Abstract
Coronavirus Disease 2019 (COVID-19) continues to spread rapidly. Monoclonal antibodies as well as anti-tumor necrosis factor are considered promising treatments for COVID-19. A prospective cohort study in which patients are divided into three groups. Group 1: moderate and severe COVID-19 patients received standard treatment; Group 2: moderate and severe COVID-19 patients received tocilizumab; Group 3: moderate and severe COVID-19 patients received treatment with infliximab and tocilizumab. 153 patients were recruited in the study. 40 received standard treatment alone, 70 received tocilizumab with standard treatment, and 43 received tocilizumab/infliximab with standard treatment. There was a significant difference in length of hospital stay (10.3, 8.9, and 7.6 days respectively P = 0.03), need for a non-invasive mechanical ventilator (4, 5, and one patient; P = 1.2E−8), intensive care admission (32, 45, and 16 patients; P = 2.5E−5), the occurrence of sepsis (18, 12, and 10 patients; P = 0.005) and in death (42.5%, 14.2%, and 7%; P = 0.0008) which were significantly lower in tocilizumab/infliximab group compared to tocilizumab and standard of care groups. Our study showed that tocilizumab/ infliximab in addition to standard of care was considered a promising treatment for moderate and severe COVID-19 patients.
Trial registration number: ClinicalTrials.gov NCT04734678; date of registration: 02/02/2021.
Subject terms: Viral infection, Biomarkers
Introduction
From the beginning of the COVID-19 pandemic, confirmed cases exceeded 25 million worldwide; around 100 thousand are in Egypt. Until now, several therapeutic approaches have been found for COVID-19, including antivirals, antibodies, anti-inflammatory drugs, targeted immunomodulatory therapies, and anticoagulants. However, responses to such treatments are variable among different patient populations and different stages and manifestations of the disease1. In mid-December-2021, COVID-19 deaths exceeded 5.3 million people globally including more than 21 thousand deaths in Egypt2.
Tocilizumab is a monoclonal antibody that acts as an antagonist on the interleukin-6 (IL-6) receptor. It has been approved as a treatment for idiopathic arthritis and rheumatoid arthritis3 and lately among the therapeutic choices for cytokine storm syndrome (CSS)4, which results from activation of the immune system and release of the pro-inflammatory mediators, chemokines, and cytokines5. The majority of COVID-19 hospitalized patients with evidence of respiratory failure show features that coincide with cytokine storm6,7, so it was assumed that tocilizumab as a hyperinflammatory inflammatory state could be a promising therapeutic option for these patients with CSS8.
Recently, Anti-tumor Necrosis Factor (TNF) therapy has been debated for its potential protective action in severe COVID-19 treatment as shown in a study by Neurath9. TNF may exacerbate lymphopenia by TNF/TNFR1 signalling in T cells8 and T cell dysfunction10. Therefore, TNF inhibitors could be a promising treatment for severe COVID-19 patients. A recent study confirms this finding by showing that patients with inflammatory bowel disease (IBD) who were treated with anti-TNF had significantly fewer hospitalizations and deaths compared to patients treated with other anti-inflammatory medications11.
In this study, we compared the outcomes of hospitalized patients with moderate to severe COVID-19 treated with tocilizumab plus standard management to those treated with infliximab/tocilizumab plus standard treatment and patients treated with standard care alone.
Results
Baseline patients’ characteristics
A total of 153 hospitalized COVID-19 patients were enrolled in the study. Of these, 70 patients received treatment with tocilizumab, 43 received treatment with infliximab/tocilizumab, and 40 received the standard treatment. Table 1 summarizes the baseline characteristics of the three groups. There was no statistically significant difference between the three groups when it came to mean age, inflammatory mediators (Lactate dehydrogenase (LDH), serum ferritin, C-reactive protein (CRP), and liver and heart enzymes), or any other measured parameters. However, there was a significant difference in both oxygen saturation and respiratory rate between the tocilizumab and tocilizumab/ infliximab groups compared to the standard of care group (P value = 0.006 and 0.004, respectively).
Table 1.
Demographic characteristics of studied groups at baseline.
| Variable as (mean ± SD) | Group 1 (Standard care) n = 40 |
Group 2 (Tocilizumab) n = 70 |
Group 3 (Tocilizumab/infliximab) n = 43 |
Significance P < 0.05 |
|---|---|---|---|---|
| Age | 59.6 ± 13.5 | 60.3 ± 11.3 | 60.1 ± 12.9 | P = 0.258 |
| Gender (M/F) (%) | 68/32 | 59/41 | 61/39 | P = 0.38 |
| Oxygen saturation | 89.8 ± 10.5 | 82.5 ± 13.1 | 80.8 ± 13.9 | P = 0.006* |
| P/F ratio | 252.4 ± 128.3 | 170.4 ± 82.3 | 164.5 ± 83.5 | P = 0.163 |
| Respiratory rate | 20.4 ± 5.4 | 28.1 ± 5.3 | 26.9 ± 4.9 | P = 0.004* |
| Maximum temperature | 38 ± 0.84 | 38.2 ± 0.8 | 38.2 ± 0.94 | P = 0.277 |
| Baseline C-reactive protein (CRP) | 230 ± 10.5 | 78 ± 1.1 | 110 ± 1.5 | P = 0.306 |
| Baseline D-dimmer | 731.2 ± 64.4 | 993.9 ± 99.7 | 880.2 ± 96.6 | P = 0.667 |
| Baseline interleukin-6 | 12.4 ± 2.9 | 16.1 ± 1.7 | 14.8 ± 2.5 | P = 0.14 |
| Baseline ferritin | 1017 ± 8.7 | 1224 ± 17.6 | 1267 ± 14.1 | P = 0.337 |
| Serum creatinine | 1.8 ± 1.4 | 1.4 ± 0.5 | 1.8 ± 2.2 | P = 0.647 |
| Total leucocyte count (TLC) | 7.9 ± 4.4 | 7.1 ± 3.5 | 8.9 ± 3.4 | P = 0.568 |
| Absolute lymphocytic count (ALC) | 15.5 ± 9.7 | 15.2 ± 8.4 | 12.1 ± 4.7 | P = 0.871 |
| Neutrophils lymphocytic ratio (NLR) | 8.1 ± 1.8 | 9.6 ± 1.1 | 9.2 ± 2.5 | P = 0.122 |
| Alanine transaminase (ALT) | 51.5 ± 5.6 | 50.7 ± 8.4 | 41.6 ± 12.9 | P = 0.233 |
| Aspartate transaminase (AST) | 51.1 ± 4.7 | 52.3 ± 8.3 | 45.2 ± 9.7 | P = 0.802 |
| Creatinine kinase MB (CKMB) | 7.3 ± 1.6 | 4.6 ± 0.01 | 5.8 ± 1.6 | P = 0.613 |
| Troponin | 0.01 ± 0.01 | 0.01 ± 3.4 | 0.66 ± 2.1 | P = 0.617 |
| Remdesivir (%) | 38% | 28% | 34% | P = 0.03* |
| Lopinavir/ritonavir (%) | 25% | 9.5% | 65.5% | P = 0.007* |
| Hydroxychloroquine (%) | 50% | 27% | 23% | P = 0.62 |
| Ivermectin (%) | 42% | 19% | 39% | P = 0.41 |
SD standard deviation, n number of cases within the group, (%): P > 0.05.
