Abstract
Coronavirus disease 2019 (COVID-19) is caused by a severe acute respiratory syndrome coronavirus (SARS-CoV-2) and became pandemic after emerging in Wuhan, China, in December 2019. We aimed to investigate the prevalence, clinical characteristics, and risk factors for SARS-CoV-2 infections in districts of southwest Ethiopia. A study was conducted on COVID-19 surveillance data in the diagnostic center of the southwest district of Ethiopia from July 1, 2020, to February 30, 2021. A total of 10 618 nasopharyngeal specimens were tested for SARS-COV-2 using the detection of unique sequences of virus RNA by reverse transcriptase PCR. Data were entered into Epidata version 3.1 and analyzed using SPSS version 25. Logistic regression was used to determine the relationship between COVID-19 and risk factors, with a significance level of P = 0.05. A total of 10 618 individuals were tested for SARS-CoV-2. Of these, 419 (3.9%) patients tested positive for SARS-CoV-2. Among a total of 419 patients who tested positive for SARS-CoV-2, 80.2% were asymptomatic, 264 (63.0%) were males, and 233 (55.6%) were aged 19 to 35 years. Comorbidity was present in 37 (8.8%). The risk of getting SARS-CoV-2 infections was increased with male sex (AOR = 1.248; 95% CI: 1.007, 1.547), health workers (AOR = 3.187; 95% CI: 1.960, 5.182), prisoners (AOR = 2.118; 95% CI: 1.104, 4.062), and comorbid conditions (AOR = 2.972; 95% CI: 1.649, 5.358), such as diabetes (AOR = 4.765; 95% CI: 1.977-11.485) and other respiratory problems (AOR = 3.267; 95% CI: 1.146-9.317). Despite the fact that overall laboratories confirmed prevalence of SARS-CoV-2 infections in the study area was low and dynamic, it was spread to all zones of the study area. This highlights the importance of implementing the most effective public health strategies to prevent the further spread and reduce the burden of SARS-CoV-2 infections.
Keywords: SARS-CoV-2 infections, clinical character, risk factors, southwest Ethiopia, 2020 to 2021
What do we already know about this topic?
COVID-19 is a pandemic disease that can attack all people, especially those with co-morbidity, and presents different clinical characteristics.
How does your research contribute to the field?
Our research contributes to the field by providing magnitude, clinical characteristics, and associated risk factors in the study area.
What are your research’s implications toward theory, practice, or policy?
This work can provide meaningful information on the prevalence of SARS-CoV-2 infections, clinical characteristics, and related risk factors for this topic and may support local government for decision-making on strategies to handle this public health emergency at the community, local, and national level.
Introduction
The coronavirus is a member of a group of viruses that can lead to a number of symptoms, including pneumonia, fever, breathing difficulty, and lung infection. From the earliest months, it became increasingly clear that in addition to affecting the upper airways and lungs, there were other organs that could be affected including the skin. 1 Although these viruses commonly infect animals worldwide, very few cases have been known to affect humans.2,3 The severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2) was first identified as the 2019 novel coronavirus-2 by the World Health Organization (WHO) and Centers for Disease Control and Prevention (CDC) on December 29, 2019, after it infected the lower respiratory tracts of pneumonia patients in Wuhan, China.4-6
As the SARS-CoV-2 is a recently discovered pathogen that caused the pandemic disease outbreak, there is insufficient data to understand the whole nature of this virus. More investigation is required to determine whether SARS-CoV-2-infected pneumonia is transmitted directly from bats or via an intermediate host. 7 It is believed that the structural and cellular foundations are important for understanding the multistep SARS-CoV-2 entry process and the roles of furin-like proteases, transmembrane proteases, serine 2, and cathepsin L in these processes, as well as delineating the features of Angiotensin converting enzyme (ACE2) orthologs in reservoir animal species and S protein adaptations that facilitate efficient human transmission. 8
The decision to test should be based on clinical and epidemiological factors and linked to an assessment of the likelihood of infection. Using polymerase chain reaction (PCR), testing of asymptomatic or mildly symptomatic contacts can be considered in the assessment of individuals who have had contact with SARS-CoV-2 infected cases. The case definitions are being regularly reviewed and updated as new information becomes available.9,10 Given the spread of the new Corona virus and its consequences for human health, a rapid response to the prevention and control of this new virus’s spread is required.
In response to the outbreak, the Ethiopian government and ministry of health also stand for prevention and control of this emergency, mostly through mass media and announcing the emergency restrictions throughout the country. 11 Regional states established command posts that were taking serious measures to prevent the spread of SARS-CoV-2 infections in their respective jurisdictions. In order for these efforts to be effective, health authorities will need timely and factional data to design policies and interventions that are easily understood and relevant to the lives of inhabitants. This work can provide meaningful information on SARS-CoV-2 infections, clinical characteristics, and related risk factors for future research related to this topic and may support government decision-making on strategies to handle this public health emergency at the community, national, and international levels.
