Abstract
Any long-term medical condition or disability among children is a significant health issue. This study measured the incidence rate of any medical condition or disability among children from a nationally representative birth cohort, then used the random effect parametric survival regression model to assess whether the hazard of any medical condition or disability in children is associated with maternal physical and mental health characteristics (obesity, general health status, having a medical condition, stressful life events or mental illness). The study followed up 5019 children from the Longitudinal Study of Australian Children, assessing their time-to-event data from birth (2004) to 14 or 15 years of age (2018). The hazard rate of any medical condition or disability was 26.11 per 1000 person-years for all the children and 29.29 for the males—a noticeable gender difference. It was the highest (hazard rate: 62.90) among the children when their mothers had a medical condition, while the hazard rate was 22.40 per 1000 person-years among the children whose mothers had no medical conditions. The parametric panel regression results also suggested that the children of mothers with a medical condition during the 15-year study period were more likely to have a medical condition or disability (hazard ratio [HR]: 2.61, 95% confidence interval [CI]: 2.24–3.02) compared to the children of mothers with none. Similar trends were observed among children of mothers who had fair or poor general health (HR: 1.48, 95% CI: 1.15–1.91), obesity (HR: 1.40, 95% CI: 1.18–1.66) or experienced stressful life events (HR: 1.23, 95% CI: 1.06–1.43) over time compared to those whose mothers did not. These findings suggest that additional healthcare interventions targeting mothers with medical conditions, obesity, poor general health, or mental illness would help minimise the risk of medical conditions and disabilities among children.
Keywords: Longitudinal study, Maternal health, Child health, Hazard rate, Hazard ratio, Long-term health condition, Disability, Survival analysis
Highlights
-
•The hazard rate of any medical condition or disability in children was
-
o26.11 per 1000 person-year.
-
ohighest (62.98) among the children whose mothers had a medical condition.
-
o
-
•Children were more likely to have a medical condition or disability if their mothers
-
ohad a medical condition.
-
oexperienced fair or poor health, obesity or mental illness.
-
o
1. Introduction
Medical conditions and disabilities are significant disease burdens for children. Based on the Centers for Disease Control and Prevention's definitions, the term ‘medical condition or disability’ refers to any disability or long-term medical condition of adults or children. Such conditions include sight, hearing and speech problems, blackouts, chronic pain, nervousness, head injury, difficulty breathing, gripping, or learning, limited use of arms, fingers, legs, or feet, and other long-term health conditions (National Center on Birth Defects, 2020). The Global Burden of Disease study estimates that of children aged 14 or younger worldwide, 5.1% (93 million) and 0.7% (13 million) live with moderate and severe disability respectively (World Health Organization, 2008). Likewise, within Australia, disability among children is a significant health issue. In 2018, almost 7.7% (357,500) of children under 15 years of age had a medical condition or disability. Further, of all the children, 4.5% (209,300) had profound or severe disability (Australian Bureau of Statistics, 2019).
Universal health coverage is a core aim of the United Nations' Sustainable Development Goal 3: ‘to ensure healthy lives and promote wellbeing for all, at all ages’ (United Nations, 2015). To promote the wellbeing of children and adolescents, who are a significant proportion of the population, and monitor their ongoing health, there is a dire need to better identify problems and essential indicators in health areas to inform national programs and policies. Only a few epidemiological studies have investigated the relationship between maternal health characteristics and medical conditions or disabilities in children from national longitudinal cohorts (Obel et al., 2009; Ou et al., 2010; O'Reilly & Reynolds, 2013). Identifying children's health and disability issues in a national population can contribute to planning appropriate prevention and intervention strategies for target population groups.
The extant literature shows that children's health status, such as having medical conditions or disabilities in childhood, depends on their mothers' physical and mental health characteristics (Chen et al., 2020; Maïano et al., 2016; Schendel & Bhasin, 2008; Schieve et al., 2016; Zhong et al., 2017). It is well established that mothers' good physical health and healthy lifestyles can reduce chronic morbidity risks for children (Anderson et al., 2020; Obel et al., 2009; O'Reilly & Reynolds, 2013). Several studies have linked suboptimal children's health and lifestyle environments to adult disease (Ou et al., 2010; O'Reilly & Reynolds, 2013; Park et al., 2012). For example, mothers with obesity are more likely to have children with obesity who, in turn, are more likely to become obese adults (Park et al., 2012). Maternal obesity is associated with increased body mass index (BMI) of offspring across infancy (Linabery et al., 2013), adolescence (Naess et al., 2016) and adulthood (Eriksson et al., 2015; Hochner et al., 2012). Maternal stress or anxiety during pregnancy and mental illness in later life after childbirth are also associated with children's and adolescents' poor general health and long-term health condition (Ahmad, Kabir, Keramat, et al., 2021). A recent review paper determined that maternal obesity during pregnancy negatively affected aspects of children's learning, memory and motivation and increased their likelihood of experiencing affective disorders, attention-deficit hyperactivity disorder or autism spectrum disorders (Contu & Hawkes, 2017). However, none of these studies deployed a longitudinal survival analysis to identify these risk factors. Whereas a survival analysis answers to the following question: how long did it take until a child develop the disease? The hazard function, derived from the regression of survival analysis, can lend more insight in the time-to-event analysis which is absent in linear or logistic regression (Ahmad et al., 2022). This is because logistic regression simply answers the question of whether a child has faced the disease (of study) or not (Geoge et al., 2014). Thus, evaluating the prevalence and risk factors of any medical condition or disability through the survival analysis of time-to-event data is very scare in the extant literature.
This study addresses these limitations of the extant literature and contributes knowledge to the longitudinal dimension of the survival analysis. Based on the study evidence of the well-known developmental origins hypothesis of health and disease (Ahmad, Kabir, Keramat, et al., 2021; Eriksson et al., 2015; Hochner et al., 2012; Linabery et al., 2013; Naess et al., 2016), the present study hypothesised that mothers’ physical and mental health (namely obesity, general health, medical conditions, stressful life events, and mental illness) are associated with the hazard of having medical conditions and disabilities among their children over time. To test this hypothesis, the study examined a nationally representative Australian birth cohort (a 15-year follow-up study) to determine their hazard rate of having any medical condition or disability, then assessed the association of this hazard rate with maternal physical and mental health.
2. Methods
2.1. Data source and sample selection
The birth cohort of the Longitudinal Study of Australian Children (LSAC) was used as the data source. LSAC is a representative household survey of Australian children that began in 2004. Every two years, it collects information about the children's development and physical and socio-emotional health using a model based on the bio-ecological framework of human development (Zubrick et al., 2000). The present study used LSAC Wave 1 (2004) as its baseline (n = 5107) and followed the children up to Wave 8 (n = 3127). All the children and their mothers were recruited in 2004 at Wave 1. The survey was conducted when the children were at their age of 3–15 months. Over the waves, few non-mother caregivers were respondents for the interviews to report their children's conditions. However, as we are looking into the foetal origins, which is solely related with biological mothers, we excluded the observations (around 3%) which are not from biological mothers. This study considered the relevant maternal demographic characteristics and health indicators that the LSAC study measured across the waves to devise the survival model of whether a child had a medical condition or disability.
2.2. Analytical strategy
This study modelled the influence of maternal health on the incidence of any medical condition or disability in children. Maternal different health indicators were summarized across all waves and any medical condition or disability of the child was considered as the time-to-event variable over the whole follow-up period. The longitudinal survival model handled the time varying covariates through summarising them across all waves and thus measured the hazard ratio as a longitudinal estimate.
