adopted in dentistry in the early 1970 s (Walsh and Brostek, 2013). The better understanding of the etiopathogenesis of dental caries process and its dynamic nature has revolutionized treatment strategies and shifted the oral health paradigm toward preventive intervention rather than operative intervention (Fejerskov, 1997). The implementation of Minamata Convention on Mercury since 2013 with all the apprehensions on mercury toxicity mandated phasing down dental amalgam restorations (Fisher et al., 2018). Nowadays the overwhelming desire for aesthetic dental restorations became a trendy demand more than a necessary need (Kelleher, 2010). All the aforementioned five factors contributed to the loss of glory and popularity of dental amalgam restoration (Shenoy, 2008).
After the initial euphoria of the more aesthetic and conservative restoration, it was realized that this new material is not without disadvantages including; greater technique sensitivity, time consuming during placement, polymerization shrinkage, and higher cost than dental amalgam (Akbar, 2015, Chan et al., 2010). Therefore, there is still little justification for continued use of dental amalgam restoration, and it is still widely used especially in developing countries (Arotiba et al., 2020, Haque et al., 2019).
However, failure of both amalgam and resin composite restorations is not uncommon, and their replacement consumes more than half of general dental practice services (Gordan et al., 2012). Restoration failure and replacement, in general, for both restorations could be attributed to several factors (Bernardo et al., 2007). As for both restorations fracture and secondary caries are the main reasons for their failure (Alanazi et al., 2019, Mahajan et al., 2015, Montagner et al., 2018, Olaleye and Shaba, 2020, Pouralibaba et al., 2010).
The aim of this study was to clinically evaluate the most common reasons for replacement of amalgam and composite restorations and analyze the failure pattern among our patients presenting at Jordan University Hospital for routine dental treatment at its dental restorative clinics.
2. Materials and methods
This cross-sectional study was carried out on 297 patients aged 18 years and above, who visited the restorative dental clinics of Jordan University Hospital. Amalgam and direct composite restorations to be replaced in permanent posterior teeth were included. The demographic information of patients like sex and age were recorded. Restoration class (according to GV Black classification) distribution between amalgam and composite according to type of tooth (premolar or molar), number of surfaces (Cl I, Cl II, MOD) was examined and recorded on a case sheet form specially designed for this study. We noted several tooth and restoration characteristics to further investigate their relationship with failure. These characteristics included the age of restoration (<5 years old, 5–10 years old, greater than 10 years old), the plaque index (good, fair, poor), occlusal remarks (bruxism).
All restorations were examined by two examiners (restorative consultants) clinically (visual-tactile) and radio-graphically (bitewing) to find out the reasons of the failed amalgam and composite restorations which needed replacement while the teeth were still vital and restorable or need endodontic treatment. After getting a thorough history of the patient, examination was carried out on dental chair using examination instruments and other examination aids if needed such as bitewing or periapical radiographs and thermal tests using refrigerant spray containing tetrafluoroethane (-50 °C). The examination of patients involved the sequential assessment of all restorations for the evidence of secondary caries, restoration or tooth fracture, discoloration (marginal, material, tooth), amalgam ditching or degradation with macro-leakage space, composite debonding, proximal overhang or open proximal contact point, pain or sensitivity, wear and loss of anatomy, aesthetic reasons for replacement of the restoration.
The collected information and responses were coded and statistical analysis was performed using the software SPSS Statistics for Windows, Version 16.0 (SPSS Inc., Chicago, IL, USA). All data were tested for normality using the Shapiro-Wilk test to examine whether our sample data had been drawn from a normally distributed population. Descriptive statistics were generated and Chi-square test was used to determine if the difference between the observed data and the expected data is due to chance, or if it is significant and due to a relationship between the variables we are studying. The significance level was set at P < 0.05.
