ABSTRACT
The molecular evolutionary mechanisms underpinning virus-host interactions are increasingly recognized as key drivers of virus emergence, host specificity, and the likelihood that viruses can undergo a host shift that alters epidemiology and transmission biology. Zika virus (ZIKV) is mainly transmitted between humans by Aedes aegypti mosquitoes. However, the 2015 to 2017 outbreak stimulated discussion regarding the role of Culex spp. mosquitoes in transmission. Reports of ZIKV-infected Culex mosquitoes, in nature and under laboratory conditions, resulted in public and scientific confusion. We previously found that Puerto Rican ZIKV does not infect colonized Culex quinquefasciatus, Culex pipiens, or Culex tarsalis, but some studies suggest they may be competent ZIKV vectors. Therefore, we attempted to adapt ZIKV to Cx. tarsalis by serially passaging virus on cocultured Ae. aegypti (Aag2) and Cx. tarsalis (CT) cells to identify viral determinants of species specificity. Increasing fractions of CT cells resulted in decreased overall virus titer and no enhancement of Culex cell or mosquito infection. Next-generation sequencing of cocultured virus passages revealed synonymous and nonsynonymous variants throughout the genome that arose as CT cell fractions increased. We generated nine recombinant ZIKVs containing combinations of the variants of interest. None of these viruses showed increased infection of Culex cells or mosquitoes, demonstrating that variants associated with passaging were not specific to increased Culex infection. These results reveal the challenge of a virus adapting to a new host, even when pushed to adapt artificially. Importantly, they also demonstrate that while ZIKV may occasionally infect Culex mosquitoes, Aedes mosquitoes likely drive transmission and human risk.
IMPORTANCE ZIKV is mainly transmitted between humans by Aedes mosquitoes. In nature, ZIKV-infected Culex mosquitoes have been found, and ZIKV infrequently infects Culex mosquitoes under laboratory conditions. Yet, most studies show that Culex mosquitoes are not competent vectors for ZIKV. We attempted to adapt ZIKV to Culex cells to identify viral determinants of species specificity. We sequenced ZIKV after it was passaged on a mixture of Aedes and Culex cells and found that it acquired many variants. We generated recombinant viruses containing combinations of the variants of interest to determine if any of these changes enhance infection in Culex cells or mosquitoes. Recombinant viruses did not show increased infection in Culex cells or mosquitoes, but some variants increased infection in Aedes cells, suggesting adaptation to those cells instead. These results reveal that arbovirus species specificity is complex, and that virus adaptation to a new genus of mosquito vectors likely requires multiple genetic changes.
KEYWORDS: arbovirus, mosquito, species specificity, virology
INTRODUCTION
Zika virus (ZIKV; genus Flavivirus) is an arthropod-borne virus (arbovirus) transmitted mainly by Aedes aegypti and secondarily by Ae. albopictus mosquitoes across large parts of the world. ZIKV was first isolated from a sentinel rhesus monkey in the Ziika forest of Uganda in 1947 (1) and only a few sporadic cases in various African countries were reported over the next 60 years. In 2007 however, a large outbreak was reported on Yap Island in Indonesia, infecting over 70% of the population (2) and a second Asian lineage of ZIKV was identified in 2012 (3). During 2013 and 2014, the virus caused outbreaks in various Pacific islands, such as French Polynesia, Easter Island, the Cook Islands, and New Caledonia (4, 5), and was likely introduced to the Americas in late 2013 or early 2014 (6), but remained undetected until early 2015. The mosquito vectors for these outbreaks were thought to be Ae. aegypti and Ae. polynesiensis (specifically in the Pacific islands) (7, 8). However, once ZIKV reached Brazil, researchers increasingly started implicating the Southern house mosquito, Culex quinquefasciatus, in ZIKV transmission (7, 9).
Many studies have evaluated the ability of ZIKV to infect and be transmitted by various Culex spp. mosquitoes. ZIKV has been isolated from pools of Cx. quinquefasciatus collected during the pandemic, but generally with low levels of viral RNA present (10, 11). There are two laboratory studies demonstrating substantial infection rates (+80%) of Cx. quinquefasciatus mosquitoes, and in one study, 80% transmission (12, 13). Conversely, there are over 17 studies showing none to minimal infection of, and no transmission of ZIKV by Cx. quinquefasciatus mosquitoes (9, 11, 14–18). Studies evaluating additional Culex species, including Cx. tarsalis, Cx. pipiens, Cx. restuans, and Cx. coronator, reveal similar results; while Culex mosquitoes can occasionally become infected, there is no convincing evidence that they are competent vectors for ZIKV (19), particularly compared with established Aedes vectors. The literature on the subject remains controversial, and there are at least three potential explanations for this variability: successful ZIKV infection of Culex mosquitoes depends on (i) the specific ZIKV genotype, (ii) the genetic background of the mosquito population, or (iii) complex environmental factors (e.g., microbiome).
There are many instances of arboviruses acquiring small genetic changes that lead to either improved fitness in mosquitoes or the ability to infect a new species more efficiently. Chikungunya virus, which is most frequently transmitted by Ae. aegypti mosquitoes, acquired a single coding change in the envelope protein, which led to a significant increase in the virus's ability to be transmitted by Ae. albopictus mosquitoes (20). As West Nile virus spread throughout North America, a new subtype (WN02) emerged containing a single amino acid change (E-V159A) (21, 22). This change led to increased replication in Cx. pipiens and Cx. tarsalis mosquitoes and a shorter extrinsic incubation period (22, 23), leading to the displacement of the original NY99 genotype. In a laboratory setting, Mayaro virus was adapted to Ae. aegypti cells, which identified a single envelope coding change (E2-T179N) that resulted in increased transmission by Ae. aegypti mosquitoes (24). In a similar experiment, Sindbis virus was passaged on cocultures of BHK-21 (highly susceptible) and CHO cells (poorly susceptible) to improve fitness on CHO cells. The authors showed that a gradual increase in the “novel host cell” (CHO) over 25 passages resulted in increased Sindbis virus fitness in CHO cells with the virus acquiring many genetic changes likely contributing to the improved fitness (25).
In this study, we tested vector competence of multiple Culex spp. mosquitoes to three ZIKV isolates, both through artificial bloodmeal and intrathoracic microinjection to set a baseline of vector competence for our existing colonies. We then aimed to determine whether the Puerto Rican ZIKV isolate can be adapted to replication in Cx. tarsalis CT cells through a coculture approach using highly susceptible Ae. aegypti Aag2 and less susceptible CT cells, similar to previous experiments by Morley et al. (25). While this is an artificial set-up and not meant to directly mimic natural conditions of ZIKV replication, it creates conditions where CT cells are constantly exposed to ZIKV, possibly allowing for the selection of adaptive mutations to arise. For our purposes, Aag2 and CT cells are highly suitable for this type of approach as they grow under the same culture conditions. We infected a culture with predominantly Aag2 cells and passaged the virus through cocultures with ever increasing proportions of CT cells (see results section). Once we reached 90% CT cells within the coculture (18 passages), a point where we may have “adapted” the virus to growth on CT cells, we sequenced virus populations from all coculture passages to identify single nucleotide variants (SNVs) of interest and associated with increasing ratios of CT cells. Using our infectious clone, we generated recombinant ZIKVs containing the SNVs of interest and evaluated viruses for ability to infect Aedes and Culex cells and mosquitoes. We found that while the virus accumulated many coding and noncoding changes during passaging, none of the variants studied improved infection of Culex cells or mosquitoes. These results reveal that likely multiple genetic changes would need to occur for ZIKV to be efficiently transmitted by Culex in nature.