2.3. Outcome variables
The children's caregivers provided information about the children's medical conditions and disabilities. The term ‘any medical condition or disability’ included long-term medical conditions and disabilities and other disabilities that limited everyday activities. Long-term medical conditions and disabilities were identified from the responses of the children's mothers, if they report any of the following: sight problems, hearing problems, speech problems, blackouts, difficulty learning, limited use of arms or fingers, difficulty gripping, limited use of legs and feet, other physical conditions or disfigurements, shortness of breath or breathing difficulties, chronic or recurring pain or discomfort causing restriction, nervous conditions causing restriction, head injuries and long-term effects as a result of head injuries or brain damage or brain stroke, other long-term conditions causing restriction, or other long-term treated conditions such as arthritis, asthma, heart disease, Alzheimer's disease, or dementia that had lasted or were likely to last for six months or more. The details of this particular questionnaire have been provided in Appendix A. A dichotomous variable was generated and coded with the value 1 for having any of these conditions and 0 for not having any of them. Later, to estimate the hazard rate of any health condition or disability, time-to-event data were generated from the longitudinal data of all waves using the survival function of the statistical software package Stata 16.
2.4. Independent variables
Based on the existing literature (Ahmad, Kabir, Keramat, & Khanam, 2021a, Ahmad et al., 2021b), this study included the following maternal physical or mental health related variables as independent variables: obesity, general health status, having a medical condition, stressful life events, mental illness and mental stress or anxiety during pregnancy. Maternal obesity was measured based on BMI scores and categorised as follows: underweight (BMI <18.00), healthy weight (BMI 18.00–24.99), overweight (BMI >25.00) and obesity (BMI >30.00). The general health was measured from the self-rated health status reported by the mothers and categorised as per the following ordinal scale: excellent, very good, good, fair/poor. Mothers having a medical condition (yes or no) were measured based on whether the mothers had any medical condition or disability (as listed in the outcome variable section) that had lasted or were likely to last for six months or more. Any stressful life events (yes or no) variable accounts for capturing whether mothers faced any of the more than twenty listed events in the last year from the date of interviews, for example, marriage separation or demise of friend or relatives, losing job or thought of losing job, valuable lost or stolen, legal problems, moving to a new house, affected by natural disaster, etc. Mental illness of mothers were measured from the K6 depression scale scores. They were asked how often they had felt: i) nervous, ii) hopeless, iii) restless or fidgety, iv) that everything was an effort, v) so sad that nothing would cheer you up, or vi) worthless. The responses were scored on a 5-point scale from 1 = all of the time to 5 = none of the time; then the scores were reverse coded, summed and adjusted to generate a total score ranging from 1 to 30, where higher scores represented higher levels of psychological distress. LSAC categorised the respondents’ mental illness based on the K6 scores as per the previous research suggestion and the recommendation of Australian Bureau of Statistics (Australian Bureau of Statistics, 2007). Respondents were categorised as experiencing probable serious mental illness if their K6 scores were in between 19 and 30.
The above-mentioned variables were measured in all the waves and reflect the physical and mental health status of mothers over the 15-year follow-up period of this study. Besides, this study also considered maternal mental status during pregnancy, revealed from the question: “During this pregnancy, did you have problems with stress, anxiety or depression? (yes or no)”. This variable was measured only in Wave 1 and hence included in the model as a time-invariant independent variable to predict the longitudinal medical condition or disability in the study children.
2.5. Control variables
This study considered the following socio-demographic covariates as confounding variables while the regression models were fitted: the child's age, their sex (male or female), whether English was spoken at home (yes or no), whether the child was living with both parents or with a single parent, the indigenous status of the child (yes or no), the age of the mother at childbirth, the employment statuses of the parents (employed, unemployed, or not in the labour force), the mother's level of education (Year 12 or less, certificate, graduate degree or diploma, or postgraduate) and the remoteness of the family residence (highly accessible, accessible to moderately accessible, or remote to very remote).
2.6. Statistical analyses
Initially, descriptive statistics were used to summarise the characteristics of the children and mothers. Then, the survival analysis was performed to determine the incidence (hazard) of any medical condition or disability from the 15 years of longitudinal data. In modeling the survival analysis, the panel data parametric survival sub-model – the random effect multiplicative or proportional hazard model was used. The multivariate model was fitted to adjust for confounders related to child and maternal health. Further, to analyse the gender differences the survival models were analysed on samples stratified by sex.
To estimate the hazard rate against maternal health indicators across all waves, the number of incidents of occurring any medical condition or disability per 1000 person-years among children against each category of maternal health indicators across all waves were considered. For estimating the hazard ratio of developing any medical condition or disability, the panel data parametric hazard model was utilised using Weibull distribution, instead of Cox regression model. Hence, this study did not require to provide the assumption of the proportional hazards. The basic detail of the statistical method for survival analysis has been described below.
A survival model has a tri-variate response – , t, d, where is the starting time under observation ≥ 0; t is the ending time under observation t ≥ ; and d is an indicator for having any medical condition or disability (failure), d ∈ (0,1). Let i = 1,…, n panels, j = 1,…, , and be unobservable panel-level random effects that are independent and identically distributed N (0, ). The hazard function as per the multiplicative or proportional hazards (PH) model is as below:
for some baseline hazard function , which is assumed to be parametric. The survivor function for the Weibull family is the complement of the cumulative distribution function:
The conditional density for having a medical condition or disability (failure) at time t is:
and the conditional probability of survival without having any medical condition or disability (failure) up to time t is:
In this paper, the Weibull models have been implemented through the STATA command syntax –xtstreg. The multivariate model was fitted with adjustment for confounders related to child and maternal health. Further, to analyse the gender differences the survival models were analysed on samples stratified by sex. If the p-value of a particular exposure was less than or equal to 0.05 in the multivariate regression analyses, only then the predictor was considered as statistically significant.
3. Results
3.1. Study participants
Table 1 shows the mothers and children's characteristics both at the baseline (Wave 1) and in the follow-ups (Waves 2 to 8). Among the 5019 participating children at baseline, 5.48% had a medical condition or disability and 51.03% were male. Among the mothers, 42.71% had a graduate/diploma or post graduate degree and 49.31% were employed, 20.14% and 14.33% were overweight and obese respectively, 24.43% had a medical condition, 54.77% were facing stressful life events and 15.32% had mental stress or anxiety during pregnancy. Repeated measures of maternal health characteristics of obesity, general health status, having any medical condition, stressful life events and mental illness based on Kesssler-6 scores have been presented in Table 1. During the 15-year follow-up period, 1980 participants (mother–child pairs) dropped out or were lost to follow-up. The number of mothers reported a medical condition were 24% at Wave 1 and dropped to 7–13% in subsequent waves. It is evident from existing research that women are at increased risk for chronic conditions during and after pregnancy, including gestational diabetes, hypertension, type 2 diabetes, and depression (Brown et al., 2015; Kim et al., 2017; Nicholson et al., 2006). However, over time these incidents are reduced to its normal prevalence rates. Details of the maternal medical condition or disability in Wave 1 and across all waves are shown in Appendix B. In Wave 8, 3127 mother–child pairs participated; among the mothers, 13.19% had a medical condition or disability, 28.26% were with obesity, 78.44% had stressful life events and 2.96% were experiencing mental illness.
Table 1.
Characteristics of the participants during baseline (Wave 1) and subsequent follow-ups, LSAC study, 2004–2018.
