The Canadian Journal of Kidney Health and Disease recognizes its responsibility as a knowledge provider and is proud to announce a special collection on environmentally sustainable kidney care entitled “Introduction, Perspectives, and Pathways to Low Carbon Kidney Care.”
Herein, we open this collection with a perspective outlining this urgent requirement.
Anthropogenic Emissions Are Disrupting Earth’s Life and Ecology
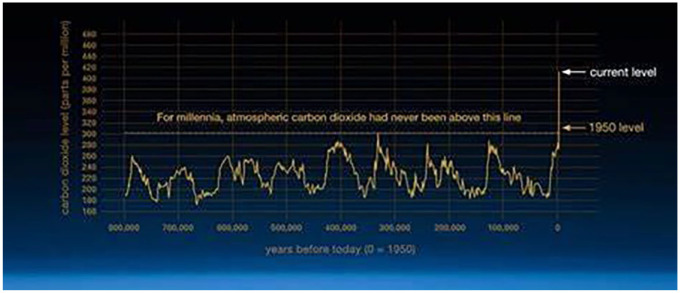
The climate crisis threatens Earth’s natural systems on which we all depend. Since the industrial revolution in the mid-1700s, annual anthropogenic emissions of greenhouse gases (GHGs) have increased from 9 million1,2 to more than 32 billion tons. 3 Levels of atmospheric carbon dioxide, the most common but by no means the most potent of the GHGs, now approach 420 parts per million (ppm), an increase of nearly 50% in a short 300 years from the preceding 800 000-year baseline range of 170 to 300 ppm (Figure 1). 4 Greenhouse gases capture solar energy radiated from Earth’s surface, preventing heat from being released to space. The Intergovernmental Panel on Climate Change (IPCC), the United Nations body responsible for assessing the science related to climate change, clearly states that increasing emissions cause further warming.
Figure 1.
Atmospheric carbon dioxide has doubled in the industrial era.
Source. Data from NOAA.
Note. Carbon Dioxide| Vital Signs—Climate Change: Vital Signs of the Planet (nasa.gov). https://climate.nasa.gov/vital-signs/carbon-dioxide/
Excess retained heat from higher atmospheric concentration of GHGs warms Earth’s atmosphere, land, and seas, causing melting of sea and land ice, which in turn changes ocean currents and weather patterns, and thaw permafrost. Even 1/10th degree Celsius temperature rise increases risk to terrestrial and marine species and ecosystems, most of which currently approach or exceed limits of the conditions in which they have evolved and existed, 5 highlighting the peril of Earth’s current average temperature that is 1.1°C above the preindustrial 1850-1900 referent period. 5 Already we are witnessing changes that were predicted decades ago—an ever rising burden of extreme weather, changes in rainfall that challenge crop yields and land livability, and rising sea levels that threaten coastal ecosystems as well as the livelihoods of the 40% of people worldwide who reside in or near these ecosystems. 5 These changes contribute to the second crisis of our era, that of biodiversity, such that we have entered what is now considered the sixth great extinction event in Earth’s 4.6-billion-year history. 6 Under all emissions scenarios, further temperature rise is expected, 5 with a recent World Meteorological Organization warning of accelerated warming and a significant chance that the 1.5°C rise, beyond which the effects of climate change are predicted to be even more marked, will be reached in the next 5 years. 7 If global emissions continue on the current trajectory, a global mean temperature increase of 3°C is conservatively predicted by the end of this century. The IPCC report itemizes well over 100 regional and global risks, 5 most of which are at moderate or high risk of occurring at 1.5°C rise but almost at uniformly high or very high risk at 3°C temperature increase. In the North American setting, these include changes to terrestrial, fresh, and ocean water ecosystem structure, including water scarcity for agriculture and power generation, changes in fisheries predominantly in the Arctic, reduced crop yields, species range shifts, biodiversity loss, tree and kelp forest losses, and compounding climate events that jeopardize coastal infrastructure, including cities, from sea-level rise. The most alarming projections, however, are of self-perpetuating warming by exceeding climate “tipping points,” leading to irreversible, massive, and cascading changes. Of note, our current global warming is already within the lower end of the uncertainty ranges of 5 of these points, including the collapse of Arctic and Antarctic sea ice sheets, forest dieback with northern expansion, and Atlantic current collapse. 8 Therefore, the need for humanity’s response is now, via urgent and ambitious reductions in GHG emissions, the result of which will determine the fate of all life, including that of humans.