RESULTS
Infection of Cx. quinquefasciatus with three strains of ZIKV.
We first sought to determine if Culex mosquitoes are competent vectors of ZIKV using three genetically distinct virus strains. Cx. quinquefasciatus mosquitoes were provided an infectious virus bloodmeal or injected intrathoracically with virus and held at either 28°C or 32°C postinfection for 7 days (Table 1). We observed low infection rates (<2%) following bloodmeal infection, independent of the virus strain or external incubation temperature (P > 0.05). Due to these extremely low infection rates, we did not test for dissemination or transmission. Following intrathoracic injection, which bypasses the midgut barrier, we observed significantly higher infection rates for the Ugandan strain (MR766; 20%) and the Dakar strain (41525; 57%), but there was still no dissemination to the saliva. These data confirm that while Culex mosquitoes can occasionally become infected with ZIKV (26, 27), there are likely multiple barriers to infection and transmission. Further, they confirm virus strain-dependent variation in replication within mosquitoes.
TABLE 1.
Vector competence of Cx. quinquefasciatus for three ZIKV strainsa
| Infection by | Extrinsic incubation temp | ZIKV strain | ZIKV pos bodies | ZIKV pos legs/wings | ZIKV pos saliva |
|---|---|---|---|---|---|
| Bloodmeal | 28°C | PRVABC59 | 1/72 (1.4%) | Not tested | Not tested |
| MR766 | 1/66 (1.5%) | Not tested | Not tested | ||
| 41525 | 1/72 (1.4%) | Not tested | Not tested | ||
| Bloodmeal | 32°C | PRVABC59 | 1/108 (0.9%) | Not tested | Not tested |
| MR766 | 2/108 (1.9%) | Not tested | Not tested | ||
| 41525 | 2/108 (1.9%) | Not tested | Not tested | ||
| Intrathoracic injection | 28°C | PRVABC59 | 0/30 (0%) | 0/30 (0%) | 0/30 (0%) |
| MR766 | 6/30 (20%)b | 1/30 (3.3%) | 0/30 (0%) | ||
| 41525 | 17/30 (57%)c | 10/30 (33%)d | 0/30 (0%) |
ZIKV infection was determined by standard plaque assay on Vero cells. Significant differences between MR766 and 41525 compared to PRVABC59 for each tissue type and infection condition using a Chi-square test are shown.
P < 0.005.
P < 0.0005.
P < 0.0001.
Low level infection of Culex cells with ZIKV.
We next wanted to see if a Cx. tarsalis cell line (CT cells, originally derived from embryonic tissue) could support low level ZIKV replication, since it has previously been shown that Cx. tarsalis mosquitoes are more easily infected than other Culex spp. (27). We infected cells at a high multiplicity of infection (MOI = 20), sampled supernatant daily, and assayed for both viral RNA and infectious virus (Fig. 1). We observed an increase in extracellular viral RNA in the first 2 days to a level that was sustained throughout the time course (Fig. 1A). While infectious virus levels dropped early following infection, levels increased by 4 days postinfection and remained elevated, suggesting some production of infectious ZIKV by CT cells (Fig. 1B).
FIG 1.

Low level replication of ZIKV in CT cells. Cx. tarsalis CT cells were infected at an MOI of 20 with ZIKV PRVABC59 virus, supernatant collected daily, and analyzed for (A) viral RNA via qRT-PCR and (B) infectious virus via plaque assays. Experiment was performed in biological triplicate (mean ± standard deviation).
Adapting ZIKV to Culex cells.
Because we saw low level infection of ZIKV in both Culex mosquitoes and cells, we attempted to adapt ZIKV to Culex cells through copassaging with a highly susceptible cell line to further increase infection and replication efficiency (Fig. 2). Aag2 cells (highly competent for ZIKV) were mixed with CT cells, infected with ZIKV for 6 days, then supernatant was passaged onto new cocultured cells. The ratio of Aag2 to CT cells started high (90% Aag2 to 10% CT), and gradually decreased with each passage until CT cells were 90% by the final passage (Fig. 2A). Virus titers began to decrease when CT cells were >60% of the population, but infectious virus was still detected even in the last passage (Fig. 2B). Due to the low level of infectious virus in the last passage, this passage was expanded once on Vero cells (Co18.1-3V) and evaluated for its ability to infect CT cells at an MOI of 20 (Fig. 2C and D). We saw low-level infection of the passaged virus on CT cells (Fig. 2C and D), similar to the original ZIKV PRVABC59 (Fig. 1).
FIG 2.
ZIKV passaging on Aag2 and CT cells. (A) Schematic of passaging experimental design. Ae. aegypti-derived Aag2 and Cx. tarsalis-derived CT cells were mixed at an initial ratio of 90:10, infected with ZIKV PRVABC59 isolate for 6 days, then culture supernatant was passaged onto new cells. The ratio of Aag2:CT slowly decreased to a final 10:90 ratio over the course of 18 passages. Passaging experiment was performed in biological triplicate. (B) After each passage, supernatant was assayed for infectious virus. (C–D) Cx. tarsalis CT cells were infected at an MOI of 20 with each triplicate of ZIKV passage 18 coculture virus that was passaged once on Vero cells (Co18.1V, Co18.2V and Co18.3V), supernatant collected daily, and analyzed for (C) viral RNA via qRT-PCR and (D) infectious virus via plaque assays. Growth curve experiment was performed in biological triplicate (mean ± standard deviation). Dashed line represents limit of detection. Graphics were generated using BioRender.com.
Infection of three Culex species with passaged virus stocks.
We next evaluated the ability of the passaged virus to infect three species of Culex mosquitoes compared to the parental WT ZIKV via an infectious bloodmeal (Table 2). Due to the low titer of p18 virus (Fig. 2B), we first grew a high titer stock on Vero cells (Co18.1-3V) and exposed Cx. tarsalis, Cx. pipiens, and Cx. quinquefasciatus mosquitoes with these stocks (1 × 107 PFU/mL). We found low levels of ZIKV infection across all species, with Cx. tarsalis having the highest levels of infection. The three cocultured virus stocks showed variable low levels of infection in Cx. tarsalis, ranging from 2.3 to 8.3% positive (compared to 3.3% positive with WT ZIKV) (Table 2). Despite these minor fluctuations, there were no significant differences between infection rates (P > 0.05).
TABLE 2.
Vector competence of Culex mosquitoes with passage 18 virus stocksa
| Species | WT ZIKV | Co18.1V | Co18.2V | Co18.3V |
|---|---|---|---|---|
| Cx. tarsalis | 2/60 (3.3%) | 5/60 (8.3%) | 2/60 (3.3%) | 1/44 (2.3%) |
| Cx. pipiens | 0/32 (0%) | 1/40 (2.5%) | 0/37 (0%) | 0/32 (0%) |
| Cx. quinquefasciatus | 0/47 (0%) | 0/40 (0%) | 0/40 (0%) | 0/32 (0%) |
ZIKV infection was determined by standard plaque assay on Vero cells. Co18.1-3V were not significantly different than WT ZIKV for any mosquito species by a Chi-square test (P > 0.05).
Next-generation-sequencing of ZIKV passages.
