Abstract
Introduction
Individuals with multimorbidity often receive high numbers of hospital outpatient services in concurrent trajectories. Nevertheless, little is known about factors associated with initiating new hospital outpatient trajectories; identified as the continued use of outpatient contacts for the same medical condition.
Purpose
To investigate whether the number of chronic conditions and sociodemographic characteristics in adults with multimorbidity is associated with entering a hospital outpatient trajectory in this population.
Methods
This population-based register study included all adults in Denmark with multimorbidity on January 1, 2018. The exposures were number of chronic conditions and sociodemographic characteristics, and the outcome was the rate of starting a new outpatient trajectory during 2018. Analyses were stratified by the number of existing outpatient trajectories. We used Poisson regression analysis, and results were expressed as incidence rates and incidence rate ratios with 95% confidence intervals. We followed the individuals during the entire year of 2018, accounting for person-time by hospitalization, emigration, and death.
Results
Incidence rates for new outpatient trajectories were highest for individuals with low household income and ≥3 existing trajectories and for individuals with ≥3 chronic conditions and in no already established outpatient trajectory. A high number of chronic conditions and male gender were found to be determinants for initiating a new outpatient trajectory, regardless of the number of existing trajectories. Low educational level was a determinant when combined with 1, 2, and ≥3 existing trajectories, and increasing age, western ethnicity, and unemployment when combined with 0, 1, and 2 existing trajectories.
Conclusion
A high number of chronic conditions, male gender, high age, low educational level and unemployment were determinants for initiation of an outpatient trajectory. The rate was modified by the existing number of outpatient trajectories. The results may help identify those with multimorbidity at greatest risk of having a new hospital outpatient trajectory initiated.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12889-023-15453-w.
Keywords: Denmark, Outpatient, Hospital, Multimorbidity, Healthcare utilization, Trajectory
Plain Language Summary
Many people with multiple chronic diseases (multimorbidity) need to see a doctor regularly. They must often go to several different hospital units for check-ups and medical examinations, and these consultations are rarely coordinated to provide integrated care. This means that these patients are often treated in parallel trajectories in several specialized outpatient clinics, and many receive fragmented care. This study investigates determinants for having a new ‘care trajectory’ initiated. It documents that men have a higher rate than women of initiating a new trajectory and that the rate increases with higher age, more chronic conditions, and low income. These results can be used to identify those at greatest risk of entering an additional trajectory, who may require special attention. Such information will enable clinicians to offer better, planned outpatient services and perhaps also more coherent care.
Introduction
An increasing number of people are living with multimorbidity (coexistence of two or more chronic conditions) [1]. This development is due to aging populations and improved treatment of chronic conditions [2–6]. Most individuals with multimorbidity are managed in general practice, but some require additional care in the form of outpatient specialized services delivered by hospitals [7–11]. However, research shows that it is difficult for patients and healthcare professionals to navigate healthcare plans and numerous appointments [12, 13]. Multiple chronic conditions can lead to concurrent use of outpatient clinics [7, 8], which may lead to high healthcare utilization, less integrated health care, low medical quality, and low patient satisfaction [9, 11, 14, 15]. Substantial utilisation of outpatient attendances can add to the healthcare workload and the impact on well-being experienced by individuals with multimorbidity, known as treatment burden. This can negatively affect quality-of-life and adherence to treatments [16, 17].
Multimorbidity is associated with socioeconomic deprivation [15, 18], which has been linked with lower probability of specialist visits [14, 19, 20]. While former studies have described disease patterns, demographics, and social disparities according to outpatient contacts and hospitalizations [14, 15, 19, 21, 22], no evidence exists on factors for entering hospital outpatient trajectories studied as the continued use of outpatient contacts. Multimorbidity trajectories have often been studied as change or accumulation in the number of distinguishable conditions [23] but can also be regarded as the patient’s way through the healthcare system considered as a series of events [24, 25]. The benefits of receiving interprofessional health care have been widely recognized, particularly in complex patient trajectories [1]. Identifying determinants for initiation of trajectories in specialized outpatient clinics may promote proactive targeting of services and facilitate collaboration between specialists.
This study aimed to investigate the number of chronic conditions and sociodemographic characteristics as determinants of initiating a hospital outpatient trajectory in adults with multimorbidity.
Materials and Methods
Setting
A population of 5.8 million people are residing in Denmark [26]. The healthcare system is mostly funded through taxation, and residents have free access to general practitioners and to public hospitals after referral. Nearly all Danish residents (99%) are registered with a general practitioner (GP). The GP is the patient’s first point of contact to the healthcare system and serves as gatekeeper to specialized care through a referral system. For each healthcare encounter, data is routinely collected and stored in national registers. All Danish residents are provided with a unique 10-digit civil registration number at birth or immigration. This number enables individual-level linkage between registers. Information about residence status, vital status, and migration with long-term follow-up can be obtained from the Danish Civil Registration System (CRS) through the civil registration number [27–29].
Design
This population-based cohort study was based on data from adult Danish residents identified with multimorbidity in Danish registers at the index date, January 1, 2018. Study participants were divided into four categories of existing hospital outpatient trajectories (0, 1, 2, or ≥3) at the index date, then followed prospectively from January 1, 2018, to December 31, 2019.
Study participants
The CRS was used to identify all legal residents aged 18 years or more residing in Denmark on January 1, 2018. We linked the civil registration number to diagnoses recorded in the Danish National Patient Register (NPR), the Danish Psychiatric Central Register (DPCR), or the Danish National Prescription Registry (DNPR). The NPR contains information on all inpatient and outpatient visits to somatic hospitals, including diagnoses [30]. The DPCR covers similar information for psychiatric hospitals [31]. Medical conditions recorded according to the International Classification of Diseases 10th version (ICD-10) were extracted from the NPR (inpatient visits from 1993 onwards and outpatient visits from 1995 onwards) and from the DPCR (from 1995 onwards) [30]. Additionally, from the DNPR, repeated codes for physician drug prescriptions redeemed at pharmacies and recorded in accordance with the Anatomical Therapeutic Chemical Classification System (ATC) [32] were obtained the one years prior to the index date. To ensure condition chronicity, medical conditions and drug prescriptions were limited to those occurring for the first time at least six months prior to the index date.