Methods
Study Area and Period
This study was conducted in the Mizan-Tepi University COVID-19 Diagnostic Center, southwest district of Ethiopia, from July 1, 2020, to February 30, 2021. The district is large and contains 4 zones: Kaffa, Bench-Sheko, Sheka, and West Omo zones. These 4 zones are located at 449, 585, 605, and 708 km, respectively, from Addis Ababa, the capital city of Ethiopia. There are 11 woredas and 2 town administrations in Kaffa zone. Bench-Sheko Zone is administratively divided into 6 woredas (districts) and 2 town administrations. Likewise, the Sheka and West Omo zones have 5 and 7 woredas, respectively. Each woreda and city in all zones has SARS-CoV-2 clinical screening, sample collection, quarantine, and isolation centers. According to the population projection of Ethiopia for 2014 to 2017, the Bench Sheko and West Omo Zones had a total population of 847 168 (417 751 males and 429 417 females). Similarly, the Kaffa and Sheka Zones had a total population size of 1102,278 (541 682 males and 560 596 females) and 975 246 (514 323 males and 460 923 females), respectively. 12
Study Design and Subjects
This study was conducted based on an analysis of the COVID-19 surveillance data that was generated for the southwest district of Ethiopia at Mizan-Tepi University’s COVID-19 diagnostic center. All clinically suspected cases, contacts of confirmed cases, high risks and vulnerable groups in the community and whose clinical specimens received at Mizan-Tepi university COVID-19 diagnostic center and those laboratory requests contained with complete information about sociodemographic and clinical characteristics were included in our study.
Sample Size and Sampling Techniques
Since the study was retrospective and based on COVID-19 surveillance, sample size calculation was not applicable. All study participants (10 618) who tested for SARS-CoV-2 during the first 8 months of the surveillance study period were included.
Operational Definition
Clinically suspected case
An individual who has at least 3 symptoms out of the following symptoms a new cough, fever, shortness of breath, sore throat, headache, and fatigue.
Specimen Collection and Shipment
Nasopharyngeal specimens were collected from clinically suspected cases, contacts of confirmed cases, and high risks groups in the community. The staffs from different health facilities in the catchment area were trained for appropriate specimen collection, storage, packaging, and transport. All specimens for laboratory investigations were collected and then transported using viral transport medium (VTM) to the COVID-19 diagnostic center. In addition, the patients’ laboratory requests that contained with sociodemographic, clinical characteristics, comorbidity conditions, and other risk factors, including exposures to patients with similar symptoms and travel histories, were received at the diagnostic center and extracted using data abstraction tools. All health care workers who collect specimens were adhered rigorously to infection prevention and control guidelines. 13
Laboratory Testing for COVID-19
Laboratory testing for SARS-CoV-2 was performed by staff trained in the relevant technical and safety procedures and in strict adherence with biosafety practices as per the WHO guideline for laboratory testing of COVID-19.13,14 The detection of SARS-CoV-2 was done based on the detection of unique sequences of virus RNA by real-time reverse transcription polymerase chain reaction (rRT-PCR), which is the gold standard test for the detection of SARS-CoV-2 RNA in clinical samples. In the molecular biology laboratory, RNA extraction was performed using Da An Gene Co., Ltd. of Sun Yat-sen University Version 1, as per the manufacturer’s instructions. After the RNA extraction, 10 µl of the sample extract were added to 20 µl of the master mix for the BGI Genomics’ 2019-nCoV Fluorescence Detection Real-Time RT-PCR kit. The result interpretation was done by analyzing an S-shaped standard curve at the FAM channel with a specified Ct value as per the BGI instruction. All RT-PCR confirmed cases were traced by the surveillance team from the laboratory database, and their laboratory requests were reviewed to check their socio-demographic and clinical characteristics. Then, the team reported the confirmed case to the regional health bureau and to the facilities that sent the patient’s specimens, as they link all individual cases to COVID-9 treatment centers as required.
Data Analysis
Data collected on sociodemographic factors, clinical features, and laboratory test results of study participants were entered into Epidata version 3.1 and analyzed using SPSS version 25 statistical software. First, frequency distributions and descriptive statistics such as number and percent were computed and summarized in tables and text. Logistic regression was used to see the association between the explanatory and outcome variables. A P-value of <.05 with 95% confidence intervals was considered as statistically significant.
Results
Sociodemographic Characteristics of Study Participants
In this study, a total of 10 618 study participants suspected of having an infection due to SARS-COV-2 were enrolled. Among these, 6262 (59.0%) were males and 4356 (41.0%) were females. The majority of the study participants, 5534 (52.1%), were between the ages of 19 and 35, and the average age of the study participants was 34.5. Most of the specimens, 3680 (34.6%), were collected from Kaffa Zone, and 5635 (53.1%) of them were collected from the community. Specimens from health facilities accounted for 2190 (20.6%) of the total, but only 1856 (17.5%) were from health workers and 1376 (12.9%) were from quarantine centers (Table 1).
Table 1.
