Abstract
Objectives
To investigate the effectiveness of utility arch (UA) with inter-maxillary elastics compared with fixed anterior bite plane (FABP) for treating deep bite in brachy-facial children.
Materials and Methods
This was a single-center, randomized controlled trial. Participants were children aged between 9 and 12 years with deep bite and a hypodivergent skeletal pattern. The sample was divided into the following two groups: (1) a UA group that was composed of patients with UAs with posterior inter-maxillary elastics and (2) an FABP group as a control. Outcomes were skeletal and dentoalveolar variables on cephalometric X-rays.
Results
A total of 28 patients (13 boys, 15 girls) with a mean age of 10.66 years were enrolled. The treatment duration was 8.16 months in the UA group and 7.22 months in the FABP group. After treatment, the angle between the anterior cranial base and the mandible in the vertical plane increased significantly (P = .000) in both groups (about 1.97 degrees in the UA group and 2.75 degrees in the FABP group). Overbite decreased significantly in both groups (−2.1 m in the UA group and −3.64 m in the FABP group), but it decreased less significantly in the UA group than in the FABP group. The upper incisors flared significantly after treatment with both appliances (6.6 degrees in the UA group and 5.9 degrees in the FABP group).
Conclusions
Treatment of deep bite in children with a horizontal growth pattern by each of the appliances used in this study is effective. The mandible showed minor, significant backward rotation after treatment. The overbite decreased less in the UA group than in the FABP group.
Keywords: Deep bite, Overbite, Orthodontic treatment, Children, Mixed dentition
INTRODUCTION
Deep bite is considered one of the most deleterious malocclusion traits for the masticatory apparatus and dental units.1 Graber and Vanarsdall defined “deep bite” as a condition of excessive overbite in which the vertical measurement between the maxillary and mandibular incisal margins is excessive when the mandible is brought into habitual or centric occlusion.2 When increased overbite is combined with palatally tipped upper incisors, it is called “deckbiss” (cover bite).3 Deep bite can be skeletal or dentoalveolar in origin. Skeletal deep bite is defined as convergence of the upper and lower jaw bases, which is caused by either backward inclination of the maxilla or forward rotation of the mandible or both.1 Skeletal deep bite with a hypodivergent growth pattern often accompanies Class II division 2 malocclusion. Many features are clear in this malocclusion, such as concave lip profile, pronounced chin, and short lower facial height.4
Extrusion of the posterior teeth, intrusion of the incisors, and proclination of the incisors are modalities for deep bite correction.5 Extrusion of the posterior teeth is the most common modality indicated in horizontal growth pattern patients. Many appliances have been used for this purpose, such as bite planes, myofunctional appliances, and cervical headgear.6,7 The classic treatment for deep bite in growing patients consists of a bite plane.8,9 The fixed anterior bite plane (FABP) is often used to treat deep bite, especially when combined with Class II.8,10–13 The utility arch (UA) may also be indicated for deep bite treatment. It was used for incisor protrusion, incisor intrusion, and posterior extrusion.14 In general, when deep bite is combined with retroclined upper incisors, treatment is indicated as soon as possible as it considered a risk factor for temporomandibular disorders.15
In the literature, there is no previous randomized controlled trial that studied deep bite correction in the mixed dentition according to a recent systematic review.16 The objective of this study was to assess the effectiveness of a UA with inter-maxillary elastics by evaluating the skeletal and dental changes induced during treatment of skeletal deep bite, mandibular in origin, combined with retroclined upper incisors (cover bite) in the mixed dentition.
MATERIALS AND METHODS
Trial Design
The Consolidated Standards of Reporting Trials (CONSORT) checklist was used as a guideline for conducting and reporting this trial.17 This study was a clinical randomized controlled trial. This study was approved by the local ethics committee of the University of Damascus Dental School, Syria (UDDS-638-18062019/SRC-3870). This study was registered with the German Clinical Trials Register (https://www.drks.de/drks_web/navigate.do?navigationId=trial.HTML&TRIAL_ID=DRKS00028870).
Participants
Children were recruited between December 2019 and January 2022 in the Department of Orthodontics, Damascus University.
Inclusion Criteria
Children with skeletal deep bite that resulted from forward rotation of the mandible (NSGoMe < 30).18
Children aged between 9 and 12 years before the cervical stage 3 (CS3) according to McNamara et al.19
Horizontal growth pattern according to Bjork (BJORK < 390).18
Skeletal Class I or mild to moderate Class II (ANB from 2 to 6).
Retroclined upper incisors (U1:SN < 98).
Overbite more than 40% (> 3.5 mm).20
Exclusion Criteria
Children who received previous orthodontic treatment.
Children with dental deep bite with normal upper and lower jaw bases.
Children with skeletal deep bite that resulted from maxillary origin (SN:Spp > 12).
