Abstract
Introduction
Telemedicine services saw substantial surges in their use during the COVID-19 pandemic due to the lockdowns and characteristics of the pandemic. Therefore, the authors aimed to systematically review the telemedicine services provided during the COVID-19 pandemic and their potential applications.
Methods
The authors searched PubMed, Scopus, and Cochrane databases on September 14, 2021. Then, the retrieved records underwent two-step title/abstract and full-text screening processes, and the eligible articles were included for qualitative synthesis.
Results
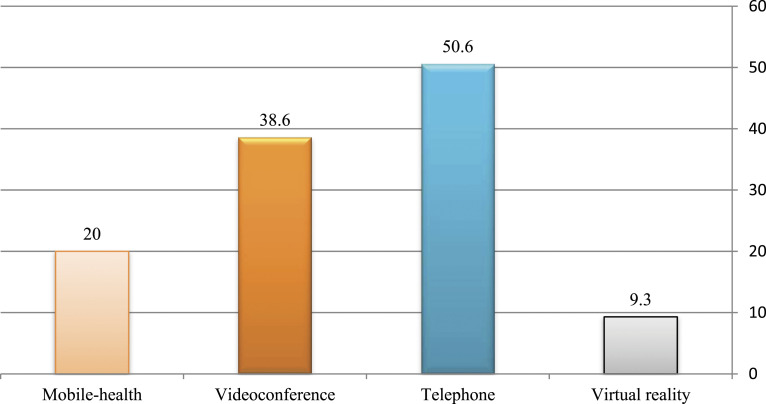
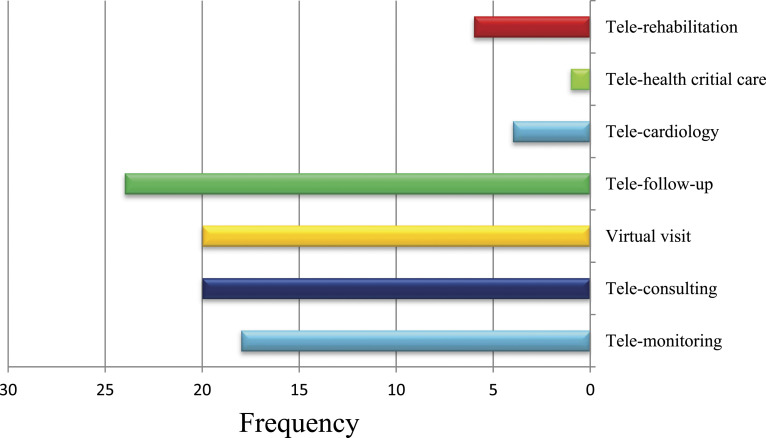
The review of studies demonstrated that the telephone is listed 38 times, making it the most common technology used in telemedicine. Video conferencing is also mentioned in 29 articles, as well as other technologies: Mobile-health (n = 15), Virtual reality (n = 7). According to the findings of the present study, Tele-follow-up (n = 24), Tele-consulting (n = 20), Virtual visits (20), and Tele-monitoring (n = 18) were the most widely used telemedicine applications.
Conclusion
Telemedicine has been an effective approach to COVID-19 management. Telemedicine technology is going to play a key role in the future of health medicine, patient consultation, and many other extended applications of health care in remote rural locations.
Keywords: COVID-19, SARS-CoV-2, telemedicine, telemonitoring, teleconsulting, applications
Introduction
On March 2020, the World Health Organization (WHO), after the large expansion of SARS-CoV-2 infection, declared the coronavirus disease 2019 (COVID-19) outbreak as a public health emergency. 1 The extension rate of COVID-19 and its characteristics have highlighted the need for quick solutions. 2 To mitigate infection risk and the spread of the virus, various public health policies have been implemented, including the use of face coverings, social distancing mandates, closure of nonessential businesses and quarantine strategies.3–5 The healthcare systems also changed the way healthcare services were delivered to comply with these policies and prioritized social distancing as a substantial factor in slowing the spread of viruses.6–9 The healthcare systems have been confronted with challenges not only in treating COVID-19-afflicted cases but also in managing patients with other acute and chronic diseases.5,10 Therefore, the COVID-19 pandemic has significantly impacted the routine patient care workflow and health care resources.11,12 In this regard, health services have had to adapt and prioritize the safe delivery of care, limiting outpatient care. 13
As a result, there is a clear need for effective and innovative tools to address the continuum of care for patients with COVID-19 and others in need healthcare of service. 14 Telemedicine has been considered an ideal tool to manage these emergency and rapid regulatory changes. 15 Out of necessity, telemedicine and e-health platforms have been suggested as a main strategy for continuous patient care while mitigating the spread of viruses and conserving valuable healthcare resources.10,16
There are various definitions of telemedicine. The formal definition of telemedicine according to the WHO is the “delivery of healthcare services, where distance is a critical factor, by all healthcare professionals using information and communication technologies for the exchange of valid information for the diagnosis, treatment, and prevention of disease and injuries, research and evaluation, and for continuing education of health care providers (HCPs), all in the interest of advancing the health of individuals and their communities. 3 ”
During the COVID-19 pandemic era, telemedicine has become a key component in patient healthcare delivery. 5 The use of telemedicine technology brings essential benefits to improve access to quality and timely care while maintaining physical distancing, preventing disease, home COVID-19 screening and monitoring in epidemic conditions.17–19 Telemedicine offers great potential to provide services without the need for face-to-face contact and avoid exposure to respiratory secretions. 10 Telemedicine allows healthcare providers to focus more resources on pandemic usage and at the same time, continue caring for patients with chronic diseases who need follow-up and clinical intervention. 20 The use of telemedicine during the COVID-19 pandemic will help to decrease the time required to get a diagnosis and initiate treatment, quarantine or follow-up a patient.21,22 This technology uses electronic communication tools such as smartphones application or videoconferences. It allows clinicians to evaluate rapidly and detect patients with early signs of COVID-19 before they arrive at the emergency department. 21 Telemedicine is the best approach to avoid the inundation of hospitals with COVID-19 patients. 20 Through video calls, they determine which patients are at high risk and require an urgent referral and avoid overloading the healthcare system. 12
On the other hand, the benefits of using telemedicine technologies in epidemics allow helping patients with chronic diseases that are not infected with COVID-19 to receive medical attention without the risk of exposure to other patients in the hospital.16,7 Likewise, telemedicine technologies allow rapid consultation among specialists for medical decision-making in the face of COVID-19.12,23 This is an important achievement for rural areas. 12
Although the various applications and advantages of telemedicine hold promise for managing pandemic response, its adoption has limitations such as technological infrastructure, provider and patient education, quality of healthcare services, equipment costs, the privacy of sensitive patient data, legal issues and low motivation of providers.24,25 Establishing clear rules and regulations by governments and health organizations can contribute to avoiding misused telemedicine. Improving telemedicine infrastructure will facilitate a higher quality of care to a larger scale of patients. Furthermore, ethical considerations must be taken into account.26,27
Telemedicine technologies are tools specializing in the e-health sector. The solutions developed and functioned by these technologies contribute to the development of the health care system, patient care or clinical and epidemiological study in a wide range of uses. Telemedicine technologies’ activity is at the convergence of various disciplines (software engineering, space technologies, big data and data science, medicine and clinical operations, etc.) in an international environment and a start-up spirit. 24 During the current pandemic, the development of telemedicine applications using above mentioned technologies, increased as the healthcare system sought ways to improve access to safe and affordable care. Telemedicine applications provide remote healthcare delivery with the help of telecommunications technology. 28 This systematic review aimed to summarize the status related to the use of telemedicine technologies and applications and provide an overview of how these tools are being used to face the current COVID-19 pandemic.
Methods
Research question
In this comprehensive review, we are going to determine the telemedicine technologies and applications during the COVID-19 era by going through the available resources. To ensure the validity and reliability of results, this study adhered to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) checklist. Considering the important role of the result of systematic reviews, the use of standard methodology has an effective role in confirming the study results. One of the standard methodology tools is the PRISMA checklist.
The PRISMA statement provides updated reporting guidance for systematic reviews that reflects advances in methods to identify, select, appraise, and synthesis studies. We anticipate that the PRISMA statement will benefit authors, editors, and peer reviewers of systematic reviews, and different users of reviews, including guideline developers, policy makers, healthcare providers, patients, and other stakeholders.
The aim of this study was to investigate telemedicine technologies and applications during the COVID-19 era. In this research, we sought answers to the following questions:
1- What kind of telemedicine technologies are used during the COVID-19 pandemic?
2- What are the applications for providing remote services during the COVID-19?
3- What are the advantages, disadvantages and impact of these technologies on the healthcare services for COVID-19?
Information sources
The authors systematically searched three widely used academic online search sources, including PubMed, Scopus, and Cochrane. We searched the medical subject heading (MeSH) database and looked upon similar studies to generate the keywords for COVID-19 and telemedicine.