To determine genetic changes resulting from passaging of ZIKV on cocultured Aag2 and CT cells, we performed total RNA sequencing of the cocultured stocks after each passage (Co1-18) and from the Vero propagated high titer Co18 stocks (Co18.1-3V). We found 13 single SNVs of interest (Table 3, Fig. 3A), as determined by their increasing frequency once CT cell ratios reached and surpassed 50% of the coculture. We hypothesized that these mutations arose in frequency because of the increasing proportion of CT cells in the culture. Numerous other SNVs were detected that either did not change in frequency, were reduced in frequency over coculture passaging, or changed in frequency randomly between passages. The 13 SNVs of interest spanned the entire genome, were comprised of both synonymous (non-coding) and nonsynonymous (coding) changes and were equally distributed among structural and nonstructural proteins (Fig. 3A). Three such mutations (T1435A, C7460T, C9800T) were found in all three replicate passages and became part of the consensus sequence (>50% allele frequency) by passage 18 in two out of the three replicates (Fig. 3B to D). Frequencies for these mutations were near identical between replicates, suggesting that these SNVs were present on the same ZIKV haplotype. Other SNVs increased to a lower extent, such as A1437G, which gradually increased to ~20% at passage 16, but then decreased in the following passage. The SNVs T1435A and A1437G were of particular interest due to their location at (1437) or immediately adjacent to (1435) the glycosylation site in E (N154). Both SNVs rose in frequency over passaging and resulted in a negatively charged amino acid with a probable (V153D) and definite (N154D) loss of glycosylation at this site.
TABLE 3.
Summary of SNVs of interest
| Genome position | nt constant | nt variant | Viral protein | aa position | S/NS | aa change | Stock SNV frequency | Co18.1-3 SNV frequencya | Detected in replicate |
|---|---|---|---|---|---|---|---|---|---|
| 1019 | T | C | E | 14 | S | - | <0.01 | 0.08 | Co18.3 |
| 1435 | T | A | E | 153 | NS | V > D | <0.01 | 0.53 | Co18.1-3 |
| 1437 | A | G | E | 154 | NS | N > D | <0.01 | 0.14 | Co18.1-3 |
| 1915 | C | T | E | 313 | NS | T > I | <0.01 | 0.20 | Co18.2 |
| 2095 | A | G | E | 373 | NS | K > R | <0.01 | 0.06 | Co18.2 |
| 2150 | C | T | E | 391 | S | - | <0.01 | 0.06 | Co18.2 |
| 2592 | C | T | NS1 | 35 | NS | H > Y | <0.01 | 0.28 | Co18.1-2 |
| 3961 | T | C | NS2A | 139 | NS | I > T | <0.01 | 0.06 | Co18.2-3 |
| 6372 | A | C | NS3 | 590 | NS | K > Q | <0.01 | 0.19 | Co18.1-3 |
| 6559 | T | C | NS4A | 32 | NS | M > T | <0.01 | 0.10 | Co18.1 |
| 7460 | C | T | NS4B | 182 | S | - | <0.01 | 0.39 | Co18.1-3 |
| 8744 | A | G | NS5 | 359 | S | - | <0.01 | 0.24 | Co18.1-2 |
| 9800 | C | T | NS5 | 711 | S | - | <0.01 | 0.42 | Co18.1-3 |
Whenever an SNV was represented in more than one replicate, the mean SNV frequency is shown.
FIG 3.
SNVs associated with ZIKV passaging on Aag2/CT cocultures. (A) Schematic overview of SNVs of interest along the ZIKV PRVABC59 genome. (B–D) Proportion of SNVs out of total virus population (i.e., variant frequencies) for three mutations of interest (B) T1435A, (C) C7460T, (D) and C9800T. Variant frequencies for each passage and each independent passaging replicate are shown. Co18V indicates the Vero propagated virus stock generated by inoculation of Vero cells with Co18 culture supernatant. Dashed line represents 0.5.
Generating viral mutants incorporating SNVs.
To determine the role of any of the SNVs either individually, or in combination with others, we generated mutants using our ZIKV PRVABC59 reverse genetics infectious clone (28) (Fig. 4A). Recombinant viruses were designed for those SNVs considered of highest interest: T1435A (Mut1) and A1437G (Mut2), due to their location on E. A combination of both mutants (Mut3), and a combination of mutations expected to be on the same haplotype as T1435A (Mut4). Other mutations that arose above 15% were introduced individually (Mut5 and Mut7), as well as combinations of those synonymous mutations potentially associated with the same haplotypes (Mut6 and Mut8). The two synonymous mutations likely associated with the T1435A haplotype were also introduced in combination (Mut9). Recombinant viruses were recovered and passaged once on Vero cells to generate working stocks. All viruses grew to high titers (~106-7 PFU/mL) and had similar plaque morphologies (Fig. 4B and C).
FIG 4.
Design and characterization of ZIKV recombinant viruses. (A) Schematic of ZIKV genome, with synonymous (blue) and nonsynonymous (red) variants of interest shown as lines. Genome location and type (synonymous versus nonsynonymous) of variants of each of the recombinant viruses is shown (Mut1-9). (B) Recombinant viruses were recovered, stocks generated, and assayed for infectious virus titer (performed in technical duplicate, mean ± 95% confidence intervals). (C) Plaque morphology of ZIKV recombinant viruses on Vero cells.
Evaluation of recombinant virus’s ability to infect Culex cells and mosquitoes.
CT cells were infected with WT ZIKV and the nine recombinant viruses at an MOI of 5, and supernatant was sampled daily and evaluated for viral RNA and infectious virus (Fig. 5). We saw no indication of enhanced viral replication across any of the chimeric recombinant viruses compared to WT parental virus, revealing that none of the variants lead to increased replication in CT cells (Fig. 5A and B). We then infected two species of Culex mosquitoes (Cx. tarsalis and Cx. quinquefasciatus) with each of the viruses via a bloodmeal and looked at whole body positivity at 7 days postinfection (Table 4). There were only two positive mosquitoes in total, both in Cx. tarsalis; however, none of the recombinant viruses showed substantial improved infection in either species relative to the WT ZIKV (Table 4).
FIG 5.
ZIKV mutants do not infect CT cells. Cx. tarsalis CT cells were infected at an MOI of 5 with ZIKV recombinant mutants, supernatant collected daily, and analyzed for (A) viral RNA via qRT-PCR and (B) infectious virus via plaque assays. Experiment was performed in biological triplicate (mean ± standard deviation). Dashed line represents limit of detection.
TABLE 4.
Vector competence of Culex mosquitoes with ZIKV recombinant virusesa
| Species | WT | Mut1 | Mut2 | Mut3 | Mut4 | Mut5 | Mut6 | Mut7 | Mut8 | Mut9 |
|---|---|---|---|---|---|---|---|---|---|---|
| Cx. tarsalis | 0/40 (0%) | 1/40 (2.5%) | 0/40 (0%) | 0/40 (0%) | 0/40 (0%) | 1/40 (2.5%) | 0/40 (0%) | 0/40 (0%) | 0/40 (0%) | 0/40 (0%) |
| Cx. quinquefasciatus | 0/38 (0%) | 0/40 (0%) | 0/40 (0%) | 0/32 (0%) | 0/40 (0%) | 0/40 (0%) | 0/25 (0%) | 0/40 (0%) | 0/40 (0%) | 0/40 (0%) |
ZIKV infection was determined by standard plaque assay on Vero cells using whole body samples at day 7 postinfection.
Passaging virus increased Aag2 infection.
Because we did not see evidence that passaging virus increased infection of Culex cells or mosquitoes, we hypothesized that passaging instead adapted viruses to Aag2 cells in culture. To test this, we evaluated all viruses for their ability to replicate in Aag2 cells at a high MOI (Fig. 6). We saw significant increases (P < 0.05) of viral RNA replication in many of the recombinants above that of WT ZIKV (Fig. 6A), suggesting adaptation to Aag2 cells. Replication of infectious virus was also significantly increased above that of WT ZIKV for some of the recombinant viruses (Fig. 6B).