*Significant difference < 0.05.
Change in monitoring parameters before and after each treatment protocol
No discernible change in parameters was seen between the two sets of monitors used before and after therapy among the studied groups except for neutrophils lymphocytic ratio (NLR), which was significantly increased among group 3 compared to the other groups (P = 0.007), as shown in Table 2. Additionally, after treatment, CRP was significantly higher in both groups 1 and 3 compared to group 2 which showed a significant reduction in CRP (P = 0.004). However, for the absolute lymphocytic count (ALC), groups 1 and 3 showed a significant reduction in ALC values compared to group 2 (P = 0.04), as shown in Table 3.
Table 2.
Comparison of the studied groups for the change in the monitoring parameters before and after each treatment protocol among moderate and severe COVID-19 patients.
| Variable | Group 1 (Standard care) n = 40 |
Group 2 (Tocilizumab) n = 70 |
Group 3 (Tocilizumab/infliximab) n = 43 |
Significance P < 0.05 |
|---|---|---|---|---|
| C-reactive protein (CRP) | − 62.5 ± 83.4 | − 102.5 ± 94 | − 83.3 ± 110.2 | P = 0.355 |
| Lactate dehydrogenase (LDH) | − 182 ± 344.6 | − 120.5 ± 402.2 | − 14.3 ± 336.1 | P = 0.457 |
| D-dimmer | − 1.53 ± 10.4 | 0.68 ± 5.4 | 0.46 ± 3.3 | P = 0.567 |
| Ferritin | − 333.2 ± 475.7 | − 43.3 ± 773.7 | − 29.5 ± 553.3 | P = 0.491 |
| Total leucocytic count (TLC) | 1.73 ± 4.5 | 3.5 ± 5.1 | 2.29 ± 5.2 | P = 0.594 |
| Absolute lymphocytic count (ALC) | − 5.3 ± 10.8 | − 2.5 ± 14.8 | − 1.02 ± 5.5 | P = 0.349 |
| Neutrophils lymphocytic ratio (NLR) | − 0.13 ± 9.2 | 2.33 ± 12.1 | 4.9 ± 11.4 | P = 0.007* |
| Alanine transaminase (ALT) | 1.43 ± 7.5 | 33.6 ± 13.5 | 76.8 ± 123.5 | P = 0.118 |
| Aspartate transaminase (AST) | − 8.8 ± 6.5 | 0.73 ± 47.8 | 51.3 ± 58.7 | P = 0.215 |
| Troponin | − 0.001 ± 0.006 | 0.002 ± 0.008 | 0.66 ± 2.1 | P = 0.587 |
SD standard deviation, variables are represented as a mean ± SD.
*Significant difference < 0.05.
Table 3.
Comparison between the studied groups in monitoring parameters post treatment among moderate and severe COVID-19 patients.
| Variable as (mean ± SD) | Group 1 (standard care) n = 40 |
Group 2 (tocilizumab) n = 70 |
Group 3 (tocilizumab/infliximab) n = 43 |
Significance P value |
|---|---|---|---|---|
| Time to improvement | 6.3 ± 4.1 | 5.9 ± 3.9 | 6.4 ± 4.8 | P = 0.097 |
| Length of hospital stay | 10.3 | 8.9 | 7.6 | P = 0.03* |
| PF | 228.7 ± 124.6 | 180.7 ± 62.4 | 210.8 ± 78.8 | P = 0.661 |
| C-reactive protein (CRP) | 43.1 ± 7.5 | 46.8 ± 7.5 | 23.4 ± 8.2 | P = 0.004 |
| Lactate dehydrogenase (LDH) | 297.2 ± 122.8 | 435.6 ± 56.4 | 457.1 ± 177.5 | P = 0.110 |
| D-dimmer | 1.7 ± 1.03 | 2.15 ± 7.3 | 1.67 ± 3.2 | P = 0.185 |
| Ferritin | 561.7 ± 27.1 | 1126.2 ± 86.4 | 937.9 ± 46.8 | P = 0.358 |
| Total leucocytic count (TLC) | 10.4 ± 5.2 | 10.8 ± 5.4 | 11.2 ± 4.9 | P = 0.862 |
| Absolute lymphocytic count (ALC) | 11.7 ± 5.9 | 13.6 ± 12.7 | 10.9 ± 10.8 | P = 0.04* |
| Neutrophils lymphocytic ratio (NLR) | 8.9 ± 1.6 | 14.5 ± 1.8 | 10.1 ± 1.5 | P = 0.355 |
| Alanine transaminase (ALT) | 71.4 ± 7.7 | 102.2 ± 24.7 | 140.7 ± 27 | P = 0.280 |
| Aspartate transaminase (AST) | 56.2 ± 6.9 | 59.2 ± 4.6 | 112.1 ± 6.8 | P = 0.432 |
| Troponin | 0.02 ± 0.014 | 0.003 ± 0.004 | 0.07 ± 0.012 | P = 0.527 |
SD standard deviation, n number of cases within the group.