Anthropogenic Emissions Harm Human Health and Have a Major Impact on Kidney Disease
Climate change, and the carbon pollution that causes it, affects human health in multiple direct and indirect ways, 9 including through its effects on water and vector-borne diseases, food insecurity, conflict over limited resources, forced migration, and injury and fatality from severe weather (Figure 2). More than 4.6 million deaths per year between 2000 and 2019 were temperature-relate. 10 Furthermore, an alarming 1 in 5 deaths worldwide have been attributed to the fossil fuel component of air pollution 11 due to the proinflammatory, profibrotic, and proatherogenic effect of particulate matter (PM) air pollutants, most notably those below 2.5 µm in diameter, “PM2.5.” 12 PM2.5 affect kidney health too, with one analysis attributing more than 3 million incident cases of chronic kidney disease (CKD) worldwide to their effect and an enormous Canadian CKD burden of 64 000 to 106 800 cases. 13 Heat stress, via severe and/or recurrent volume depletion, contributes to acute and CKDs, 14 as well as highly morbid and costly conditions such as nephrolithiasis. 15
Figure 2.
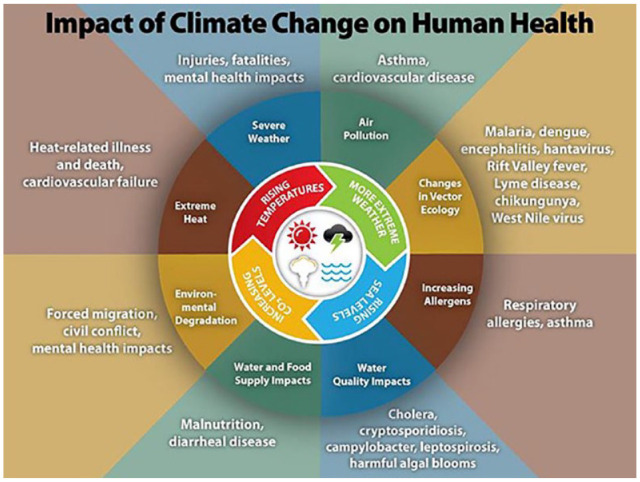
The health effects of climate change.
Note. Climate Effects on Health—CDC. https://www.cdc.gov/climateandhealth/effects/
People who require kidney replacement therapies are uniquely vulnerable to climate-related impacts on health infrastructure in view of their dependence on the provision of chronic life–sustaining medications and dialysis processes. Extreme weather events can affect the availability of electricity, supply chains, road networks, and communications required to support our patients.16,17
Kidney Care Is a Significant Source of GHG Emissions
Health care contributes to fossil fuel emissions and climate crisis—in fact, were health care a country, it would be the fifth highest emitter worldwide, exceeding airplane travel. The most recent estimates suggest that the health care sector is now responsible for 5.2% of global GHG. 18
Kidney care has a disproportionately high footprint within clinical care,19-21 owing to intensive carbon emissions from dialysis therapies with their considerable water, single-use plastic, and energy expenditures. Published per treatment, GHG emissions range from 24.5 to 65.1 kg CO2 equivalents (CO2-eq) (equivalency refers to the warming potential of other non-CO2 GHGs in reference to that of carbon dioxide) for hemodialysis therapy, hence resulting in annual per-patient emissions between 3.8 22 and 10.2 23 ton CO2-eq. The lower estimate of per-treatment emissions equates to that of an average-sized vehicle traveling 100 km. 24 With an estimated 20 000 patients dialyzing thrice weekly, 1 year of average CO2-eq emissions from hemodialysis treatments prescribed in Canada alone equate to vehicle travel of an alarming 312 million kilometers, which approximates a hypothetical equatorial vehicle circumnavigation of Earth 7785 times. The data for peritoneal dialysis (PD) are less robust, but PD emissions may be roughly equivalent to hemodialysis when production and transportation of the large volumes of plastic-enclosed sterile dialysate are considered. 19 There are no published data on emissions from kidney transplantation, although Grafals et al in abstract form reported 95% lower emissions from transplantation than hemodialysis. 25 Data are not yet available on the carbon cost of nondialysis conservative care, though intuitively this would be lower than any dialysis modality because lower resource use is generally less carbon-intensive.
