Abstract—
The cGAS-STING signaling pathway senses the presence of cytosolic DNA, induces strong type I interferon responses, and enhances inflammatory cytokine production, placing it as an important axis in infection, autoimmunity, and tumor immunity. Recent studies have shown that the abnormalities and/or dysfunctions of cGAS-STING signaling are closely related to the pathogenesis of skin diseases and/or cancers. Additionally, a variety of new therapeutics targeting the cGAS-STING signaling are in development for the treatment of skin disorders. However, the precise molecular mechanisms of cGAS-STING-mediated cutaneous disorders have not been fully elucidated. In this review, we will summarize the regulatory roles and mechanisms of cGAS-STING signaling in skin disorders and recent progresses of cGAS-STING-related drugs as well as their potential clinical applications.
KEY WORDS: cGAS-STING signaling, skin diseases, melanoma, molecular drugs.
INTRODUCTION
Cutaneous disorders, also called skin disorders or skin diseases, is an umbrella term for a variety of skin conditions. Cutaneous disorders can be divided into two broad categories, including the non-cancerous skin diseases and the cancerous skin disorders or skin cancers. The non-cancerous skin diseases are mainly composed of acne, atopic dermatitis, psoriasis, etc., while the skin cancers are mainly composed of basal cell carcinoma, squamous cell carcinoma, and melanoma [1–3]. Different cutaneous disorders vary greatly in symptoms and severity. Some of the cutaneous disorders can be temporary and/or painless, whereas the others can be permanent and/or painful [4–7]. Some of the cutaneous disorders only affect people’s appearance, while the others can be life-threatening if left untreated [8]. Thus, it is important to understand the molecular mechanisms and therapeutic strategies targeting cutaneous disorders. Recently, accumulating evidence have shown that cGAS-STING signaling plays crucial roles in the pathogenesis of cutaneous disorders [9–11]. In addition, molecules or therapeutics targeting the cGAS-STING pathway represent novel strategies for the treatment of skin disorders [12]. Therefore, we systematically review the regulatory roles of cGAS-STING signaling in cutaneous disorders and summarize the recent progresses of cGAS-STING-related therapeutics in the treatment of cutaneous disorders.
THE cGAS-STING SIGNALING PATHWAY
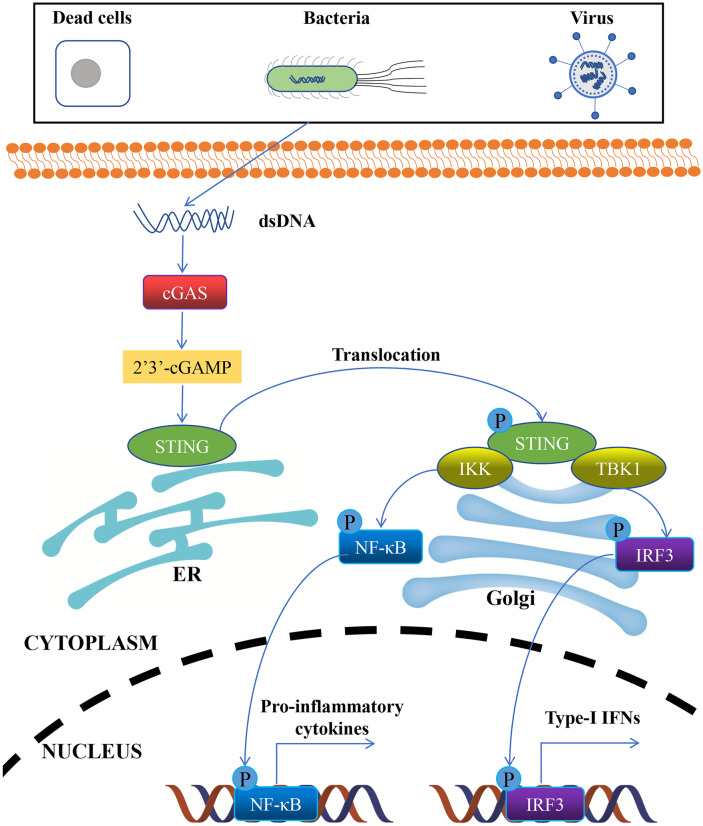
The cGAS-STING signal axis is mainly composed of the synthase for the second messenger cyclic GMP-AMP synthase (cGAS) and the cyclic GMP-AMP receptor stimulator of interferon genes (STING) [13, 14]. The cGAS-STING pathway can detect pathogen DNAs and sense microbial DNAs [15, 16]. Moreover, it can also be activated by endogenous DNAs, which in turn induces innate immunity involving type I interferon [15–17] (Fig. 1). Exogenous/endogenous DNAs introduced into the host cytoplasm by microbial infections, DNA viruses, damaged mitochondria or nucleus, dying cells, and genomic instability [18–22], also known as cytosolic DNAs, are recognized as pathogen-associated molecular patterns by cGAS, which subsequently binds to the cytosolic DNAs in a DNA sequence-independent manner [23, 24]. Once binds to the cytosolic DNA, cGAS facilitates the production of a special cyclic dinucleotide called cGAMP, from GTP and ATP [15, 23, 24]. cGAMP is an endogenous second messenger, which holds high affinity for STING [25, 26]. The binding of cGAMP to STING induces the activation and oligomerization of STING on ER, which is accompanied by the translocation of STING to the Golgi apparatus [27, 28], where it recruits and phosphorylates kinases tank binding kinase 1 (TBK1) and IκB kinase (IKK) [29–32]. Activated TBK1 and IKK recruit and phosphorylate interferon regulatory factor 3 (IRF3) and nuclear factor kappa-light-chain-enhancer of activated B cells (NF-κB) at the C-terminal tail of STING [29, 30, 33]. Then, phosphorylated IRF3 and NF-κB enter the nucleus, leading to potently increased type I IFN and pro-inflammatory cytokine/chemokine production, separately [33].
Fig. 1.
A diagram of the cGAS-STING signaling pathway. DNAs from dead cells, bacteria, or virus are introduced into the cytoplasm, and sensed by cGAS as cytosolic DNAs or dsDNAs. cGAS subsequently binds to the dsDNAs in a DNA sequence-independent manner. Once binds to the dsDNA, cGAS catalyzes the synthesis of cGAMP, which is an endogenous second messenger that holds high affinity for STING. The binding of cGAMP to STING induces the activation and oligomerization of STING on ER, which is accompanied by the translocation of STING to the Golgi, where it recruits and phosphorylates kinases TBK1 and IKK. Activated TBK1 and IKK recruit and phosphorylate IRF3 and NF-κB at the C-terminal tail of STING. Then, phosphorylated IRF3 and NF-κB translocate into the nucleus, leading to increased transcription of IFN-I and inflammation-related genes, respectively.
THE REGULATORY ROLE OF cGAS-STING SIGNALING IN CUTANEOUS DISEASES
The cGAS-STING pathway is an important part of the innate immunity, and its main function is to detect the presence of cytosolic DNAs and trigger the expression of inflammation-related genes, resulting in the activation of host defense mechanisms. Therefore, it plays important roles in inflammatory response and autoimmunity [15–17], while its dysfunction may lead to multiple cutaneous diseases [34–37].
STING is the most important downstream modulator of cGAS-STING pathway, which engages in recognizing cytosolic DNA and activating innate immune. Upon activation, STING induces type I interferon response, which is crucial for the pathogenesis of psoriasis [38]. Meanwhile, it was reported that STING and its downstream targets were upregulated in the lesional skins of psoriasis patients when compared with skin samples of healthy people [39], revealing the potential involvement of STING dysregulation in psoriasis pathogenesis. Interestingly, STING deficiency alleviates psoriatic inflammation in IMQ-induced mouse model [40]. Furthermore, STING induces NF-κB activation and subsequent expression of inflammatory factors in keratinocytes (KCs) [40]. Finally, 5,6-dimethylxanthenone-4-acetic acid (DMXAA), a STING agonist, aggravates psoriatic symptom and inflammation, whereas H-151, a STING antagonist, displays anti-inflammatory activity in IMQ-induced psoriatic mice [39, 40]. Thus, STING activation contributes to the psoriatic inflammation and targeting STING represents a potential therapeutic approach to psoriasis.
Psoriasis and type 2 diabetes mellitus (T2DM) share similar inflammatory pathways in their pathogenesis. Meanwhile, the activation of STING-IRF3 pathway is detected in both cellular and mouse model of psoriasis comorbidities with T2DM [41]. Additionally, C-176, the STING inhibitor, ameliorates the inflammation in IMQ-induced diabetic mice [41], indicating that STING could be targeted for psoriasis comorbidities with T2DM. However, it remains unclear the precise mechanism that the STING manifestation regulates the pathogenesis of psoriasis comorbidities with T2DM.
Recently, accumulating evidence has demonstrated that the imbalance and dysbiosis of cutaneous microbiota can result in inflammatory skin diseases, such as atopic dermatitis, acne vulgaris, and psoriasis [42–45]. Mechanistically, the skin microbiota promotes the expression of endogenous retroviruses (ERVs) and triggers the activation of skin immunity, which is cGAS-STING pathway dependent. Additionally, cGAS-STING signaling is required for skin microbiota-induced immune response, since the number and activity of specific T cell subsets significantly decreased in cGAS/STING deletion mice compared to control mice in the presence of microbiota stimulation. Thus, the cGAS-STING signaling plays an essential role in the microbiota-induced cutaneous inflammation [46].