FIG 6.
Increased replication of ZIKV recombinant viruses in Aag2 cells. Ae. aegypti-derived Aag2 cells were infected at an MOI of 5 with ZIKV recombinant viruses, supernatant collected daily, and analyzed for (A) viral RNA via qRT-PCR and (B) infectious virus via plaque assays. Recombinant viruses are grouped by the general location of their SNVs. Experiment was performed in biological triplicate (mean ± 95% confidence intervals). Two-way ANOVA with Dunnett’s multiple comparison was performed comparing each recombinant virus to WT at each time point. Only statistically significant relationships are shown (*, P < 0.05; **, P < 0.01; ***, P < 0.005).
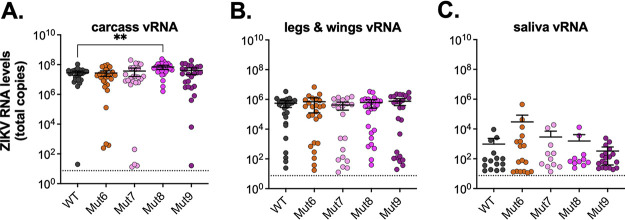
We next sought to determine whether the increased Aag2 replication was general cell-culture adaptation, or adaptation to Aedes cells. We infected Ae. aegypti mosquitoes with four of the recombinant viruses (Mut 6–9) that had the highest replication in Aag2 cells (Fig. 6A and B) and compared that to WT ZIKV infection. At day 7 postinfection, mosquitoes were salivated and dissected to determine infection, dissemination, and transmission rates (Table 5). We saw similar infection rates across all viruses; however, dissemination and transmission rates were significantly decreased in some of the mutants relative to WT ZIKV (Fig. 6C). When comparing levels of viral RNA (vRNA) measured by qRT-PCR in each of these samples (carcass, legs and wings, and saliva) we saw similar levels of vRNA across viruses; however, Mut8 had significantly (P < 0.005) more vRNA compared to WT in the carcass only (Fig. 7A to C).
TABLE 5.
Vector competence of Ae. aegypti mosquitoes with ZIKV recombinant virusesa
| Tissue | WT | Mut6 | Mut7 | Mut8 | Mut9 |
|---|---|---|---|---|---|
| Carcass | 26/30 (87%) | 25/30 (83%) | 24/30 (80%) | 27/30 (90%) | 23/30 (77%) |
| Legs and wings | 24/30 (80%) | 18/30 (60%) | 13/30 (43%)c | 18/30 (60%) | 16/30 (53%)b |
| Saliva | 7/30 (23%) | 6/30 (20%) | 3/30 (10%) | 2/30 (7%) | 0/30 (0%)c |
ZIKV infection was determined by standard plaque assay on Vero cells. Significant differences between Mut6-9 compared to WT for each tissue type using a Chi-square test are shown.
P < 0.05.
P < 0.005.
FIG 7.
ZIKV recombinant viruses in Ae. aegypti mosquitoes. Ae. aegypti mosquitoes were infected with ZIKV recombinant viruses, and at day 7 salivated, dissected, and (A) carcass, (B) legs and wings, and (C) saliva were collected. Levels of viral RNA in mosquito tissues and saliva were quantified by qRT-PCR (mean ± 95% confidence intervals). Dashed line represents the limit of detection. Infection was performed in groups of 30 mosquitoes, only samples with detectable levels of virus are shown. One-way ANOVA with Dunnett’s multiple comparison was performed comparing each recombinant virus to WT. Only statistically significant relationships are shown (**, P < 0.005). Dashed line represents limit of detection.
DISCUSSION
In the present study, we attempted to adapt ZIKV to Cx. tarsalis cells to identify viral determinants of species specificity and blocks to efficient Culex infection and transmission. We found that in serial passaging of ZIKV on a mixed culture of Ae. aegypti and Cx. tarsalis cells with ever increasing proportions of Cx. tarsalis cells, the virus acquired numerous genetic changes at a consensus and minority level. When SNVs of interest were introduced into a ZIKV infectious clone, individually and in combination, we found that none resulted in increased infection of Culex cells or mosquitoes. Conversely, some of the mutations appeared to result in increased infection of Aag2 cells, but no increase in the infection, dissemination, or transmission of Ae. aegypti mosquitoes, suggesting overall adaptation to these cells and cell culture more generally.
Serial passage of viruses to adapt to cells, receptors, escape antibodies, etc. is a common technique used to identify viral genetic determinants. Serial passaging of ZIKV on Culex cells would be impossible due to the extremely low viral titers produced by Culex cells (Fig. 1). Coculturing two different cell types is less commonly used because it requires the cells to use the same, or compatible growth conditions (media type, temperature, etc.); however, the technique is becoming more common, especially within the fields of synthetic biology, drug development, and developmental biology (29, 30). Coculturing cells in the context of infection is occasionally described (31–33), but rarely with the goal of adapting a virus from a more permissive cell line to a less permissive one. We designed our approach loosely based on Morley et al. (25) which serially passaged SINV on a coculture of BHK-21 (highly permissive) and CHO (poorly permissive) cells. The technique of passaging virus on cells generally relies on the virus having some baseline infection in the cells of interest. We hypothesized that constant exposure of CT cells with ZIKV generated by Aag2 cells would ultimately allow for virus adaptation and increased replication in CT cells. However, in our experiments, the low level ZIKV replication in CT cells was likely not sufficient to allow adaptation and selection for improved infection in those cells. Since we observed the highest levels of prolonged replication with ZIKV strain 41525 in vivo, future strategies to evaluate Culex-adaptive SNVs may include passaging of ZIKV 41525 via microinjections in vivo. Additionally, it is possible that under different conditions of cell and mosquito infection (temperature, humidity, length of infection, etc.) that we would see higher permissiveness to infection.
Interestingly, a subset of the variants that emerged during coculture passaging (as CT cell ratios increased) resulted in improved viral replication in Aag2 cells; however, there was no increase in infection, dissemination, transmission rates in Ae. aegypti mosquitoes. These results reveal that while the virus adapted to mosquito cells in culture, the variants were likely more associated with tissue culture adaptation broadly, similar to what has been seen in other studies (34). Of note, Mut2 and Mut3 result in a loss of N-glycosylation at position 154 in E, without impact on virus titers or plaque formation in Vero cells and slightly increased replication in Aag2 cells. While N-glycosylation of E is important for flavivirus attachment to host cell receptors and viral release, as reviewed by Carbaugh and Lazear (35), a ZIKV N154Q mutant was previously shown to increase infectivity in C6/36 cells but reduce infection in vivo in mosquitoes and mice (36). We found no previous reports of the K590Q mutation in the helicase domain of NS3 (Mut7), which increased ZIKV replication in Aag2. However, since no significant increase in infectivity was observed in vivo, no follow-up studies were performed. It is currently still unclear whether the block to ZIKV infection observed in most Culex mosquitoes is efficient virus entry, lacking replication host factors, inability to evade immune responses, or virus maturation/egress. It is likely a combination of factors that overall suppress ZIKV replication in Culex cells to such an extent that adaptation is not possible in this type of a passaging set-up.
Importantly, our results reveal the challenge of arboviruses overcoming mosquito species barriers. In many examples with other arboviruses (WNV, CHIKV, MAYV, etc.), the viruses acquired genetic changes that improved viral infection or replication within an already competent mosquito species (20–24) but did not allow it to replicate in a previously noncompetent species. Aedes and Culex mosquitoes are genetically quite different (37), so ZIKV (and other Aedes-specific arboviruses) likely needs to acquire multiple genetic changes (likely in addition to other complex environmental factors) to allow the virus to gain the ability to infect Culex mosquitoes or other new species (38–40).