Search strategy
The search was based on two search themes (COVID-19 and telemedicine) using the Boolean operator “OR.” The searches were combined by using the Boolean term “AND.” Alternative names for telemedicine, identified through various literature sources, as well as details on searching each database were added (Supplementary material 1). Search strategy for PubMed is mentioned in as an example:
A. [COVID-19] OR [SARS-CoV-2] OR [SARS-CoV2] OR [Novel coronavirus] OR [2019-nCoV]
B. [Telemedicine] OR [Tele-health] OR [Tele-care] OR [Tele-monitoring,] OR [Tele-consulting]
C. [A] and [B]
Selection process
After downloading identified studies, the duplicate records were removed. Two investigators followed a two-phase screening process to determine the eligible results. They were aware, vigilant, educated and had PhD degree and did not have any conflict of interest. They also have expertise in reviewing articles and manuscripts and were a member of Pueblo’s reviewer database. First, they examined the title and abstract of the retrieved records and the ineligible studies were removed. Then, their full texts were evaluated based on their cohesion to the aim and inclusion/exclusion criteria and the eligible studies were included for qualitative synthesis.
Eligibility criteria
The authors included the original articles related to the research question from the initiation of the pandemic (December 2019) until September 14, 2021. Therefore, the exclusion criteria are as follows:
1) Non-original studies, including reviews, commentaries, opinions, or any studies with no original data,
2) Pure laboratory or animal studies not conducted on humans,
3) Case reports,
4) Ongoing projects (e.g., articles discussing the protocol of a future study),
5) Abstracts or conference abstracts, or no available full text.
Data collection process
Five investigators read the full texts of the eligible articles and extracted the data from the relevant included studies. We collected the following data from each study: A) the first author and country; B) results of identified telemedicine technologies, service receivers (Who? Which patients or staff?), their applications to provide healthcare services for COVID-19, and other findings to construct the results section. All included studies were English language and across all countries. Another independent investigator reviewed the extracted data and solved discrepancies and issues between the other investigators.
Risk of bias assessment
We utilized the Newcastle-Ottawa Scale (NOS) risk assessment tool to calculate the risk of bias in the included studies (Table 1). NOS provide a maximum score of nine for each study in three categories of selection, comparability, and exposure.
Table 1.
The results of Newcastle-Ottawa scale (NOS) risk of bias assessment.
| The first author (reference) | Selection (out of 4) | Comparability (out of 2) | Exposure/outcome (out of 3) | Total score (out of 9) |
|---|---|---|---|---|
| Accorsi, TAD 29 | **** | * | *** | 8 |
| Alessi, J 30 | *** | * | ** | 6 |
| Alhadramy, 31 OM | **** | * | *** | 8 |
| Anuran, GO 32 | **** | ** | ** | 8 |
| Boehm, K 33 | *** | ** | ** | 7 |
| Ceccato, F 34 | **** | * | *** | 8 |
| D’Anna, L 35 | *** | - | ** | 5 |
| Deeb, W 36 | *** | * | ** | 6 |
| DenkboyOngen, Y 37 | *** | ** | *** | 8 |
| De Matheus, A.SM 38 | ** | * | ** | 5 |
| Dhahri, A A 39 | ** | * | ** | 5 |
| Domínguez-Moreno, R 40 | **** | * | ** | 7 |
| Esper, CD 41 | **** | ** | *** | 9 |
| Gadzinski, AJ 42 | *** | ** | *** | 8 |
| Garcia-Huidobro, D 43 | **** | ** | ** | 9 |
| Garg, S 44 | *** | ** | ** | 7 |
| Ghai, B 45 | **** | ** | ** | 8 |
| Gios, L 46 | *** | - | *** | 6 |
| Gonzalez Gerez, JJ 47 | *** | - | ** | 5 |
| Graça, TUS 48 | **** | * | *** | 8 |
| Guo, Z 49 | **** | * | *** | 8 |
| Indraratna P 50 | *** | - | *** | 6 |
| Jurado, JR 51 | **** | * | *** | 8 |
| Kim, JW 52 | **** | * | *** | 8 |
| Kwon, CY 53 | *** | * | *** | 7 |
| Lai, FH 54 | ** | * | ** | 5 |
| Lau, K 55 | *** | - | *** | 6 |
| Lavery, MJ 56 | **** | * | *** | 8 |
| Lee, J M 57 | **** | ** | *** | 9 |
| Li, J 58 | **** | * | *** | 8 |
| Li, JO 59 | **** | - | *** | 7 |
| Lott, A 60 | **** | ** | *** | 9 |
| Martínez García, M 61 | *** | ** | *** | 8 |
| Martos Pérez, F 62 | **** | ** | ** | 9 |
| Meyer, B.C 63 | *** | ** | ** | 7 |
| Mortezavi, M 64 | **** | ** | ** | 8 |
| Munusamy, T 65 | *** | - | *** | 6 |
| Naves, LA 66 | **** | ** | *** | 9 |
| Ozturk, B 67 | **** | * | *** | 8 |
| Pépin, JL 68 | **** | * | *** | 8 |
| Raad, M 69 | *** | - | ** | 5 |
| Ribeiro, E 70 | *** | - | *** | 6 |
| Raposo, A 71 | **** | - | *** | 7 |
| Rodriguez-Blanco, C 72 | **** | * | *** | 8 |
| Rogers, BG 73 | **** | - | *** | 7 |
| Shaw, JG 74 | *** | - | *** | 6 |
| Sicsic, I 75 | **** | - | *** | 7 |
| Silven, AV 76 | **** | * | *** | 8 |
| Silver, JK 77 | **** | ** | ** | 8 |
| So, H 78 | *** | ** | ** | 7 |
| Tan, WPM 79 | **** | * | *** | 8 |
| Tourkmani MA 80 | *** | - | ** | 5 |
| Vasta, R 81 | *** | * | ** | 6 |
| Wilkinson, J.E 82 | *** | ** | *** | 8 |
| Wong, AKC 83 | *** | * | ** | 6 |
| Zweig, 84 S | *** | * | ** | 6 |
Informed consent
This article was a review one and we have not an informed consent.
Results
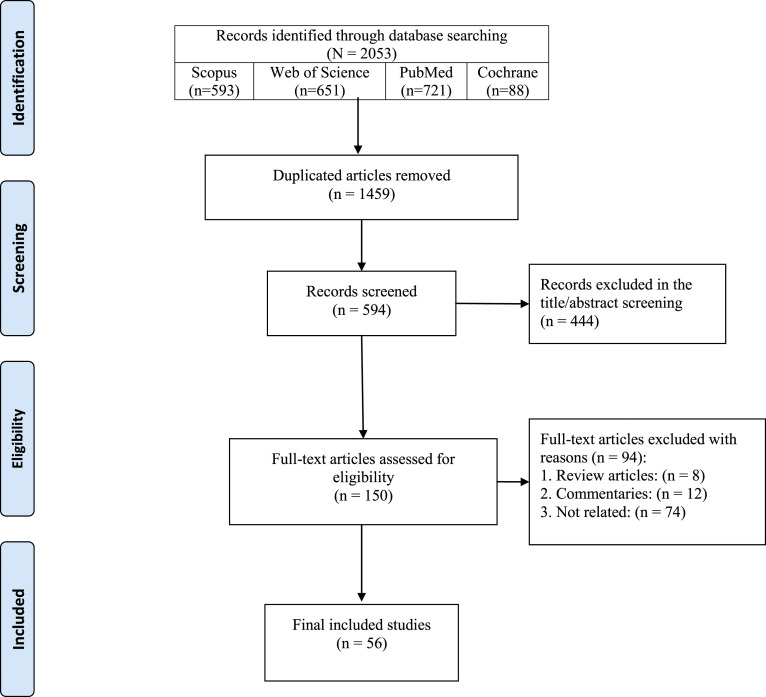
In this study, 2,053 documents were identified using a systematic search strategy. After an initial review of the retrieved articles, 1,459 duplicates were removed, and the titles and abstracts of the remaining sources were assessed. After applying the selection criteria, 538 articles were deleted in the two-phase screening process, and 56 articles met the inclusion criteria and were included in the final review (Figure 1).
Figure 1.
PRISMA flow diagram of the study’s selection process.
We have reviewed 56 studies. In this review, we evaluated identified telemedicine technologies and applications to provide healthcare services for COVID-19. Our findings are based on two categories: Telemedicine Technologies and Applications. In this study, service receivers were also examined (Table 2). The advantages, disadvantages, and impact of telemedicine tools and applications on healthcare services during the COVID-19 pandemic are shown in Table 3.
Table 2.
