Abstract
We compared the prevalence of reporting difficulty with basic and instrumental activities of daily living without help received for persons with cognitive impairment living alone versus those living with others. We used data on 13,782 community-dwelling participants aged 55+ with cognitive impairment in the Health and Retirement Study (2000–2016). Models were stratified by gender and race/ethnicity. Among cognitively impaired older adults, those living alone were more likely to report difficulty without help received than those living with others. Results were similar by gender and race/ethnicity. Providers and policymakers might focus their efforts on ensuring the adequate provision of home and community-based services for older adults living alone with cognitive impairment.
Keywords: Aging in place, cognitive impairment, disability, living arrangement, racial/ethnic disparity
INTRODUCTION
It is estimated that cognitive impairment (CI) affects 16 million individuals in the United States (US) [1]. Community-dwelling older adults with CI generally need more support from their caregivers than those with other chronic conditions [2]. Furthermore, most support provided to people with CI comes from cohabiting unpaid caregivers (e.g., family members or friends) [3, 4]. However, an estimated 4.3 million older adults with CI live alone in the US [5].
Living alone in a familiar home environment and community is often preferred to living in a nursing home [6]. However, while some older adults living alone may have better health and/or greater financial security to age in place [7], the vast majority of adults who live alone have fewer financial resources, worse health, and a higher level of unmet needs compared to those living with others [8–12]. Indeed, older adults living alone report difficulty with a greater number of basic activities of daily living (ADLs) and have more unmet caregiving needs than their peers living with others [13–15]. However, to date, many studies have utilized small, regional samples, which poses challenges for generalizability. In addition, to our knowledge, no national studies have evaluated patterns of caregiving receipt for older adults with CI who live alone as compared to those living with others. This is an important gap since disparities in both the need for and receipt of caregiving by living arrangements could be exacerbated among older adults with CI.
In this study, we used population-based data on community-dwelling older adults with CI and evaluated differences by living arrangement in the prevalence of reporting difficulty with any basic or instrumental activities of daily living (I/ADL) without caregiving help received. We hypothesized that among older adults with CI, those who live alone (versus live with others) would have a higher prevalence of reporting I/ADL difficulty without help received from either formal or informal sources of care. We further expected that living arrangement-related disparities in reporting I/ADL difficulty without care received would be greater for racial and ethnic minorities and women. In particular, Black and Latinx subgroups have a higher risk of dementia incidence [16, 17], more functional limitations [18, 19], and limited access to formal healthcare and other services [20] due to long-standing structural inequities. Older women are more likely to live longer alone, while also having fewer financial resources to pay for sufficient non-family caregiving in the absence of co-residing family members who may provide formal or informal care [21].
MATERIALS AND METHODS
Data and analytical sample
We used data from the 2000–2016 biennial waves of the Health and Retirement Study (HRS), a national representative survey of adults aged 50 and over in the US. The sample is replenished every six years with younger cohorts not previously represented. The pooled data were used to improve sample sizes in evaluating racial/ethnic patterns. We restricted our sample to community-dwelling adults aged 55+, excluding those living in institutional settings (e.g., nursing homes). We restricted our sample to the respondents with probable CI or dementia based on an established algorithm based on self-reported cognitive assessment and proxy report of cognition [22, 23]. We further excluded those with missing data with one or more covariates (see Supplementary Figure1). This yielded an analytical sample of 13,782 respondents and 33,540 person-wave observations (each participant on average contributes 2.43 person-wave records).
Measures
I/ADL difficulty without help received
Our primary outcome of interest is self- and proxy-reported difficulty with basic and instrumental activities of daily living (I/ADLs) without help received. Basic activities of daily living (ADLs) were assessed by asking whether respondents reported difficulty with six items: dressing, walking across room, bathing, eating, getting in and out of bed, and toileting. The five instrumental activities of daily living (IADLs) included: preparing a hot meal, shopping for groceries, making phone calls, taking medications, and managing money. Respondents were first asked whether they reported difficulty with each of these 11 tasks. We coded respondents as having difficulty with a specific I/ADL if they answered “yes” or “can’t do,” and coded them as having no difficulty if they answered “no”. Those who answered “don’t do”, “don’t know”, or “refused” were set to missing. We then summed these individual I/ADL measures to create a binary indicator of whether respondents reported difficulty with ≥1 I/ADL versus no difficulties with any I/ADLs.