The Sociodemographic Characteristics of Study Participants Tested for SARS-CoV-2 Infections at the COVID-19 Diagnostic Center, Southwest Districts of Ethiopia.
| Characteristics of patients | Total |
Positive (n = 419) |
Negative (n = 10 199) |
|---|---|---|---|
| N (%) | N (%) | N (%) | |
| Age in years | |||
| ≤18 | 860 (5.2) | 31 (7.4) | 529 (5.2) |
| 19-35 | 5534 (52.1) | 233 (55.6) | 5301 (52.0) |
| 36-59 | 4389 (41.3) | 146 (34.8) | 4243 (42.6) |
| ≥60 | 134 (1.3) | 9 (2.2) | 125 (1.2) |
| Sex | |||
| Male | 6262 (59.0) | 264 (63.0) | 5998 (58.8) |
| Female | 4356 (41.0) | 155 (37.0) | 4201 (37.2) |
| Zones or city administrations | |||
| Kaffa | 3680 (34.6) | 122 (29.1) | 3558 (34.9) |
| Bench-Sheko | 2853 (26.9) | 117 (27.9) | 2736 (26.8) |
| Sheka | 2162 (20.4) | 105 (25.1) | 2057 (20.2) |
| South Omo | 1574 (14.8) | 56 (13.4) | 1518 (14.9) |
| Other | 350 (3.3) | 19 (4.5) | 331 (3.2) |
| Occupations | |||
| Health care worker | 1856 (17.5) | 113 (27.0) | 1743 (17.1) |
| Other government employees | 2634 (24.8) | 84 (20.0) | 2550 (25.0) |
| Self-employees | 2825 (26.6) | 71 (16.9) | 2754 (27.0) |
| Driver | 626 (5.9) | 32 (7.6) | 594 (5.8) |
| Prisoners | 1074 (10.1) | 107 (25.5) | 967 (9.5) |
| Others a | 1603 (15.1) | 12 (2.9) | 1591 (15.6) |
| Origins of specimens collections | |||
| Health facilities | 2190 (20.6) | 102 (24.3) | 2088 (20.5) |
| Quarantine center | 1376 (12.9) | 84 (20.0) | 1292 (12.7) |
| Community | 5635 (53.1) | 114 (27.2) | 5521 (54.1) |
| Treatment centers (follow-up) | 343 (3.2) | 12 (2.9) | 331 (3.2) |
| Prison | 1074 (10.1) | 107 (25.5) | 967 (9.5) |
NB: others: hotel workers and students.
Prevalence of SARS-CoV-2 Infections and Clinical Features of Patients
In this study, among a total of 10 618, 419 (3.9%) patients were confirmed to have SARS-CoV-2 infections. Among the 419 COVID-19 confirmed cases, 264 (63.0%) were male and 233 (55.6%) were from the age group of 19 to 35 years. Only 83 (19.8%) of the COVID-19 confirmed cases had one or more clinical symptoms, with cough accounting for 53 (63.8%), headache accounting for 44 (53.0%), fever >37°C, 32 (38.5%), and shortness of breath accounting for 23 (27.7%). From all patients with COVID-19, 37 (8.8%) presented with other comorbid conditions, of which 11 (2.6%) had diabetic mellitus, 8 (1.9%) had chronic respiratory disease, and 6 (1.4%) had cardiac problems. About 41 (9.8%) had a history of contact with confirmed cases, and 102 (24.4%) had a travel history to a high-risk place (Addis Ababa). Of all the tested cases, 275 (2.6%) were tested as follow-up, and 17 (4.1%) of them were positive for the second time (Table 2).
Table 2.
SARS COV-2 Infection and Clinical Feature of Patients Tested for SARS COV-2 at the COVID-19 Diagnostic Center, Southwest Districts of Ethiopia.