| Characteristics of the study participants | Baseline |
Subsequent follow-ups |
Baseline characteristics of drop-outs & losses in follow-ups (Waves 2–8, n = 1948) |
||||||
|---|---|---|---|---|---|---|---|---|---|
| Total sample in Wave 1, 2004 (n = 5019) |
Wave 2, 2006 (n = 4533) |
Wave 3, 2008 (n = 4315) |
Wave 4, 2010 (n = 4178) |
Wave 5, 2012 (n = 4020) |
Wave 6, 2014 (n = 3706) |
Wave 7, 2016 (n = 3327) |
Wave 8, 2018 (n = 3071) |
||
| % | % | % | % | % | % | % | % | % | |
| CHILDREN’S HEALTH | |||||||||
| Have any medical condition or disability | |||||||||
| Yes | 5.48 | 8.03 | 9.48 | 8.47 | 4.05 | 4.94 | 4.81 | 5.76 | 6.37 |
| MATERNAL HEALTH, 2004–2018 | |||||||||
| Obesity | |||||||||
| Underweight | 9.38 | 7.96 | 7.53 | 8.21 | 7.29 | 6.53 | 5.80 | 5.24 | 9.91 |
| Healthy weight | 35.86 | 34.94 | 37.78 | 40.16 | 39.90 | 38.37 | 35.32 | 33.41 | 29.16 |
| Overweight | 20.14 | 16.74 | 21.55 | 24.63 | 25.65 | 25.31 | 26.24 | 27.52 | 17.61 |
| Obese | 14.33 | 11.27 | 15.20 | 20.18 | 22.91 | 23.91 | 26.21 | 28.26 | 12.53 |
| Missing | 20.28 | 29.08 | 17.94 | 6.82 | 4.25 | 5.88 | 6.43 | 5.57 | 30.80 |
| General health | |||||||||
| Excellent | 15.66 | 15.40 | 18.59 | 20.54 | 17.21 | 18.46 | 15.57 | 15.79 | 12.22 |
| Very good | 36.92 | 36.05 | 38.77 | 44.04 | 43.58 | 42.04 | 41.24 | 40.15 | 31.16 |
| Good | 25.24 | 19.90 | 22.27 | 26.54 | 27.84 | 27.85 | 28.25 | 30.38 | 24.28 |
| Fair or poor | 6.59 | 4.74 | 7.14 | 6.99 | 8.11 | 7.15 | 10.28 | 10.32 | 7.60 |
| Missing | 15.58 | 23.91 | 13.23 | 1.89 | 3.26 | 4.51 | 4.66 | 3.35 | 24.74 |
| Have a medical condition | |||||||||
| Yes | 24.43 | 10.17 | 7.88 | 7.35 | 9.73 | 11.25 | 11.63 | 13.19 | 24.28 |
| Facing any stressful life events | |||||||||
| Yes | 54.77 | 51.38 | 48.09 | 83.34 | 79.73 | 78.44 | 78.63 | 78.44 | 51.49 |
| Mental illness of mothers based on Kessler-6 depression scale score | |||||||||
| Yes, have probable serious mental illness | 2.23 | 1.90 | 1.11 | 2.44 | 1.87 | 2.37 | 2.55 | 2.96 | 2.52 |
| Maternal mental stress or anxiety during pregnancya | |||||||||
| Yes | 15.32 | - | - | - | - | - | - | - | - |
| SOCIO-DEMOGRAPHIC CHARACTERISTICS | |||||||||
| Gender of the child | |||||||||
| Female | 48.97 | 49.04 | 48.64 | 48.40 | 48.68 | 48.70 | 48.69 | 48.55 | 49.64 |
| Male | 51.03 | 50.96 | 51.36 | 51.60 | 51.32 | 51.30 | 51.31 | 51.45 | 50.36 |
| Immunisation Status of child | |||||||||
| Not completely up-to-date | 9.33 | 8.67 | 8.64 | 8.90 | 9.05 | 8.66 | 8.66 | 8.53 | 10.59 |
| Breast feeding status | |||||||||
| Breastfed <6 months | 45.37 | 44.29 | 43.49 | 43.01 | 42.60 | 41.28 | 39.61 | 38.84 | 44.53 |
| Child has both parents | |||||||||
| Yes | 90.54 | 89.59 | 88.41 | 87.00 | 85.72 | 84.48 | 82.12 | 81.76 | 84.14 |
| Language spoken at home | |||||||||
| English | 89.43 | 90.24 | 90.75 | 90.71 | 90.82 | 91.12 | 91.61 | 91.53 | 86.13 |
| Is the child indigenous? | |||||||||
| Yes | 4.48 | 3.88 | 3.36 | 3.45 | 3.36 | 2.83 | 2.58 | 2.51 | 7.60 |
| Age of mothers at childbirth | |||||||||
| ≤ 18 | 1.20 | 0.90 | 0.88 | 0.74 | 0.67 | 0.51 | 0.42 | 0.36 | 2.52 |
| 19–34 | 72.92 | 72.20 | 71.87 | 72.02 | 71.67 | 71.24 | 70.63 | 70.43 | 76.85 |
| ≥ 35 | 25.88 | 26.89 | 27.25 | 27.24 | 27.66 | 28.25 | 28.94 | 29.21 | 20.64 |
| Employment status of mother | |||||||||
| Employed | 49.31 | 58.22 | 64.52 | 68.60 | 73.36 | 77.31 | 79.05 | 83.69 | 40.40 |
| Unemployed | 3.25 | 2.74 | 1.81 | 2.51 | 2.71 | 2.78 | 2.65 | 1.99 | 3.75 |
| Not in the labour force | 47.44 | 39.05 | 33.67 | 28.89 | 23.93 | 19.91 | 18.30 | 14.32 | 55.86 |
| Education of mother | |||||||||
| < 12 years of education | 31.62 | 30.34 | 29.64 | 29.63 | 29.07 | 27.83 | 26.71 | 26.03 | 40.45 |
| 12 years of education | 25.66 | 25.41 | 25.16 | 24.72 | 24.54 | 24.43 | 23.91 | 23.88 | 28.46 |
| Graduate or diploma | 35.71 | 36.83 | 37.73 | 38.18 | 38.73 | 39.82 | 40.99 | 41.38 | 26.76 |
| University Masters | 7.00 | 7.42 | 7.47 | 7.47 | 7.67 | 7.91 | 8.39 | 8.70 | 4.32 |
This variable, maternal stress or anxiety during pregnancy, was measured only once, in Wave 1; in the subsequent waves of the retained samples, the recollected percentages of ‘yes’ were close to 15%.
3.2. Hazard rate of any medical condition or disability
For all participants, as shown in Table 2, the hazard rate of having at least one medical condition or disability between ages 0 and 15 (2004–2018) was 26.11 per 1000 person-years. Table 2 also shows the hazard rate against different maternal health conditions considering cumulative incidents across all waves. This rate was the highest among the children of mothers with a medical condition (62.90 incidents per 1000 person-years), much higher than those of mothers without medical conditions (22.40 incidents per 1000 person-years). Similar trends were observed among the children of mothers experiencing mental illness (54.99 incidents per 1000 person-years), fair or poor health (45.46 incidents per 1000 person-years), obesity (31.43 incidents per 1000 person-years) and stressful life events (26.13 incidents per 1000 person-years), compared to the children of healthier mothers.
Table 2.
Hazard rate of any medical condition or disabilitya per 1000 person-years according to maternal health conditions for Australian children followed from age 0 to 15 (2004–2018).
| Characteristics |
All children |
Female |
Male |
|---|---|---|---|
| Hazard rate (95% CIb) |
Hazard rate (95% CI) |
Hazard rate (95% CI) |
|
| All participants | 26.11 (24.74–27.57) | 22.93 (21.13–24.88) | 29.29 (27.25–31.48) |
| MATERNAL HEALTH 2004–2018 | |||
| Obesity | |||
| Underweight | 24.76 (20.22–30.3) | 20.17 (14.41–28.22) | 28.42 (22.07–36.6) |
| Healthy weight | 21.18 (19.21–23.34) | 19.47 (16.87–22.47) | 22.89 (20.05–26.13) |
| Overweight | 25.07 (22.34–28.14) | 22.73 (19.19–26.92) | 27.53 (23.52–32.22) |
| Obese | 31.43 (27.98–35.3) | 27.29 (22.87–32.57) | 35.54 (30.45–41.48) |
| General health status | |||
| Excellent | 18.88 (16.24–21.94) | 18.30 (14.72–22.75) | 19.44 (15.79–23.93) |
| Very good | 22.38 (20.42–24.52) | 18.99 (16.50–21.86) | 25.75 (22.83–29.05) |
| Good | 29.66 (26.78–32.85) | 26.72 (22.94–31.13) | 32.56 (28.38–37.34) |
| Fair or poor | 45.46 (38.8–53.27) | 41.27 (32.71–52.08) | 49.85 (40.15–61.89) |
| Had a medical condition | |||
| No | 22.4 (21.04–23.84) | 19.82 (18.04–21.77) | 24.97 (22.97–27.14) |
| Yes | 62.90 (56.25–70.33) | 55.26 (46.63–65.5) | 70.27 (60.60–81.50) |
| Faced stressful life events | |||
| No | 22.6 (20.05–25.49) | 18.59 (15.42–22.41) | 26.64 (22.78–31.15) |
| Yes | 26.13 (24.46–27.91) | 23.94 (21.71–26.40) | 28.28 (25.86–30.92) |
| Mental illness based on Kessler-6 scores | |||
| No mental illness | 24.37 (22.95–25.87) | 21.45 (19.59–23.47) | 27.27 (25.18–29.54) |
| Have mental illness |
54.99 (42.12–71.8) |
59.89 (41.35–86.74) |
50.53 (34.41–74.22) |
| Mental stress or anxiety during pregnancy in 2004 | |||
| No | 24.34 (22.92–25.85) | 21.29 (19.42–23.35) | 27.31 (25.20–29.60) |
| Yes | 36.68 (32.57–41.30) | 32.05 (26.84–38.28) | 41.56 (35.32–48.9) |
‘Any medical condition or disability’ meant long-term medical conditions or disabilities and other disabilities that limited everyday activities. Long-term medical conditions or disabilities meant sight problems, hearing problems, speech problems, blackouts, difficulty learning, limited use of arms or fingers, difficulty gripping, limited use of legs and feet, and other physical conditions or disfigurements that lasted or were expected to last six months or more. Disabilities that limited everyday activities meant difficulty breathing, chronic pain, nervous conditions, head injuries, other long-term conditions, or other treated conditions.
