Abstract
Objectives
To assess the impact of applicant and program characteristics on preference signaling outcomes during the 2021 and 2022 application cycles in otolaryngology.
Methods
The Texas Seeking Transparency in Applications to Residency survey was used for otolaryngology applicants during the 2021 and 2022 match years. The primary outcome of interest was signal yield, defined as the number of interviews at signaled programs divided by the total number of signals sent. Associations with applicant‐reported characteristics, geographic connections to programs, and program reputation were assessed.
Results
On average 59.5% of signals resulted in an interview (signal yield). There was a positive correlation between the number of signals sent to a program with a reported geographic connection and signal yield, with each additional signal resulting in a 3.4% increase in signal yield (p = .03). Signal yield was positively associated with number of publications (p < .001); number of abstracts, posters, and presentations (p = .04); and whether the applicant took a research year (p = .003). Applicants with higher USMLE Step 1 (p = .01) and Step 2 (p = .003) scores, publications (p = .03), volunteer (p = .008) and leadership (p = .001) experiences received a lower percentage of their total interviews from signaled programs whereas applicants from the 3rd (p < .001) and 4th (p = .03) cumulative class ranked quartiles received a higher percentage of their total interviews from signaled programs.
Conclusions
Signal yield appears to have a significant association with geographic connections to programs and applicant competitiveness. This study may help applicants, advisors, and programs maximize the benefit of the preference signaling system.
Levels of evidence: Level 4.
Keywords: graduate medical education, otolaryngology, preference signaling, residency application
1. INTRODUCTION
The rising number of otolaryngology applicants, which reached a record high in 2022, has led to concerns regarding each applicant receiving a holistic review of their application. 1 , 2 Further, COVID‐19 related changes including virtual interviews and a cap on the number of away rotations has limited applicants' abilities to convey their interest to programs. 3 , 4 To address these mounting challenges, the Otolaryngology Program Director Organization instituted a preference signaling system during the 2021 and 2022 application cycles whereby students were able to formally signal interest in specific programs. 5 , 6 , 7 Applicants were granted five signals during the 2021 cycle and four signals during the 2022 cycle. Initial data from the preference signaling program has revealed significantly higher interview rates among signaled programs across all levels of applicant competitiveness, with relatively higher interview rates at signaled programs for less competitive applicants. 6 , 7 Survey data from both years of signaling has shown that the majority of applicants and programs support the continuation of preference signaling programs. 7
With the continuation of preference signaling into the 2022–2023 cycle, both applicants and programs are seeking information on how best to leverage signaling to their advantage. Although existing analyses provide important information regarding the impact of signaling on interview offer rates across levels of applicant competitiveness, they lack additional information relevant to applicants and programs such as the impact of geographic connections, program reputation, and applicant‐specific characteristics (e.g., USMLE scores, clinical grades, research output, etc.). This information may help applicants and their advisors better understand where to send signals to maximize their chances of receiving interviews.
The primary aim of this study was to investigate the impact of applicant and program characteristics on preference signaling outcomes in the otolaryngology match during the 2021 and 2022 application cycles. We hypothesized that signals sent to a program with a geographic connection would have a greater impact on receiving an interview than signals sent to programs without geographic connections, that signals sent to higher Doximity ranked programs would have a lower signal yield, and that more competitive applicants based upon traditional metrics would be more likely to signal higher ranked programs. By combining data from the first 2 years of preference signaling in the otolaryngology application process, this study can be used to help inform applicants, advisors, and programs on how best to use and adapt preference signaling moving forward.
2. METHODS
2.1. Data and sample
Data were sourced from the Texas Seeking Transparency in Applications to Residency (STAR) survey, which contains self‐reported, de‐identified information from US allopathic and osteopathic medical students for the 2018–2022 match years. 8 The Texas STAR survey is distributed to fourth year medical students by medical school deans for their respective school between match day and April 10th of each application cycle. The survey is sent to allopathic and osteopathic medical schools throughout the United States. The 2021 STAR survey included 7418 respondents from 115 medical schools and the 2022 STAR survey included 6912 respondents from 123 medical schools. Applicants are instructed to report data in the survey as it appeared on their applications.