THE REGULATORY ROLE OF cGAS-STING SIGNALING IN CUTANEOUS CANCERS
Skin cutaneous melanoma (SKCM) is a rare but the most lethal form of skin cancers, which accounts for 75% of all skin cancer deaths [8]. Moreover, melanoma is one of the most malignancy, invasive, and therapy-resistant skin cancers [8, 47]. Due to its high mortality, we will take cutaneous melanoma as an example to review the recent progress of cGAS-STING pathway in skin cancers.
STING Dysfunction Contributes to Melanoma Pathogenesis
As the most important downstream component of cGAS-STING pathway, the STING is recurrently suppressed by epigenetic silencing in human melanomas and melanoma cells [9, 48–50], where this event may enable immune escape after DNA damage. For instance, Xu et al. reported that STING was epigenetically inhibited by the histone modulator H3K27me3, resulting in decreased type I IFN production in melanomas [50]. Interestingly, the inhibition of STING leads to decreased MHC I expression and loss of tumor antigenicity, which are indispensable for the melanoma-immune evasion [9, 48–50]. In vitro, melanoma cell-derived DNA could trigger IFN-β production and dendritic cell activation via STING and IRF3 signaling [51]. In vivo, melanoma tumor-infiltrating APCs uptake tumor-derived DNA and produce IFN-β in a STING-dependent way [51]. Thus, the melanoma-intrinsic STING impairment results in reduced type I IFN production and systemic immune suppression in melanoma, demonstrating a novel mechanism involving STING dysfunction in melanoma malignancy.
Activation of cGAS-STING Pathway Contributes to Cancer Therapy in Melanoma
Since the persistently suppressed cGAS-STING signaling plays critical roles in melanoma pathogenesis, its activation may represent a novel therapeutic for melanoma treatment. Recent data indicated that ATM inhibition (booster of cellular innate immunity) potently activated the cGAS-STING pathway and enhanced antitumor immunity in melanoma [52]. Mechanistically, ATM inhibitor increased the cytoplasmic release of mtDNA, resulting in the cGAS-STING activation and lymphocyte infiltration into the tumor microenvironment [52]. Recently, Shae et al. designed a STING-activating nanoparticle (STING-NP), which can significantly enhance the therapeutic efficacy of cGAMP (a natural STING agonist) in melanoma [53], highlighting the potential of STING activation in melanoma treatment.
Carboplatin is a cisplatin analog used for the treatment of various cancers. In the human melanoma cells, carboplatin activates TREX1/cGAS/STING axis, leading to cell growth arrest and cellular apoptosis [54]. Thus, targeting of cGAS-STING pathway using carboplatin could be a therapeutic alternative to melanoma. However, it is important to seriously consider the side effect of carboplatin in melanoma treatment.
Malignant melanoma escaping immunosurveillance is a major obstacle in melanoma immunotherapy. It was previously reported that cyclic diguanylate monophosphate (c-di-GMP, a ligand of the STING signaling) potentiated the immunogenicity and antitumor effects against mouse melanoma when combined with a peptide vaccine [55]. Additionally, c-di-GMP efficiently induced the type I IFN production and exhibited significant antitumor immunity in metastatic mouse melanoma model when loaded in YSK05 liposomes (c-di-GMP/YSK05-Lip) [56]. Moreover, c-di-GMP/YSK05-Lip potently promoted the infiltration and activation of NK cells [56], indicating that STING activation represents a potential immunotherapeutic against malignant melanomas.
Activation of cGAS/STING Pathway Helps to Overcome Chemotherapy/Immunotherapy Resistance in Melanoma
Melanoma is the most aggressive type in skin cancers, which may get resistance to the conventional chemotherapy, resulting in its poor prognosis [57–59]. Abrogation of NRF2 and enhancement of oxidative stress is the primary cause for BRAF inhibitor resistance in melanoma [60, 61]. Meanwhile, type I IFNs negatively regulate NRF2 response [62]. Theoretically, type I IFN production upon STING activation could sensitize melanoma cells to the clinically used BRAF inhibitors. Recently, dimeric amino-benzimidazole (diABZI, a newly developed STING agonist [63]), was found to downregulate NRF2-dependent anti-oxidative responses and exhibit antitumor effects in melanoma when combined with BRAF inhibitors [64], revealing that STING activation is a potential alternative in the treatment of chemotherapy-resistant melanoma.
Resistance to immune checkpoint inhibitors is another major obstacle in melanoma therapy, especially immunotherapy [65–68]. Recently, accumulating evidence has demonstrated that activation of cGAS-STING signaling efficiently induced antitumor effect via the activation of tumor immunity [69, 70]. Meanwhile, the STING agonist c-di-GMP was shown to enhance cancer immunotherapy against metastatic melanoma [56, 71]. Moreover, the combination of c-di-GMP and anti-PD-1 exerted a synergistic antitumor immunity in an anti-PD-1-resistant mouse melanoma model [72], providing a clue that targeting cGAS-STING pathway is a promising candidate for immunotherapy-resistant melanoma.
RESEARCH PROGRESS IN TARGETED THERAPY FOR cGAS-STING PATHWAY
As summarized above, the cGAS-STING pathway is one of the currently most studied pathways that play important roles in inflammatory skin diseases and cutaneous melanomas. It is also widely accepted that modulating the cGAS-STING pathway holds promising therapeutic potential for fighting inflammatory diseases and/or cancers, even though it is still necessary to further understand the full potential of this pathway in these diseases.
cGAS Antagonists
cGAS is a sensor of aberrant pathogen DNAs or self-DNAs, and plays essential roles in innate immunity against infection and cellular damage. Moreover, its abnormal activation can lead to serious autoimmune disorders, whereas its inhibition may act anti-inflammation. Therefore, a variety of strategies have been adopted to develop cGAS antagonists (Table 1). Through high-throughput compound screenings, Lama et al. identified a subset of human cGAS-specific small-molecule inhibitors with high specificity and potency [73], which could be potentially used in cGAS-related disorders. The limitation of this study lies that there are few data supporting the clinical use of these molecular inhibitors. Recently, Vincent et al. discovered a cGAS inhibitor called RU.521, which could potently and selectively inhibit cGAS signaling, leading to the reduction of constitutive IFN production in macrophages from a mouse model of Aicardi-Goutières syndrome (AGS) [74]. More recently, the same research team reported that RU.521 is capable of inhibiting both mouse and human cGAS in vitro [75]. Additionally, RU.521 suppressed the production of dsDNA-induced intracellular cGAMP in a dose-dependent manner [75], validating its potential for pre-clinical use in autoimmune diseases. Coincidentally, Tan et al. also identified a tetrahydro-γ-carboline derivative called Compound 25, potently inhibiting both human and mouse cGAS [76]. More importantly, Compound 25 demonstrated superior in vivo anti-inflammatory effects in the lipopolysaccharide-induced mouse model [76], providing evidence for its future use as an anti-inflammatory treatment.
Table 1.
cGAS Antagonists Used in Inflammatory or Autoimmune Diseases
| Compounds/Molecules | Experimental models | Functions/Biological effects | Refs |
|---|---|---|---|
| Human cGAS-specific inhibitors (G108, G140, and G150) | Human THP1 and primary macrophages | These compounds specifically and potently inhibit human cGAS activity in macrophages | [73] |
| RU.521 | Macrophages from AGS mouse model, THP1 cells, and primary human PBMCs | RU.521 selectively and actively inhibits mouse and human cGAS-mediated signaling and reduces constitutive interferon synthesis in macrophages from a mouse model of AGS | [74, 75] |
| Compound 25 | Lipopolysaccharide (LPS)-induced mouse model | Compound 25 potently inhibits both human and mouse cGAS. Meanwhile, Compound 25 demonstrates superior anti-inflammatory effects in the LPS-induced mouse model | [76] |
| Aspirin | AGS patient cells and AGS mouse model | Aspirin directly acetylates cGAS and inhibits cGAS-mediated immune activation | [79] |
| Suramin | THP1 cells | In THP1 cells, suramin displaces the bound DNA from cGAS and reduces the IFN-β production | [81] |
| A151 | TREX1-deficient monocytes and mouse model of stroke | A151 inhibits the activation of cGAS in TREX1-deficient monocytes and dampens immune response in the mouse stroke model | [82, 83] |
| Perillaldehyde (PAH) | AGS mouse model | Administration of PAH markedly ameliorates self-DNA-induced autoinflammatory responses in a AGS mouse model | [84] |
| EGCG and RSVL | AGS mouse model | EGCG and RSVL inhibit the cGAS activation through disrupting the G3BP1-cGAS complexes, alleviating the autoinflammatory responses in the AGS mouse model | [85, 86] |
| 2′OMe ASOs | THP1 cells, human bone marrow-derived mesenchymal stem cells, etc. | 2′OMe ASOs inhibit cGAS sensing in a sequence-dependent manner | [87] |
Aspirin is a nonsteroidal anti-inflammatory drug, which is commonly used to reduce pain, fever, and/or inflammation [77, 78]. Interestingly, aspirin can effectively suppress autoimmunity in AGS patient cells and AGS mouse model [79]. Mechanistically, aspirin directly acetylates cGAS and inhibits cGAS-mediated immune activation [79]. Suramin is a nucleic acid analog and essential drug for anti-parasitic treatment [80]. In THP1 cells, suramin displaces the bound DNA from cGAS and reduces the IFN-β production through inhibiting the cGAS enzymatic activity [81], suggesting its potential use in the treatment of chronic inflammation. A151 is a synthetic oligodeoxynucleotide, which has recently been shown to inhibit the activation of cGAS [82]. In addition, A151 effectively inhibits cGAS activation in the TREX1-deficient monocytes [82]. Importantly, A151 administration dampens immune response in a mouse model of stroke [83], representing a potential therapeutic opportunity for autoimmune/inflammatory diseases. Perillaldehyde (PAH) is a natural compound derived from Perilla frutescens, which suppresses cytosolic DNA-induced innate immunity by directly inhibiting cGAS activity [84]. Meanwhile, PAH administration markedly ameliorates the autoinflammatory responses in a AGS mouse model, suggesting its therapeutic potential toward the cGAS-mediated autoimmunity. Interestingly, two natural chemicals that are abundant and easy to acquire from plants, called epigallocatechin gallate (EGCG) and resveratrol (RSVL), inhibit the cGAS activation through blocking the GTPase-activating protein SH3 domain-binding protein 1 (G3BP1) and disrupting the G3BP1-cGAS complexes, effectively alleviating the autoinflammatory responses in the AGS mouse model and providing a potential treatment for cGAS-related autoimmune diseases [85, 86].