Confidence interval.
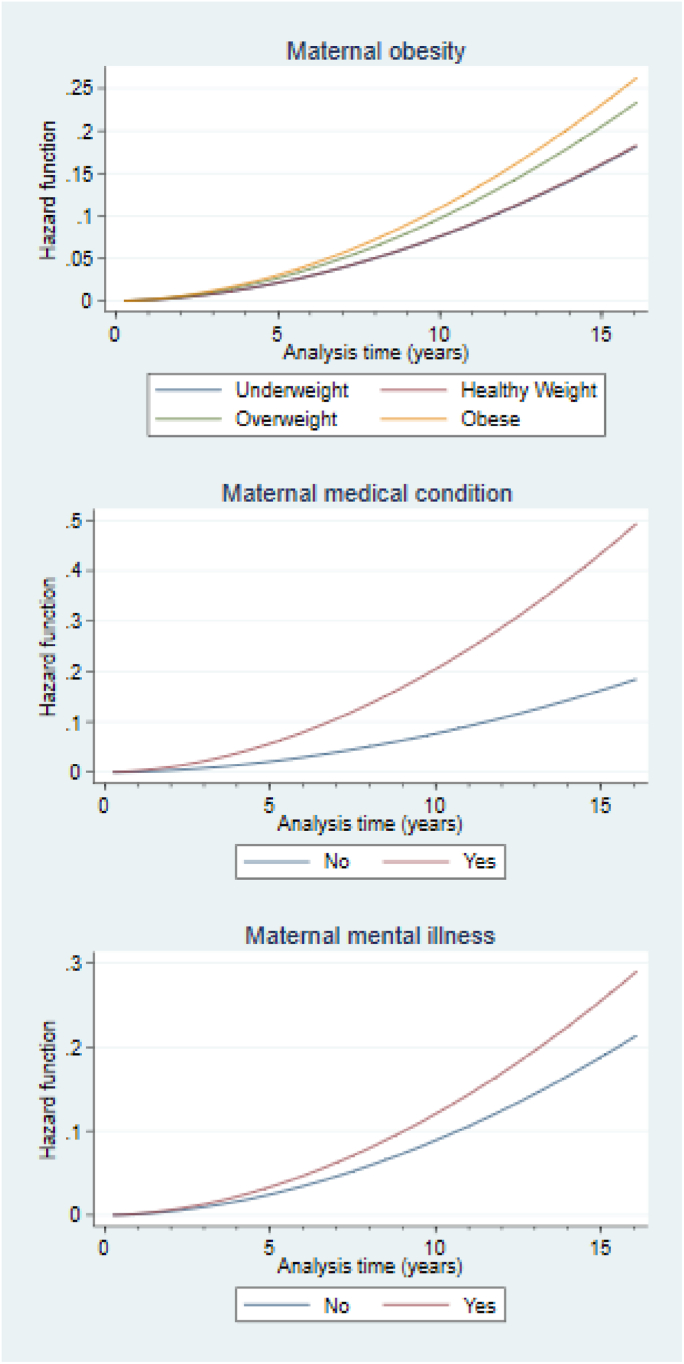
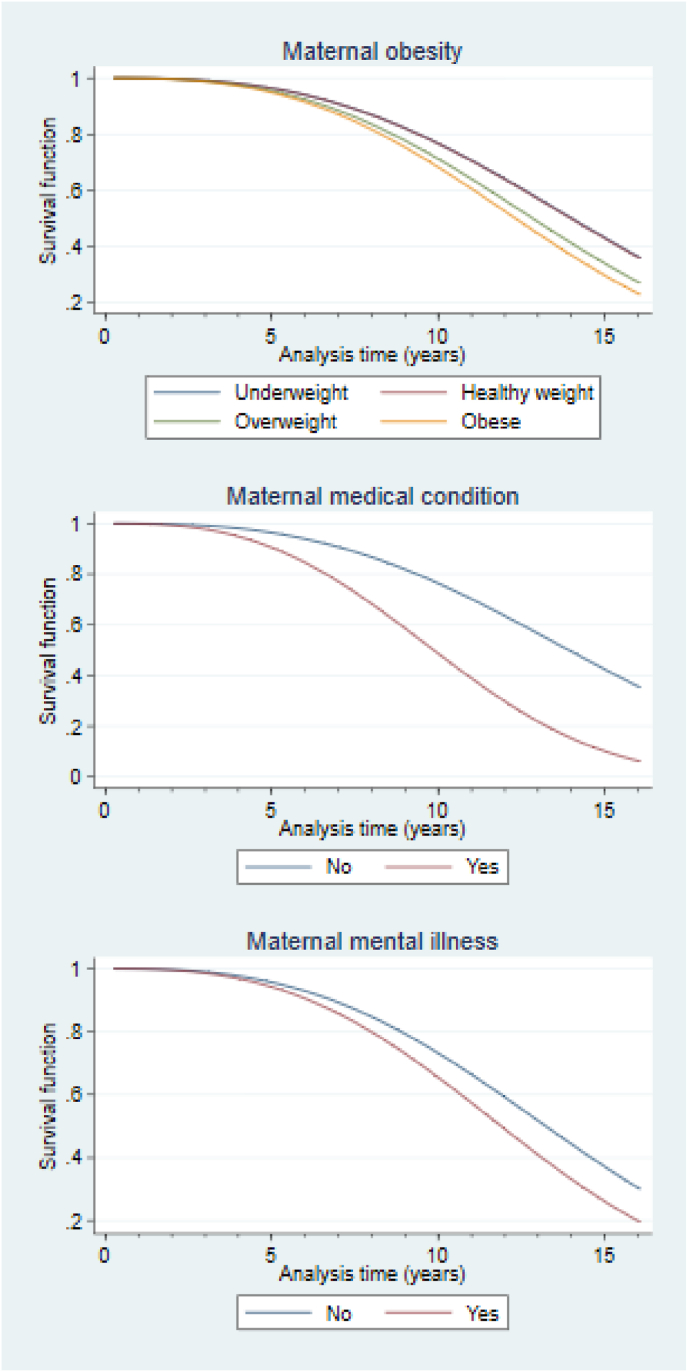
Fig. 1 displays the random-effects proportional Weibull hazard regression curves relating the hazard ratio of children's incurring any medical condition or disability over time to mothers' obesity, medical-condition and mental-illness characteristics. The graph clearly shows that the hazard ratios for all risk factors increased over time. The increase was greatest for the children of mothers who had medical conditions. Fig. 2 displays the corresponding survival function, showing diminishing trends in the children's survival of morbidity related to potential medical conditions or disabilities. Lower survival ratios were observed for the children of mothers who were overweight, had a medical condition or were experiencing mental illness compared to the respective reference categories. The downward trend is steepest for the children of mothers who were suffering from a medical condition.