Survey respondents were included in our study if they applied into otolaryngology during the 2021 and 2022 application cycles. Respondents were excluded if they did not report preference signaling data (Figure S1). Participation in the survey was completely voluntary, use was explained to participants, and participation served as consent for data collection. This study was deemed not regulated by the University of Michigan Institutional Review Board (HUM00217169).
2.2. Variables
The primary outcome of interest was signal yield, calculated as the number of interviews at signaled programs divided by the total number of signals sent. Secondary outcomes included percentage of signals sent to a program with a geographic connection, percentage of signals sent to a program ranking in the Top 10 and Top 20 Doximity reputation rankings based on the 2021 survey, 9 and signal‐to‐interview ratio, calculated as the total number of interviews at signaled programs divided by total interviews. Signal yield and signal‐to‐interview ratio were multiplied by 100 and reported as percentages.
On the STAR survey, applicants were asked to report whether they had a geographic connection, signaled, interviewed, and matched at each program to which they applied. Geographic connection was ascertained from the question “Please select each of the programs in this discipline to which you applied and indicate if you had a personal geographic connection to the area.” This was intentionally broad and may include things such as an applicant's hometown; home institution; an area an away rotation was completed; an area where relatives live; an area where a significant other lives; and an area where they went to school, worked, or did research. Importantly, applicants were advised against sending signals to their home institution and institutions where they completed an away rotation.
Applicant‐level variables included number of signals sent, match status, whether the applicant matched at a signaled program, United States Medical Licensing Exam (USMLE) Step 1 and Step 2 scores (reported in 5‐point intervals), class rank (reported as cumulative quartile), clinical grades, honor‐society membership, research output, and volunteering and leadership experiences. USMLE scores were centered for analysis (i.e., 220–224 was centered at 222).
2.3. Statistical analysis
Wilcoxon‐Rank Sum testing was used to compare signal yield by any geographic connection and total number of geographic connections. Correlation between percentage of signals sent to a geographic connection and percentage of signals sent to Top 10 and Top 20 Doximity ranked programs were analyzed with Spearman's rank correlation testing. Applicant‐level predictors of signal yield, signal‐to‐interview ratio, percentage of signals sent to a geographic connection, and percentage of signals sent to Doximity Top 10 and Top 20 ranked programs were completed using ordinary least squares (OLS) regression. All statistical analyses were carried out at a significance criterion of p < .05 and two‐sided testing was used. SAS v9.4 (Cary, NC) and R v4.2 (R Development Core) were used for analyses and figure generation.
3. RESULTS
3.1. General characteristics
There were 217 otolaryngology applicants who met inclusion and exclusion criteria for our study. Mean signals sent were 3.97 (SD 1.1). Two‐hundred and five (94.5%) applicants interviewed with at least one signaled program. On average, 59.5% (SD 29.8%) of signals resulted in an interview (signal yield) and interviews at signaled institutions constituted 21.2% (SD 13.5%) of total interviews (signal‐to‐interview ratio). Each applicant averaged 2.8 (SD 1.2) interviews at signaled programs in 2021 and 1.9 (SD 1.2) interviews at signaled programs in 2022. Of 217 applicants, 168 (77.4%) matched into otolaryngology. Of matched applicants, 49 (29.2%) matched at a signaled program and 119 (70.8%) matched at a non‐signaled program (Table 1).
TABLE 1.
Descriptive statistics of applicant‐reported signaling variables.
