Abstract
We report the case of a 55-year-old woman with multiple comorbid conditions in whom acute left main coronary artery dissection occurred during attempted percutaneous transluminal coronary angioplasty. After the dissection, the patient underwent emergency off-pump coronary revascularization of the left anterior descending coronary artery and ramus intermedius with use of the left internal thoracic artery and a saphenous vein graft, respectively. The procedure was successful.
The risks and benefits of avoiding the extracorporeal circuit in this case of catheterization laboratory salvage are discussed herein, along with some of the concerns about anesthesia that contributed to our decision to perform the operation off-pump.
Key words: Cardiopulmonary bypass, coronary artery bypass/methods/off-pump, coronary dissection, emergency treatment
During the past few years, there has been a resurgence of interest in off-pump (“beating-heart”) coronary artery bypass surgery (OPCAB). 1 This interest has been fueled in part by economic considerations, but, more importantly, OPCAB has been shown to decrease the postoperative morbidity associated with extracorporeal circulation. 2 The reported benefits of avoiding cardiopulmonary bypass (CPB) include a lower incidence of pulmonary complications, 3 renal complications, 4 neurologic complications, 5 and neurocognitive impairment, 6 along with attenuation of the systemic inflammatory response 7,8 and lower transfusion requirements. 9 Which groups of patients represent the best candidates for this technique with respect to safety and benefits is a question that has yet to be answered. There is still controversy over whether emergency operations should be performed without use of the heart-lung machine. 10,11
We report the case of a patient with several comorbid conditions who underwent successful off-pump coronary revascularization after attempted angioplasty led to acute left main coronary dissection.
Case Report
In December 1999, a 55-year-old woman presented at the emergency room, having experienced chest pain and shortness of breath for the past 24 hours. Her medical history included morbid obesity (body mass index, 41 kg/m2), severe asthma, sleep apnea, hypertension, and hypercholesterolemia. There was a strong family history of early coronary artery disease. Her medications included 6 unspecified bronchodilators that were self-administered several times daily, hydrochlorothiazide, and home oxygen (2 L/min). At emergency room admission, the patient underwent laboratory tests that included a complete blood count and coagulation and electrolyte panels, the results of which were all within normal limits. Cardiac enzymes showed an elevated MB isoenzyme fraction of creatine kinase consistent with acute non-Q wave myocardial infarction. An electrocardiogram showed T wave flattening in the lateral leads.
The patient was immediately taken to the cardiac catheterization laboratory, where coronary angiography revealed an 80% stenosis of the left anterior descending artery and a 50% stenosis of the ramus intermedius (Fig. 1A). The plan was to perform percutaneous transluminal coronary angioplasty and stent placement; however, when the guide catheter was advanced, the patient developed acute chest pain. Angiography disclosed a left main trunk dissection extending down the left anterior descending and circumflex coronary arteries (Fig. 1B), with markedly reduced flow in both vessels. The estimated ejection fraction was 0.30 to 0.35. An intraaortic balloon pump was inserted, and the patient was intubated and taken to the operating room for emergency coronary artery bypass grafting. Of note, the patient had received aspirin, 120 U of low-molecular-weight heparin, and abciximab before going to the operating room, and bleeding from all percutaneous vascular access sites was noted.
