Abstract
We performed this study to determine if bilateral internal thoracic artery grafts provide greater benefit than single internal thoracic artery grafts. Six hundred ninety-four consecutive patients who received 2 coronary grafts in a single operation during 1983–1989 were given 10 years of follow-up and then analyzed retrospectively.
Group 1 (n=382) received 2 internal thoracic artery grafts, Group 2 (n=139) received 1 internal thoracic artery graft and 1 saphenous vein graft, and Group 3 (n=173) received 2 saphenous vein grafts. Patient demographics, preoperative angiographic findings, and operative indications were the same.
Hospital mortality rates were 2.6%, 2.2%, and 2.3%, respectively. Hemorrhage, sternal wound infection, mediastinitis, sternal dehiscence, and prolonged ventilatory support showed no group differences. Follow-up over 10 years was complete in 677 survivors. Mortality rates during follow-up were 1.8%, 2.9%, and 4.7%, respectively. Cardiac-related mortality rates were 71%, 75%, and 88%, respectively (Group 1 vs Group 3, P=0.0412). Ten-year survival was better for Group 1 than for Groups 2 and 3 (P=0.0356 and P <0.0001). Cardiac-event-free survival at 10 years was 93% in Group 1, 84% in Group 2, and 74% in Group 3 (all P <0.0001).
The use of 2 internal thoracic artery grafts resulted in significantly lower risk of cardiac death and re-intervention, compared with the use of 1 internal thoracic artery, which in turn was superior to the use of vein grafts. Use of double internal thoracic arteries did not increase postoperative complications.
Key words: Coronary artery bypass, internal thoracic artery, myocardial revascularization, retrospective studies, saphenous vein grafts, survival analysis, survival rate, treatment outcome
The use of 1 internal thoracic artery (ITA) as a conduit in myocardial revascularization (CABG) has become standard at most cardiac centers, because of the ITA's superiority over saphenous vein grafts in regard to long-term patency, patient survival, and the frequency of cardiac-related events and re-intervention. 1–6 To optimize the positive benefits of the ITA graft, this conduit has also been used with good results as a sequential bypass graft for revascularization of the anterolateral part of the heart. 5,7 The outcomes achieved with ITA grafts in these applications, when compared with vein-graft outcomes, heightened interest in using ITA grafts bilaterally. 8
However, many conflicting reports have led to confusion. On the negative side, several investigators reported higher frequency of sternal infection, reoperation for hemorrhage, prolonged ventilatory support, 9,10 and even increased mortality, 2 when double ITA grafts were used. Skepticism was strengthened by reports of failure to demonstrate additional survival advantages, when the use of 2 ITA grafts was compared with the use a single ITA. 3,9,11,12 On the other hand, some investigators reported additional benefits when 2 ITA grafts were used. 13,14 Possible reasons for these conflicting data are short follow-up periods and small patient populations. In a recent study, Lytle and associates 15 from Cleveland Clinic demonstrated in a large patient population over the course of a 15-year follow-up period that patients who received 2 ITA grafts had a lower risk of death, reoperation, and angioplasty than did those who received a single ITA graft.
In our present retrospective study, we report our experience, with 10 years of follow-up, in 694 patients who underwent CABG with the use of 2 ITA grafts, or 1 ITA and 1 saphenous vein graft, or 2 saphenous vein grafts.
Patients and Methods
In search of the optimal surgical strategy for patients undergoing primary surgical myocardial revascularization, we evaluated the effects upon long-term outcome of double and single internal thoracic artery bypass grafts.
Our study design called for 3 consecutive series of patients who had required at least 2 coronary artery bypass grafts. For the necessary retrospective analysis, patients had to have undergone at least 10 years of postoperative follow-up. Group 1 patients received 2 ITA grafts, Group 2 received 1 ITA and 1 saphenous vein graft, and Group 3 received 2 saphenous vein grafts without any arterial grafts. To avoid selecting patients, we chose to examine the records of consecutive patients from the following periods: Group 1 patients had undergone operation from the end of 1984 through mid-1989, Group 2 patients from mid-1984 through the end of 1985, and Group 3 patients during 1983 and the beginning of 1984. Throughout this entire period, techniques for anesthesia and cardiopulmonary bypass were not changed at our institution. Preoperative patient characteristics, angiographic findings, and operative data were collected and analyzed to ensure that the study groups were comparable.
