In the last decade, the use of high-flow nasal oxygen (HFNO), a technique of noninvasive respiratory support, has become widespread in critically ill patients.
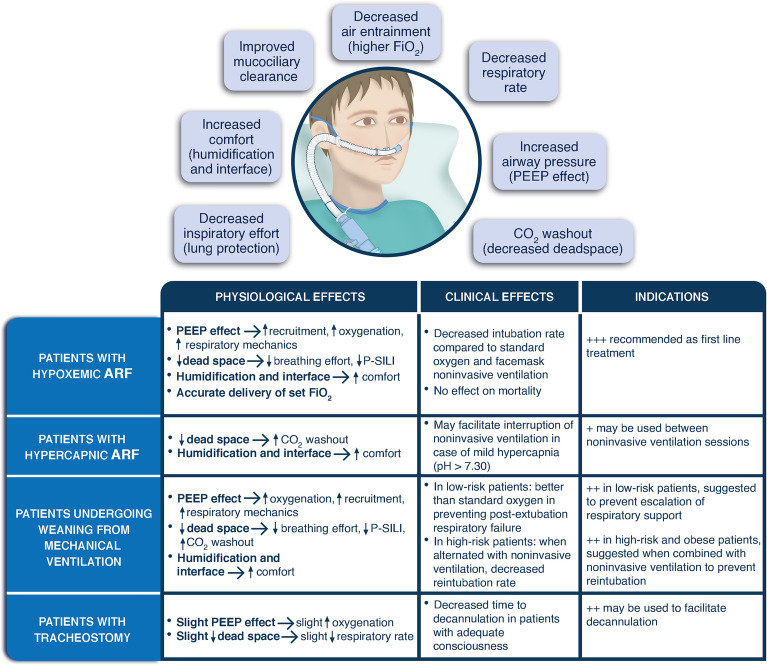
With HFNO, up to 60 L/min of fresh gas flow generated by an air/oxygen blender or a turbine is conditioned by a heated humidifier (temperature 31–37°C, absolute humidity 30–44 mgH2O/L) and administered to the patient through large-bore nasal cannulas. HFNO has several beneficial physiological effects including the accurate delivery of the set FiO2, the washout of anatomical deadspace and the reduction of breathing effort, the increase in positive airway pressure with improvement in lung aeration, in oxygenation and in respiratory mechanics, and the optimization in patients’ comfort (Fig. 1) [1]. As many of the effects of HFNO are flow-dependent, maximum tolerated flows should be delivered to maximize the respiratory support, while temperature should be set according to patient’s comfort and FiO2 should be tailored on the target SpO2.
Fig. 1.
Physiologic/clinical effects and indications for high-flow oxygen. TOP PANEL: main physiological effects of high-flow nasal oxygen are shown. Please note that some of these effects might potentially be linked to others. For example, the amount of pressure generated within the airway might influence carbon dioxide washout (e.g., the higher the pressure, the greater the carbon dioxide washout). As well, the generation of positive airway pressure and carbon dioxide washout provided by the system would both potentially influence the inspiratory effort. BOTTOM TABLE: physiological and clinical effects of high-flow nasal oxygen are detailed, together with its indications in different clinical scenarios. FiO2: inspired fraction of oxygen, CO2 carbon dioxide, ARF acute respiratory failure, PEEP positive end-expiratory pressure, P-SILI patient self-inflicted lung injury
More recently, HFNO delivered through asymmetric nasal cannulas has been proposed with the aim of further enhancing carbon dioxide washout and increasing the airway pressure generation. The physiological effects of this design are currently under investigation.
We hereby summarize the most recent evidence regarding HFNO use in the intensive care unit.
