Abstract
Objective:
Previous studies have examined whether spiritual well-being is associated with cancer outcomes, but minority populations are under-represented. This study examines associations of baseline spiritual well-being and change in spiritual well-being with change in distress and quality of life, and explores potential factors associated with changes in spiritual well-being among Hispanic women undergoing chemotherapy.
Methods:
Participants completed measures examining spiritual well-being, distress, and quality of life prior to beginning chemotherapy and at weeks 7 and 13. Participants’ acculturation and sociodemographic data were collected prior to treatment. Mixed models were used to examine the association of baseline spiritual well-being and change in spiritual well-being during treatment with change in distress and quality of life, and to explore whether sociodemographic factors, acculturation and clinical variables were associated with change in spiritual well-being.
Results:
A total of 242 participants provided data. Greater baseline spiritual well-being was associated with less concurrent distress and better quality of life (p < 0.001), as well as with greater emotional and functional well-being over time (p values < 0.01). Increases in spiritual well-being were associated with improved social well-being during treatment, whereas decreases in spiritual well-being were associated with worsened social well-being (p < 0.01). Married participants reported greater spiritual well-being at baseline relative to non-married participants (p < 0.001).
Conclusions:
Greater spiritual well-being is associated with less concurrent distress and better quality of life, as well as with greater emotional, functional, and social well-being over time among Hispanic women undergoing chemotherapy. Future work could include developing culturally targeted spiritual interventions to improve survivors’ well-being.
Keywords: cancer, chemotherapy, Hispanic, oncology, quality of life, spirituality
Spiritual well-being is a multidimensional concept defined as “meaning, wholeness, transcendence, connection, joy and peace, that do not rely on one’s participation in an organized religion.”1 For research purposes, spiritual well-being is commonly operationalized as a combination of meaning, peace, faith.2 Spiritual well-being is important for up to 70%–90% of patients with cancer.3 Many patients, particularly older women,4 report increased spiritual well-being and religious identification after cancer diagnosis.5 Patients often find in spiritual well-being a resource to cope, adapt, and manage cancer.6,7 There has been increasing interest in understanding how spiritual well-being and its components relate to other aspects of cancer patients’ well-being. For example, a series of meta-analyses concluded that spiritual well-being is associated with better patient-reported physical, social and mental well-being.8–10 Interestingly, these associations were not moderated by demographic or clinical variables and the role of spiritual well-being dimensions varied as a function of the domains assessed. However, these meta-analyses were characterized by mostly cross-sectional studies and under-representation of minority populations.
Hispanics are the largest ethnic group minority in the United States, comprising 18% of the population in 2019.11 Projections estimate that the proportion of Hispanics among the United States population will increase to 29% by 2060.12 Cancer is the leading cause of death among Hispanics,13 who are often diagnosed at advanced stages14 and experience more treatment-related symptoms relative to other ethnicities. For example, Hispanic women with breast cancer experience more symptoms of depression and anxiety, fear of cancer recurrence, fatigue, pain, sleep problems and nausea relative to their non-Hispanic counterparts.15,16 It is not surprising therefore that Hispanic women with breast cancer also report worse quality of life compared to non-Hispanic White women with breast cancer.15,17
Data suggest that Hispanic patients identify spiritual well-being as a key resource for coping with cancer and its treatment18,19 and do so more often than non-Hispanic Whites.20,21 Less is known about how acculturation contributes to quality of life and spirituality in this population. Some studies suggest that low acculturation is associated with anxiety and depression,22 poor mental health,15 and poor social, functional and emotional well-being,23 but not with spiritual well-being, among Hispanic women with cancer.18 However, another study has found that lower acculturation is associated with better mental health in Hispanic women with breast cancer relative to their White Hispanic counterparts.24 Nevertheless, acculturation has been mostly measured in cross-sectional studies by language preference (i.e., English vs. Spanish) and thus, failed to capture other components informing the extent of the integration into the social structure of the majority group (i.e., media preferences, ethnic social relations).25
This study examines spiritual well-being, quality of life, and distress over time among Hispanic women receiving chemotherapy. The goals of the current paper were twofold. The first goal was to examine associations of baseline spiritual well-being and change in spiritual well-being with change in distress (i.e., depression, anxiety) and quality of life (i.e., physical, social, emotional, functional well-being) over time. The second goal was to explore factors associated with baseline spirituality and change in spirituality over time from among sociodemographic factors, acculturation, and clinical factors. We hypothesized that greater baseline spiritual well-being and change in spiritual well-being would be associated with less depression and anxiety and better quality of life.