| Otolaryngology applicants | |
|---|---|
| Variable | N = 217 |
| Signals sent 2021—Mean (SD) | 4.5 (1.0) |
| Signals sent 2022—Mean (SD) | 3.5 (1.0) |
| Interviews at signaled programs in 2021—Mean (SD) | 2.8 (1.2) |
| Interviews at signaled programs in 2022—Mean (SD) | 1.9 (1.2) |
| Signal yield (interviews at signaled programs/signals sent)—Mean (SD) | 59.5% (29.8%) |
| Signal to interview ratio (interviews at signaled programs/total interviews)—Mean (SD) | 21.2% (13.5%) |
| Matched | 168 (77.4) |
| Matched at signaled program—No. (%) | 49 (22.6) |
| Matched a non‐signaled program—No. (%) | 119 (54.8) |
| Matched at an away rotation—No. (%) | 33 (15.2) |
| Interviewed at signaled program—No. (%) | 205 (94.5) |
| Any signal sent to an institution with a geographic connection—No. (%) | 118 (53.4) |
| Any signal sent to an institution where a virtual away was completed—No. (%) | 26 (11.9) |
| Any signal sent to an institution ranked in the Doximity Top 10—No. (%) | 93 (42.9) |
| Any signal sent to an institution ranked in the Doximity Top 20—No. (%) | 137 (63.1) |
| Signals sent to geographic connection—Mean (SD) | 1.1 (1.3) |
| Signals sent to institution where a virtual away was completed—Mean (SD) | 0.2 (0.4) |
| Signals sent to institution where a virtual seminar was completed—Mean (SD) | 0.1 (0.2) |
| Signals sent to an institution ranked in the Doximity Top 10—Mean (SD) | 0.6 (0.9) |
| Signals sent to an institution ranked in the Doximity Top 20—Mean (SD) | 1.16 (1.22) |
| Percent of signals sent to institution with geographic connection—Mean (SD) | 27.1% (31.5%) |
| Percent of signals sent to institution where virtual away was completed—Mean (SD) | 3.7% (11.7%) |
| Percent of signals sent to institution where virtual seminar was completed—Mean (SD) | 5.6% (16.1%) |
| Percent of signals sent to institution ranked in the Doximity Top 10—Mean (SD) | 15.9% (22.8%) |
| Percent of signals sent to institution ranked in Doximity Top 20—Mean (SD) | 29.1% (30.3%) |
3.2. Impact of geographic connections on signaling and interview outcomes
One hundred and eighteen (54.8%) applicants sent at least one signal to a program with a geographic connection. On average 27.1% (SD 31.5%) of signals were sent to programs with a geographic connection and each applicant averaged 1.1 (SD 1.3) signals to institutions with geographic connections (Table 1). There was a significant correlation between percentage of signals sent to a program with a geographic connection and signal yield (ρ = 0.15, p = .03) (Figure 1A). Further, each additional signal was associated with a 3.4% increase in signal yield (β = 3.4, p = .03) (Figure 2).
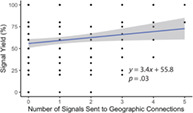
FIGURE 1.
Scatter plots with Spearman Regression coefficients of signal yield with percentage of signals sent to a program with a geographic connection (A), percentage of signals sent to a Doximity Top 10 ranked program (B), and percentage of signals sent to a Doximity Top 20 ranked program (C).
FIGURE 2.
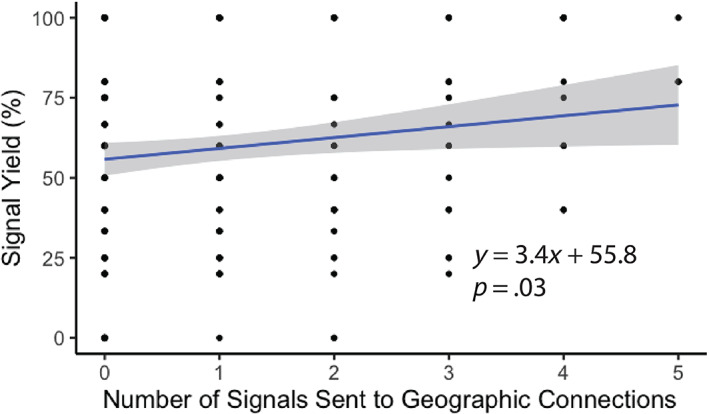
Ordinary least squares regression model of number of signals sent to geographic connections predicting signal yield.
3.3. Analysis of percentage of signals sent to geographic connections and percentage of signals sent to Doximity Top 10 and Top 20 Programs
There was no significant association between percentage of signals sent to Doximity Top 10 (ρ = 0.01; p = .88) or Doximity Top 20 ranked programs and signal yield (ρ = 0.05; p = .40) (Figure 1B,C). Univariable OLS models assessing the impact of applicant‐level predictors on percentage of signals sent to institutions with a geographic connection were notable for applicants belonging to Gold Humanism Honor Society (GHHS) was correlated with a negative percentage of signals sent to geographic connections (β: −11.6, p = .04) (Table 2). Factors traditionally considered to make an applicant more competitive were associated with a higher percentage of signals sent to Doximity Top 10 and Top 20 programs. For Doximity Top 10 programs this included being in GHHS (β: 9.7, p = .02); USMLE Step 1 (β: 0.4, p = .001); USMLE Step 2 (β: 0.04, p = .008); number of abstracts, posters and presentations (β: 1.3, p = .006); number of publications (β: 1.6, p < .001); and whether the student completed a research year (β: 14.6, p < .001). Similar associations were found for Doximity Top 20 ranked programs (Table 2).