The 2015 to 2016 ZIKV outbreak was unprecedented, resulting in an estimated ~1 million human infections in the Americas alone, which is likely still a vast underreporting (41). As the virus spread across the globe between mosquitoes and humans from 2013 to 2017, it acquired many genetic changes, with some of these mutations becoming fixed in the American lineage viruses (prM-17, NS1-188, etc.) (42, 43). While the roles of these mutations are not fully elucidated, none have been shown to improve infection in Culex cells or mosquitoes. It is still possible that ZIKV could naturally acquire mutations and subpopulations of Culex-infecting viruses may exist in nature. It is also possible that complex environmental factors such as the mosquito microbiome or the presence of other Culex-borne pathogens (e.g., filarial worms) may influence ZIKV transmission in natural settings. However, it is unlikely that these mosquitoes are playing a major role in ZIKV transmission.
MATERIALS AND METHODS
Cells and viruses.
African green monkey-derived Vero cells were maintained in DMEM (Corning, number 10-017-CV) supplemented with 5% fetal bovine serum (FBS) at 37°C and 5% CO2. Ae. aegypti-derived Aag2 cells (44), and Cx. tarsalis-derived CT cells (45) were maintained in Schneider's media (Gibco, number 21720-024) supplemented with 7% FBS at 28°C. All media were further supplemented with 10 units/mL penicillin, 10 μg/mL streptomycin, and 2.5 μg/mL amphotericin B.
ZIKV strains PRVABC59 (Accession number KU501215) and MR766 (Accession number AY632535) were obtained from the CDC (Fort Collins Branch), while ZIKV strain 41525 (Accession number KU955591) was obtained from the University of Texas Medical Branch. These strains represent the American/Asian line (ZIKV PRVABC59), the East African line (MR766) and the West African line (41525). Passage histories have been previously described in detail (46). All wild-type/isolates of ZIKV were propagated in Vero cells by infection of a single flask of cells per virus at an MOI of 0.01, clarified by centrifugation, aliquoted, and stored at –80°C. ZIKV PRVABC59 infectious clones (wild-type and mutants) were propagated on Vero cells as previously described (28).
Virus passaging.
Aag2 and CT cells were plated 1 day prior to infection at the noted proportions (from 90:10 to 10:90). For the initial infection, cells were infected with WT ZIKV PRVABC59 at a multiplicity of infection of 1 in three independent replicates. Virus was passaged on each proportion two consecutive passages (e.g., 90:10 two times, 80:20 two times, etc.) to allow the virus time to gradually adjust to the higher proportion of CT cells. The final passage contained 10% Aag2 cells and 90% CT cells due to concerns that we see a drastic drop of infectious virus titer in a 100% CT cells culture. Six days after infection, 500 μL of supernatant was transferred to the next passage of cells (for each replicate) while another 500 μL of supernatant were clarified by centrifugation and frozen at –80°C. This process was repeated for 18 passages total. The final cocultured virus was then passaged once on Vero cells to generate a working stock which was used for all experiments (denoted Co.18.1V, Co.18.2V and Co.18.3V).
Growth curves.
CT or Aag2 cells were seeded one or 2 days prior to infection to be ~80% confluent at the time of infection. In biological triplicate for each virus, cells were infected for 1 h at 28°C, inoculum removed, cells washed twice with media, before fresh medium was added. Each day, 100 μL of supernatant (10% of volume) was sampled, immediately frozen at –80°C, and replaced with fresh media. Viral genomic RNA copies were determined as described below and viral titers were measured using standard plaque assay on Vero cells.
qRT-PCR and plaque assays.
Viral RNA was isolated using Mag-Bind Viral DNA/RNA 96 kit (Omega Bio-tek) on a KingFisher Flex Magnetic Particle Processor (Thermo Fisher Scientific). qRT-PCR was performed using EXPRESS qPCR Supermix and Enzyme (Invitrogen), with previously published primers and probes (47) and an RNA-based ZIKV standard curve (48). For plaque assays, Vero cells were seeded 1 day prior to infection. Virus samples were serially diluted in DMEM supplemented with 1 to 2% FBS, added to Vero cell monolayer, and incubated for 1 h at 37°C. Cells were overlaid with 0.6% tragacanth media, incubated for 4 days, then fixed and stained with 20% ethanol and 0.1% crystal violet (Fisher Chemical, C481-100) in water. Plaques were counted manually.
Mosquitoes.
Laboratory colonies of Ae. aegypti (established from wild populations collected in Poza Rica, Mexico in 2012), Cx. quinquefasciatus (established from wild populations collected in 1988 in Sebring County, Florida), Cx. tarsalis (established from a colony maintained by WK Reisen collected in 1953 from California), and Cx. pipiens (established from egg rafts collected in 2002 in Pennsylvania), were maintained at 28°C (Ae. aegypti) or 26 to 27°C (Culex spp.) with a 12:12 light:dark cycle (Ae. aegypti) or 16:8 light:dark cycle (Culex spp.) and 70%–80% relative humidity, with water and sugar provided ad libitum. Larvae were raised on powdered fish food (TetraMin, Tropic Flakes).
Mosquito infections.
In a BSL-3/ACL-3 insectary, a single carton (per each virus) of female mosquitoes at 5 to 7 days post-eclosion were fed an infectious bloodmeal containing equal parts defibrinated calf blood (Colorado Serum Company, number 31033) and virus stock (~3–6 × 106 PFU/mL final concentration). Bloodmeals were added to water-jacketed glass feeders sealed with a layer of hog’s gut and heated to 37°C via a water bath. Mosquitoes were allowed to feed for approximately 1 h, then anesthetized at 4°C and sorted for engorged females. Culex mosquitoes exposed to ZIKV by bloodmeal were held for 7 days and whole bodies were placed into microcentrifuge tubes containing mosquito diluent (PBS, 20% FBS, 50 μg/mL penicillin/streptomycin, 50 μg/mL gentamicin, and 2.5 μg/mL amphotericin B) and a steel bead, then homogenized. For intrathoracic microinjections, 5 to 7 day old mosquitoes were anesthetized at 4°C and held on ice. Female mosquitoes were intrathoracically injected with 138 nL of virus (4140 PFU/mosquito) using a Nanoject II microinjector and placed into a humid cage. Following blood meal or injection, mosquitoes (~30–60 per virus and infection condition, actual number is noted in tables) were held for 7 days with water and sugar provided ad libitum in a single carton per virus. Mosquitoes were cold-anesthetized, legs and wings removed, salivated into capillary tubes containing immersion oil (Cargille, type B high-viscosity) for 30 min, then carcasses were collected. Carcasses, and legs and wings were placed in tubes containing mosquito diluent, and a steel bead, then homogenized. Capillary tubes containing saliva were placed in tubes containing mosquito diluent, and centrifuged at 15,000 × g for 5 min at 4°C. For select experiments, complete mosquitoes were collected to only test infection rates. These mosquito bodies were treated in an identical fashion to carcasses, and legs and wings. All samples were stored at −80°C until sample processing. Detailed metadata for all mosquito infection experiments is provided in Table S1.
Metadata of mosquito virus experiments. Download Table S1, XLSX file, 0.02 MB (22.7KB, xlsx) .
Copyright © 2023 Gallichotte et al.