Fig. 1.
Hazard function curves. Random-effects panel hazard regression curve over time (in years) on the hazard function relating children's having any medical condition or disability to their mother's health-related characteristics.
Fig. 2.
Survival function curves. Random-effects panel hazard regression curve over time (in years) on the survival function relating children's surviving a potential medical condition or disability to their mother's health-related characteristics.
3.3. Regression results
Table 3 presents the results of panel data parametric survival modeling of having any medical condition or disability. The parametric panel regression results, which were adjusted for control variables, suggested that children of mothers who had medical conditions during the follow-up period were more likely to have a medical condition or disability (HR: 2.61, 95% CI: 2.24–3.03) than the children of mothers who did not. Similar trends were observed among children of mothers who experienced obesity (HR: 1.40, 95% CI: 1.18–1.66), fair or poor health (HR: 1.48, 95% CI: 1.15–1.91) and stressful life events (HR: 1.23, 95% CI: 1.06–1.43) compared to the children of mothers who did not experience the respective problems.
Table 3.
Panel data parametric survival model for any medical condition/disability health hazard among Australian children, 2004–2018.
| Risk factors | Random-effects hazard regression modelsd |
||
|---|---|---|---|
| Model 1: All children |
Model 2: Female |
Model 3: Male |
|
| HRa (95% CIb), p-value | HR (95% CI), p-value | HR (95% CI), p-value | |
| MATERNAL HEALTH CHARACTERISTICS DURING THE FOLLOW-UP PERIOD | |||
| Obesity | |||
| Healthy weight (ref.)c | |||
| Underweight | 1.01 (0.79–1.29), 0.927 | 0.94 (0.63–1.4), 0.754 | 1.07 (0.78–1.47), 0.669 |
| Overweight | 1.19 (1.01–1.40), 0.032 | 1.24 (0.98–1.57), 0.077 | 1.16 (0.93–1.45), 0.19 |
| Obese | 1.40 (1.18–1.66), <0.001 | 1.25 (0.96–1.63), 0.099 | 1.54 (1.23–1.93), <0.001 |
| General health status | |||
| Excellent (ref.) | |||
| Very good | 1.11 (0.92–1.34), 0.271 | 0.97 (0.74–1.28), 0.828 | 1.24 (0.96–1.6), 0.104 |
| Good | 1.25 (1.02–1.52), 0.029 | 1.16 (0.87–1.55), 0.324 | 1.34 (1.02–1.77), 0.036 |
| Fair or poor | 1.48 (1.15–1.91), 0.002 | 1.28 (0.89–1.86), 0.186 | 1.68 (1.18–2.38), 0.004 |
| Had a medical condition | |||
| No (ref.) | |||
| Yes | 2.61 (2.24–3.03), <0.001 | 2.63 (2.09–3.3), <0.001 | 2.59 (2.13–3.17), 0 < 0.001 |
| Faced stressful life events | |||
| No (ref.) | |||
| Yes | 1.23 (1.06–1.43), 0.006 | 1.42 (1.12–1.79), 0.003 | 1.12 (0.92–1.36), 0.263 |
| Mental illness based on Kessler-6 scores | |||
| No (ref.) | |||
| Yes | 1.28 (0.93–1.77), 0.125 | 1.59 (1.03–2.43), 0.034 | 1.02 (0.62–1.65), 0.950 |
| Mental stress or anxiety during pregnancy | |||
| No (ref.) | |||
| Yes | 1.19 (1.03–1.39), 0.02 | 1.28 (1.03–1.6), 0.026 | 1.13 (0.92–1.39), 0.249 |
Hazard ratio.
Confidence interval.
Reference category.
All the three models were controlled for: child's age, whether English was spoken at home, whether the child has both parents, the indigenous status of the child, the age of the mother at childbirth, the employment statuses of the parents, the mother's level of education, and the remoteness of the family residence. Model 1 was controlled for sex of the child, along with these covariates.
Gender differences were observed in the hazard ratio of having any medical condition or disability while we conducted the modeling on the subpopulations by gender. Although girls whose mothers experienced mental stress or anxiety during pregnancy had a higher risk of having a medical condition or disability (HR: 1.19, 95% CI: 1.03–1.39) compared to the female children of mothers who did not, the same test of association was not significant among the sub-population of boys. Moreover, mothers' mental illness and stressful life events during the 15-year follow-up period had a statistically significant influence on girls’ medical conditions (HR: 1.59, 95% CI: 1.03–2.43 and HR: 1.42, 95% CI: 1.12–1.79 respectively) but not on those of boys. For further information, the unadjusted results of the parametric panel regression models are shown in Appendix C.
4. Discussion
This study measured the incidence rate of any medical condition or disability among children from LSAC, a nationally representative Australian birth cohort, then assessed to what extent the hazard rate of this incidence was associated with maternal health characteristics. The key point revealed by the study is that the children of mothers who had medical conditions during 15-year study period had a higher hazard ratio depicting the increased risk of incurring a medical condition or disability than those whose mothers did not. This reinforces the findings of earlier studies that provided evidence that mothers' having chronic medical conditions, such as hypoglycaemia or jaundice, increases their children's likelihood of acquiring a chronic condition up to adolescence (Gaillard et al., 2014; Ingstrup et al., 2012; O'Reilly & Reynolds, 2013; Watkins & Botto, 2001). The results also agree with those of other studies that have shown associations between maternal obesity and increased BMI of their offspring in adulthood (Eriksson et al., 2015; Hochner et al., 2012). However, the present study reveals that the hazard of having a medical condition or disability is greater among children of mothers with medical conditions than among those of mothers with other morbidities such as poor general health or mental stress. It also reveals that in the context of survival analysis, children's medical condition or disability significantly depends on their mothers' health status.
This study indicates that the hazard of facing a medical condition or disability is higher for children of mothers with overweight or obesity compared to those of mothers whose weight is healthy. The result agrees with those of other studies that have shown associations between maternal obesity and increased BMI from infancy to adulthood (Callaway et al., 2006, Eriksson et al., 2015; Hochner et al., 2012). Similarly, a review of UK clinical studies reports that maternal obesity has been associated with several long-term adverse health outcomes in the offspring. These include lifelong risk of obesity and metabolic dysregulation with increased insulin resistance, hypertension and dyslipidaemia, as well as behavioural problems (O'Reilly & Reynolds, 2013). Another study revealed that maternal pre-pregnancy obesity and excessive weight gain during pregnancy are common and important risk factors for adverse childhood adiposity, cardiovascular, and respiratory outcomes (McCormack et al., 1989). The present study contributes the further insight that in the context of time-to-event survival up to 15 years from birth, the likelihood of medical conditions or disabilities is higher among children of overweight and obese mothers than among those of mothers whose weight is healthy.
The present study observed that children whose mothers faced stressful life events had a greater risk of living with disabilities or medical conditions in childhood. Likewise, a study of the existing literature reported a significant association between maternal stressful life events and poor general health status (Ahmad, Kabir, Keramat, et al., 2021). The causes of this association are likely to be mothers' mental or behavioural difficulties resulting in reduced access to health care services for their children, which may worsen the children's health. Interestingly, our study revealed that mental stress or anxiety during pregnancy and maternal mental illness occurring longitudinally over time increase the risk of experiencing a medical condition or disability only for the mothers' female children. Further research is needed to explain this gender difference.
This study also suggests that the children of mothers with poor general health are more likely to develop a medical condition or disability than the children of mothers with excellent general health. Two studies in Australian and US settings corroborate this finding; however, the later study reveals the associations between mothers' poor general health and children's chronic illness and lower physical health index scores only during adolescence, not in infancy (Ahmad, Kabir, Keramat, et al., 2021; Waters et al., 2000). Using a different context to the present study, one conducted with children aged 5 to 18 confirmed that mothers' poor general health is associated with children's poor general health up to adolescence (Waters et al., 2000). One possible reason could be that these children's poor self-ratings of general health were generated from experiences of health complications, including disability.
