Abstract
Objectives
To evaluate the effects of treatment of posterior crossbite (PXB) in the mixed dentition with the Function Generating Bite (FGB) appliance on the transverse dimension of the dental arches.
Materials and Methods
This study included 84 PXB patients (female = 46; male = 38; mean age, 8.2 ± 1.8 years) and 69 control (C) patients (female = 31; male = 38; mean age, 8.9 ± 1.4 years). Measurements were taken with digital calipers on maxillary and mandibular study casts before (T0) and after (T1) treatment for the following measures: intermolar (IMD), intermolar gingival (IMGD), intercanine (ICD), and intercanine gingival distances (ICGD).
Results
At T0, there was a significant difference in all maxillary measurements between the PXB and C groups (P < .001), reflecting maxillary hypoplasia in PXB patients. At T1, there was no difference between the groups. In PXB patients, the mean increase between T0 and T1 for IMD was 4.34 ± 2.42 mm; this difference measured 3.51 ± 2.19 mm for IMGD, 2.78 ± 2.37 mm for ICS, and 1.89 ± 1.7 mm for ICGD. There was no significant difference in mandibular measurements between groups at T0 and T1.
Conclusions
Functional therapy with FGB is effective in significantly increasing the transverse dimension of the maxillary dental arch in PXB patients. Considering its efficacy in treating masticatory dysfunction, FGB may be considered a good treatment option for the correction of PXB in growing children.
Keywords: Malocclusion, Crossbite, Functional orthodontic appliance, Interceptive orthodontics, Function Generating Bite
INTRODUCTION
Posterior crossbite is a serious malocclusion characteristic associated with maxillary hypoplasia and masticatory dysfunction.1–5 It is defined as the inversion of the occlusal relationship between upper and lower posterior teeth so that one or more maxillary buccal cusps are positioned in the central fossae of the mandibular teeth.6 However, it further entails a severe alteration of the neuromuscular control of mastication that involves the central nervous system and has serious consequences for the development of the individual.4 Mastication on the side of the malocclusion shows a significant alteration, characterized by a high prevalence of reverse-sequencing patterns.5,7–9 Reverse mastication on the side of the malocclusion is associated with reduced muscular activation, which deprives the affected side (or both sides, in instances of bilateral posterior crossbite) of the most important stimulus to growth and development: alternating, balanced functional activation.10 If the early form of positional posterior crossbite is left untreated, it progresses to irreversible dentoalveolar and skeletal asymmetry, including that of the temporomandibular joint.11,12 Early treatment of posterior crossbite is therefore of the utmost importance in order to correct both the occlusal and functional alterations.
Since the 1960s, different treatment options have been proposed for the correction of unilateral or bilateral posterior crossbite in mixed-dentition patients, including rapid maxillary expansion (RME) and slow expansion protocols with fixed appliances or removable plates.13 The functional appliance called the Function Generating Bite (FGB)14,15 is a fully removable appliance without any dental anchorage. It is uniquely characterized by resilient stainless-steel bite planes that level the occlusal plane and allow the mandible to self-reposition. In previous studies5 it was shown that treatment with FGB was associated with a significant reduction in the prevalence of reverse chewing cycles, effectively resolving masticatory dysfunction and balancing the two sides. Additionally, treatment with FGB was shown16 to be associated with a significant improvement and symmetry of temporomandibular joint function.
The aim of this study was to evaluate the effect of treatment of posterior crossbite with FGB in the mixed dentition on the transverse dimension of the dental arches in both the posterior and anterior regions.
MATERIALS AND METHODS
Patient Selection
This retrospective study sequentially included patients referred to the Department of Orthodontics at the Dental School at the University of Turin between 2019 and 2021. Written informed consent was obtained from all parents or legal guardians before the beginning of treatment. The study was conducted in accordance with the Declaration of Helsinki and was approved by the Ethics Committee of Turin University Hospital Health and Science Complex, University Hospital Ordine Mauriziano, A.S.L (Local Health Authority) City of Turin (protocol code 0069193).