1 |. METHODS
1.1 |. Participants
Patients were recruited from the Moffitt Cancer Center in Tampa, Florida, and the University of Miami Comprehensive Cancer Center in Miami, Florida between March 2012 and August 2016. Eligible patients were (1) females diagnosed with cancer, (2) ≥18 years of age, (3) self-identified as Hispanic, (4) able to speak and read Spanish, (5) scheduled to begin outpatient intravenous chemotherapy for reasons other than palliation, and (6) able to sign written informed consent. Patients who had received chemotherapy in the past 2 months or had observable visual, auditory, psychiatric, or neurological disorders that could interfere with the study were excluded.
1.2 |. Procedures
Potential participants were identified through electronic medical records in collaboration with their medical oncologists. Participants completed the baseline assessment prior to beginning chemotherapy; follow-up assessments were conducted at weeks 7 and 13. The study was approved by the Institutional Review Boards at the University of South Florida (Pro00006699) and University of Miami (20111145).
1.3 |. Measures
Participants self-reported sociodemographic information at baseline, including age, race, marital status, education, annual household income, employment, years residing in the United States, and country of birth. Clinical data such as diagnosis, disease stage and months since diagnosis were abstracted from medical records.
Spiritual well-being was assessed with the validated Spanish-language version26 of Functional Assessment of Chronic Illness Therapy-Spiritual Well-Being Scale (FACIT-Sp).2 The FACIT-Sp is a 12-item scale measuring spiritual well-being as well as meaning/peace and faith in cancer patients. Items are scored on a 0 to 4 scale. Higher scores indicate greater spiritual well-being.
Psychological distress was assessed using the validated Spanish-language version27 of the Hospital Anxiety and Depression Scale (HADS).28 The HADS is a 14-item scale assessing depression and anxiety symptomatology. Items are scored on a 0 to 3 scale. Scores higher than 7 indicate symptoms of depression and/or anxiety.
Quality of life was examined using the validated Spanish-language version29 of the Functional Assessment of Cancer Therapy-General (FACT-G) Version 4.30 The FACT-G is a 27-item questionnaire that assesses quality of life in cancer patients and provides a total score and subscale scores for physical, social, emotional, and functional well-being. Analyses focused on physical, social, emotional, and functional well-being scores. Items are scored on a 0 to 4 scale. Higher scores indicate greater well-being.
Acculturation was assessed using the validated Spanish-language version of the Marin Acculturation Scale (MAC).25 The MAC is an 8-item questionnaire examining Hispanic acculturation in relation to language use, media preferences, and ethnic social relations. Four additional items derived by Hoogland et al.31 addressing language preferences for receiving health information were included. Items are scored on a 1–5 scale. Higher scores indicate greater acculturation. The psychometric properties of the combined 12 items were reported previously.31
1.4 |. Statistical analysis
Data were drawn from a larger randomized trial evaluating a stress management intervention versus usual care.31 Because no effects of the intervention were observed,31 study arms were collapsed for the current secondary data analyses. Means and frequencies were used to describe participant characteristics (i.e., age, race, marital status, education, annual household income, employment, years residing in the United States, country of birth, diagnosis, disease stage and months since diagnosis). Mixed models were used to examine the association of baseline and change in spiritual well-being with change in depression and anxiety; and physical, social, emotional, and functional well-being over time. Mixed models were run with both linear and quadratic effects; quadratic effects were dropped from the models if not significant. A one-half standard deviation (SD) was used to define clinically significant change in spiritual well-being32; two-point differences between estimates indicated clinically meaningful change in quality of life.33 Statistically significant time by baseline spirituality interactions were depicted graphically with mean change in spiritual well-being (from baseline to week 13) as a categorical variable (one SD above mean change in spiritual well-being, mean change in spiritual well-being, and one SD below mean change in spiritual well-being) for illustrative purposes.32 Mixed models were used to explore examine participants characteristics (i.e., age, marital status, education, race, disease stage, recruitment site, acculturation) as predictors of baseline and change in spiritual well-being over time. Data were analyzed with SAS, version 9.4 (SAS Institute).
2 |. RESULTS
A total of 324 patients were approached to participate in the study and 258 provided informed consent. Of these, four were lost to follow up, eight were ineligible after consent, and four withdrew prior to data collection. Thus, 242 participants were included in the analyses. Participant characteristics are described in Table 1. On average, participants were 51 years old (SD = 10.6). Most participants were white, married, did not have a college degree, and were diagnosed with breast cancer.