| Clinical and other information | Total |
Positives |
Negatives |
|---|---|---|---|
| N (%) | N (%) | N (%) | |
| Patients with COVID-19 symptoms | |||
| Yes | 814 (7.7) | 83 (19.8) | 731 (7.2) |
| No | 9804 (92.3) | 336 (80.2) | 9468 (92.8) |
| Clinical symptoms | N = 814 | N = 83 | N = 731 |
| Cough | 426 (52.3) | 53 (63.8) | 373 (51.0) |
| Fever | 643 (79.0) | 32 (38.5) | 511 (69.9) |
| Shortness of breath | 234 (28.7) | 23 (27.7) | 211 (28.9) |
| Sore throat | 201 (24.7) | 15 (18.1) | 186 (25.4) |
| Headache | 455 (55.9) | 44 (53.0) | 411 (56.2) |
| Easy fatigue | 727 (89.3) | 56 (67.5) | 671 (91.8) |
| More than 1 symptoms | 794 (97.5) | 81 (97.6) | 713 (97.5) |
| Patient with chronic disease | |||
| Yes | 250 (2.4) | 37 (8.8) | 213 (2.1) |
| No | 10 368 (97.6) | 382 (91.2) | 9986 (97.9) |
| Patient with chronic disease conditions | |||
| Diabetic mellitus | 42 (0.4) | 11 (2.6) | 31 (0.3) |
| Hypertension | 34 (0.3) | 4 (1.0) | 30 (0.3) |
| HIV/AIDS | 41 (0.4) | 3 (0.7) | 38 (0.4) |
| Chronic respiratory problems | 32 (0.3) | 8 (1.9) | 24 (0.2) |
| Cardiac problems | 37 (0.3) | 6 (1.4) | 31 (0.3) |
| Pregnancy | 64 (0.6) | 5 (1.2) | 59 (0.6) |
| More than 1 chronic disease | 24 (0.2) | 8 (1.9) | 16 (0.2) |
| Contact with confirmed cases | |||
| Yes | 91 (0.9) | 41 (9.8) | 50 (0.5) |
| No | 10 527 (99.1) | 378 (90.2) | 10 149 (99.5) |
| History of visit to high-risk place (Addis Ababa) | |||
| Yes | 1185 (11.2) | 102 (24.4) | 1083 (10.6) |
| No | 9433 (88.8) | 317 (75.6) | 9116 (89.4) |
| Reason with testing | |||
| New | 10 343 (97.4) | 402 (95.9) | 9941 (97.5) |
| Follow-up | 275 (2.6) | 17 (4.1) | 258 (2.5) |
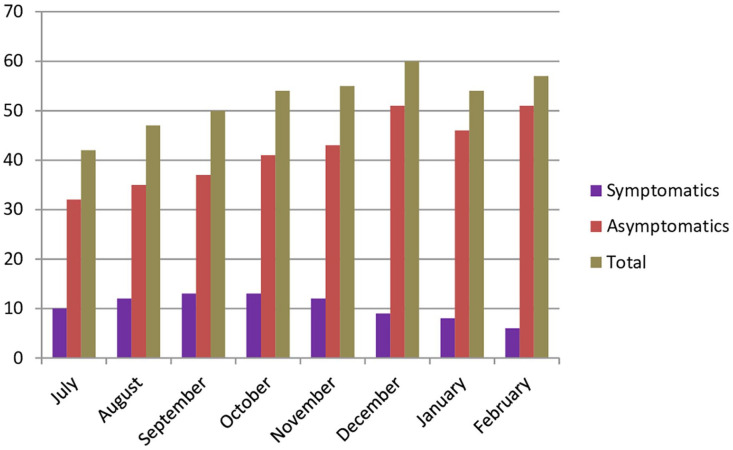
Monthly Comparison of Symptomatic and Asymptomatic COVID-19 Cases
From a total of 419 COVID-19 cases, only 83 (19.8%) patients show at least 1 clinical symptom of COVID-19 disease. The number of relatively asymptomatic cases increased from the first month of surveillance to the last (Figure 1).
Figure 1.
Monthly comparison of symptomatic and asymptomatic COVID-19 cases at the COVID-19 diagnostic center, southwest districts of Ethiopia.
Factors Associated With SARS COV-2 infections
Using a bivariate and multivariate logistic regression, many variables were analyzed for their significant association with SARS COV-2 infections. The age category of 36 to 59, male sex, and occupations were the independent predictors of SARS-CoV-2 infections based on the analysis using a bivariate logistic regression. Similarly, the presence of comorbid conditions was an independent predictor of SARS-CoV-2 infections among clinical variables. However, after adjusting for potential confounding factors using multivariate analysis, male sex, occupations, and the presence of comorbid conditions were the independent predictors for SARS-CoV-2 infections. Compared with females, males were found to be 1.25 times (AOR = 1.248; 95% CI: 1.007, 1.547) more likely to develop SARS-CoV-2 infections. Patients with a health worker’s occupation and prisoners were 3.19 times (AOR = 3.187; 95% CI: 1.960, 5.182) and 2.12 times (AOR = 2.118; 95% CI: 1.104, 4.062) more likely to get SARS-CoV-2 infections, respectively, than drivers. Patients with other comorbid conditions were 2.97 times (AOR = 2.972; 95% CI: 1.649, 5.358) more likely to develop SARS-CoV-2 infections than patients without a history of the events (Table 3).
Table 3.
Factors Associated With SARS-COV-2 Infections at the COVID-19 Diagnostic Center, Southwest Districts of Ethiopia.