The inclusion criteria were mixed dentition, unilateral or bilateral posterior crossbite without indication for surgical treatment, no signs or symptoms of dental or myofascial disorders, no previous orthodontic treatment, and presence of complete clinical data. Patients fulfilling the same inclusion criteria with mild deep bite or Class I malocclusion (crowding) and without posterior or anterior crossbite were included as a control group. The diagnosis of the malocclusion was carried out clinically and on study casts for all included patients.
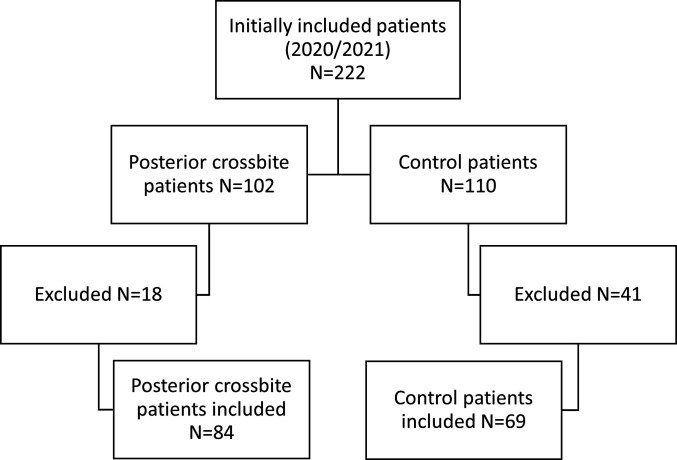
This study initially included 102 posterior crossbite patients and 110 control patients, based on initial case evaluation. Eleven posterior crossbite patients elected not to be treated after initial case evaluation; five posterior crossbite patients were treated with a different appliance; and in two patients, treatment was unsuccessful owing to lack of compliance. These 18 posterior crossbite patients were, therefore, excluded from the study. Seventeen control patients elected not to proceed with treatment after initial case evaluation; 20 control patients were treated with a different appliance; and four control patients elected to discontinue treatment before its completion (Figure 1).
Figure 1.
Flow chart of patient selection.
After the exclusion of 18 posterior crossbite patients and 41 control patients, a total of 153 patients were included in data collection and analysis: 84 posterior crossbite patients (female = 46; male = 38; mean age, 8.2 ± 1.8 years) and 69 control patients (female = 31; male = 38; mean age, 8.9 ± 1.4 years). In the posterior crossbite group, bilateral posterior crossbite represented 16% of the total; in the remaining 84% of unilateral posterior crossbite patients, 48% were posterior right and 36% were posterior left. Two percent of posterior crossbite patients also presented with deep bite and 5% with open bite. Molar classification in the posterior crossbite group was asymmetric in 17% of cases; in the remaining 83% of cases, the molar classification was symmetric (Angle Class I, 76%; Angle Class II, 19%; Angle Class III, 5%). In the control group, mild deep bite malocclusion represented 56% of the total; the remaining 44% were represented by mild crowding. Molar classification in the control group was strictly symmetric in all included patients. No patients with Angle Class II, Angle Class III, or open bite were included in the control group.
Measurements on Study Casts
To evaluate the increase in the transverse dimension of the arches following treatment with FGB, measurements were carried out with digital calipers on maxillary and mandibular study casts at two time points: before the beginning of treatment (T0) and following a stabilization period of 6 months after correction of the malocclusion (T1). Maxillary and mandibular interdental distances were measured as follows, adapting a methodology previously described17 (Figure 2):
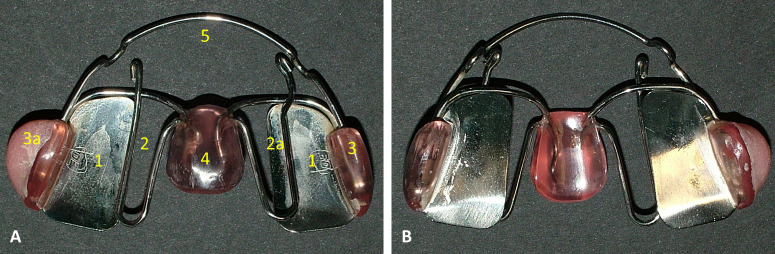
Figure 2.