TABLE 2.
Univariable ordinary least squares regression models of applicant‐level factors predicting percent of signals sent to a geographic connection and percent of signals sent to Doximity Top 10 and Top 20 programs.
| Percent of signals sent to Geographic connection | Percent of signals sent to Doximity top 10 | Percent of signals sent to Doximity top 20 | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Beta | 95% CI | p value | Beta | 95% CI | p value | Beta | 95% CI | p value | |
| AOA | |||||||||
| No | – | – | – | – | – | – | – | – | – |
| Yes | 8.8 | (−0.2 to 17.8) | .06 | 3.7 | (−2.8 to 10.2) | .26 | 8.5 | (−0.1 to 17.1) | .06 |
| No chapter | 7.7 | (−5.5 to 20.8) | .25 | 10.5 | (1.0–20.0) | .03 | 12.6 | (−0.1 to 25.3) | .06 |
| GHHS | |||||||||
| No | – | – | – | – | – | – | – | – | – |
| Yes | −11.6 | (−23.2 to −0.1) | .04 | 9.7 | (1.4–17.8) | .02 | 2.1 | (−9.1 to 13.2) | .71 |
| No chapter | −0.8 | (−14.9 to 13.1) | .90 | 12.6 | (2.6–22.6) | .01 | 10.9 | (−2.6 to 24.5) | .11 |
| Honors in specialty | |||||||||
| No | – | – | – | – | – | –– | – | – | – |
| Yes | −14.7 | (−41.8 to 12.4) | .29 | 5.9 | (−15.2 to 27.0) | .58 | 2.9 | (−25.0 to 30.7) | .84 |
| Number of clerkship honors | −0.6 | (−2.2 to 1.0) | .48 | 0.4 | (−0.7 to 1.7) | .45 | 0.7 | (−0.8 to 2.4) | .37 |
| Cumulative quartile | |||||||||
| 1st | – | – | – | – | – | – | – | – | – |
| 2nd | −3.5 | (−16.8 to 9.8) | .60 | −5.9 | (−14.4 to 2.7) | .17 | −9.1 | (−20.8 to 2.5) | .12 |
| 3rd | −3.4 | (−20.8 to 14.1) | .70 | −3.9 | (−15.2 to 7.2) | .48 | −7.7 | (−23.0 to 7.5) | .31 |
| 4th | 13.5 | (−24.5 to 51.6) | .48 | −16.5 | (−41.0 to 7.8) | .18 | −29.9 | (−63.2 to 3.4) | .17 |
| Step 1 | 0.1 | (−0.2 to 0.4) | .58 | 0.4 | (0.1–0.6) | .001 | 0.5 | (0.2–0.9) | .001 |
| Step 2 | 0.4 | (−0.01 to 0.9) | .06 | 0.4 | (0.1–0.7) | .008 | 0.6 | (0.2–1.1) | .002 |
| Abstracts, posters, and presentations | −0.9 | (−2.3 to 3.7) | .16 | 1.3 | (0.3–2.3) | .006 | 2.0 | (0.7–3.2) | .002 |
| Publications | 0.5 | (−0.8 to 1.8) | .44 | 1.6 | (0.7–2.6) | <.001 | 2.7 | (1.5–3.9) | <.001 |
| Research experiences | 0.2 | (−1.4 to 1.9) | .81 | 0.3 | (−0.9 to 1.5) | .63 | 1.3 | (−0.2 to 2.9) | .09 |
| Volunteer experiences | 0.0 | (−1.6 to 1.6) | .99 | −0.1 | (−1.3 to 1.0) | .81 | −0.1 | (−1.7 to 1.4) | .86 |
| Leadership positions | −0.2 | (−1.7 to 1.3) | .79 | 0.8 | (−0.3 to 1.9) | .15 | 0.8 | (−0.6 to 2.4) | .25 |
| Couples match | 0.01 | (−0.15 to 0.17) | .89 | ||||||
| No | – | – | – | – | – | – | – | – | – |
| Yes | 1.1 | (−15.1 to 17.3) | .89 | 1.3 | (−10.4 to 13.0) | .83 | 6.3 | (−9.2 to 21.9) | .42 |
| Research year | |||||||||
| No | – | – | – | – | – | – | – | – | – |
| Yes | −0.01 | (−0.11 to 0.10) | .95 | 14.6 | (7.1–22.0) | <.001 | 23.4 | (13.6–33.2) | <.001 |
Abbreviations: AOA: Alpha Omega Alpha Honor Society; GHHS: Gold Humanism Honor Society.