This content is distributed under the terms of the Creative Commons Attribution 4.0 International license.
Next-generation-sequencing (NGS).
Sequencing libraries were generated with an in-house optimized protocol for total viral RNA sequencing using Nextera XT (Illumina). Viral RNA was reverse transcribed into cDNA using SuperScript IV (Invitrogen) and random pentadecamers. RNA was then digested using RNaseH (New England Biolabs, number M02976), denatured, and random pentadecamers were annealed. NEBNext Ultra II Q5 Master Mix was added and samples incubated for 10 min at 72°C to complete second strand-synthesis. Ampure XP beads were used for DNA purification and Nextera XT (Illumina) was used for tagmentation (fragmentation and adapter addition) according to the manufacturer’s protocol. Libraries were amplified with indexing primers for 12 cycles using the NEBNext Ultra II Q5 Master Mix, size selected using Ampure XP beads, and real-time amplified using the KAPA HiFi HotStart Real-Time Library Amp kit (Roche). Library QC was performed, libraries were pooled at equimolar ratios, and sequenced on an Illumina NextSeq 500.
Data analysis.
All NGS data were analyzed using a previously described workflow (49); this workflow was generated using Snakemake (50) and the workflow and related documentation can be found at https://bitbucket.org/murrieta/snakemake/src. Briefly, Read 1 and Read 2.fastq files from paired-end Illumina NextSeq 500 data were trimmed for Illumina adaptors and quality of phred scores < 30 from the 3′ and 5′ read ends using Cutadapt (51). Reads were then mapped to the ZIKV-PRVABC59 reference sequence (GenBank number KU501215) using MOSAIK (52). We used Picard (https://broadinstitute.github.io/picard/), Genome Analysis Toolkit (GATK) (53), and SAMtools (54) for variant calling preprocessing. To identify SNV’s as well as any inserts and deletions (indelS) we used LoFreq (55) with a cutoff of 1% variant frequency. Consensus sequences were generated using VCFtools (56).
Cloning of recombinant viruses.
Recombinant ZIKVs containing SNVs of interest were introduced into our two-plasmid infectious ZIKV clone (28) using site-directed mutagenesis, Gibson assembly, and standard plasmid preparation. All recombinant viruses were confirmed by Sanger sequencing and virus was propagated from wild-type and mutant clones as previously described (28). Recombinant and wild-type viruses were passaged once on Vero cells to generate a working stock which was used in all experiments.
Statistics.
Chi-square was used to compare infection rates across mosquito species, virus strains, infection types, and tissue samples. One-way and two-way ANOVAs with Dunnett’s multiple-comparison tests were used when comparing mutant virus levels to WT ZIKV. Details of specific statistical tests are noted in figure legends.
Data availability.
All sequencing data are available through the NCBI SRA database (BioProject PRJNA933633).
ACKNOWLEDGMENTS
We acknowledge the Arbovirus Reference Collection of the Centers for Disease Control and Prevention and the World Reference Center for Emerging Viruses and Arboviruses (UTMB) for providing ZIKV strains used in this study. This work was supported by grants from the National Institute of Allergy and Infectious Diseases, National Institutes of Health under grant numbers AI067380 and AI125996. A.D.B. was supported by the National Institutes of Health T32 training grant T32OD010437. R.A.M. was supported by the National Institutes of Health AI134108. We thank Barbara Graham for assistance with statistical analyses. Graphics in Figure 2A were generated using BioRender.com under publication license VW24BW9NT5.
Contributor Information
Claudia Rückert, Email: crueckert@unr.edu.
Shirit Einav, Stanford University School of Medicine.
REFERENCES
- 1.Dick GW, Kitchen SF, Haddow AJ. 1952. Zika virus. I. Isolations and serological specificity. Trans R Soc Trop Med Hyg 46:509–520. doi: 10.1016/0035-9203(52)90042-4. [DOI] [PubMed] [Google Scholar]
- 2.Duffy MR, Chen TH, Hancock WT, Powers AM, Kool JL, Lanciotti RS, Pretrick M, Marfel M, Holzbauer S, Dubray C, Guillaumot L, Griggs A, Bel M, Lambert AJ, Laven J, Kosoy O, Panella A, Biggerstaff BJ, Fischer M, Hayes EB. 2009. Zika virus outbreak on Yap Island, Federated States of Micronesia. N Engl J Med 360:2536–2543. doi: 10.1056/NEJMoa0805715. [DOI] [PubMed] [Google Scholar]
- 3.Faye O, Freire CC, Iamarino A, Faye O, de Oliveira JV, Diallo M, Zanotto PM, Sall AA. 2014. Molecular evolution of Zika virus during its emergence in the 20th century. PLoS Negl Trop Dis 8:e2636. doi: 10.1371/journal.pntd.0002636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Cao-Lormeau VM, Roche C, Teissier A, Robin E, Berry AL, Mallet HP, Sall AA, Musso D. 2014. Zika virus, French Polynesia, South Pacific, 2013. Emerg Infect Dis 20:1085–1086. doi: 10.3201/eid2006.140138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Petersen LR, Jamieson DJ, Powers AM, Honein MA. 2016. Zika Virus. N Engl J Med 374:1552–1563. doi: 10.1056/NEJMra1602113. [DOI] [PubMed] [Google Scholar]
- 6.Massad E, Burattini MN, Khan K, Struchiner CJ, Coutinho FAB, Wilder-Smith A. 2017. On the origin and timing of Zika virus introduction in Brazil. Epidemiol Infect 145:2303–2312. doi: 10.1017/S0950268817001200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Boyer S, Calvez E, Chouin-Carneiro T, Diallo D, Failloux AB. 2018. An overview of mosquito vectors of Zika virus. Microbes Infect 20:646–660. doi: 10.1016/j.micinf.2018.01.006. [DOI] [PubMed] [Google Scholar]
- 8.Richard V, Paoaafaite T, Cao-Lormeau VM. 2016. Vector competence of French Polynesian Aedes aegypti and Aedes polynesiensis for Zika virus. PLoS Negl Trop Dis 10:e0005024. doi: 10.1371/journal.pntd.0005024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.van den Hurk AF, Hall-Mendelin S, Jansen CC, Higgs S. 2017. Zika virus and Culex quinquefasciatus mosquitoes: a tenuous link. Lancet Infect Dis 17:1014–1016. doi: 10.1016/S1473-3099(17)30518-2. [DOI] [PubMed] [Google Scholar]