Multimorbidity was defined as two or more chronic conditions in an individual according to the definition by the World Health Organization (WHO) [1]. Medical conditions were identified based on the algorithm from the Danish Multimorbidity Index by Prior et al., which operates with 39 medical conditions and/or related redeemed drug prescriptions [33] (Appendix 1). The algorithm was developed for register-based research, based on established multimorbidity indices. It recognizes that medical conditions must be present simultaneously to emerge as multimorbidity and that some chronic conditions may be resolved.
Existing outpatient trajectories
All outpatient contacts were labelled with a disease category from the Danish Multimorbidity Index, which served as proxies of outpatient trajectories. This involved 31 medical conditions in nine outpatient trajectories (circulatory, endocrinal, pulmonary, gastrointestinal, urogenital, musculoskeletal, hematologic, neurologic system, and cancer) [33] (Appendix 1). An outpatient trajectory was defined as at least two hospital outpatient contacts for the same medical condition within 12 months. Thus, from the index date, we searched back in time for an outpatient appointment in 2017 and an additional encounter within 12 months for the same condition.
New outpatient trajectories and related contacts
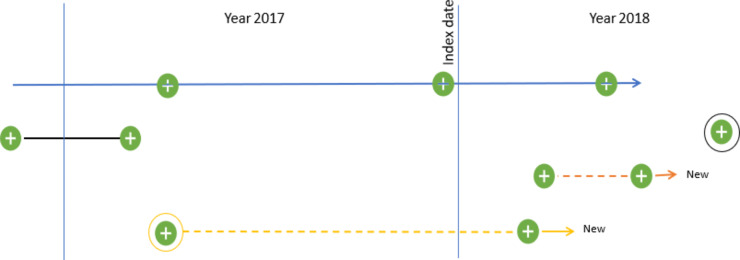
Being in a new hospital outpatient trajectory was prospectively determined from January 1, 2018, and 12 months onwards. We defined a new hospital outpatient trajectory as two or more outpatient contacts for the same medical condition within a 12-month interval. Thus, we identified the first outpatient contact occurring in 2018 and additional contacts within one year from the date of the first contact; this was done both forward and backwards in time (Fig. 1). After establishing new trajectories, we counted the outpatient contacts in 2018 that were related to these new trajectories.
Fig. 1.
Example of current and new trajectories
The colored lines represent trajectories, and the green dots represent contacts to outpatient clinics. In this example, the patient was in two trajectories in 2017 (black and blue solid lines). The orange and yellow solid lines represent new trajectories, as they both involve a second contact for the same chronic condition within a 12-month period. Contacts were estimated for only new trajectories
Exposure variables
The number of chronic conditions was counted for the 39 medical conditions listed in the Danish Multimorbidity Index, and these counts were grouped into 2, 3, 4, and ≥5 chronic conditions. From Statistics Denmark, we obtained information on gender, age, educational level, country of origin, civil status, population density, labor market attachment, and household income at the index date. Age was divided into <50, 50–59, 60–69, 70–79, and ≥80 years. Information on educational level was categorized in accordance with the International Standard Classification of Education (ISCED) 2011 into groups of <10 years, 10–15 years, and >15 years of education [34]. Ethnicity was categorized into western and non-western countries in accordance with the approach of Statistics Denmark [26]. Population density was based on registered place of residence and divided into <5,000, 5,000–99,999, and >100,000 inhabitants per town. Civil status was dichotomized into living with a partner or living alone. Labor market attachment was categorized into employed, unemployed (incl. retirement), or studying [26]. Household income was estimated for the year 2017 and divided into <20,000, 20,000–34,999, 35,000–49,999, and >50,000 EUR.
Directed acyclic graphs (DAGs) were used to illustrate associations and find relevant variables to adjust for. Information on disease severity was unavailable in the registers, instead we used the number of chronic conditions as a proxy. As educational level is often linked with household income and labor market attachment, educational level was selected as a common measure for socioeconomic status to adjust for. The number of contacts with general practice and health behavior were identified as intermediate factors and colliders and were not adjusted for.
Statistical analysis
We expected the initiation of new outpatient trajectories to vary by existing use of outpatient trajectories. Therefore, we stratified all analyses by the number of existing trajectories (0, 1, 2, and ≥3).
Descriptive statistics using counts with percentages and medians with interquartile intervals were applied to obtain baseline characteristics of the population. Person-time was calculated, starting from January 1, 2018, until death, emigration, or end of follow-up on December 31, 2018, whichever came first. Person-time for periods of hospitalization were subtracted from the length of observation time for each individual. Incidence rates (IR) and incidence rate ratios (IRR) with 95% confidence intervals (CI) for entering a new outpatient trajectory were estimated in unadjusted and adjusted Poisson regression models for each exposure. Adjusted IRRs for outpatient contacts for those entering a new trajectory were displayed in a forest plot to depict each exposure variable for each of the four existing trajectory categories (0, 1, 2, and ≥3) (Fig. 2) (Appendix 2). Model assumption of linearity was evaluated with a scatterplot for each exposure variable against log-odds of events to check that the rates were constant within covariate patterns. From assessing model assumptions, age showed a parable shaped association and was presented as a grouped exposure to account for the effect that new outpatient utilization may decrease when a person reaches a high age. All data analyses were performed in Stata statistical software, version 17.
Fig. 2.