Table 1.
Demographic and clinical characteristics of the sample (n = 242)
| Recruitment site: n (%) | |
| Moffitt Cancer Center | 125 (52) |
| University of Miami Comprehensive Cancer Center | 117 (48) |
| Age: Mean (SD) | 51 (10.6) |
| Race: White: n (%) | 192 (82.4) |
| Marital status: Married: n (%) | 127 (52.7) |
| Education: College degree: n (%) | 93 (38.6) |
| Annual household income: ≥$20,000: n (%) | 77 (44.3) |
| Employment: At least part-time: n (%) | 90 (38.0) |
| Years residing in the United States: M (SD) | 24 (16.7) |
| Country of birtha: n (%) | |
| Cuba | 75 (44.6) |
| United States | 30 (17.9) |
| Mexico | 22 (13.1) |
| Colombia | 16 (9.5) |
| Puerto Rico | 25 (14.9) |
| Diagnosisa: n (%) | |
| Breast cancer | 194 (81.2) |
| Ovarian cancer | 14 (6) |
| Other | 31 (13) |
| Disease stagea: n (%) | |
| I | 45 (19.0) |
| II | 102 (43.0) |
| III | 73 (30.8) |
| IV | 17 (7.2) |
| Months since initial diagnosis: Mean (SD) | 3.47 (10.2) |
| Acculturation: Mean (SD) | 2.10 (1.15) |
Abbreviation: SD, standard deviation.
Numbers do not add to 242 due to missing data.
At week 7 (n = 229), 32% of participants reported decreased spiritual well-being and 42% improved spiritual well-being relative to baseline. At week 13 (n = 202), 42% reported worsened spiritual well-being and 32% improved spiritual well-being. Results of the linear mixed models examining baseline spiritual well-being as a predictor of changes in distress (i.e., depression, anxiety) and quality of life (i.e., physical, social, emotional, and functional well-being) are shown in Table 2. At baseline, greater spiritual well-being was associated with less concurrent depression and anxiety (all p values < 0.001) and better physical, social, emotional, and functional well-being (all p values < 0.001). Baseline spiritual well-being was also associated with changes over time in emotional and functional well-being (all p values < 0.01). As shown in Figure 1A, participants with low baseline spiritual well-being reported worse emotional well-being at baseline that, despite improving over time, remained worse relative to participants with high baseline spiritual well-being in whom emotional well-being did not change. As shown in Figure 1B, participants with low baseline spiritual well-being reported worse functional well-being at baseline that, despite declining over time in both groups, remained worse relative to participants with high spiritual well-being. Change in functional well-being among patients with high baseline spiritual well-being was clinically meaningful.33 Baseline spiritual well-being was not associated with changes in depression, anxiety, physical and social well-being (all p values > 0.05).
Table 2.
Parameter estimates for the mixed models examining baseline spiritual well-being with change in distress and quality of life
| Depression | Anxiety | Physical well-being | Social well-being | Emotional well-being | Functional well-being | |
|---|---|---|---|---|---|---|
| Intercept | 4.73*** | 7.69*** | 21.76*** | 21.67*** | 16.61*** | 17.10*** |
| Time | 0.79*** | −0.62*** | −2.55*** | −0.40* | 0.61*** | −0.95*** |
| Spiritual well-being at baseline | −0.31*** | −0.31*** | 0.30*** | 0.25*** | 0.41*** | 0.52*** |
| Time*Spiritual well-being at baseline | 0.02 | 0.02 | <0.01 | <0.01 | −0.07*** | −0.07** |
Note: Intercept at baseline.
p < 0.05;
p < 0.01;
p < 0.001.
Figure 1.