The present study contributes to the current literature in several ways. It is the first study to investigate the association between maternal health characteristics and Australian children's medical conditions and disabilities from the perspective of survival analysis. Moreover, it considered 15 years of follow-up data from a large, nationally representative children's birth cohort, and by considering a wide range of diseases under the term ‘any medical condition or disability’, it encompassed the many diseases that frequently occur during childhood (World Health Organization, 2011) and also prevalent in adulthood (Keramat et al., 2022). Further, it included a wide range of maternal health characteristics while controlling for confounding variables related to maternal and child health problems.
The findings of this study and discovery of existing literature on foetal origins and environment impact (Ahmad, Kabir, Keramat, & Khanam, 2021a, Ahmad, Kabir, Ormsby, & Khanam, 2021c, Ahmad et al., 2021b; Behrman & Rosenzweig, 2004; Lin & Liu, 2009; Nakamuro et al., 2013) portrays the extended thought that intergenerational disease associations are usually a mix of genetics and environment. Hence, the policy implications need to address the risk of occurrences in such a way that both the environment and parental health conditions could be improved. If not, then interventions should be designed with the aim to support families (both mothers and children) with the limitation of the conditions to maximise their wellbeing. Further research is warranted to elaborate the interaction of intergenerational disease and environmental impact and design the appropriate interventions.
The study had several limitations. First, because of unbalanced longitudinal data, it was not possible to examine the causal relationships. Future studies could attempt to identify underlying causal associations. Second, both exposure (maternal medical condition) and outcome (offspring medical condition) were likely to be reported by the mother, which can lead to dependent errors. In such cases, non-differential misclassification may occur if the percentage of errors are equal in both exposure and dependent variables. Then, it may cause an underestimate of the hazard ratio. However, if data is more accurate in one of the comparison groups, then differential misclassification will occur. Depending on the circumstance, it may cause either an under-estimate or an over-estimate of the association. Further, self-reporting of general health and BMI of mothers may have resulted in a reporting bias, as they are based on subjective responses on a Likert scale (for general health) or self-measurements (for BMI). Third, the inequality of the sample size across the waves may have influenced the statistical power. Fourth, analysis of this study's intergenerational association is impacted with unknown extent of limitations on the gender differences. This is because, firstly, the study has engaged with analysing data only on the mothers (without including fathers), while genetic inheritance is from both parents. Secondly, family environments are shared by all living in the same household, but the analyses here (and in the existing literature) appear to be only of the association between mother and child.
5. Conclusion
Children of mothers who had medical conditions had a higher hazard of having a medical condition or disability than those of mothers who did not, considering the whole 15-year follow-up period. This hazard was also higher among children of obese mothers than among healthy-weight mothers. Children of mothers experiencing mental illness, fair or poor general health, or mental stress and anxiety during pregnancy had a higher hazard of having a medical condition or disability, compared to the children of mothers with better health conditions in the respective categories. Gender variations were observed; these need further research. Overall, the findings confirm that maternal health influences children's health from birth to 14 or 15 years of age in the perspective of time-to-event or survival analysis. This suggests that additional healthcare monitoring of mothers experiencing prenatal mental stress during pregnancy or living with obesity, fair or poor health, medical conditions or mental illness over the period of 15 years after childbirth would help enhance the health and wellbeing of children as well as mothers.
Authors’ contributions
KA was the principal investigator, designed the study, conducted the data analysis and drafted the manuscript. GO partially wrote the manuscript and assisted with the critical review and final editing of the manuscript. RK and EK contributed to the study design, the development and editing of the manuscript and supervised the study. The authors followed the STROBE guidelines for writing the manuscript. All authors read and approved the final manuscript.
Financial disclosure
This research did not receive any specific grants from funding agencies in the public, commercial, or not-for-profit sectors.
Ethics approval
The LSAC study was approved by the Australian Institute of Family Studies Ethics Committee. The de-identified unit record dataset was released to the current researchers at the University of Southern Queensland for the purposes of this research. To obtain this dataset, the authors completed and signed the Confidentiality Deed Poll and sent it to the National Centre for Longitudinal Data (NCLD) (ncldresearch@dss.gov.au) and the Australian Data Archive (ada@anu.edu.au). Therefore, datasets analysed or generated during the current study are subject to the signed confidentiality deed.
Consent for publication
Not applicable.
Author statement
Kabir Ahmad: Conceptualization, Methodology, Software, Data curation, Formal analysis, Writing- Original draft, Writing - Review & Editing.
Gail M Ormsby: Writing- Reviewing and Editing.
Enamul Kabir: Supervision, Methodology, Writing- Reviewing and Editing.
Rasheda Khanam: Supervision, Writing – review & editing.
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgements
This paper uses the data from Wave 1 to Wave 8 of the LSAC. The authors thank the Australian Institute of Family Studies for providing this data. The authors also thank Dr Barbara Harmes for proofreading the manuscript before submission.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.ssmph.2023.101385.
Appendix A
In LSAC, under any medical condition/disability, the following questions are available for Children:
| Question | Response |
|---|---|
| Does Study Child have any medical conditions or disabilities that have lasted or are likely to last for six months or more (e.g. sight problems not corrected by glasses or contact lenses, difficulty learning or understanding things, limited use of limbs, any condition that restricts physical activity or physical work (e.g. back problems, migraines) disfigurement or deformity, and any mental illness for which help or supervision is required)? | 1 No; 2 Yes |
These questions are available in all waves from Wave 1 to Wave 8. Further, for tracing the medical conditions/disability in specific, the following questions were asked subsequently.
| Questions | Responses |
|---|---|
| Which medical conditions or disabilities does the family member have? | |
| Has sight problems not corrected by glasses or contact lenses | 0 No; 1 Yes |
| Has Hearing problems | 0 No; 1 Yes |
| Has speech problems | 0 No; 1 Yes |
| Has blackouts, fits or loss of consciousness | 0 No; 1 Yes |
| Difficulty learning or understanding | 0 No; 1 Yes |
| Has Limited use of arms or fingers | 0 No; 1 Yes |
| Has difficulty gripping things | 0 No; 1 Yes |
| Has limited use of legs or feet | 0 No; 1 Yes |
| Has physical condition that restricts physical activity or physical work (eg back problems, migraines) | 0 No; 1 Yes |
| Has disfigurement or deformity | 0 No; 1 Yes |
| Has shortness of breath or breathing difficulties causing restriction | 0 No; 1 Yes |
| Has chronic or recurring pain or discomfort causing restriction | 0 No; 1 Yes |
| Has a nervous or emotional condition causing restriction | 0 No; 1 Yes |
| Has head injury and long term effects as a result of head injury, stroke or other brain damage causing restriction | 0 No; 1 Yes |
| Has other long-term conditions causing restriction | 0 No; 1 Yes |
| Has any other long term condition such as arthritis, asthma, heart disease, Alzheimer's disease, dementia etc. | 0 No; 1 Yes |
Appendix B
Table B1: Prevalence of having medical condition or disability by specific disability among the mothers in Wave 1.
| Category | Disability Description | Prevalence |
|---|---|---|
| Sensory | Has sight problems not corrected by glasses or contact lenses | 1.91% |
| Has hearing problems | 1.51% | |
| Has speech problems | 0.08% | |
| Physical | Limited use of arms or fingers | 0.36% |
| Difficulty gripping things | 0.18% | |
| Limited use of legs and feet | 0.26% | |
| Any condition that restricts physical work (For example, back problems, migraines) | 4.72% | |
| Physical disfigurement or deformity | 0.12% | |
| Has shortness of breath or breathing difficulties causing restriction | 0.92% | |
| Psychological | Has nervous or emotional condition causing restriction | 2.25% |
| Has mental illness for which help or supervision is required | 1.08% | |
| Has blackouts, fits or loss of consciousness | 0.60% | |
| Long-term effects as a result of a head injury, stroke or other brain damage | 0.12% | |
| Other long-term conditions | Has difficulty learning or understanding things | 0.60% |
| Has a long-term condition or ailment which is still restrictive even though it is being treated or medication being taken for it | 4.88% | |
| Has other long-term conditions such as arthritis, asthma, heart disease, Alzheimer's disease, dementia etc | 8.67% | |
| Has chronic or recurring pain or discomfort causing restriction | 1.85% | |
| Total* | 30.11% |
* This total accounts for multiple counts. The actual total prevalence of having any medical condition or disability is 24.43% among the wave 1 mothers, as shown in Table 1 of the manuscript.