Intervention Group
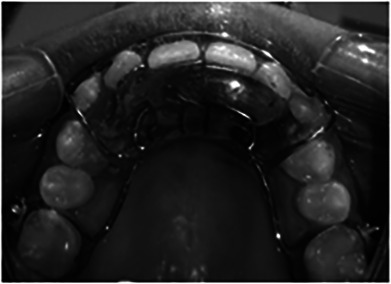
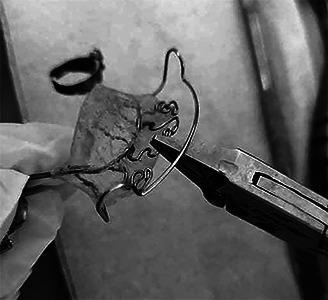
Edgewise 0.022-inch bands were cemented on the permanent maxillary first molars, and brackets were bonded to the incisors. Leveling and alignment of the upper incisors was performed with the following nickel-titanium arch wire sequence: 0.014 inches, 0.016 inches, and 0.016 × 0.016 inches. Then, a UA of 0.016 × 0.022-inch blue elgiloy was inserted. The UA design is shown in Figure 1. It was activated with a straight plier by making the angle between the posterior vertical step and the buccal segment obtuse (Figure 2).21 After the incisors reached their normal torque, the UA was fixed in a passive position, and bands with a lingual arch were cemented to the mandibular permanent first molars. Resin-modified glass ionomer cement (RMGIC) was bonded to the palatal surfaces of the upper incisors as bite planes (Figure 3). The posterior vertical space ranged from 1 to 2 mm. Vertical posterior inter-maxillary elastics (1/8-inch medium 4.5 oz) were applied from the upper first molar to the lower first molar (Figure 4). Once the posterior segments achieved occlusal contact, the RMGIC plane was modified and raised to create a posterior separation, and patients were asked to continue using the elastics. When the overbite reached the normal value (40%), the bands and brackets were debonded, and the retention appliance was delivered.
Figure 1.
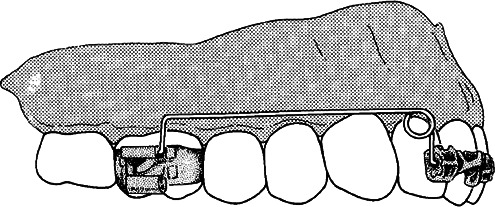
UA design.
Figure 2.
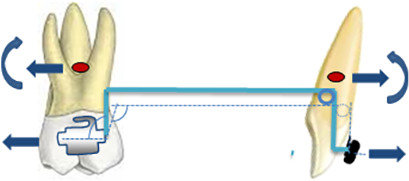
UA activation.
Figure 3.
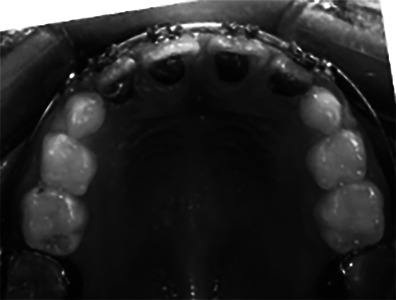
RMGIC on palatal surfaces of incisors.
Figure 4.

The posterior inter-maxillary elastic.
Control Group
A fixed, acrylic flat anterior bite plane soldered to the permanent first molars bands with a labial bow (stainless steel [SS] 0.7 mm) and palatal Z springs (SS 0.5 mm) was applied. The thickness of the bite plane was determined to exceed the freeway space, creating a vertical posterior separation ranging between 2 to 4 mm, according to Hellsing et al.8 Fixation of the appliance was achieved after activation of the Z springs by using glass ionomer cement as adhesive cement (Figure 5). Patients had visits every 3 weeks. At each visit, the appliance was removed, the incisor angulation was assessed, and reactivation was achieved when necessary. The springs were activated by a straight plier by pulling the wire 2-mm facially in the same horizontal plane (Figure 6). When the incisors reached the normal angulation in the buccolingual plane, the activation stopped. The treatment finished when overbite reached the normal value (40%) and the appliance was replaced by another for retention.
Figure 5.
The FABP.
Figure 6.
The activation of Z springs.
Primary Outcomes
The primary outcome measures were changes in SN:GoMe and overbite.
Secondary Outcomes
Secondary outcomes were vertical and sagittal angular and linear measurements. The variables are shown in Table 1. The outcomes were assessed on lateral cephalometric radiographs taken at time 0 (T0) and time 1 (T1). The cephalometric radiographs were traced using WebCeph (WebCeph, AssembleCircle Corp, Korea) (www.webceph.com) (Figures 7 and 8). The treatment time was also recorded.
Table 1. .
Skeletal and Dentoalveolar Variables
| Abbreviation |
Definition |
| SNA | Angle between anterior cranial base and maxilla in sagittal plane |
| SNB | Angle between anterior cranial base and mandible in sagittal plane |
| ANB | Angle between maxilla and mandible in sagittal plane |
| SNAr | Saddle angle |
| SArGo | Articular angle |
| ArGoMe | Gonial angle |
| BJORK sum | Sum of the three previous angles |
| SN:Spp | Angle between anterior cranial base and maxilla in vertical plane |
| SN:GoMe | Angle between anterior cranial base and mandible in vertical plane |
| MM | Angle between maxilla and mandible in vertical plane |
| S-Go | Posterior facial height |
| N-Me | Anterior facial height |
| Jarabak | Facial height percentage |
| Overjet | Horizontal distance between the buccal surface of upper incisor and lower incisor in sagittal plane |
| Overbite | Vertical overlap of upper incisor to lower incisor |
| U1-Spp | Distance between the crown's tip of upper incisor and maxillary plane |
| U6-Spp | Distance between the buccal groove of upper molar and maxillary plane |
| L1-MP | Distance between the crown's tip of lower incisor and mandible plane |
| L6-MP | Distance between the mesio-buccal groove of lower molar and mandible plane |
| U1:SN | Angle between upper incisor and anterior cranial base |
| L1:Go Me | Angle between lower incisor and mandible plane |
Figure 7.