Unlike the abovementioned cGAS inhibitors, Valentin et al. identified a highly potent cGAS inhibitor, called 2′-O-methyl gapmer antisense oligonucleotides (2′OMe ASOs), which could inhibit cGAS sensing in a sequence-dependent manner, paving the way for the development of oligonucleotide-based cGAS inhibitors [87].
In summary, the identification of specific and potent cGAS inhibitors contributes to the development of drugs for cGAS-mediated diseases, like AGS. However, few attentions were paid to the regulatory role or therapeutic potential of these novel inhibitors in inflammatory skin diseases mediated by cGAS dysfunction.
STING Agonists
STING Agonists with Antiviral Properties
STING is an important signal transducer in innate immunity and plays a central role in the initiation of host defense against pathogens. Upon activation, it induces type I IFN response, which is critical for the control of certain microbial infections, revealing the therapeutic potential of STING agonists against infectious diseases. Herpes simplex virus 1 (HSV-1) is a double-stranded DNA virus that presents in approximately 40–90% of the population globally [88, 89]. It is reported that 5,6-dimethylxanthenone-4-acetic acid (DMXAA, a STING agonist) can significantly protect peripheral and central nervous systems against HSV-1 infection [90]. Meanwhile, administration of DMXAA inhibits viral replication through increasing type I IFN production [90], demonstrating the potential of STING agonist for immunotherapy against DNA virus.
In addition to its role in restricting DNA viral infection, STING activation also holds antiviral effects against RNA virus. In Zhu’s studies, the previously discovered STING agonist diABZI potently inhibited the replication of parainfluenza virus type 3 and human rhinovirus 16 [91], two representative respiratory RNA viruses, expanding the use of STING agonists in viral infections. Recently, diABZI was found to restrict severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) viral replication by transiently stimulating IFN signaling in primary human bronchial epithelial cells and in mice [92]. Thus, activation of STING may represent a promising therapeutic strategy to control multiple viral infections, including SARS-CoV-2.
Cyclic Dinucleotide-Based STING Agonist in Cancer Therapy
As discussed in the “STING Dysfunction Contributes to Melanoma Pathogenesis” section, STING signaling is recurrently suppressed in melanoma cells, which usually leads to the tumor malignancy. Therefore, pharmacological activation of STING represents a promising therapeutic for melanoma (Table 2). It was reported that intratumoral injection of cyclic dinucleotide GMP-AMP (cGAMP, a natural STING agonist) potently enhanced antitumor responses in mouse model of melanoma [93]. Moreover, intratumoral injection of cGAMP normalized tumor vasculatures in implanted and spontaneous mouse cancer models [94]. Notably, cGAMP synergizes with VEGFR2 blockade or immune checkpoint blockade (PD-1, PD-L1, or CTLA-4) to further enhance antitumor effects [94, 95], supporting a rationale for the combination of STING-based therapy and antiangiogenic therapy and/or immunotherapy.
Table 2.
STING Agonists Used in Cancer Therapy
| Compounds/Molecules | CDN-based (Yes or No) | Study models | Functions/Biological effects | Refs |
|---|---|---|---|---|
| cGAMP | Yes | Mouse bearing B16F10 melanoma tumor | Intratumoral injection of cGAMP potently enhances antitumor responses in mouse model of melanoma. Moreover, cGAMP synergizes with immune checkpoint blockade to further enhance antitumor effects | [93–95] |
| ADU-S100 | Yes | Pancreatic cancer-bearing mice, glioblastoma mouse models, phase I clinical study, and melanoma mouse model | ADU-S100 activates systemic antitumor response, modulates tumor microenvironment, and inhibits tumor growth in different mouse cancer models. Meanwhile, ADU-S100 is well tolerated in patients with advanced cancers | [96–100] |
| IACS-8803 and IACS-8779 | Yes | B16 murine model of melanoma | IACS-8803 and IACS-8779 show robust and superior tumor regression in the murine melanoma model when compared with ADU-S100 | [101, 102] |
| DMXAA | No | L929 cells, pancreatic tumor-bearing mice, and breast cancer/colon cancer/melanoma mouse models | DMXAA changes the tumor immune architecture in the pancreatic cancer mouse model. Moreover, DMXAA induces strong anti-tumor immunity in a murine melanoma model | [103–105] |
| MSA-2 | No | Advanced MC38 tumor model and melanoma xenograft mouse model | MSA-2 is orally available, which synergizes with anti-PD-1 therapy for durable antitumor immunity in multiple mouse models | [106] |
| 5-Fluorouracil (5-FU) | No | Murine colon and melanoma tumor models | 5-FU effectively reduces tumor burden by activating the cancer intrinsic STING in murine colon and melanoma tumors | [107] |
ADU-S100 is a synthetic cyclic dinucleotide that activates both human and mouse STING [96]. In a pancreatic cancer-engrafted mouse model, ADU-S100 dramatically reduces local and distal tumor burden and activates systemic antitumor responses [97], revealing the therapeutic potential of STING agonist in cancer immunotherapy. Moreover, ADU-S100 promotes the inflammatory cytokine secretion and modulates the tumor microenvironment in glioblastoma [98]. Furthermore, a phase I clinical study regarding ADU-S100 showed that ADU-S100 was well tolerated in patients with advanced/metastatic cancers, with the systemic immune activation observed [99]. Most importantly, intratumoral delivery of low-dose ADU-S100 leads to tumor growth inhibition in established melanoma mouse model [100], suggesting its potential use in melanoma treatment.
IACS-8803 is a synthetic CDN analog, which shows superior potency in STING activation and antitumor immunity both in vitro and in vivo, as compared with natural CDNs [101]. Moreover, IACS-8803 and IACS-8779, two synthetic STING agonists, show robust and superior tumor regression in the B16 murine model of melanoma when compared with the clinical benchmark ADU-S100 [102]. However, the precise mechanisms of the above STING agonists for melanoma treatment remain largely unexplored.
Non-nucleotide STING Agonist in Cancer Therapy
In addition to cyclic dinucleotide-based STING activation, non-nucleotide STING agonists have also shown their antitumor activities in multiple cancer models. For example, DMXAA is a xanthenone analog, which could activate murine STING [103]. Meanwhile, DMXAA treatment potently changes the tumor immune architecture by activating the cytotoxic T cells and suppressing the regulatory T cells within tumors, which helps to inhibit the cancer progression and increase the overall survival in the pancreatic cancer mouse model [104]. Moreover, DMXAA induces strong antitumor immunity in a spontaneous murine melanoma model via a STING-dependent way [105]. MSA-2, an orally available non-nucleotide human STING agonist, dramatically stimulates IFN secretion and induces tumor regression in the mouse models [106]. Moreover, MSA-2 synergizes with anti-PD-1 therapy for durable antitumor immunity in multiple mouse tumor models, including melanoma xenograft model [106]. 5-Fluorouracil (5-FU) is a widely used chemotherapeutic drug. In murine melanoma tumors, 5-FU effectively reduces tumor burden by activating the cancer intrinsic STING [107], supporting the idea of treating 5-FU as a STING agonist for antitumor immunity in melanoma. Thus, the non-nucleotide STING agonists represent a novel therapeutic strategy for melanoma.
STING Agonist Delivery System in Cancer Therapy
The STING agonists hold great potential in melanoma treatment. However, the clinical value of STING agonists was dramatically limited by their unfavorable pharmacological properties, including poor uptake and fast clearance. Therefore, engineered delivery systems were designed to deliver the STING agonist (Table 3). In B16F10 mouse melanoma tumor, exosomes containing cGAMP (the STING agonist) showed superior potency with tumor suppression when compared with cGAMP treatment alone [108], highlighting the potential use of exosomes in STING agonist delivery to enhance melanoma therapy. Polyvalent STING agonist is a pH-sensitive polymer bearing a seven-membered ring with a tertiary amine (PC7A), which could activate innate immunity through the polymer-induced formation of STING-PC7A condensates [109]. Meanwhile, the combination of PC7A and cGAMP leads to potent STING activation and synergistic therapeutic effects in mice bearing tumors [109], offering a new opportunity for cancer treatment.