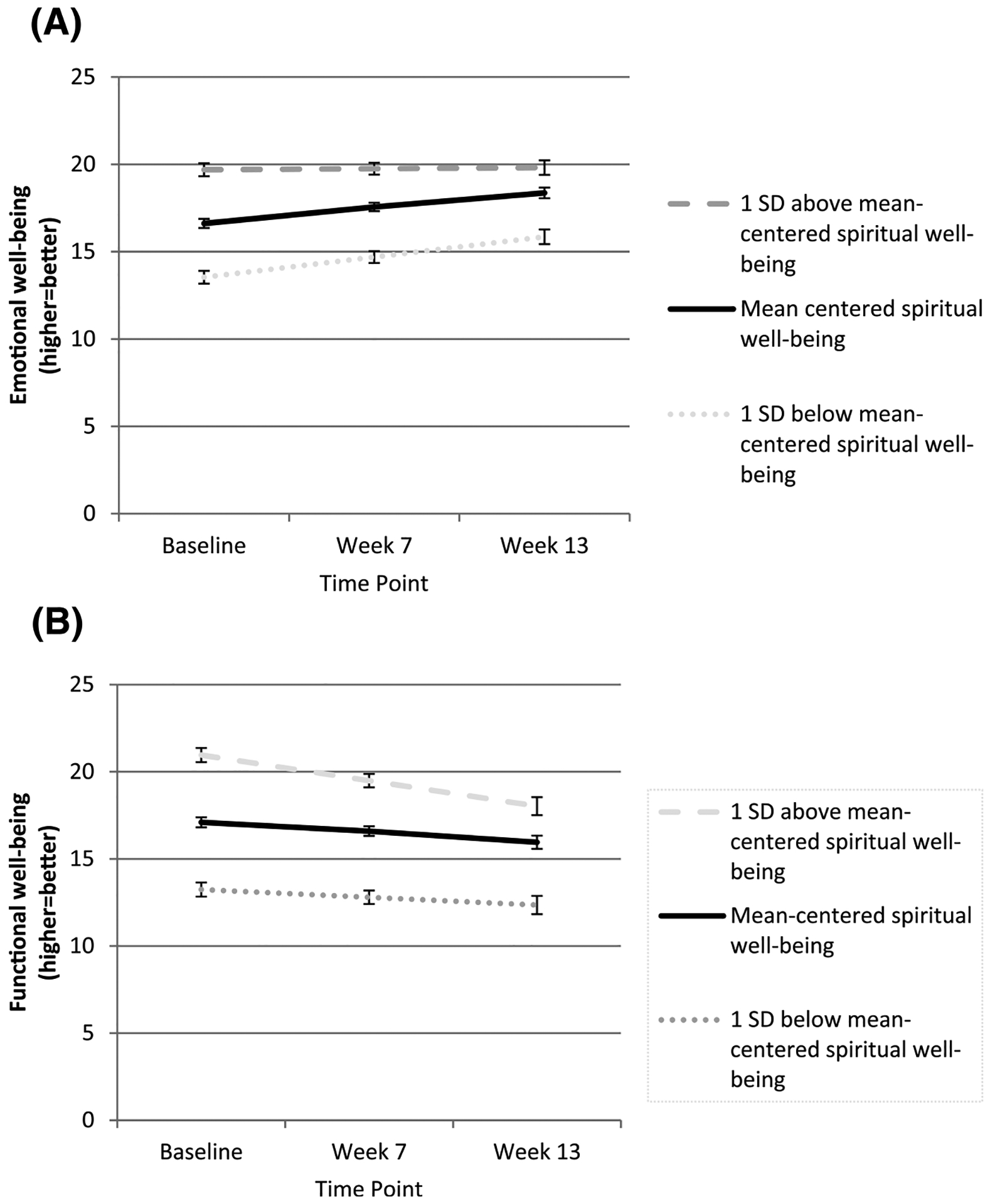
(A) Associations between participants’ baseline spiritual well-being and emotional well-being over time.
(B) Associations between participants’ baseline spiritual well-being and functional well-being over time. SD, standard deviation
Results of the mixed models examining associations between change in spiritual well-being and changes in distress and quality of life are described in Table 3. Changes in spiritual well-being were significantly associated with change in social well-being over time (p < 0.01). Social well-being improved among participants who reported increases in spiritual well-being, whereas social well-being worsened among participants who reported decreases in spiritual well-being over time. The extent to which social well-being worsened in participants with declining spiritual well-being was clinically meaningful.33 Changes in spiritual well-being were not associated with changes in depression, anxiety, physical, emotional, or functional well-being (p values > 0.05).
Table 3.
Parameter estimates for the mixed models examining change in spiritual well-being with change in distress and quality of life
| Effect | Depression | Anxiety | Physical well-being | Social well-being | Emotional well-being | Functional well-being |
|---|---|---|---|---|---|---|
| Intercept | 14.68*** | 16.80*** | 11.27*** | 13.36*** | 2.85* | −0.20 |
| Time | 1.54* | 0.12 | −4.15*** | −2.76** | 1.07 | −0.76 |
| Spiritual well-being | −0.25*** | −0.23*** | 0.27*** | 0.21*** | 0.35*** | 0.44*** |
| Time*Spiritual well-being | −0.02 | −0.02 | 0.04 | 0.06** | −0.01 | <0.01 |
Note: Intercept at baseline.
p < 0.05;
p < 0.01;
p < 0.001.