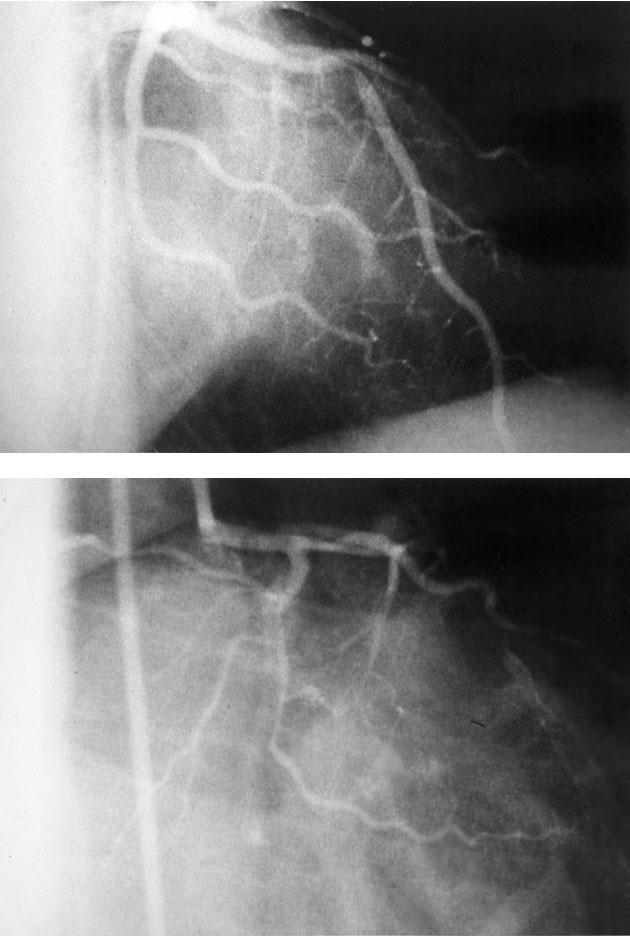
Fig. 1. Selective injection of the left main coronary artery in the right anterior oblique projection showing A) critical narrowing of the left anterior descending artery (arrow), and B) dissection of the left main coronary artery (arrow), with poor opacification of the left anterior descending artery and the circumflex coronary artery.
Entering the operating room, the patient underwent placement of invasive monitors, including a brachial arterial line and a pulmonary artery catheter. Her hemodynamic values included blood pressure of 110/50 mmHg; heart rate, 110 to 120 beats/min; pulmonary artery pressure, 33/22 mmHg; and cardiac index, 1.57 L · min−1 · m−2 on intra-aortic balloon pump and low-dose inotropic support (dopamine at 3 μg · kg−1 · min−1) that had been started in the catheterization laboratory. Her condition was further stabilized in the operating room with an epinephrine infusion (0.05 μg · kg−1 · min−1) and optimization of her volume sta-tus (correction of hypovolemia secondary to blood loss from coagulopathy and catheterization), which increased her cardiac index to 2.2 L · min−1 · m−2.
We decided to proceed with off-pump coronary artery bypass grafting because of the patient's ongoing coagulopathy from administration of anticoagulants and antiplatelet agents, along with the obesity and pulmonary history. Heparin (2,000 U) was administered, which brought the activated clotting time up to 306 seconds (target value, 300 seconds) from a baseline value of 171 seconds. She underwent grafting of the left anterior descending coronary artery and ramus intermedius through a midline sternotomy, with the left internal thoracic artery and a saphenous vein graft, respectively, as conduits. The circumflex artery was not graftable because of small diameter (<1 mm) and extension of the dissection flap. A suction cardiac stabilizer system (Octopus® 2, Medtronic, Inc.; Minneapolis, Minn) was used to immobilize the anastomotic sites, and a Silastic snare was used for proximal occlusion of the target vessels. The patient's hemodynamic values improved dramatically after reperfusion of the left anterior descending artery. The total estimated blood loss at the end of the procedure was 600 cc. The patient had received platelets (20 U), fresh frozen plasma (2 U), and packed red blood cells (2 U), intraoperatively. After chest closure, the cardiac index was 2.3 L · min−1 · m−2 with the patient on intra-aortic balloon pump support alone.
After intensive pulmonary therapy and broncho-dilator therapy, the patient was extubated on the 1st postoperative day. She was discharged from the intensive care unit on postoperative day 3 and left the hospital on day 5. There were no bleeding complications. She had 1 episode of atrial fibrillation, which was treated successfully with digoxin. A transthoracic echocardiogram on postoperative day 3 showed normal chamber size and an estimated ejection fraction of 0.55 to 0.60. At postoperative follow-up 1 month later, she remained asymptomatic. She continues to do well from a cardiac standpoint.