The study's primary end-points were hospital mortality, postoperative complications, long-term survival, and cardiac-event-free survival. Hospital mortality (death within 30 postoperative days) and postoperative complications were analyzed for each group. During the follow-up period, deaths (both cardiac and noncardiac), re-interventions (whether redo CABG, percutaneous transluminal coronary angioplasty [PTCA], or both), and symptomatic myocardial infarction were recorded. Cumulative survival and cardiac-event-free survival rates were calculated.
Because coronary control angiography was not performed routinely during the study period, complete records concerning graft patency were unavailable. However, at redo CABG and PTCA, the patency of ITA and saphenous vein grafts was analyzed, which yielded some indication of patency rates for the different graft materials.
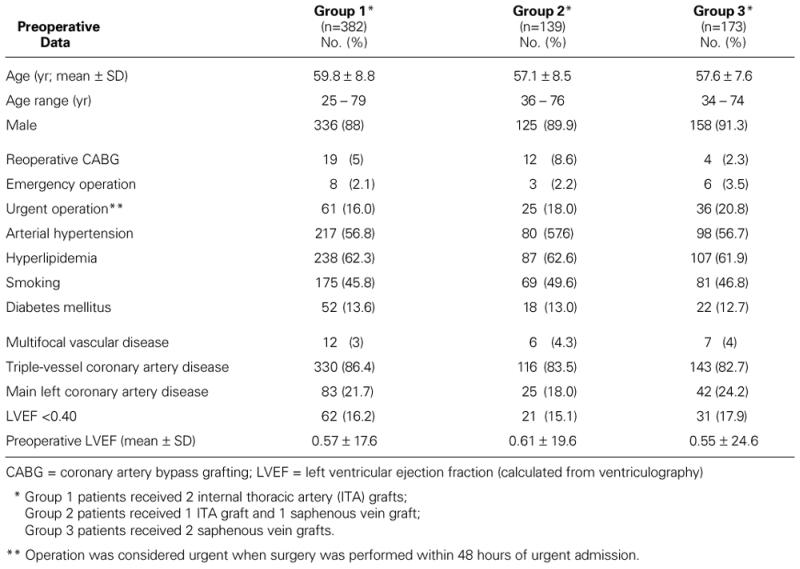
Preoperative patient characteristics and preoperative angiographic findings are summarized in Table I. In comparing each group with the others, we found no statistically significant differences in any of the parameters, except for a lower mean preoperative left ventricular ejection fraction (LVEF) (P=0.0001) in Group 1 and 3 patients, when compared with Group 2 patients. Other than that, the groups were indeed comparable.
TABLE I. Preoperative Data in 3 Groups of Patients* Undergoing Coronary Artery Bypass Grafting
Surgical Data.
All patients underwent operation through a median sternotomy with cardiopulmonary bypass (CPB) support at a moderate hypothermic (28°C) level. Myocardial protection was achieved by antegrade, intermittent administration of cold St. Thomas's cardioplegic solution and by cardiac cooling with ice slush. There were no group differences in operative parameters, except with regard to the conduits used. The ITA conduits were prepared as pedicled grafts.
Statistical Analysis.
All statistical analyses were performed using StatView software, version 4.5 (Abacus Concepts; Berkeley, Calif). Student's t-test (1-sample paired test), the Mann-Whitney test, and the Fisher exact test were used to examine the differences between groups for statistical significance, where appropriate. A probability level of P <0.05 was regarded as significant. Nonparametric estimates of survival (avoidance of death from any cause, both in the hospital and after discharge) and of cardiac-event-free survival (avoidance of death, together with freedom from myocardial infarction or cardiac re-intervention such as redo CABG and PTCA) were calculated for each group by the Kaplan-Meier method.