Post hoc analyses explored the relationships among the spiritual well-being subscales (i.e., peace, meaning and faith) and study outcomes to further understand patterns of spiritual well-being among this population. Similar patterns of results were observed for the subscales compared to the total score (Tables S1–S3).
Additional exploratory analysis examining the association of baseline sociodemographic factors, acculturation and clinical variables with baseline spiritual well-being and change in spiritual well-being over time were conducted. These analyses revealed that married participants reported greater spiritual well-being relative to participants who were not married (p < 0.001). There were no other significant associations between sociodemographic or disease characteristics (i.e., age, education, race, disease stage, recruitment site, acculturation) and spirituality at baseline or over time (all p values > 0.05).
3 |. DISCUSSION
This study examined whether baseline spiritual well-being and changes in spiritual well-being predicted change in distress and quality of life among Hispanic women with cancer during chemotherapy and explored potential factors associated with baseline and change in spiritual well-being over time. Results indicated that greater baseline spiritual well-being is associated with less concurrent distress and better quality of life, which is particularly relevant for Hispanic women with cancer are at risk of developing clinically significant symptoms of anxiety and depression22 and quality of life impairments prior to treatment.15,17
Greater baseline spiritual well-being was significantly associated with greater functional and emotional well-being over time. Despite undergoing cancer treatment, functional and emotional well-being among participants with greater spiritual well-being was comparable to that reported by the general population.34 In addition, increases in spiritual well-being over time were associated with improved social well-being, whereas decreased spiritual well-being over time was associated with worsened social well-being over time. These results align with previous findings indicating that greater levels of spiritual well-being are characterized, for example, by a sense of equanimity, peacefulness, and harmony, and result in better social health. In contrast, low spiritual well-being may involve sense of struggle with or alienation from faith among others that can result in reduced social well-being.10 Results of the post hoc analyses revealed that spiritual well-being subscales (i.e., faith, meaning and peace) showed similar patterns of quality of life outcomes as total score and as reported in Hispanic and non-Hispanic participants.35
Married participants in the current study reported greater spiritual well-being relative to participants who were not married, contrasting with results from the meta-analyses showing that the association between spiritual well-being and patients’ well-being was not limited to any demographic or clinical characteristic.8–10 Nevertheless, married cancer patients were found to pray more for health relative to those who were divorced or separated, according to a national survey conducted in the United States.36 No other studies, to our knowledge, have reported this association, pointing to the need to further investigate its underlying mechanisms. No other demographic and clinical variables, nor acculturation, were associated with baseline or changes in spiritual well-being over time, in line with that reported by others in Hispanic women with cancer.18
Overall, results of our study expand understanding of bi-variate associations reported in meta-analyses8–10 to show that greater spiritual well-being may have effects on Hispanic female cancer patients’ functional, emotional and social well-being over time. Patients can find in spiritual well-being affective resources (e.g., meaning and purpose in life, sense of transcendence), cognitive (e.g., spiritual beliefs, casual attributions, post-traumatic growth) and other resources (e.g., religious affiliation, spiritual support),8–10 that have the potential to facilitate adjustment to cancer,6,7 increase resilience and personal growth,3,6 and reinforce relationships.6
This is among the first studies prospectively examining spiritual well-being among a large sample of Spanish-speaking Hispanic women with cancer before and after being treated with chemotherapy. The current study addressed gaps in previous meta-analyses, such as the lack of longitudinal studies, underrepresentation of minorities, small sample sizes, heterogeneity in terms of or lack of clinical data (e.g., stages of diseases, tumor classification, phases of illness trajectory) and the lack of psychometrically rigorous measures to examine spiritual well-being.8–10
3.1 |. Study limitations
Limitations should be noted. This is a secondary analysis of a randomized clinical trial testing an intervention to reduce chemotherapy-related stress. However, as there were no differences between intervention groups on outcomes, we believe the design and the sample is adequate for the purpose of the current study. In addition, participants were treated at academic medical centers in Tampa and Miami, and almost half were born in Cuba; therefore, results may not generalize to other Hispanic patients treated and born elsewhere. Future studies are also needed to examine spiritual well-being among Hispanic men.
