Abstract
Objective
We aimed to compare the graft success rate and hearing outcomes in patients with large tympanic membrane (TM) perforation in underlay and over‐underlay approaches.
Methods
This is a prospective double‐blind randomized controlled clinical trial with a parallel design. Patients aged 15–75 years old with large TM perforation (more than 50% of TM) who operated at Khalili hospital affiliated with Shiraz University of Medical Science, Iran, were enrolled. Exclusion criteria were recent otorrhea, revision surgery, and pathologic intraoperative findings such as the presence of cholesteatoma, cholesterol granuloma, ear canal polyp, or damaged ossicle. In the first group, the underlay method and in the second group over‐underlay method were performed. Graft success rate, atelectasis, and audiology outcomes were evaluated after 6 months.
Results
The investigation was conducted on 84 patients in the underlay and 67 patients in the over‐underlay group. Although there was a higher rate of graft failure (9%) in the over‐underlay group in comparison with the underlay group (4.8%), the difference was not statistically significant (p‐value = .34). No atelectasis was seen in both group. Although, between‐groups comparison of the preoperative and postoperative speech reception thresholds (SRT) and air‐bone gaps (ABG) values showed statistically significantly lower SRT and ABG in the over‐underlay technique, the difference was clinically negligible.
Conclusion
Both techniques provide the same graft success rate, but SRT and ABG were significantly lower in the over‐underlay technique after the operation.
Levels of Evidence
1b
Keywords: graft success rate, over‐underlay, tympanic membrane perforation, tympanoplasty, underlay method
1. INTRODUCTION
Chronic otitis media (COM) surgery is common all over the world, especially in developing countries. The aim of COM surgery is the reconstruction of tympanic membrane (TM) perforation and the establishment of a sound‐conducting structure in a well‐aerated middle ear. 1 , 2 , 3 Surgical technique is an important factor in the graft success rate. 4 , 5 Different materials and techniques have been developed for tympanoplasty. 6 , 7 , 8 The two main methods commonly used are overlay and underlay. 4
The underlay method is commonly used due to its relatively easy procedure. This procedure is perfect for restoring posterior perforations. In this procedure, TM reconstructs at the right level relative to the annulus and ossicles. 9 The disadvantages of this method are diminished middle ear cavity space, the possibility of adhesions and atelectasis, increased failure rate due to low vascularity of the graft, and limited middle ear visibility. 9 , 10
In the overlay procedure, the graft is inserted lateral to the annulus after the complete removal of the surface epithelium. 11 , 12 The overlay technique is usually used for total perforations, anterior perforations, or in cases of failure of the underlay method. 11 In this technique, extremely good visualization of the anterior TM remnant, which is essential for anterior perforations in an attempt to reach the anterior annulus, is provided. Additionally, the graft success rate is high (more than 90%). The most major disadvantages are the blunting of the anterior portion of TM, iatrogenic cholesteatoma, and lateralization of the graft; however, this procedure needs more experience of the surgeon, and the recovery time is slower. 11 , 12
Few surgeons have used a more recent surgical procedure called the over‐underlay method. 13 The graft is inserted medial to the TM remnant (similar to the underlay method) and lateral to the malleus (similar to the overlay method). It would reduce the disadvantages of the overlay method (such as the graft lateralization and closure of the anterior canal angel) and mitigate underlay technique problems (such as atelectasis). 13 , 14 This method was described for the first time by Kartush et al. 15
However, there is still uncertainty about the outcomes of over‐underlay tympanoplasty and significant variations in the reported graft success rates.
Therefore, we purposed to compare the graft success rate and hearing outcomes in patients with large TM perforation in underlay and over‐underlay approaches.
2. MATERIALS AND METHODS
2.1. Trial design
This is a double‐blind randomized controlled clinical trial with a parallel design. Patients aged 15–75 years old with large TM perforation (>50%) were operated by the first author at Khalili hospital affiliated with Shiraz University of Medical Science, Shiraz, Iran, from September 2021 to March 2022.