Results
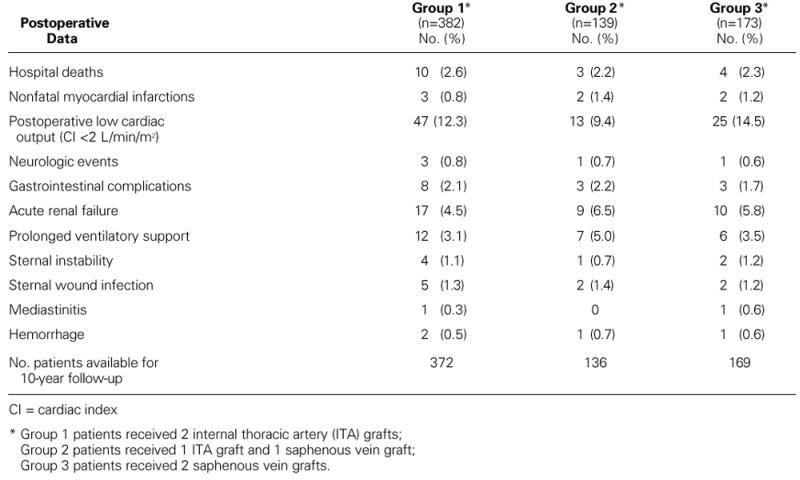
Postoperative complications in the 3 groups are listed in Table II. The hospital mortality rates were 2.6%, 2.2%, and 2.3%, respectively. There were no statistically significant differences in any of the postoperative parameters when each group was compared with each of the others.
TABLE II. Postoperative Data in 3 Groups of Patients* Undergoing Coronary Artery Bypass Grafting
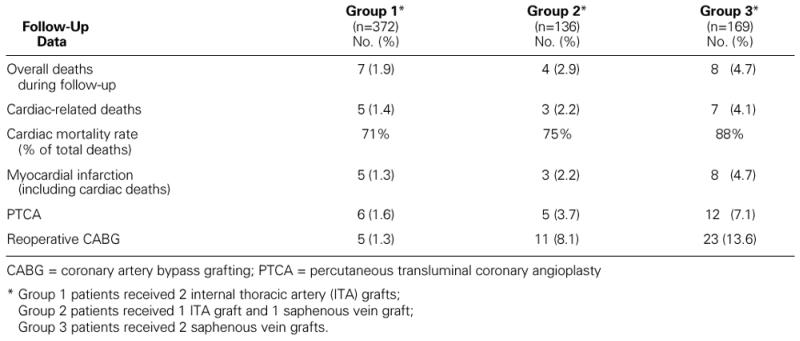
Follow-up over 10 years was complete in 677 out of 694 hospital survivors, leaving only 17 patients (2.5%) lost to follow-up. The patients lost to follow-up were equally distributed among the groups. Some follow-up results are summarized in Table III. The overall mortality rates during follow-up were 1.8% (Group 1), 2.9% (Group 2), and 4.7% (Group 3), without statistically significant differences. Cardiac related mortality rates were 1.4%, 2.2% and 4.1% respectively, and here Group 1 showed a statistically significant (P=0.0412) reduction in mortality when compared with Group 3. Redo CABG and PTCA occurred more frequently in Groups 2 and 3 than in Group 1 (P <0.0001), and redo CABG was required more often in Group 2 than in Group 1 (P <0.0001) (Table III). When all cardiac events that occurred during follow-up (cardiac death, redo CABG, PTCA, and instances of myocardial infarction not related to interventions) were totaled, Group 1 showed significant superiority to Group 2 (P <0.0001), and patients in Group 2 demonstrated significantly fewer cardiac events than did patients in Group 3 (P <0.0001).
TABLE III. Follow-Up Data during the 10-Year Follow-Up after CABG in 3 Groups of Patients*
Survival and Cardiac-Event-Free Survival.
Early cumulative survival rates were similar for all 3 groups, but at 10 years, survival was best in Group 1, in comparison with Groups 2 and 3 (P=0.0356 and P <0.0001, respectively). Cardiac-event-free survival at 10 years also showed highly significant differences between the groups: 92.6% in Group 1, 83.5% in Group 2, and 74.4% in Group 3 (all group comparisons resulted in P <0.0001) (Fig. 1).