*Significant, level of significance < 0.05.
Change in monitoring parameters between tocilizumab and tocilizumab/infliximab groups
There was a significant difference in length of hospital stay and in monitoring parameters before and after treatment in favour of the tocilizumab/infliximab group, including CRP, LDH, ALC, and NLR which were significantly lower in the tocilizumab/infliximab group, compared to tocilizumab group. On the other hand, post-treatment liver enzymes were significantly higher in the tocilizumab/infliximab group, as shown in Table 4.
Table 4.
Comparison between the tocilizumab and infliximab/tocilizumab groups among patients with severe COVID-19 symptoms in monitoring parameters post-treatment (Subgroup analysis).
| Variable as (mean ± SD) | Tocilizumab n = 29 |
Tocilizumab/infliximab n = 34 |
Significance P value |
|---|---|---|---|
| Time to improvement | 7.35 ± 4.7 | 7.13 ± 4.1 | P = 0.147 |
| Length of hospital stay | 8.61 | 6.85 | P = 0.04* |
| PF | 210.8 ± 78.8 | 204 ± 97.2 | P = 0.381 |
| C-reactive protein (CRP) | 47.8 ± 8.2 | 20.6 ± 6.2 | P = 0.004* |
| Lactate dehydrogenase (LDH) | 457.1 ± 177.5 | 259.7 ± 105.2 | P = 0.0.005* |
| D-dimmer | 1.67 ± 3.2 | 1.44 ± 4.6 | P = 0.306 |
| Ferritin | 937.9 ± 46.8 | 790.4 ± 78.9 | P = 0.399 |
| Total leucocytic count (TLC) | 11.2 ± 4.9 | 10.6 ± 5.3 | P = 0.07 |
| Absolute lymphocytic count (ALC) | 12.2 ± 10.8 | 7.3 ± 12.7 | P = 0.004* |
| Neutrophils lymphocytic ratio (NLR) | 14.5 ± 1.5 | 10.1 ± 1.7 | P = 0.01* |
| Alanine transaminase (ALT) | 83.6 ± 9.9 | 140.7 ± 8.3 | P = 0.003* |
| Aspartate transaminase (AST) | 57.4 ± 6.2 | 112.2 ± 6.8 | P = 0.0001* |
| Troponin | 0.01 ± 0.01 | 0.07 ± 0.01 | P = 0.27 |
SD standard deviation, n number of cases within the group.
*Significant, level of significance < 0.05.
Clinical outcomes
There was a significant difference among the three groups in need for oxygen, mechanical ventilator, ICU admission, and development of sepsis, as illustrated in Table 5. By the completion of treatment, 34 patients in the tocilizumab/infliximab group (group 3) compared to 26 patients in the tocilizumab (group 2), and 29 patients in the standard treatment group (group 1) were severe (P = 4.6E−6). Eight patients in group 3, compared to 27 patients in group 2 and 18 in group 1 needed low oxygen (P = 0.027). Thirty patients in group 3 required high oxygen or NIMV compared to 10 patients in group 2 and 19 patients in group 1 (P = 0.046). The need for invasive mechanical ventilation (MV) was 1 patient in group 3 versus 5 patients in group 2 and 4 patients in group 1 (P = 1.2E−8). Sixteen patients in group 3, compared to 45 patients in group 2 and 32 in group 1 required ICU admission (P = 2.5E−5). Ten patients in group 3, compared to 12 in group 2 and 18 in group 1 showed subsequent bacterial infection, often established as sepsis (P = 0.005). Additionally, 3 patients died in group 3 compared to 10 patients in group 2 and 17 patients in group 1 (P = 0.0008).
Table 5.
Comparison between the studied groups for moderate and severe COVID-19 patients ‘clinical outcomes.
| Variable % | Group 1 (standard care) n = 40 |
Group 2 (tocilizumab) n = 70 |
Group 3 (tocilizumab/infliximab) n = 43 |
Significance P value |
||||
|---|---|---|---|---|---|---|---|---|
| Severity at enrollment | χ2 = 23.8 | |||||||
| Moderate/severe | 27.5/72.5 | 62.8/37.2 | 20.1/ 79.9 | P = 4.6E−6* | ||||
| Need for low oxygen | ||||||||
| No/yes | 55/45 | 61.4/38.6 | 81.4/18.6 |
χ2 = 7.26 P = 0.027* |
||||
| Need for NIMV OR High oxygen | ||||||||
| No/yes | 52.5/47.5 | 85.7/14.3 | 30.2/69.8 |
χ2 = 36.4 P = 0.046* |
||||
| Need for invasive MV | ||||||||
| No/yes | 90/10 | 93/7 | 97.5/2.5 |
χ2 = 9 P = 1.2E−8* |
||||
| ICU admission | ||||||||
| No/yes | 18.6/81.4 | 35/65 | 62.8/37.2 |
χ2 = 21.2 P = 2.5E−5* |
||||
| Clinical improvement | ||||||||
| No/yes | 22.5/77.5 | 14.2/85.8 | 20.9/79.1 |
χ2 = 4.4 P = 0.36 |
||||
| Death | ||||||||
| No/yes | 57.5/42.5 | 85.8/14.2 | 93/7 |
χ2 = 1.4 P = 0.0008* |
||||
| Occurrence of sepsis | ||||||||
| No/yes | 55.8/44.2 | 82.9/17.1 | 77.5/22.5 |
χ2 = 10.5 P = 0.005* |
||||
| Occurrence of myocarditis | ||||||||
| No/yes | 85/15 | 91.4/8.6 | 90.7/9.3 |
χ2 = 1.2 P = 0.54 |
||||
| Occurrence of MI | ||||||||
| No/yes | 100/0 | 98.6/1.4 | 93/7 |
χ2 = 4.7 P = 0.09 |
||||
| Occurrence of HF | χ2 = 1.1 | |||||||
| No/yes | 100/0 | 97.1/2.9 | 97.7/2.3 | P = 0.57 | ||||
| Occurrence of PE | ||||||||
| No/yes | 95/5 | 98.6/1.4 | 95.3/4.7 |
χ2 = 1.4 P = 0.49 |
||||
| Occurrence of hypertension | ||||||||
| No/yes | 100/0 | 98.6/1.4 |
χ2 = 1.2 P = 0.55 |
|||||
| Occurrence of tachycardia | ||||||||
| No/yes | 95/5 | 97.1/2.9 | 100/0 |
χ2 = 2.1 P = 0.36 |
||||
%: percentages of cases within the group, χ2: Chi-square value, S: significant difference < 0.05.