3. Results
The sample population comprised of 191 females and 106 males. The majority of the sample population fell in the age group of 40–50 years (n = 110) and 18–28 years (n = 94). The average age of the patients was 37.43 (M = 37.43, SD = 12.22). The 297 patients attended the restorative dental clinics of Jordan University Hospital demand the replacement of 318 restorations (n = 318). 82% of examined teeth were restored with amalgam (n = 261), while posterior composite restorations comprised 18% of the examined teeth (n = 57). All restorations to be replaced were placed out of the university hospital either in the private sector or other general dental facilities in and outside the country, placed mostly by general practitioners. The distribution of both amalgam and resin composite restorations placed on the premolar and molar dentition are shown in (Table 1).
Table 1.
Distribution of the different restorations to be replaced depending on cavity classification, tooth type, and number of surfaces restored.
| Amalgam n = 261 |
Composite n = 57 |
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Molar n = 191 |
Premolar n = 70 |
Molar n = 29 |
Premolar n = 28 |
||||||||
| Class 1 | class2 | MOD | Class 1 | class2 | MOD | Class 1 | class2 | MOD | Class 1 | class2 | MOD |
| n = 97 (51%) | n = 66 (34%) | n = 28 (15%) | n = 21 (30%) | n = 30 (43%) | n = 19 (27%) | n = 16 (55%) | n = 8 (28%) | n = 5 (17%) | n = 10 (36%) | n = 7 (25%) | n = 11 (39%) |
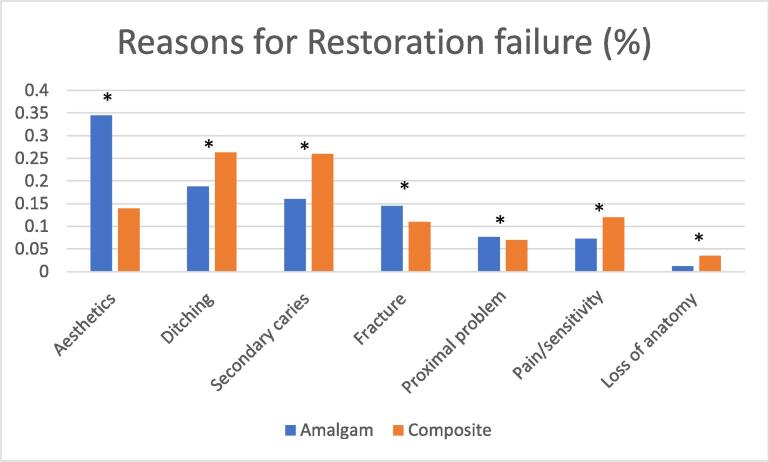
Among all restorations demanded to be replaced by the patients (n = 318), aesthetic need of the patient was the most common reason (n = 98), followed by Ditching or discoloration (n = 64), secondary caries (n = 57), and fracture (n = 44). Loss of anatomy was the least common cause to replace both amalgam and resin composite restorations (n = 5). The different reasons of failure were all significant between amalgam and resin composite restorations as shown in (Fig. 1) (p < 0.005).
Fig. 1.
Reasons for replacement of restoration by type of material. A star indicates statistically significant difference between amalgam and resin composite restoration.
The main reason to replace amalgam restoration among all cavity preparation surfaces was aesthetic demand except for Cl II on premolars and MOD on molars which was secondary caries, and Cl II on molars which was fracture (Table 2). 49 patients ask to replace amalgam restorations due to secondary caries or discoloration which was diagnosed after clinical and radiographic examination as ditching or corrosion. Thirty-eight restored teeth with amalgam showed fractures in which only two of them were tooth fracture in molar (Cl I and MOD), while the other 36 teeth demonstrated restoration fracture which was prominent in Cl II molars (n = 19). Out of the 19 amalgam restorations which were associated with pain, 3 of them needed occlusal adjustment and 5 of them were referred to endodontic treatment after clinical and radiographic examination. The remaining 11 restorations were replaced with a liner or a base as needed. Proximal defects in amalgam restorations (n = 20) were more overhangs (n = 13) than open contacts (n = 7).
Table 2.