Respondents who reported difficulty with a specific I/ADL were then asked whether “anyone helps you” with that specific task. We created a binary indicator of whether respondents reported ≥1 I/ADL difficulty without any help received (versus no I/ADL difficulties without help or ≥1 I/ADL difficulty with help).
For ease of interpretation, we report combined I/ADL measures as our primary outcomes below and present ADL- and IADL-specific measures in the Supplementary Material.
Living alone versus living with others
We defined community-dwelling respondents’ living arrangements as those individuals living alone versus living with others. As previously described [22], we used information on the number of residents in the household as reported in the RAND longitudinal File (which was derived by counting the number of people reported in the household roster) and created a dichotomous predictor of living alone (number of residents=1) versus with others (number of residents >1).
Socio-demographic covariates
We considered covariates that would be important predictors of both living arrangement and I/ADL outcomes. These included age (in years), self-reported gender identity (women/men), race/ethnicity (non-Hispanic White, non-Hispanic Black, and Latinx/Hispanic), education (less than high-school, high school diploma/GED, some college, college and above), and current Medicaid coverage (yes/no). Given known socio-demographic inequalities in I/ADL difficulties and differential access to home and community-based services [5, 24, 25], and all models were stratified by gender and race/ethnicity.
Statistical analyses
We first present the demographic characteristics of older adults with CI by respondent gender and living arrangement. We then estimated prevalence ratios that compared the prevalence of I/ADL difficulty overall (in the Supplementary Material) and I/ADL difficulty without help received by living arrangement via generalized estimating equations (GEE) with a Poisson distribution, logit link function, and an unstructured covariance matrix to account for repeated observations of individuals [26]. We show the results of the GEE models first stratified by gender and then further stratified by race/ethnicity. To formally test whether there were racial/ethnic differences in the association between living arrangements and our outcome variables, we also tested a multiplicative interaction term between race/ethnicity and living arrangements. All models were adjusted for socio-demographic covariates and were weighted to account for the complex survey design (individual average weights were calculated by using all available wave-specific weights). Analyses were carried out in R version 4.1.0.
RESULTS
Descriptive statistics
The share of living alone was higher among women than men in our sample. The mean age of living alone persons was 78 for women and 73 for men. Moreover, older men and women living alone were more likely to be enrolled in Medicaid compared to their counterparts living with others (Table 1).
Table 1.
Descriptive characteristics and unadjusted prevalence of I/ADL difficulty and help received for adults aged 55+ with probable dementia or CIND, by gender and living arrangement
| Women | Men | |||
|---|---|---|---|---|
|
|
||||
| Lives alone | Lives with others | Lives alone | Lives with others | |
| Study participants (unweighted) | 6,602 | 12,205 | 2,973 | 11,760 |
| Age, mean (SD) | 78.27 (10.54) | 72.35 (10.78) | 72.52 (11.16) | 71.50 (10.16) |
| Race/Ethnicity | ||||
| Non-Hispanic White | 70.59% | 59.20% | 67.20% | 69.14% |
| Non-Hispanic Black | 18.71% | 21.60% | 24.19% | 16.20% |
| Latinx/Hispanic | 10.70% | 19.19% | 8.61% | 14.66% |
| Education | ||||
| Less than High School | 42.46% | 45.25% | 40.42% | 42.63% |
| High School | 35.57% | 33.50% | 36.10% | 31.92% |
| Some college | 15.48% | 14.58% | 15.30% | 15.34% |
| College | 6.50% | 6.68% | 8.18% | 10.11% |
| Rural/Urban Residence | ||||
| Urban | 42.06% | 45.50% | 43.05% | 41.86% |
| Suburban | 24.24% | 22.85% | 21.76% | 22.68% |
| Rural | 33.70% | 31.66% | 35.18% | 35.46% |
| Medicaid | 22.45% | 20.04% | 20.98% | 12.28% |
| Proxy respondent | 8.75% | 12.08% | 5.42% | 18.80% |
| Cognitive Status | ||||
| CIND | 76.31% | 73.77% | 78.80% | 78.71% |
| Probable Dementia | 23.69% | 26.23% | 21.20% | 21.29% |
| 11-item I/ADLs | ||||
| Any difficulty | 48.04% | 48.03% | 39.27% | 40.52% |
| Any difficulty without help | 33.73% | 28.65% | 30.48% | 23.61% |
| 6-item ADLs | ||||
| Any difficulty | 36.49% | 37.17% | 28.56% | 27.46% |
| Any difficulty without help | 28.39% | 23.64% | 24.78% | 18.43% |
| 5-item IADLs | ||||
| Any difficulty | 36.18% | 38.07% | 27.44% | 31.03% |
| Any difficulty without help | 12.59% | 9.75% | 12.55% | 8.44% |
Underlying data are pooled person-wave observations of respondents in the 2000–2016 waves of the Health and Retirement Study. All statistics are estimated using wave-specific sample weights. CIND, cognitive impaired but no dementia; ADL, basic activities of daily living (6 items including: dressing, walking across room, bathing, eating, getting in and out of bed, and toileting); IADL, instrumental activities of daily living (5 items including: preparing a hot meal, shopping for groceries, making phone calls, taking medications, and managing money); I/ADL, basic and instrumental activities of daily living.