3.4. Impact of applicant‐level factors on interview and signaling outcomes
OLS regression of applicant‐level actors predicting number of interview offers received was notable for factors traditionally associated with applicant‐competitiveness being positively associated with more interviews received. These included AOA membership (β: 5.8, p < .001), number of clerkship honors (β: 0.8, p < .001), each 10 point increase in USMLE Step 1 (β: 2.2, p < .001) and USMLE Step 2 (β: 3.0, p < .001), number of abstracts, posters, and presentations (β: 0.5, p = .005), publications (β: 0.9, p < .001), leadership positions (β: 0.5, p = .007) and taking a research year (β: 6.9, p < .001). Additionally, applicants from the second (β: −4.3, p = .002), third (β: −7.1, p < .001), and fourth (β: −9.9, p = .01) class quartiles received significantly fewer interview offers that the first quartile (Table S1).
Simple OLS regression of applicant‐level factors predicting signal yield was notable for factors relating to research output being associated with a higher signal yield including number of abstracts, posters, and presentations (β: 1.3, p = .04), number of publications (β: 2.4, p < .001), and taking a research year (β:15.3, p = .003). Additionally, having no GHHS chapter (β: 16.1, p = .02) and couples matching (p: 17.0, p = .03) were significantly associated with a higher signal yield (Table 3).
TABLE 3.
Univariable ordinary least squares regression models of applicant‐level factors predicting signal yield and signal‐to‐interview ratio.
| Signal yield | 95% CI | p‐value | Signal to interview ratio | 95% CI | p‐value | |
|---|---|---|---|---|---|---|
| AOA | ||||||
| No | – | – | – | – | – | – |
| Yes | 3.5 | (−5.1 to 12.0) | .42 | −9.0 | (−12.7 to −5.3) | <.001 |
| No chapter | 9.4 | (−3.1 to 22.0) | .14 | −1.2 | (−6.6 to 4.2) | .65 |
| GHHS | ||||||
| No | – | – | – | – | – | – |
| Yes | −1.5 | (−12.3 to 9.4) | .79 | −3.7 | (−8.7 to 1.2) | .14 |
| No chapter | 16.1 | (2.9–29.4) | .02 | 3.4 | (−2.7 to 9.4) | .27 |
| Honors in specialty applied to | ||||||
| No | – | – | – | – | – | – |
| Yes | −9.4 | (−36.3 to 17.6) | .49 | −5.1 | (−17.1 to 7.0) | .41 |
| Number of clerkship honors | 1.0 | (−0.6 to 2.6) | .19 | −0.6 | (−1.3 to 0.1) | .11 |
| Cumulative quartile | ||||||
| 1st | – | – | – | – | – | – |
| 2nd | −4.9 | (−16.3 to 6.6) | .40 | 3.9 | (−1.3 to 9.1) | .13 |
| 3rd | 0.6 | (−14.4 to 15.6) | .94 | 12.6 | (5.8–19.4) | <.001 |
| 4th | −21.8 | (−54.6 to 10.9) | .19 | 15.9 | (1.2–30.7) | .03 |
| Step 1 | 0.2 | (−0.2 to 0.5) | .35 | −0.2 | (−0.4 to −0.1) | .01 |
| Step 2 | 0.2 | (−0.3 to 0.6) | .49 | −0.3 | (−0.5 to −0.1) | .003 |
| Abstracts, posters, and presentations | 1.3 | (0.1–2.6) | .04 | −0.3 | (−0.8 to 0.3) | .36 |
| Publications | 2.4 | (1.1–3.6) | <.001 | −0.6 | (−1.2 to −0.1) | .03 |
| Research experiences | 0.9 | (−0.7 to 2.5) | .27 | −0.5 | (−1.3 to 0.2) | .14 |
| Volunteer experiences | −1.0 | (−2.5 to 0.5) | .21 | −0.9 | (−1.6 to −0.2) | .008 |
| Leadership positions | −0.3 | (−1.7 to 1.2) | .73 | −1.1 | (−1.7 to −0.4) | .001 |
| Couples match | ||||||
| No | – | – | – | – | – | – |
| Yes | 17.0 | (1.9–32.1) | .03 | −6.1 | (−12.9 to 0.8) | .08 |
| Research year | ||||||
| No | – | – | – | – | – | – |
| Yes | 15.3 | (5.3–25.2) | .003 | −3.9 | (−8.4 to 0.7) | .09 |
Abbreviations: AOA: Alpha Omega Alpha Honor Society; GHHS: Gold Humanism Honor Society.