Identified telemedicine technologies and applications to provide healthcare services for COVID-19.
| ID | The first author (reference) | Country | Service receivers (who? Which patients or staff?) | Telemedicine technologies | Applications | Other | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Virtual reality | Telephone | Videoconference | Mobile-health | Tele-monitoring | Tele-consulting | Virtual visit | Tele-follow-up | Tele-cardiology | Tele-health critical care (TCC) | Tele-rehabilitation | |||||
| 1 | Accorsi, TAD 29 | Brazil | Patients with COVID-19 | ✓ | — | — | ✓ | ✓ | ✓ | ✓ | ✓ | — | — | — | Eligible patients were instructed to examine themselves and perform exhalation maneuvers to obtain a Roth score. Calculating Ruth’s score involves teaching patients to breathe deeply and trying to count loudly from 1 to 30 before exhaling. After this procedure, patients are asked to take three deep breaths and the test is repeated. Time is calculated by the examiner. The second test is valid |
| 2 | Alessi, J 30 | Brazil | Patients with type 2 DM | — | ✓ | — | — | — | ✓ | — | — | — | — | — | The intervention was a included weekly telephone calls and providing educational materials on issues related to mental health, healthy habits, and diabetes care |
| 3 | Alhadramy, 31 OM | Saudi Arabia | All patients over 18 years of age seeking cardiac counseling | ✓ | ✓ | — | — | — | — | — | ✓ | ✓ | — | — | When standardized heart-to-heart counseling is compromised, a structured TBCC is considered feasible, an effective and promising alternative to providing the most cardiac care to the community. When done correctly, testing patients is helpful, follow-up, monitoring, Remote counseling for heart patients |
| 4 | Anuran, GO 32 | Philippine | Employees and students | ✓ | ✓ | — | ✓ | — | — | — | ✓ | — | — | — | (OCRA) system, email, SMS, follow-up |
| 5 | Boehm, K 33 | Germany | Urologic patients | — | ✓ | ✓ | — | — | ✓ | — | — | — | — | — | — |
| 6 | Ceccato, F 34 | Italy | Endocrine patients | ✓ | ✓ | — | — | — | — | — | — | — | — | — | Tele-Endo visit: Clinical data are reported in the web-based database of the AOU Padova, used as an(eCRF), to guide the endocrinologist during the endocrine triage, a multiple-choice questionnaire (with yes/no answer) has been adopted, email, follow-up |
| 7 | D'Anna, L 35 | UK | Patients with transient ischemic attack | ✓ | ✓ | — | — | — | ✓ | — | — | ✓ | — | — | Virtual consultations, electronic medical records of eligible patients were retrieved from the Imperial College healthcare NHS trust online medical notes system |
| 8 | Deeb, W 36 | USA | Individuals with parkinsonism | — | ✓ | ✓ | — | ✓ | ✓ | — | — | — | — | — | A laptop computer was the most commonly used device/zoom and facetime application |
| 9 | DenkboyOngen, Y 37 | Turkey | Pediatric endocrinology patients | — | ✓ | — | — | ✓ | — | ✓ | ✓ | — | — | — | The patients were supported in terms of receiving their prescriptions/Data were obtained from e-mail and e-messages |
| 10 | De Matheus, A.SM 38 | Brazil | Patients with type 1 DM | — | ✓ | — | — | ✓ | ✓ | — | — | — | — | — | Tele monitoring protocol included phone calls and e-mails |
| 11 | Dhahri, A A 39 | UK | Patients and clinicians | — | ✓ | ✓ | — | — | ✓ | — | — | — | — | — | Video-enabled telemedicine/A laptop computer was the most commonly used device |
| 12 | Domínguez-Moreno, R 40 | Mexico | Patients with neurological disorders | — | ✓ | ✓ | — | — | ✓ | ✓ | ✓ | — | — | — | Zoom, Doxy.me, and WhatsApp |
| 13 | Esper, CD 41 | USA | Patients with movement disorders | — | ✓ | ✓ | — | — | — | ✓ | ✓ | — | — | — | Zoom |
| 14 | Gadzinski, AJ 42 | USA | Urology patients | — | ✓ | ✓ | ✓ | — | — | ✓ | — | — | — | — | A desktop, laptop, smartphone, or tablet can all be used |
| 15 | Garcia-Huidobro, D 43 | Chile | Patients receiving telemedicine | — | — | ✓ | — | — | — | ✓ | — | — | — | — | Patients and providers receive a Zoom link |
| 16 | Garg, S 44 | India | Patients | — | ✓ | ✓ | ✓ | ✓ | ✓ | — | ✓ | — | — | — | Using platforms such as Doxy.me, eVisit, Vsee, Mendetc. |
| 17 | Ghai, B 45 | India | Patients with chronic pain | — | ✓ | ✓ | ✓ | — | ✓ | — | ✓ | — | — | — | These include apps/videoconference programs installed on the patient’s phone/tab/home computer with a high speed internet connection |
| 18 | Gios, L 46 | Italy | Home-quarantined patients with COVID-19 | — | ✓ | — | ✓ | ✓ | — | — | — | — | — | — | TeleCovid19 |
| App was used for monitoring patients | |||||||||||||||
| 19 | Gonzalez Gerez, JJ 47 | Spain | Patients with COVID-19 | — | ✓ | ✓ | ✓ | — | — | — | ✓ | — | — | ✓ | A desktop, laptop, smartphone, or tablet can all be used, StepsApp |
| 20 | Graça, TUS 48 | Brazil | Patients | — | ✓ | — | — | ✓ | ✓ | — | ✓ | — | — | — | UsdREDcap platform |
| 21 | Guo, Z 49 | China | Outpatient Infant for Retinopathy of prematurity | — | — | — | ✓ | ✓ | ✓ | — | ✓ | — | — | — | |
| 22 | Indraratna P 50 | Australia | Patients with acute coronary syndrome | — | ✓ | — | ✓ | ✓ | — | — | ✓ | ✓ | — | — | TeleClinical care - cardiac (TCC-cardiac) app |
| 23 | Jurado, JR 51 | Colombia | Patients who required an endoscopic procedure | — | ✓ | — | — | — | — | — | ✓ | — | — | — | |
| 24 | Kim, JW 52 | USA | Patients | — | — | ✓ | — | — | ✓ | ✓ | ✓ | — | ✓ | — | Standardizededucation using online training modules, live interactivewebinars, video tutorials, and one-on-one mentoring sessionswith an experienced tele provider for tele providers |
| 25 | Kwon, CY 53 | Korea | Patients with COVID-19 | — | — | — | ✓ | — | — | — | — | — | — | — | Individuals may achieve efficient self-management of their symptoms through YouTube videos. Communication software, such as Zoom |
| 26 | Lai, FH 54 | China | Patients with cognitive impairment | — | ✓ | ✓ | — | — | — | — | — | — | — | ✓ | Zoom, WhatsApp, or FaceTime |
| 27 | Lau, K 55 | UK | Patients on the waiting list for consideration of bone conduction hearing devices | — | ✓ | — | — | — | ✓ | — | — | — | — | — | All patients proceeding with surgery were happy with the remote assessment |
| 28 | Lavery, MJ 56 | UK | Patient with Dermatologic diagnosis | — | ✓ | ✓ | — | — | ✓ | — | ✓ | — | — | — | Video tele dermatology service |
| 29 | Lee, J M 57 | USA | Patients with type 1 DM | — | ✓ | ✓ | — | — | — | — | — | — | — | — | Zoom (most popular), FaceTime, Microsoft teams, Doximity, WebEx, BlueJeans, health system developed technology, google Duo, WhatsApp |
| 30 | Li, J 58 | China | Patients with COVID-19 | — | — | — | ✓ | ✓ | ✓ | — | — | — | — | ✓ | RehabApp, consultation via cell phone or WeChat voice call |
| 31 | Li, JO 59 | UK | Patients with urgent ophthalmic concern | — | — | ✓ | — | — | ✓ | ✓ | ✓ | — | — | — | Video call |
| 32 | Lott, A 60 | USA | Pediatric and adult patients | — | — | ✓ | — | — | — | ✓ | ✓ | — | — | — | Primary zip code was used as surrogate for socioeconomic status through use of the zip code median household income |
| 33 | Martínez García, M 61 | Spain | Positive PCR test who were considered high-risk | — | — | — | — | ✓ | — | — | — | — | — | — | In recent years, the Galician health service has developed the TELEA tool, which is integrated into the electronic medical record and is able to perform at-home telemedicine and tele monitoring. With this tool, any patient who has provided the pertinent permission can send information in a pre-established format to their own electronic medical record |
| 34 | Martos Pérez, F 62 | Spain | Mostly elderly | — | ✓ | — | — | — | — | ✓ | ✓ | — | — | — | Videoconferencing was dismissed given the technical difficulties and the heterogeneity of our patients, many of whom are elderly |
| 35 | Meyer, B.C 63 | USA | Inpatient and ambulatory care patient | — | ✓ | ✓ | — | — | — | ✓ | — | — | — | — | UCSDH implemented an electronic health record (EHR), integrated, video visit solution several years ago, but had not scaled the deployment. We chose a mobile-to-mobile ‘‘bring your own device’’ solution for our providers to access and use the EHR and other video visit solutions, which allowed providers to start conducting video visits as soon as they were trained |
| 36 | Mortezavi, M 64 | USA | Rheumatology patients | — | ✓ | ✓ | — | — | — | ✓ | ✓ | — | — | — | The appointment type (in-person, telephone, or video) was recorded. Both telephone and video visits were qualified as “telemedicine,” and patient satisfaction was assessed. Video encounters were completed using the following third-party vend |
| 37 | Munusamy, T 65 | UK | Neurocritical patients | ✓ | — | — | — | — | — | — | — | — | — | — | A random pair of neurosurgery resident and specialist conducted consecutive virtual and physical ward rounds on neurocritical patients. A virtual ward round was first conducted remotely by a specialist who received real-time audiovisual information from a resident wearing smart glasses integrated with telemedicine. Subsequently, a physical ward round was performed together by the resident and specialist on the same patient. The management plans of both ward rounds were compared, and the interrater reliability was measured. On study completion a qualitative survey was performed |
| 38 | Naves, LA 66 | Brazil | Acromegaly outpatients | — | ✓ | ✓ | — | ✓ | ✓ | ✓ | — | — | — | — | The laboratory results were shared with patients by e-mail. A printed prescription was sent to patients' addresses, and an electronic prescription was sent directly to the central pharmacy. Medicine was delivered directly to the patients' homes |