| Variables | SARS-CoV-2 infections | COR (95% CI) | AOR (95% CI) | |
|---|---|---|---|---|
| Yes, N (%) | No, N (%) | |||
| Age in years | ||||
| ≤18 | 31 (7.4) | 529 (5.2) | 1.229 (0.570-2.646) | ― |
| 19-35 | 233 (55.6) | 5301 (52.0) | 1.638 (0.822-3.263) | ― |
| 36-59 | 146 (34.8) | 4243 (42.6) | 2.092 (1.043-4.198) a | ― |
| ≥60 | 9 (2.2) | 125 (1.2) | Ref | ― |
| Sex | ||||
| Male | 264 (63.0) | 5993 (58.8) | 1.198 (0.977-1.463) a | 1.248 (1.007, 1.547) a |
| Female | 155 (37.0) | 4206 (37.2) | Ref | Ref |
| Occupation | ||||
| Health workers | 113 (27.0) | 1743 (17.1) | 3.150 (1.953, 5.082) a | 3.187 (1.960, 5.182) a |
| Government employee | 84 (20.0) | 2550 (25.0) | 5.504 (3.394, 8.923) | ― |
| Self-employee | 71 (16.9) | 2754 (27.0) | 2.905 (1.866, 4.524) | ― |
| Driver | 32 (7.6) | 594 (5.8) | Ref | Ref |
| Prisoners | 107 (25.5) | 967 (9.5) | 3.052 (1.659, 5.615) a | 2.118 (1.104, 4.062) a |
| Others | 12 (2.9) | 1591 (15.6) | 2.543 (1.601, 3.998) | ― |
| Comorbid conditions | ||||
| Yes | 37 (8.8) | 213 (2.1) | 4.541 (3.156, 6.533) a | 2.972 (1.649, 5.358) a |
| No | 382 (91.2) | 9986 (97.9) | Ref | Ref |
| History of visit to high-risk place (Addis Ababa) | ||||
| Yes | 102 (24.4) | 1083 (10.6) | 0.920 (0.732, 1.157) | ― |
| No | 317 (75.6) | 9116 (89.4) | ||
NB: variables showing significant associations.
SARS-COV-2 Infections With Regard to Comorbidity Conditions
Using a bivariate and multivariate logistic regression, different comorbid conditions were analyzed for their significant association with SARS-CoV-2 infections in this study. Of these, diabetic mellitus, chronic respiratory disease, cardiac problems, and patients with hypertension were the independent predictors for SARS-CoV-2 infections on analysis using a bivariate logistic regression. However, after adjusting for potential confounding factors using multivariate analysis, diabetes Mellitus, and chronic respiratory problems were the independent predictors for SARS-CoV-2 infections. Patients with diabetes were found to be 4.76 times (AOR = 4.765; 95% CI: 1.977-11.485) more likely to develop SARS-CoV-2 infections. Similarly, those with other respiratory problems were 3.27 times (AOR = 3.267; 95% CI: 1.146-9.317) more likely to develop SARS-CoV-2 infections (Table 4).
Table 4.
SARS-COV-2 Infections With Regard to Comorbidity Conditions at the COVID-19 Diagnostic Center, Southwest Districts of Ethiopia.
| Types of chronic disease | COVID-19 infections | COR (95% CI) | AOR (95% CI) | P-value | |
|---|---|---|---|---|---|
| Yes, N (%) | No, N (%) | ||||
| Diabetics mellitus | |||||
| Yes | 11 (2.6) | 31 (0.3) | 8.843 (4.414, 17.718) a | 8.235 (4.039-16.789) a | .001 |
| No | 408 (97.4) | 10 168 (99.7) | |||
| Chronic respiratory disease | |||||
| Yes | 8 (1.9) | 24 (0.2) | 8.252 (3.685-18.480) a | 7.847 (3.451-17.854) a | .001 |
| No | 411 (98.1) | 10 155 (99.8) | |||
| Cardiac problems | |||||
| Yes | 6 (1.9) | 31 (0.3) | 4.765 (1.977-11.485) a | 2.480 (0.932-6.600) | .069 |
| No | 413 (98.1) | 10 168 (99.7) | |||
| Hypertension | |||||
| Yes | 4 (1.0) | 30 (0.3) | 3.267 (1.146-9.317) a | 1.335 (0.394-4.518) | .323 |
| No | 415 (99.0) | 10 169 (99.7) | |||
| HIV/AIDS | |||||
| Yes | 3 (0.7) | 38 (0.4) | 1.928 (0.593-6.272) | ― | .267 |
| No | 416 (99.3) | 10 160 (99.6) | |||
| Pregnancy | |||||
| Yes | 5 (1.2) | 59 (0.6) | 2.076 (0.829-5.199) | ― | .119 |
| No | 414 (98.8) | 10 140 (99.4) | |||
NB: variables showing significant associations.
Discussion
This study was conducted to assess the magnitude of SARS-CoV-2 infections, clinical characteristics, and associated risk factors in the southwest district of Ethiopia. Accordingly, about 3.9% of tested patients were confirmed to have SARS-CoV-2 infections. This result is comparable with a study finding in Oromia region, Ethiopia, 15 in which the magnitude of SARS-CoV-2 infections was 5.5%. In comparing other African countries, our finding is lower than a finding from Nigeria, 16 in which the magnitude of SARS-CoV-2 infections was 14.6%. Our finding is also lower than findings from Thailand 17 and Germany, 18 where the magnitude of SARS-CoV-2 infections was 13.1% and 13.8%, respectively. These differences in the proportions of SARS-CoV-2 infections could result from different methods of testing, types of study populations, different study settings, and differences in the age groups studied. In addition, the progress toward improving care and reducing COVID-19 morbidity and mortality may not be similar among countries.
