Abstract
We describe our technique for harvesting the radial artery for coronary revascularization. Anatomy and preoperative preparation are also presented, as well as the history of the radial artery as a bypass conduit, the advantages, and some contraindications.
We have found that, with proper harvesting, the radial artery is an effective means of coronary artery revascularization.
Key words: Cardiac revascularization, coronary artery bypass/methods/trends, myocardial revascularization, radial artery
Since Garrett and colleagues 1 1st performed coronary artery bypass grafting using the greater saphenous vein, cardiothoracic surgeons have been searching for the optimal conduit. 2 Grafting the left internal mammary artery to the left anterior descending artery was shown by Loop and associates 3 to increase survival rates and decrease the incidence of long-term cardiac events. In another retrospective study, Lytle and coworkers 4 found additional benefits to patients receiving both of the internal mammary arteries. Use of the radial artery by Carpentier's group 5 in the early 1970s was considered unsuccessful. However, its use was reintroduced into clinical practice by Acar and colleagues 6 in the early 1990s to increase the number of arterial grafts available to patients undergoing coronary revascularization. Currently, the use of the radial artery is dependent on proper harvesting and handling techniques for success. We review the pertinent anatomy and our technique for harvesting the radial artery for use as a coronary artery bypass graft at our institution.
Surgical Anatomy
The radial artery is a muscular artery lying under the antebrachial fascia between the brachioradialis muscle and the flexor carpi radialis. It originates at the bifurcation of the brachial artery about 1 cm below the antecubital fossa and traverses along the radial aspect of the forearm to the wrist, where it passes deep to the tendons of the abductor pollicis longus and the extensor pollicis brevis across the anatomic snuffbox. In the proximal one third of the forearm, the radial artery is situated in an ulnar position relative to the biceps brachii tendon, and it passes deep to the muscular belly of the brachioradialis. The remainder of its course in the forearm is deep to the deep fascia and medial to the brachioradialis tendon.
Two branches of the radial artery serve as landmarks for dissection. The takeoff of the radial recurrent artery approximately 1 cm distal to the radial edge of the bicipital aponeurosis is the landmark that defines the proximal boundary for dissection in radial artery harvesting. The 2nd major arterial branching point is the superficial palmar artery, which marks the distal extent of dissection in the forearm.
Two nerves that provide sensory innervation to the forearm, parts of the thumb, and the dorsum of the hand may be encountered during radial artery harvesting. One is the lateral cutaneous nerve, which is a branch of the musculocutaneous nerve that provides sensory innervation to the radial aspect of the forearm. The other is the superficial branch of the radial nerve, which travels in close proximity to the radial artery and serves a portion of the thenar eminence in the palm and the radial aspect of the dorsum of the hand.
Preoperative Preparation
A modified Allen's test is performed in all patients before they are taken to the operating room. In this test, the patient makes a tight fist, and the radial and ulnar arteries are compressed firmly at the wrist by the examiner. While compression is maintained, the patient slowly opens the wrist and only partially extends the fingers, because hyperextension can produce a false-positive result. When the ulnar artery is released, a hyperemic response in the hand extending to the thenar eminence and thumb within 5 seconds indicates adequate collateral circulation by the ulnar artery and nondominance of the radial artery.
Harvesting Technique
If the results of the Allen's test are normal in both upper extremities, the nondominant extremity is generally selected as the harvest site. The nondominant forearm is surgically prepped circumferentially and draped from the mid-arm to the hand. The forearm is extended and supinated directly perpendicular to the patient's torso. The upper extremity is draped in such a manner that, after harvesting, the radial artery can be easily placed parallel to the torso in preparation for coronary artery bypass grafting.
Exposure of the radial artery requires a thorough understanding of its course along the forearm. A curvilinear incision is made, extending from approximately 2 cm below the antecubital crease, along the length of the forearm, to the wrist crease point (Fig. 1). The incision parallels the medial edge of the brachioradialis muscle. The skin and subcutaneous tissue are incised down to the fascia overlying the flexor carpi radialis muscle. The fascial sheath that overlies the superficial muscles of the volar forearm is divided between the brachioradialis muscle and the flexor carpi radialis. The lateral cutaneous nerve of the forearm usually overlies the brachioradialis in the same plane as the fascial sheath. Care is taken to prevent injury to this nerve: this is accomplished by displacing it laterally (Fig. 2).