However, there was no significant difference between the three groups in the occurrence of myocarditis, myocardial infarction (MI), heart failure, pulmonary embolism (PE), hypertension, and tachycardia, as demonstrated in Table 5.
Risk factors associated with COVID-19 severity by binary logistic regression analysis
The binary logistic regression analysis revealed that the severity of COVID-19 at enrollment and less clinical improvement were associated with the need for high oxygen and NIMV (OR = 6.45, 2.96–14.02, P = 1.09E−6), ICU admission (OR = 4.7, 2–11.1, P = 2.2E−4) and occurrence of secondary infection (OR = 3.36, 1.56–7.23, P = 0.002), as shown in Table 6. In addition, therapeutic interventions (tocilizumab and tocilizumab/infliximab) in group 2 and group 3 significantly reduced COVID-19 severity compared to group 1 (OR = 0.78 and 0.67, 0.64–0.91 and 0.59–0.98, P = 0.033 and 0.04, respectively) (Table 6). However, after correction for covariates with P value < 0.2 in multiple logistic regression, only need for high oxygen/NIMV (Adjusted OR = 4.98, 2.23–10.53, P = 0.0006), ICU admission (Adjusted OR = 3.37, 1.92–8.74, P = 0.001), the occurrence of secondary bacterial infection (Adjusted OR = 2.99, 1.38–6.13, P = 0.009) and therapeutic intervention, for both group 2 and group 3 (Adjusted OR = 0.82 and 0.73, 0.69–0.98 and 0.64–0.88, P = 0.041 and 0.047, respectively) remain significant as shown in Table 7.
Table 6.
Risk factors associated with COVID-19 Severity by binary logistic regression analysis.
| Risk factor | Odd ratio | 95% CI | P value |
|---|---|---|---|
| Tocilizumab treatment (Group 2/Group 1) | 0.78 | 0.64–0.91 | 0.033* |
| Tocilizumab/infliximab treatment (Group 3/Group 1) | 0.67 | 0.59–0.98 | 0.04* |
| Severity at enrollment | 3.78 | 1.66–8.62 | 0.001* |
| Need for low oxygen | 0.33 | 0.14–0.78 | 0.013* |
| Need for high oxygen/NIMV | 6.45 | 2.96–14.02 | 1.09E−6* |
| Need for invasive MV | 1.71 | 0.42–3.07 | 0.81 |
| ICU admission | 4.7 | 2–11.1 | 2.2E−4* |
| HTN | 0.87 | 0.43–1.76 | 0.72 |
| DM | 0.77 | 0.37–1.58 | 0.59 |
| HF | 0.719 | 0.65–0.79 | 0.94 |
| CKD | 1.3 | 0.31–5.45 | 0.71 |
| Chronic liver disease | 0.71 | 0.64–0.79 | 0.58 |
| Ischemic heart disease | 0.43 | 0.14–1.35 | 0.22 |
| Atrial fibrillation | 0.70 | 0.64–0.78 | 0.19 |
| COPD | 0.85 | 0.09–8.4 | 0.98 |
| Asthma | 0.30 | 0.04–2.5 | 0.45 |
| Clinical improvement | 0.79 | 0.33–1.9 | 0.64 |
| Death | 1.27 | 0.52–3.1 | 0.64 |
| Occurrence of secondary infection | 3.36 | 1.56–7.23 | 0.002* |
| Occurrence of myocarditis | 0.84 | 0.26–2.76 | 0.82 |
| Occurrence of MI | 8.18 | 0.83–80.89 | 0.06 |
| Occurrence of HF | 1.29 | 0.11–14.56 | 0.99 |
| Occurrence of PE | 1.74 | 0.28–10.79 | 0.62 |
| Occurrence of tachycardia | 0.71 | 0.65–0.79 | 0.58 |
| Occurrence of HTN | 0.71 | 0.65–0.79 | 0.62 |
Group 1 was coded as 1; group 2 coded as 2 and group 3 coded as 3.
*Significant, level of significance < 0.05.
Table 7.
Multiple logistic regression analysis showing risk factors associated significantly with COVID-19 Severity.
| Risk factor | Adjusted odd ratio | Adjusted 95% CI | P value |
|---|---|---|---|
| Tocilizumab treatment (Group 2/Group 1) | 0.82 | 0.69–0.98 | 0.041* |
| Tocilizumab/infliximab treatment (Group 3/Group 1) | 0.73 | 0.64–0.88 | 0.047* |
| Severity at enrollment | 2.64 | 1.45–5.82 | 0.003* |
| Need for high oxygen/NIMV | 4.98 | 2.23–10.53 | 0.0006* |
| ICU admission | 3.73 | 1.92–8.74 | 0.001* |
| Occurrence of secondary infection | 2.99 | 1.38–6.13 | 0.009* |
*Significant difference < 0.05.
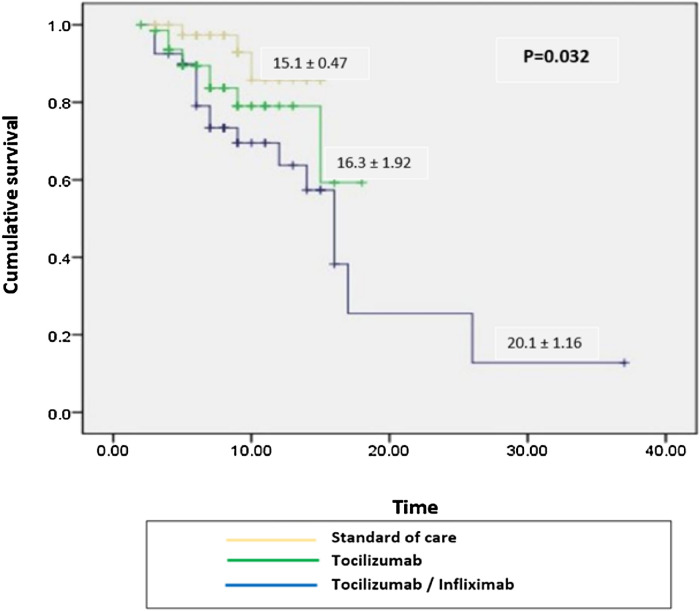
Survival analysis
We followed patients from admission till discharge, and overall cumulative death were reported. We found that patients who received Infliximab/tocilizumab treatment showed better survival than those who received tocilizumab and standard of care alone (P = 0.032), as shown in Fig. 1.