Determinants for having contact in new outpatient trajectories among individuals with multimorbidity according to existing number of trajectories. IRR: incidence rate ratio
Results
Participants and descriptive data
We identified 1,321,003 Danish adults with multimorbidity. Tables 1 and 2 show the characteristics of the study population. Chronic conditions related to the circulatory system were most prevalent (77.3-92.6%). Within each disease category, the frequency of chronic conditions rose in concordance with the number of existing trajectories, except for mental health diseases. A little less than half (41.8%) of the individuals with no existing trajectories had two chronic conditions, whereas the majority (82.8%) of individuals in ≥3 trajectories had five or more chronic conditions (Table 1).
Table 1.
The disease distribution in adults living with multimorbidity in Denmark on 1 January 2018 according to number of existing trajectories
| Categories and diagnoses | Existing outpatient trajectories | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| All | 0 | 1 | 2 | ≥ 3 | ||||||
| N | % | N | % | N | % | N | % | N | % | |
| Total | 1,321,003 | 100 | 974,147 | 100 | 298,981 | 100 | 42,856 | 100 | 5,019 | 100 |
| Circulatory system | 1,020,746 | 77.3 | 752,481 | 77.3 | 227,796 | 76.2 | 35,819 | 83.6 | 4,650 | 92.6 |
| Hypertension | 796,033 | 60.3 | 588,181 | 60.4 | 175,843 | 58.8 | 28,218 | 65.8 | 3,791 | 75.5 |
| Dyslipidemia | 375,603 | 28.4 | 287,064 | 29.5 | 76,430 | 25.6 | 10,874 | 25.4 | 1,235 | 24.6 |
| Ischemic heart disease | 226,702 | 17.2 | 151,985 | 15.6 | 59,737 | 20.0 | 12,846 | 30.0 | 2,134 | 42.5 |
| Atrial fibrillation | 142,040 | 10.8 | 88,710 | 9.1 | 42,229 | 14.1 | 9,480 | 22.1 | 1,621 | 32.3 |
| Heart failure | 67,021 | 5.1 | 37,357 | 3.8 | 22,067 | 7.4 | 6,283 | 14.7 | 1,314 | 26.2 |
| Peripheral artery occlusive disease | 86,385 | 6.5 | 53,655 | 5.5 | 25,330 | 8.5 | 6,246 | 14.6 | 1,154 | 23.0 |
| Stroke | 131,702 | 10.0 | 95,654 | 9.8 | 29,691 | 9.9 | 5,563 | 13.0 | 794 | 15.8 |
| Endocrine system | 384,537 | 29.1 | 255,110 | 26.2 | 104,515 | 35.0 | 21,528 | 50.2 | 3,384 | 67.4 |
| Diabetes mellitus | 237,883 | 18.0 | 150,728 | 15.5 | 69,393 | 23.2 | 15,179 | 35.4 | 2,583 | 51.5 |
| Thyroid disorder | 128,949 | 9.8 | 88,812 | 9.1 | 33,052 | 11.1 | 6,202 | 14.5 | 883 | 17.6 |
| Gout | 56,543 | 4.3 | 36,721 | 3.8 | 15,017 | 5.0 | 3,967 | 9.3 | 838 | 16.7 |
| Pulmonic system and allergy | 293,791 | 22.2 | 214,565 | 22.0 | 65,482 | 21.9 | 11,865 | 27.7 | 1,879 | 37.4 |
| Chronic pulmonary disease | 203,839 | 15.4 | 143,827 | 14.8 | 48,634 | 16.3 | 9,738 | 22.7 | 1,640 | 32.7 |
| Allergy | 138,526 | 10.5 | 107,314 | 11.0 | 26,852 | 9.0 | 3,845 | 9.0 | 515 | 10.3 |
| Urogenital system | 136,041 | 10.3 | 85,131 | 8.7 | 39,226 | 13.1 | 9,693 | 22.6 | 1,991 | 39.7 |
| Chronic kidney disease | 36,242 | 2.7 | 15,447 | 1.6 | 13,807 | 4.6 | 5,520 | 12.9 | 1,468 | 29.2 |
| Prostate disorder | 105,840 | 8.0 | 71,774 | 7.4 | 27,925 | 9.3 | 5,297 | 12.4 | 844 | 16.8 |
| Gastrointestinal system | 225,673 | 17.1 | 152,344 | 15.6 | 60,569 | 20.3 | 11,066 | 25.8 | 1,694 | 33.8 |
| Ulcer/chronic gastritis | 77,161 | 5.8 | 55,003 | 5.6 | 17,968 | 6.0 | 3,607 | 8.4 | 583 | 11.6 |
| Chronic liver disease | 34,395 | 2.6 | 18,219 | 1.9 | 13,171 | 4.4 | 2,593 | 6.1 | 412 | 8.2 |
| Inflammatory bowel disease | 35,942 | 2.7 | 19,773 | 2.0 | 13,313 | 4.5 | 2,492 | 5.8 | 364 | 7.3 |