Reasons for replacing amalgam restorations.
| Amalgam Restoration N = 261 |
Molars |
Premolars |
Total | ||||
|---|---|---|---|---|---|---|---|
|
n = 191 (73%) |
n = 70 (27%) |
||||||
|
Cl I |
Cl II |
MOD |
Cl I |
Cl II |
MOD |
||
| n = 97 | n = 66 | n = 28 | n = 21 | n = 30 | n = 19 | ||
| Aesthetics | 48 | 14 | 6 | 14 | 3 | 5 | 90 (34%) |
| Ditching/discoloration | 29 | 9 | 3 | 2 | 4 | 2 | 49 (19%) |
| Secondary caries | 7 | 11 | 7 | 2 | 10 | 5 | 42 (16%) |
| Fracture (tooth/restoration) | 3 | 19 | 6 | – | 7 | 3 | 38 (15%) |
| Proximal overhang/open contact | – | 8 | 3 | – | 6 | 3 | 20 (8%) |
| Pain/sensitivity | 9 | 5 | 2 | 2 | – | 1 | 19 (7%) |
| Loss of anatomy | 1 | – | 1 | 1 | – | – | 3 (1%) |
Secondary caries (n = 15) and marginal discoloration (n = 15) were the most prevalent reasons for resin composite restorations replacement or repair (Table 3). Patients with teeth diagnosed with marginal discoloration came to replace their discolored teeth due to fear of the presence of secondary caries (n = 9), while others demanded the replacement for aesthetic reasons (n = 6). All fractures in composite restorations were associated with the material fracture itself rather than tooth fracture. Out of 4 teeth with proximal defects in composite restorations, two have proximal overhang (connected teeth), while the other two restorations have proximal open contacts. Two composite restorations out of seven which suffered from sensitivity, have a history of replacement less than one year ago after amalgam restoration (Cl I on molar). Another one restoration showed defected/open margin (Cl II on premolar), and another one was debonded and mobile (Cl II on premolar).
Table 3.
Reasons for replacing resin composite restorations.
| Composite restoration N = 57 |
Molars |
Premolars |
Total | ||||
|---|---|---|---|---|---|---|---|
|
n = 29 (51%) |
n = 28 (49%) |
||||||
|
Cl I |
Cl II |
MOD |
Cl I |
Cl II |
MOD |
||
| n = 16 | n = 8 | n = 5 | n = 10 | n = 7 | n = 11 | ||
| Secondary caries | 3 | 4 | 1 | 3 | 2 | 2 | 15 (26%) |
| Marginal discoloration | 4 | 2 | 1 | 3 | 2 | 3 | 15 (26%) |
| Aesthetics | 4 | – | – | 3 | – | 1 | 8 (14%) |
| Pain/sensitivity | 3 | 1 | – | 1 | 1 | 1 | 7 (12%) |
| Fracture (tooth/restoration) | – | – | 2 | – | 2 | 2 | 6 (11%) |
| Proximal overhang/open contact | – | 1 | 1 | – | – | 2 | 4 (7%) |
| Loss of anatomy | 2 | – | – | – | – | – | 2 (4%) |
More than 140 of the replaced amalgam restorations (56%) were more than 10 years old compared to 18 of the replaced composite resin restorations (32%). Patients with poor oral hygiene have more teeth replaced with composite resin restorations (37%) compared to amalgam (28%). While, Patients with bruxism and cuspal attrition have more teeth replaced with amalgam restorations (26%) compared to composite resin restorations (5%). Four percent of the replaced amalgam restorations (n = 10) and 5% of replaced composite restorations (n = 3) were diagnosed in patients showed bruxism and cuspal attrition (Table 4).
Table 4.