| 39 | Ozturk, B 67 | Turkey | People with overweight and obese | — | — | ✓ | — | — | — | — | — | — | — | ✓ | A significant improvements was obtained in all parameters of physical fitness, quality of life in the telerehabilitation group |
| 40 | Pépin, JL 68 | France | Patients with COVID-19 and other respiratory infections | — | — | — | — | ✓ | — | — | ✓ | ✓ | — | — | Every night tele monitoring data on continuous positive airway pressure (CPAP) device use, the first-line therapy for obstructive sleep apnea (OSA), is collected worldwide |
| 41 | Raad, M 69 | UK | Trauma and orthopedics patients | — | ✓ | — | — | — | ✓ | ✓ | — | — | — | — | During COVID-19, all clinics were converted to telephone clinics unless a patient required a plaster change or wound check |
| 42 | Ribeiro, E 70 | Portugal | Psychological patients | — | ✓ | — | ✓ | — | — | — | — | — | — | — | During COVID-19 pandemic Psychologist communicate with patient via telephone and its necessary because of pandemic Consequences |
| 43 | Raposo, A 71 | Portugal | Patients with COVID-19 | — | ✓ | — | — | — | — | ✓ | — | — | — | — | A new app was introduced that name is e-CoVing |
| 44 | Rodriguez-Blanco, C 72 | Spain | Patients with COVID-19 | — | ✓ | ✓ | ✓ | — | — | — | ✓ | — | — | ✓ | A desktop, laptop, smartphone, or tablet can all be used, StepsApp |
| 45 | Rogers, BG 73 | USA | Patients with HIV and COVID-19 | — | ✓ | ✓ | — | ✓ | — | ✓ | — | — | — | — | Zoom was used but offering telephone for some people who can’t use zoom |
| 46 | Shaw, JG 74 | USA | Patients with COVID-19 | — | ✓ | — | — | ✓ | — | — | — | — | — | — | Physicians and nurses (RNs) participate in program, were trained using Microsoft Teams™ |
| 47 | Sicsic, I 75 | USA | Patients with COVID-19 | — | — | ✓ | — | ✓ | — | — | — | — | — | — | Zoom was used |
| 48 | Silven, AV 76 | Netherlands | Patients with COVID-19 | — | — | ✓ | — | ✓ | — | — | — | — | — | — | They gave patients a COVID box that contain a thermometer, pulse oximeter, blood pressure monitor, and a safety bag (for return of the devices) and then monitored them with telemedicine |
| 49 | Silver, JK 77 | USA, Israel | People with overweight or obesity | — | — | ✓ | — | — | ✓ | — | — | — | — | — | Zoom® |
| 50 | So, H 78 | China | Lupus patients | — | — | ✓ | — | — | — | — | ✓ | — | — | — | Telemedicine use in clinic to reduce potential exposure to COVID-19 |
| 51 | Tan, WPM 79 | Singapore | Orthopedic patients | — | — | ✓ | — | ✓ | ✓ | — | ✓ | — | — | — | Zoom was used |
| 52 | Tourkmani MA 80 | Saudi Arabia | Adult patients with type 2 DM | ✓ | ✓ | — | ✓ | — | ✓ | — | — | — | — | ✓ | Patients were educated about the risk of COVID-19 to patients with DM, and about the importance of precautionary measures such as wearing masks, frequent hand washing, social distancing and avoiding crowded places where the risk of infection is highو monitoring, consulting, follow-up |
| 53 | Vasta, R 81 | Italy | Neurological or psychological patients | — | ✓ | ✓ | — | — | — | ✓ | — | — | — | — | Patients can directly talk with their doctor |
| 54 | Wilkinson, J.E 82 | USA | Primary care patients who no-showed to appointments and did not receive care | — | ✓ | — | — | — | — | ✓ | — | — | — | — | Calls were monitored to be better |
| 55 | Wong, AKC 83 | China | Older adults who are homebound | — | ✓ | — | ✓ | — | — | ✓ | ✓ | — | — | — | telephone call and weekly video messages via WhatsApp |
| 56 | Zweig, 84 S | Columbia | Patients with respiratory complaints | — | — | ✓ | — | — | — | ✓ | — | — | — | — | Zoom was used |
| Frequency | 7 | 38 | 29 | 15 | 18 | 20 | 20 | 24 | 4 | 1 | 6 | ||||
Abbreviations: DM: Diabetes Mellitus, TBCC; Telephone-based cardiac consultation, PGH; Philippine General Hospital, UPM; UP Manila, OCRA; Online Consultation, AOU; AziendaOspedale-Università, eCRF; electronic Case Report/Record Form, NHS; National Health Service.
Table 3.
Advantages, disadvantages, and impact identified technologies on the healthcare services for COVID-19.
| ID | Advantages | Disadvantages | Impact |
|---|---|---|---|
| Virtual reality | -Telemedicine care | -Non-fulfillment of immediate intervention (if face-to-face consultation is required) | -Virtual clinic |
| -Self-examination | |||
| -Initial medical evaluation | -Geographical separation of patients and providers | -Potentially universal resource | |
| -Prevent burnout of health care providers | -Lack of physical examination | -Healthcare systems virtual- and telecommunication-care | |
| -Virtual triaging | -Absence of a physician-patient relationship | ||
| -Telemonitoring | -Limited access to medical records | ||
| -Social distancing | -Limitations on virtual physical examination | ||
| -Management of long-term chronic diseases | -Poor quality of care | ||
| Telephone | -Telemedicine care | -Non-fulfillment of immediate intervention (if face-to-face consultation is required) | -Virtual clinic |
| -Prompt inexpensive medical consultation around the clock | -Absence of a physician-patient relationship | -Healthcare systems virtual- and telecommunication-care | |
| -Virtual triaging | -Limited access to medical records | ||
| -Telemonitoring | -Limitations on virtual physical examination | ||
| -Social distancing | -Poor quality of care | ||
| -Management of long-term chronic diseases | - Requirement of internet access | ||
| -Some patients were followed more closely | - Insufficient technological ability of the patients | ||
| -Preserve inpatient resources and prevent avoidable staff and patient exposures | - Inability to charge the patient due to lack of hospital system | ||
| -Inability to document official record | |||
| -Request for communication after working hours | |||
| -Inappropriate use of the line due to either inadequate expectations regarding the provided services or clients’ personality characteristics | |||
| Videoconference | -More time-efficient | -Lack of familiarity | -Virtual clinic |
| -Able to see the doctor and the doctor to see the patient | -Provider cannot perform as thorough of an examination through video | ||
| Mobile-health | -Telemedicine care | -Non-fulfillment of immediate intervention (if face-to-face consultation is required) | -Virtual clinic |
| -Self-examination | -Geographical separation of patients and providers | -Potentially universal resource | |
| -Prompt inexpensive medical consultation around the clock | -Lack of physical examination | ||
| -Initial medical evaluation | -Absence of a physician-patient relationship | ||
| -Prevent burnout of health care providers | -Limited access to medical records | ||
| -Virtual triaging | -Limitations on virtual physical examination | ||
| -Telemonitoring | -Poor quality of care | ||
| -Social distancing | -Lack of familiarity with using the internet | ||
| Tele-monitoring | -Self-examination | -Geographical separation of patients and providers | -Potentially universal resource |
| -Initial medical evaluation | -Lack of physical examination | ||
| -Prevent burnout of health care providers | -Lack of familiarity with using the internet | ||
| Tele-consulting | -Telemedicine care | -Non-fulfillment of immediate intervention (if face-to-face consultation is required) | -Virtual clinic |
| -Self-examination | -Geographical separation of patients and providers | -Potentially universal resource | |
| -Prompt inexpensive medical consultation around the clock | -Lack of physical examination | ||
| -Initial medical evaluation | |||
| -Prevent burnout of health care providers | |||
| Virtual visit | -Self-examination | -Geographical separation of patients and providers | -Potentially universal resource |
| -Initial medical evaluation | -Lack of physical examination | ||
| -Prevent burnout of health care providers | -Chances of misdiagnosis | ||
| -Not all pharmacy services can be provided remotely | - Lack of clarity on medico legal implications | ||
| -Reduce the need for personal protective equipment leading to reduction in resource consumption | -Reduced educational opportunities are given limited opportunities to conduct physical exams | ||
| -Reducing COVID-19 exposure and use of personal protective equipment (PPE) without significantly compromising quality of care | |||
| Tele-follow-up | -Self-examination | -Geographical separation of patients and providers | -Potentially universal resource |
| -Initial medical evaluation | -Lack of physical examination | -Healthcare systems virtual- and telecommunication-care | |
| -Prevent burnout of health care providers | -Absence of a physician-patient relationship | ||
| -Virtual triaging | -Limited access to medical records | ||
| -Tele-monitoring | -Limitations on virtual physical examination | ||
| -Management of long-term chronic diseases | -Poor quality of care | ||
| Tele-cardiology | -Telemedicine care | -Lack of physical examination | -Healthcare systems virtual- and telecommunication-care |
| Tele-health critical care (TCC) | -Telemedicine care | N/A | -Virtual clinic |
| Tele-rehabilitation | -Telemedicine care | -Non-fulfillment of immediate intervention (if face-to-face consultation is required) | -Virtual clinic |
Telemedicine technologies, as well as the applications of these technologies, were reviewed. Studies in these articles have shown that the telephone is listed 38 times, making it the most common technology used in telemedicine. Video conferencing has also been mentioned in 29 articles (Figure 2).