| Diverticular disease of intestine | 100,141 | 7.6 | 72,534 | 7.5 | 22,933 | 7.7 | 4,037 | 9.4 | 637 | 12.7 |
| Musculoskeletal | 483,638 | 36.6 | 341,403 | 35.1 | 118,503 | 39.6 | 20,779 | 48.5 | 2,953 | 58.8 |
| Connective tissue disorders | 81,671 | 6.2 | 43,096 | 4.4 | 30,648 | 10.3 | 6,822 | 15.9 | 1,105 | 22.0 |
| Osteoporosis | 137,673 | 10.4 | 88,895 | 9.1 | 39,910 | 13.3 | 7,765 | 18.1 | 1,103 | 22.0 |
| Painful condition | 356,233 | 27.0 | 260,987 | 26.8 | 79,730 | 26.7 | 13,510 | 31.5 | 2,006 | 40.0 |
| Hematological | 94,724 | 7.2 | 59,517 | 6.1 | 28,179 | 9.4 | 5,909 | 13.8 | 1,119 | 22.2 |
| HIV/AIDS | 4,848 | 3.7 | 335 | < 1 | 3,957 | 1.3 | 488 | 1.1 | 68 | 1.4 |
| Anemias | 90,002 | 6.8 | 59,186 | 6.1 | 24,313 | 8.1 | 5,447 | 12.7 | 1,056 | 21.0 |
| Neurological | 452,727 | 34.3 | 305,810 | 31.4 | 122,462 | 41.0 | 21,522 | 50.2 | 2,933 | 58.4 |
| Vision problems | 198,345 | 15.0 | 134,279 | 13.8 | 52,268 | 17.5 | 10,208 | 23.8 | 1,590 | 31.7 |
| Hearing problems | 201,363 | 15.2 | 133,289 | 13.7 | 56,540 | 18.9 | 10,176 | 23.7 | 1,358 | 27.1 |
| Migraine | 41,826 | 3.2 | 33,181 | 3.4 | 7,807 | 2.6 | 780 | 1.8 | 58 | 1.2 |
| Epilepsy | 37,803 | 2.9 | 24,452 | 2.5 | 11,173 | 3.7 | 1,917 | 4.5 | 261 | 5.2 |
| Parkinson’s disease | 8,698 | 6.6 | 4,005 | < 1 | 3,919 | 1.3 | 681 | 1.6 | 93 | 1.9 |
| Multiple sclerosis | 10,553 | 8.0 | 4,399 | < 1 | 5,441 | 1.8 | 658 | 1.5 | 55 | 1.1 |
| Neuropathies | 32,543 | 2.6 | 17,629 | 18.1 | 11,937 | 4.0 | 2,572 | 6.0 | 405 | 8.0 |
| Cancers | 114,704 | 8.7 | 41,508 | 4.2 | 58,443 | 19.5 | 12,931 | 30.2 | 1,822 | 36.3 |
| Mental health | 314,456 | 23.8 | 246,337 | 25.3 | 59,041 | 19.7 | 8,075 | 18.8 | 1,003 | 20.0 |
| Mood/stress-related/anxiety disorders | 50,722 | 3.8 | 39,093 | 4.0 | 10,150 | 3.4 | 1,319 | 3.1 | 160 | 31.9 |
| Psychological distress | 188,826 | 14.3 | 146,056 | 15.0 | 36,800 | 12.3 | 5,273 | 12.3 | 697 | 13.9 |
| Alcohol problems | 21,016 | 1.6 | 16,275 | 1.7 | 4,034 | 1.3 | 638 | 1.5 | 69 | 1.4 |
| Substance abuse | 4,986 | < 1 | 4,369 | < 1 | 551 | < 1 | 61 | < 1 | 5 | < 1 |
| Anorexia/bulimia | 1,546 | < 1 | 1,336 | < 1 | 184 | < 1 | 23 | < 1 | < 5 | - |
| Bipolar affective disorder | 19,823 | 1.5 | 16,359 | 1.7 | 3,081 | 1.0 | 359 | < 1 | 25 | < 1 |
| Schizophrenia/schizoaffective disorder | 21,156 | 1.6 | 17,927 | 1.8 | 2,906 | < 1 | 298 | < 1 | 25 | < 1 |
| Dementia | 35,512 | 26.9 | 29,483 | 3.0 | 5,332 | 1.8 | 626 | 1.5 | 71 | 1.4 |
| Number of chronic conditions | ||||||||||
| 2 | 492,276 | 37.3 | 406,913 | 41.8 | 80,853 | 27.0 | 4,402 | 10.3 | 108 | 2.2 |
| 3 | 320,977 | 24.3 | 244,727 | 25.1 | 69,550 | 23.3 | 6,438 | 15.0 | 262 | 5.2 |
| 4 | 207,144 | 15.7 | 145,487 | 14.9 | 53,776 | 18.0 | 7,389 | 17.2 | 492 | 9.8 |
| ≥ 5 | 300,606 | 22.8 | 177,020 | 18.2 | 94,802 | 31.7 | 24,627 | 57.5 | 4,157 | 82.8 |
Table 2.
Sociodemographic characteristics in adults living with multimorbidity in Denmark on 1 January 2018 according to number of existing trajectories
| Variables | Existing outpatient trajectories | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| All | 0 | 1 | 2 | ≥ 3 | ||||||
| N | % | N | % | N | % | N | % | N | % | |
| Total | 1321003 | 100 | 974147 | 100 | 298981 | 100 | 42856 | 100 | 5019 | 100 |
| Gender, female | 718801 | 54.4 | 541011 | 55.5 | 155189 | 51.9 | 20478 | 47.8 | 2123 | 42.3 |
| Age groups, years | ||||||||||
| < 50 | 187,442 | 14.2 | 142,302 | 14.6 | 41,246 | 13.8 | 3,687 | 8.6 | 207 | 4.1 |
| 50–59 | 222,277 | 16.8 | 168,137 | 17.3 | 47,932 | 16.0 | 5,641 | 13.2 | 567 | 11.3 |