The proposal was reviewed and approved by the Ethics Committee of Shiraz University of Medical Sciences (IR.SUMS.MED.REC.1398.306). The study was registered at the Iranian Registry of Clinical Trials (IRCT20200209046432N1; http://www.irct.ir/). All interventions were in agreement with the Helsinki Declaration of 1964. Participation in this study was completely voluntary. All patients signed the written informed consent before their involvement.
2.2. Participants
Inclusion criteria were age 15–75 years old, large TM perforation (more than 50% of TM), at least 1 month without otorrhea, and primary surgery. Exclusion criteria were recent ear infection (otorrhea), revision surgery, and pathologic intraoperative findings such as the presence of cholesteatoma, cholesterol granuloma, ear canal polyp, or damaged ossicle.
2.3. Interventions
Under general anesthesia, after a postauricular incision, the auricle was retracted to the front. The edge of the perforation was freshened, and after that, the tympanomeatal flap was elevated along with the posterior annulus to go in the middle ear. Subsequently, the status of the ossicular chain and the existence of pathology were assessed.
In the first group, the temporalis facia graft was placed medial to the TM residue and handle of the malleus (underlay technique). In the second group, the temporalis facia graft was inserted medial to the TM remnant and lateral to the malleus handle (over‐underlay technique).
Gelfoam (Gelita‐Spon®; Gelita Medical, Eberbach, Germany) was put in to pack the middle ear. Then, the tympanomeatal flap gives back to its normal place. The medial portion of the external meatus was also filled with gelfoam. A tetracycline‐impregnated gauze ointment was put in the external auditory canal. After that, the posterior auricular incision was sutured in two layers. A pressure bandage was used on the first day. A light dressing was applied after the first day.
Post‐operatively, a capsule of cephalexin (500 mg) was prescribed every 6 h for 1 week. Ciprofloxacin (four drops every 6 h) and betamethasone (three drops every 8 h) ear drops were used by patients for 1 week.
Tetracycline‐impregnated gauze pack was removed 3 days after the operation. Postauricular sutures were removed 10 days after the operation. Gentle ear suction was done to remove the remained gelfoam in the external auditory canal 21 days after the operation. The participants were visited by the main otolaryngologist as a routine follow‐up. In addition, the other independent surgeon visits the patients to prevent bias. The rate of graft success and atelectasis were assessed by microscopic otoscopy after 6 months.
Preoperative and postoperative air conduction (AC), bone conduction (BC), air‐bone gaps (ABG), speech reception thresholds (SRT), and speech discrimination score (SDS) were measured. A preoperative audiogram was done 1 week before the surgery, and an audiogram 6 months after the surgery was designated as a postoperative audiogram. To calculate ABG, we computed the mean of AC–BC at frequencies 500, 1000, 2000, and 4000 Hz.
2.4. Outcomes
The primary outcome was graft success rate and atelectasis 6 months after surgery according to a microscopic ear examination. The secondary outcome was postoperative audiometric tests 6 months after the surgery.
2.5. Sample size
Based on the results of Khalifa et al.'s 16 study (post‐operative atelectasis rate in over‐underlay (3.8%) and underlay (20%) group), considering alpha = 0.05 and beta = 0.2, at least 62 patients were required in each group. By considering a drop‐out rate of 20%, at least 77 patients should be enrolled in each group.
2.6. Randomization
The study population was randomly divided into two groups (Groups A and B) (allocation ratio: 1:1) using the random allocation rule and online randomization website (https://randomization.com).
According to that list, the relevant envelope was delivered to the patients. Patients were asked not to open the envelopes delivered to them containing the letter A or B and to only deliver the closed envelope on the day of the operation to the surgeon. The patients underwent surgery based on their groups: A, underlay method; B, over‐underlay method.
2.7. Blinding
Participants, outcome assessors (independent surgeon and audiologist), and the statistician were all blinded to the participants' group until the statistical analysis was done. The patients did not have an operation note when referring to the audiologist and independent otolaryngologist for a postoperative visit. Thus, the second otolaryngologist and audiologist were not informed about the patients' groups.