Health Care GHG Emissions: Current Regulatory Environment
Canada is a signatory of the Paris Accord, and as such has committed to achieve net-zero GHG emissions by 2050. Canadian emissions reductions are further mandated by the Net-Zero Emissions Accountability Act, requiring “credible, science-based emissions reductions plans” to achieve GHG emissions reductions of 40% to 45% below 2005 levels by 2030. 26 At the 26th Conference of the Parties (COP) meeting in Scotland in November 2021, Canada signed the COP26 Health agreement, thereby committing to the development of low-carbon, sustainable, and climate-resilient health systems. It is our collective responsibility to determine how our kidney care community will meet this obligation.
Requirements of emissions reductions for Canadian clinical care are, for now, both aspirational and altruistically and voluntarily sought. Greenhouse gas emissions are neither currently tracked in kidney care nor nationally collected for any other realm of clinical care in Canada. Growing national and global interest in the health sector’s role in low carbon transition is creating an increasingly supportive environment for emissions reductions. In the meantime, as disproportionately large emitters, the nephrology community has both opportunity and obligation to steward our care resources wisely, working toward our responsibility to achieve lowest attainable GHG emissions.
Health Care GHG Emissions: Roadmap to Net Zero
Salas et al 27 have called for health care institutions to regularly collect and report valid, widely accepted indicators of GHG emissions, aided by “eco-labelling” of products and supplies. The English National Health Service (NHS) presents the clearest strategy, with a plan to fully decarbonize a range of directly and indirectly controlled health care–associated GHG emissions by 2040 28 and expand the net-zero mandate to supply chains and patient and visitor travel by 2045.
Canada-specific decarbonization recommendations that emphasize the need for widespread infrastructure improvements exist, such as renewable energy generation, building upgrades, zero-emissions transport, and local and sustainably grown food. 29 Pertinent to our community of kidney care providers, however, changes in clinical care are necessary to reduce the remaining “emissions gap,” with one source estimating 15 million tons of carbon dioxide equivalents originating from Canadian health care each year once societal-level infrastructure improvements are fully adopted.
The Sustainable Nephrology Action Planning committee of the Canadian Society of Nephrology has introduced a planetary health model of kidney care that addresses this emissions gap and provides numerous pathways for kidney care providers to engage in low carbon care. 30 This approach emphasizes reducing demand for health services via health promotion and renewed attention to chronic disease management, matching supply to demand for health services including optimizing access to transplantation and consideration of conservative nondialysis care when appropriate, and reducing the environmental impact of care provision via innovations in dialysis and introduction of circular materials economies.
Kidney Care GHG Emissions Reduction in Canada: An Emerging Plan
Medical leaders, with duty of care as well as moral responsibility, must respond to the health and equity crises wrought by climate change. In adapting to these emerging crises, we must consider both mitigation of and adaptation to climate change. Nephrologists must align our preventive efforts and care provision to reduce the impacts of climate change on both health and care delivery, and ensure that our patients can continue to receive the essential and high-quality care that they need. In summary, caring for the environment is now part of caring for our patients.
The Canadian Society of Nephrology has recognized the need for kidney care to adapt in serving our patients in this era of climate crisis. Our Sustainable Nephrology Action Planning (“SNAP”) committee strives to educate, innovate, and advocate for low-carbon high-quality kidney care.
Over the next year, this Journal will feature articles from a diverse group of patients and care providers representing multiple stakeholders in Canadian kidney care, as well as offer perspectives from our international colleagues. For patients ready to adopt a low carbon lifestyle, we will introduce a Planetary Health kidney diet, and for funders and prescribers of kidney care services, we will describe low carbon therapeutic substitutions available now and on the near horizon. Nursing leaders will outline their distinctive roles in sustainable kidney care, and we will learn how to optimally steward existing dialysis resources. We will collaborate with our primary care partners to explore how to optimally recognize and delay progression of early stages of kidney disease. Our Canadian Quality Improvement colleagues will offer what is, to our knowledge, the first rigorously derived sustainability quality indicators, balanced with patient outcomes. Finally, we will describe ongoing projects in British Columbia to report carbon emissions of kidney care, a major advance toward the SNAP goal of providing carbon calculation for kidney care services so that individual prescribers can, when equipoise exists, facilitate treatment decisions that care for the environment while caring for patients.