Distribution of reasons for restorations replacement on associated factors.
| N = 318 | Amalgam |
Composite |
||||
|---|---|---|---|---|---|---|
| n = 261 (82%) |
n = 57 (18%) |
|||||
| AOR |
PI |
OR |
AOR |
PI |
OR |
|
| greater than10 | poor | bruxism | greater than10 | poor | bruxism | |
| Secondary caries | 29 | 30 | – | 5 | 9 | – |
| Fracture (tooth/restoration) | 28 | 4 | 5 | 1 | – | 2 |
| Ditching/marginal discoloration | 25 | 11 | – | 7 | 6 | – |
| Proximal overhang/open contact | 4 | 7 | 3 | 1 | – | – |
| Loss of anatomy | 2 | – | 2 | 1 | – | 1 |
| Pain/sensitivity | 10 | 4 | – | – | 1 | – |
| Aesthetics | 49 | 18 | – | 3 | 5 | – |
| Total | 147 | 74 | 10 | 18 | 21 | 3 |
| 56% | 28% | 4% | 32% | 37% | 5% | |
4. Discussion
Restorations replacement accounts for more than half of restorations placed by dentists, and the proportion of restorations replacement continues to increase worldwide (Eltahlaha et al., 2018). Most dentists practicing in Jordan had an undergraduate training in favor of placing amalgam when restoring posterior cavities (Al-Rabab’ah et al., 2016). Furthermore, <20% of dentists practicing in Jordan had an undergraduate training in favor of placing composites in posterior teeth (Al-Rabab’ah et al., 2016). A large number of dentists believe that amalgam possessed greater longevity and superior mechanical properties, with less sensitive technique compared to tooth-colored restorations. This is in agreement with our study data where more than 80% of examined teeth were restored with amalgam while posterior composite restorations comprised the remaining proportion.
Successful amalgam restorations require a precise cavity design and a special resistance and retention forms to withstand occlusal forces during mastication and to retain the non-adhesive material inside the restored tooth. Faulty cavity design and mismanagement of using dental amalgam will lead eventually to restoration failure due to secondary caries or fractures. Many previous studies reported that the most common reason for amalgam restoration replacement is secondary caries (Al-Negrish, 2001, Bernardo et al., 2007, Kimyai et al., 2007, Silvani et al., 2014) or fractures (Pouralibaba et al., 2010) especially for complex cavity designs and multi-surface restorations. A previous study research carried on the same population showed that secondary caries, in class II and MOD restorations, was the most frequent reason for replacement of failed restorations in permanent teeth accounting for more than 56% of failed restorations (Al-Kayed, 1996). Furthermore, fractures were the second reason for replacement of failed restorations in 25% of retreated restorations (Al-Kayed, 1996). This is in agreement with our finding where class 2 and MOD on premolars and molars had failed due to either secondary caries or fractures. However, taking all amalgam restorations into consideration, our research data showed that aesthetic was the most common reason for amalgam replacement. These findings are not surprising and concur with several recent reports found that patients’ main concerns about treatment are related to the cosmetic appearance of the fillings (Braga et al., 2007, Faraj et al., 2015). A recent cross-sectional study found that dentists in Jordan start implementing a ‘phase-down’ of dental amalgam in their dental clinics due to current dental practice trends and patients’ aesthetic demands rather than commitment to the Minamata Convention (Al-Asmar et al., 2019). Change in patients’ caries risk and improvement of the dentists’ skills, among our studied population, might also lead to decreased prevalence of secondary caries and fractures in amalgam restorations.
Marginal ditching was the second most common reason for replacing amalgam restoration. Ditching is a deficiency of amalgam along the junction between the tooth and the restoration. Although ditching is not necessarily related to secondary caries, this deficient area usually appears as a blueish-gray discolored margin due to accumulation of corrosion products coming from amalgam or stains from the oral cavity (Magalhaes et al., 2009). Therefore, most patients will come to clinic demanding replacement of ditched restorations due to aesthetic reasons or fear of caries presence. This is in agreement with our study where 49 patients ask to replace amalgam restorations due to secondary caries or discoloration which was diagnosed after clinical and radiographic examination as ditching or corrosion.