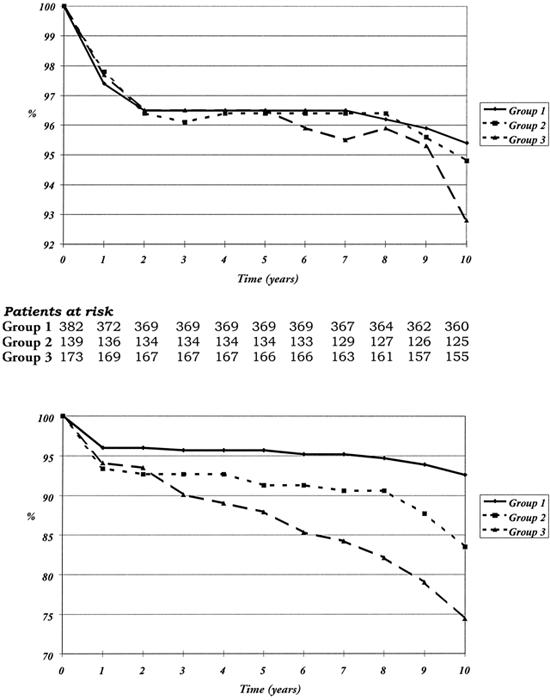
Fig. 1 Comparison of patients who underwent myocardial revascularization with 2 ITA grafts (Group 1), 1 ITA plus 1 vein graft (Group 2), and only vein grafts (Group 3) in terms of A) cumulative survival and B) cumulative cardiac-event-free survival. The numbers of patients at risk during each interval of follow-up are listed between the figures.
Mortality Analysis.
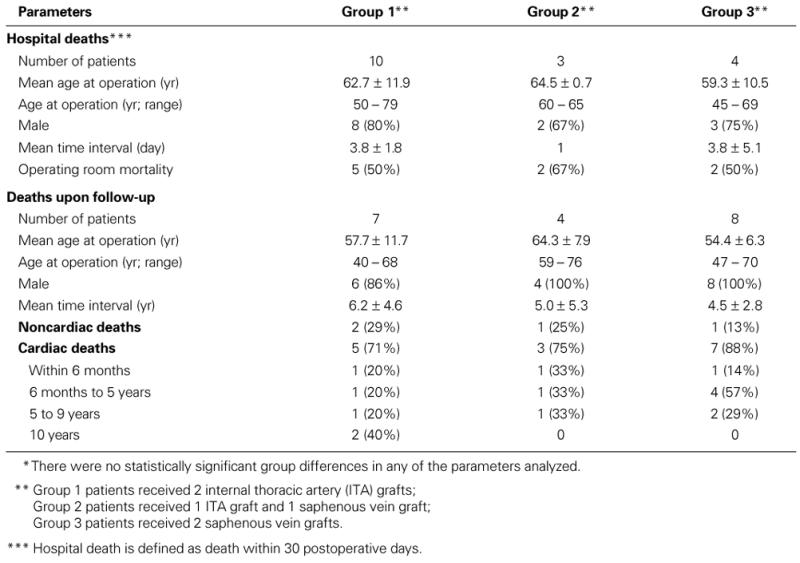
Both hospital deaths and deaths occurring during the follow-up period are summarized in Table IV. As a consequence of the small numbers, no statistically significant group differences were found, but there was a clear trend in Group 1 towards later death, when compared with Group 3.