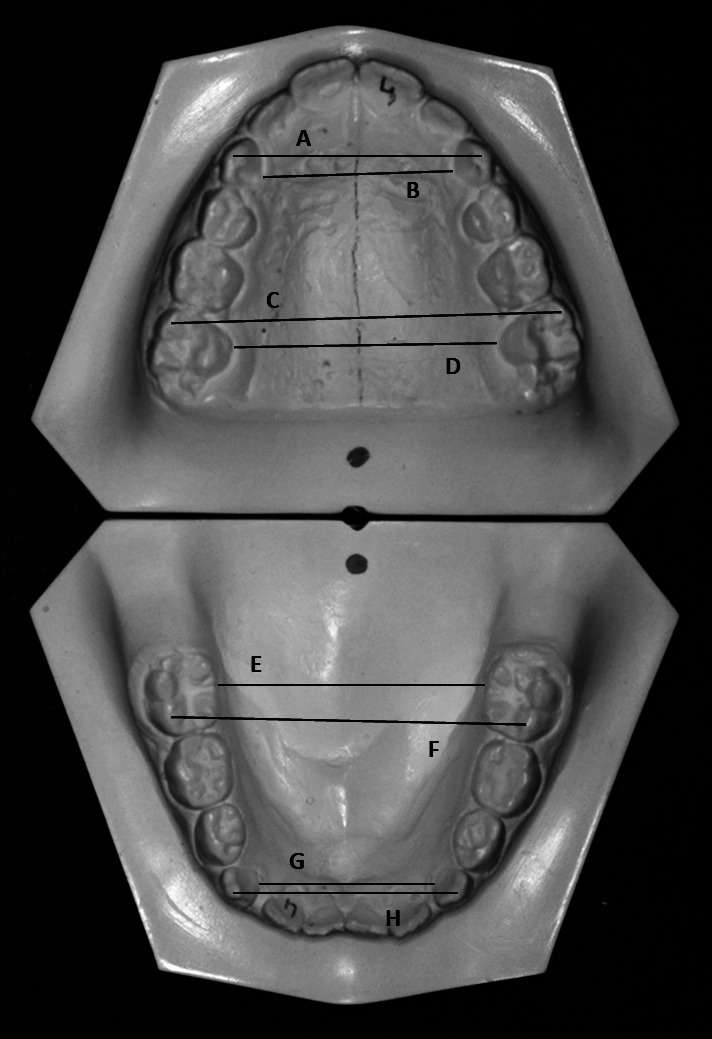
Digital caliper measurements on study casts. Maxillary intercanine (A), intercanine gingival (B), intermolar (C), and intermolar gingival (D) distances. Mandibular intermolar gingival (E), intermolar (F), intercanine gingival (G), and intercanine (H) distances.
Intermolar distance (IMD): the shortest distance between the tips of the mesiobuccal cusps of the first permanent molars;
Intermolar gingival distance (IMGD): the shortest distance between the first permanent molars at the gingival margin;
Intercanine distance (ICD): the shortest distance between the tips of deciduous or permanent canines; and
Intercanine gingival distance (ICGD): the shortest distance between deciduous or permanent canines at the gingival margin.
FGB Treatment Protocol
All included patients were treated with the functional FGB appliance4 (Figure 3). Each appliance was individually manufactured in acrylic resin and resilient stainless-steel, with occlusal metallic bite planes preventing the teeth from intercuspal contacts, aligning the occlusal plane and allowing the mandible to self-reposition in the three planes of space. The expansion springs were designed to lay 2 mm below the equator of the posterior maxillary teeth at rest and to reach it during swallowing in order to transmit the force generated by the activated masseter muscles. During the course of treatment, the expansion springs were activated in accord with the need to achieve transverse growth, as well as to adapt the appliance to the changes occurring in a developing individual. The orthodontic forces exerted by the expansion springs of this appliance, which come from the patient's neuromuscular activation when swallowing, are intermittent, self-regulating, and, therefore, individual and are suitable for the growing child. Posterior crossbite was considered corrected when the buccal cusps of the upper teeth, which were previously in crossbite, overlapped the lower teeth, thus providing the appropriate physiological stimuli from peripheral receptors and proprioceptors. During the active phase of treatment, patients were instructed to wear the appliance as much as possible during the day and night, except for during mealtimes. After the correction of the malocclusion, the appliance was worn at night only for retention.