Prevalence ratios: I/ADL difficulty
Among older women, those with CI living alone had a lower prevalence of any I/ADL difficulty compared to those living with others (prevalence ratio [PR]: 0.89, 95% confidence interval [CI]: 0.85, 0.92). Among older men with CI, the prevalence of I/ADL difficulty overall was similar for those living alone versus living with others (PR: 0.92, 95% CI: 0.86, 0.98) (Supplementary Table 1).
Prevalence ratios: I/ADL difficulty without help received
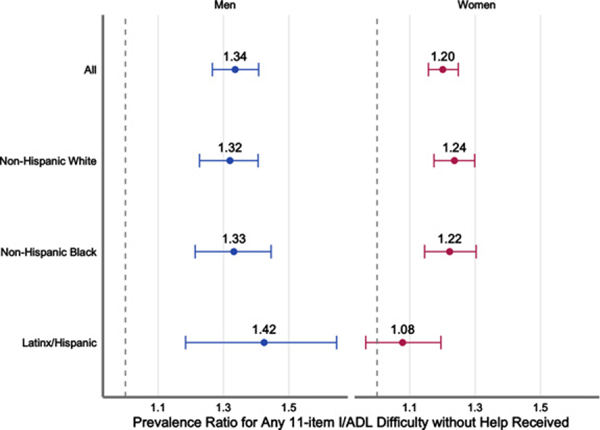
Among older adults with CI, those living alone had a higher prevalence of reporting ≥1 I/ADL difficulty without help received by any source than those living with others (Table 2, Fig. 1). The magnitude of association was larger for men with CI (PR:1.20, 95% CI: 1.09, 1.31) than that for women (PR:1.08, 95% CI:1.01, 1.14), although 95% confidence intervals overlapped. In the models further stratified by race/ethnicity, a relatively larger effect estimate was observed for Latinx men as compared to other groups (PR: 1.34, 95% CI: 0.97, 1.77), although the estimate was imprecise and crossed the null.
Table 2.
Adjusted generalized estimating equation (GEE) models of any 11-item I/ADL difficulty without help among with probable dementia or CIND by gender and race/ethnicity
| Total Obs. (living alone) | Prevalence ratio [95% CI] | ||
|---|---|---|---|
| Model 1 | All Women, living alone (versus with others) | 18,807(6,602) | 1.08 [1.01, 1.14]∗∗ |
| Model 1A | Non-Hispanic White Women, living alone (versus with others) | 9,872(3,996) | 1.06 [0.99, 1.15] |
| Model 1B | Non-Hispanic Black Women, living alone (versus with others) | 5,463(1,773) | 1.07 [0.97, 1.20] |
| Model 1C | Latina/Hispanic Women, living alone (versus with others) | 3,472(833) | 1.06 [0.89, 1.25] |
| Model 2 | All Men, living alone (versus with others) | 14,733(2,973) | 1.20 [1.09, 1.31]∗∗∗ |
| Model 2A | Non-Hispanic White Men, living alone (versus with others) | 8,724(1736) | 1.21 [1.07, 1.34]∗∗∗ |
| Model 2B | Non-Hispanic Black Men, living alone (versus with others) | 3,679(962) | 1.11 [0.94, 1.31] |
| Model 2C | Latinx/Hispanic Men, living alone (versus with others) | 2,330(275) | 1.34 [0.97, 1.77] |
Underlying data are pooled observations of respondents with cognitive impaired not dementia (CIND) or probable dementia observed in the 2000–2016 waves of the Health and Retirement Study. Sample weights are set equal to the respondent’s average weight in the sample. The prevalence ratios and their 95% confidence intervals are presented from a generalized estimating equation (“geeglm”) configured to the Poisson distribution, logit link function, and unstructured within-group correlation. Covariates include age in years, survey wave, educational attainment, urban rural residency, and Medicaid. I/ADL, basic and instrumental activities of daily living (11 items including: dressing, walking across room, bathing, eating, getting in and out of bed, toileting, preparing a hot meal, shopping for groceries, making phone calls, taking medications, and managing money); CIND, Cognitive impairment no dementia (describes individuals whose cognitive functioning falls below normal but who do not meet dementia criteria). Asterisks denote statistical significance at
p < 0.05.