Discussion
Increasingly, off-pump coronary artery bypass sur-gery is becoming accepted as a viable alternative to conventional revascularization with CPB and cardioplegia. The development of cardiac stabilization devices, as well as aggressive anesthetic management strategies, has made complete revascularization of the heart without CPB feasible for experienced surgeons and anesthesiologists to perform. 12 Cardiopulmonary bypass has adverse systemic effects, which include activation of the systemic inflammatory response, 7,8 coagulopathy, 7,8 and pulmonary, 3 neurologic, 5 and neurocognitive 6 dysfunction. Early results of studies examining patient outcomes after OPCAB surgery are promising and show some clear advantages over conventional techniques. 13 Certain patients presenting for coronary artery bypass grafting who are at increased risk for morbidity associated with extracorporeal circulation may prove to be the most suitable candidates in terms of risk-to-benefit ratio. 14–16 There are few data, however, concerning the use of the off-pump approach in emergency situations. 10
The patient presented in this report had several comorbid factors that placed her at increased risk for complications associated with anesthesia and CPB. Among these complications was a pharmacological-ly induced coagulopathy (aspirin, low-molecular-weight heparin, and abciximab) that would have been exacerbated by use of the heart-lung machine.
This patient's size was also of concern in terms of respiratory management. Morbid obesity imposes ventilatory restriction, with reductions in expiratory reserve volume, vital capacity, and functional residual capacity. With such a patient in the supine position, atelectasis can develop, as well as ventilation– perfusion mismatch. Cardiac surgery further alters ventilatory function, and anesthetic effects are additive. 17 In addition, obesity, emergency cardiac sur-gery, and prolonged CPB time have been shown to be risk factors for postoperative hypoxemia. 18 The elevated airway pressures that can occur during ventilation of morbidly obese patients (as a result of pressure on the diaphragm by intra-abdominal contents) can have severe hemodynamic consequences, including reduced venous return leading to low cardiac output. Such circumstances can affect both on-pump and off-pump procedures.
This patient had severe asthma, making her intraoperative ventilatory management even more challenging. The anesthesia machine used in this instance was equipped with a pressure-control ventilator, which, for this patient, was superior to the standard volume-control ventilator that is routinely used. Had this machine not been available, use of an intensive-care-unit ventilator and a total intravenous anesthetic technique would have been an acceptable alternative.
Being a female is considered by most to be an independent risk factor for patients undergoing cardiac surgery and has been associated with longer intubation times and hospital lengths-of-stay. 19,20 In this instance, the sex of the patient was not a major consideration in the decision to perform the surgery off pump; however, this additional factor could have led to increased postoperative morbidity, particularly respiratory complications.
We decided to proceed with OPCAB surgery in this patient on the basis of several factors, including the surgeon's experience and comfort level with the technique (>200 OPCAB procedures), the anesthesiologist's ability to stabilize the patient and maintain acceptable hemodynamics during grafting, and the patient's ongoing coagulopathy, obesity, and reactive airways disease. In the absence of such risk factors, we might have given greater consideration to a more conventional approach.
Off-pump coronary artery bypass surgery is now considered by many to be an acceptable alternative to coronary artery bypass grafting with CPB. Early data on graft patency are promising, with a 97.7% patency rate reported in 1 series of 125 consecutive patients at Emory University. 21 Whether OPCAB surgery should be used in patients presenting for emergency surgery is less clear, as few data are available for comparison. In our patient, emergency OPCAB surgery was successful for treatment of acute left main coronary dissection after failed angioplasty. We conclude that off-pump coronary artery bypass surgery should be considered in carefully selected patients presenting for emergency surgery when adequate hemodynamics can be maintained—particularly when comorbid conditions in association with cardiopulmonary bypass might constitute an unacceptable risk to the patient.
Footnotes
Address for reprints: Reprints will not be available.