Figure 1.
Kaplan Meier survival curve of COVID-19 patients who received Infliximab/Tocilizumab versus Tocilizumab and standard of care (P = 0.032).
Discussion
Covid-19 pneumonia therapeutic approaches are needed for the different races and ethnicities who were excessively affected by the pandemic12,13.
Covid-19 might be associated with a hyper-inflammatory state, which may play a role in the development of acute respiratory distress syndrome14,15. High levels of the inflammatory cytokine interleukin-6 (IL-6) were associated with severe manifestations of the Covid-19 virus, while low IL-6 levels were associated with mild disease16,17. Additionally, the elevation of interleukin-6 levels has been shown as a predictor of the need for ventilator support18.
This is the first study we are aware of to directly compare the effects of treatment with tocilizumab/infliximab versus treatment with tocilizumab in moderate-severe COVID patients.
This study showed that the need for oxygen, mechanical ventilator, ICU admission, death and occurrence of sepsis were lower significantly in the tocilizumab/infliximab group and tocilizumab group compared to the standard of care group. However, there was no significant difference between the three groups in the occurrence of myocarditis, myocardial infarction (MI), heart failure, pulmonary embolism (PE), hypertension and tachycardia. To add, the tocilizumab/infliximab group had significantly lower CRP, LDH, ALC, and NLR levels before and after therapy compared to the tocilizumab group.TNF is a pro-inflammatory cytokine that contributes to the hyperinflammatory response. TNF is increased in COVID-19 patients, and high baseline levels may be a predictor of mortality. Inhibiting tumour necrosis factor (TNF) is an example of an immunomodulatory strategy that shows significant potential as a treatment for COVID-1919,20. Additionally, TNF inhibitors are capable of reducing inflammation, especially pro-inflammatory cytokines associated with poor COVID patient outcomes21. Neuharth’s study questioned whether or not TNF inhibitors provide protection against severe COVID-199.
Additionally, the TNF inhibitor, tocilizumab has been approved as one of the treatment options available for multiple inflammatory diseases22–24 and in several previous studies, had shown to improve COVID-19 patients with respiratory symptoms in different populations globally25. Nevertheless, tocilizumab clinical studies showed conflicting results among patients with COVID-19 who have varying levels of disease severity and variable standards of care approaches26,27.
Similar to this study findings was the Evaluating Minority Patients with Actemra study (EMPACTA), which investigated the use of tocilizumab in Covid-19 pneumonia patients who were not on mechanical ventilation. In this study, Tocilizumab lowered the incidence of the composite outcome of mechanical ventilation or mortality in hospitalized patients with Covid-19 pneumonia who were not receiving mechanical ventilators, but it did not enhance survival28.
Supportive of the presented study results, Stallmach et al.29 retrospectively explored the effect of infliximab on patients in severe conditions who have tested positive for COVID-19 compared to patients with COVID-19 who were receiving supportive therapy only. Among patients treated with infliximab, the inflammatory markers; IL-6, CRP, and LDH have shown a rapid reduction in their levels in addition to a marked increase in the lymphocytic count from baseline to post-treatment as well as an obvious clinical improvement29.
Contrariwise, the Surveillance Epidemiology of Coronavirus Under Research Exclusion for Inflammatory Bowel Disease (SECURE-IBD) study which compared anti-TNF administration to placebo, showed no significant association between TNF inhibitor use and the following clinical outcomes; ICU admission, ventilator use, and/or death30. However, infliximab use was strongly associated with a reduction in hospitalization and mortality rate consistent with the other studies31,32. Additionally, a case series study showed that patients who received infliximab treatment did not require a mechanical ventilator and showed no mortality compared to patients on other COVID-19 medications33.
In alignment with the current study, concomitant serious infection especially sepsis was significantly lower in patients on long-term treatment with infliximab (Li, 2020). However, in studies evaluating infliximab use as a treatment for the septic shock of bacterial origin, patients showed no significant difference in mortality rate though infective and inflammatory markers did not deteriorate34,35.
Similar to the current study, Hachem et al. showed a rapid resolution of lymphopenia for patients with baseline lymphopenia. These patients, upon discharge had a significant increase in lymphocytic and monocyte counts from baseline and a significant reduction of the inflammatory mediators involved in the pathogenesis of severe COVID-19 infection36. Additionally, patients on infliximab therapy showed improvement in respiratory parameters in terms of SpO2/FiO2 and reduced need for ventilator support36.
Indicators of the severity of illness, such as the necessity for intensive care, multi-organ failure, and mortality, have been linked to elevated serum concentrations of tumour necrosis factor alpha (TNF) and its established regulatory targets, such as interleukin-6 (IL-6) and ferritin6,37.
In the current study, there was a decrease in ferritin and CRP in the tocilizumab/infliximab group. In the context of these results, Liu et al. concluded that patients with elevated IL-6 levels at baseline (> 10 pg/ml) were positively correlated with increased baseline levels of CRP, LDH, ferritin, and D‐dimer38. Additionally, this study showed that patients who received Infliximab/Tocilizumab had significantly better survival compared to the standard of care, and the parameter neutrophil lymphocytic ratio (NLR) was suitable to distinguish between those patients who could eventually be discharged and those who died with AUC of 76.5%38.