| 60–69 | 321,670 | 24.4 | 237,383 | 24.4 | 72,201 | 24.2 | 10,818 | 25.2 | 1,268 | 25.3 |
| 70–79 | 367,817 | 27.8 | 260,321 | 26.7 | 90,123 | 30.1 | 15,271 | 35.6 | 2,102 | 41.9 |
| ≥ 80 | 221,786 | 16.8 | 165,996 | 17.0 | 47,477 | 15.9 | 7,438 | 17.4 | 875 | 17.4 |
| Educational level, years | ||||||||||
| < 10 | 462,469 | 35.0 | 344,542 | 35.4 | 100,981 | 33.8 | 15,115 | 35.3 | 1,831 | 36.5 |
| 10–15 | 763,988 | 57.8 | 560,392 | 57.5 | 175,954 | 58.9 | 24,784 | 57.8 | 2,858 | 56.9 |
| ≥ 16 | 66,329 | 5.0 | 47,762 | 4.9 | 16,254 | 5.4 | 2,104 | 4.9 | 209 | 4.2 |
| Missing | 28,217 | 2.1 | 21,451 | 2.2 | 5,792 | 1.9 | 853 | 2.0 | 121 | 2.4 |
| Civil status, living alone | 543945 | 41.2 | 407005 | 41.8 | 117988 | 39.5 | 16912 | 39.5 | 2040 | 40.7 |
| Ethnicity | ||||||||||
| Western | 1,255,886 | 95.1 | 926,724 | 95.1 | 283,707 | 94.9 | 40,672 | 94.9 | 4,787 | 95.3 |
| Non-western | 64,526 | 4.9 | 46,961 | 4.8 | 15,165 | 5.1 | 2,168 | 5.1 | 232 | 4.6 |
| Missing | 591 | 0.0 | 462 | 0.1 | 109 | 0.0 | 16 | 0.0 | - | - |
| Population density | ||||||||||
| < 5000 | 595,155 | 45.1 | 447,190 | 45.9 | 128,578 | 43.0 | 17,440 | 40.7 | 1,947 | 38.8 |
| 5000-99,999 | 488,814 | 37.0 | 362,857 | 37.3 | 108,990 | 36.5 | 15,215 | 35.5 | 1,752 | 34.9 |
| ≥ 100,000 | 237,019 | 17.9 | 164,088 | 16.8 | 61,413 | 20.5 | 10,201 | 23.8 | 1,320 | 26.3 |
| Missing | 15 | 0.0 | 12 | 0.0 | < 5 | - | < 5 | - | < 5 | - |
| Labor market attachment | ||||||||||
| Working | 396,557 | 30.0 | 301,233 | 30.9 | 85,640 | 28.6 | 9,007 | 21.0 | 677 | 13.5 |
| Not working | 901,440 | 68.2 | 655,492 | 67.3 | 208,301 | 69.7 | 33,344 | 77.8 | 4,306 | 85.8 |
| Studying | 22,872 | 1.7 | 17,304 | 1.8 | 5,027 | 1.7 | 505 | 1.2 | 36 | 0.7 |
| Missing | 134 | 0.0 | 118 | 0.0 | 13 | 0.0 | < 5 | - | < 5 | - |
| Household income, EUR | ||||||||||
| < 20,000 | 31,241 | 2.4 | 23,816 | 2.4 | 6,553 | 2.2 | 790 | 1.8 | 82 | 1.6 |
| 20,000–34,999 | 331,773 | 25.1 | 248,495 | 25.5 | 70,912 | 23.7 | 10,971 | 25.6 | 1,395 | 27.8 |
| 45,000–49,999 | 322,052 | 24.4 | 233,063 | 23.9 | 75,398 | 25.2 | 12,030 | 28.1 | 1,561 | 31.1 |
| ≥ 50,000 | 635,926 | 48.1 | 468,765 | 48.1 | 146,118 | 48.9 | 19,065 | 44.5 | 1,981 | 39.5 |
| Missing | 11 | 0.0 | 8 | 0.0 | < 5 | - | < 5 | - | < 5 | - |
More than half of the study population with no existing trajectory were women (55.5%), and 42.3% of the cohort in ≥3 existing trajectories were women. Below age 80 years, increasing age was associated with being in more existing trajectories (Table 2). Residents living in high-density areas accounted for 17.9% of the study population. This proportion increased in concordance with increasing number of existing trajectories (16.8-26.6%). The majority (68.2%) had no labor marked attachment; this percentage rose in concordance with increasing number of existing trajectories (67.3-85.8%) (Table 2).
The rate of initiating new trajectories
Table 3 shows the rate of newly initiated trajectories for one person-year. The highest incidence of entering a new trajectory was seen for individuals with ≥4 chronic conditions and no existing trajectories and for individuals with an annual household income <20,000 euros and ≥3 existing trajectories. The lowest rate of a new trajectory was seen in individuals with two chronic conditions and age <50 years. Overall seen, the lowest IRs (≤0.10) were seen in individuals with two chronic conditions across the stratified groups (Table 3).
Table 3.