- 10.Correa-Morales F, Gonzalez-Acosta C, Mejia-Zuniga D, Huerta H, Perez-Renteria C, Vazquez-Pichardo M, Ortega-Morales AI, Hernandez-Triana LM, Salazar-Bueyes VM, Moreno-Garcia M. 2019. Surveillance for Zika in Mexico: naturally infected mosquitoes in urban and semi-urban areas. Pathog Glob Health 113:309–314. doi: 10.1080/20477724.2019.1706291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Elizondo-Quiroga D, Medina-Sanchez A, Sanchez-Gonzalez JM, Eckert KA, Villalobos-Sanchez E, Navarro-Zuniga AR, Sanchez-Tejeda G, Correa-Morales F, Gonzalez-Acosta C, Arias CF, Lopez S, Del Angel RM, Pando-Robles V, Elizondo-Quiroga AE. 2018. Zika virus in salivary glands of five different species of wild-caught mosquitoes from Mexico. Sci Rep 8:809. doi: 10.1038/s41598-017-18682-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Guedes DR, Paiva MH, Donato MM, Barbosa PP, Krokovsky L, Rocha S, Saraiva K, Crespo MM, Rezende TM, Wallau GL, Barbosa RM, Oliveira CM, Melo-Santos MA, Pena L, Cordeiro MT, Franca RFO, Oliveira AL, Peixoto CA, Leal WS, Ayres CF. 2017. Zika virus replication in the mosquito Culex quinquefasciatus in Brazil. Emerg Microbes Infect 6:e69. doi: 10.1038/emi.2017.59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Guo XX, Li CX, Deng YQ, Xing D, Liu QM, Wu Q, Sun AJ, Dong YD, Cao WC, Qin CF, Zhao TY. 2016. Culex pipiens quinquefasciatus: a potential vector to transmit Zika virus. Emerg Microbes Infect 5:e102. doi: 10.1038/emi.2016.102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hery L, Boullis A, Delannay C, Vega-Rua A. 2019. Transmission potential of African, Asian and American Zika virus strains by Aedes aegypti and Culex quinquefasciatus from Guadeloupe (French West Indies). Emerg Microbes Infect 8:699–706. doi: 10.1080/22221751.2019.1615849. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lourenco-de-Oliveira R, Marques JT, Sreenu VB, Atyame Nten C, Aguiar E, Varjak M, Kohl A, Failloux AB. 2018. Culex quinquefasciatus mosquitoes do not support replication of Zika virus. J Gen Virol 99:258–264. doi: 10.1099/jgv.0.000949. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.MacLeod HJ, Dimopoulos G. 2020. Detailed analyses of Zika virus tropism in Culex quinquefasciatus reveal systemic refractoriness. mBio 11. doi: 10.1128/mBio.01765-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Smartt CT, Shin D, Kang S, Tabachnick WJ. 2018. Culex quinquefasciatus (Diptera: culicidae) from Florida transmitted Zika virus. Front Microbiol 9:768. doi: 10.3389/fmicb.2018.00768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Elizondo-Quiroga D, Ramirez-Medina M, Gutierrez-Ortega A, Elizondo-Quiroga A, Munoz-Medina JE, Sanchez-Tejeda G, Gonzalez-Acosta C, Correa-Morales F. 2019. Vector competence of Aedes aegypti and Culex quinquefasciatus from the metropolitan area of Guadalajara, Jalisco, Mexico for Zika virus. Sci Rep 9:16955. doi: 10.1038/s41598-019-53117-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Viveiros-Rosa SG, Regis EG, Santos WC. 2020. Vector competence of Culex mosquitoes (Diptera: Culicidae) in Zika virus transmission: an integrative review. Rev Panam Salud Publica 44:e7. doi: 10.26633/RPSP.2020.7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Tsetsarkin KA, Vanlandingham DL, McGee CE, Higgs S. 2007. A single mutation in chikungunya virus affects vector specificity and epidemic potential. PLoS Pathog 3:e201. doi: 10.1371/journal.ppat.0030201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Davis CT, Ebel GD, Lanciotti RS, Brault AC, Guzman H, Siirin M, Lambert A, Parsons RE, Beasley DW, Novak RJ, Elizondo-Quiroga D, Green EN, Young DS, Stark LM, Drebot MA, Artsob H, Tesh RB, Kramer LD, Barrett AD. 2005. Phylogenetic analysis of North American West Nile virus isolates, 2001–2004: evidence for the emergence of a dominant genotype. Virology 342:252–265. doi: 10.1016/j.virol.2005.07.022. [DOI] [PubMed] [Google Scholar]
- 22.Ebel GD, Carricaburu J, Young D, Bernard KA, Kramer LD. 2004. Genetic and phenotypic variation of West Nile virus in New York, 2000–2003. Am J Trop Med Hyg 71:493–500. doi: 10.4269/ajtmh.2004.71.493. [DOI] [PubMed] [Google Scholar]
- 23.Moudy RM, Meola MA, Morin LL, Ebel GD, Kramer LD. 2007. A newly emergent genotype of West Nile virus is transmitted earlier and more efficiently by Culex mosquitoes. Am J Trop Med Hyg 77:365–370. doi: 10.4269/ajtmh.2007.77.365. [DOI] [PubMed] [Google Scholar]
- 24.Roesch F, Cereghino C, Carrau L, Hardy A, Ribeiro-Filho H, Lacritick AH, Koh C, Marano J, Bates T, Rai P, Chuong C, Akter S, Vallet T, Blanc H, Elliot T, Brown AM, Michalak P, LeRoith T, Bloom J, Marques RE, Saleh M-C, Vignuzzi M, Weger-Lucarelli J. 2022. The E2 glycoprotein holds key residues for Mayaro virus adaptation to the urban Aedes aegypti mosquito. bioRxiv. doi: 10.1101/2022.04.05.487100. [DOI] [PMC free article] [PubMed]
- 25.Morley VJ, Mendiola SY, Turner PE. 2015. Rate of novel host invasion affects adaptability of evolving RNA virus lineages. Proc Biol Sci 282:20150801. doi: 10.1098/rspb.2015.0801. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kenney JL, Romo H, Duggal NK, Tzeng WP, Burkhalter KL, Brault AC, Savage HM. 2017. Transmission incompetence of Culex quinquefasciatus and Culex pipiens from North America for Zika Virus. Am J Trop Med Hyg 96:1235–1240. doi: 10.4269/ajtmh.16-0865. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Main BJ, Nicholson J, Winokur OC, Steiner C, Riemersma KK, Stuart J, Takeshita R, Krasnec M, Barker CM, Coffey LL. 2018. Vector competence of Aedes aegypti, Culex tarsalis, and Culex quinquefasciatus from California for Zika virus. PLoS Negl Trop Dis 12:e0006524. doi: 10.1371/journal.pntd.0006524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Weger-Lucarelli J, Duggal NK, Bullard-Feibelman K, Veselinovic M, Romo H, Nguyen C, Ruckert C, Brault AC, Bowen RA, Stenglein M, Geiss BJ, Ebel GD. 2017. Development and characterization of recombinant virus generated from a New World Zika virus infectious clone. J Virol 91. doi: 10.1128/JVI.00172-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Goers L, Freemont P, Polizzi KM. 2014. Co-culture systems and technologies: taking synthetic biology to the next level. J R Soc Interface 11. doi: 10.1098/rsif.2014.0065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Luo Y, Sun GB, Qin M, Yao F, Sun XB. 2012. [Application of cell co-culture techniques in medical studies]. Zhongguo Zhong Yao Za Zhi 37:3345–3349. [PubMed] [Google Scholar]
- 31.Han B, Mo H, Svarovskaia E, Mateo R. 2021. A primary human hepatocyte/hepatic stellate cell co-culture system for improved in vitro HBV replication. Virology 559:40–45. doi: 10.1016/j.virol.2021.03.012. [DOI] [PubMed] [Google Scholar]
- 32.Loh L, Koutsakos M, Kedzierska K, Hinks TSC. 2020. Influenza A virus-infected lung epithelial cell co-culture with human peripheral blood mononuclear cells. Methods Mol Biol 2098:141–147. doi: 10.1007/978-1-0716-0207-2_9. [DOI] [PubMed] [Google Scholar]
- 33.Parreno R, Torres S, Almagro L, Bello-Perez M, Estepa A, Perez L. 2016. Induction of viral interference by IPNV-carrier cells on target cells: a cell co-culture study. Fish Shellfish Immunol 58:483–489. doi: 10.1016/j.fsi.2016.09.052. [DOI] [PubMed] [Google Scholar]