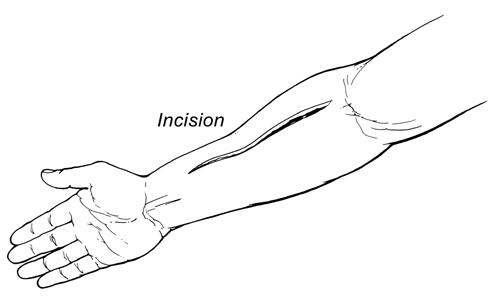
Fig. 1 The Initial skin incision for radial artery harvesting.
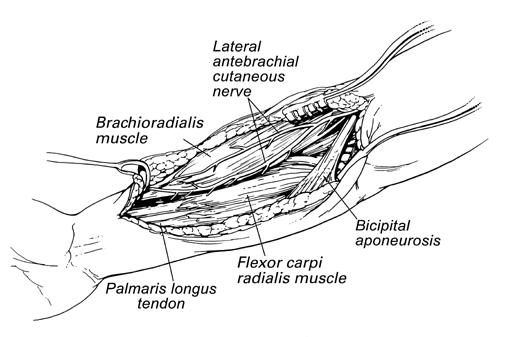
Fig. 2 The musculature and nerves of forearm exposed during radial artery harvesting.
After the superficial volar muscular sheath is incised, careful retraction of the brachioradialis and flexor carpi radialis muscles, 1st laterally and then medially, is performed with a self-retaining retractor. This maneuver reveals the entire course of the radial artery from the biceps tendon to the radial styloid. The easiest site to begin dissection of the radial artery pedicle is the middle portion of the forearm as the artery emerges from beneath the brachioradialis muscle. The radial artery pedicle is gently mobilized to lift it from its muscular bed. As the pedicle is lifted, the side branches of the radial artery are exposed. Careful, gentle, and progressively upward traction of the pedicle is performed. The side branches are then isolated and either clipped or ligated with the harmonic scalpel.
When the entire radial artery pedicle is completely mobilized, the proximal and distal ends of the pedicle are prepared for division. A 2-0 silk suture is placed around the radial pedicle along the length where the radial styloid meets the radial pedicle, and the distal end of the radial artery is ligated. The stump of the remnant radial artery is then palpated in order to document its pulsation and verify ulnar artery collateral circulation. Next, the proximal end of the radial artery pedicle is prepared. The pedicle is lifted perpendicular to the forearm, ligated with a 2-0 silk suture, and divided (Fig. 3). We place a small cannula in the proximal end of the graft and gently flush the entire graft with papaverine, being careful not to over-distend the vessel. The harvested radial artery graft is inspected to ensure that all side branches are ligated securely. The entire radial artery pedicle graft is then wrapped in papaverine-soaked gauze (1 mg papaverine per 1 mL saline).
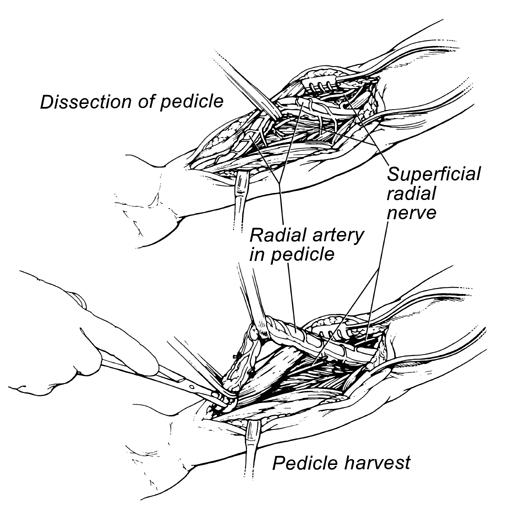
Fig. 3 Dissection and harvesting of the pedicle.
Hemostasis of the radial artery harvest site is achieved with electrocautery. The forearm wound is closed before the administration of systemic heparin. The deep fascia of the forearm is closed with a running 2-0 polyglycolic suture. The skin is closed with a running 4-0 polyglycolic suture. No drains are placed unless moderate drainage persists despite hemostasis.