Figure 2.
Percentage of studies that identified telemedicine technologies.
According to the findings of the present study, Tele-follow-up (n = 24), Tele-consulting (n = 20), Virtual visits (20), and Tele-monitoring (n = 18) were the most widely used telemedicine applications. The frequency of these applications is demonstrated in Figure 3.
Figure 3.
Percentage of studies that identified applications of telemedicine technologies.
Most studies were related to the USA with 13, the UK with seven, Brazil with five, china with four, Spain with four and Italy with three articles. The rest of the selected articles were for countries Turkey, India, Colombia, and Portugal with two articles and the Philippines, Germany, Mexico, Chile, Korea, Australia, France, Singapore, and the Netherlands with one article.
Discussion
With the outbreak of the COVID-19 pandemic, the authors provide a comprehensive review of telemedicine and its applications and roles in the delivery of healthcare organizations. The present study, in which a total of 56 articles related to telemedicine solutions and applications are analyzed, indicates the application of telemedicine technology. This review has proved the high usage of telemedicine, especially during the COVID-19 pandemic, applications in Tele-follow-up, Tele-consulting, Virtual visits, as well as Tele-monitoring. Telephone, Video conferencing, Mobile-health and Virtual reality are the four main telemedicine technologies that are mentioned in the articles. The highest frequency of telemedicine services was through these four technologies. Also, since these technologies had been useful before accruing the COVID-19 pandemic, some of the articles suggested that the role and applications of these technologies will never diminish. Accordingly, this systematic review aimed to identify the telemedicine services provided and meaningful telemedicine applications through the COVID-19 pandemic.
Telemedicine technology holds great promise for patients during the pandemic duration. The most significant effect is provided to reduce potential exposure to SARS-CoV-2.85,86 Many people point out that telemedicine has existed in some way or another since the telephone was invented. 85 Telephone calls were the first method of connecting patients with HCPs at a distance, and it remains a crucial component of care in different situations. The telephone is now used in medical areas such as cardiology,35,50,87 dermatology, 56 mental health,36,54,78 rheumatology, 64 trauma and orthopedics, 69 neurologic disorders,40,81 urology,33,42 endocrine disorders34,39,57,65 to deliver improved treatment, follow up, consulting, monitoring and primary care to populations underserved by healthcare providers. It is often thought to be a way to reduce notably the expense of treating health problems such as diabetes type I and II, heart failure, and HIV which benefit from continuous observation of a patient’s condition38,50,73,80 Telephone calls deal with these problems in various areas, including performing cognitive or psychiatric assessments, consulting, drug therapies or social/lifestyle changes, primary care and remotely observing patients.50,54,82 The results of our study are consistent with the results of studies by Cervinoetla and Matthewson on the role of Telephone Triage before Attending Medical Office and telephone support service during the COVID-19 pandemic.88,89
Virtual Reality (VR) systems have modified communication in telemedicine devices, making them more immersive. In VR, physicians and their teams can now observe a 3D monitor when performing operations.87,90 The telehealth platform might use VR to simulate the patient’s data, and a graphical environment with video conferencing to streamline communication with a physician. 45 Specialists such as endocrinologists, cardiologists, infectious diseases, and neurosurgeons can answer electronically and educate about COVID-19, perform virtual examination and triage, virtual consulting, virtual monitoring and follow-up, and also patients can set up a virtual meeting with the physician.29,32,80 These virtual consultations can remove avoidable in-person referrals to specialists, reduce wait times for a specialist response, and avoid unnecessary travel.31,34 The results of our study are consistent with the results of a study by Ravi Pratap Singh et al., On the Significant applications of virtual reality for the COVID-19 pandemic. VR technology can reduce the face-to-face interaction of doctors with infected COVID-19 patients and avoid unnecessary travel. 91
Video conference technologies offer quick and simple methods of providing care remotely during the current pandemic. By employing video conferencing, physicians can educate groups of patients. Also, this enables medical teams to cooperate and hold video meetings on complex and urgent situations.64,73,75,76,84 Video conferencing was one of the most common technologies during the COVID-19 pandemic. Video conferencing is used in various situations, such as learning and videoconference and its role in teaching medical students and using this technology to maintain the education of residents, doctor-patient communication and communication between the medical team, Videoconference for clinical recommendations for treatment by the family of patients via providers during COVID‐19. In this regard, the results of the present study are in the same direction as previous studies such as Chick et al., and Matheson et al.92–94
Mobile-health let allows patients to count calories, record vital signs, record exercise, and control prescription doses and schedules, which are very useful and crucial for patient self-management and monitoring like hypertension, heart failure, diabetes and home-quarantined patients with COVID-19 during the pandemic. Mobile apps are also used for telehealth visits or electronic visits.44,46,50 Telemedicine application software companies utilize app connectivity and cloud technologies to grant real-time distant patient follow-up, monitoring, visiting and consulting. It saves time for both patients and physicians by monitoring health progress. 9 The telehealth apps and platforms ensure accurate patient record data. It helps pharmacies, customers, and prescribing physicians by delivering healthcare services more quickly.46,48,66 With an e-prescription feature, physicians can convey prescriptions with minor errors. It would help to save time while also improving linkage and customer satisfaction. 66 Thus Telemedicine via mobile health apps and tools, with the rise of digital devices and wearable and portable sensors, can help monitor and manage signs and symptoms. The results of the present study are consistent with Ming et al., and Lukas et al., studies on emerging telemedicine tools and the importance of health services through mobile apps.20,95
The wide variety of free software and platforms currently available, such as Zoom, WeChat, WhatsApp, Google Duo, WebEx, FaceTime, Redcap platform, Doxy.me platform, emails and also new software were introduced like e-CoVig, Microsoft Teams and TELEA tool; adequate lighting; good camera quality; and a good internet connection allow for the proper evaluation of patients.40,41,44,48,53,54,57,71,73–75,79,84 In current studies, Zoom was the most frequent application used mostly for Video-conference and virtual visits.36,40,41,43,54,53,57,71,73,77,79,84
As telemedicine is being used widely, preparing specific guidelines by worldwide institutions (e.g., WHO) might help HCPs and patients feel safe when using telemedicine. Moreover, developers should pay attention to data security and assure physicians and patients regarding their privacy. Despite the extent of the use of telemedicine, there are also opportunities to expand the area of applying this modern way of communication. For instance, providing specific platforms for each sub-specialty of medicine so that patients could communicate with their most appropriate healthcare provider as fast as they can. 96 Optimization of telemedicine could be summarized in the following domains: (1) safety: decreasing HCPs and patients’ exposure to infected cases and decreasing spread of COVID-19 for the so called “social distancing”; (2) effective: providing care not only for severely ill cases but also for all community with mild symptoms that require care to prevent delayed treatment and diagnosis, and even for decreasing stress and concern; (3) conservation: preventing waste of time, energy, and equipment; (4) timely: decreasing unwanted delays to prevent waste of time and energy of both HCPs and patients, also to decrease potential harms of delayed treatment; (5) patient-centered: to provide care based on patient’s needs and individual values; (6) balanced: same care quality for all individuals and avoid bias due to different socioeconomic status; (7) availability: infrastructures for delivering care and connectivity at both ends; (8) regulations: decreasing all restriction by governments also providing formal licenses for telemedicine implementation; (9) reporting: quality assurance mechanisms to report adverse events.21,96,97
Telemedicine, as a novel approach, is encountered various challenges. First, it is a primarily internet-based platform; thus, it would be difficult for people in developing countries to use telemedicine, as their internet access and quality are quite poor. Consequently, prioritizing expanding internet access worldwide to benefit from telemedicine should be considered. Physical examination is not applicable in telemedicine due to its virtual nature. Therefore, the quality of care in telemedicine is not the same as in-person care, especially for elderly patients that cannot use new technologies properly. Data privacy and security is another challenge due to the vulnerability of software platforms, which requires protective measures. Lack of regulations and legal obligations act as a barrier to limiting the extension of telemedicine Providers should prepare backgrounds of trust for patients, so that a wide range of people can turn to using telemedicine as their first choice when it comes to clinical issues. Specific benefits can be considered for physicians and HCPs to encourage them to utilize these platforms.