Secondary caries is the same as primary caries located at the margin of a restoration (Mjör and Toffenetti, 2000). It is usually difficult to diagnose clinically until a new cavity formed at the margin (Mjör and Toffenetti, 2000). Amalgam restoration are considered non-adhesive restoration. This means that a small gap between the restoration and the tooth structure will be present until the corrosion product fill that space. However, other factors can play a role in the formation of secondary caries which includes, the presence of residual caries, mismanagement of the material and the presence of large gaps between the restoration and the tooth structure (Mjör and Toffenetti, 2000). Bad oral hygiene and failure to educate patients about dental caries and motivate them to change their caries risk might also play a role in the formation of secondary caries (Noaman and Fattah, 2021).
As discussed earlier, fractures in amalgam restorations are related to poor cavity design; mainly inadequate resistance form (Shashank et al., 2010). Fractures could be in the tooth structure or the restoration in-self. Our study data demonstrated that restoration fracture was more prominent (95%) than tooth fracture, and the majority of fractures occur within class 2 on molar teeth. This is in agreement with a previous study which found that class 2 cavity design had lower fractured resistance compared to MOD design (Shashank et al., 2010).
Recently dental composite resin materials developed sufficient mechanical properties that make them suitable for restoring posterior teeth. However, placement of composite resin in posterior teeth is a technique sensitive procedure, and its cost is much higher than amalgam (Bernardo et al., 2007). Poor isolation and mismanagement of the material will lead eventually to failure. In comparison to amalgam restorations, the most prevalent reasons for resin composite restorations replacement or repair were secondary caries and marginal discoloration. This is in agreement with previous studies conducted on the same population (Al Kayed, 1999, Al-Negrish, 2002), and other studies conducted worldwide (Braga et al., 2007, Kopperud et al., 2012). Although composite resin is an adhesive material, secondary caries is still forming at the restoration margins (Bernardo et al., 2007). Furthermore, composite resin restorations are at much higher risk of developing secondary caries compared to amalgam (Lai et al., 2013, Worthington et al., 2021). This is in agreement with our findings were 26% of composite resin restorations were diagnosed with secondary caries compared to 16% for amalgam. This can be explained by many factors that affect the bonding between tooth structure and the composite material leading to micro-leakage which includes; techniques of placement, isolation, type of composite, and bonded substrate. Additionally, some resin-based composite components have the ability to promote bacterial growth which increase the chance of retaining plaque and developing secondary caries (Leinfelder, 2000, Page et al., 1999). This also can explain our findings where patients with poor oral hygiene have more teeth replaced with composite resin restorations (37%) compared to amalgam (28%).
Loss of anatomy was found to be higher in teeth restored with composite resin compared to amalgam. This is in agreement with many researchers reported low wear resistance of most types of posterior composite resin materials (Tsujimoto et al., 2018).
Teeth restored with composite resin had lesser fractures compared to teeth restored with amalgam. All fractures in composite restorations were associated with the material fracture itself rather than tooth fracture. Although most researchers found no difference in fractures development between composite and amalgam (Worthington et al., 2021). Recent research found that fractures of composite resin is 10 time lesser than amalgam (Wong et al., 2021). As stated previously, fractures could also be related to poor cavity design and insufficient resistance form.
More than 55% of replaced amalgam restorations were more than 10 years old compared to 32% of replaced composite resin restorations. Although contradictory findings are found in literature, concerning restoration longevity, amalgam has been reported more often to have lesser failure rate and longer longevity (Antony et al., 2008) compared to composite resin which is in agreement with our findings.
Although it was not easy to identify a particular significant factor for the failure of any restoration since the study is a retrospective one, yet poor oral hygiene was clearly associated with composite resin restorations’ failure while large amalgam restorations were associated with failure more than small ones.
5. Conclusion
With the limitation of this study, we can conclude that:
-
-
The most common reason for amalgam replacement is aesthetic followed by ditching and secondary caries.
-
-
The most common reason for replacing or repairing composite were secondary caries and ditching followed by aesthetic.
-
-
Amalgam restorations had longer longevity, lesser secondary caries, lesser marginal ditching, pain/sensitivity, and lesser loss of anatomy compared to composite resin restorations.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Footnotes
Peer review under responsibility of King Saud University. Production and hosting by Elsevier.