2.8. Statistical methods
Categorical parameters were expressed as frequency and percentage. Quantitative parameters were described as mean ± SD. Chi‐square or Fisher's exact test was applied to determine the probable relations between the categorical variables, if suitable. Parametric and nonparametric continuous parameters were analyzed via paired sample t‐test, independent t‐test, Mann–Whitney U tests, and Wilcoxon, where appropriate. The p‐values < .05 were considered statistically significant. The data were analyzed by SPSS 25 software (SPSS Inc., Chicago, Illinois).
3. RESULTS
Totally 180 patients were selected and divided into two groups. Each group contained 90 patients. In the underlay and over‐underlay groups, 6 and 23 patients did not continue the follow‐up, respectively. Finally, the investigation was conducted on 84 patients in the underlay and 67 patients in the over‐underlay group (Figure 1).
FIGURE 1.
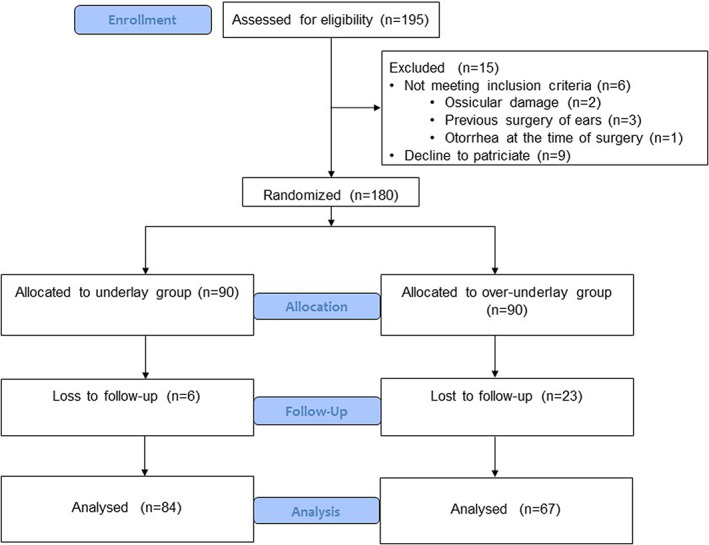
Flowchart of the study participants.
The mean (±SD) age of the study population was 40.8 ± 11.9 years (range 20–72). 74.8% of patients were female (N = 113) and 25.2% were male (N = 38). The results of baseline characteristics and preoperative examination are shown in Table 1. There was no significant difference between the two groups regarding age, gender, and side and site of perforation.
TABLE 1.
Baseline characteristics of the study population.
| Variables | Total (N = 151) | Underlay method (N = 84) | Over‐underlay method (N = 67) | p‐Value |
|---|---|---|---|---|
| Age | ||||
| Mean ± SD | 40.8 ± 11.9 | 40.4 ± 11.6 | 41.3 ± 12.3 | .67 a |
| Gender | ||||
| Male | 38 (25.2%) | 21 (25%) | 17 (25.4%) | 1.00 b |
| Female | 113 (74.8%) | 63 (75%) | 50 (74.6%) | |
| Smoking | .06 b | |||
| Yes | 48 (31.8%) | 26 (31.0%) | 22 (32.8%) | |
| No | 103 (68.2%) | 58 (69.0%) | 45 (67.2%) | |
| Side of perforation | ||||
| Right | 62 (41.1%) | 39 (46.4%) | 23 (34.3%) | .14 b |
| Left | 89 (58.9%) | 45 (53.6%) | 44 (65.7%) | |
| Site of perforation | ||||
| Subtotal | 68 (45%) | 32 (38.1%) | 36 (53.7%) | |
| Central | 51 (33.8%) | 32 (38.1%) | 19 (28.4%) | .14 b |
| Inferior | 1 (0.7%) | — | 1 (1.5%) | |
| Posterior | 19 (12.6%) | 14 (16.7%) | 5 (7.5%) | |
| Anterior | 12 (7.9%) | 6 (7.1%) | 6 (9%) |
Independent t‐test.