Table 3.
STING Agonist Delivery System in Cancer Therapy
| Compounds/Molecules | Delivery vehicles/vectors | Types of models | Functions/Biological effects | Refs |
|---|---|---|---|---|
| iExoSTINGa | Exosomes | B16F10 mouse melanoma model | iExoSTINGa shows superior potency with growth suppression when compared with STING agonist treatment alone in B16F10 mouse melanoma tumor | [108] |
| STING-PC7A | Polymer with a cyclic seven-membered ring (PC7A) | MC38 and TC-1 tumor-bearing mice | The combination of PC7A and cGAMP (STING-PC7A) shows potent STING activation and synergistic therapeutic effects in mice bearing tumors | [109] |
| cGAMP-NP/LP-cGAMP | Nanoparticle/lipid nanoparticle-incorporated/conjugated | TNBC, B16F10, and BRAF-mutated murine melanoma models | Both cGAMP-NP and LP-cGAMP show synergistic effects when combined with anti-PD-L1 in murine melanoma models | [111, 112] |
| STING-NPs, STING-LNP, CPs-CDN, and CDN-PEG-lipids | Based on CDNs and nanoparticles | B16F10 tumors, human melanoma tissue, mouse melanoma model with lung metastasis, and MC38-tumor-bearing mice | All of the 4 systems promote STING activation and penetration of tumors, induce tumor repression, and enhance the anti-melanoma therapy. Additionally, the combination of nanoparticle-based CDN delivery and anti-PD-1 exerts a synergistic antitumor effect in melanoma models | [53, 72, 113, 114] |
| PL/APMP-DOX NPs, Mn-cGAMP NVs, and MnP-PEG | Manganese (Mn)-based delivery systems | 4T1 tumor model and B16F10 murine melanoma model | Both PL/APMP-DOX NPs and Mn-cGAMP NVs show versatile applications in tumor immunotherapy. Moreover, the combination of Mn-cGAMP NVs/MnP-PEG and immune checkpoint inhibitor synergistically boosts the antitumor immunity in the murine melanoma model | [117–119] |
To overcome the challenge of systemic delivery of STING agonists to solid tumors and enhance the antitumor immunity in melanoma, several nanoparticle-based delivery systems were developed [110]. For example, Cheng et al. showed that liposomal nanoparticle-delivered cGAMP (cGAMP-NP) activated STING more effectively than soluble cGAMP [111]. Moreover, cGAMP-NP potently reduced the tumor load of melanoma with limited responsivity to anti-PD-L1 [111]. Coincidentally, Li et al. reported that LP-cGAMP (cGAMP encapsulated into lipid nanoparticles) induced STING-related pro-inflammation more efficiently, when compared to free cGAMP [112]. Furthermore, the combination of LP-cGAMP and anti-PD-L1 showed an obvious antitumor effect in B16F10 and BRAF-mutated murine melanoma models, confirming that targeted delivery of cGAMP could enhance the immunotherapy in melanoma [112].
Based on CDNs and nanoparticles, several other delivery systems were designed, called STING-NPs (STING-activating nanoparticles), STING-LNP (lipid nanoparticle containing STING agonist), CPs-CDN (CDN-loaded chimeric polymersomes), and CDN-PEG-lipids (CDNs conjugated to PEGylated lipids), respectively [53, 72, 113, 114]. Meanwhile, all of the above delivery systems efficaciously promoted STING activation and penetration of tumors, markedly induced tumor repression, and significantly enhanced the anti-melanoma therapy [53, 72, 113, 114]. Additionally, the combination of nanoparticle-based STING agonist and anti-PD-1 exerted a synergistic antitumor effect in metastatic B16 melanoma cells [72, 113], indicating that the nanoparticle-based CDN delivery may help to overcome the immunotherapy resistance in melanoma. Nanoparticles thus appear promising as a vehicle for robust delivery of STING agonists throughout solid tumors, which helps to overcome the delivery barriers of CDNs and also represents an effective strategy to potentiate cancer immunotherapy.
Manganese (Mn) is an essential micronutrient, which plays important roles in various biological and physiological processes [115]. Recent studies showed that Mn is indispensable for the host defense against cytosolic dsDNA by activating cGAS-STING [116], suggesting its regulatory role in innate and/or tumor immunity. Meanwhile, Mn-based nanoparticles are now showing versatile applications in tumor immunotherapy [117]. Co-delivery of cGAMP and Mn2+ by a Mn2+ coordinated cyclic dinucleotide nanovaccine (termed as Mn-cGAMP NVs) potently potentiates the antitumor response in B16F10 melanoma mice [118]. Moreover, the combination of Mn-cGAMP NVs and anti-PD-L1 antibody synergistically boosted the antitumor immune response [118]. Consistently, Gao et al. reported that MnP-PEG nanocluster (a PEGylated manganese phosphate nanocluster that actives STING signaling) in combination with a checkpoint inhibitor leads to significant tumor regression in the murine melanoma model [119]. Moreover, a phase I clinical trial with the combined Mn2+ and anti-PD-1 antibody showed promising efficacy in patients with advanced metastatic solid tumors [120], confirming the considerable potential for Mn-based cancer immunotherapy via cGAS-STING activation.
STING Antagonists
While STING agonists are expected to be of value mostly for viral infection or cancer therapy, STING antagonists have a chance to find their home in inflammatory/autoinflammatory diseases [121] (Table 4). In 2018, Haag et al. reported the discovery of highly potent and selective STING antagonists, namely C-178, C-176, and H-151 [31]. Functionally, the identified compounds covalently target the transmembrane cysteine residue 91 and thereby block the palmitoylation-induced STING activation [31]. Mechanistically, these compounds and their derivatives reduce STING-mediated chemokine/cytokine production in both human and mouse cells [31], demonstrating their potential therapeutics for the treatment of autoinflammatory disease. In addition, H151 (targets both human and murine STING) is applied in ameliorating acute kidney injury associated with STING hyperactivation and inflammation [122]. Moreover, pharmacological inhibition of STING using H-151 reduces the aberrant lung inflammation induced by SARS-CoV-2 in mice [123], establishing a mechanistic basis for the STING antagonist-directed therapeutics for COVID-19. Most importantly, STING deficiency alleviates psoriatic inflammation, while the STING antagonist H-151 displays anti-inflammatory activity in IMQ-induced psoriatic mice [39], indicating the therapeutic potential of targeting STING in psoriasis.
Table 4.
STING Antagonists Used in Inflammatory and Autoinflammatory Diseases
| Compounds/Molecules | Types of disease/model | Study outcomes | Refs |
|---|---|---|---|
| H-151 | Psoriasis, THP1 cells, acute kidney injury, COVID-19 infection | H151 targets both human and murine STING, reduces STING-mediated chemokine production, and alleviates inflammation | [31, 39, 122, 123] |
| Astin C | Trex1−/− BMDM cells and TREX1-deficient mouse model | Astin C blocks the recruitment of IRF3 onto the STING signalosome and inhibits the STING-mediated inflammation | [124] |
| ISD017 | Systemic lupus erythematosus | ISD017 selectively blocks the trafficking of STING from the ER to Golgi and inhibits the downstream activities of STING | [125] |
| SN-011 | TREX1-deficient monocytes and a mouse model of stroke | SN-011 specifically and potently inhibits mouse and human STING, resulting in decreased interferon and inflammatory cytokine production | [126] |
| Compound 18 | NA | Compound 18 exhibited good oral bioavailability, slow binding and dissociation kinetics, and functional inhibition of STING-mediated cytokine release | [127] |
With the development of science and technology, more and more compounds or molecular inhibitors targeting STING were identified. For instance, astin C, a cyclopeptide isolated from the medicinal plant Aster tataricus, specifically blocks the recruitment of IRF3 onto the STING signalosome and inhibits the STING-mediated inflammation [124]. ISD017, a specific STING antagonistic peptide, selectively blocks the essential trafficking of STING from the ER to Golgi and inhibits the downstream activities of STING in lupus [125]. SN-011 is a specific and potent mouse and human STING inhibitor that locks STING in an open inactive conformation, which decreases IFN and inflammatory cytokine production [126]. Recently, Siu et al. successfully identified a STING inhibitor called compound 18, which exhibited good oral bioavailability, slow binding and dissociation kinetics, and functional inhibition of STING-mediated cytokine release [127]. All the above STING antagonists have shown their beneficial use and promising for STING-driven disorders. However, it remains unclear whether these STING antagonists could be applied in the treatment of other inflammatory skin diseases besides psoriasis.
PROSPECT AND PERSPECTIVES
The dysregulations of cGAS-STING pathway are increasingly being recognized as important mechanisms in the pathogenesis of cutaneous disorders. Meanwhile, molecules that target cGAS-STING pathway represent a novel therapeutic strategy for autoinflammatory diseases and/or cancers. Although numerous studies have shown that these compounds (agonists or antagonists) hold great promise for the treatment of skin diseases/cancers, the detailed and precise mechanisms remain to be elucidated, and many problems remain to be solved for their better clinical applications:
Most of the current studies regarding cGAS-STING pathway and cutaneous disorders were conducted on cellular or mouse models, and some were conducted on preclinical or phase I clinical models, there is still a long way to go before these investigations can be truly applied to the clinic.