Patients with acute hypoxemic respiratory failure
Recent data suggest that outcome of acute hypoxemic respiratory failure is similar to that of acute respiratory distress syndrome. It has been proposed that widening acute respiratory distress syndrome definition to include patients on HFNO may enable earlier identification of the syndrome [2]. In these patients, noninvasive respiratory support should aim to a balance between the benefit of avoiding sedation and intubation vs. the harmful effects of self-inflicted lung injury and delayed intubation. Thanks to its capability to improve oxygenation and reduce the inspiratory effort, HFNO is widely applied in hypoxemic patients and is currently recommended as the first-line intervention [1]. Several studies in patients with acute hypoxemic respiratory failure, including patients affected by coronavirus disease 2019 (COVID-19), demonstrated that HFNO, as compared to conventional oxygen, reduces the rate of endotracheal intubation, although results on mortality are conflicting [3, 4]. Data from a randomized meta-trial indicate that combining HFNO with prone position sessions lasting at least 8 h per day may further improve the efficacy of the technique [5]. Whether alternating HFNO and noninvasive ventilation sessions with specific settings may provide additional benefit, especially in patients with intense inspiratory effort, is under investigation in ongoing trials (NCT05089695) [6].
Similar to other noninvasive strategies, prompt detection of treatment failure is crucial during HFNO not to delay endotracheal intubation and protective ventilation. The ratio of SpO2/FiO2 to respiratory rate (Respiratory rate – OXygenation, ROX index) has been shown to provide excellent accuracy in early predicting the need for subsequent intubation. Whether a strategy providing early intubation based on the ROX index improves patient-centred outcomes is currently investigated in an ongoing randomized trial (NCT04707729).
Patients with acute hypercapnic respiratory failure
The first-line intervention for the management of acute hypercapnic respiratory failure is facemask noninvasive ventilation. Thanks to the washout effect of the upper airways and the optimal tolerability, applying HFNO instead of conventional oxygen between noninvasive ventilation sessions may provide physiological benefits [7]. In a multicentre trial, HFNO was not inferior to noninvasive ventilation for the initial management of hypercapnic respiratory failure (pH 7.25–7.35) in terms of PaCO2 after 2 h of treatment. However, 32% of patients receiving HFNO required escalation to noninvasive ventilation within 6 h from treatment start to avoid invasive mechanical ventilation [8].
These data suggest that, although noninvasive ventilation remains the cornerstone of treatment for patients with acute hypercapnic respiratory failure, HFNO combined with noninvasive ventilation can be a promising strategy for the management of these patients.
Patients undergoing weaning from mechanical ventilation
Weaning from mechanical ventilation is crucial for the respiratory management of critically ill patients. Re-intubation is needed in a variable 10–40% of patients and is independently associated with increased mortality [9]. Initials trials showed that pre-emptive HFNO may prevent post-extubation respiratory failure and decrease reintubation compared to conventional oxygen in low-risk patients, and may perform as well as pre-emptive noninvasive ventilation in case of a high risk for post-extubation respiratory failure. More recent studies focused on the use of HFNO combined with other interventions in specific populations of patients. These trials indicate that, in low-risk patients, HFNO does not reduce the rate of endotracheal intubation vs. conventional oxygenation devices if patients treated with conventional oxygen can receive escalation of respiratory support with noninvasive ventilation before reintubation [10]. In high-risk patients (e.g., pre-existing respiratory or cardiac disease, or age > 65 years), alternating HFNO with noninvasive ventilation improves outcome compared to HFNO alone, especially in case of obesity [11]. In very high-risk patients, continuous noninvasive ventilation applied for 48 h seems to perform better than HFNO alone [12].
Taken together, these data indicate that HFNO, alone or combined with sessions of noninvasive ventilation, represents the optimal tool for delivering respiratory support to patients after scheduled extubation in the intensive care unit.