Chi‐square.
The middle ear risk index (MERI) score consists of the presence of otorrhea, perforation, presence of cholesteatoma, ossicular status, ossicular head fixation, previous surgery, and patient smoking. 17 Based on our inclusion and exclusion criteria, we did not include patients with otorrhea, revision surgery, cholesteatoma, cholesterol granuloma, and ossicular abnormality. There was only a number of patients with a history of smoking (Table 1). Therefore, the MERI score is between 1 and 3 in all of our cases which are considered mild diseases.
Table 2 compares the graft success rate and atelectasis between the two groups. Although there was a higher rate of graft failure (9%) in the over‐underlay group in comparison with the underlay group (4.8%), the difference was not statistically significant (p‐value = 0.34). No atelectasis was seen in both group. The outcome of tympanoplasty was compared between groups based on the site of perforation, as shown in Table 3.
TABLE 2.
The outcome of tympanoplasty.
| Variables | Outcome | Total | Underlay method | Over‐underlay method | p‐Value |
|---|---|---|---|---|---|
| Graft success rate | Successful | 141 (93.4%) | 80 (95.2%) | 61 (91%) | .34 a |
| Unsuccessful | 10 (6.6%) | 4 (4.8%) | 6 (9%) | ||
| Atelectasis | No | 151 (100%) | 84 (100%) | 67 (100%) | ND |
| Yes | (0%) | 0 (0%) | 0 (0%) |
Abbreviation: ND, nondeterminable.
Chi‐square.
TABLE 3.
The outcome of tympanoplasty based on the site of perforation.
| Site of perforation | Successful | Unsuccessful | p‐Value a | |
|---|---|---|---|---|
| Underlay method | Subtotal | 31 (96.88%) | 1 (3.12%) | .85 |
| Central | 30 (93.75%) | 2 (6.25%) | ||
| Inferior | 0 (0%) | 0 (0%) | ||
| Posterior | 13 (92.86%) | 1 (7.14%) | ||
| Anterior | 6 (100%) | 0 (0%) | ||
| Over‐underlay method | Subtotal | 33 (91.67%) | 3 (8.33%) | .01 |
| Central | 19 (100%) | 0 (0%) | ||
| Inferior | 0 (0%) | 1 (100%) | ||
| Posterior | 4 (80.00%) | 1 (20.00%) | ||
| Anterior | 5 (83.33%) | 1 (16.67%) | ||
Chi‐square.
The results of preoperative and postoperative audiometry are reported in Table 4. Between‐group comparison of the preoperative and postoperative SDS was not statistically significant (p‐value = .18). Although, between‐groups comparison of the preoperative and postoperative SRT and ABG values showed statistically significantly lower SRT and ABG in the over‐underlay technique, the difference was clinically negligible.
TABLE 4.
The results of preoperative and postoperative audiometry.
| Variables | Total | Underlay method | Over‐underlay method | p‐Value a | p‐Value b |
|---|---|---|---|---|---|
| SDS | |||||
| Preoperative | 98.1 ± 4.33 | 98.1 ± 4.8 | 98.0 ± 3.65 | .89 | .18 |
| Postoperative | 97.8 ± 4.1 | 97.9 ± 4.9 | 97.7 ± 2.9 | .77 | |
| SRT | |||||
| Preoperative | 32.8 ± 11.7 | 30.7 ± 11.0 | 35.5 ± 12.1 | .11 | <.001 |
| Postoperative | 20.33 ± 9.2 | 17.9 ± 7.7 | 23.3 ± 10.1 | <.001 | |
| ABG | |||||
| Preoperative | 24.5 ± 7.25 | 23.5 ± 7.3 | 25.6 ± 7.0 | .07 | <.001 |
| Postoperative | 11.4 ± 6.5 | 10.4 ± 6.3 | 12.8 ± 6.4 | .02 |
Abbreviations: ABG, air‐bone gaps; SDS, speech discrimination score; SRT, speech reception thresholds.