Similar to this study findings was Salama et al.’s28 study, in which there was reduced mortality among severe COVID-19 hospitalized patients who received tocilizumab added to standard treatment versus those treated with placebo. In contrast to our study results, two previous studies suggested that IL-6 receptor inhibition has an extensive therapeutic effect on patients with Covid-19. On the contrary, the results of a limited number of unpublished randomized controlled trials are not suggestive of its use39,40. The mean time to hospital discharge was 2.11 days shorter in the Infliximab/Tocilizumab group than in the Tocilizumab and standard of care group. Similar to our study findings was Salama et al.28 study, which showed that tocilizumab plus standard care showed a significantly shorter hospital stay by 1.5 days than placebo plus standard care.
Conclusion
Our study showed that infliximab/tocilizumab added to standard treatment was more effective than tocilizumab added to standard treatment in reducing death and biochemical inflammatory markers and in improving clinical outcomes among severely hospitalized patients with Covid-19.
Methods
Patients and setting
From December 2020 through June 2021, a cohort of COVID-19 hospitalized patients in the inflammatory phase were recruited for a prospective observational study at Teacher's Hospital, Cairo, Egypt, ClinicalTrials.gov (NCT04734678). Written informed consent was obtained from all patients recruited in the study.
Study design
The present investigation is a prospective cohort study in which patients are divided into three groups. Group 1 includes hospitalized COVID-19 patients who received standard treatment. Group 2 includes hospitalized COVID-19 patients who received treatment with tocilizumab PLUS standard management. Group 3 includes hospitalized COVID-19 patients who received treatment with infliximab/tocilizumab PLUS standard management.
Eligibility criteria
Patients over 18 who were hospitalized with pneumonia confirmed by chest CT scan and tested positive for COVID-19 infection using RT-PCR were included in the study. We included patients who had CSS which was detected by inflammatory markers elevation; either C-reactive protein (CRP) ≥ 100 mg/L or ferritin ≥ 900 ng/mL, along with lactate dehydrogenase (LDH) > 220 U/L and interleukin-6 level (IL-6) > 10 pg/ml. In addition to one of the following: respiratory rate ≥ 30 respirations/min, oxygen saturation ≤ 93%, ratio of pressure arterial oxygen partial pressure to inspired oxygen fraction (PaO2/FiO2) < 300 or who showed worsening of pulmonary areas of consolidation, defined as increase in number and size of patches41,42.
Patients with evidence of concurrent bacterial infection, use of other immunosuppressant, and levels of alanine aminotransferase (ALT) or aspartate aminotransferase (AST) that are five times higher than the upper range of normal were excluded. Additionally, patients who received treatment with anti-TNFα in the previous month and show hypersensitivity to any TNFα inhibitor as well as active or latent tuberculosis were excluded. Patients who received any COVID-19 vaccine or those who were previously infected with SARS-COV were also excluded from the study.
Treatment
All patients received the standard treatment of 400 mg of hydroxychloroquine once daily, or 400/100 mg of lopinavir/ritonavir twice daily, or remdesivir 200 mg as a loading dose followed by 100 mg once daily as a maintenance dosage, in addition to dexamethasone 6 mg once daily for 7–10 days. Anticoagulant enoxaparin is administered subcutaneously once daily as a preventative measure if the D-dimer is between 500 and 1000, and twice daily as a therapeutic measure if the D-dimer is greater than 1000. Patients also received supportive treatments of quetiapine (25 mg once a day at bedtime) and paracetamol (1 g every 6 h). Intravenously (IV) tocilizumab was administrated at a dose of 4–8 mg/kg/day divided into two doses, 12–24 h apart when steroid therapy has failed to improve the condition for 24 h. After 24 h, a second dose was administered if the patient experienced any sign of respiratory worsening, including the requirement of ventilator support invasive or non-invasive. Infliximab was given as an IV infusion at a dose of 400 mg only once. The cardiologist was the one responsible for detecting any cardiovascular complications.
Study outcomes
Primary outcomes
The length of patients' hospital stays, and admission to the intensive care unit (ICU) were first evaluated as primary outcomes.
Secondary outcomes
Secondary outcomes include death, the use of NIV or invasive mechanical ventilation, the development of secondary infections (such as bacterial or fungal infections), and an elevation in liver enzymes above three times the normal threshold.
Sample size calculation
By using a two-sided hypothesis and an alpha of 0.05, we found that a sample size of 134 patients gave us over 80% power to detect an effect size of f2 of 0.16. With the knowledge that some of our recruits would inevitably drop out, we made sure to get in an extra 10%.
Statistical analysis
The data were analyzed using SPSS, a statistical package for the social sciences, version 22.0 (SPSS, Chicago, IL-USA). The mean and standard deviation are presented for continuous data. Numerical and percentage-based displays of categorical information are used. The normality of the data was investigated with the help of the Kolmogorov–Smirnov test and the Shapiro–Wilk test. When comparing two groups based on numerical variables that followed a normal distribution, we used the student’s t test. The analysis of variance (ANOVA) was used to compare the groups and to track the evolution of the data over time, while the Chi-square test was used to evaluate the continuous variables. The Mann–Whitney U test was utilized to make group comparisons for non-normally distributed variables. Over time, we compared two numerical variables using the Wilcoxon signed-rank test. When comparing the two groups in terms of categorical information, Fisher's exact tests were used. Biochemical and clinical predictors of each outcome of interest were evaluated using regression analysis. In addition to the variables that were already considered in the univariate analysis because of their association with the outcome (clinical covariates), we also considered additional variables with P values of less than 0.2. All clinical predictors in the final model had to have a P value of 0.05 or lower to be considered significant. Survival curves were calculated using Kaplan–Meier and compared with a log-rank test. All P values are two-tailed, and a value of 0.05 was taken to indicate statistical significance.
Ethical approval
The study protocol was reviewed and approved by the institutional review boards (IRBs) of faculty of Pharmacy, October 6 University (PRC-Ph-2206019). Written informed consent was obtained from all patients recruited in the study. This study was performed according to the Declaration of Helsinki.
Author contributions
A.E., H.S. performed the research; N.M.S., M.F.S. wrote the research; A.E., N.M.S., M.F.S. designed the research; N.M.S., S.H. analyzed the data. All authors read and approved the final manuscript.