OLS regression of applicant‐level factors predicting signal‐to‐interview ratio was notable for factors associated with more competitive applicants being negatively associated with signal‐to‐interview ratio. This included Alpha Omega Alpha (AOA) membership (β: −9.0, p < .001), USMLE Step 1 score (β: −0.2, p = .01), USMLE Step 2 score (β: −0.3, p = .003), number of volunteer experiences (β: −0.9, p = .008), and number of leadership positions (β: −1.1, p = .001). Similarly, applicants from the 3rd (β: 12.6, p < .001) and 4th (β: 15.9, p = .03) class ranked quartile were significantly more likely to have a higher signal‐to‐interview ratio than those from the 1st or 2nd quartile (Table 3).
4. DISCUSSION
Using applicant‐reported data from the Texas STAR survey, this study assessed preference signaling outcomes among 217 applicants into otolaryngology during the 2021 and 2022 application cycles. Our findings suggest that sending more signals to programs with a geographic connection is associated with higher chances of receiving an interview. Further, we found that competitive applicants were more likely to signal programs ranked in the Top 10 and Top 20 by Doximity reputation. Lastly, we found that applicants with more research output were more likely to receive interviews from signaled programs, whereas less competitive applicants were more likely to receive a higher percentage of their interviews from signaled programs.
Our finding that geographic connections to signaled programs is associated with a higher number of interviews received is important for future applicants and advisors as they seek to maximize the utility of preference signaling for their application. Initial results from the preference signaling experience in otolaryngology have found that signaling a program increases chances of receiving an interview; however, information related to the impact of geographic connections is notably missing. 6 , 7 Interestingly, our findings also suggest that more competitive applicants may be less likely to submit signals to institutions where they have geographic connections. Further, we identified that factors traditionally related to applicant competitiveness are significantly associated with a higher percentage of signals sent to Doximity Top 10 and Top 20 programs. These findings potentially highlight the importance of sending signals to programs with geographic connections for applicants, as it may improve their chances of receiving an interview. Further, sending signals to geographic connections may be particularly beneficial for less competitive applicants, especially if those signals are sent to programs receiving fewer overall signals. Notably, a separate novel initiative allowing applicants to preference up to three geographic regions on their application was trialed during the 2022 application cycle by internal medicine, internal medicine‐preliminary year, and dermatology. Initial results indicated that most programs utilized geographic preferences in their holistic review. 10 , 11 Although otolaryngology did not participate in this program, it does provide evidence of the value of geographic information during application review. Taken together, these findings may help applicants make more informed decisions regarding their preference signals.