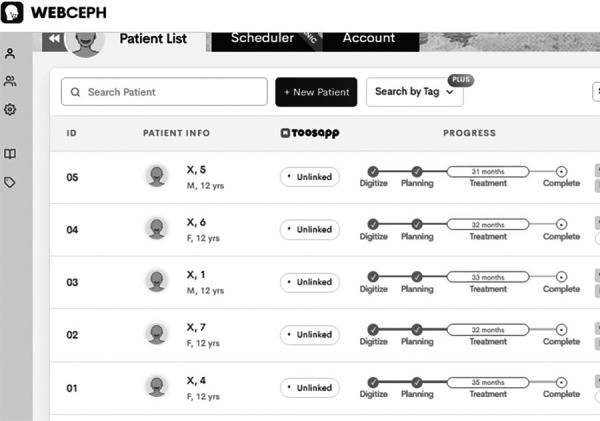
WebCeph records.
Figure 8.
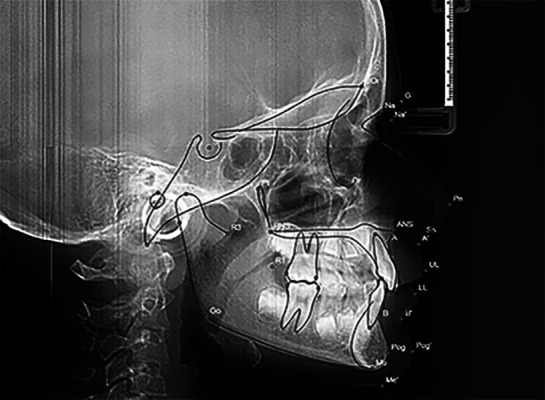
Landmarks detection and tracing.
Sample Size Calculation
Sample size was calculated using G-Power version 3.0.10 (Universitate Keil, Keil, Germany). Because no previous study compared overbite correction between UAss and bite planes, data from a study assessing the effectiveness of FABP were used.22 The means and standard deviations of the primary outcome (SN:GoMe) before and after treatment were 32.5 ± 4.3 and 34.1 ± 4.4, respectively, and the mean of the difference was 1.6 ± 2.25. The effect size was calculated to be 0.71. If α = 5% and β is 95% with a paired t-test, 14 patients were required in each group (Figure 9). To compensate for any possible attrition, a 5% attrition percentage (one patient in each group) was added. The total sample size was 30.
Figure 9.
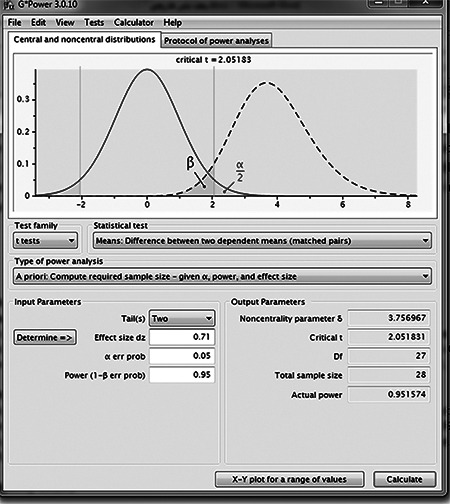
Sample size calculation.
Randomization, Allocation Concealment, and Blinding
Simple randomization was conducted by one of the academic staff members who was not involved in this research. Computer-generated random numbers were used with an allocation ratio of 1:1. The allocation sequence was concealed using sequentially numbered, opaque, sealed envelopes. Blinding of personnel and participants were not applicable. Therefore, blinding was applied only for the outcome assessor.
Statistical Methods
The statistical analysis was conducted using IBM (Armonk, N.Y.) SPSS Statistic Data Editor version 24. The Shapiro-Wilk normality test was conducted. When data were normally distributed, paired-sample and two-sample t-tests were applied. When a non-normal distribution was detected, nonparametric tests were applied (Wilcoxon matched pair signed rank, Mann-Whitney U-test). Statistical analysis was performed by one author who was blinded to all measurements.
Error of the Method
A total of 16 cephalometric radiographs were randomly chosen after a 1-month interval. The intraclass correlation coefficient (ICC) test was used to determine the random error,23 and a paired t-test was used to determine any systematic error.
RESULTS
A total of 30 patients were enrolled in this trial. One patient in the UA group did not receive the allocated intervention because of noncompliance, and one patient in the FABP group was lost to follow-up for personal reasons. A total of 28 patients (14 in each group) with a mean age of 10.66 ± 1.1 years were analyzed. Patient allocation and follow-up are shown in Figure 10. The basic characteristics of the sample are presented in Table 2. The treatment duration was 8.16 ± 2.42 months in the UA group and 7.22 ± 2.63 months in the FABP group; however, the difference in duration between groups was not significant (P = .335) (Table 3).
Figure 10.
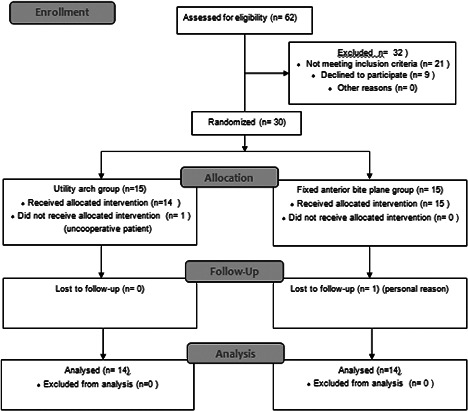
CONSORT flow diagram.