Supplementary data to this article can be found online at https://doi.org/10.1016/j.sdentj.2023.02.003.
Contributor Information
Ayah A Al-Asmar, Email: dr.ayahalasmar@yahoo.com.
Alaa HA Sabrah, Email: sabralolo@yahoo.com.
Islam M Abd-Raheam, Email: islam.raheam@gmail.com.
Noor H Ismail, Email: noor.ismail26@yahoo.com.
Yara G Oweis, Email: yara.oweis@mail.mcgill.co.
Appendix A. Supplementary material
The following are the Supplementary data to this article:
References
- Akbar I. Knowledge and attitudes of general dental practitioners towards posterior composite Restorations in Northern Saudi Arabia. J. Clin. Diagn. Res. 2015;9:61–64. doi: 10.7860/JCDR/2015/11843.5610. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Al Kayed M.A. Reasons and age for replacement of amalgam dental restorations. Dirasat Med. Biol. Sci. 1996;23:128–140. [Google Scholar]
- Al Kayed M.A. A clinical study of placement and replacement for composite restorations in Jordan. Saudi Dent. J. 1999;11:53–59. [Google Scholar]
- Alanazi A.M., Mian R.I., Alshammari M.S., Al Ibrahim I.K., Alnasrallah F.A., Alshammar A.S. Evaluating the trends for restorative treatment, reasons and management of failures in general dental practices of hail region, Saudi Arabia. Dent. Res. Manag. 2019;3:9–12. [Google Scholar]
- Al-Asmar A.A., Al-Khatib K.M., Al-Amad T.Z., Sawair F.A. Has the implementation of the Minamata convention had an impact on the practice of operative dentistry in Jordan? J. Inter. Med. Res. 2019;47:361–369. doi: 10.1177/0300060518802523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Al-Negrish A.R. Reasons for placement and replacement of amalgam restorations in Jordan. Int. Dent. J. 2001;51:109–115. doi: 10.1002/j.1875-595x.2001.tb00831.x. [DOI] [PubMed] [Google Scholar]
- Al-Negrish A.R. Composite resin restorations: a cross-sectional survey of placement and replacement in Jordan. Int. Dent. J. 2002;52:461–468. doi: 10.1111/j.1875-595x.2002.tb00643.x. [DOI] [PubMed] [Google Scholar]
- Al-Rabab’ah, M.A., Bustani, M.A., Khraisat, A.S., Sawair, F.A., 2016. Phase down of amalgam; Awareness of Minamata convention among Jordanian dentists. Saudi Med. J. 37, 1381-1386 [DOI] [PMC free article] [PubMed]
- Antony, K., Genser, D., Hiebinger, C., Windisch, F., 2008. Longevity of dental amalgam in comparison to composite materials. GMS. Health. Technol. Assess. 13, Doc12. [PMC free article] [PubMed]
- Arotiba G.T., Ijarogbe O.A., Awotile A.O., Loto O.A., Menakaya I., Umesi D.C., Ajayi Y., Ukpong M.O., Otoh E.C., Adogame L. Accelerating the phase down of dental amalgam in Africa and developing economies: a ‘Leapfrogging’ strategy. J. Oral Health Dent. Sci. 2020;4:1–7. [Google Scholar]
- Bernardo M., Luis H., Martin M.D., Leroux B.G., Rue T., Leitao J., DeRouen T.A. Survival and reasons for failure of amalgam versus composite posterior restorations placed in a randomized clinical trial. J. Am. Dent. Assoc. 2007;138:775–783. doi: 10.14219/jada.archive.2007.0265. [DOI] [PubMed] [Google Scholar]
- Braga S.R., Vasconcelos B.T., de Paula Macedo M.R., Geraldo Martins V.R., Pita Sobral M.A. Reasons for placement and replacement of direct restorative materials in Brazil. Quintessence Int. 2007;38:189–194. [PubMed] [Google Scholar]
- Chan K., Mai Y., Kim H., Tong K., Desmond N., Hsiao J. Review: resin composite filling. Materials. 2010;3:1228–1243. [Google Scholar]