TABLE IV. Analysis of Mortality Rates* after Coronary Artery Bypass Grafting Using Different Bypass Conduits
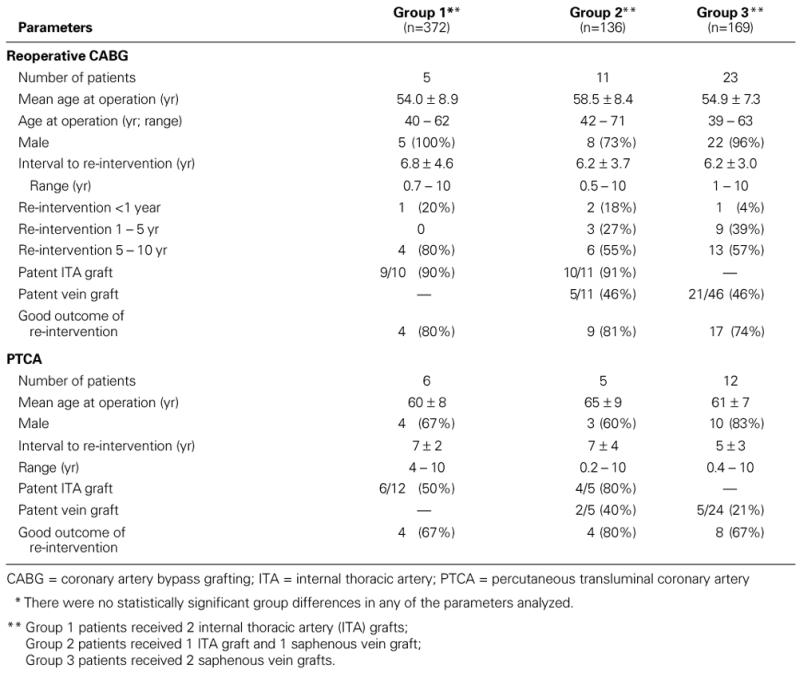
Re-Interventions.
Among patients who needed reoperative CABG during the follow-up period, Group 1 patients also demonstrated a trend towards a much longer delay before redo CABG became necessary, when compared with their counterparts in Group 3 (Table V). Strikingly, at redo CABG, 90% of the ITA grafts were patent, which indicated general progression of the disease rather than conduit failure; conversely, vein graft patency was only 46%, which indicated progression of disease within the conduit itself, in addition to the general progression that could be expected during the course of a decade. Findings were similar for patients who required PTCA as intervention during follow-up (Table V).
TABLE V. Analysis of Re-Interventions* during 10 Years' Follow-Up of Coronary Artery Bypass Grafting
Discussion
Excellent clinical results in patients undergoing myocardial revascularization with single ITA grafts (compared with saphenous vein grafts) have prompted surgeons to use bilateral ITA grafts. 3,8,9 Despite longer aortic occlusion times and slightly longer CPB times among patients who received 2 ITA grafts, Pick's group 14 did not observe any important differences in perioperative mortality and morbidity rates when these patients were compared with those who had received only 1 ITA graft. These findings correspond with our results in the present study.
Even though several reports have shown a significantly diminished reoperation rate and fewer cardiac-related events when double ITA grafts were used (compared with single ITA grafts), 3,4,12 other investigators have described higher frequency of sternal infections and reoperations for hemorrhage. 2,10 Particularly in patients with insulin-dependent diabetes, bilateral ITA grafts have been associated with a dramatic increase in sternal wound infections. 6,16 However, Uva and co-authors 17 recently reported their experience of double ITA myocardial revascularization in young patients with diabetes, which was accomplished without increased morbidity or mortality. This observation is similar both to our findings and to those recently reported by the Cleveland Clinic group, 15 which showed that the slightly increased rate of sternal wound infections in diabetic patients who received bilateral ITA grafts was negligible when compared with the corresponding sternal wound infection rate that they observed after single ITA grafting. These findings are important because diabetes is a major independent risk factor for coronary atherosclerosis: patients with diabetes are at higher risk than the general population for both myocardial infarction and more extensive coronary artery disease. 18 In patients with diabetes who have multiple-vessel disease, PTCA usually yields less complete revascularization than does surgery.