Table B2: Longitudinal prevalence of having medical condition or disability by specific disability among the mothers across all waves
| Category | Disability Description | Pooled Prevalence |
|---|---|---|
| Sensory | Has sight problems not corrected by glasses or contact lenses | 1.32% |
| Has hearing problems | 1.46% | |
| Has speech problems | 0.44% | |
| Physical | Limited use of arms or fingers | 0.44% |
| Difficulty gripping things | 0.47% | |
| Limited use of legs and feet | 0.49% | |
| Any condition that restricts physical work (For example, back problems, migraines) | 3.95% | |
| Physical disfigurement or deformity | 0.16% | |
| Has shortness of breath or breathing difficulties causing restriction | 0.94% | |
| Psychological | Has nervous or emotional condition causing restriction | 1.54% |
| Has mental illness for which help or supervision is required | 0.91% | |
| Has blackouts, fits or loss of consciousness | 0.34% | |
| Long-term effects as a result of a head injury, stroke or other brain damage | 0.23% | |
| Other long-term conditions | Has difficulty learning or understanding things | 0.50% |
| Has a long-term condition or ailment which is still restrictive even though it is being treated or medication being taken for it | 2.70% | |
| Has other long-term conditions such as arthritis, asthma, heart disease, Alzheimer's disease, dementia etc | 3.75% | |
| Has chronic or recurring pain or discomfort causing restriction | 2.19% | |
| Total* | 21.83% |
* This total accounts for multiple counts. The average prevalence of having any medical condition or disability among the pooled observations is 13.64%.
Appendix C
Table C1: Panel data parametric survival model (unadjusted) for any medical condition/disability health hazard among Australian children, 2004–2018
| Random-effects hazard regression models | |||
|---|---|---|---|
| Risk factors | Model 1: All children | Model 2: Female | Model 3: Male |
| HRa (95% CIb), p-value | HR (95% CI), p-value | HR (95% CI), p-value | |
| MATERNAL HEALTH CHARACTERISTICS DURING THE FOLLOW-UP PERIOD | |||
| Obesity | |||
| Healthy weight (ref.)c | |||
| Underweight | 1.10 (0.88–1.38), 0.394 | 0.97 (0.67–1.40), 0.882 | 1.20 (0.90–1.60), 0.211 |
| Overweight | 1.18 (1.01–1.37), 0.036 | 1.15 (0.97–1.44), 0.210 | 1.19 (0.97–1.47), 0.096 |
| Obese | 1.43 (1.22–1.67), <0.001 | 1.31 (1.03–1.66), 0.027 | 1.53 (1.24–1.89), <0.001 |
| General health status | |||
| Excellent (ref.) | |||
| Very good | 1.14 (0.95–1.36), 0.156 | 1.02 (0.78–1.32), 0.906 | 1.25 (0.98–1.59), 0.072 |
| Good | 1.34 (1.11–1.61), 0.002 | 1.29 (0.98–1.69), 0.069 | 1.40 (1.08–1.80), 0.011 |
| Fair or poor | 1.52 (1.20–1.93), <0.001 | 1.37 (0.97–1.93), 0.077 | 1.68 (1.22–2.32), 0.002 |
| Had a medical condition | |||
| No (ref.) | |||
| Yes | 2.72 (2.37–3.12), <0.001 | 2.80 (2.27–3.45), <0.001 | 2.66 (2.21–3.20), 0 < 0.001 |
| Faced stressful life events | |||
| No (ref.) | |||
| Yes | 1.27 (1.11–1.46), 0.001 | 1.39 (1.12–1.72), 0.003 | 1.19 (0.99–1.43), 0.059 |
| Mental illness based on Kessler-6 scores | |||
| No (ref.) | |||
| Yes | 1.45 (1.09–1.92), 0.010 | 1.78 (1.20–2.65), 0.004 | 1.21 (0.80–1.81), 0.358 |
| Mental stress or anxiety during pregnancy | |||
| No (ref.) | |||
| Yes | 1.22 (1.06–1.40), 0.005 | 1.24 (1.01–1.52), 0.039 | 1.20 (0.99–1.45), 0.053 |
Appendix ASupplementary data
The following is the Supplementary data to this article:
Data availability
The data underlying the results presented in the study have some restrictions on its use and the data application’s approval is subject to a signed confidentiality deed. Those interested in accessing this data should contact the Australian Department of Social Services via https://dataverse.ada.edu.au/dataverse/lsac.
References
- Ahmad K., Kabir E., Keramat S.A., Khanam R. Maternal health and health-related behaviours and their associations with child health: Evidence from an Australian birth cohort. PLoS One. 2021;16(9) doi: 10.1371/journal.pone.0257188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ahmad K., Kabir E., Ormsby G.M., Khanam R. Are wheezing, asthma and eczema in children associated with mother’s health during pregnancy? Evidence from an Australian birth cohort. Archives of Public Health. 2021;79(1):19. doi: 10.1186/s13690-021-00718-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ahmad K., Kabir E., Ormsby G.M., Khanam R. Clustering of asthma and related comorbidities and their association with maternal health during pregnancy: Evidence from an Australian birth cohort. BMC Public Health. 2021;21(1):1952. doi: 10.1186/s12889-021-11997-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ahmad K., Keramat S.A., Sathi N.J., Kabir E., Khanam R. Association of infant and child health characteristics with the hazard of any medical condition or disability in Australian children. Archives of Public Health. 2022;80(1):158. doi: 10.1186/s13690-022-00913-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Anderson L.N., Sandhu R., Keown-Stoneman C.D.G., De Rubeis V., Borkhoff C.M., Carsley S., Maguire J.L., Birken C.S. Latent class analysis of obesity-related characteristics and associations with body mass index among young children. Obesity Science and Practice. 2020;6(4):390–400. doi: 10.1002/osp4.414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Australian Bureau of Statistics National survey of mental health and wellbeing: Summary of results. 2007. https://www.abs.gov.au/statistics/health/mental-health/national-survey-mental-health-and-wellbeing-summary-results/latest-release [9 Dec]. Available from.