We also assessed factors associated with interview offers, which showed that AOA membership, USMLE scores, research output, clinical grades, and leaderships positions were significantly associated with more interview offers. Further, our analysis of applicant‐level characteristics and signal yield showed that research output and couples matching were significantly associated with an increased yield. Research plays an important role in the otolaryngology application and match process with studies showing that number of publications significantly increases the odds of matching in general and matching at highly ranked programs. 12 , 13 Our finding of increased yield among couples matching applicants indicate that a partner interviewing at the same institution may serve as an additional factor for programs when deciding who to interview. 14
Additionally, we found that students with high USMLE scores, more publications, and more volunteering and leadership positions had a lower percentage of their total interviews come from signaled programs. These findings are consistent with previous studies from otolaryngology, which have noted relatively higher signal yield for more competitive applicants. However, previous studies have only extrapolated applicant competitiveness from interview yield, 6 , 7 whereas our study is the first to report on metrics including clinical grades, cumulative quartile, USMLE scores, and research output. Due to this, our findings provide more individualized data for applicants to consider when deciding where to send signals. Lastly, we identified that students from a lower class quartile had a significantly higher frequency of their interviews come from signaled programs. These findings help illustrate that in the new preference signaling era, less competitive applicants by traditional metrics may potentially derive marginal benefits from signaling—possibly by targeting less competitive programs who receive fewer signals.
The primary limitation of this study is generalizability. Our study included 217 US MD and DO seniors which is only 19.2% of total applicants during those cycles. 1 , 2 Additionally, there is the potential for recall bias since the Texas STAR survey was administered 7 months following ERAS submission. Further, match rates for this sample were 74.8% in 2021 and 79.8% in 2022 which overestimate the true otolaryngology match rates of 68.3% and 69.2%, respectively. This indicates that there may be a selection bias with matched applicants being more likely to respond to the survey than unmatched applicants. However, average USMLE scores and research output are similar to those reported in the NMRP Charting the Outcomes of the Match. 15 (Table S2). We further lacked important sociodemographic data that would have enabled us to better assess the impact of signaling on diversity, equity, and inclusion goals. Lastly, our study includes applicant‐reported factors that program directors may use in decision making; however, we are lacking important information that would occur during a holistic application review including the personal statement and letters of recommendation. This, in addition to an established correlation between number of interviews attended and odds of matching alongside increasing matching rates by number of contiguous ranks, led us to focus our analysis on individual criteria that have been shown to be impactful on match success. 12 , 13 , 15
Despite these limitations, our study addresses a critical gap in the literature at a time of rapid change for the residency application process. Average applications submitted per otolaryngology applicant have increased from 32.3 in 2017 to 72.2 in 2021, which may result in programs receiving hundreds of applications for a handful of positions. 16 Further, this influx of applications coincides with a heightened focus on a holistic review of applications. Preference signaling was introduced in part to mitigate rising applications numbers, while also providing applicants with formalized manner to demonstrate interest to particular programs. Since its introduction into otolaryngology in 2021, preference signaling was expanded into four additional specialties during the 2022 match and will be used in 18 total specialties during the 2023 match cycle. 17 In the setting of this novel and expanding system, we believe our findings, especially those relating to the impact of geographic connections on signaling outcomes, convey important information to applicants and their advisors as they seek to leverage preference signaling to their advantage. Further, our study provides important transparency to applicants, who can better understand how their metrics may interplay with the new signaling system. Lastly, our findings can help inform future research on preference signaling including the impact of various types of geographic connections, the relative importance of signaling following the change to pass/fail USMLE Step 1 reporting, and how signaling outcomes relate to diversity, equity, and inclusion goals.
5. CONCLUSION
Signals sent to programs with applicant‐reported geographic connections appear to be more impactful than ones sent to those without. More competitive applicants were more likely to signal Doximity Top 10 and 20 rated programs. Research output was significantly associated with a higher signal yield. Applicants with higher USMLE scores, research output, volunteer experiences and leadership experiences received a lower percentage of their total interviews from signaled programs, whereas applicants from lower class ranked quartiles received a higher percentage. These findings may help provide transparency to applicants and programs about the preference signaling system.
FUNDING INFORMATION
No funding sources to report.
CONFLICT OF INTEREST STATEMENT
The authors declare no conflicts of interest.
Supporting information
Supplemental Figure S1: Inclusion/exclusion diagram
Supplemental Table S1: Applicant‐level factors predicting interview offer totals and match outcomes
Supplemental Table S2: Comparison between Texas STAR and NRMP Charting the Outcomes
ACKNOWLEDGMENTS
None.