Discussion
Carpentier and coworkers 1st reported their use of the radial artery as a bypass conduit in 1973. 5 Its use was abandoned, however, after 12-month follow-up revealed an extremely high occlusion rate secondary to intimal hyperplasia and vasospasm of the denervated artery. 7 The occlusion was most likely caused by trauma to the vessel associated with harvesting techniques, such as mechanical dilation with metal dilators, and forced hydrostatic dilation. 7 The vasoconstriction response of the radial artery is higher than that of the internal mammary artery, presumably because of its thicker media. The use of calcium channel blockers and minimal manipulation of the vessel during harvesting is thought to prevent spasm secondary to smooth-muscle vasoconstriction.
Use of the radial artery as a conduit for coronary artery bypass grafting has several technical advantages: the artery is approximately 20 cm long; it has a diameter greater than that of the internal mammary artery; it is normally subjected to systemic blood pressure; it has thick and resistant walls; and it is rarely affected by atherosclerosis. 8 Several contraindications to using the radial artery also exist: inadequate ulnar circulation; a history of vasculitis; Raynaud's phenomenon; severe chronic renal insufficiency; carpal tunnel syndrome; brachial plexus injury; and trauma to the extremity.
During dissection of the radial artery, several techniques can be used to improve the outcome. For example, care should be taken to avoid excessive manipulation of the vessel, and electrocautery should not be used to divide branches—although the harmonic scalpel works well for this and is acceptable. The artery should be harvested as a pedicle and covered with papaverine during the period before insertion. A thorough understanding of the anatomy of the forearm is also vital to avoid injury to adjacent structures.
Conclusion
The superiority of the internal mammary artery in terms of long-term patency rates has led many surgeons to increase their use of arterial conduits for coronary revascularization. During the last decade, the radial artery has been shown to be an effective means of revascularization if harvested properly. Herein, we have described our method for harvesting the radial artery, which we have used successfully at our institution to provide patients with total arterial coronary artery revascularization.
Footnotes
Address for reprints: Michael J. Reardon, MD, 6565 Fannin, #A853, Houston, TX 77030
References
- 1.Garrett HE, Dennis EW, DeBakey ME. Aortocoronary bypass with saphenous vein graft. Seven-year follow-up. JAMA 1973;223:792–4. [PubMed]
- 2.Reardon MJ, Conklin LD, Reardon PR, Baldwin JC. Coronary artery bypass conduits: review of current status. J Cardiovasc Surg (Torino) 1997;38:201–9. [PubMed]
- 3.Loop FD, Lytle BW, Cosgrove DM, Stewart RW, Goormastic M, Williams GW, et al. Influence of the internal-mammary-artery graft on 10-year survival and other cardiac events. N Engl J Med 1986;314:1–6. [DOI] [PubMed]
- 4.Lytle BW, Blackstone EH, Loop FD, Houghtaling PL, Arnold JH, Akhrass R, et al. Two internal thoracic artery grafts are better than one. J Thorac Cardiovasc Surg 1999;117:855–72. [DOI] [PubMed]
- 5.Carpentier A, Guermonprez JL, Deloche A, Frechette C, DuBost C. The aorta-to-coronary radial artery bypass graft. A technique avoiding pathological changes in grafts. Ann Thorac Surg 1973;16:111–21. [DOI] [PubMed]
- 6.Acar C, Jebara VA, Portoghese M, Beyssen B, Pagny JY, Grare P, et al. Revival of the radial artery for coronary artery bypass grafting. Ann Thorac Surg 1992;54:652–60. [DOI] [PubMed]
- 7.Tatoulis J, Buxton BF, Fuller JA. Bilateral radial artery grafts in coronary reconstruction: technique and early results in 261 patients. Ann Thorac Surg 1998;66:714–20. [DOI] [PubMed]
- 8.Kulshrestha P, Rao L, Gard JL, Rousou JA, Engelman RM, Wait RB. Use of extrafascially harvested radial artery for coronary artery revascularization: technical considerations. J Card Surg 1999;14:26–31. [DOI] [PubMed]