- Australian Bureau of Statistics . Australian Bureau of Statistics; Canberra: 2019. Disability, ageing and carers, Australia: Summary of findings.https://www.abs.gov.au/statistics/health/disability/disability-ageing-and-carers-australia-summary-findings/2018 Oct 24. [Google Scholar]
- Behrman J.R., Rosenzweig M.R. Returns to birthweight. The Review of Economics and Statistics. 2004;86(2):586–601. [Google Scholar]
- Brown H.K., Speechley K.N., Macnab J., Natale R. Elevated risk of depression in high-risk pregnancy: A systematic review and meta-analysis. Journal of Obstetric, Gynecologic, and Neonatal Nursing. 2015;44(5):563–575. [Google Scholar]
- Callaway L., Prins J., Chang A., McIntyre H. The prevalence and impact of overweight and obesity in an Australian obstetric population. Medical Journal of Australia. 2006;184(2):4. doi: 10.5694/j.1326-5377.2006.tb00115.x. [DOI] [PubMed] [Google Scholar]
- Chen Y.C., Fan H.Y., Yang C., Lee Y.L. Early pubertal maturation and risk of childhood asthma: A mendelian randomization and longitudinal study. Allergy. 2020;75(4):892–900. doi: 10.1111/all.14009. [DOI] [PubMed] [Google Scholar]
- Contu L., Hawkes C.A. A review of the impact of maternal obesity on the cognitive function and mental health of the offspring. International Journal of Molecular Sciences. 2017;18(5) doi: 10.3390/ijms18051093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eriksson J.G., Sandboge S., Salonen M., Kajantie E., Osmond C. Maternal weight in pregnancy and offspring body composition in late adulthood: Findings from the helsinki birth cohort study (HBCS) Annals of Medicine. 2015;47(2):94–99. doi: 10.3109/07853890.2015.1004360. [DOI] [PubMed] [Google Scholar]
- Gaillard R., Felix J.F., Duijts L., Jaddoe V.W. Childhood consequences of maternal obesity and excessive weight gain during pregnancy. Acta Obstetricia et Gynecologica Scandinavica. 2014;93(11):1085–1089. doi: 10.1111/aogs.12506. [DOI] [PubMed] [Google Scholar]
- Geoge B., Seals S., Aban I. Survival analysis and regression models. Journal of Nuclear Cardiology. 2014;21(686):94. doi: 10.1007/s12350-014-9908-2. George et al 2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hochner H., Friedlander Y., Calderon-Margalit R., Meiner V., Sagy Y., Avgil-Tsadok M., Burger A., Savitsky B., Siscovick D.S., Manor O. Associations of maternal prepregnancy body mass index and gestational weight gain with adult offspring cardiometabolic risk factors: The Jerusalem Perinatal family follow-up study. Circulation. 2012;125(11):1381–1389. doi: 10.1161/CIRCULATIONAHA.111.070060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ingstrup K.G., Andersen C.S., Ajslev T.A., Pedersen P., Sorensen T.I., Nohr E.A. Maternal distress during pregnancy and offspring childhood overweight. Journal of Obesity. 2012;2012:7. doi: 10.1155/2012/462845. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keramat S.A., Ahammed B., Mohammed A., Seidu A.A., Farjana F., Hashmi R.…Ahinkorah B.O. Disability, physical activity, and health-related quality of life in Australian adults: An investigation using 19 waves of a longitudinal cohort. PLoS One. 2022;17(5) doi: 10.1371/journal.pone.0268304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim S.Y., Sappenfield W., Sharma A.J., Callaghan W.M., Dietz P.M. Gestational diabetes mellitus and risk of hypertensive disorders of pregnancy. American Journal of Obstetrics and Gynecology. 2017;217(3):282-e1. [Google Scholar]
- Linabery A.M., Nahhas R.W., Johnson W., Choh A.C., Towne B., Odegaard A.O., Czerwinski S.A., Demerath E.W. Stronger influence of maternal than paternal obesity on infant and early childhood body mass index: The fels longitudinal study. Pediatric Obesity. 2013;8(3):159–169. doi: 10.1111/j.2047-6310.2012.00100.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lin M.J., Liu J.T. Do lower birth weight babies have lower grades? Twin fixed effect and instrumental variable method evidence from Taiwan. Social Science & Medicine. 2009;68(10):1780–1787. doi: 10.1016/j.socscimed.2009.02.031. [DOI] [PubMed] [Google Scholar]
- Maïano C., Hue O., Morin A.J., Moullec G. Prevalence of overweight and obesity among children and adolescents with intellectual disabilities: A systematic review and meta-analysis. Obesity Reviews. 2016;17(7):599–611. doi: 10.1111/obr.12408. [DOI] [PubMed] [Google Scholar]
- McCormack C., Brooks-Gunn J., Shorter T., Holmes J.H., Heagarty M.C. Factors associated with maternal rating of infant health in central Harlem. Developmental and Behavioural Pediatrics. 1989;10(3):139–144. [PubMed] [Google Scholar]
- Naess M., Holmen T.L., Langaas M., Bjorngaard J.H., Kvaloy K. Intergenerational transmission of overweight and obesity from parents to their adolescent offspring—the HUNT study. PLoS One. 2016;11(11) doi: 10.1371/journal.pone.0166585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nakamuro M., Uzuki Y., Inui T. The effects of birth weight: Does fetal origin really matter for long-run outcomes? Economics Letters. 2013;121(1):53–58. [Google Scholar]
- National center on birth Defects and developmental disabilities, Centers for disease control and prevention: Disability and health overview. Centers for Disease Control and Prevention; Atlanta, GA: 2020. https://www.cdc.gov/ncbddd/disabilityandhealth/disability.html [Updated 2020 Sep 16; cited 2022 Jan 04] [Google Scholar]
- Nicholson W.K., Asao K., Brancati F.L., Coresh J., Pankow J.S., Powe N.R., Hsia J. Parity and risk of type 2 diabetes: The atherosclerosis risk in communities study. Diabetes Care. 2006;29(11):2349–2354. doi: 10.2337/dc06-0825. [DOI] [PubMed] [Google Scholar]
- Obel C., Linnet K.M., Henriksen T.B., Rodriguez A., Jarvelin M.R., Kotimaa A., Moilanen I., Ebeling H., Bilenberg N., Taanila A., et al. Smoking during pregnancy and hyperactivity-inattention in the offspring—comparing results from three Nordic cohorts. International Journal of Epidemiology. 2009;38(3):698–705. doi: 10.1093/ije/dym290. [DOI] [PubMed] [Google Scholar]
- O'Reilly J.R., Reynolds R.M. The risk of maternal obesity to the long-term health of the offspring. Clinical Endocrinology. 2013;78(1):9–16. doi: 10.1111/cen.12055. [DOI] [PubMed] [Google Scholar]
- Ou L., Chen J., Hillman K., Eastwood J. The comparison of health status and health services utilisation between Indigenous and non-Indigenous infants in Australia. Australian & New Zealand Journal of Public Health. 2010;34(1):50–56. doi: 10.1111/j.1753-6405.2010.00473.x. [DOI] [PubMed] [Google Scholar]
- Park M.H., Falconer C., Viner R.M., Kinra S. The impact of childhood obesity on morbidity and mortality in adulthood: A systematic review. Obesity Reviews. 2012;13(11):985–1000. doi: 10.1111/j.1467-789X.2012.01015.x. [DOI] [PubMed] [Google Scholar]
- Schendel D., Bhasin T.K. Birth weight and gestational age characteristics of children with autism, including a comparison with other developmental disabilities. Pediatrics. 2008;121(6):1155–1164. doi: 10.1542/peds.2007-1049. [DOI] [PubMed] [Google Scholar]
- Schieve L.A., Tian L.H., Rankin K., Kogan M.D., Yeargin-Allsopp M., Visser S., Rosenberg D. Population impact of preterm birth and low birth weight on developmental disabilities in US children. Annals of Epidemiology. 2016;26(4):267–274. doi: 10.1016/j.annepidem.2016.02.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- United Nations . United Nations; New York: 2015. Transforming our world: The 2030 agenda for sustainable development.https://sdgs.un.org/2030agenda [Google Scholar]
- Waters E., Doyle J., Wolfe R., Wright M., Wake M., Salmon L. Influence of parental gender and self-reported health and illness on parent-reported child health. Pediatrics. 2000;106(6):1422–1428. doi: 10.1542/peds.106.6.1422. [DOI] [PubMed] [Google Scholar]
- Watkins M.L., Botto L.D. Maternal prepregnancy weight and congenital heart defects in the offspring. Epidemiology. 2001;12(4):439–446. [PubMed] [Google Scholar]
- World Health Organization . World Health Organization; Geneva: 2008. The global burden of disease: 2004 update.https://apps.who.int/iris/handle/10665/43942 [Google Scholar]
- World Health Organization . World Health Organization; Geneva: 2011. World report on disability.https://www.who.int/publications/i/item/9789241564182 [Google Scholar]
- Zhong Y., Wang J., Nicholas S. Gender, childhood and adult socioeconomic inequalities in functional disability among Chinese older adults. International Journal for Equity in Health. 2017;16(1):1–11. doi: 10.1186/s12939-017-0662-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zubrick S., Williams A., Silburn S., Vimpani G. Department of Family and Community Services, Commonwealth of Australia; Canberra: 2000. Indicators of social and family functioning.https://www.dss.gov.au/our-responsibilities/families-and-children/publications-articles/indicators-of-social-and-family-functioning [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data underlying the results presented in the study have some restrictions on its use and the data application’s approval is subject to a signed confidentiality deed. Those interested in accessing this data should contact the Australian Department of Social Services via https://dataverse.ada.edu.au/dataverse/lsac.