3.2 |. Clinical implications
Results describe the need to address spiritual well-being when caring for Hispanic women with cancer receiving chemotherapy. Early identification and referral to appropriate resources is needed for patients at risk of worse outcomes. Meaning-making interventions, for example, have resulted in improved spiritual well-being, quality of life and sense of meaning,37 with positive effects on sense of personal growth and positive relations lasting up to 2-years.38 This type of intervention has been adapted to Spanish-speaking patients with advanced cancer.39,40 Referrals to the chaplaincy may also be of help for patients who wish to discuss struggles they may be having with religious faith. Future studies are needed to develop and adapt interventions targeting spiritual well-being in Spanish-speaking Hispanic women with cancer receiving chemotherapy.
4 |. CONCLUSIONS
This study examines spiritual well-being in Hispanic women with cancer undergoing chemotherapy. Results indicate that greater spiritual well-being is associated with less concurrent distress and better quality of life, as well as with greater emotional, functional and social well-being over time among this population. Further studies examining spiritual well-being for extended periods of time are needed.
Supplementary Material
ACKNOWLEDGMENTS
This work has been supported in part by the Participant Research, Interventions, and Measurement Core Facility at the H. Lee Moffitt Cancer Center & Research Institute, a National Cancer Institute designated comprehensive cancer center (P30-CA076292), American Cancer Society, Grant/Award Numbers: RSG-12-087-01-CPPB. The content is solely the responsibility of the authors and does not necessarily represent the official views of the abovementioned parties or the National Cancer Institute. Grants currently supporting Dr. Antoni and relevant to this manuscript: 1P30CA240139-01, 7R01CA206456-01A1, R01CA206456-03S1, UG3 CA260317, R37 CA255875, R01CA196953, Sylvester Comprehensive Cancer Center Bridge Grant PG013720.
Funding information
H. Lee Moffitt Cancer Center & Research Institute, Grant/Award Number: P30-CA076292; American Cancer Society, Grant/Award Numbers: RSG-12-087-01-CPPB, 1P30CA240139-01, 7R01CA206456-01A1, R01CA206456-03S1, UG3 CA260317, R37 CA255875, R01CA196953; Sylvester Comprehensive Cancer Center Bridge, Grant/Award Number: PG013720
Footnotes
SUPPORTING INFORMATION
Additional supporting information can be found online in the Supporting Information section at the end of this article.
DATA AVAILABILITY STATEMENT
Deidentified data upon which the manuscript is based are available upon request to the corresponding author.
REFERENCES
- 1.Mytko JJ, Knight SJ. Body, mind and spirit: towards the integration of religiosity and spirituality in cancer quality of life research. Psycho-oncology. 1999;8(5):439–450. [DOI] [PubMed] [Google Scholar]
- 2.Peterman AH, Fitchett G, Brady MJ, Hernandez L, Cella D. Measuring spiritual well-being in people with cancer: the functional assessment of chronic illness therapy—Spiritual Well-being Scale (FACIT-Sp). Ann Behav Med. 2002;24(1):49–58. 10.1207/s15324796abm2401_06 [DOI] [PubMed] [Google Scholar]
- 3.Costanzo ES, Ryff CD, Singer BH. Psychosocial adjustment among cancer survivors: findings from a national survey of health and well-being. Health Psychol. 2009;28(2):147–156. 10.1037/a0013221 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Davis LZ, Cuneo M, Thaker PH, Goodheart MJ, Bender D, Lutgendorf SK. Changes in spiritual well-being and psychological outcomes in ovarian cancer survivors. Psycho-oncology. 2018;27(2):477–483. 10.1002/pon.4485 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Balboni TA, Vanderwerker LC, Block SD, et al. Religiousness and spiritual support among advanced cancer patients and associations with end-of-life treatment preferences and quality of life. J Clin Oncol. 2007;25(5):555–560. 10.1200/jco.2006.07.9046 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hunter-Hernández M, Costas-Muñíz R, Gany F. Missed opportunity: spirituality as a bridge to resilience in Latinos with cancer. J Relig Health. 2015;54(6):2367–2375. 10.1007/s10943-015-0020-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Garduno-Ortega O, Morales-Cruz J, Hunter-Hernandez M, Gany F, Costas-Muniz R. Spiritual well-being, depression, and quality of life among Latina breast cancer survivors. J Relig Health. 