Incidence rate per person-year and relative risk of new outpatient trajectories according to number of existing outpatient trajectories
| Existing outpatient trajectories | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 0 | 1 | 2 | ≥3 | |||||||||
| Risk of entering new trajectories | ||||||||||||
| Crude | Adj.* | Crude | Adj.* | Crude | Adj.* | Crude | Adj.* | |||||
| IR | IRR (95%CI) | IRR (95%CI) | IR | IRR (95%CI) | IRR (95%CI) | IR | IRR (95%CI) | IRR (95%CI) | IR | IRR (95%CI) | IRR (95%CI) | |
| Gender | ||||||||||||
|
Female Male |
0.13 0.16 |
1 (ref) 1.2 (1.21–1.23) |
1 (ref) 1.2 (1.21–1.23) |
0.13 0.15 |
1 (ref) 1.2 (1.17–1.21) |
1 (ref) 1.2 (1.17–1.21) |
0.14 0.16 |
1 (ref) 1.2 (1.15–1.27) |
1 (ref) 1.2 (1.15–1.27) |
0.16 0.19 |
1 (ref) 1.2 (1.01–1.34) |
1 (ref) 1.2 (1.01–1.34) |
| Age groups, years | ||||||||||||
|
<50 50–59 60–69 70–79 ≥80 |
0.09 0.11 0.14 0.18 0.16 |
1 (ref) 1.2 (1.18–1.23) 1.6 (1.56–1.63) 2.1 (2.01–2.09) 1.9 (1.85–1.93) |
1 (ref) 1.2 (1.16–1.22) 1.6 (1.54–1.60) 2.0 (1.98–2.06) 1.9 (1.86–1.94) |
0.06 0.10 0.14 0.18 0.17 |
1 (ref) 1.6 (1.53–1.69) 2.3 (2.15–2.35) 2.9 (2.73–2.97) 2.7 (2.57–2.81) |
1 (ref) 1.6 (1.52–1.67) 2.2 (2.13–2.33) 2.8 (2.71–2.95) 2.7 (2.57–2.81) |
0.07 0.11 0.15 0.18 0.17 |
1 (ref) 1.6 (1.35–1.81) 2.1 (1.84–2.40) 2.5 (2.22–2.87) 2.5 (2.14–2.80) |
1 (ref) 1.5 (1.33–1.79) 2.1 (1.80–2.35) 2.5 (1.63–2.81) 2.4 (2.10–2.76) |
0.14 0.12 0.18 0.19 0.17 |
1 (ref) 0.8 (0.53-1.29) 1.3 (0.87-1.92) 1.4 (0.93-2.01) 1.2 (0.81-1.84) |
1 (ref) 0.8 (0.54-1.33) 1.3 (0.88-1.97) 1.4 (0.94-2.06) 1.3 (0.82-1.89) |
| Number of chronic conditions | ||||||||||||
|
2 3 ≥4 |
0.10 0.13 0.20 |
1 (ref) 1.4 (1.35–1.39) 2.0 (2.01–2.06) |
1 (ref) 1.3 (1.27–1.31) 1.9 (1.82–1.87) |
0.07 0.11 0.19 |
1 (ref) 1.5 (1.46–1.57) 2.8 (2.68–2.84) |
1 (ref) 1.4 (1.34–1.44) 2.3 (2.27–2.41) |
0.06 0.09 0.18 |
1 (ref) 1.4 (1.21–1.63) 2.9 (2.59–3.32) |
1 (ref) 1.3 (1.13–1.52) 2.5 (2.20–2.84) |
0.05 0.09 0.18 |
1 (ref) 2.0 (0.74-5.13) 3.8 (1.57–9.12) |
1 (ref) 1.8 (0.70-4.83) 3.3 (1.37-8.00) |
| Educational level, years | ||||||||||||
|
<10 10–15 >15 |
0.14 0.14 0.14 |
1 (ref) 9.7 (0.96-0.98) 0.95 (0.93-0.98) |
1 (ref) 1.0 (1.03–1.06) 1.1 (1.04–1.10) |
0.15 0.13 0.11 |
1 (ref) 0.9 (0.89-0.93) 0.8 (0.71-0.79) |
1 (ref) 1.0 (0.97-1.02) 0.9 (0.86-0.95) |
0.17 0.14 0.13 |
1 (ref) 0.9 (0.81-0.90) 0.8 (0.66-0.85) |
1 (ref) 0.9 (0.85-0.95) 0.8 (0.73-0.94) |
0.19 0.18 0.07 |
1 (ref) 0.9 (0.79-1.05) 0.4 (0.22-0.65) |
1 (ref) 0.9 (0.79-1.06) 0.4 (0.23-0.66) |
| Civil living status | ||||||||||||
|
With partner Living alone |
0.14 0.14 |
1 (ref) 0.97 (0.96-0.98) |
1 (ref) 0.9 (0.93-0.95) |
0.14 0.14 |
(ref) 1.0 (1.01–1.05) |
1 (ref) 1.0 (0.99-1.03) |
0.15 0.15 |
1 (ref) 1.0 (0.92-1.02) |
1 (ref) 1.0 (0.91-1.01) |
0.18 0.17 |
(ref) 0.9 (0.80-1.06) |
1 (ref) 0.9 (0.81-1.08) |
| Ethnicity | ||||||||||||
|
Western Non-western |
0.14 0.12 |
1 (ref) 0.8 (0.81-0.85) |
1 (ref) 0.8 (0.81-0.85) |
0.14 0.11 |
1 (ref) 0.8 (0.78-0.86) |
1 (ref) 0.8 (0.78-0.86) |
0.15 0.13 |
1 (ref) 0.8 (0.73-0.94) |
1 (ref) 0.8 (0.73-0.94) |
0.17 0.17 |
(ref) 1.0 (0.69-1.34) |
(ref) 1.0 (0.69-1.34) |
| Population density | ||||||||||||
|
<5000 5000-99,999 ≥100,000 |
0.14 0.14 0.15 |
1 (ref) 1.0 (1.02–1.05) 1.1 (1.06–1.09) |
1 (ref) 1.0 (1.03–1.06) 1.1 (1.09–1.12) |
0.14 0.14 0.14 |
1 (ref) 1.0 (1.02–1.07) 1.0 (1.00-1.04) |
1 (ref) 1.0 (1.01–1.06) 1.1 (1.06–1.12) |
0.15 0.15 0.15 |
1 (ref) 1.0 (0.93-1.05) 1.0 (0.94-1.05) |
1 (ref) 1.0 (0.95-1.06) 1.0 (0.96 − 1.10) |
0.18 0.17 0.17 |
1 (ref) 1.0 (0.82 − 1.3) 0.9 (0.78-1.11) |
1 (ref) 1.0 (0.84-1.17) 1.0 (0.83-1.19) |
| Labor market attachment | ||||||||||||
|
Working Not working Studying |
0.11 0.16 0.09 |
1 (ref) 1.5 (1.43–1.47) 0.8 (0.78–0.87) |
1 (ref) 1.1 (1.07–1.11) 0.9 (0.87-0.97) |
0.09 0.16 0.08 |
1 (ref) 1.7 (1.70–1.78) 0.9 (0.84-1.03) |
1 (ref) 1.2 (1.15–1.22) 1.1 (0.98-1.21) |
0.10 0.17 0.09 |
1 (ref) 1.6 (1.47–1.70) 0.9 (0.68-1.22) |
1 (ref) 1.2 (1.07–1.25) 0.9 (0.68-1.31) |
0.14 0.18 0.09 |
1 (ref) 1.3 (1.06–1.65) 0.6 (0.20-1.96) |
(ref) 1.1 (0.88–1.40) 0.7 (0.22-2.19) |
| Household income, EUR | ||||||||||||
|
<20,000 20,000–34,999 35,000–49,999 ≥50,000 |
0.11 0.15 0.16 0.13 |
1 (ref) 1.3 (1.27–1.38) 1.5 (1.38–1.49) 1.2 (1.13–1.22) |
1 (ref) 1.0 (0.95-1.04) 1.1 (1.03–1.12) 1.1 (1.01–1.10) |
0.11 0.15 0.16 0.12 |
1 (ref) 1.4 (1.27–1.48) 1.5 (1.34–1.55) 1.1 (1.00-1.16) |
1 (ref) 0.9 (0.87-1.02) 1.0 (0.91-1.07) 0.9 (0.86 − 1.00) |
0.12 0.16 0.17 0.13 |
(ref) 1.3 (1.05–1.59) 1.4 (1.14–1.73) 1.1 (0.88-1.34) |
1 (ref) 1.1 (0.85-1.34) 1.1 (0.91-1.43) 1.1 (0.84-1.32) |
0.22 0.17 0.18 0.17 |
1 (ref) 0.8 (0.47–1.33) 0.9 (0.51–1.43) 0.8 (0.45–1.28) |
1 (ref) 0.7 (0.38–1.14) 0.7 (0.39–1.18) 0.7 (0.41–1.19) |