Funding
Open access funding provided by The Science, Technology & Innovation Funding Authority (STDF) in cooperation with The Egyptian Knowledge Bank (EKB).
Data availability
The datasets generated during and/or analyzed during the current study and the study protocol are available from the corresponding author upon reasonable request.
Competing interests
The authors declare no competing interest.
Footnotes
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Wiersinga WJ, Rhodes A, Cheng AC, Peacock SJ, Prescott HC. Pathophysiology, transmission, diagnosis, and treatment of coronavirus disease 2019 (COVID-19): A review. JAMA. 2020;324(8):782–793. doi: 10.1001/jama.2020.12839. [DOI] [PubMed] [Google Scholar]
- 2.Johns Hopkins. COVID-19 Dashboard by the Center for Science and Engineering. 2021. https://coronavirus.jhu.edu/map.html. Accessed 14 December 2021.
- 3.Kaur S, Bansal Y, Kumar R, Bansal G. A panoramic review of IL-6: Structure, pathophysiological roles and inhibitors. Bioorgan. Med. Chem. 2020 doi: 10.1016/j.bmc.2020.115327. [DOI] [PubMed] [Google Scholar]
- 4.Le RQ, Li L, Yuan W, et al. FDA approval summary: Tocilizumab for treatment of chimeric antigen receptor T cell-induced severe or life- threatening cytokine release syndrome. Oncologist. 2018;23(8):943–947. doi: 10.1634/theoncologist.2018-0028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lee DW, Gardner R, Porter DL, et al. Current concepts in the diagnosis and management of cytokine release syndrome. Blood. 2014;124(2):188–195. doi: 10.1182/blood-2014-05-552729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Huang C, Wang Y, Li X, Ren L, Zhao J, Hu Y, Zhang L, Fan G, Xu J, Gu X, Cheng Z, Yu T, Xia J, Wei Y, Wu W, Xie X, Yin W, Li H, Liu M, Xiao Y, Gao H, Guo L, Xie J, Wang G, Jiang R, Gao Z, Jin Q, Wang J, Cao B. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395(10223):497–506. doi: 10.1016/S0140-6736(20)30183-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ruan Q, Yang K, Wang W, Jiang L, Song J. Clinical predictors of mortality due to COVID-19 based on an analysis of data of 150 patients from Wuhan, China. Intensive Care Med. 2020 doi: 10.1007/s00134-020-05991-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Liu B, Li M, Zhou Z, Guan X, Xiang Y. Can we use interleukin-6 (IL-6) blockade for coronavirus disease 2019 (COVID-19)-induced cytokine release syndrome (CRS)? J. Autoimmun. 2020 doi: 10.1016/j.jaut.2020.102452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Neurath MF. Covid-19 and immunomodulation in IBD. Gut. 2020;69(7):1335–1342. doi: 10.1136/gutjnl-2020-321269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Riva G, Nasillo V, Tagliafico E, Trenti T, Luppi M. COVID-19: Room for treating T cell exhaustion? Crit. Care. 2020;24(1000-Genomes):1–2. doi: 10.1186/s13054-020-02960-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Brenner EJ, Ungaro RC, Gearry RB, Kaplan GG, Kissous-Hunt M, Lewis JD, Ng SC, Rahier J-F, Reinisch W, Ruemmele FM, et al. Corticosteroids, but not TNF antagonists, are associated with adverse COVID-19 outcomes in patients with inflammatory bowel diseases: Results from an international registry. Gastroenterology. 2020;159:481–491.e3. doi: 10.1053/j.gastro.2020.05.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Williamson EJ, Walker AJ, Bhaskaran K, et al. Factors associated with COVID-19-related death using OpenSAFELY. Nature. 2020;584:430–436. doi: 10.1038/s41586-020-2521-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Egede LE, Walker RJ. Structural racism, social risk factors, and Covid-19—A dangerous convergence for Black Americans. N. Engl. J. Med. 2020;383(12):e77. doi: 10.1056/NEJMp2023616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Giamarellos-Bourboulis EJ, Netea MG, Rovina N, et al. Complex immune dysregulation in COVID-19 patients with severe respiratory failure. Cell Host Microbe. 2020;27(6):992–1000.e3. doi: 10.1016/j.chom.2020.04.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Mehta P, McAuley DF, Brown M, et al. COVID-19: Consider cytokine storm syndromes and immunosuppression. Lancet. 2020;395:1033–1034. doi: 10.1016/S0140-6736(20)30628-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Aziz M, Fatima R, Assaly R. Elevated interleukin-6 and severe COVID-19: A meta- analysis. J. Med. Virol. 2020;92:2283–2285. doi: 10.1002/jmv.25948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Zhu J, Pang J, Ji P, et al. Elevated interleukin- 6 is associated with severity of COVID-19: A meta-analysis. J. Med. Virol. 2020;93(1):35. doi: 10.1002/jmv.26085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Herold T, Jurinovic V, Arnreich C, et al. Elevated levels of IL-6 and CRP predict the need for mechanical ventilation in COVID-19. J. Allergy Clin. Immunol. 2020;146(10):128–136.e4. doi: 10.1016/j.jaci.2020.05.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Feldmann M, Maini RN, Woody JN, Holgate ST, Winter G, Rowland M, Richards D, Hussell T. Trials ofanti-tumour necrosis factor therapy for COVID19 are urgently needed. Lancet. 2020;395:1407–1409. doi: 10.1016/S0140-6736(20)30858-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Robinson PC, Richards D, Tanner HL, Feldmann M. Accumulating evidence suggests anti-TNF therapy needs to be given trial priority in COVID-19 treatment. LancetRheumatol. 2020;2:E653–E655. doi: 10.1016/S2665-9913(20)30309-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Del Valle DM, Kim-Schulze S, Huang H-H, Beckmann ND, Nirenberg S, Wang B, Lavin Y, Swartz TH, Madduri D, Stock A, et al. An inflammatory cytokine signature predicts COVID-19 severity and survival. Nat. Med. 2020;26:1636–1643. doi: 10.1038/s41591-020-1051-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Actemra prescribing information. South San Francisco, CA: Genentech, 2019 (package insert).