p < 0.01.
p < 0.001.
Fig. 1.
Adjusted Prevalence Ratio for Any 11-Item I/ADL Difficulty without Help Received. Underlying data are pooled observations of respondents with cognitive impaired but not dementia(CIND)orprobabledementiaobservedinthe2000–2016 waves of the Health and Retirement Study. Adjusted prevalence ratios are presented from a generalized estimating equation (“geeglm”) configured to the Poisson distribution, logit link function, and unstructured within-group correlation. I/ADL, basic and instrumental activities of daily living (11 items include: dressing, walking across room, bathing, eating, getting in and out of bed, toileting, preparing a hot meal, shopping for groceries, making phone calls, taking medications, and managing money). Covariates include age in years, survey wave, educational attainment, urban-rural residency, and Medicaid.
In supplemental analysis, we found similar patterns for ADLs and IADLs separately (Supplementary Tables 2 and 3). In analyses restricted to those with ≥1 I/ADL difficulty, results were in the same direction but were generally of greater magnitude than estimates reported in our primary analyses (Supplementary Table 4). We also performed analysis excluding proxy responses, given that 13.5% of person-wave observations were based on proxy reports, and results hold but were with greater magnitude for all groups (Supplementary Table 5). However, we note that these associations may be driven by selection factors, so we urge readers to interpret these findings with caution.
DISCUSSION
In a nationally-representative sample of community-dwelling adults age 55+ in the US, we compared difficulty with activities of daily living without help received for older adults with cognitive impairment (CI) by living arrangement. Among women (but not men), those living alone had a lower prevalence of I/ADL difficulty than those living with others. Nevertheless, the prevalence of I/ADL difficulty without help received by any source of care was 8% higher for women and 20% higher for men with CI living alone compared to their counterparts living with others. Contrary to our hypothesis, we did not observe significant differences in the relationship between living arrangements and I/ADL difficulty by racial and ethnic group. While prior studies have examined the relation between living alone and CI [5, 15, 27], none of those studies have directly considered whether living alone is a risk factor for reporting I/ADL difficulty without caregiving help for older adults with CI. To our knowledge, our paper is the first to compare the prevalence of I/ADL difficulty without help received by living arrangement among older adults with CI using nationally-representative data in the US.
Our findings showing that living alone (versus living with others) was associated with higher prevalence of I/ADL difficulty without help received among older adults with CI could reflect the fact that those living alone are more likely to experience unmet needs for care, given that they lack cohabitating family members or others who provide the majority of dementia caregiving in the US [3, 4]. It is possible that existing home and community-based services (HCBS) might not always be sufficient, leading to older adults living alone with CI having a disproportionate risk of unmet care needs relative to their counterparts living with others.
On the other hand, the HRS measures of help received with I/ADLs are meant to capture the severity of I/ADL disability [5], whereby those who report receiving help are presumed to have a more severe need for assistance with that particular I/ADL. Taken together, responses may therefore be picking up on both unmet needs and disability severity due to several reasons: First, it is possible that individuals with CI living alone might be more vulnerable and have more unmet needs because they have less support compared to those living with others. Second, individuals with CI living alone might also represent a more select sample with less severe I/ADL disability and may not need others’ help relative to those with CI who may live with others as the result of more severe I/ADL disability and their need for assistance from others. However, we note these explanations are speculative and teasing this apart would require more detailed follow-up measures about unmet needs for care in the HRS.