STING-related activators have shown great application prospects in the treatment of tumors and/or diseases caused by infection, but we cannot ignore the side effects they may have, such as systemic immune responses and inflammatory factor storms.
The epigenetic silencing and hypoactivation of STING signaling are common in SKCM, suggesting its crucial roles in melanoma pathogenesis. Thus, most of the researchers focus on the implications of STING agonists in SKCM. However, quite few attentions were paid to the dysregulations of cGAS-STING pathway in other skin cancers, like cutaneous squamous cell carcinoma [128, 129] and Merkel cell carcinoma [130, 131].
Molecules that target cGAS-STING pathway represent a novel therapeutic for inflammatory or autoimmune disorders. However, to date, almost no attempts or quite few attempts have been made in the treatment of autoinflammatory skin disease (besides psoriasis) using these compounds.
Author Contribution
Cong Huang was the major contributor in designing and writing the manuscript. Wenting Li, Xuanyao Ren, Mindan Tang, Kaoyuan Zhang, and Fan Zhuo participated in collecting and reviewing published articles. Xia Dou provided substantial advice in designing and revising the paper. Bo Yu supervised the study and contributed to manuscript preparation. All authors reviewed and approved the final manuscript.
Funding
This work was supported by grants from the National Natural Science Foundation of China (82103726), Guangdong Basic and Applied Basic Research Foundation (2021A1515011558 and 2023A1515010575), Shenzhen Science and Technology Program (JCYJ20210324110008023), Shenzhen Sanming Project (SZSM201812059), Shenzhen Key Medical Discipline Construction Fund (SZXK040), and Scientific Research Foundation of Peking University Shenzhen Hospital (KYQD2021038 and KYQD2021049).
Data Availability
Not applicable.
DECLARATIONS
Ethics Approval
Not applicable.
Consent for Publication
Not applicable.
Competing Interests
The authors declare no competing interests.
Footnotes
Cong Huang and Wenting Li are co-first authors.
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Hay RJ, Johns NE, Williams HC, et al. The global burden of skin disease in 2010: an analysis of the prevalence and impact of skin conditions. The Journal of Investigative Dermatology. 2014;134(6):1527–1534. doi: 10.1038/jid.2013.446. [DOI] [PubMed] [Google Scholar]
- 2.Karimkhani C, Dellavalle RP, Coffeng LE, et al. Global skin disease morbidity and mortality: an update from the global burden of disease study 2013. JAMA Dermatology. 2017;153(5):406–412. doi: 10.1001/jamadermatol.2016.5538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Tan TY, Zhang L, Lim CP. Intelligent skin cancer diagnosis using improved particle swarm optimization and deep learning models. Applied Soft Computing. 2019;84:105725. doi: 10.1016/j.asoc.2019.105725. [DOI] [Google Scholar]
- 4.Saguil A, Kane S, Mercado M, et al. Herpes zoster and postherpetic neuralgia: prevention and management. American Family Physician. 2017;96(10):656–663. [PubMed] [Google Scholar]
- 5.Grennan D. Genital warts. Journal of the American Medical Association. 2019;321(5):520. doi: 10.1001/jama.2018.20181. [DOI] [PubMed] [Google Scholar]
- 6.Fuxench ZCC. Pain in atopic dermatitis: it’s time we addressed this symptom further. British Journal of Dermatology. 2020;182(6):1326–1327. doi: 10.1111/bjd.18785. [DOI] [PubMed] [Google Scholar]
- 7.Maghfour J, Ly S, Haidari W, et al. Treatment of keratosis pilaris and its variants: a systematic review. The Journal of Dermatological Treatment. 2022;33(3):1231–1242. doi: 10.1080/09546634.2020.1818678. [DOI] [PubMed] [Google Scholar]
- 8.Arnold M, Singh D, Laversanne M, et al. Global burden of cutaneous melanoma in 2020 and projections to 2040. JAMA Dermatology. 2022;158(5):495–503. doi: 10.1001/jamadermatol.2022.0160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Falahat R, Perez-Villarroel P, Mailloux AW, et al. STING signaling in melanoma cells shapes antigenicity and can promote antitumor T-cell activity. Cancer Immunology Research. 2019;7(11):1837–1848. doi: 10.1158/2326-6066.CIR-19-0229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Feng Z, Zang C, Zhang L, et al. STING activation promotes inflammatory response and delays skin wound healing in diabetic mice. Biochemical and Biophysical Research Communications. 2022;611:126–131. doi: 10.1016/j.bbrc.2022.04.085. [DOI] [PubMed] [Google Scholar]
- 11.Pyclik M, Durslewicz J, Papinska JA, et al. STING agonist-induced skin inflammation is exacerbated with prior systemic innate immune activation. International Journal of Molecular Sciences. 2023;24(4):4128. doi: 10.3390/ijms24044128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hong Z, Mei J, Guo H, et al. Intervention of cGAS-STING signaling in sterile inflammatory diseases. Journal of Molecular Cell Biology. 2022;14(2):mjac005. doi: 10.1093/jmcb/mjac005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Chen Q, Sun L, Chen ZJ. Regulation and function of the cGAS-STING pathway of cytosolic DNA sensing. Nature Immunology. 2016;17(10):1142–1149. doi: 10.1038/ni.3558. [DOI] [PubMed] [Google Scholar]
- 14.Skopelja-Gardner S, An J, Elkon KB. Role of the cGAS-STING pathway in systemic and organ-specific diseases. Nature Reviews. Nephrology. 2022;18(9):558–572. doi: 10.1038/s41581-022-00589-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Sun L, Wu J, Du F, et al. Cyclic GMP-AMP synthase is a cytosolic DNA sensor that activates the type I interferon pathway. Science. 2013;339:786–791. doi: 10.1126/science.1232458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Motwani M, Pesiridis S, Fitzgerald KA. DNA Sensing by the cGAS-STING Pathway in Health and Disease. Nature Reviews Genetics. 2019;20(11):657–674. doi: 10.1038/s41576-019-0151-1. [DOI] [PubMed] [Google Scholar]
- 17.Hopfner KP, Hornung V. Molecular mechanisms and cellular functions of cGAS-STING signalling. Nature Reviews Molecular Cell Biology. 2020;21(9):501–521. doi: 10.1038/s41580-020-0244-x. [DOI] [PubMed] [Google Scholar]
- 18.Li XD, Wu J, Gao D, et al. Pivotal roles of cGAS-cGAMP signaling in antiviral defense and immune adjuvant effects. Science. 2013;341(6152):1390–1394. doi: 10.1126/science.1244040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Watson RO, Bell SL, MacDuff DA, et al. The cytosolic sensor cGAS detects Mycobacterium tuberculosis DNA to induce type i interferons and activate autophagy. Cell Host & Microbe. 2015;17(6):811–819. doi: 10.1016/j.chom.2015.05.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Riley JS, Tait SW. Mitochondrial DNA in inflammation and immunity. EMBO Reports. 2020;21(4):e49799. doi: 10.15252/embr.201949799. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Jackson SP, Bartek J. The DNA-damage response in human biology and disease. Nature. 2009;461(7267):1071–1078. doi: 10.1038/nature08467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Mackenzie KJ, Carroll P, Martin CA, et al. cGAS surveillance of micronuclei links genome instability to innate immunity. Nature. 2017;548(7668):461–465. doi: 10.1038/nature23449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Zhang X, Wu J, Du F, et al. The cytosolic DNA sensor cGAS forms an oligomeric complex with DNA and undergoes switch like conformational changes in the activation loop. Cell Reports. 2014;6(3):421–430. doi: 10.1016/j.celrep.2014.01.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Li X, Shu C, Yi G, et al. Cyclic GMP-AMP synthase is activated by double-stranded DNA-induced oligomerization. Immunity. 2013;39(6):1019–1031. doi: 10.1016/j.immuni.2013.10.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Zhang X, Shi H, Wu J, et al. Cyclic GMP-AMP containing mixed phosphodiester linkages is an endogenous high-affinity ligand for STING. Molecular Cell. 2013;51(2):226–235. doi: 10.1016/j.molcel.2013.05.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Wu J, Sun L, Chen X, et al. Cyclic GMP-AMP is an endogenous second messenger in innate immune signaling by cytosolic DNA. Science. 2013;339(6121):826–830. doi: 10.1126/science.1229963. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Ablasser A, Goldeck M, Cavlar T, et al. cGAS produces a 2'-5'-linked cyclic dinucleotide second messenger that activates STING. Nature. 2013;498(7454):380–384. doi: 10.1038/nature12306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Shang G, Zhang C, Chen ZJ, et al. Cryo-EM structures of STING reveal its mechanism of activation by cyclic GMP-AMP. Nature. 2019;567(7748):389–393. doi: 10.1038/s41586-019-0998-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Tanaka Y, Chen ZJ. STING specifies IRF3 phosphorylation by TBK1 in the Cytosolic DNA signaling pathway. Science Signaling. 2012;5(214):ra20. doi: 10.1126/scisignal.2002521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Liu S, Cai X, Wu J, et al. Phosphorylation of innate immune adaptor proteins MAVS, STING, and TRIF induces IRF3 activation. Science. 2015;347(6227):aaa2630. doi: 10.1126/science.aaa2630. [DOI] [PubMed] [Google Scholar]