We hope these series of articles, the first sustainability collection in the kidney literature, will equip Canadian and international kidney care communities with the necessary tools to provide quality patient care in our era of escalating climate change, recognizing that caring for the environment is caring for patients. Inaction is not an option. What will you tell your patients that you did to protect their health in this changing climate, and what will you tell our youth, and yourself, that you did to avert climate disaster?
Footnotes
Ethics Approval and Consent to Participate: Not applicable.
Consent for Publication: All contributing authors freely consent to their participation in and contribution to this editorial.
Availability of Data and Materials: No primary data was used for this editorial. All data cited in the text is fully referenced.
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iDs: Caroline E. Stigant  https://orcid.org/0000-0003-2578-0966
https://orcid.org/0000-0003-2578-0966
Tasleem Rajan  https://orcid.org/0000-0003-4343-2041
https://orcid.org/0000-0003-4343-2041
References
- 1.Historical (1750–2014) anthropogenic emissions of reactive gases and aerosols from the Community Emissions Data System (CEDS). Geosci Model Dev. 2018;11:369-408. doi: 10.5194/gmd-11-369-2018. [DOI] [Google Scholar]
- 2.Andrew RM.A comparison of estimates of global carbon dioxide emissions from fossil carbon sources. Earth Syst Sci Data. 2020;12:1437-1465. doi: 10.5194/essd-12-1437-2020. [DOI] [Google Scholar]
- 3.Friedlingstein P, Jones MW, O-Sullivan M, et al. Global carbon budget 2021. Earth Syst Sci Data. 2022;14:1917-2005. doi: 10.5194/essd-14-1917-2022. [DOI] [Google Scholar]
- 4.Carbon Dioxide| Vital Signs—Climate Change: Vital Signs of the Planet (nasa.gov). https://climate.nasa.gov/vital-signs/carbon-dioxide/. Accessed November 12, 2022.
- 5.IPCC. Summary for policymakers [Pörtner H-O, Roberts DC, Poloczanska ES, et al., eds.]. In: Pörtner H-O, Roberts DC, Tignor M., et al. eds. Climate Change 2022: Impacts, Adaptation and Vulnerability. Contribution of Working Group II to the Sixth Assessment Report of the Intergovernmental Panel on Climate Change. Cambridge, UK and New York, NY: Cambridge University Press; 2022:3-33. doi: 10.1017/9781009325844.001. [DOI] [Google Scholar]
- 6.Thomas CD, Cameron A, Green RE, et al. Extinction risk from climate change. Nature. 2004;427(6970):145-148. [DOI] [PubMed] [Google Scholar]
- 7.World Meteorological Association c/o UN News. https://news.un.org/en/story/2021/05/1092842. Accessed November 12, 2022.
- 8.Armstrong McKay DI, Staal A, Abrams JF, et al. Exceeding 1.5 C global warming could trigger multiple climate tipping points. Science. 2022;377(6611):eabn7950. [DOI] [PubMed] [Google Scholar]
- 9.Climate Effects on Health— CDC. https://www.cdc.gov/climateandhealth/effects/. Accessed November 12, 2022.