Table 2. .
Characteristics of the Sample
|
|
N |
Age, Years |
Difference Between Groups (Two-Sample t-Test) |
Sex |
Difference Between Groups, χ2 |
||||||
| Mean |
Standard Deviation |
No. of Boys |
Percentage of Boys |
No. of Girls |
Percentage of Girls |
||||||
| UA group | 14 | 10.65 | 0.97 | Mean | 0.01357 | 8 | 57 | 6 | 43 | ||
| FABP group | 14 | 10.67 | 1.25 | Standard error difference | 0.42592 | 7 | 50 | 7 | 50 | ||
| Total | 28 | 10.66 | 1.10 | P value | .975 | 15 | 53 | 13 | 47 | P value | .705 |
| Significance | NS | Significance | NS | ||||||||
Table 3. .
Treatment Time
| Treatment Time, Months |
UA Group |
FABP Group |
Difference Between Groups |
|
| Mean | 8.1629 | 7.2229 | Mean difference | 0.94 |
| Standard deviation | 2.42306 | 2.63211 | Standard error difference | 0.956 |
| P value | .335 | |||
| Significance | NS | |||
A paired-sample t-test was conducted to assess the systematic error. It showed that there was no significant difference between the two measurements (P > .05) (Supplemental Table 1). For evaluating the random error, the ICC was calculated. It ranged from .913 to .997, meaning high reproducibility for the measurements made on cephalometric radiographs (Supplemental Table 2).
The normality test (Shapiro-Wilk) was used to assess the distribution of data. All the data at T0 and T1 in both groups were normally distributed (Table 4).
Table 4. .
Normality Test Results (Shapiro-Wilk)
| Variable |
T0 |
T1 |
||||||||||
| UA Group |
FABP Group |
UA Group |
FABP Group |
|||||||||
| Statistic |
P Value |
Significance |
Statistic |
P Value |
Significance |
Statistic |
P Value |
Significance |
Statistic |
P Value |
Significance |
|
| SNA | .935 | .354 | NS | .948 | .534 | NS | .969 | .862 | NS | .905 | .135 | NS |
| SNB | .959 | .712 | NS | .913 | .176 | NS | .959 | .706 | NS | .894 | .092 | NS |
| ANB | .960 | .727 | NS | .896 | .099 | NS | .945 | .489 | NS | .967 | .832 | NS |
| SN:Spp | .958 | .698 | NS | .946 | .501 | NS | .955 | .644 | NS | .945 | .492 | NS |
| SN:GoMe | .889 | .077 | NS | .911 | .165 | NS | .912 | .167 | NS | .980 | .976 | NS |
| MM | .929 | .294 | NS | .968 | .855 | NS | .922 | .232 | NS | .911 | .162 | NS |
| SNAr | .946 | .496 | NS | .905 | .134 | NS | .918 | .202 | NS | .961 | .736 | NS |
| SArGo | .961 | .739 | NS | .935 | .362 | NS | .979 | .969 | NS | .969 | .869 | NS |
| ArGoMe | .945 | .492 | NS | .943 | .456 | NS | .894 | .094 | NS | .986 | .995 | NS |
| BJORK sum | .933 | .341 | NS | .884 | .067 | NS | .984 | .991 | NS | .953 | .609 | NS |
| S-Go | .964 | .788 | NS | .882 | .062 | NS | .914 | .183 | NS | .967 | .832 | NS |
| N-Me | .936 | .373 | NS | .895 | .095 | NS | .946 | .501 | NS | .946 | .505 | NS |
| Jarabak | .934 | .349 | NS | .893 | .091 | NS | .937 | .376 | NS | .937 | .382 | NS |
| Overjet | .937 | .378 | NS | .937 | .386 | NS | .912 | .170 | NS | .928 | .287 | NS |
| Overbite | .919 | .213 | NS | .957 | .675 | NS | .920 | .219 | NS | .923 | .241 | NS |
| U1-Spp | .924 | .251 | NS | .922 | .232 | NS | .975 | .939 | NS | .886 | .071 | NS |
| U6-Spp | .943 | .454 | NS | .960 | .721 | NS | .969 | .868 | NS | .889 | .079 | NS |
| L1-MP | .957 | .679 | NS | .921 | .225 | NS | .945 | .481 | NS | .893 | .089 | NS |
| L6-MP | .883 | .064 | NS | .892 | .085 | NS | .960 | .717 | NS | .957 | .672 | NS |
| U1:SN | .951 | .584 | NS | .961 | .745 | NS | .946 | .500 | NS | .933 | .332 | NS |
| L1:Go Me | .936 | .366 | NS | .942 | .439 | NS | .978 | .962 | NS | .960 | .730 | NS |
All the skeletal and dentoalveolar outcomes measures showed insignificant differences between the groups at T0 (Tables 5 and 6). After treatment, SN:GoMe increased significantly (P < .001) in both groups (about 1.97 degrees in UA group and 2.75 degrees in FABP group). However, the difference between groups was not significant. The angle between the maxilla and mandible in the vertical plane increased significantly in both groups (1.55 degrees ± 1.82 degrees in the UA group, P = .007; 2.81 degrees ± 1.74 degrees in the FABP group, P < .001), but the difference between groups was negligible and not significant. The BJORK sum increased significantly in both groups (0.79 degrees ± 1.24 degrees in the UA group, 1.37 degrees ± 1.12 degrees in the FABP group). In the UA group, the N-Me and ANS-ME heights increased significantly, whereas the Jarabak outcome decreased significantly (−0.80 ± 1.08). The anterior and posterior facial heights increased significantly in the FABP group; however, the Jarabak percentage did not decrease significantly (Table 7).