Figure 3.
Function Generating Bite (FGB): view from above (A) and below (B). (A) Shows the main components of FGB: resilient stainless-steel bite planes (1), expansion springs (2 and 2a), resin buccal shields (3 and 3a), palatal button (4), and vestibular arch (5). Note that the expansion spring on the right (2a) was activated more than the expansion spring on the left and that the buccal shield on the left (3a) was made thicker than the buccal shield on the right (3) in order to provide true asymmetric action in a case of right unilateral posterior crossbite (Figure 3). The thicker buccal shield (3a) intercepts the left masseter and transfers the force to the more active spring on the right (2a).
In control patients, the appliance was used to level the occlusal plane during the course of interceptive orthodontic treatment, before the finishing phase with fixed appliance at the beginning of the permanent dentition period. In control patients, the action of the FGB appliance was restricted to that exerted by the stainless-steel bite planes, and the expansion springs were not activated. Transverse growth of the dental arches therefore took place without any expansion as a result of the treatment with FGB. Mean treatment time was 6.9 ± 2.6 months for posterior crossbite patients and 6.5 ± 3.4 months for the control group.
Statistical Analysis
Data are represented as mean ± standard deviation or median (25th percentile–75th percentile). Normality of distribution was evaluated with the Shapiro-Wilks test. All variables (maxillary and mandibular IMD, IMGD, ICD, and ICGD) showed a non-normal distribution. To evaluate the error of the method, a subset of 15 included patients were randomly selected and the measurements were retaken by the same author. Paired-sample Student's t-tests were performed on all considered variables, and intraclass correlation coefficients (ICCs) were assessed with a two-way mixed-effect model. Intergroup analysis (T0/T1) was performed with the Mann-Whitney U-test. Intragroup analysis (T0; T1) was performed with the Wilcoxon signed-rank test. Statistical significance was set at P < .01. The software STATA 17 (StataCorp LLC, College Station, Tex) was employed for all statistical analyses.
RESULTS
The error of the method was small enough to be nonsignificant for all included variables, and the ICC indicated excellent reliability (individual >90%).
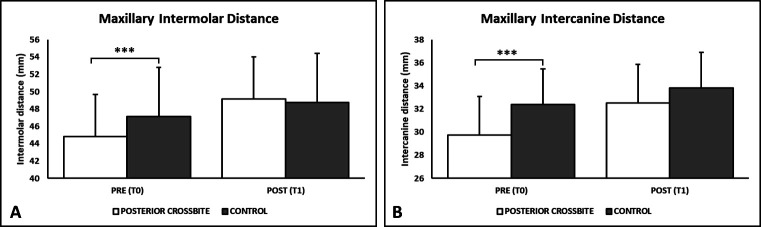
The results are shown in Table 1. For maxillary measurements (Figure 4), intergroup comparison at T0 showed a highly significant difference in all measurements between posterior crossbite and control patients (P < .001). At T1, there was no difference between the groups. In the posterior crossbite group, the mean increase between T0 and T1 for IMD was 4.34 ± 2.42 mm; this increase was 3.51 ± 2.19 mm for IMGD, 2.78 ± 2.37 mm for ICS, and 1.89 ± 1.7 mm for ICGD. Intragroup comparison between T0 and T1 was highly significant for all considered variables (P < .001).
Table 1. .