In this study, SARS-CoV-2 detection was made by using RT-PCR, and 80.2% of SARS-CoV-2 confirmed cases were asymptomatic. This finding is in agreement with other study finding in Ethiopia,15,19 in Bahrain, 20 and in Qatar, 21 in which the average prevalence of asymptomatic COVID-19 cases was 81.0%. Other systematic review and meta-analysis reported, the proportion of asymptomatic COVID-19 cases among the included studies ranged from 1.4% to 78.3% and the pooled proportion was 25%. 22 In this study, from the reported (19.8%) symptoms at the time of diagnosis, headache, cough, and fever were the most common symptoms. In agreement with this finding, a systematic review and meta-analysis, 23 study reported in Iran, 24 and WHO interim clinical guidance, 25 fever, cough, fatigue, and anorexia are the most common signs of SARS-CoV-2 infections. Therefore, since, asymptomatic cases play an essential role in transmitting SARS-CoV-2 infection; this study may have significant contribution to our knowledge in the area of prevalence, clinical features and possible risk factors of SARS-CoV-2 infections for clinical workers, policy makers and for other researchers.
With regard to age distributions, despite it is not statistical significant, the high frequency (55.6%) of SARS-CoV-2 infected patients was found to be in the age group of 19 to 35 years. Our finding is similar with a regional study finding in Ethiopia,15,19 in which majority of SARS-CoV-2 infected patients was found to be in the age group of 20 to 39 years. This is an indication that productive age groups may also have a great chance for SARS-CoV-2 infection, although it may be asymptomatic and non- progressive.
In this study, from socio-demographic variables, being male sex was significant contributing factors for SARS-CoV-2 infections, which also reported in other study findings.18,26 This may be explained by the fact that, in our situation, those males may frequently move from place to place, which may increase the chances of exposure to SARS-CoV-2 infected people. This finding is also supported by other studies,27,28 in which possibility of human to human transmission in a closed environment and among family members is greater.
Furthermore, being health worker and prisoners as their occupation increases the chances of getting SARS-CoV-2 infections by 3.19 and 2.12 times, respectively. The contributions of individual’s occupations for SARS-CoV-2 infections were also reported in other studies.29,30 This study also revealed that, the chances of SARS-CoV-2 detection were also 2.12 and 1.10 times higher for specimen originated from prisoners and from health facilities, respectively. This may also be indicated by the fact that individuals living in a risky and closed environment have a higher likelihood of transmission and a higher positivity rate.
In this study, many co-diseases conditions were checked their significant association with SARS-CoV-2 infections using binary and multivariate logistic regression model. Of these, diabetic mellitus and chronic respiratory disease were 4.76 and 3.27 times increased the risk of having SARS-CoV-2 infection, respectively. This result is supported by other studies done in Saudi Arabia, 31 In India, 32 and in Ethiopia,19,33 in which diabetic mellitus and chronic respiratory disease was the determinant factor for infection with SARS-CoV-2. Other studies also indicated that, a SARS-CoV-2 infections and severity is very significant in people with immunocompromised and non- communicable disease conditions.26,34-37 Thus, this finding suggests that, although currently an effective vaccine is ready, its distribution is limited, and hence to reduce transmission, continuous identifications and isolate individuals who are contagious are essentials. In additions, to prevent the burden of SARS-CoV-2 infections, the efforts should be focused not only on the preventions of SARS-CoV-2 infections but also on the other contributing co-morbidity factors, such as non- communicable diseases.
There are limitations in our study. First, we are unable to do association for certain risk factors due to incomplete information in the surveillance database sheet. Second, we did not include the clinical course during follow-up in this report as the surveillance database included only clinical status at requesting laboratory diagnosis. Hence, patients who were asymptomatic during the initial diagnosis might have developed symptoms later that could have underestimated the number of symptomatic cases.
Conclusion
Despite the fact that overall laboratories confirmed COVID-19 prevalence in the study area was low and dynamic, it was spread to all study zones. This highlights the importance of implementing the most effective public health strategies to prevent further spread and reduce the burden of SARS-CoV-2 infections. In addition, early detection and management, as well as intervening on other comorbidities, are essential.
Footnotes
Authors’ Contributions: DM, MA, AS, TW, TD, ET, GA YM, AN, MT, AB and MA were participated in the study design and were responsible for recruitment, sampling and for the laboratory result analyses. DM analyzed the data and drafted the manuscript. All the authors have contributed to the manuscript and approved the final version.
Availability of Data and Materials: All the data used in this study are available and can be obtained from the corresponding author (dmuleta4all@gmail.com) up on request.
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Ethical Approval and Consent to Participate: The authors have obtained authorization and ethical approval from Mizan-Tepi University research ethics review committee and community service coordinating office to use and analysis the surveillance data. Informed consent was obtained directly from the study subjects and for those under the age of 18 years; it was obtained from their parents or from their legal guardians. All methods were performed in accordance with the relevant guidelines and regulations.