A p‐value for within‐groups comparison.
A p‐value for between‐groups comparison.
4. DISCUSSION
In this study, although there was a higher rate of graft failure in the over‐underlay group in comparison with the underlay group, the difference was not statistically significant.
The over‐underlay tympanoplasty was described for the first time by Kartush et al. 15 They reported a 100% success rate in 120 patients. This method is a simple technique that combines the advantages of overlay and underlay techniques and minimizes the disadvantages of those methods. The ideal reconstructive method must provide a fine, conically formed, vibrating membrane replacing the original TM to stop the infection and reestablish the auditory function. 13 , 16
In the case of large TM perforation, the failure rate is high due to procedural difficulty and bigger areas that should be vascularized and epithelialized. 5 , 13 The absence of a suitable TM remnant in subtotal or total TM perforations is a challenge.
Several studies on these two methods have been reported. Karela et al. 18 published the results of 211 participants who underwent underlay tympanoplasty for perforations of any dimensions and location. They attained a 91.5% success rate and 14.67 dB improvement in ABG in these patients. Panchal et al. 19 compared the results of the over‐underlay method with the underlay myringoplasty. Underlay myringoplasty was done for 20 patients underwent and 20 patients underwent over‐underlay myringoplasty. After a follow‐up interval of 3 months, although the graft success rate was 90% in underlay myringoplasty in comparison with 95% in over‐underlay myringoplasty, the difference was not significant (p = .5). There was a statistically significant difference in ABG gain in the underlay myringoplasty (14.5 ± 7.236 dB) compared with over‐underlay myringoplasty (18.75 ± 5.349; p = .04). They concluded that the over‐underlay technique provided a more graft success rate and auditory outcome in subtotal and large perforations. Another similar study compared over‐underlay and underlay myringoplasty. A total of 62 patients were studied. After 6 months of follow‐up, the graft success rate was 94.1% in the over‐underlay technique and 92.8% in the underlay technique (p < .05). Medialization of the graft was reported in 1 patient (2.9%) in the over‐underlay group, while it was seen in 5 (17.8%) patients in the underlay group (p > .05). Lateralization of the graft was not observed in any case in both group. The mean ABG closure was 10.8 ± 5.56 dB in the over‐underlay group compared with 11.3 ± 5.84 dB in the underlay group (p < .05). They concluded that the over‐underlay method was similar to the underlay technique in terms of graft success rate and auditory outcomes. 20 In a retrospective study by Babu et al., 21 long‐term outcomes and complications of over‐under tympanoplasty were compared with medial tympanoplasty. A total of 111 patients were included; 84 of them were in the over‐underlay group and 27 in the medial tympanoplasty group. After an 18‐month follow‐up, the graft success rate was 100% in the medial tympanoplasty group in comparison with 84% in the over‐under group. The mean ABG closure was similar between the two groups (11.6 dB in medial tympanoplasty versus 11.9 dB for the over‐under tympanoplasty, p < .001). Graft lateralization, anterior blunting, and hearing loss were not reported in any patients. They found this method to be an effective tympanoplasty technique. In another research, Jung and Parks 22 used the mediolateral graft technique to reconstruct subtotal and anterior perforations. They showed 97% TM healing and complications in 5% of cases.
In some studies, the over‐underlay technique was performed using cartilage. In the investigation by Kazikdas et al., 23 the graft success rate was 95.7% by over‐under method with cartilage tympanoplasty, and 75% using temporal fascia in 51 patients with subtotal perforations. A retrospective study by Erbele et al. 24 investigated the over‐under cartilage tympanoplasty technique. In this study, 68 patients were included. The average improvement in air conduction was 6 dB (95% CI: 4–9 dB; p < .0001). The overall healing rate was 97%. They concluded that over‐under cartilage tympanoplasty was a good method for significant improvement of auditory outcomes with a low rate of postoperative complications. Çetin and Erdem 25 evaluated the outcome of cartilage tympanoplasty for the reconstruction of dry subtotal perforations. They performed the endaural over‐underlay method. Cartilage perichondrium tympanoplasty showed a graft success rate of 96% in a total of 195 participants.