2021;60(3): 1895–1907. 10.1007/s10943-020-01147-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Jim HS, Pustejovsky JE, Park CL, et al. Religion, spirituality, and physical health in cancer patients: a meta-analysis. Cancer. 2015;121(21):3760–3768. 10.1002/cncr.29353 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Salsman JM, Pustejovsky JE, Jim HS, et al. A meta-analytic approach to examining the correlation between religion/spirituality and mental health in cancer. Cancer. 2015;121(21):3769–3778. 10.1002/cncr.29350 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Sherman AC, Merluzzi TV, Pustejovsky JE, et al. A meta-analytic review of religious or spiritual involvement and social health among cancer patients. Cancer. 2015;121(21):3779–3788. 10.1002/cncr.29352 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.US Census Bureau. Annual Estimates of the Resident Population for the United States, States, Counties and Puerto Rico Commonwealth and Municipios: April 1, 2010 to July 1, 2019. US Census Bureau; 2020. [Google Scholar]
- 12.United States Census Bureau. Demographic Turning Points for the United States: Population Projections for 2020 to 2060; 2020. https://www.census.gov/library/publications/2020/demo/p25-1144.html
- 13.Miller KD, Ortiz AP, Pinheiro PS, et al. Cancer statistics for the US Hispanic/Latino population, 2021. Cancer J Clin. 2021;71(6):466–487. 10.3322/caac.21695 [DOI] [PubMed] [Google Scholar]
- 14.Klein A, Villareal M, Radpour S, et al. Demonstrating higher incidence of advanced breast malignancies in our young Hispanic population. Am Surg. 2018;84(11):1787–1789. 10.1177/000313481808401136 [DOI] [PubMed] [Google Scholar]
- 15.Yanez B, Thompson EH, Stanton AL. Quality of life among Latina breast cancer patients: a systematic review of the literature. J Cancer Surviv. 2011;5(2):191–207. 10.1007/s11764-011-0171-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Eversley R, Estrin D, Dibble S, Wardlaw L, Pedrosa M, Favila-Penney W. Post-treatment symptoms among ethnic minority breast cancer survivors. Oncol Nurs Forum. 2005;32(2):250–256. 10.1188/05.onf.250-256 [DOI] [PubMed] [Google Scholar]
- 17.Miller AM, Ashing KT, Modeste NN, Herring RP, Sealy DA. Contextual factors influencing health-related quality of life in African American and Latina breast cancer survivors. J Cancer Surviv. 2015;9(3):441–449. 10.1007/s11764-014-0420-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Wildes KA, Miller AR, de Majors SS, Ramirez AG. The religiosity/spirituality of Latina breast cancer survivors and influence on health-related quality of life. Psycho-oncology. 2009;18(8):831–840. 10.1002/pon.1475 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ashing-Giwa KT, Padilla GV, Bohórquez DE, Tejero JS, Garcia M. Understanding the breast cancer experience of Latina women. J Psychosoc Oncol. 2006;24(3):19–52. 10.1300/j077v24n03_02 [DOI] [PubMed] [Google Scholar]
- 20.Costas-Muñiz R, Garduño-Ortega O, Hunter-Hernández M, Morales J, Castro-Figueroa EM, Gany F. Barriers to psychosocial services use for Latina versus non-Latina white breast cancer survivors. Am J Psychother. 2021;74(1):13–21. 10.1176/appi.psycho-tnqh_9;therapy.20190036 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Costas-Muñiz R, Hunter-Hernández M, Garduño-Ortega O, Morales-Cruz J, Gany F. Ethnic differences in psychosocial service use among non-Latina white and Latina breast cancer survivors. J Psychosoc Oncol. 2017;35(4):424–437. 10.1080/07347332.2017.1310167 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Lee MS, Tyson DM, Gonzalez BD, et al. Anxiety and depression in Spanish-speaking Latina cancer patients prior to starting chemotherapy. Psycho-oncology. 2018;27(1):333–338. 10.1002/pon.4462 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Janz NK, Mujahid MS, Hawley ST, Griggs JJ, Hamilton AS, Katz SJ. Racial/ethnic differences in adequacy of information and support for women with breast cancer. Cancer. 2008;113(5):1058–1067. 10.1002/cncr.23660 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Maly RC, Liu Y, Liang LJ, Ganz PA. Quality of life over 5 years after a breast cancer diagnosis among low-income women: effects of race/ethnicity and patient-physician communication. Cancer. 2015;121(6): 916–926. 10.1002/cncr.29150 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Marin G, Sabogal F, Vanos Marin B, Otero-Sabogal R, Perez-Stable EJ. Development of a short acculturation scale for Hispanics. Hispanics J Behav Sci. 1987;9(2):183–205. 10.1177/07399863870092005 [DOI] [Google Scholar]