Several groups 2,9,12,14,19 have attempted to determine whether double ITA grafting results in better long-term survival than does single ITA grafting, but their efforts have failed to show increased survival rates with double ITA after 5 years. However, all these studies have shown that patients with double ITA grafts had significantly fewer complications of ischemic heart disease during follow-up than did those with only 1 ITA graft. This reduction in cardiac-related events further supports the hypothesis that use of 2 ITA grafts decreases late cardiac deaths, compared with use of 1 ITA. 4,9,11,12
One important issue in investigating the benefits of double ITA grafting, compared with single, is that of patient selection. Patients of advanced age (>70 years), women, and patients with insulin-dependent diabetes are less likely to receive double ITA grafts. 15 In the present report, there were no differences between the study groups in regard to these or any other parameters that would seriously bias patient selection. It should be emphasized that during the period when patients in this study underwent operation, the indications for using double ITA grafts were very liberal. One limitation of our study is that it was a retrospective, nonrandomized study of consecutive patients who underwent myocardial revascularization at 1 institution. On the other hand, our study groups were directly comparable to one another, with no differences regarding preoperative patient characteristics, preoperative angiographic findings, or operative data. A 2nd limitation was the absence of routine follow-up angiography, which precluded analysis of graft patency rates. However, our survival data (particularly in regard to the impact of cardiac death), together with cardiac-event-free survival rates for the 3 study groups, directly imply good conduit function in the long term, even though other factors, such as completeness of revascularization and subsequent progression of native vessel disease, also have an important impact on these indicators. 8
The duration of follow-up and the number of patients studied are other potential limiting factors in evaluating the impact of double and single ITA grafts on long-term survival rates. The lack of evidence that bilateral ITA grafting affords better long-term survival than does single ITA grafting has been the main argument used by the opponents of multiple arterial revascularization.
In their recent study, Lytle and coworkers 15 used multiple statistical strategies to evaluate the records of more than 10,000 patients who had received either single or bilateral ITA grafts, and whose cases had been followed for as long as 20 years. In so doing, they proved beyond doubt that patients who received 2 ITA grafts demonstrated decreased risks of death, reoperation, and angioplasty, when compared with those who had only 1 ITA graft. 15 A European study done in a similar fashion, 19 also with a large number of patients, had failed to show an advantage of double ITA over single ITA grafting with regard either to survival or to reoperation-free survival. Lytle and colleagues 15 speculated that this conflicting outcome could be attributed to differences between the European and American medical environments, in customary indications both for primary bypass surgery and for reintervention. However, the present study from a European cardiac center shows results very similar to those reported by Lytle's group. 15 Although our experience was drawn from a smaller number of patients, all of our patients underwent careful follow-up over the course of 10 years.
We have shown clearly that the strategy of bilateral ITA grafting has a significant effect at 10 years on lowering both mortality and re-intervention rates (whether CABG or PTCA), when compared with the rates observed when single ITA grafts are used as bypass conduits, together with saphenous vein grafts (P <0.0001). It was shown, furthermore, that both survival and cardiac-event-free survival were significantly better when 1 ITA graft was used in combination with saphenous vein grafts, than when only vein grafts were used for myocardial revascularization. Because double ITA grafting does not increase postoperative morbidity, its choice constitutes the optimal surgical strategy in patients undergoing primary CABG.
Footnotes
Address for reprints: Dr. Jan T. Christenson, Clinic for Cardiovascular Surgery, Department of Surgery, University Hospital, 24 av. Micheli-du-Crest., CH-1211 Geneva 14, Switzerland
References
- 1.Loop FD, Irarrazaval MJ, Bredee JJ, Siegel W, Taylor PC, Sheldon WC. Internal mammary artery graft for ischemic heart disease. Effect of revascularization on clinical status and survival. Am J Cardiol 1977;39:516–22. [DOI] [PubMed]
- 2.Barner HB, Standeven JW, Reese J. Twelve-year experience with internal mammary artery for coronary artery bypass. J Thorac Cardiovasc Surg 1985;90:668–75. [PubMed]
- 3.Galbut DL, Traad EA, Dorman MJ, DeWitt PL, Larsen PB, Kurlansky PA, et al. Seventeen-year experience with bilateral internal mammary artery grafts. Ann Thorac Surg 1990; 49:195–201. [DOI] [PubMed]
- 4.Loop FD, Lytle BW, Cosgrove DM, Stewart RW, Goormastic M, Williams GW, et al. Influence of the internal-mammary-artery graft on 10-year survival and other cardiac events. N Engl J Med 1986;314:1–6. [DOI] [PubMed]
- 5.Dion R, Verhelst R, Rousseau M, Goenen M, Ponlot R, Kestens-Servaye Y, et al. Sequential mammary grafting. Clinical, functional, and angiographic assessment 6 months postoperatively in 231 consecutive patients. J Thorac Cardiovasc Surg 1989;98:80–9. [PubMed]
- 6.Grondin CM, Campeau L, Lesperance J, Enjalbert M, Bourassa MG. Comparison of late changes in internal mammary artery and saphenous vein grafts in two consecutive series of patients 10 years after operation. Circulation 1984;70(3 Pt 2):I208–12. [PubMed]
- 7.Christenson JT, Bucher E, Velebit V, Simonet F, Schmuziger M. Sequential internal mammary artery conduits in coronary artery bypass grafting. Med Principles Pract 1994–95;4:189–96.