Conclusion
The current review discusses the telemedicine services provided and applications of available telemedicine technologies during the COVID-19 pandemic. The results indicate that telemedicine provides remote healthcare services and can help better control the disease. The study also determines the applications and frequency use of four main technologies used in the delivery services during the COVID-19 pandemic and their applications. As telemedicine technology further evolves with the expansion of the internet in rural areas, it will play a key role in the future of health medicine, patient consultation, and many other extended health care applications. The effectiveness of these telemedicine technologies as a critical topic can be investigated in upcoming research. Future research, particularly related to the implementation and compliance of telemedicine technologies during the non-emergency in delivering health services to support patients, will yield help.
Supplemental Material
Supplemental material for Telemedicine technologies and applications in the era of COVID-19 pandemic: A systematic review by Esmaeil Mehraeen, Seyed Ahmad Seyed Alinaghi, Mohammad Heydari, Amirali Karimi, Abdollah Mahdavi, Mehrnaz Mashoufi, Arezoo Sarmad, Peyman Mirghaderi, Ahmadreza Shamsabadi, Kowsar Qaderi, Pegah Mirzapour, Amirata Fakhfouri, Hadiseh Azadi Cheshmekabodi, Kimia Azad, Seyed Ali Bagheri Zargande, Shahram Oliaei, Parisa Yousefi Konjdar, Farzin Vahedi, Tayebeh Noori in Health Informatics Journal
Supplemental material for Telemedicine technologies and applications in the era of COVID-19 pandemic: A systematic review by Esmaeil Mehraeen, Seyed Ahmad Seyed Alinaghi, Mohammad Heydari, Amirali Karimi, Abdollah Mahdavi, Mehrnaz Mashoufi, Arezoo Sarmad, Peyman Mirghaderi, Ahmadreza Shamsabadi, Kowsar Qaderi, Pegah Mirzapour, Amirata Fakhfouri, Hadiseh Azadi Cheshmekabodi, Kimia Azad, Seyed Ali Bagheri Zargande, Shahram Oliaei, Parisa Yousefi Konjdar, Farzin Vahedi, Tayebeh Noori in Health Informatics Journal
Acknowledgements
The present study was extracted from the research project with research code IR-KH-1400-07-023 and ethics committee code IR.KHALUMS.REC.1400.007 entitled “A framework for implementing of telemedicine technology with COVID-19 pandemic approach in Emam Khomeini Hospital” conducted at Khalkhal University of Medical Sciences in 2020. We thank the statistical population and all the participants for taking the time to contribute to the study.
Author contributions: The conception and design of the study: Esmaeil Mehraeen and Tayebeh Noori. Methodology: Esmaeil Mehraeen, SeyedAhmad SeyedAlinaghi and Mohammad Heydari. Acquisition of data: Amirali Karimi, Esmaeil Mehraeen, Abdollah Mahdavi, Tayebeh Noori and Mehrnaz Mashoufi. Writing original draft preparation: Arezoo Sarmad, Peyman Mirghaderi, Ahmadreza Shamsabadi, Kowsar Qaderi, Pegah Mirzapour, Amirata Fakhfouri, Hadiseh Azadi Cheshmekabodi, Kimia Azad, Seyed Ali Bagheri Zargande, Shahram Oliaei, Parisa Yousefi Konjdar, and Farzin Vahedi. Writing—Review and Editing: SeyedAhmad SeyedAlinaghi and Amirali Karimi. Validation: Esmaeil Mehraeen, Mohammad Heydari and Tayebeh Noori.
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Transparency statement: Tayebeh Noori affirms that this manuscript is an honest, accurate, and transparent account of the study being reported; that no important aspects of the study have been omitted; and that any discrepancies from the study as planned (and, if relevant, registered) have been explained.
Availability of data and material: The authors confirm that the data supporting the findings of this study are available within the article [and/or] its supplementary materials.
Supplemental material: Supplemental material for this article is available online.
ORCID iDs
Esmaeil Mehraeen https://orcid.org/0000-0003-4108-2973
SeyedAhmad SeyedAlinaghi https://orcid.org/0000-0003-3210-7905
Farzin Vahedi https://orcid.org/0000-0002-9847-0638
Tayebeh Noori https://orcid.org/0000-0001-9295-0756
References
- 1.Dadras O, Alinaghi SAS, Karimi A, et al. Effects of COVID-19 prevention procedures on other common infections: A systematic review. Eur J Med Res 2021; 26(1): 67–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Puro NA, Feyereisen S. Telehealth availability in US hospitals in the face of the COVID-19 pandemic. J Rural Health 2020; 36(4): 577–583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Samarrai R, Riccardi AC, Tessema B, et al. Continuation of telemedicine in otolaryngology post-COVID-19: Applications by subspecialty. Am J Otolaryngol 2021; 42(3): 102928–■■■■. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Mohammad H, Elham M, Mehraeen Eet al. Identifying data elements and key features of a mobile based self care application for patients with COVID-19 in Iran. Health Informatics J 2021; 27(4): 1–15, doi: 10.1177/14604582211065703. [DOI] [PubMed] [Google Scholar]
- 5.Colbert GB, Venegas-Vera AV, Lerma EV. Utility of telemedicine in the COVID-19 era. Rev Cardiovasc Med 2020; 21(4): 583–587. [DOI] [PubMed] [Google Scholar]
- 6.Contreras CM, Metzger GA, Beane JD, et al. Telemedicine: Patient-provider clinical engagement during the COVID-19 pandemic and beyond. J Gastrointest Surg 2020; 24(7): 1692–1697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bitar H, Alismail S. The role of eHealth, telehealth, and telemedicine for chronic disease patients during COVID-19 pandemic: A rapid systematic review. Digit Health 2021; 7: e-collection 2021 January–December. doi: 10.1177/20552076211009396 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Mehraeen E, Safdari R, Mohammadzadeh N, et al. Mobile based applications and functionalities for self management of people living with HIV. Stud Health Technol Inform 2018; 248: 172–179. [PubMed] [Google Scholar]
- 9.Mehraeen E, Safdari R, Seyedalinaghi SA, et al. Identifying and validating requirements of a mobile based self management system for people living with HIV. Stud Health Technol Inform 2018; 248: 140–147. [PubMed] [Google Scholar]
- 10.Shanbehzadeh M, Kazemi-Arpanahi H, Kalkhajeh SG, et al. Systematic review on telemedicine platforms in lockdown periods: Lessons learned from the COVID-19 pandemic. J Educ Health Promot 2021; 10: 211–221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Khoshrounejad F, Hamednia M, Mehrjerd A, et al. Telehealth-based services during the COVID-19 pandemic: A systematic review of features and challenges. Front Public Health 2021; 9: 711762–■■■■. doi: 10.3389/fpubh.2021.711762 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hincapié MA, Gallego JC, Gempeler A, et al. Implementation and usefulness of telemedicine during the COVID-19 pandemic: a scoping review. J Prim Care Community Health 2020; 11: 2150132720980612–■■■■. doi: 10.1177/2150132720980612 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Seron P, Oliveros MJ, Gutierrez-Arias R, et al. Effectiveness of telerehabilitation in physical therapy: A rapid overview. Phys Ther 2021; 101(6): pzab053–■■■. doi: 10.1093/ptj/pzab053 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Monaghesh E, Hajizadeh A. The role of telehealth during COVID-19 outbreak: a systematic review based on current evidence. BMC Public Health 2020; 20(1): 1193–■■■. doi: 10.1186/s12889-020-09301-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Eichberg DG, Basil GW, Di L, et al. Telemedicine in Neurosurgery: Lessons learned from a systematic review of the literature for the COVID-19 era and beyond. Neurosurgery 2020; 88(1): 1–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Alonso SG, Marques G, Barrachina I, et al. Telemedicine and e-health research solutions in literature for combatting COVID-19: A systematic review. Health Technol (Berl) 2021; 11(2): 257–266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Vidal-Alaball J, Acosta-Roja R, Pastor Hernández N, et al. Telemedicine in the face of the COVID-19 pandemic. Aten Primaria 2020; 52(6): 418–422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Galiero R, Pafundi PC, Nevola R, et al. The importance of telemedicine during COVID-19 pandemic: A focus on diabetic retinopathy. J Diabetes Res 2020; 2020: 9036847–■■■. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ajibade A, Younas H, Pullan M, et al. Telemedicine in cardiovascular surgery during COVID-19 pandemic: A systematic review and our experience. J Card Surg 2020; 35(10): 2773–2784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Lukas H, Xu C, Yu Y, et al. Emerging telemedicine tools for remote COVID-19 diagnosis, monitoring, and management. ACS Nano 2020; 14(12): 16180–16193. [DOI] [PubMed] [Google Scholar]