- Eltahlaha D., Lynch C.D., Chadwick B.L., Blum I.R., Wilson N.H.F. An update on the reasons for placement and replacement of direct restorations. J. Dent. 2018;72:1–7. doi: 10.1016/j.jdent.2018.03.001. [DOI] [PubMed] [Google Scholar]
- Faraj B.M., Mohammad H.M., Mohammad K.M. The changes in dentists’ perception and patient’s acceptance on amalgam restoration in Kurdistan-Iraq: a questionnaire-based cross-sectional study. J. Clin. Diagn. Res. 2015;9:22–25. doi: 10.7860/JCDR/2015/13028.5790. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fejerskov O. Concepts of dental caries and their consequences for understanding the disease. Community Dent. Oral. Epidemiol. 1997;25:5–12. doi: 10.1111/j.1600-0528.1997.tb00894.x. [DOI] [PubMed] [Google Scholar]
- Fisher J., Varenne B., Narvaezc D., Vickers C. The Minamata Convention and the phase down of dental amalgam. Bull. World Health Organ. 2018;96:436–438. doi: 10.2471/BLT.17.203141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gordan V.V., Riley J.L., Geraldeli S., Rindal D.B., Qvist V., Fellows J.L., Kellum H.P., Gilbert G.H. DPBRN Collaborative Group. Repair or replacement of defective restorations by dentists in The Dental PBRN. J. Am. Dent. Assoc. 2012;143:593–601. doi: 10.14219/jada.archive.2012.0238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haque N., Yousaf S., Nejatian T., Youseffi M., Mozafari M., Sefat F. In: Advanced Dental Biomaterials. Khurshid Z., Najeeb S., Zafar M.S., Sefat F., editors. Woodhead Publishing; 2019. Dental amalgam; pp. 105–125. [Google Scholar]
- Kelleher M. The “daughter test” in aesthetic (esthetic) or cosmetic dentistry. Dent. Update. 2010;37:5–11. [PubMed] [Google Scholar]
- Kimyai S., Mehdipour M., Oskoee S.S., Oskoee P.A., Abbaszadeh A. Reasons for retreatment of amalgam and composite restorations among the patients referring to Tabriz faculty of dentistry. J. Dent. Res. Dent. Clin. Dent. Prospects. 2007;1:27–32. doi: 10.5681/joddd.2007.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kopperud S.E., Tveit A.B., Garden T., Sandvik L., Espelid I. Longevity of posterior dental restorations and reasons for failure. Eur. J. Oral. Sci. 2012;120:539–548. doi: 10.1111/eos.12004. [DOI] [PubMed] [Google Scholar]
- Lai G.Y., Zhu L.K., Li M.Y., Wang J. An in vitro study on the secondary caries-prevention properties of three restorative materials. J. Prosthet. Dent. 2013;110:363–368. doi: 10.1016/j.prosdent.2013.06.011. [DOI] [PubMed] [Google Scholar]
- Leinfelder K.F. Do restorations made of amalgam outlast those made of resin-based composite? J. Am. Dent. Assoc. 2000;131:1186–1187. doi: 10.14219/jada.archive.2000.0355. [DOI] [PubMed] [Google Scholar]
- Magalhaes C.S., Aniceto de Freitas A.B., Moreira A.N., Ferreira E.F. Validity of staining and marginal ditching as criteria for diagnosis of secondary caries around occlusal amalgam restorations: an in vitro study. Braz. Dent. J. 2009;20:307–313. doi: 10.1590/s0103-64402009000400008. [DOI] [PubMed] [Google Scholar]
- Mahajan V., Bhondwe S., Doot R., Balpande R., Bhandari S., Dahiwale S. Failure in composite restoration. Inter. J. Dent. Res. 2015;3:10–14. [Google Scholar]
- Mendiratta M., Manjunath B.C., Kumar A., Yadav V., Wig M., Kumar A. Minimal invasive dentistry: a narrative review. Eur. J. Mol. Clin. Med. 2021;8:3167–3179. [Google Scholar]