Resultsa
| Maxillary Measurements |
Posterior Crossbite—T0 |
Control—T0 |
Posterior Crossbite/ Control—T0b |
||||
| Mean (SD) |
Median (25th–75th) |
N |
Mean (SD) |
Median (25th–75th) |
N |
P-Value |
|
| Intermolar distance | 44.84 (4.84) | 46.00 (42.06–48.08) | 84 | 47.12 (5.67) | 48.13 (41.9–51.73) | 69 | <.001 |
| Intermolar gingival distance | 29.71 (3.26) | 30.13 (28.02–31.84) | 84 | 32.72 (3.39) | 33.1 (31.4–35) | 69 | <.001 |
| Intercanine distance | 29.76 (3.34) | 30.01 (28.1–32.07) | 77 | 32.40 (3.07) | 32.59 (30.75–33.8) | 64 | <.001 |
| Intercanine gingival distance | 22.97 (2.57) | 22.8 (22–25.16) | 77 | 24.91 (3.25) | 24.70 (23.14–26.95) | 64 | <.001 |
| Mandibular Measurements | – | – | – | ||||
| Intermolar distance | 42.62 (4.63) | 43.78 (39.29–45.66) | 82 | 41.37 (4.76) | 41.56 (37.96–45.51) | 69 | n.s. |
| Intermolar gingival distance | 32.25 (3.45) | 32.87 (31.04–34.19) | 82 | 31.82 (3.46) | 32.35 (30.1–33.85) | 67 | n.s. |
| Intercanine distance | 25.2 (3.30) | 25.54 (24.15–27.16) | 80 | 26.19 (2.58) | 25.98 (24.6–27.98) | 59 | n.s. |
| Intercanine gingival distance | 19.71 (2.61) | 19.99 (19.1–20.94) | 80 | 19.99 (2.30) | 20.2 (19–21.5) | 59 | n.s. |
| Maxillary Measurements |
Posterior Crossbite—T1 |
Control—T1 |
Posterior Crossbite/ Control—T1b |
||||
| Mean (SD) |
Median (25th–75th) |
N |
Mean (SD) |
Median (25th–75th) |
N |
P-Value |
|
| Intermolar distance | 49.18 (5.24) | 50.22 (46.05–52.88)c*** | 83 | 48.77 (6.22) | 49.85 (44.19–53.58)c*** | 69 | n.s. |
| Intermolar gingival distance | 33.22 (3.75) | 33.34 (31.34–35.91)c*** | 83 | 34.07 (3.67) | 34.4 (32.44–36.9)c*** | 69 | n.s. |
| Intercanine distance | 32.54 (3.01) | 32.78 (30.95–34.84)c*** | 72 | 33.84 (3.91) | 33.80 (32–36)c*** | 58 | n.s. |
| Intercanine gingival distance | 24.86 (2.48) | 24.83 (23.51–26.50)c*** | 72 | 25.98 (2.91) | 26.06 (24–28.35)c*** | 58 | n.s. |
| Mandibular Measurements | – | – | – | ||||
| Intermolar distance | 43.25 (5.04) | 44.83 (40.7–46.94)c*** | 78 | 42.00 (5.42) | 42.72 (37.7–46.05)c*** | 69 | n.s. |
| Intermolar gingival distance | 32.68 (3.24) | 33.23 (30.7–35.1)c*** | 78 | 32.38 (3.61) | 32.8 (30.7–34.9)c*** | 69 | n.s. |
| Intercanine distance | 25.82 (2.90) | 25.97 (24.59–27.5)c*** | 73 | 26.86 (3.30) | 26.76 (25.8–28.69)c*** | 63 | n.s. |
| Intercanine gingival distance | 19.94 (2.68) | 20.45 (18.83–21.4)c*** | 71 | 20.09 (2.64) | 20.43 (19.1–21.5)cn.s. | 63 | n.s. |
SD indicates standard deviation; T0, before treatment; and T1, after treatment.
Intergroup comparison (T0/T1): Mann-Whitney U-test.
Intragroup comparison (T0/T1): Wilcoxon signed-rank test.
P < .001; n.s. indicates not significant. Shapiro-Wilks test for normally distributed variables: P < .001 for all variables.
Figure 4.
Histograms showing the comparison between maxillary intermolar distance (A) and maxillary intercanine distance (B) before (T0) and after (T1) the correction of the malocclusion with Function Generating Bite.