- 23.RoActemra summary of product characteristics. Grenzach-Wyhlen, Germany: Roche, 2020.
- 24.Roche. Roche provides an update on the phase III COVACTA trial of Actemra/RoActemra in hospitalised patients with severe COVID-19 associated pneumonia. July 29, 2020. https://www.roche.com/investors/updates/inv-update-2020-07-29.htm.
- 25.Morrison AR, Johnson JM, Griebe KM, et al. Clinical characteristics and predictors of survival in adults with coronavirus disease 2019 receiving tocilizumab. J. Autoimmun. 2020;114:102512. doi: 10.1016/j.jaut.2020.102512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Hermine O, Mariette X, Tharaux P-L, et al. Effect of tocilizumab vs usual care in adults hospitalized with COVID-19 and moderate or severe pneumonia: A randomized clinical trial. JAMA Intern. Med. 2020;181(1):32–40. doi: 10.1001/jamainternmed.2020.6820. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Stone JH, Frigault MJ, Serling-Boyd NJ, et al. Efficacy of tocilizumab in patients hospitalized with Covid-19. N. Engl. J. Med. 2020 doi: 10.1056/NEJMoa2028836. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Salama C, Han J, Yau L, Reiss WG, Kramer B, Neidhart JD, Mohan SV. Tocilizumab in patients hospitalized with Covid-19 pneumonia. N. Engl. J. Med. 2021;384(1000-Genomes):20–30. doi: 10.1056/NEJMoa2030340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Stallmach A, Kortgen A, Gonnert F, Coldewey SM, Reuken P, Bauer M. Infliximab against severe COVID-19-induced cytokine storm syndrome with organ failure-a cautionary case series. Crit. Care. 2020;24:444. doi: 10.1186/s13054-020-03158-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Brenner EJ, Ungaro RC, Colombel JF, Kappelman MD. IBD in the COVID-19 era: The value of international collaboration. Lancet Gastroenterol. Hepatol. 2020;5(1000-Genomes):887–888. doi: 10.1016/S2468-1253(20)30269-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Rodríguez-Lago I, de la Piscina PR, Elorza A, Merino O, de Zárate JO, Cabriada JL. Characteristics and prognosis of patients with inflammatory bowel disease during the SARS-CoV-2 pandemic in the Basque country (Spain) Gastroenterology. 2020;159:781–783. doi: 10.1053/j.gastro.2020.04.043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Waggershauser CH, Tillack-Schreiber C, Berchtold-Benchieb C, Szokodi D, Howaldt S, Ochsenkühn T. Letter: immunotherapy in IBD patients in a SARS-CoV2 endemic area. Aliment. Pharmacol. Ther. 2020;52:898–899. doi: 10.1111/apt.15897. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Winthrop KL, Brunton AE, Beekmann S, Polgreen P, Baddley J, Saag KG, Calabrese C, Calabrese L, Robinson PC, Wallace ZS, Curtis JR, COVID-19 Study Team SARS CoV-2 infection among patients using immunomodulatory therapies. Ann. Rheum. Dis. 2020 doi: 10.1136/annrheumdis2020-218580. [DOI] [PubMed] [Google Scholar]
- 34.Abraham E, Wunderink R, Silverman H, Perl TM, Nasraway S, Levy H, Bone R, Wenzel RP, Balk R, Allred R, et al. Efficacy and safety of monoclonal antibody to human tumor necrosis factor a in patients with sepsis syndrome. A randomized, controlled, doubleblind, multicenter clinical trial.TNF-a MAb Sepsis Study Group. JAMA. 1995;273:934–941. doi: 10.1001/jama.1995.03520360048038. [DOI] [PubMed] [Google Scholar]
- 35.Cohen J, Carlet J, International Sepsis Trial Study Group INTERSEPT: An international, multicenter, placebo-controlled trial of monoclonal antibody to human tumor necrosis factor-alpha in patients with sepsis. Crit. Care Med. 1996;24:1431–1440. doi: 10.1097/00003246-199609000-00002. [DOI] [PubMed] [Google Scholar]
- 36.Hachem H, Godara A, Schroeder C, Fein D, Mann H, Lawlor C, Marshall J, Klein A, Poutsiaka D, Breeze JL, Joshi R, Mathew P. Rapid and sustained decline in CXCL-10 (IP-10) annotates clinical outcomes following TNFα-antagonist therapy in hospitalized patients with severe and critical COVID-19 respiratory failure. J. Clin. Transl. Sci. 2021;5(1000-Genomes):e146. doi: 10.1017/cts.2021.805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Lin Z, Long F, Yang Y, Chen X, Xu L, Yang M. Serum ferritin as an independent risk factor for severity in COVID-19 patients. J. Infect. 2020;81(4):647–679. doi: 10.1016/j.jinf.2020.06.053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Liu T, Zhang J, Yang Y, Ma H, Li Z, Zhang J, Yi J. The role of interleukin-6 in monitoring the severe case of coronavirus disease 2019. EMBO Mol. Med. 2020;12(7):e12421. doi: 10.15252/emmm.202012421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Benucci M, Giannasi G, Cecchini P, Gobbi FL, Damiani A, Grossi V, Manfredi M. COVID-19 pneumonia treated with sarilumab: A clinical series of eight patients. J. Med. Virol. 2020;92:2368. doi: 10.1002/jmv.26062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Furlow B. COVACTA trial raises questions about tocilizumab's benefit in COVID-19. Lancet Rheumatol. 2020;2(10):e592. doi: 10.1016/S2665-9913(20)30313-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Chousterman, B. G., Swirski, F. K., & Weber, G. F. (2017). Cytokine storm and sepsis disease pathogenesis. In Seminars in Immunopathology (Vol. 39, pp. 517–528). [DOI] [PubMed]
- 42.Lee DW, Gardner R, Porter DL, Louis CU, Ahmed N, Jensen M, Mackall CL. Current concepts in the diagnosis and management of cytokine release syndrome. Blood J. Am. Soc. Hematol. 2014;124(2):188–195. doi: 10.1182/blood-2014-05-552729. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets generated during and/or analyzed during the current study and the study protocol are available from the corresponding author upon reasonable request.