- Mjör I.A., Toffenetti F. Secondary caries: a literature review with case reports. Quintessence Int. 2000;31:165–179. [PubMed] [Google Scholar]
- Montagner A.F., van de Sande F.H., Müller C., Cenci M.S., Susin A.H. Survival, reasons for failure and clinical characteristics of anterior/posterior composites: 8-year findings. Braz. Dent. J. 2018;29:547–554. doi: 10.1590/0103-6440201802192. [DOI] [PubMed] [Google Scholar]
- Noaman B.R., Fattah L.D. The relationship of caries risk and oral hygiene level with placement and replacement of dental restorations. Acta Med. Acad. 2021;50:406–413. doi: 10.5644/ama2006-124.362. [DOI] [PubMed] [Google Scholar]
- Olaleye A.O., Shaba O.P. Treatment and failure of amalgam restoration analyzed according to class of restoration. J. Dent. Probl. Solut. 2020;7:84–89. [Google Scholar]
- Page J., Welbury R.R. In: Pediatric Dentistry. 3rd ed. Welbury R.R., editor. Oxford University Press; Oxford: 1999. Operative treatment of dental caries; pp. 121–123. [Google Scholar]
- Pouralibaba F., Joulaei M., Kashefimehr A., Pakdel F., Jamali Z., Esmaeili A. Clinical evaluation of reasons for replacement of amalgam restorations in patients referring to a dental school in Iran. J. Dent. Res. Dent. Clin. Dent. Prospects. 2010;4:56–59. doi: 10.5681/joddd.2010.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shashank K., Chole D.G., Ranga B. An evaluation of the fracture resistance of class 2 amalgam restorations with different cavity designs on maxillary premolars. J. Inter. Clin. Dent. Res. Organ. 2010;2:70–74. [Google Scholar]
- Shenoy A. Is it the end of the road for dental amalgam? a critical review. J. Conserv. Dent. 2008;11:99–107. doi: 10.4103/0972-0707.45247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Silvani S., Trivelato R.F., Nogueira R.D., Gonçalves L., Geraldo-Martins V.R. Factors affecting the placement or replacement of direct restorations in a dental school. Contemp. Clin. Dent. 2014;5:54–58. doi: 10.4103/0976-237X.128664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Talabani R.M. Placement and reasons for failure of amalgam versus composite posterior restorations for patient attending to dental school. Int. J. Dev. Res. 2015;5:5059–5064. [Google Scholar]
- Tsujimoto A., Barkmeier W.W., Fischer N.G., Nojiri K., Nagura Y., Takamizawa T., Latta M.A., Miazaki M. Wear of resin composites: current insights into underlying mechanisms, evaluation methods and influential factors. Jpn. Dent. Sci. Rev. 2018;54:76–87. doi: 10.1016/j.jdsr.2017.11.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walsh L.J., Brostek A.M. Minimum intervention dentistry principles and objectives. Aust. Dent. J. 2013;58:3–16. doi: 10.1111/adj.12045. [DOI] [PubMed] [Google Scholar]
- Wong V.Y.Y., Chua Y.K., Jr, Koh H., Low K.M.T. A retrospective cross-sectional study of early patient-reported failures of direct restorations placed in a primary dental care setting. Br. Dent. J. 2021;231:43–48. doi: 10.1038/s41415-021-3166-x. [DOI] [PubMed] [Google Scholar]
- Worthington H.V., Khangura S., Seal K., Mierzwinski-Urban M., Veitz-Keenan A., Sahrmann P., Schmidlin P.R., Davis D., Iheozor-Ejiofor Z., Rasines Alcaraz M.G. Direct composite resin fillings versus amalgam fillings for permanent posterior teeth. Cochrane Database Syst. Rev. 2021;13(8):CD005620. doi: 10.1002/14651858.CD005620.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.