*** P < .001.
For mandibular measurements, intergroup comparison at T0 did not show any significant difference between the groups. At T1, there was no significant difference between the groups. Intragroup comparison between T0 and T1 was highly significant for all considered variables (P < .001) except ICGD for the control group.
DISCUSSION
The aim of this study was to evaluate the efficacy of the functional FGB appliance in achieving significant increases in the transverse dimension of the dental arches when treating posterior crossbite malocclusion. This is the first publication to describe this treatment outcome with FGB. The results showed that correction of posterior crossbite with FGB was associated with significant and clinically relevant increases of the maxillary transverse dimension in both the molar and the canine regions.
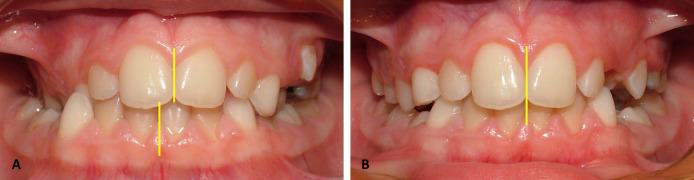
To evaluate the transverse dimension of the dental arches, a previously published methodology was followed.17–19 In the orthodontic literature, transverse expansion of the upper dental arch is most commonly evaluated with maxillary IMD. As shown in Table 1 and Figure 3A, this study found a highly significant difference in IMD between posterior crossbite and control patients before the beginning of treatment (P < .001), with posterior crossbite patients showing a constricted maxillary arch. After the correction of posterior crossbite with FGB, there was no difference in IMD between the groups. The mean increase in maxillary IMD in posterior crossbite patients was 4.34 ± 2.42 mm, a value that is not only statistically significant but also clinically relevant. This was comparable with the overall increase in maxillary IMD reported19 in a recent metanalysis of the effects of RME. On the contrary, in previous studies17 the effectiveness of removable tooth-anchored expansion plates was reported to be smaller than that associated with use of RME. In this context, the activity of FGB in the posterior region was remarkable because the activation of this appliance comes from the contraction of the masseter muscles every time the patient swallows. FGB is characterized by point-contacts with the teeth without any dental anchorage; when the patient is not swallowing, the appliance is freely floating in the mouth and there is no contact between the expansion springs and the maxillary posterior teeth. When the patient swallows, the force exerted by the contraction of the masseter muscles brings the appliance up; the bite planes are now in contact with the posterior teeth and the expansion springs intercept the equator of the posterior teeth (Figure 3). At each act of swallowing, therefore, a couple of forces, perpendicular to each other, are transmitted to the posterior teeth, a condition necessary to obtain orthodontic bodily movement. Concurrently, the force from masseter muscle contraction is transmitted through the buccal shields to the expansion spring on the opposite side of the appliance, allowing the asymmetric activation of the appliance, when needed.4 In this way, FGB is able to make use of the self-regulating and intermittent forces developed by the patient to bring about an orthodontic effect in a physiological and nontraumatic way. In unilateral posterior crossbite (Figure 5), the masseter muscle on the side of the malocclusion is known to be hypotrophic, whereas the masseter muscle on the non-crossbite side compensates for the reduced activation.20 The biomechanics of FGB takes advantage of this, transmitting the greater force coming from the hyperactive masseter muscle on the opposite side of the malocclusion, through the buccal shield, to the activated expansion spring on the side of the malocclusion. Thus, an asymmetric action suitable to move the teeth out of crossbite and to stimulate dentoalveolar bone growth is possible, when necessary, which is very important for the stability of the correction of the malocclusion. The forces that drive orthodontic effects of the FGB are, therefore, not mechanically predetermined but rather are a function of the loading capacity of the individual system. The forces generated by the masseter during swallowing are powerful and frequent enough to obtain these results. The posterior bite planes also protect the teeth from the signaling effects of the prematurities that inevitably occur with any orthodontic movement and allow for effective levelling of the occlusal plane.
Figure 5.