Our study stands in contrast to prior evidence that has found that living alone was associated with higher odds of any disability [12], compared with living with a spouse only. In contrast, we found that among older women (but not men) with CI, those living alone were less likely than those living with others to report having any I/ADL disability. This may reflect the fact that older adults with CI who live alone may be a highly select group. That is, older adults who remained living alone with CI may have had distinct resources/abilities and/or health profiles: some of them might have greater resources and favorable health profiles, while others might have no choice but to live alone (e.g., in our sample, 70% older women living alone were widowed).
Limitations
We report several limitations. First, there is the potential for error in self- or proxy-reported disability measures not accounted for in our study. Second, the experience and consequences of having any I/ADL difficulty without help received may vary across different living settings (e.g., house with stairs versus age-friendly housing) and other factors. In addition, older adults living alone and living with others constitute highly heterogeneous groups. For example, living with spouses and non-spouse others might have different implications for support with I/ADLs. Third, although we restricted our sample to individuals with probable CIND or dementia, this may also be a highly heterogeneous group with variation by severity of cognitive and functional impairment given the lack of specific measures in our study. Lastly, while the scope of this study was to estimate the prevalence of I/ADL difficulty without help received among older adults with CI by living arrangements, future work will focus on the trajectories of both unmet I/ADL needs and living arrangements over time.
Conclusion
Using a nationally-representative sample of community-dwelling older adults aged 55+ living alone with probable dementia or cognitive impairment, we found that those living alone had a higher prevalence of I/ADL difficulty without help received by any sources of care. The magnitude of this difference was larger for men as compared to women, although results were similar across racial/ethnic subgroups. Our findings may reflect a higher prevalence of unmet needs among older adults with CI, which would suggest that currently available HCBS may not adequately ensure that older adults living alone with CI are receiving necessary assistance with activities of daily living [28]. However, future research should extend this analysis to additional outcome measures that triangulate self-reports of caregiving receipt with other sources (e.g., proxy informants, claims data) and utilize survey data that better captures the consequences of not receiving care.
Supplementary Material
ACKNOWLEDGMENTS
The authors would like to thank M. Maria Glymour and Julene Johnson for their comments on the conceptualization and data analyses.
This work was supported by National Institute on Aging, National Institutes of Health (R56AG062165 & R01AG069147 PI Portacolone, 1K99AG066846 PI Duchowny). No funding source had any role in the study design; collection, analysis, or interpretation of data; writing of the report; or the decision to submit the article for publication. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Authors’ disclosures available online (https://www.j-alz.com/manuscript-disclosures/22-0172r2).
Footnotes
SUPPLEMENTARY MATERIAL
The supplementary material is available in the electronic version of this article: https://dx.doi.org/10.3233/JAD-220172.
REFERENCES
- [1].Centers for Disease Control and Prevention (2011) Cognitive Impairment: A Call for Action, Now! https://www.cdc.gov/aging/pdf/cognitiveimpairment/cogimppoilicyfinal.pdf
- [2].Pinquart M, Sörensen S (2003) Differences between caregivers and noncaregivers in psychological health and physical health: A meta-analysis. Psychol Aging 18, 250–267. [DOI] [PubMed] [Google Scholar]
- [3].Schulz R, Martire LM (2004) Family caregiving of persons with dementia: Prevalence, health effects, and support strategies. Am J Geriatr Psychiatry 12, 240–249. [PubMed] [Google Scholar]
- [4].Wolff JL, Spillman BC, Freedman VA, Kasper JD (2016) A national profile of family and unpaid caregivers who assist older adults with health care activities. JAMA Intern Med 176, 372–379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Edwards RD, Brenowitz WD, Portacolone E, Covinsky KE, Bindman A, Glymour MM, Torres JM (2020) Difficulty and help with activities of daily living among older adults living alone with cognitive impairment. Alzheimers Dement 16, 1125–1133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Duane F, Brasher K, Koch S (2013) Living alone with dementia. Dementia 12, 123–136. [DOI] [PubMed] [Google Scholar]