Benjamin WJ, Lenze NR, Yalamanchi P, et al. Impact of applicant and program factors on preference signaling outcomes in otolaryngology. Laryngoscope Investigative Otolaryngology. 2023;8(2):401‐408. doi: 10.1002/lio2.1025
REFERENCES
- 1. Results and Data—2021 Main Residency Match. NMRP; 2021:1‐128. Accessed August 22, 2022. https://www.nrmp.org/match-data-analytics/residency-data-reports/ [Google Scholar]
- 2. Results and Data—2022 Main Residency Match. NMRP; 2022:1‐131. [Google Scholar]
- 3. Izreig S, Torabi SJ, Kasle DA, Rahmati RW, Manes RP. Otolaryngology match 2020‐21: survey of prospective applicants in the setting of COVID‐19. Ann Otol Rhinol Laryngol. 2021;130(5):450‐458. doi: 10.1177/0003489420952470 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Salehi PP, Benito D, Michaelides E. A novel approach to the national resident matching program—the star system. JAMA Otolaryngol Neck Surg. 2018;144(5):397‐398. doi: 10.1001/jamaoto.2018.0068 [DOI] [PubMed] [Google Scholar]
- 5. Chang CWD, Pletcher SD, Thorne MC, Malekzadeh S. Preference signaling for the otolaryngology interview market. Laryngoscope. 2021;131(3):E744‐E745. doi: 10.1002/lary.29151 [DOI] [PubMed] [Google Scholar]
- 6. Pletcher SD, Chang CWD, Thorne MC, Malekzadeh S. The otolaryngology residency program preference signaling experience. Acad Med. 2022;97(5):664‐668. doi: 10.1097/ACM.0000000000004441 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Chang CWD, Thorne MC, Malekzadeh S, Pletcher SD. Two‐year interview and match outcomes of otolaryngology preference signaling. Otolaryngol Head Neck Surg. 2022. doi: 10.1177/01945998221121312 [DOI] [PubMed] [Google Scholar]
- 8. UT Southwestern Medical Center . Texas Seeking Transparency in Application to Residency (STAR) Survey . Texas STAR. Accessed August 22, 2022. https://www.utsouthwestern.edu/education/medical-school/about-the-school/student-affairs/texas-star.html
- 9. Doximity Residency Navigator. Doximity. Published 2022. Accessed August 22, 2022. https://www.doximity.com/residency/programs?specialtyKey=4667266b-9685-49c5-8a72-33940db2c9d6-otolaryngology&sortByKey=reputation&trainingEnvironmentKey=all&intendedFellowshipKey=
- 10. Mavilia M. AAMC Supplemental ERAS® Application: Key Findings From the 2022 Application Cycle . Published Online 2022:10.
- 11. Mavilia M. AAMC Supplemental ERAS® Application: Final Results of the Program Director Reaction Survey for the 2022 Application Cycle . Published Online 2022:24.
- 12. Lenze NR, Mihalic AP, DeMason CE, et al. Predictors of otolaryngology applicant success using the Texas star database. Laryngoscope Investig Otolaryngol. 2021;6(2):188‐194. doi: 10.1002/lio2.549 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Thangamathesvaran LM, Patel N, Siddiqui SH, et al. The otolaryngology match: a bibliometric analysis of 222 first‐year residents: bibliometric analysis of 222 ENT interns. Laryngoscope. 2019;129(7):1561‐1566. doi: 10.1002/lary.27460 [DOI] [PubMed] [Google Scholar]
- 14. Massenzio SS, Uhler TA, Massenzio EM, et al. Navigating the ophthalmology & urology match with a significant other. J Surg Educ. 2022;80:135‐142. doi: 10.1016/j.jsurg.2022.07.026 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. NMRP . Charting the Outcomes in the Match: Senior Students of U.S. M.D. Schools; 2022. Accessed October 24, 2022. https://www.nrmp.org/match-data-analytics/residency-data-reports/
- 16. ERAS Statistics—Otolaryngology . AAMC; 2021. Accessed October 24, 2022. https://www.aamc.org/data-reports/interactive-data/eras-statistics-data
- 17. AAMC . Supplemental ERAS Application Guide; 2022. Accessed August 22, 2022. https://students-residents.aamc.org/media/12326/download
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental Figure S1: Inclusion/exclusion diagram
Supplemental Table S1: Applicant‐level factors predicting interview offer totals and match outcomes
Supplemental Table S2: Comparison between Texas STAR and NRMP Charting the Outcomes