- 31.Haag SM, Gulen MF, Reymond L, et al. Targeting STING with covalent small-molecule inhibitors. Nature. 2018;559(7713):269–273. doi: 10.1038/s41586-018-0287-8. [DOI] [PubMed] [Google Scholar]
- 32.Zhang C, Shang G, Gui X, et al. Structural basis of STING binding with and phosphorylation by TBK1. Nature. 2019;567(7748):394–398. doi: 10.1038/s41586-019-1000-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Abe T, Barber GN. Cytosolic-DNA-mediated, STING-dependent proinflammatory gene induction necessitates canonical NF-kappaB activation through TBK1. Journal of Virology. 2014;88(10):5328–5341. doi: 10.1128/JVI.00037-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Mizutani Y, Kanbe A, Ito H, et al. Activation of STING signaling accelerates skin wound healing. Journal of Dermatological Science. 2020;97(1):21–29. doi: 10.1016/j.jdermsci.2019.11.008. [DOI] [PubMed] [Google Scholar]
- 35.Beck MA, Fischer H, Grabner LM, et al. DNA hypomethylation leads to cGAS-induced autoinflammation in the epidermis. EMBO Journal. 2021;40(22):e108234. doi: 10.15252/embj.2021108234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Wu T, Gao J, Liu W, et al. NLRP3 protects mice from radiation-induced colon and skin damage via attenuating cGAS-STING signaling. Toxicology and Applied Pharmacology. 2021;418:115495. doi: 10.1016/j.taap.2021.115495. [DOI] [PubMed] [Google Scholar]
- 37.Zhou M, Cheng X, Zhu W, et al. Activation of cGAS-STING pathway - A possible cause of myofiber atrophy/necrosis in dermatomyositis and immune-mediated necrotizing myopathy. Journal of Clinical Laboratory Analysis. 2022;36(10):e24631. doi: 10.1002/jcla.24631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Zhang LJ. Type1 Interferons Potential initiating factors linking skin wounds with psoriasis pathogenesis. Frontiers in Immunology. 2019;10:1440. doi: 10.3389/fimmu.2019.01440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Pan Y, You Y, Sun L, et al. The STING antagonist H-151 ameliorates psoriasis via suppression of STING/NF-kB-mediated inflammation. British Journal of Pharmacology. 2021;178(24):4907–4922. doi: 10.1111/bph.15673. [DOI] [PubMed] [Google Scholar]
- 40.Yu Y, Xue X, Tang W, et al. Cytosolic DNA-mediated STING-dependent inflammation contributes to the progression of psoriasis. The Journal of Investigative Dermatology. 2022;142(3):898–906. doi: 10.1016/j.jid.2021.08.430. [DOI] [PubMed] [Google Scholar]
- 41.Li X, Zhang Z, Yu Y, et al. Activation of the STING-IRF3 pathway involved in psoriasis with diabetes mellitus. Journal of Cellular and Molecular Medicine. 2022;26(8):2139–2151. doi: 10.1111/jcmm.17236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Nakamizo S, Egawa G, Honda T, et al. Commensal bacteria and cutaneous immunity. Seminars in Immunopathology. 2015;37(1):73–80. doi: 10.1007/s00281-014-0452-6. [DOI] [PubMed] [Google Scholar]
- 43.Bjerre RD, Bandier J, Skov L, et al. The role of the skin microbiome in atopic dermatitis: a systematic review. British Journal of Dermatology. 2017;177(5):1272–1278. doi: 10.1111/bjd.15390. [DOI] [PubMed] [Google Scholar]
- 44.O'Neill AM, Gallo RL. Host-microbiome interactions and recent progress into understanding the biology of acne vulgaris. Microbiome. 2018;6(1):177. doi: 10.1186/s40168-018-0558-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Wang S, Wang R, Song Y, et al. Dysbiosis of nail microbiome in patients with psoriasis. Experimental Dermatology. 2022;31(5):800–806. doi: 10.1111/exd.14528. [DOI] [PubMed] [Google Scholar]
- 46.Lima-Junior DS, Krishnamurthy SR, Bouladoux N, et al. Endogenous retroviruses promote homeostatic and inflammatory responses to the microbiota. Cell. 2021;184(14):3794–3811. doi: 10.1016/j.cell.2021.05.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Skudalski L, Waldman R, Kerr PE, et al. Melanoma: an update on systemic therapies. JAMA Dermatology. 2022;86(3):515–524. doi: 10.1016/j.jaad.2021.09.075. [DOI] [PubMed] [Google Scholar]
- 48.Xia T, Konno H, Barber GN. Recurrent loss of STING signaling in melanoma correlates with susceptibility to viral oncolysis. Cancer Research. 2016;76(22):6747–6759. doi: 10.1158/0008-5472.CAN-16-1404. [DOI] [PubMed] [Google Scholar]
- 49.Falahat R, Berglund A, Putney RM, et al. Epigenetic reprogramming of tumor cell–intrinsic STING function sculpts antigenicity and T cell recognition of melanoma. Proceedings of the National Academy of Sciences. 2021;118(15):e2013598118. doi: 10.1073/pnas.2013598118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Xu T, Dai J, Tang L, et al. EZH2 inhibitor enhances the STING agonist-induced antitumor immunity in melanoma. The Journal of Investigative Dermatology. 2022;142(4):1158–1170. doi: 10.1016/j.jid.2021.08.437. [DOI] [PubMed] [Google Scholar]
- 51.Woo SR, Fuertes MB, Corrales L, et al. STING-dependent cytosolic DNA sensing mediates innate immune recognition of immunogenic tumors. Immunity. 2014;41(5):830–842. doi: 10.1016/j.immuni.2014.10.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Hu M, Zhou M, Bao X, et al. ATM inhibition enhances cancer immunotherapy by promoting mtDNA leakage and cGAS/STING activation. The Journal of Clinical Investigation. 2021;131(3):e139333. doi: 10.1172/JCI139333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Shae D, Becker KW, Christov P, et al. Endosomolytic polymersomes increase the activity of cyclic dinucleotide STING agonists to enhance cancer immunotherapy. Nature Nanotechnology. 2019;14(3):269–278. doi: 10.1038/s41565-018-0342-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Ma Z, Xiong Q, Xia H, et al. Carboplatin activates the cGAS-STING pathway by upregulating the TREX-1 (three prime repair exonuclease 1) expression in human melanoma. Bioengineered. 2021;12(1):6448–6458. doi: 10.1080/21655979.2021.1972198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Wang Z, Celis E. STING activator c-di-GMP enhances the anti-tumor effects of peptide vaccines in melanoma-bearing mice. Cancer Immunology, Immunotherapy. 2015;64(8):1057–1066. doi: 10.1007/s00262-015-1713-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Nakamura T, Miyabe H, Hyodo M, et al. Liposomes loaded with a sting pathway ligand, cyclic di-GMP, enhance cancer immunotherapy against metastatic melanoma. Journal of Controlled Release. 2015;216:149–157. doi: 10.1016/j.jconrel.2015.08.026. [DOI] [PubMed] [Google Scholar]
- 57.Long GV, Stroyakovskiy D, Gogas H, et al. Combined BRAF and MEK inhibition versus BRAF inhibition alone in melanoma. New England Journal of Medicine. 2014;371(20):1877–1888. doi: 10.1056/NEJMoa1406037. [DOI] [PubMed] [Google Scholar]
- 58.Dulgar O, Kutuk T, Eroglu Z. Mechanisms of resistance to BRAF-targeted melanoma therapies. American Journal of Clinical Dermatology. 2021;22(1):1–10. doi: 10.1007/s40257-020-00572-6. [DOI] [PubMed] [Google Scholar]
- 59.Yue J, Vendramin R, Liu F, et al. Targeted chemotherapy overcomes drug resistance in melanoma. Genes & Development. 2020;34(9–10):637–649. doi: 10.1101/gad.333864.119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Cesi G, Walbrecq G, Zimmer A, et al. ROS production induced by BRAF inhibitor treatment rewires metabolic processes affecting cell growth of melanoma cells. Molecular Cancer. 2017;16(1):102. doi: 10.1186/s12943-017-0667-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Khamari R, Trinh A, Gabert PE, et al. Glucose metabolism and NRF2 coordinate the antioxidant response in melanoma resistant to MAPK inhibitors. Cell Death & Disease. 2018;9(3):325. doi: 10.1038/s41419-018-0340-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Hos NJ, Ganesan R, Gutiérrez S, et al. Type I interferon enhances necroptosis of Salmonella Typhimurium–infected macrophages by impairing antioxidative stress responses. Journal of Cell Biology. 2017;216(12):4107–4121. doi: 10.1083/jcb.201701107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Ramanjulu JM, Pesiridis GS, Yang J, et al. Design of amidobenzimidazole STING receptor agonists with systemic activity. Nature. 2018;564(7736):439–443. doi: 10.1038/s41586-018-0705-y. [DOI] [PubMed] [Google Scholar]