Comparing our results to related studies revealed that the overall success rate of both operations was acceptable in our center, which is comparable to similar centers around the world. The statistical analysis could not demonstrate a significant difference between the underlay and over‐underlay intervention groups regarding the hearing outcomes and success rate; however, the underlay technique showed a slightly higher graft success rate.
The most important strength of this instigation was its design which was a prospective randomized clinical trial. In addition, we included a relatively large sample size and a control group. The only limitation was a quite short follow‐up time.
5. CONCLUSION
Therefore, we can conclude that both techniques are efficient and successful methods of tympanoplasty surgery. Further investigations are needed to explain the short‐term and long‐term advantages and disadvantages of these surgery methods.
CONFLICT OF INTEREST STATEMENT
The authors declare that they have no conflict of interest.
ACKNOWLEDGMENTS
This article was extracted from the residency thesis written by Dr. Dorna Biniaz and supported by the Vice‐Chancellor for Research of Shiraz University of Medical Sciences (97‐01‐01‐17598). The authors would like to thank Shiraz University of Medical Sciences, Shiraz, Iran and also the Center for Development of Clinical Research of Nemazee Hospital and Dr. Nasrin Shokrpour for editorial assistance.
Shishegar M, Faramarzi M, Biniaz D, Rabiei N, Babaei A. Comparison of the underlay and over‐underlay tympanoplasty: A randomized, double‐blind controlled trial. Laryngoscope Investigative Otolaryngology. 2023;8(2):518‐524. doi: 10.1002/lio2.1015
REFERENCES
- 1. Visvanathan V, Vallamkondu V, Bhimrao SK. Achieving a successful closure of an anterior tympanic membrane perforation: evidence‐based systematic review. Otolaryngol Head Neck Surg. 2018;158(6):1011‐1015. [DOI] [PubMed] [Google Scholar]
- 2. Hardman J, Muzaffar J, Nankivell P, Coulson C. Tympanoplasty for chronic tympanic membrane perforation in children: systematic review and meta‐analysis. Otol Neurotol. 2015;36(5):796‐804. [DOI] [PubMed] [Google Scholar]
- 3. Faramarzi M, Kazemi T, Shishegar M, et al. Does intraoperative ciprofloxacin‐soaked gelfoam have adverse effects on graft success rate? A randomized, double‐blind controlled trial. Laryngoscope Investig Otolaryngol. 2021;6(5):1182‐1187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Aggarwal R, Saeed SR, Green KJ. Myringoplasty. J Laryngol Otol. 2006;120(6):429‐432. [DOI] [PubMed] [Google Scholar]
- 5. Darouassi Y, Aljalil A, Ennouali A, et al. Prognostic factors of myringoplasty: study of a 140 cases series and review of the literature. Pan Afr med J. 2019;33:323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Shakya D, Nepal A. Long‐term results of type I tympanoplasty with perichondrium reinforced cartilage palisade vs temporalis fascia for large perforations: a retrospective study. J Otol. 2021;16(1):12‐17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Arora RD, Thakur N, Kamble P, Jati M, Nagarkar NM, Thakur JS. Circumferential subannular tympanoplasty: surgical and hearing outcome in 224 ears with subtotal perforation. Acta Otolaryngol. 2022;142(3–4):254‐258. [DOI] [PubMed] [Google Scholar]
- 8. Brar S, Watters C, Tympanoplasty WR. StatPearls. StatPearls Publishing; 2022. [PubMed] [Google Scholar]