- 21.Bokolo AJ. Exploring the adoption of telemedicine and virtual software for care of outpatients during and after COVID-19 pandemic. Ir J Med Sci 2021; 190(1): 1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Bokolo J. Use of telemedicine and virtual care for remote treatment in response to COVID-19 pandemic. J Med Syst 2020; 44(7): 132–141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Busch AB, Sugarman DE, Horvitz LE, et al. Telemedicine for treating mental health and substance use disorders: Reflections since the pandemic. Neuropsychopharmacology 2021; 46(6): 1068–1070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Hong YR, Lawrence J, Williams D, et al. Population level interest and telehealth capacity of US hospitals in response to COVID-19: Cross sectional analysis of google search and national hospital survey data. JMIR Public Health Surveill 2020; 6(2): 18961–■■■. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Parisien RL, Shin M, Constant M, et al. Telehealth utilization in response to the novel coronavirus (COVID-19) pandemic in orthopaedic surgery. J Am Acad Orthop Surg 2020; 28(11): 487–492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Jaffe DH, Lee L, Huynh S, et al. Health inequalities in the use of telehealth in the united states in the lens of COVID-19. Popul Health Manag 2020; 23(5): 368–377. [DOI] [PubMed] [Google Scholar]
- 27.Garfan S, Alamoodi A, Zaidan B, et al. Telehealth utilization during the Covid-19 pandemic: A systematic review. Computers in Biology and Medicine 2021; 138(3); 104878–■■■. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Wittenberg E, Goldsmith JV, Chen C, et al. Opportunities to improve COVID-19 provider communication resources: A systematic review. Patient Educ Couns 2021; 104(3): 438–451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Accorsi TAD, Amicis KD, Brígido ARD, et al. Assessment of patients with acute respiratory symptoms during the COVID-19 pandemic by telemedicine: Clinical features and impact on referral. Einstein 2020; 18: 1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Alessi J, de Oliveira GB, Franco DW, et al. Telehealth strategy to mitigate the negative psychological impact of the COVID-19 pandemic on type 2 diabetes: A randomized controlled trial. Acta Diabetol 2021; 58(7): 899–909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Alhadramy OM. The structure and the outcome of telephone based cardiac consultations during lockdown: A lesson from COVID-19. Cureus 2020; 12(11): 11585–■■■. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Anuran GO, Villarante KL, Mejia-Samonte MD, et al. Telemedicine services in the University of the Philippines health service during the COVID-19 pandemic: A two week process documentation and analysis. Acta Med Philipp 2021; 55(2): 256–263. [Google Scholar]
- 33.Boehm K, Ziewers S, Brandt MP, et al. Telemedicine online visits in urology during the COVID-19 pandemic potential, risk factors, and patients’ perspective. Eur Urol 2020; 78(1): 16–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Ceccato F, Voltan G, Sabbadin C, et al. Telemedicine versus face to face consultation in endocrine outpatients clinic during COVID-19 outbreak: A single center experience during the lockdown period. J Endocrinol Invest 2021; 44(8): 1689–1698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.D’Anna L, Ellis N, Bentley P, et al. Delivering telemedicine consultations for patients with transient ischaemic attack during the COVID-19 pandemic in a comprehensive tertiary stroke centre in the United Kingdom. Eur J Neurol 2021; 28(10): 3456–3460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Deeb W, Hess CW, Gamez N, et al. Response to telemedicine visits from patients with parkinsonism during the COVID-19 pandemic on postvisit surveys. J Patient Exp 2021; 8: 2374373521997224–■■■. doi: 10.1177/2374373521997224 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Denkboy Ongen Y, Eren E, Sahin KC, et al. Telemedicine experiences at a pediatric endocrinology clinic during the COVID-19 pandemic. Ir J Med Sci 2022; 191: 985–990, Epub ahead of print 2021 Jun 7. doi: 10.1007/s11845-021-02677-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.De Mattos Matheus AS, Cabizuca CA, Tannus LRM, et al. Telemonitoring type 1 diabetes patients during the COVID-19 pandemic in Brazil: Was it useful? Arch Endocrinol Metab 2021; 65(1): 105–111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Dhahri AA, Iqbal MR, Pardoe H. Agile application of video telemedicine during the COVID-19 pandemic. Cureus 2020; 12(11): 11320–■■■. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Domínguez-Moreno R, García-Grimshaw M, Chávez-Martínez OA, et al. Global and community health: implementation of and patient satisfaction with the first neurologic telemedicine program in Mexico during COVID-19. Neurology 2021; 97(6): 293–296. [DOI] [PubMed] [Google Scholar]
- 41.Esper CD, Scorr L, Papazian S, et al. Telemedicine in an academic movement disorders center during COVID-19. J Mov Disord 2021; 14(2): 119–125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Gadzinski AJ, Ellimoottil C, Odisho AYet al. Telemedicine in urology: A crash course during the COVID-19 pandemic. Urol Times 2020; 48(4): 35–42. [Google Scholar]
- 43.Garcia Huidobro D, Rivera S, Valderrama Chang S, et al. System wide accelerated implementation of telemedicine in response to COVID-19: Mixed methods evaluation. J Med Internet Res 2020; 22(10): 22146–■■■. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Garg S, Gangadharan N, Bhatnagar N, et al. Telemedicine: embracing virtual care during COVID-19 pandemic. J Family Med Prim Care 2020; 9(9): 4516–4520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Ghai B, Malhotra N, Bajwa SJS. Telemedicine for chronic pain management during COVID-19 pandemic. Indian J Anaesth 2020; 64(6): 456–462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Gios L, Crema Falceri G, Micocci S, et al. Use of eHealth platforms and apps to support monitoring and management of home quarantined patients with COVID-19 in the province of Trento, Italy: App development and implementation. JMIR Form Res 2021; 5(5): 25713–■■■. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Gonzalez-Gerez JJ, Saavedra-Hernandez M, Anarte-Lazo E, et al. Short term effects of a respiratory telerehabilitation program in confined COVID-19 patients in the acute phase: a pilot study. Int J Environ Res Public Health 2021; 18(14): 7511–■■■. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Graça TUdS, Santos AL, Yamamoto G, et al. Telemonitoring programme on COVID-19 for a low-income community in Brazil: Case study. BMJ Innov 2021; 7(2): 342–346. [DOI] [PubMed] [Google Scholar]
- 49.Guo Z, Ma N, Wu Y, et al. The safety and feasibility of the screening for retinopathy of prematurity assisted by telemedicine network during COVID-19 pandemic in Wuhan, China. BMC Ophthalmol 2021; 21(1): 258–■■■. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Indraratna P, Biswas U, Yu J, et al. Trials and tribulations: mhealth clinical trials in the COVID-19 pandemic. Yearb Med Inform 2021; 30(1): 272–279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Jurado JR, Nieto JHS, Gaitán JO, et al. Endoscopy mitigation strategy with telemedicine and low-cost device use for COVID-19 prevention: A fourth-level Colombian center experience. Arab J Gastroenterol 2021; 22(2): 170–173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Kim JW, Lame M, Szalay L, et al. Telemedicine surge for pediatric patients in response to the COVID-19 pandemic in New York City. Telemed J E Health 2021; 27(10): 1105–1110. [DOI] [PubMed] [Google Scholar]
- 53.Kwon CY, Kwak HY, Kim JW. Using mind body modalities via telemedicine during the COVID-19 crisis: Cases in the republic of Korea. Int J Environ Res Public Health 2020; 17(12): 4477–■■■. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Lai FHY, Yan EWH, Yu KKY, et al. The protective impact of telemedicine on persons with dementia and their caregivers during the COVID-19 pandemic. Am J Geriatr Psychiatry 2020; 28(11): 1175–1184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Lau K, Greenwood L, Proctor V, et al. Remote assessments for bone conduction hearing devices during the COVID-19 pandemic. Eur Arch Otorhinolaryngol 2022; 279(7): 3297–3300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Lavery MJ, Phillips D, Yip V, et al. Survey to evaluate the patient experience of virtual telephone consultations during the COVID-19 pandemic. Clin Dermatol 2021; 39(2): 334–336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Lee JM, Carlson E, Albanese-O’Neill A, et al. Adoption of telemedicine for type 1 diabetes care during the COVID-19 pandemic. Diabetes Technol Ther 2021; 23(9): 642–651. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Li J, Xia W, Zhan C, et al. A telerehabilitation programme in post-discharge COVID-19 patients (TERECO): A randomised controlled trial. Thorax 2022; 77(7): 697–706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Li JPO, Thomas AAP, Kilduff CLS, et al. Safety of video-based telemedicine compared to in-person triage in emergency ophthalmology during COVID-19. EClinicalMedicine 2021; 34: 100818–■■■. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Lott A, Campbell KA, Hutzler L, et al. Telemedicine utilization at an academic medical center during COVID-19 pandemic: Are some patients being left behind? Telemed J E Health 2022; 28(1): 44–50. [DOI] [PubMed] [Google Scholar]
- 61.Martínez-García M, Bal-Alvarado M, Santos Guerra F, en nombre del Equipo de Seguimiento Compartido TELEA-COVID Lugo. Equipo TELEA COVID-19 Lugo , et al. Monitoring of COVID-19 patients by telemedicine with telemonitoring. Rev Clin Esp 2020; 220(8): 472–479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Martos Pérez F, Martín-Escalante MD, Olalla Sierra J, et al. The value of telephone consultations during COVID-19 pandemic. An observational study. QJM 2021; 114(10): 715–720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Meyer BC, Friedman LS, Payne K, et al. Medical undistancing through telemedicine: A model enabling rapid telemedicine deployment in an academic health center during the COVID-19 pandemic. Telemed J E Health 2021; 27(6): 625–634. [DOI] [PubMed] [Google Scholar]