ORCID iDs: Dassalegn Muleta  https://orcid.org/0000-0001-9895-722X
https://orcid.org/0000-0001-9895-722X
Teshale Worku  https://orcid.org/0000-0001-9804-0278
https://orcid.org/0000-0001-9804-0278
References
- 1.Cazzato G, Colagrande A, Cimmino A, et al. HMGB1-TIM3-HO1: a new pathway of inflammation in skin of SARS-CoV-2 patients? A retrospective pilot study. Biomolecules. 2021;11(8):1219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Li Q, Guan X, Wu P, et al. Early transmission dynamics in Wuhan, China, of novel coronavirus–infected pneumonia. N Engl J Med. 2020;382:1199-1207. doi: 10.1056/nejmoa2001316 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Zhu N, Zhang D, Wang W, et al. A novel coronavirus from patients with pneumonia in China, 2019. N Engl J Med. 2020;382:727-733. doi: 10.1056/nejmoa2001017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.European Centre for Disease Prevention and Control. Rapid risk assessment: outbreak of acute respiratory syndrome associated with a novel corona virus, Wuhan, China; first update – 22 January 2020. ECDC: Stockholm; 2020. [Google Scholar]
- 5.CDC. 2019 novel coronavirus, Wuhan, China. 2020. Accessed February 1, 2020. https://www.cdc.gov/coronavirus/2019-nCoV/summary.html
- 6.WHO. Novel coronavirus–China. 2020. Accessed February 1, 2020. https://www.who.int/csr/don/12-january-2020-novel-coronavirus-china/en/
- 7.Zhou P, Yang XL, Wang XG, et al. A pneumonia outbreak associated with a new coronavirus of probable bat origin. Nature. 2020;579:270-273. doi: 10.1038/s41586-020-2012-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Jackson CB, Farzan M, Chen B, Choe H.Mechanisms of SARS-CoV-2 entry into cells. Nat Rev Mol Cell Biol. 2022;23(1):3-20. doi: 10.1038/s41580-021-00418-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Perlman S.Another decade, another coronavirus. N Engl J Med. 2020;382:760-762. doi: 10.1056/nejme2001126 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.World Health Organization. Global surveillance for human infection with corona virus disease (COVID-2019), Interim guidance, Geneva. 2020. https://www.who.int/publicationsdetail/global-surveillance-for-humaninfection-with-novel-coronavirus-(2019-ncov)
- 11.National Public Health Emergency Operation Center (PHEOC) of Ethiopia. COVID-19 Weekly Bulletin. Ethiopian Public Health Institute. https://www.ephi.gov.et/ [Google Scholar]
- 12.Federal Democratic Republic of Ethiopia Central Statistical Agency. Population projection of Ethiopia for all regions at Wereda level from 2014–2017. 2013:1–118. https://www.scribd.com/document/343869975/Population-Projection-At-Wereda-Level-from-2014-2017-pdf
- 13.World Health Organization. Laboratory biosafety guidance related to the novel coronavirus (2019-nCoV). 2020. https://www.who.int/docs/defaultsource/coronaviruse/laboratory-biosafety-novelcoronavirus-version-1-1.pdf?sfvrsn=912a9847_2
- 14.World health Organization (WHO). Laboratory testing for coronavirus disease (COVID-19) in suspected human cases. Interim guidance. March19, 2020. [Google Scholar]
- 15.Gudina EK, Gobena D, Debela T, Donaldson LJ, Jones GT.COVID-19 in Oromia Region of Ethiopia: a review of the first 6 months’ surveillance data. BMJ Open. 2021;11:e046764. doi: 10.1136/bmjopen-2020-046764 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Salako AO, Amoo OS, Odubela OO, et al. Prevalence and clinical characteristics of coronavirus disease 2019 seen at a Testing Centre in Lagos Nigeria. West Afr J Med. 2021;38(1):54-58. [PubMed] [Google Scholar]
- 17.Bruminhent J, Ruangsubvilai N, Nabhindhakara J, Ingsathit A, Kiertiburanakul S.Clinical characteristics and risk factors for Coronavirus disease 2019 (COVID-19) among patients under investigation in Thailand. PLoS One. 2020;15(9):e0239250. doi: 10.1371/journal.pone.0239250 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Jacob L, Koyanagi A, Smith L, Haro JM, Rohe AM, Kostev K.Prevalence of and factors associated with COVID-19 diagnosis in symptomatic patients followed in general practices in Germany between March 2020 and March 2021. Int J Infect Dis. 2021;111:37-42. doi: 10.1016/j.ijid.2021.08.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Abraha HE, Gessesse Z, Gebrecherkos T, et al. Clinical features and risk factors associated with morbidity and mortality among patients with COVID-19 in northern Ethiopia. Int J Infect Dis. 2021;105:776-783. doi: 10.1016/j.ijid.2021.03.037 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Almadhi MA, Abdulrahman A, Sharaf SA, et al. The high prevalence of asymptomatic SARS-CoV-2 infection reveals the silent spread of COVID-19. Int J Infect Dis. 2021;105:656-661. doi: 10.1016/j.ijid.2021.02.100 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Musa OAH, Chivese T, Bansal D, et al. Prevalence and determinants of symptomatic COVID-19 infection among children and adolescents in Qatar: a cross-sectional analysis of 11 445 individuals. Epidemiol Infect. 