- 8.Cosgrove DM, Lytle BW, Loop FD, Taylor PC, Stewart RW, Gill CC, et al. Does bilateral internal mammary artery grafting increase surgical risk? J Thorac Cardiovasc Surg 1988;95:850–6. [PubMed]
- 9.Fiore AC, Naunheim KS, Dean P, Kaiser GC, Pennington G, Willman VL, et al. Results of internal thoracic artery grafting over 15 years: single versus double grafts. Ann Thorac Surg 1990;49:202–9. [DOI] [PubMed]
- 10.Kouchoukos NT, Wareing TH, Murphy SF, Pelate C, Marshall WG. Risks of bilateral internal mammary artery bypass grafting. Ann Surg 1990;49:210–9. [DOI] [PubMed]
- 11.Naunheim KS, Barner HB, Fiore AC. 1990: Results of internal thoracic artery grafting over 15 years: single versus double grafts. 1992 update. Ann Thorac Surg 1992;53:716–8. [DOI] [PubMed]
- 12.Dewar LR, Jamieson WR, Janusz MT, Adeli-Sardo M, Germann E, MacNab JS, Tyers GF. Unilateral versus bilateral internal mammary revascularization. Survival and event-free performance. Circulation 1995;92(9 Suppl):II8–13. [DOI] [PubMed]
- 13.Carrel T, Horber P, Turina MI. Operation for two-vessel coronary artery disease: midterm results of bilateral ITA grafting versus unilateral ITA and saphenous vein grafting. Ann Thorac Surg 1996;62:1289–94. [DOI] [PubMed]
- 14.Pick AW, Orszulak TA, Anderson BJ, Schaff HV. Single versus bilateral internal mammary artery grafts: 10 year outcome analysis. Ann Thorac Surg 1997;64:599–605. [DOI] [PubMed]
- 15.Lytle BW, Blackstone EH, Loop FD, Houghtaling PL, Arnold JH, Akhrass R, et al. Two internal thoracic artery grafts are better than one. J Thorac Cardiovasc Surg 1999; 117:855–72. [DOI] [PubMed]
- 16.Grossi EA, Esposito R, Harris LJ, Crooke GA, Galloway AC, Colvin SB, et al. Sternal wound infections and use of internal mammary artery grafts. J Thorac Cardiovasc Surg 1991;102:342–7. [PubMed]
- 17.Uva MS, Braunberger E, Fisher M, Fromes Y, Deleuze PH, Celestin JA, Bical OM. Does bilateral internal thoracic artery grafting increase surgical risk in diabetic patients? Ann Thorac Surg 1998;66:2051–5. [DOI] [PubMed]
- 18.Webster MW, Scott RS. What cardiologists need to know about diabetes. Lancet 1997;350(Suppl 1):SI23–8. [DOI] [PubMed]
- 19.Sergeant P, Blackstone E, Meyns B. Validation and interdependence with patient-variables of the influence of procedural variables on early and late survival after CABG. K. U. Leuven Coronary Surgery Program. Eur J Cardiothorac Surg 1997;12:1–19. [DOI] [PubMed]