Special populations
Immunocompromised patients with acute respiratory failure
Acute hypoxemic respiratory failure remains one of the most frequent reasons for intensive care unit admission in immunocompromised patients. Initial studies addressed the importance of avoiding intubation in these patients, mostly aiming at limiting the infectious complications related to invasive mechanical ventilation. However, due to improvement in cancer treatment and management, outcome of these patients has greatly improved in the last decade. Also, bundles to limit the risks of ventilator-induced lung injury and infectious complications reduced the mortality of invasively ventilated immunocompromised patients. However, almost 50% of intubated patients may die in hospital. Then, the role of noninvasive oxygenation strategies remains an important matter of debate in this setting.
Compared to standard oxygen, noninvasive ventilation was not associated with better outcome in a randomized study involving 374 immunocompromised patients, most of whom had hematologic malignancies. In a randomized trial comparing HFNO to standard oxygen, mortality rates were not different between groups, although a trend toward lower rates of intubation was detected in the HFNO group [13]. A more recent study including 299 patients receiving either facemask noninvasive ventilation and HFNO or HFNO alone did not find any difference in terms of mortality and intubation rates [14].
Altogether, most recent evidence seems to indicate that therapeutic protocols for respiratory support in immunocompromised patients should not be different from those applied to non-immunocompromised patients with acute hypoxemic respiratory failure. In fact, thanks to the improvement in the prevention of infectious complications related to invasive mechanical ventilation and contrarily to what was previously thought, immunocompromised patients do not benefit from an approach aimed at avoiding endotracheal intubation and invasive ventilation at any cost. Studies are warranted to establish whether HFNO alternated or not with noninvasive ventilation delivered with alternative interfaces (e.g., helmet) and specific settings may improve clinical outcome in specific subgroups of immunocompromised patients.
Tracheostomised patients
Through a dedicated interface with an open circuit, high-flow oxygen can also be delivered through a tracheostomy. Tracheal high-flow oxygen at the highest flow rates (50–60 L/min) provides small degree of positive airway pressure, slightly improves oxygenation, and reduces respiratory rate. These effects are, however, significantly milder than those of HFNO at similar flow rates [15]. Clinically, a multicentre trial showed that a strategy combining continuous tracheal high-flow oxygen with suctioning frequency as indicator of readiness for decannulation can shorten the time to decannulation, compared to a strategy based on the intermittent high-flow oxygen application plus capping trials [16].
These data indicate that, in tracheostomised patients, high-flow oxygen delivered through a dedicated interface can result in beneficial physiological effects and can reduce the time to successful decannulation.
Author contributions
All authors contributed to literature search and manuscript drafting. All the authors reviewed the final draft of the manuscript and agreed on submitting it to Intensive Care Medicine.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors. Outside of the submitted work, DLG is supported by research grants by ESICM and SIAARTI.
Data availability
Not applicable.
Declarations
Conflicts of interest
DLG has received payments for travel expenses by Getinge and Air Liquide, personal fees by Gilead, Intersurgical, Fisher and Paykel and GE Healthcare, and discloses a research grant by GE Healthcare. SMM discloses having received speaking fees by GE Healthcare, Masimo, and Aspen.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Rochwerg B, Einav S, Chaudhuri D, et al. The role for high flow nasal cannula as a respiratory support strategy in adults: a clinical practice guideline. Intensive Care Med. 2020;46:2226–2237. doi: 10.1007/s00134-020-06312-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Grasselli G et al (2023) European Society of Intensive Care Medicine Guidelines on Acute Respiratory Distress Syndrome: definition, phenotyping and respiratory support strategies. Intensive Care Med. 10.1007/s00134-023-07050-7 [DOI] [PMC free article] [PubMed]