- 26.Webster K, Odam L, Peterman A, Lent L, Cella D. The Functional Assessment of Chronic Illness Therapy (FACIT) measurement system: validation of version 4 of the questionnaire. Qual Life Res. 1999;8:604. [Google Scholar]
- 27.Herrero MJ, Blanch J, Peri JM, De Pablo J, Pintor L, Bulbena A. A validation study of the hospital anxiety and depression scale (HADS) in a Spanish population. Gen Hosp Psychiatry. 2003;25(4):277–283. 10.1016/s0163-8343(03)00043-4 [DOI] [PubMed] [Google Scholar]
- 28.Zigmond AS, Snaith RP. The hospital anxiety and depression scale. Acta Psychiatr Scand. 1983;67(6):361–370. 10.1111/j.1600-0447.1983.tb09716.x [DOI] [PubMed] [Google Scholar]
- 29.Dapueto JJ, Francolino C, Gotta I, et al. Evaluation of the Functional Assessment of Cancer Therapy-General Questionnaire (FACT-G) in a South American Spanish speaking population. Psycho-oncology. 2001;10(1):88–92. [DOI] [PubMed] [Google Scholar]
- 30.Cella DF, Tulsky DS, Gray G, et al. The Functional Assessment of Cancer Therapy scale: development and validation of the general measure. J Clin Oncol. 1993;11(3):570–579. 10.1200/jco.1993.11.3.570 [DOI] [PubMed] [Google Scholar]
- 31.Hoogland A, Lechner SC, Gonzalez BD, et al. Efficacy of a Spanish-Language Self-Administered Stress Management Training intervention for Latinas undergoing chemotherapy. Psycho-oncology. 2018;27(2):1305–1311. 10.1002/pon.4673 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Norman G, Sloan JA, Wyrwich KW. Interpretation of changes in health-related quality of life: the universality of a half standard deviation. Med Care. 2003;41(5):582–592. 10.1097/01.mlr.0000062554.74615.4c [DOI] [PubMed] [Google Scholar]
- 33.Yost K, Eton DT. Combining distribution-and anchor-based approaches to determine minimally important differences: the FACIT experience. Eval Health Prof. 2005;28(2):172–191. 10.1177/0163278705275340 [DOI] [PubMed] [Google Scholar]
- 34.Pearman T, Yanez B, Peipert J, Wortman K, Beaumont J, Cella D. Ambulatory cancer and US general population reference values and cutoff scores for the functional assessment of cancer therapy. Cancer. 2014;120(18):2902–2909. 10.1002/cncr.28758 [DOI] [PubMed] [Google Scholar]
- 35.Murphy PE, Canada AL, Fitchett G, et al. An examination of the 3-factor model and structural invariance across racial/ethnic groups for the FACIT-Sp: a report from the American Cancer Society’s Study of Cancer Survivors-II (SCS-II). Psycho-oncology. 2010;19(3): 264–272. 10.1002/pon.1559 [DOI] [PubMed] [Google Scholar]
- 36.Ross L, Hall IJ, Fairley TL, Taylor YJ, Howard DL. Prayer and self-reported health among cancer survivors in the United States, National Health Interview Survey, 2002. J Altern Complement Med. 2008;14(8):931–938. 10.1089/acm.2007.0788 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Breitbart W, Pessin H, Rosenfeld B, et al. Individual meaning-centered psychotherapy for the treatment of psychological and existential distress: a randomized controlled trial in patients with advanced cancer. Cancer. 2018;124(15):3231–3239. 10.1002/cncr.31539 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Holtmaat K, van der Spek N, Lissenberg-Witte B, Breitbart W, Cuijpers P, Verdonck-de Leeuw I. Long-term efficacy of meaning-centered group psychotherapy for cancer survivors: 2-year follow-up results of a randomized controlled trial. Psycho-oncology. 2020;29(4):711–718. 10.1002/pon.5323 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Costas-Muniz R, Torres-Blasco N, Castro-Figueroa EM, Gonzalez CJ, Breitbart W, Gany F. Meaning-centered psychotherapy for Latino patients with advanced cancer: cultural adaptation process. J Palliat Med. 2020;23(4):489–497. 10.1089/jpm.2019.0423 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Torres-Blasco N, Castro-Figuero E, Garduno-Ortega O, Costas-Muniz R. Cultural adaptation and open pilot of meaning-centered psychotherapy for Puerto Rican patients with advanced cancer. Sci J Educ. 2020;8(4):100–107. 10.11648/j.sjedu.20200804.12 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Deidentified data upon which the manuscript is based are available upon request to the corresponding author.