Unilateral posterior crossbite in the mixed dentition (A). Same patient after the correction of unilateral posterior crossbite with Function Generating Bite (B). Note that the midline deviation was corrected (yellow lines, A and B) as a result of mandibular self-repositioning.
In the anterior region, the maxillary ICD in posterior crossbite patients increased by 2.78 ± 2.37 mm. After correction of the malocclusion, posterior crossbite patients did not show any significant difference in ICD compared to control subjects.
There was no significant difference in mandibular interdental measurements between the groups, either before or after correction of the malocclusion. This reflects the association between posterior crossbite and maxillary hypoplasia.
This study had some limitations. For ethical reasons, untreated crossbite cases could not be used as controls, an approach that would have provided a more direct comparison. Alternatively, the choice was to select a control group with mild, symmetric malocclusion, whose treatment need was the levelling of the occlusal plane as part of interceptive orthodontic treatment. Studies21 based on the classical data from the Bolton-Brush Growth Study and the Burlington Growth Center showed a rate of maxillary transverse growth of about 1 mm/y between the ages of 6 and 14 years, measured on postero-anterior radiographs. Even though a direct comparison is not possible, this rate of maxillary growth was consistent with the increase in maxillary variables observed in the control group of the current study between T0 and T1.
In the future, it would be clinically interesting to evaluate the follow-up stability of the transverse dimensions of the dental arches in posterior crossbite patients treated with the FGB appliance.
CONCLUSIONS
The results of this study showed that the functional appliance, FGB, is effective in significantly increasing the transverse dimension of the maxillary dental arch in posterior crossbite patients in the mixed dentition.
Considered together with previously published reports of its efficacy in treating the reverse mastication associated with this malocclusion, FGB may be considered a good treatment option for the correction of posterior crossbite in growing children.
Funding Statement
ACKNOWLEDGMENT This work was funded in part by the Italian Ministry of Education, University and Research, “Ex60% 2020”.
REFERENCES
- 1.Moller E, Troelstrup B. Functional and morphologic asymmetry in children with unilateral cross-bite. J Dent Res . 1975;5(special issue):178. doi: 10.1111/j.1600-0722.1970.tb02092.x. [DOI] [PubMed] [Google Scholar]
- 2.Pinto AS, Buschang PH, Throckmorton GS, Chen P. Morphological and positional asymmetries of young children with functional unilateral posterior crossbite. Am J Orthod Dentofacial Orthop . 2001;120:513–520. doi: 10.1067/mod.2001.118627a. [DOI] [PubMed] [Google Scholar]
- 3.Harrison JE, Ashby D. Orthodontic treatment for posterior crossbites. Cochrane Database Syst Rev . 1CD000979. 2001. [DOI] [PubMed]
- 4.Piancino MG, Kyrkanides S. Ames, Iowa: John Wiley & Sons; 2016. Understanding Masticatory Function in Unilateral Crossbites. [DOI] [Google Scholar]
- 5.Piancino MG, Talpone F, Dalmasso P, Debernardi C, Lewin A, Bracco P. Reverse-sequencing chewing patterns before and after treatment of children with a unilateral posterior crossbite. Eur J Orthod . 2006;28:480–484. doi: 10.1093/ejo/cjl014. [DOI] [PubMed] [Google Scholar]
- 6.Ferro KJ, Morgano SM, Driscoll CF, Freilich MA, Guckes AD, Knoernschild KL, McGarry TJ. The glossary of prosthodontic terms. 9th edition. J Prosthet Dent . 2017;117:e1–e105. doi: 10.1016/j.prosdent.2016.12.001. [DOI] [PubMed] [Google Scholar]