Table 5. .
Skeletal Characteristics at T0
| T0 |
UA Group |
FABP Group |
Difference Between Groups (Two-Sample t-Test) |
|||||||
| Variable |
N |
Mean |
Standard Deviation |
N |
Mean |
Standard Deviation |
Mean Difference |
Standard Error Difference |
P Value |
Significance |
| SNA | 14 | 79.9271 | 3.61461 | 14 | 80.1000 | 2.72918 | −0.17286 | 1.21049 | .888 | NS |
| SNB | 14 | 75.2443 | 2.96545 | 14 | 76.2121 | 3.22098 | −0.96786 | 1.17012 | .416 | NS |
| ANB | 14 | 4.6829 | 1.74454 | 14 | 3.8864 | 2.04136 | 0.79643 | 0.71766 | .277 | NS |
| SN-Spp | 14 | 9.6457 | 1.24654 | 14 | 9.0886 | 1.56208 | 0.55714 | 0.53412 | .307 | NS |
| SN:GoMe | 14 | 29.2000 | 0.57032 | 14 | 28.8529 | 1.16851 | 0.34714 | 0.34751 | .330 | NS |
| MM | 14 | 19.5543 | 1.12034 | 14 | 19.7643 | 2.04635 | −0.21000 | 0.62351 | .740 | NS |
| SNAr | 14 | 124.7843 | 4.67361 | 14 | 124.3943 | 3.68320 | 0.39000 | 1.59034 | .808 | NS |
| SArGo | 14 | 144.9150 | 5.74281 | 14 | 143.7750 | 4.45871 | 1.14000 | 1.94312 | .562 | NS |
| ArGoMe | 14 | 119.0614 | 2.79303 | 14 | 119.8207 | 3.44833 | −0.75929 | 1.18599 | .528 | NS |
| BJORK sum | 14 | 388.7607 | 1.27051 | 14 | 387.9900 | 2.39259 | 0.77071 | 0.72401 | .300 | NS |
| S-Go | 14 | 66.7843 | 4.00768 | 14 | 66.8357 | 5.09330 | −0.05143 | 1.73212 | .977 | NS |
| N-Me | 14 | 99.7779 | 5.81403 | 14 | 99.7750 | 6.96393 | 0.00286 | 2.42457 | .999 | NS |
| Jarabak | 14 | 66.9860 | 2.85647 | 14 | 66.9754 | 2.71707 | 0.01058 | 1.05363 | .992 | NS |
Table 6. .
Dentoalveolar Characteristics at T0
| T0 |
UA Group |
FABP Group |
Difference Between Groups (Two-Sample t-Test) |
|||||||
| Variable |
N |
Mean |
Standard Deviation |
N |
Mean |
Standard Deviation |
Mean Difference |
Standard Error Difference |
P Value |
Significance |
| Overjet | 14 | 4.3621 | 1.32861 | 14 | 4.7114 | 1.34243 | −0.34929 | 0.50478 | .495 | NS |
| Overbite | 14 | 4.9586 | 1.18425 | 14 | 5.4829 | 1.59868 | −0.52429 | 0.53172 | .333 | NS |
| U1-Spp | 14 | 23.9557 | 1.38417 | 14 | 24.5893 | 2.16151 | −0.63357 | 0.68598 | .364 | NS |
| U6-Spp | 14 | 16.8236 | 1.80051 | 14 | 17.0979 | 1.94123 | −0.27429 | 0.70762 | .701 | NS |
| L1-MP | 14 | 33.4093 | 1.79093 | 14 | 33.5386 | 2.60101 | −0.12929 | 0.84400 | .879 | NS |
| L6-MP | 14 | 23.3864 | 1.71376 | 14 | 23.0857 | 2.00632 | 0.30071 | 0.70520 | .673 | NS |
| U1:SN | 14 | 91.8493 | 4.91451 | 14 | 94.2979 | 5.61870 | −2.44857 | 1.99503 | .231 | NS |
| L1:Go Me | 14 | 92.4093 | 5.50449 | 14 | 90.7529 | 5.06934 | 1.65643 | 1.99996 | .415 | NS |
Table 7. .