- [7].Lee SM, Edmonston B (2019) Living alone among older adults in Canada and the US. Healthcare (Basel) 7, 68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Klinenberg E (2015) Heatwave: A social autopsy of disaster in Chicago, University of Chicago Press. [Google Scholar]
- [9].Wilmoth JM, Chen PC (2003) Immigrant status, living arrangements, and depressive symptoms among middle-aged and older adults. J Gerontol B Psychol Sci Soc Sci 58, S305–S313. [DOI] [PubMed] [Google Scholar]
- [10].Greenfield EA, Russell D (2011) Identifying living arrangements that heighten risk for loneliness in later life: Evidence from the US National Social Life, Health, and Aging Project. J Appl Gerontol 30, 524–534. [Google Scholar]
- [11].Pimouguet C, Rizzuto D, Schön P, Shakersain B, Angleman S, Lagergren M, Fratiglioni L, Xu W (2016) Impact of living alone on institutionalization and mortality: A population-based longitudinal study. Eur J Public Health 26, 182–187. [DOI] [PubMed] [Google Scholar]
- [12].Henning-Smith C (2017) Where do community-dwelling older adults with disabilities live? Distribution of disability in the United States of America by household composition and housing type. Ageing Soc 37, 1227–1248. [Google Scholar]
- [13].Edwards DF, Morris JC (2007) Alone and confused: Community-residing older African Americans with dementia. Dementia 6, 489–506. [Google Scholar]
- [14].Webber PA, Fox P, Burnette D (1994) Living alone with Alzheimer’s disease: Effects on health and social service utilization patterns. Gerontologist 34, 8–15. [DOI] [PubMed] [Google Scholar]
- [15].Gibson AK, Richardson VE (2017) Living alone with cognitive impairment. Am J Alzheimers Dis Other Demen 32, 56–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Mayeda ER, Glymour MM, Quesenberry CP, Whitmer RA (2016) Inequalities in dementia incidence between six racial and ethnic groups over 14 years. Alzheimers Dement 12, 216–224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Chen C, Zissimopoulos JM (2018) Racial and ethnic differences in trends in dementia prevalence and risk factors in the United States. Alzheimers Dement (N Y) 4, 510–520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].Schoeni RF, Martin LG, Andreski PM, Freedman VA (2005) Persistent and growing socioeconomic disparities in disability among the elderly: 1982–2002. Am J Public Health 95, 2065–2070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].Martin LG, Zimmer Z, Lee J (2017) Foundations of activity of daily living trajectories of older Americans. J Gerontol B Psychol Sci Soc Sci 72, 129–139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20].Bowen ME, Gonzalez HM (2008) Racial/ethnic differences in the relationship between the use of health care services and functional disability: The health and retirement study (1992–2004). Gerontologist 48, 659–667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].Reher D, Requena M (2018) Living alone in later life: A global perspective. Popul Dev Rev 44, 427–454. [Google Scholar]
- [22].Bugliari D, Campbell N, Chan C, Hayden O, Hayes J, Hurd M, Karabatakis A, Main R, Mallett J, McCullough C (2019) RAND HRS longitudinal file 2016 (V1) documentation. RAND Center for the Study of Aging, Santa Monica, CA. [Google Scholar]
- [23].Langa KM (2020) Langa-Weir classification of cognitive function (1995 Onward). Survey Research Center Institute for Social Research, University of Michigan. [Google Scholar]
- [24].Henning-Smith C, Shippee T, Capistrant B (2018) Later-life disability in environmental context: Why living arrangements matter. Gerontologist 58, 853–862. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [25].Brown RT, Diaz-Ramirez LG, Boscardin WJ, Cappola AR, Lee SJ, Steinman MA (2021) Changes in the hierarchy of functional impairment from middle age to older age. J Gerontol A Biol Sci, doi: 10.1093/gerona/glab250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [26].Barros AJ, Hirakata VN (2003) Alternatives for logistic regression in cross-sectional studies: An empirical comparison of models that directly estimate the prevalence ratio. BMC Med Res Methodol 3, 21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [27].Amjad H, Roth DL, Samus QM, Yasar S, Wolff JL (2016) Potentially unsafe activities and living conditions of older adults with dementia. J Am Geriatr Soc 64, 1223–1232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [28].Portacolone E, Torres JM, Johnson JK, Benton D, Rapp T, Tran T, Martinez P, Graham C (2022) The Living Alone with Cognitive Impairment Project’s policy advisory group on long-term services and supports: Setting a research equity agenda. Int J Environ Res Public Health 19, 6021. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.