- 64.Chipurupalli S, Ganesan R, Dhanabal SP, et al. Pharmacological STING activation is a potential alternative to overcome drug-resistance in melanoma. Frontiers in Oncology. 2020;10:758. doi: 10.3389/fonc.2020.00758. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Larkin J, Chiarion-Sileni V, Gonzalez R, et al. Five-year survival with combined nivolumab and ipilimumab in advanced melanoma. New England Journal of Medicine. 2019;381(16):1535–1546. doi: 10.1056/NEJMoa1910836. [DOI] [PubMed] [Google Scholar]
- 66.Schoenfeld AJ, Hellmann MD. Acquired resistance to immune checkpoint inhibitors. Cancer Cell. 2020;37(4):443–455. doi: 10.1016/j.ccell.2020.03.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Nguyen TT, Ramsay L, Ahanfeshar-Adams M, et al. Mutations in the IFNγ-JAK-STAT pathway causing resistance to immune checkpoint inhibitors in melanoma increase sensitivity to oncolytic virus treatment. Clinical Cancer Research. 2021;27(12):3432–3442. doi: 10.1158/1078-0432.CCR-20-3365. [DOI] [PubMed] [Google Scholar]
- 68.Srour N, Villarreal OD, Hardikar S, et al. PRMT7 ablation stimulates anti-tumor immunity and sensitizes melanoma to immune checkpoint blockade. Cell Reports. 2022;38(13):110582. doi: 10.1016/j.celrep.2022.110582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Yum S, Li M, Frankel AE, et al. Roles of the cGAS-STING pathway in cancer immunosurveillance and immunotherapy. Annual Review of Cancer Biology. 2019;3:323–344. doi: 10.1146/annurev-cancerbio-030518-055636. [DOI] [Google Scholar]
- 70.Sato S, Sawada Y, Nakamura M. STING signaling and skin cancers. Cancers (Basel) 2021;13(22):5603. doi: 10.3390/cancers13225603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Miyabe H, Hyodo M, Nakamura T, et al. A new adjuvant delivery system ‘cyclic di-GMP/YSK05 liposome’ for cancer immunotherapy. Journal of Controlled Release. 2014;184:20–27. doi: 10.1016/j.jconrel.2014.04.004. [DOI] [PubMed] [Google Scholar]
- 72.Nakamura T, Sato T, Endo R, et al. STING agonist loaded lipid nanoparticles overcome anti-PD-1 resistance in melanoma lung metastasis via NK cell activation. Journal for Immunotherapy of Cancer. 2021;9(7):e002852. doi: 10.1136/jitc-2021-002852. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Lama L, Adura C, Xie W, et al. Development of human cGAS-specific small molecule inhibitors for repression of dsDNA triggered interferon expression. Nature Communications. 2019;10(1):2261. doi: 10.1038/s41467-019-08620-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Vincent J, Adura C, Gao P, et al. Small molecule inhibition of cGAS reduces interferon expression in primary macrophages from autoimmune mice. Nature Communications. 2017;8(1):750. doi: 10.1038/s41467-017-00833-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Wiser C, Kim B, Vincent J, et al. Small molecule inhibition of human cGAS reduces total cGAMP output and cytokine expression in cells. Science and Reports. 2020;10(1):7604. doi: 10.1038/s41598-020-64348-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Tan J, Wu B, Chen T, et al. Synthesis and pharmacological evaluation of tetrahydro-γ-carboline derivatives as potent anti-inflammatory agents targeting cyclic GMP-AMP synthase. Journal of Medicinal Chemistry. 2021;64(11):7667–7690. doi: 10.1021/acs.jmedchem.1c00398. [DOI] [PubMed] [Google Scholar]
- 77.Platt B, Belarski E, Manaloor J, et al. Comparison of risk of recrudescent fever in children with Kawasaki disease treated with intravenous immunoglobulin and low-dose vs high-dose aspirin. JAMA Network Open. 2020;3(1):e1918565. doi: 10.1001/jamanetworkopen.2019.18565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.D’Orazio JA. Aspirin’s protective effects highlight the role of inflammation in UV-induced skin damage and carcinogenesis. The Journal of Investigative Dermatology. 2021;141(1):10–11. doi: 10.1016/j.jid.2020.06.011. [DOI] [PubMed] [Google Scholar]
- 79.Dai J, Huang YJ, He X, et al. Acetylation blocks cGAS activity and inhibits self-DNA-induced autoimmunity. Cell. 2019;176(6):1447–1460. doi: 10.1016/j.cell.2019.01.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Opoku-Temeng C, Sintim HO. Potent inhibition of cyclic diadenylate monophosphate cyclase by the antiparasitic drug, suramin. Chemical Communications (Cambridge, England) 2016;52(19):3754–3757. doi: 10.1039/C5CC10446G. [DOI] [PubMed] [Google Scholar]
- 81.Wang M, Sooreshjani MA, Mikek C, et al. Suramin potently inhibits cGAMP synthase, cGAS, in THP1 cells to modulate IFN-β levels. Future Medicinal Chemistry. 2018;10(11):1301–1317. doi: 10.4155/fmc-2017-0322. [DOI] [PubMed] [Google Scholar]
- 82.Steinhagen F, Zillinger T, Peukert K, et al. Suppressive oligodeoxynucleotides containing TTAGGG motifs Inhibit cGAS activation in human monocytes. European Journal of Immunology. 2018;48(4):605–611. doi: 10.1002/eji.201747338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Li Q, Cao Y, Dang C, et al. Inhibition of double-strand DNA-sensing cGAS ameliorates brain injury after ischemic stroke. EMBO Molecular Medicine. 2020;12(4):e11002. doi: 10.15252/emmm.201911002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Chu L, Li C, Li Y, et al. Perillaldehyde inhibition of cGAS reduces dsDNA-induced interferon response. Frontiers in Immunology. 2021;12:655637. doi: 10.3389/fimmu.2021.655637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Liu ZS, Cai H, Xue W, et al. G3BP1 promotes DNA binding and activation of cGAS. Nature Immunology. 2019;20(1):18–28. doi: 10.1038/s41590-018-0262-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Cai H, Liu X, Zhang F, et al. G3BP1 inhibition alleviates intracellular nucleic acid-induced autoimmune responses. The Journal of Immunology. 2021;206(10):2453–2467. doi: 10.4049/jimmunol.2001111. [DOI] [PubMed] [Google Scholar]
- 87.Valentin R, Wong C, Alharbi AS, et al. Sequence-dependent inhibition of cGAS and TLR9 DNA sensing by 2'-O-methyl gapmer oligonucleotides. Nucleic Acids Research. 2021;49(11):6082–6099. doi: 10.1093/nar/gkab451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Cuddy SR, Schinlever AR, Dochnal S, et al. Neuronal hyperexcitability is a DLK-dependent trigger of herpes simplex virus reactivation that can be induced by IL-1. eLife. 2020;9:e58037. doi: 10.7554/eLife.58037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Guellil M, van Dorp L, Inskip SA, et al. Ancient herpes simplex 1 genomes reveal recent viral structure in Eurasia. Science Advances. 2022;8(30):eabo4435. doi: 10.1126/sciadv.abo4435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Cerón S, North BJ, Taylor SA, et al. The STING agonist 5,6-dimethylxanthenone-4-acetic acid (DMXAA) stimulates an antiviral state and protects mice against herpes simplex virus. Virology. 2019;529:23–28. doi: 10.1016/j.virol.2019.01.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Zhu Q, Hu H, Liu H, et al. A synthetic STING agonist inhibits the replication of human parainfluenza virus 3 and rhinovirus 16 through distinct mechanisms. Antiviral Research. 2020;183:104933. doi: 10.1016/j.antiviral.2020.104933. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Li M, Ferretti M, Ying B, et al. Pharmacological activation of STING blocks SARS-CoV-2 infection. Science Immunology. 2021;6(59):eabi9007. doi: 10.1126/sciimmunol.abi9007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Demaria O, De Gassart A, Coso S, et al. STING activation of tumor endothelial cells initiates spontaneous and therapeutic antitumor immunity. Proceedings of the National Academy of Sciences. 2015;112(50):15408–15413. doi: 10.1073/pnas.1512832112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Yang H, Lee WS, Kong SJ, et al. STING activation reprograms tumor vasculatures and synergizes with VEGFR2 blockade. The Journal of Clinical Investigation. 2019;129(10):4350–4364. doi: 10.1172/JCI125413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Wang H, Hu S, Chen X, et al. cGAS is essential for the antitumor effect of immune checkpoint blockade. Proceedings of the National Academy of Sciences. 2017;114(7):1637–1642. doi: 10.1073/pnas.1621363114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Flood BA, Higgs EF, Li S, et al. STING pathway agonism as a cancer therapeutic. Immunological Reviews. 2019;290(1):24–38. doi: 10.1111/imr.12765. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Vonderhaar EP, Barnekow NS, McAllister D, et al. STING activated tumor-intrinsic type I interferon signaling promotes CXCR3 dependent antitumor immunity in pancreatic cancer. Cellular and Molecular Gastroenterology and Hepatology. 2021;12(1):41–58. doi: 10.1016/j.jcmgh.2021.01.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Berger G, Knelson EH, Jimenez-Macias JL, et al. STING activation promotes robust immune response and NK cell–mediated tumor regression in glioblastoma models. Proceedings of the National Academy of Sciences. 2022;119(28):e2111003119. doi: 10.1073/pnas.2111003119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Meric-Bernstam F, Sweis RF, Hodi FS, et al. Phase I dose-escalation trial of MIW815 (ADU-S100), an intratumoral STING agonist, in patients with advanced/metastatic solid tumors or lymphomas. Clinical Cancer Research. 2022;28(4):677–688. doi: 10.1158/1078-0432.CCR-21-1963. [DOI] [PubMed] [Google Scholar]