Differences in Skeletal Outcomes Between the Groups (Two-Sample t-Test)
| Variable |
UA Group (T1-T0) |
FABP Group (T1-T0) |
Mean Difference Between Groups |
Standard Error Difference |
95% Confidence Interval of the Difference |
P Value |
Significance |
|||||||
| Mean Difference |
Standard Deviation |
P Value |
Significance |
Mean Difference |
Standard Deviation |
P Value |
Significance |
Lower |
Upper |
|||||
| SNA | −0.78643 | 1.24392 | .034 | * | 0.32286 | 1.56544 | .454 | NS | −1.10929 | 0.53438 | −2.20773 | −0.01084 | .048 | * |
| SNB | −0.20929 | 0.49476 | .137 | NS | 0.22929 | 1.50653 | .579 | NS | −0.43857 | 0.42379 | −1.33803 | 0.46089 | .316 | NS |
| ANB | −0.58000 | 0.93834 | .038 | * | 0.09357 | 0.92969 | .713 | NS | −0.67357 | 0.35303 | −1.39923 | 0.05209 | .067 | NS |
| SN-Spp | 0.42286 | 0.73547 | .051 | NS | −0.05143 | 0.77562 | .808 | NS | 0.47429 | 0.28567 | −0.11292 | 1.06149 | .109 | NS |
| SN:GoMe | 1.97286 | 1.51036 | .000 | *** | 2.75857 | 1.60014 | .000 | *** | −0.78571 | 0.58807 | −1.99452 | 0.42309 | .193 | NS |
| MM | 1.55000 | 1.82377 | .007 | ** | 2.81000 | 1.74800 | .000 | *** | −1.26000 | 0.67515 | −2.64779 | 0.12779 | .073 | NS |
| SNAr | −0.53071 | 1.75612 | .279 | NS | 1.00500 | 4.11426 | .377 | NS | −1.53571 | 1.19556 | −3.99322 | 0.92179 | .210 | NS |
| SArGo | 1.63071 | 2.82666 | .050 | NS | 1.02071 | 4.81871 | .442 | NS | 0.61000 | 1.49308 | −2.45907 | 3.67907 | .686 | NS |
| ArGoMe | −0.31000 | 2.61734 | .665 | NS | −0.57071 | 1.93004 | .289 | NS | 0.26071 | 0.86913 | −1.52581 | 2.04724 | .767 | NS |
| BJORK sum | 0.79000 | 1.24723 | .034 | * | 1.37143 | 1.12084 | .001 | ** | −0.58143 | 0.44816 | −1.50264 | 0.33978 | .206 | NS |
| S-Go | 0.43500 | 1.90781 | .409 | NS | 1.17643 | 2.00462 | .047 | * | −0.74143 | 0.73961 | −2.26171 | 0.77886 | .325 | NS |
| N-Me | 1.84929 | 2.92403 | .034 | * | 2.87929 | 3.54365 | .009 | ** | −1.03000 | 1.22787 | −3.55393 | 1.49393 | .409 | NS |
| Jarabak | −0.80292 | 1.08622 | .016 | * | −0.70224 | 2.11374 | .236 | NS | −0.10068 | 0.63515 | −1.42812 | 1.22676 | .876 | NS |
P > .05; **P > .01; ***P > .001.
In the sagittal plane, SNA and ANB decreased significantly after treatment in the UA group, whereas there were nonsignificant (NS) differences in the FABP group (Table 7).
Regarding the dentoalveolar outcomes, the overjet increases were not significant in either group. Overbite decreased significantly less in the UA group than in the FABP group. The U1-Spp did not show any significant difference in the UA group, whereas it showed a significant decrease in the FABP group. The U6-Spp, L1-MP, and L6-MP did not differ significantly. The upper incisors protruded significantly in both groups, whereas the lower incisors protruded significantly in the UA group but not significantly in the FABP group (Table 8).
Table 8. .
Differences in Dentoalveolar Outcomes Between the Groups (Two-Sample t-Test)
| Variable |
UA Group (T1-T0) |
FABP Group (T1-T0) |
Mean Difference Between Groups |
Standard Error Difference |
95% Confidence Interval of the Difference |
P Value |
Significance |
|||||||
| Mean Difference |
Standard Deviation |
P Value |
Significance |
Mean Difference |
Standard Deviation |
P Value |
Significance |
Lower |
Upper |
|||||
| Overjet | 0.36214 | 1.11931 | .248 | NS | 1.12500 | 2.19088 | .077 | NS | −0.76286 | 0.65753 | −2.11443 | 0.58871 | .257 | NS |
| Overbite | −2.10143 | 0.92874 | .000 | *** | −3.64571 | 1.87999 | .000 | *** | 1.54429 | 0.56042 | 0.37127 | 2.71730 | .013 | ** |
| U1-Spp | −0.28571 | 0.89303 | .253 | NS | −1.45643 | 1.80451 | .010 | * | 1.17071 | 0.53810 | 0.06463 | 2.27680 | .039 | * |
| U6-Spp | 0.51643 | 1.22524 | .139 | NS | 0.25071 | 1.46339 | .533 | NS | 0.26571 | 0.51009 | −0.78279 | 1.31422 | .607 | NS |
| L1-MP | 0.38214 | 0.83251 | .110 | NS | −0.31643 | 1.56355 | .462 | NS | 0.69857 | 0.47342 | −0.27456 | 1.67170 | .152 | NS |
| L6-MP | 0.63571 | 1.36928 | .255 | NS | 0.56071 | 1.12277 | .401 | NS | 0.17500 | 0.47325 | −0.79778 | 1.14778 | .715 | NS |
| U1:SN | 6.60143 | 4.32112 | .000 | *** | 5.97357 | 5.42365 | .001 | ** | 0.62786 | 1.85334 | −3.18174 | 4.43745 | .738 | NS |
| L1:Go Me | 3.39214 | 3.05518 | .001 | ** | 2.00857 | 5.19676 | .172 | NS | 1.38357 | 1.61113 | −1.92816 | 4.69530 | .398 | NS |
P > .05; **P > .01; ***P > .001.