- 10.Zhao Q, Guo Y, Ye T, et al. Global, regional, and national burden of mortality associated with non-optimal ambient temperatures from 2000 to 2019: a three-stage modelling study. Lancet Planet Health. 2021;5(7):e415-e425. [DOI] [PubMed] [Google Scholar]
- 11.Vohra K, Vodonos A, Schwartz J, Marais EA, Sulprizio MP, Mickley LJ.Global mortality from outdoor fine particle pollution generated by fossil fuel combustion: results from GEOS-Chem. Environ Res. 2021;195:110754. [DOI] [PubMed] [Google Scholar]
- 12.Araujo JA, Barajas B, Kleinman M, et al. Ambient particulate pollutants in the ultrafine range promote early atherosclerosis and systemic oxidative stress. Circ Res. 2008;102(5):589-596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Bowe B, Artimovich E, Xie Y, Yan Y, Cai M, Al-Aly Z.The global and national burden of chronic kidney disease attributable to ambient fine particulate matter air pollution: a modelling study. BMJ Glob Health. 2020;5(3):e002063. doi: 10.1136/bmjgh-2019-002063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Young SE, Khoshnaw LJ, Johnson RJ.Climate and the nephrologist: the intersection of climate change, kidney disease, and clinical care. Clin J Am Soc Nephrol. 2022;18:1-7. doi: 10.2215/CJN.08530722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Fakheri RJ, Goldfarb DS.Ambient temperature as a contributor to kidney stone formation: implications of global warming. Kidney Int. 2011;79(11):1178-1185. [DOI] [PubMed] [Google Scholar]
- 16.Berry P, Schnitter R, eds. Health of Canadians in a Changing Climate: Advancing Our Knowledge for Action. Chapter 10. Ottawa, ON, Canada: Government of Canada; 2022. [Google Scholar]
- 17.Blum MF, Feng Y, Anderson GB, Segev DL, McAdams-DeMarco M, Grams ME.Hurricanes and mortality among patients receiving dialysis. J Am Soc Nephrol. 2022;33(9):1757-1766. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Romanello M, Di Napoli C, Drummond P, et al. The 2022 report of the Lancet Countdown on health and climate change: health at the mercy of fossil fuels. The Lancet. 2022;400(10363):1619-1654. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Barraclough KA, Agar JW.Green nephrology. Nat Rev Nephrol. 2020;16(5):257-268. [DOI] [PubMed] [Google Scholar]
- 20.Bendine G, Autin F, Fabre B, et al. Haemodialysis therapy and sustainable growth: a corporate experience in France. NDT. 2020;35:2154-2160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Blankestijn PJ, Bruchfeld A, Cozzolino M, et al. Nephrology: achieving sustainability. NDT. 2020;35:2030-2033. [DOI] [PubMed] [Google Scholar]
- 22.Connor A, Lillywhite R, Cooke MW.The carbon footprints of home and in-center maintenance hemodialysis in the United Kingdom. Hemodial Int. 2011;15(1):39-51. [DOI] [PubMed] [Google Scholar]
- 23.Lim AE, Perkins A, Agar JW.The carbon footprint of an Australian satellite haemodialysis unit. Aust Health Rev. 2013;37(3):369-374. [DOI] [PubMed] [Google Scholar]
- 24.https://www.epa.gov/greenvehicles/greenhouse-gas-emissions-typical-passenger-vehicle#driving. Accessed November 12, 2022.
- 25.Grafals M, Sanchez R.The environmental impact of dialysis vs transplantation [abstract]. Am J Transplant. 2016; 16(suppl 3). [Google Scholar]
- 26.Canadian Net-Zero Emissions Accountability Act. https://www.canada.ca/en/services/environment/weather/climatechange/climate-plan/net-zero-emissions-2050/canadian-net-zero-emissions-accountability-act.html. Updated March 29, 2022. Accessed November 12, 2022.
- 27.Salas RN, Maibach E, Pencheon D, Watts N, Frumkin H.A pathway to net zero emissions for healthcare. BMJ. 2020;371:m3785. [DOI] [PubMed] [Google Scholar]
- 28.Tennison I, Roschnik S, Ashby B, et al. Health care’s response to climate change: a carbon footprint assessment of the NHS in England. Lancet Planet Health. 2021;5(2):e84-e92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Canada Health Sector Emissions Fact Sheet. Global road map for health care decarbonization. https://healthcareclimateaction.org/fact-sheets/en/English%20-%20Canada. Accessed November 12, 2022.
- 30.Rajan T, Amin SO, Davis K, et al. Redesigning Kidney Care for the anthropocene: a new framework for planetary health in nephrology. Can J Kidney Health Dis. 2022;9:20543581221116215. [DOI] [PMC free article] [PubMed] [Google Scholar]