IR: Incidence rates. IRR: Incidence rate ratios. All figures are rounded. *Gender and ethnicity were not adjusted for covariates. Age was adjusted for gender and ethnicity. Number of chronic conditions was adjusted for age, gender, educational level, and ethnicity. Educational level was adjusted for age, gender, number of chronic conditions, and ethnicity. Civil status was adjusted for age. Population density was adjusted for age, educational level, and ethnicity. Labor market attachment was adjusted for age, gender, number of chronic conditions, educational level, and ethnicity. Household income was adjusted for age, gender, number of chronic conditions, educational level, and ethnicity
Adjusted relative incidence rates (IRR) showed that male gender and increasing number of chronic conditions were determinants for entering a new trajectory across all groups with existing trajectories. In addition, the IRR of having high numbers of existing trajectories increased in concordance with the number of chronic conditions. For example, those with ≥4 chronic conditions and ≥3 existing trajectories had a 3.3 (95%CI: 1.37-8.00) times higher rate of entering a new trajectory compared to 1.9 (95%CI: 1.82–1.87) times higher in those with ≥4 chronic conditions and no existing trajectory.
A high educational level was a determinant for those with no existing trajectories. Conversely, a lower rate was seen in those with 1, 2, or ≥3 existing trajectories and a high educational level.
Individuals with ≥3 existing trajectories and a high educational level had a 0.40 (95%CI: 0.23–0.66) times higher rate of a new trajectory compared to peers with a low educational level.
For those in 0, 1, or 2 existing outpatient trajectories, rising age, western ethnicity, and no labor market attachment increased the rate of entering a new trajectory. Notably, age showed a parabolic-shaped association, which broke at age ≥80 years. A population density ≥5,000 residents per town increased the rate of a new trajectory among people in no and 1 existing outpatient trajectory. Living with a partner and having high household income increased the rate of a new trajectory in those with no existing trajectories (Table 3).
The rate of contacts in new trajectories
Figure 2 displays the rate of outpatient contacts related to initiation of new trajectories. Age and number of chronic conditions showed the highest increased risks of new contacts across the stratified groups. Age group showed parabolic associations; higher IRRs were seen for those with 0, 1, or 2 existing trajectories and (slightly lower) for those with ≥3 existing trajectories when we compared the high age group to the reference group below age 50 years.
DISCUSSION
Key results
The rates for initiating a new trajectory were highest among individuals with three or more chronic conditions and no existing outpatient trajectories, and among individuals with an annual household income below 20,000 EUR and three or more existing trajectories. A growing number of chronic conditions and male gender increased the rate of having outpatient trajectories initiated. Associations with other variables were modified by the number of existing trajectories for an individual. A low educational level was a determinant at one or more existing trajectories. For those with less than three existing trajectories, high age, western ethnicity, and no work force attachment was associated with higher rates of having a new trajectory initiated. Likewise, increasing age and increasing number of chronic conditions increased the rate of outpatient contact in new trajectories.
Existing research
Variations in healthcare utilization and associations with the characteristics of individuals with multimorbidity has previously been studied, but little is known about the use of specialized outpatient care in the hospital setting [7, 8, 14, 15, 19, 20, 35], and especially on the determinants for having outpatient trajectories initiated.
Notably, our results showed that men initiated new trajectories at a higher rate than women. In Denmark, GPs are gatekeepers to specialist outpatient care [28]. Female gender is associated with multimorbidity and the care provision in general practice is known to differ by gender as women contact GPs more frequently, although, attendance for a yearly chronic care consultation is the same across gender [11, 36]. Therefore, men are unlikely to be referred to specialist care more often than women. Unless, their disease progression is more advanced, when seeking medical care. Moreover, regular attendance and focus on disease management in general practice (by women) may prevent initiation of specialist care [37, 38]. Applying at least two contacts within a year’s distance as definition for being in an outpatient trajectory resulted in finding those with continual healthcare utilization. In Denmark, women below 65 years of age account for higher use of outpatient clinics more than men, while men from the age of 65 to 80 years constitute a higher provision than women [26].