- 100.Chelvanambi M, Fecek RJ, Taylor JL, et al. STING agonist-based treatment promotes vascular normalization and tertiary lymphoid structure formation in the therapeutic melanoma microenvironment. Journal for Immunotherapy of Cancer. 2021;9(2):e001906. doi: 10.1136/jitc-2020-001906. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Ager CR, Boda A, Rajapakshe K, et al. High potency STING agonists engage unique myeloid pathways to reverse pancreatic cancer immune privilege. Journal for Immunotherapy of Cancer. 2021;9(8):e003246. doi: 10.1136/jitc-2021-003246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Ager CR, Zhang H, Wei Z, et al. Discovery of IACS-8803 and IACS-8779, potent agonists of stimulator of interferon genes (STING) with robust systemic antitumor efficacy. Bioorganic & Medicinal Chemistry Letters. 2019;29(20):126640. doi: 10.1016/j.bmcl.2019.126640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Kim S, Li L, Maliga Z, et al. Anticancer flavonoids are mouse-selective STING agonists. ACS Chemical Biology. 2013;8(7):1396–1401. doi: 10.1021/cb400264n. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Jing W, McAllister D, Vonderhaar EP, et al. STING agonist inflames the pancreatic cancer immune microenvironment and reduces tumor burden in mouse models. Journal for Immunotherapy of Cancer. 2019;7(1):115. doi: 10.1186/s40425-019-0573-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Corrales L, Glickman LH, McWhirter SM, et al. Direct activation of STING in the tumor microenvironment leads to potent and systemic tumor regression and immunity. Cell Reports. 2015;11(7):1018–1030. doi: 10.1016/j.celrep.2015.04.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Pan BS, Perera SA, Piesvaux JA, et al. An orally available non-nucleotide STING agonist with antitumor activity. Science. 2020;369(6506):eaba6098. doi: 10.1126/science.aba6098. [DOI] [PubMed] [Google Scholar]
- 107.Tian J, Zhang D, Kurbatov V, et al. 5-Fluorouracil efficacy requires anti-tumor immunity triggered by cancer-cell-intrinsic STING. EMBO Journal. 2021;40(7):e106065. doi: 10.15252/embj.2020106065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.McAndrews KM, Che SPY, LeBleu VS, et al. Effective delivery of STING agonist using exosomes suppresses tumor growth and enhances antitumor immunity. Journal of Biological Chemistry. 2021;296:100523. doi: 10.1016/j.jbc.2021.100523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Li S, Luo M, Wang Z, et al. Prolonged activation of innate immune pathways by a polyvalent STING agonist. Nature Biomedical Engineering. 2021;5(5):455–466. doi: 10.1038/s41551-020-00675-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Zhou Q, Zhou Y, Li T, et al. Nanoparticle-mediated STING agonist delivery for enhanced cancer immunotherapy. Macromolecular Bioscience. 2021;21(8):e2100133. doi: 10.1002/mabi.202100133. [DOI] [PubMed] [Google Scholar]
- 111.Cheng N, Watkins-Schulz R, Junkins RD, et al. A nanoparticle-incorporated STING activator enhances antitumor immunity in PD-L1–insensitive models of triple-negative breast cancer. JCI Insight. 2018;3(22):e120638. doi: 10.1172/jci.insight.120638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Li K, Ye Y, Liu L, et al. The lipid platform increases the activity of STING agonists to synergize checkpoint blockade therapy against melanoma. Biomaterials Science. 2021;9(3):765–773. doi: 10.1039/D0BM00870B. [DOI] [PubMed] [Google Scholar]
- 113.Zheng H, Guo B, Qiu X, et al. Polymersome-mediated cytosolic delivery of cyclic dinucleotide STING agonist enhances tumor immunotherapy. Bioactive Materials. 2022;16:1–11. doi: 10.1016/j.bioactmat.2022.02.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Dane EL, Belessiotis-Richards A, Backlund C, et al. STING agonist delivery by tumour-penetrating PEG-lipid nanodiscs primes robust anticancer Immunity. Nature Materials. 2022;21(6):710–720. doi: 10.1038/s41563-022-01251-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Zhang, K., C. Qi, and K. Cai. 2022. Manganese-based tumor immunotherapy. Advanced Materials, e2205409. [DOI] [PubMed]
- 116.Wang C, Guan Y, Lv M, et al. Manganese increases the sensitivity of the cGAS-STING pathway for double-stranded DNA and is required for the host defense against DNA viruses. Immunity. 2018;48(4):675–687. doi: 10.1016/j.immuni.2018.03.017. [DOI] [PubMed] [Google Scholar]
- 117.Hou L, Tian C, Yan Y, et al. Manganese-based nanoactivator optimizes cancer immunotherapy via enhancing innate immunity. ACS Nano. 2020;14(4):3927–3940. doi: 10.1021/acsnano.9b06111. [DOI] [PubMed] [Google Scholar]
- 118.Chen C, Tong Y, Zheng Y, et al. Cytosolic delivery of thiolated Mn-cGAMP nanovaccine to enhance the antitumor immune responses. Small (Weinheim an der Bergstrasse, Germany) 2021;17(17):e2006970. doi: 10.1002/smll.202006970. [DOI] [PubMed] [Google Scholar]
- 119.Gao M, Xie Y, Lei K, et al. A manganese phosphate nanocluster activates the cGAS-STING pathway for enhanced cancer immunotherapy. Advanced Therapeutics. 2021;4(8):2100065. doi: 10.1002/adtp.202100065. [DOI] [Google Scholar]
- 120.Lv M, Chen M, Zhang R, et al. Manganese is critical for antitumor immune responses via cGAS-STING and improves the efficacy of clinical immunotherapy. Cell Research. 2020;30(11):966–979. doi: 10.1038/s41422-020-00395-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Decout A, Katz JD, Venkatraman S, et al. The cGAS-STING pathway as a therapeutic target in inflammatory diseases. Nature Reviews Immunology. 2021;21(9):548–569. doi: 10.1038/s41577-021-00524-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Gong W, Lu L, Zhou Y, et al. The novel STING antagonist H151 ameliorates cisplatin-induced acute kidney injury and mitochondrial dysfunction. American Journal of Physiology-Renal Physiology. 2021;320(4):608–616. doi: 10.1152/ajprenal.00554.2020. [DOI] [PubMed] [Google Scholar]
- 123.Domizio JD, Gulen MF, Saidoune F, et al. The cGAS-STING pathway drives type I IFN immunopathology in COVID-19. Nature. 2022;603(7899):145–151. doi: 10.1038/s41586-022-04421-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Li S, Hong Z, Wang Z, et al. The cyclopeptide astin C specifically inhibits the innate immune CDN sensor STING. Cell Reports. 2018;25(12):3405–3421. doi: 10.1016/j.celrep.2018.11.097. [DOI] [PubMed] [Google Scholar]
- 125.Prabakaran T, Troldborg A, Kumpunya S, et al. A STING antagonist modulating the interaction with STIM1 blocks ER-to-Golgi trafficking and inhibits lupus pathology. eBioMedicine. 2021;66:103314. doi: 10.1016/j.ebiom.2021.103314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Hong Z, Mei J, Li C, et al. STING inhibitors target the cyclic dinucleotide binding pocket. Proceedings of the National Academy of Sciences. 2021;118(24):e2105465118. doi: 10.1073/pnas.2105465118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Siu T, Altman MD, Baltus GA, et al. Discovery of a novel cGAMP competitive ligand of the inactive form of STING. ACS Medicinal Chemistry Letters. 2018;10(1):92–97. doi: 10.1021/acsmedchemlett.8b00466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Harabuchi S, Kosaka A, Yajima Y, et al. Intratumoral STING activations overcome negative impact of cisplatin on antitumor immunity by inflaming tumor microenvironment in squamous cell carcinoma. Biochemical and Biophysical Research Communications. 2020;522(2):408–414. doi: 10.1016/j.bbrc.2019.11.107. [DOI] [PubMed] [Google Scholar]
- 129.Hayman TJ, Baro M, MacNeil T, et al. STING enhances cell death through regulation of reactive oxygen species and DNA damage. Nature Communications. 2021;12(1):2327. doi: 10.1038/s41467-021-22572-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Krump NA, Wang R, Liu W, et al. Merkel cell polyomavirus infection induces an antiviral innate immune response in human dermal fibroblasts. Journal of Virology. 2021;95(13):e0221120. doi: 10.1128/JVI.02211-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Liu W, Kim GB, Krump NA, et al. Selective reactivation of STING signaling to target Merkel cell carcinoma. Proceedings of the National Academy of Sciences. 2020;117(24):13730–13739. doi: 10.1073/pnas.1919690117. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Not applicable.