DISCUSSION
This was the first randomized clinical trial comparing two techniques for treating deep overbite in children with a horizontal growth pattern.16 The combination of a UA and vertical posterior inter-maxillary elastics was evaluated for the first time in this study. However, the use of posterior vertical elastics was previously reported for extrusion to treat deep bite.24 Because the inter-maxillary elastic was applied buccally, it would cause lingual tipping of the molars. The UA was fixed in a passive position on the upper molars after incisor protrusion was achieved, and the buccal segment retained molar torque. However, for the lower molars, a lingual arch was cemented on the first permanent molars to avoid any lingual tipping. The UA was applied after leveling and aligning the incisors, correcting their torque and protruding them, thus causing facial movement of the incisor crowns and palatal movement of the roots. This may have resulted in the significant decrease of the SNA angle and, consequently, the ANB angle in the UA group because of the effect of root movement on the position of A point.25 In the FABP group, SNA did not show any significant changes as the upper incisors were protruded using palatal Z springs with more crown tipping and less root torque. After protrusion of incisors, the mandible did not seem to move forward in the sagittal plane in either group. To the contrary, point B retruded in both groups, but not significantly, because of an opening rotation of the mandible.
Ve İskeletsel evaluated the effect of an FABP for deep bite treatment in the mixed dentition. According to that study, SNB increased significantly and ANB decreased after treatment because of the anterior position of mandible.22 That contrasts with the current study, possibly because of the difference in appliance design using an inclined bite plane. In another study that assessed the effect of a removable anterior bite plane with a jackscrew, ANB decreased significantly.26
Vertically, the mandible showed a small opening rotation after treatment by both appliances, which resulted in an increase in SN:GoMe, MM, and BJORK. Applying RMGIC on the palatal surfaces of the upper incisors with posterior vertical inter-maxillary elastics resulted in extrusion of the posterior teeth in the UA group. However, although the amount of extrusion was not significant, it appeared that the growth direction of the mandible was affected. In the FABP group, passive extrusion occurred because of the posterior vertical space. Although the mandible rotated open, the gonial angle did not show any significant difference in either group. Therefore, rotation of the mandible occurred with no changes in gonial angle dimensions. Points Go and Me moved downward and backward, which affected the anterior and posterior facial heights, but the N-Me and S-Go measures increased because of a positional difference more than a dimensional difference. The facial height percentage according to Jarabak decreased significantly in the UA group but not significantly in the FABP group. However, there was no significant difference between the groups.
Forsberg and Hellsing first studied the FABP to treat Class II deep bite in children and adolescents. They found that this appliance affected mandibular growth and caused opening rotation, which is in agreement with the current study.8,10 According to another previous study, SNGoGn increased after treatment with an FABP as a result of the opening rotation of the mandible.22 In the study by Ansari et al., SNGoGn did not show any significant change, and the Jarabak percentage increased significantly.26 Another study showed that the mandible rotated open after using the anterior bite plane in children with Class II deep bite.13
Regarding the dentoalveolar outcomes, the overjet did not show any significant differences, whereas the overbite decreased significantly less in the UA than in the FABP group. This may be explained by the relative intrusion that occurred in the upper incisors in the FABP group, which was greater than in the UA group. Occlusion of the lower incisors on the acrylic bite plane with activated palatal Z springs might have caused an intrusive force in addition to the protrusive force on the upper incisors, resulting in a significant decrease in U1-Spp. A small, but NS, amount of intrusion also occurred in the lower incisors because of the fixed bite plane. Another previous study found that overbite decreased significantly after treatment with an FABP.13,22 The U6-Spp and L6-MP increased in both groups because of the extrusive force; however, this increase was not significant. The upper incisors protruded significantly in both groups. Because of the separation between the upper and lower arches in both groups, the lower incisors were released from the restriction caused by the retroclined upper incisors, thus enabling lower incisor protrusion to occur in the UA group.
Limitations
Although the appliances used in the study were fixed, the inter-maxillary elastics were dependent on patient cooperation. The application of the UA caused ulcers in some patients, and it was removed until healing occurred.
CONCLUSIONS
The mandible showed a small but significant opening rotation after treatment by both appliances.
The overbite decreased less in the UA group than in the FABP group.
The maxillary incisors protruded after treatment in both groups.
SUPPLEMENTAL DATA
Supplemental Tables 1 and 2 are available online.