- 9. Barake R, El Natout T, Bassim M, El Natout MA. Loop underlay tympanoplasty for anterior, subtotal and total tympanic membrane perforations: a retrospective review. J Otolaryngol Head Neck Surg. 2019;48(1):12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Singh NK, Nagpure PS, Yadav M, Chavan S. Comparative study of permeatal sandwich tympanoplasty and postaural underlay technique. J Clin Diagn Res. 2016;10(4):Mc01‐Mc04. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Shim DB, Kim HJ, Kim MJ, Moon IS. Three‐point fix tympanoplasty. Acta Otolaryngol. 2015;135(5):429‐434. [DOI] [PubMed] [Google Scholar]
- 12. Park SY, Lee HJ, Shim MJ, Kim DK, Suh BD, Park SN. Swing‐door overlay Tympanoplasty: surgical technique and outcomes. Clin Exp Otorhinolaryngol. 2018;11(3):186‐191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Bayazit YA, Ozer E, Kara C, Gökpinar S, Kanlikama M, Mumbuç S. An analysis of the single‐stage tympanoplasty with over‐underlay grafting in tympanosclerosis. Otol Neurotol. 2004;25(3):211‐214. [DOI] [PubMed] [Google Scholar]
- 14. Kulduk E, Dundar R, Soy FK, et al. Treatment of large tympanic membrane perforations: medial to malleus versus lateral to malleus. Indian J Otolaryngol Head Neck Surg. 2015;67(2):173‐179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Kartush JM, Michaelides EM, Becvarovski Z, LaRouere MJ. Over‐under tympanoplasty. Laryngoscope. 2002;112(5):802‐807. [DOI] [PubMed] [Google Scholar]
- 16. Khalifa MC, Khalifa BC. Over‐under myringoplasty. Med J Cairo Univ. 2011;79:165‐168. [Google Scholar]
- 17. Shishegar M, Faramarzi M, Rashidi RM. Evaluation of middle ear risk index in patients undergoing tympanoplasty. Eur Arch Otorhinolaryngol. 2019;276(10):2769‐2774. [DOI] [PubMed] [Google Scholar]
- 18. Karela M, Berry S, Watkins A, Phillipps JJ. Myringoplasty: surgical outcomes and hearing improvement: is it worth performing to improve hearing? Eur Arch Otorhinolaryngol. 2008;265(9):1039‐1042. [DOI] [PubMed] [Google Scholar]
- 19. Panchal V, Gulia JS, Yadav SP, Hernot S, Kathuria B, Kaintura M. To evaluate and compare the results of over‐underlay graft technique with conventional underlay myringoplasty. Indian J Otol. 2015;21(4):274. [Google Scholar]
- 20. Aslam MA, Aslam MJ. Comparison of over‐underlay and underlay techniques of Myringoplasty. Pak Armed Forces Med J. 2009;59(2):189‐193. [Google Scholar]
- 21. Babu S, Luryi AL, Schutt CA. Over‐under versus medial tympanoplasty: comparison of benefit, success, and hearing results. Laryngoscope. 2019;129(5):1206‐1210. [DOI] [PubMed] [Google Scholar]
- 22. Jung TT, Park SK. Mediolateral graft tympanoplasty for anterior or subtotal tympanic membrane perforation. Otolaryngol Head Neck Surg. 2005;132(4):532‐536. [DOI] [PubMed] [Google Scholar]
- 23. Kazikdas KC, Onal K, Boyraz I, Karabulut E. Palisade cartilage tympanoplasty for management of subtotal perforations: a comparison with the temporalis fascia technique. Eur Arch Otorhinolaryngol. 2007;264(9):985‐989. [DOI] [PubMed] [Google Scholar]
- 24. Erbele ID, Fink MR, Mankekar G, Son LS, Mehta R, Arriaga MA. Over‐under cartilage tympanoplasty: technique, results and a call for improved reporting. J Laryngol Otol. 2020;134:875‐881. [DOI] [PubMed] [Google Scholar]
- 25. Çetin YS, Erdem MZ. Endaural over‐underlay cartilage Tympanoplasty for repair of dry subtotal perforations. Ann Otol Rhinol Laryngol. 2021;130:1345‐1350. [DOI] [PubMed] [Google Scholar]