- 64.Mortezavi M, Lokineni S, Garg M, et al. Rheumatology patient satisfaction with telemedicine during the COVID-19 pandemic in the United States. J Patient Exp 2021; 8: 23743735211008825–■■■. doi: 10.1177/23743735211008825 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Munusamy T, Karuppiah R, Bahuri NFA, et al. Telemedicine via smart glasses in critical care of the neurosurgical patient COVID-19 pandemic preparedness and response in neurosurgery. World Neurosurg 2021; 145: 53–e60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Naves LA, Rosa IN, Lima TAdS, et al. Implementation and monitoring of a telemedicine model in acromegalic outpatients in a low income country during the COVID-19 pandemic. Telemed J E Health 2021; 27(8): 905–914. [DOI] [PubMed] [Google Scholar]
- 67.Ozturk B, Duruturk N. Effect of telerehabilitation applied during COVID-19 isolation period on physical fitness and quality of life in overweight and obese individuals. Int J Obes (Lond) 2022; 46(1): 95–99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Pépin JL, Bailly S, Borel JC, et al. Detecting COVID-19 and other respiratory infections in obstructive sleep apnoea patients through CPAP device telemonitoring. Digit Health 2021; 7: 20552076211002957–■■■. doi: 10.1177/20552076211002957. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Raad M, Ndlovu S, Neen D. Assessment of the efficacy of telephone medicine consultations in trauma and orthopaedics during COVID-19 using the ashford clinic letter score. Cureus 2021; 13(3): 13871–■■■. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Ribeiro E, Sampaio A, Gonçalves MM, et al. Telephone based psychological crisis intervention: The Portuguese experience with COVID-19. Couns Psychol Q 2020; 34(1): 432–446. [Google Scholar]
- 71.Raposo A, Marques L, Correia R, et al. E-covig: A novel mhealth system for remote monitoring of symptoms in covid-19. Sensors 2021; 21(10): 3397–■■■. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Rodriguez-Blanco C, Gonzalez-Gerez JJ, Bernal-Utrera C, et al. Short term effects of a conditioning telerehabilitation program in confined patients affected by COVID-19 in the acute phase. A pilot randomized controlled trial. Medicina (Kaunas) 2021; 57(7): 684–■■■. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Rogers BG, Coats CS, Adams E, et al. Development of telemedicine infrastructure at an LGBTQ+ clinic to support HIV prevention and care in response to COVID-19, providence, RI. AIDS Behav 2020; 24(10): 2743–2747. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Shaw JG, Sankineni S, Olaleye CA, et al. A novel large scale integrated telemonitoring program for COVID-19. Telemed J E Health 2021; 27(11): 1317–1321. [DOI] [PubMed] [Google Scholar]
- 75.Sicsic I, Jr., Chacon AR, Zaw M, et al. A case of SARS-CoV-2 reinfection in a patient with obstructive sleep apnea managed with telemedicine. BMJ Case Rep 2021; 14(2): 240496–■■■. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Silven AV, Petrus AHJ, Villalobos-Quesada M, et al. Telemonitoring for patients with COVID-19: recommendations for design and implementation. J Med Internet Res 2020; 22(9): 20953–■■■. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Silver JK, Finkelstein A, Minezaki K, et al. The impact of a culinary coaching telemedicine program on home cooking and emotional well-being during the COVID-19 pandemic. Nutrients 2021; 13(7): 2311–■■■. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.So H, Szeto CC, Tam LS. Patient acceptance of using telemedicine for follow up of lupus nephritis in the COVID-19 outbreak. Ann Rheum Dis 2021; 80: e97–■■. doi: 10.1136/annrheumdis-2020-218220 [DOI] [PubMed] [Google Scholar]
- 79.Marcus Tan WP, Sayampanathan AA, Tan TC, et al. Rapid deployment of a telemedicine service in orthopaedic surgery during the COVID-19 pandemic. Singapore Med J 2022; 63: 621–627. doi: 10.11622/smedj.2020156 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Torkamani AM, Alharbi TJ, Rsheed AMB, et al. The impact of telemedicine on patients with uncontrolled type 2 diabetes mellitus during the COVID-19 pandemic in Saudi Arabia: Findings and implications. J Telemed Telecare 2021; 0(0): 1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Vasta R, Moglia C, D’Ovidio F, et al. Telemedicine for patients with amyotrophic lateral sclerosis during COVID-19 pandemic: An Italian ALS referral center experience. Amyotroph Lateral Scler Frontotemporal Degener 2021; 22(3–4): 308–311. [DOI] [PubMed] [Google Scholar]
- 82.Wilkinson JE, Bowen G, Gonzalez-Wright J. A student telephone intervention for primary care patient safety during the COVID-19 pandemic. PRiMER 2021; 5: 10–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Wong AKC, Wong FKY, Chow KKS, et al. Effect of a telecare case management program for older adults who are homebound during the COVID-19 pandemic: A pilot randomized clinical trial. JAMA Netw Open 2021; 4(9): e2123453–■■■. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Zweig S. Patient doctor telemedicine: Virtual care in the era of COVID-19 and beyond. Mo Med 2020; 117(3): 175–176. [PMC free article] [PubMed] [Google Scholar]
- 85.Haleem A, Javaid M, Singh RP, et al. Telemedicine for healthcare: Capabilities, features, barriers, and applications. Sens Int 2021; 2: 100117–■■■. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Mahoney MF. Telehealth, telemedicine, and related technologic platforms: current practice and response to the COVID-19 pandemic. J Wound Ostomy Continence Nurs 2020; 47(5): 439–444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Bahl S, Singh RP, Javaid M, et al. Telemedicine technologies for confronting COVID-19 pandemic: A review. J Ind Intg Mgmt 2020; 05(4): 547–561. [Google Scholar]
- 88.Cervino G, Oteri G. COVID-19 Pandemic and telephone triage before attending medical office: Problem or opportunity? Medicina 2020; 56(5): 250–■■■. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Matthewson J, Tiplady A, Gerakios F, et al. Implementation and analysis of a telephone support service during COVID-19. Occup Med 2020; 70(5): 375–381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Whitten PS, Mair FS, Haycox A, et al. Systematic review of cost effectiveness studies of telemedicine interventions. BMJ 2002; 324(7351): 1434–1437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Vaishya R, Bahl S, Singh RP. Letter to the editor in response to: Telemedicine for diabetes care in India during COVID19 pandemic and national lockdown period: Guidelines for physicians. Diabetes Metab Syndr 2020; 14(4): 687–688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Li HL, Chan YC, Huang JX, et al. Pilot study using telemedicine video consultation for vascular patients’ care during the COVID-19 period. Ann Vasc Surg 2020; 68(Suppl 2): 76–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Chick RC, Clifton GT, Peace KM, et al. Using technology to maintain the education of residents during the COVID-19 pandemic. J Surg Educ 2020; 77(4): 729–732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Matheson BE, Bohon C, Lock J. Family based treatment via videoconference: Clinical recommendations for treatment providers during COVID-19 and beyond. Int J Eat Disord 2020; 53(7): 1142–1154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Ming LC, Untong N, Aliudin NA, et al. Mobile health apps on COVID-19 launched in the early days of the pandemic: Content analysis and review. JMIR Mhealth Uhealth 2020; 8(9): e19796–■■■. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Shen YT, Chen L, Yue WW, et al. Digital technology based telemedicine for the COVID-19 pandemic. Front Med (Lausanne) 2021; 8: 646506–■■■. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Bashshur R, Doarn CR, Frenk JM, et al. Telemedicine and the COVID-19 pandemic, lessons for the future. Telemed J E Health 2020; 26(5): 571–573. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material for Telemedicine technologies and applications in the era of COVID-19 pandemic: A systematic review by Esmaeil Mehraeen, Seyed Ahmad Seyed Alinaghi, Mohammad Heydari, Amirali Karimi, Abdollah Mahdavi, Mehrnaz Mashoufi, Arezoo Sarmad, Peyman Mirghaderi, Ahmadreza Shamsabadi, Kowsar Qaderi, Pegah Mirzapour, Amirata Fakhfouri, Hadiseh Azadi Cheshmekabodi, Kimia Azad, Seyed Ali Bagheri Zargande, Shahram Oliaei, Parisa Yousefi Konjdar, Farzin Vahedi, Tayebeh Noori in Health Informatics Journal
Supplemental material for Telemedicine technologies and applications in the era of COVID-19 pandemic: A systematic review by Esmaeil Mehraeen, Seyed Ahmad Seyed Alinaghi, Mohammad Heydari, Amirali Karimi, Abdollah Mahdavi, Mehrnaz Mashoufi, Arezoo Sarmad, Peyman Mirghaderi, Ahmadreza Shamsabadi, Kowsar Qaderi, Pegah Mirzapour, Amirata Fakhfouri, Hadiseh Azadi Cheshmekabodi, Kimia Azad, Seyed Ali Bagheri Zargande, Shahram Oliaei, Parisa Yousefi Konjdar, Farzin Vahedi, Tayebeh Noori in Health Informatics Journal