Supplementary Material
REFERENCES
- 1.Sreedhar C, Baratam S. Deep overbite—a review. Ann Essence Dent . 2009;1(1):8–25. [Google Scholar]
- 2.Graber TM, Vanarsdall RL., Jr . Orthodontics Current Principles and Techniques (2nd ed) St. Louis, MO: Mosby–Year Book; 1994. [Google Scholar]
- 3.Youssef M. Craniofacial growth pattern in cover-bite malocclusions and its therapeutic influencing. J Orofac Orthop . 2001;62(6):422–435. doi: 10.1007/s00056-001-9740-6. [DOI] [PubMed] [Google Scholar]
- 4.Hultgren BW, Isaacson RJ, Erdman AG, Worms FW, Rekow ED. Growth contributions to Class II corrections based on models of mandibular morphology. Am J Orthod . 1980;78(3):310–320. doi: 10.1016/0002-9416(80)90276-6. [DOI] [PubMed] [Google Scholar]
- 5.Daokar S, Agrawal G. Deep bite its etiology, diagnosis and management: a review. J Orthod Endod . 2016;2:4. [Google Scholar]
- 6.de Almeida-Pedrin RR, de Almeida MR, de Almeida RR, Pinzan A, Ferreira FPC. Treatment effects of headgear biteplane and bionator appliances. Am J Orthod Dentofacial Orthop . 2007;132(2):191–198. doi: 10.1016/j.ajodo.2005.07.030. [DOI] [PubMed] [Google Scholar]
- 7.Hans MG, Kishiyama C, Parker SH, Wolf GR, Noachtar R. Cephalometric evaluation of two treatment strategies for deep overbite correction. Angle Orthod . 1994;64(4):265–274. doi: 10.1043/0003-3219(1994)064<0265:CEOTTS>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 8.Hellsing E, Hellsing G, Eliasson S. Effects of fixed anterior biteplane therapy—a radiographic study. Am J Orthod Dentofacial Orthop . 1996;110(1):61–68. doi: 10.1016/s0889-5406(96)70088-4. [DOI] [PubMed] [Google Scholar]
- 9.Franchi L, Baccetti T, Giuntini V, Masucci C, Vangelisti A, Defraia E. Outcomes of two-phase orthodontic treatment of deepbite malocclusions. Angle Orthod . 2011;81(6):945–952. doi: 10.2319/033011-229.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Forsberg C-M, Hellsing E. The effect of a lingual arch appliance with anterior bite plane in deep overbite correction. Eur J Orthod . 1984;6(1):107–115. doi: 10.1093/ejo/6.2.107. [DOI] [PubMed] [Google Scholar]
- 11.Deregibus A, Debernardi CL, Persin L, Tugarin V, Markova M. Effectiveness of a fixed anterior bite plane in Class II deep-bite patients. Int J Orthod . 2014;25(1):15–20. [PubMed] [Google Scholar]
- 12.Zaboulian J, Ghassemi B. Fixed functional therapy with an anterior bite plane. Int J Orthod . 2014;25(4):9–12. [PubMed] [Google Scholar]
- 13.Senussi IB, Abdelgader I. Evaluation of changes on maxillo-facial skeleton of Class II patients with deep bite treated with anterior bite plane as a functional appliance. J Adv Res Dent Oral Health . 2019;4(1):1–9. [Google Scholar]
- 14.Woods MG. Sagittal mandibular changes with overbite correction in subjects with different mandibular growth directions: late mixed-dentition treatment effects. Am J Orthod Dentofacial Orthop . 2008;133(3):388–394. doi: 10.1016/j.ajodo.2006.03.037. [DOI] [PubMed] [Google Scholar]
- 15.Egermark I, Magnusson T, Carlsson GE. A. 20-year follow-up of signs and symptoms of temporomandibular disorders and malocclusions in subjects with and without orthodontic treatment in childhood. Angle Orthod . 2003;73(2):109–115. doi: 10.1043/0003-3219(2003)73<109:AYFOSA>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 16.Millett DT, Cunningham SJ, O'Brien KD, Benson PE, de Oliveira CM. Orthodontic treatment for deep bite and retroclined upper front teeth in children Cochrane Database Syst Rev. 2018. 2(2):CD005972. [DOI] [PMC free article] [PubMed]
- 17.Schulz KF, Altman DG, Moher D. CONSORT. 2010 statement: updated guidelines for reporting parallel group randomised trials. J Pharmacol Pharmacother . 2010;1(2):100–107. doi: 10.4103/0976-500X.72352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Al-Salti. M Craniofacial Morphology of Subjects With Neutral Occlusion in Syria [master's thesis] Damascus, Syria: Damascus University; 2000. [Google Scholar]
- 19.McNamara JA, Franchi L. The cervical vertebral maturation method: a user's guide. Angle Orthod . 2018;88:133–143. doi: 10.2319/111517-787.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Wang MK, Buschang PH, Behrents R. Mandibular rotation and remodeling changes during early childhood. Angle Orthod . 2009;79(2):271–275. doi: 10.2319/022808-118.1. [DOI] [PubMed] [Google Scholar]
- 21.McNamara J. Utility arches. J Clin Orthod . 1986;20(7):452–456. [PubMed] [Google Scholar]
- 22.ve İskeletsel BTD. Evaluation of the effects of fixed anterior biteplane treatment on the dental and skeletal structures and masticatory muscles in patients with deep bite. Evaluation . 2010;34(1–2):10–22. [Google Scholar]
- 23.Koo TK, Li MY. A guideline of selecting and reporting intraclass correlation coefficients for reliability research. J Chiropr Med . 2016;15(2):155–163. doi: 10.1016/j.jcm.2016.02.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Jariyavithayakul P, Charoemratrote C. Skeletal and dental changes after lower posterior tooth extrusion in Class II division 1 deep bite short-faced growing patients. APOS Trends Orthod . 2019;9(3):165–171. [Google Scholar]
- 25.Chen Q, Zhang C, Zhou Y. The effects of incisor inclination changes on the position of point A in Class II division 2 malocclusion using three-dimensional evaluation: a long-term prospective study. Int J Clin Exp Med . 2014;7(10):3454. [PMC free article] [PubMed] [Google Scholar]
- 26.Ansari G, Showkatbakhsh R, Malekshah S, Dashti M, Simaei L. The effect of anterior bite plate on deep bite correction during early mixed dentition. Avicenna J Dent Res . 2018;10(2):63–66. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