References
- 1.Spooner TH, Hart JC, Pym J. A two-year, three institution experience with the Medtronic Octopus: systematic off-pump surgery. Ann Thorac Surg 1999;68:1478–81. [DOI] [PubMed]
- 2.Boyd WD, Desai ND, Del Rizzo DF, Novick RJ, McKenzie FN, Menkis AH. Off-pump surgery decreases postoperative complications and resource utilization in the elderly. Ann Thorac Surg 1999;68:1490–3. [DOI] [PubMed]
- 3.Buffolo E, de Andrade CS, Branco JN, Teles CA, Aguiar LF, Gomes WJ. Coronary artery bypass grafting without cardiopulmonary bypass. Ann Thorac Surg 1996;61:63–6. [DOI] [PubMed]
- 4.Ascione R, Lloyd CT, Underwood MJ, Gomes WJ, Angelini GD. On-pump versus off-pump coronary revascularization: evaluation of renal function. Ann Thorac Surg 1999;68:493–8. [DOI] [PubMed]
- 5.Murkin JM, Boyd WD, Ganapathy S, Adams SJ, Peterson RC. Beating heart surgery: why expect less central nervous system morbidity? Ann Thorac Surg 1999;68:1498–501. [DOI] [PubMed]
- 6.Diegeler A, Hirsch R, Schneider F, Schilling LO, Falk V, Rauch T, Mohr FW. Neuromonitoring and neurocognitive outcome in off-pump versus conventional coronary bypass operation. Ann Thorac Surg 2000;69:1162–6. [DOI] [PubMed]
- 7.Wan S, Izzat MB, Lee TW, Wan IY, Tang NL, Yim AP. Avoiding cardiopulmonary bypass in multivessel CABG reduces cytokine response and myocardial injury. Ann Thorac Surg 1999;68:52–7. [DOI] [PubMed]
- 8.Ascione R, Lloyd CT, Underwood MJ, Lotto AA, Pitsis AA, Angelini GD. Inflammatory response after coronary revascularization with or without cardiopulmonary bypass. Ann Thorac Surg 2000;69:1198–204. [DOI] [PubMed]
- 9.Nader ND, Khadra WZ, Reich NT, Bacon DR, Salerno TA, Panos AL. Blood product use in cardiac revascularization: comparison of on- and off-pump techniques. Ann Thorac Surg 1999;68:1640–3. [DOI] [PubMed]
- 10.Hirose H, Amano A, Yoshida S, Nagao T, Sunami H, Takahashi A, Nagano N. Emergency off-pump coronary artery bypass grafting under a beating-heart. Ann Thorac Cardiovasc Surg 1999;5:304–9. [PubMed]
- 11.Perrault LP, Menasche P, Peynet J, Faris B, Bel A, de Chaumaray T, et al. On-pump, beating-heart coronary artery operations in high-risk patients: an acceptable trade-off? Ann Thorac Surg 1997;64:1368–73. [DOI] [PubMed]
- 12.Bredee JJ, Jansen EW. Coronary artery bypass grafting without cardiopulmonary bypass. Curr Opin Cardiol 1998; 13:476–82. [DOI] [PubMed]
- 13.Cartier R. Systematic off-pump coronary artery revascularization: experience of 275 cases. Ann Thorac Surg 1999;68: 1494–7. [DOI] [PubMed]
- 14.Kappert U, Gulielmos V, Knaut M, Cichon R, Schneider J, Schueler S. The application of the Octopus stabilizing system for the treatment of high risk patients with coronary artery disease. Eur J Cardiothorac Surg 1999;16(Suppl 2): S7–9. [PubMed]
- 15.Capdeville M, Lee JH, Abdel-Hady K. Off-pump coronary artery bypass surgery in a patient with a symptomatic intracranial mass. J Cardiothorac Vasc Anesth 2001;15(3): 352–5. [DOI] [PubMed]
- 16.Stamou SC, Dangas G, Dullum MK, Pfister AJ, Boyce SW, Bafi AS, et al. Beating heart surgery in octogenarians: perioperative outcome and comparison with younger age groups. Ann Thorac Surg 2000;69:1140–5. [DOI] [PubMed]
- 17.Weissman C. Pulmonary function after cardiac and thoracic surgery. Anesth Analg 1999;88:1272–9. [DOI] [PubMed]
- 18.Rady M, Ryan T, Starr NJ. Early onset of acute pulmonary dysfunction after cardiovascular surgery: risk factors and clinical outcome. Crit Care Med 1997;25:1831–9. [DOI] [PubMed]
- 19.Capdeville M, Lee JH, Taylor AL. Effect of gender on fast track recovery after coronary artery bypass graft surgery. J Cardiothorac Vasc Anesth 2001;15(2):146–51. [DOI] [PubMed]
- 20.Butterworth J, James R, Prielipp R, Cerese J, Livingston J, Burnett D. Female gender associates with increased duration of intubation and length of stay after coronary artery surgery. CABG Clinical Benchmarking Database Participants. Anesthesiology 2000;92:414–24. [DOI] [PubMed]
- 21.Puskas JD, Wright CE, Ronson RS, Brown WM 3rd, Gott JP, Guyton RA. Clinical outcomes and angiographic patency in 125 consecutive off-pump coronary bypass patients. Heart Surg Forum 1999;2:216–21. [PubMed]