2021;149:e203. doi: 10.1017/S095026882100203X. e193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Alene M, Yismaw L, Assemie MA, et al. Magnitude of asymptomatic COVID-19 cases throughout the course of infection: a systematic review and metaanalysis. PLoS One. 2021;16(3):e0249090. doi: 10.1371/journal.pone.0249090 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Badal S, Thapa Bajgain K, Badal S, Thapa R, Bajgain BB, Santana MJ.Prevalence, clinical characteristics, and outcomes of pediatric COVID-19: a systematic review and meta-analysis. J Clin Virol. 2021;135:104715. doi: 10.1016/j.jcv.2020.104715 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Goshayeshi L, Akbari Rad M, Bergquist R, Allahyari A, Hashemzadeh K, Hoseini B.Demographic and clinical characteristics of severe covid-19 infections: a cross-sectional study from Mashhad University of Medical Sciences, Iran. BMC Infect Dis. 2021;21:656. doi: 10.1186/s12879-021-06363-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.WHO. Interim clinical guidance for management of patients with confirmed Coronavirus disease (COVID-19). 2020. Accessed March 20, 2020. https://www.cdc.gov/coronavirus/2019-ncov/hcp/clinical-guidance-management-patients.html
- 26.Geng MJ, Wang LP, Ren X, et al. Risk factors for developing severe COVID-19 in China: an analysis of disease surveillance data. Infect Dis Poverty. 2021;10:81. doi: 10.1186/s40249-021-00868-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Phan LT, Nguyen TV, Luong QC, et al. Importation and human-to-human transmission of a novel coronavirus in Vietnam. N Engl J Med. 2020;382(9):872-874. doi: 10.1056/NEJMc2001272 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Yu P, Zhu J, Zhang Z, Han Y.A familial cluster of infection associated with the 2019 novel coronavirus indicating possible Person-to-Person transmission during the incubation period. J Infect Dis. 2020;221:1757-1761. doi: 10.1093/infdis/jiaa077 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Wei JT, Liu ZD, Fan ZW, Zhao L, Cao WC.Epidemiology of and risk factors for COVID-19 infection among health care workers: a multi-centre comparative study. Int J Environ Res Public Health. 2020;17(19):7149. doi: 10.3390/ijerph17197149 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Alshamrani MM, El-Saed A, Al Zunitan M, Almulhem R, Almohrij S.Risk of COVID-19 morbidity and mortality among healthcare workers working in a large tertiary care hospital. Int J Infect Dis. 2021;109:238-243. doi: 10.1016/j.ijid.2021.07.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Khan A, Althunayyan S, Alsofayan Y, et al. Risk factors associated with worse outcomes in COVID-19: a retrospective study in Saudi Arabia. East Mediterr Health J. 2020;26(11):1371-1380. doi: 10.26719/emhj.20.130 [DOI] [PubMed] [Google Scholar]
- 32.Dey K, Dey K.SARS-CoV-2 pandemic, COVID-19 case fatality rates and deaths per million populations in India. J Bioinform Comput Syst Biol. 2020;2(1):5000110. [Google Scholar]
- 33.Tolossa T, Wakuma B, Seyoum Gebre D, et al. Time to recovery from COVID-19 and its predictors among patients admitted to treatment center of Wollega University Referral Hospital (WURH), Western Ethiopia: survival analysis of retrospective cohort study. PLoS One. 2021;16(6):e0252389. doi: 10.1371/journal.pone.0252389 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Fadl N, Ali E, Salem TZ.COVID-19: risk factors associated with infectivity and severity. Scand J Immunol. 2021;93(6):e13039. doi: 10.1111/sji.13039 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Oyelade T, Alqahtani JS, Hjazi AM, Li A, Kamila A, Raya RP.Global and regional prevalence and outcomes of COVID-19 in people living with HIV: a systematic review and meta-analysis. Trop Med Infect Dis. 2022;7:22. doi: 10.3390/tropicalmed7020022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Cen Y, Chen X, Shen Y, et al. Risk factors for disease progression in patients with mild to moderate coronavirus disease 2019—a multi-centre observational study. Clin Microbiol Infect. 2020;26(9):1242-1247. doi: 10.1016/j.cmi.2020.05.041 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Lv Z, Lv S.Clinical characteristics and analysis of risk factors for disease progression of COVID-19: a retrospective cohort study. Int J Biol Sci. 2021;17(1):1-7. doi: 10.7150/ijbs.50654 [DOI] [PMC free article] [PubMed] [Google Scholar]