- 7.Piancino MG, Comino E, Talpone F, Vallelonga T, Frongia G, Bracco P. Reverse-sequencing chewing patterns evaluation in anterior versus posterior unilateral crossbite patients. Eur J Orthod . 2012;34:536–541. doi: 10.1093/ejo/cjr109. [DOI] [PubMed] [Google Scholar]
- 8.Ferrario VF, Piancino MG, Dellavia C, Castroflorio T, Sforza C, Bracco P. Quantitative analysis of the variability of unilateral chewing movements in young adults. Cranio . 2006;24:274–282. doi: 10.1179/crn.2006.043. [DOI] [PubMed] [Google Scholar]
- 9.Frongia G, Ramieri G, De Biase C, Bracco P, Piancino MG. Changes in electric activity of masseter and anterior temporalis muscles before and after orthognathic surgery in skeletal Class III patients. Oral Surg Oral Med Oral Pathol Oral Radiol . 2013;116:398–401. doi: 10.1016/j.oooo.2013.06.008. [DOI] [PubMed] [Google Scholar]
- 10.Piancino MG, Farina D, Talpone F, Merlo A, Bracco P. Muscular activation during reverse and non-reverse chewing cycles in unilateral posterior crossbite. Eur J Oral Sci . 2009;117:122–128. doi: 10.1111/j.1600-0722.2008.00601.x. [DOI] [PubMed] [Google Scholar]
- 11.Lam P, Sadowsky C, Omerza F. Mandibular asymmetry and condylar position in children with unilateral posterior crossbite. Am J Orthod Dentofacial Orthop . 115. 1999. pp. 569–575. [DOI] [PubMed]
- 12.Pirttiniemi P, Raustia A, Kantomaa T, Pyhtinen J. Relationships of bicondylar position to occlusal asymmetry. Eur J Orthod . 1991;13:441–445. doi: 10.1093/ejo/13.6.441. [DOI] [PubMed] [Google Scholar]
- 13.Ugolini A, Agostino P, Silvestrini-Biavati A, Harrison JE, Batista KB. Orthodontic treatment for posterior crossbites. Cochrane Database Syst Rev . 12CD000979. 2021. [DOI] [PMC free article] [PubMed]
- 14.Bracco P, Solinas GF. Orthognathic correction of uni- and bilateral crossbite with a functional appliance. Mondo Ortod . 1979;4:8–24. [PubMed] [Google Scholar]
- 15.Bracco P, Solinas GF. Use and control of the “functional bite plate” in the early treatment of crossbite. Mondo Ortod . 1979;4:7–17. [PubMed] [Google Scholar]
- 16.Piancino MG, Roberi L, Frongia G, Reverdito M, Slavicek R, Bracco P. Computerized axiography in TMD patients before and after therapy with “function generating bites.”. J Oral Rehabil . 2008;35:88–94. doi: 10.1111/j.1365-2842.2007.01815.x. [DOI] [PubMed] [Google Scholar]
- 17.Petrén S, Bondemark L. Correction of unilateral posterior crossbite in the mixed dentition: a randomized controlled trial. Am J Orthod Dentofacial Orthop . 2008;133:790.e7–790.e13. doi: 10.1016/j.ajodo.2007.11.021. [DOI] [PubMed] [Google Scholar]
- 18.Agostino P, Ugolini A, Signori A, Silvestrini-Biavati A, Harrison JE, Riley P. Orthodontic treatment for posterior crossbites. Cochrane Oral Health Group ed Cochrane Database Syst Rev. 2014;8(8):CD000979. doi: 10.1002/14651858.CD000979.pub2. [DOI] [PubMed] [Google Scholar]
- 19.Cannavale R, Chiodini P, Perillo L, Piancino MG. Rapid palatal expansion (RPE): meta-analysis of long-term effects. Orthod Craniofac Res . 2018;21:225–235. doi: 10.1111/ocr.12244. [DOI] [PubMed] [Google Scholar]
- 20.Piancino MG, Falla D, Merlo A, et al. Effects of therapy on masseter activity and chewing kinematics in patients with unilateral posterior crossbite. Arch Oral Biol . 2016;67:61–67. doi: 10.1016/j.archoralbio.2016.03.013. [DOI] [PubMed] [Google Scholar]
- 21.Wagner DM, Chung CH. Transverse growth of the maxilla and mandible in untreated girls with low, average, and high MP-SN angles: a longitudinal study. Am J Orthod Dentofacial Orthop . 2005;128:716–723. doi: 10.1016/j.ajodo.2004.09.028. [DOI] [PubMed] [Google Scholar]