- 34.Talavera-Aguilar LG, Murrieta RA, Kiem S, Cetina-Trejo RC, Baak-Baak CM, Ebel GD, Blitvich BJ, Machain-Williams C. 2021. Infection, dissemination, and transmission efficiencies of Zika virus in Aedes aegypti after serial passage in mosquito or mammalian cell lines or alternating passage in both cell types. Parasit Vectors 14:261. doi: 10.1186/s13071-021-04726-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Carbaugh DL, Lazear HM. 2020. Flavivirus envelope protein glycosylation: impacts on viral infection and pathogenesis. J Virol 94. doi: 10.1128/JVI.00104-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Fontes-Garfias CR, Shan C, Luo H, Muruato AE, Medeiros DBA, Mays E, Xie X, Zou J, Roundy CM, Wakamiya M, Rossi SL, Wang T, Weaver SC, Shi PY. 2017. Functional analysis of glycosylation of Zika virus envelope protein. Cell Rep 21:1180–1190. doi: 10.1016/j.celrep.2017.10.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Lorenz C, Alves JMP, Foster PG, Suesdek L, Sallum MAM. 2021. Phylogeny and temporal diversification of mosquitoes (Diptera: Culicidae) with an emphasis on the neotropical fauna. Systematic Entomology 46:798–811. doi: 10.1111/syen.12489. [DOI] [Google Scholar]
- 38.Viglietta M, Bellone R, Blisnick AA, Failloux AB. 2021. Vector specificity of arbovirus transmission. Front Microbiol 12:773211. doi: 10.3389/fmicb.2021.773211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Huang YS, Higgs S, Vanlandingham DL. 2019. Arbovirus-mosquito vector-host interactions and the impact on transmission and disease pathogenesis of arboviruses. Front Microbiol 10:22. doi: 10.3389/fmicb.2019.00022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Schulz C, Becker SC. 2018. Mosquitoes as arbovirus vectors: from species identification to vector competence. Mosquito-Borne Diseases: Implications for Public Health 10:163–212. doi: 10.1007/978-3-319-94075-5_9. [DOI] [Google Scholar]
- 41.Ikejezie J, Shapiro CN, Kim J, Chiu M, Almiron M, Ugarte C, Espinal MA, Aldighieri S. 2017. Zika Virus Transmission-Region of the Americas, May 15, 2015-December 15, 2016. MMWR Morb Mortal Wkly Rep 66:329–334. doi: 10.15585/mmwr.mm6612a4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Gutierrez-Bugallo G, Piedra LA, Rodriguez M, Bisset JA, Lourenco-de-Oliveira R, Weaver SC, Vasilakis N, Vega-Rua A. 2019. Vector-borne transmission and evolution of Zika virus. Nat Ecol Evol 3:561–569. doi: 10.1038/s41559-019-0836-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Wang L, Valderramos SG, Wu A, Ouyang S, Li C, Brasil P, Bonaldo M, Coates T, Nielsen-Saines K, Jiang T, Aliyari R, Cheng G. 2016. From mosquitos to humans: genetic evolution of Zika virus. Cell Host Microbe 19:561–565. doi: 10.1016/j.chom.2016.04.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Peleg J. 1968. Growth of arboviruses in monolayers from subcultured mosquito embryo cells. Virology 35:617–619. doi: 10.1016/0042-6822(68)90293-6. [DOI] [PubMed] [Google Scholar]
- 45.Chao J, Ball GH. 1976. A comparison of amino acid utilization by cell lines of Culex tarsalis and Culex pipiens. Invertebrate Tissue Culture: applications in Medicine, Biology, and Agriculture, p 263–266. [Google Scholar]
- 46.Weger-Lucarelli J, Rückert C, Chotiwan N, Nguyen C, Garcia Luna SM, Fauver JR, Foy BD, Perera R, Black WC, Kading RC, Ebel GD. 2016. Vector competence of American mosquitoes for three strains of Zika virus. PLoS Negl Trop Dis 10:e0005101. doi: 10.1371/journal.pntd.0005101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Lanciotti RS, Kosoy OL, Laven JJ, Velez JO, Lambert AJ, Johnson AJ, Stanfield SM, Duffy MR. 2008. Genetic and serologic properties of Zika virus associated with an epidemic, Yap State, Micronesia, 2007. Emerg Infect Dis 14:1232–1239. doi: 10.3201/eid1408.080287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Rückert C, Weger-Lucarelli J, Garcia-Luna SM, Young MC, Byas AD, Murrieta RA, Fauver JR, Ebel GD. 2017. Impact of simultaneous exposure to arboviruses on infection and transmission by Aedes aegypti mosquitoes. Nat Commun 8:15412. doi: 10.1038/ncomms15412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Murrieta RA, Garcia-Luna SM, Murrieta DJ, Halladay G, Young MC, Fauver JR, Gendernalik A, Weger-Lucarelli J, Rückert C, Ebel GD. 2021. Impact of extrinsic incubation temperature on natural selection during Zika virus infection of Aedes aegypti and Aedes albopictus. PLoS Pathog 17:e1009433. doi: 10.1371/journal.ppat.1009433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Koster J, Rahmann S. 2018. Snakemake-a scalable bioinformatics workflow engine. Bioinformatics 34:3600. doi: 10.1093/bioinformatics/bty350. [DOI] [PubMed] [Google Scholar]
- 51.Martin M. 2011. Cutadapt removes adapter sequences from high-throughput sequencing reads. EMBnet j.17:10. [Google Scholar]
- 52.Lee WP, Stromberg MP, Ward A, Stewart C, Garrison EP, Marth GT. 2014. MOSAIK: a hash-based algorithm for accurate next-generation sequencing short-read mapping. PLoS One 9:e90581. doi: 10.1371/journal.pone.0090581. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Van der Auwera GA, Carneiro MO, Hartl C, Poplin R, Del Angel G, Levy-Moonshine A, Jordan T, Shakir K, Roazen D, Thibault J, Banks E, Garimella KV, Altshuler D, Gabriel S, DePristo MA. 2013. From FastQ data to high confidence variant calls: the Genome Analysis Toolkit best practices pipeline. Curr Protoc Bioinformatics 43:11.10.1–11.10.33. doi: 10.1002/0471250953.bi1110s43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Li H, Handsaker B, Wysoker A, Fennell T, Ruan J, Homer N, Marth G, Abecasis G, Durbin R, Genome Project Data Processing S. 1000 Genome Project Data Processing Subgroup. 2009. The Sequence Alignment/Map format and SAMtools. Bioinformatics 25:2078–2079. doi: 10.1093/bioinformatics/btp352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Wilm A, Aw PP, Bertrand D, Yeo GH, Ong SH, Wong CH, Khor CC, Petric R, Hibberd ML, Nagarajan N. 2012. LoFreq: a sequence-quality aware, ultra-sensitive variant caller for uncovering cell-population heterogeneity from high-throughput sequencing datasets. Nucleic Acids Res 40:11189–11201. doi: 10.1093/nar/gks918. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Danecek P, Auton A, Abecasis G, Albers CA, Banks E, DePristo MA, Handsaker RE, Lunter G, Marth GT, Sherry ST, McVean G, Durbin R, 1000 Genomes Project Analysis Group. 2011. The variant call format and VCFtools. Bioinformatics 27:2156–2158. doi: 10.1093/bioinformatics/btr330. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Metadata of mosquito virus experiments. Download Table S1, XLSX file, 0.02 MB (22.7KB, xlsx) .
Copyright © 2023 Gallichotte et al.
This content is distributed under the terms of the Creative Commons Attribution 4.0 International license.
Data Availability Statement
All sequencing data are available through the NCBI SRA database (BioProject PRJNA933633).