- 3.Ospina-Tascón GA, Calderón-Tapia LE, García AF, et al. Effect of high-flow oxygen therapy vs conventional oxygen therapy on invasive mechanical ventilation and clinical recovery in patients with Severe COVID-19: a randomized clinical trial. JAMA. 2021;326:2161–2171. doi: 10.1001/jama.2021.20714. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Frat J-P, Quenot J-P, Badie J, et al. Effect of high-flow nasal cannula oxygen vs standard oxygen therapy on mortality in patients with respiratory failure due to COVID-19: the SOHO-COVID randomized clinical trial. JAMA. 2022;328:1212–1222. doi: 10.1001/jama.2022.15613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ehrmann S, Li J, Ibarra-Estrada M, et al. Awake prone positioning for COVID-19 acute hypoxaemic respiratory failure: a randomised, controlled, multinational, open-label meta-trial. Lancet Respir Med. 2021;9:1387–1395. doi: 10.1016/S2213-2600(21)00356-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Grieco DL, Menga LS, Cesarano M, et al. Phenotypes of patients with COVID-19 who have a positive clinical response to helmet noninvasive ventilation. Am J Respir Crit Care Med. 2022;205:360–364. doi: 10.1164/rccm.202105-1212LE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Longhini F, Pisani L, Lungu R, et al. High-flow oxygen therapy after noninvasive ventilation interruption in patients recovering from hypercapnic acute respiratory failure: a physiological crossover trial. Crit Care Med. 2019;47:e506–e511. doi: 10.1097/CCM.0000000000003740. [DOI] [PubMed] [Google Scholar]
- 8.Cortegiani A, Longhini F, Madotto F, et al. High flow nasal therapy versus noninvasive ventilation as initial ventilatory strategy in COPD exacerbation: a multicenter non-inferiority randomized trial. Crit Care. 2020;24:1–13. doi: 10.1186/s13054-020-03409-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Maggiore SM, Battilana M, Serano L, Petrini F. Ventilatory support after extubation in critically ill patients. Lancet Respir Med. 2018;6:948–962. doi: 10.1016/S2213-2600(18)30375-8. [DOI] [PubMed] [Google Scholar]
- 10.Maggiore SM, Jaber S, Grieco DL, et al. High-flow versus Venturimask oxygen therapy to prevent reintubation in hypoxemic patients after extubation: a multicenter randomized clinical trial. Am J Respir Crit Care Med. 2022;206:1452–1462. doi: 10.1164/rccm.202201-0065OC. [DOI] [PubMed] [Google Scholar]
- 11.De Jong A, Bignon A, Stephan F, et al. Effect of non-invasive ventilation after extubation in critically ill patients with obesity in France: a multicentre, unblinded, pragmatic randomised clinical trial. Lancet Respir Med. 2023 doi: 10.1016/S2213-2600(22)00529-X. [DOI] [PubMed] [Google Scholar]
- 12.Hernández G, Paredes I, Moran F, et al. Effect of postextubation noninvasive ventilation with active humidification vs high-flow nasal cannula on reintubation in patients at very high risk for extubation failure: a randomized trial. Intensive Care Med. 2022;48:1751–1759. doi: 10.1007/s00134-022-06919-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Azoulay E, Lemiale V, Mokart D, et al. Effect of high-flow nasal oxygen vs standard oxygen on 28-day mortality in immunocompromised patients with acute respiratory failure: the HIGH randomized clinical trial. JAMA. 2018;320:2099–2107. doi: 10.1001/jama.2018.14282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Coudroy R, Frat J-P, Ehrmann S, et al. High-flow nasal oxygen alone or alternating with non-invasive ventilation in critically ill immunocompromised patients with acute respiratory failure: a randomised controlled trial. Lancet Respir Med. 2022;10:641–649. doi: 10.1016/S2213-2600(22)00096-0. [DOI] [PubMed] [Google Scholar]
- 15.Natalini D, Grieco DL, Santantonio MT, et al. Physiological effects of high-flow oxygen in tracheostomized patients. Ann Intensive Care. 2019;9:114. doi: 10.1186/s13613-019-0591-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hernández Martínez G, Rodriguez M-L, Vaquero M-C, et al. High-flow oxygen with capping or suctioning for tracheostomy decannulation. N Engl J Med. 2020;383:1009–1017. doi: 10.1056/NEJMoa2010834. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Not applicable.