We found the rate of new trajectories to increase by age, although in a parabolically shaped association as it was less profound for individuals aged ≥80 years. It is well known that ageing is associated with frailty and functional impairment [39, 40] and acceleration of primary healthcare use [36], while the utilization of specialist care decreases [9]. This could be due to several factors. First, many hospital visits may seem unwarranted at a high age. Second, the healthy elderly population may receive fewer new trajectories and contacts. Third, initiation of new outpatient services might be prioritized less for the elderly, or their needs for specialist care might be met in the context of geriatric care.
Adding chronic conditions increased the rate of new trajectories. This is consistent with previous studies, which have shown an association between degree of multimorbidity and specialized healthcare utilization [9, 14, 15]. Chronic conditions tend to cluster together, and disease patterns differ in complexity and healthcare utilization [41]; this will influence the initiation of outpatient care. However, wide and unwarranted variations in healthcare provision have been reported in the Wennberg Atlas Project, where variations could not be explained by type or severity of illness or by patient preferences [42]. Despite reports of care fragmentation for specialist outpatients [43], rare attempts have been made to align trajectories and foster collaboration across specialties to reduce the number of outpatient trajectories [3, 35]. Also, it remains unknown how an individual with multimorbidity is best included in several trajectories of specialist healthcare.
Our results showed higher rates of entering a new trajectory for those with low education or unemployment. Previous studies have established an inverse socioeconomic gradient in healthcare utilization [15, 19, 20] and a recent review concluded that the most disadvantaged individuals often have lower probability of visiting specialists [20]. Unemployment may not be the only cause of socioeconomic inequality in our study; it may simply reflect that our study participants had reached pension age. However, this cannot explain why low education appeared to be a predisposing factor.
Strengths and limitations
A major strength of this study is the nationwide prospective design based on a comprehensive cohort of Danish adults with multimorbidity. An additional strength was the use of large and complete electronic registers, which reduced the risk of information bias and selection bias. Data from Danish national registers contain complete information on clinical services provided and are collected consecutively with the purpose of clinical surveillance and remuneration, and these data are known to have high validity and little loss of follow-up [28, 29]. Healthcare utilization is not affected by health insurance coverage as the Danish healthcare system offers universal access to healthcare and public hospitals. This makes the Danish health registers highly appropriate for research purposes.
A trajectory was restricted to a minimum of two outpatient visits for the same condition within 12 months to ensure consistency in the definition of being in a trajectory. In the analyses, we deducted hospitalization time and accounted for loss to follow-up by death or emigration from person-time followed, to avoid selection bias by attrition. Our analyses were stratified to account for already existing use of outpatient services as this was hypothesized to influence initiation of a new trajectory.
Some limitations should be addressed. This was an observational design, which cannot be used to determine causality. The results were confined to our definitions of both multimorbidity and trajectories with selected chronic conditions. This selection seems in line with the most frequently included chronic conditions in earlier studies and categorisation into disease system groups [44] Since outpatient visits were included for selected health conditions, our results are likely to have underestimated the true number of trajectories and contacts in outpatient clinics. Some could have been lost due to the lack of diagnosis (e.g., in general practice). However, our cohort was identified through hospital attendance during two decades and through medical prescriptions redeemed at pharmacies and recorded in the Danish Multimorbidity Index [33]. Thus, both diagnoses made in the hospital setting and diagnoses based on disease-specific prescriptions in general practice were included. Still, some diagnoses may not have been identified if no prescriptions were given for the medical condition because no register holds records of diagnoses made in general practice.
By looking back in time to establish the state of being in a trajectory, we minimized left-truncated selection bias, which could otherwise have overestimated the incidence and underestimated the prevalence of being in an existing trajectory. Moreover, we restricted to a minimum of two consecutive outpatient visits for the same condition to ensure consistency in the definition of being in a trajectory.
If individuals with short-term follow-up due to hospitalization were systematically different from those with long-term follow-up and had equally many new trajectories initiated after discharge, the resulting incidence density would depend on the combination of individuals and follow-up time. Even so, if we had not reduced person-time in the analyses, hospitalized individuals would have contributed with person-time without being at risk. Residual confounding by unmeasured factors or by the grouping of variables cannot be ruled out. Register-based research is limited to the data and level of detail recorded, and no data were available on condition severity, health behavior, lifestyle factors, or being in a trajectory. However, we conditioned our analysis on the number of chronic conditions as a proxy for health status. Since health behavior was assessed as an intermediate factor and collider in our DAGs, health behavior needed no conditioning in the analysis. As we deducted periods of hospitalization from person-time, some individuals were followed for a shorter time.
Clinical implications
Individuals with multimorbidity often encounter many different healthcare professionals across multiple provider settings [35, 45]. Knowledge about characteristics associated with initiation of new trajectories may reveal disparities in the provision of outpatient care and enable clinicians to identify individuals eligible for intensified utilization of healthcare services, who may require special attention. Such information will enable clinicians to offer better planned outpatient services and more coherent care. Better utilization will allow for more accurate allocation of resources and alignment of several different care trajectories. The reconfiguration of healthcare supporting the management of multimorbidity is urgently needed, due to increasing multimorbidity. Our results may guide reconfiguration by directing efforts towards those who often initiate new outpatient trajectories. As this study was population-based and studied the initiation of new outpatient trajectories among adults with multimorbidity, which can be observed in other health care systems, the findings are generalizable to other healthcare settings that resemble the Danish system i.e. publicly funded healthcare systems situated in Scandinavia and Northern Europe.
Conclusion
This novel research investigated determinants for initiating new outpatient trajectories for individuals with multimorbidity. One of the most noticeable results was that the rate of new trajectories was higher for men than for women. Moreover, we found that the rate of new trajectories increased with age, increasing number of chronic conditions, and low socioeconomic status (i.e., those with the highest needs for care). These rates were modified by the number of already existing outpatient trajectories. High age and high number of chronic conditions increased the rate of having outpatient contacts.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Acknowledgements
The authors wish to thank legal advisor Tommy K. Simonsen for preparing the legal agreements for this research project, data manager Marianne Pedersen for providing access to the register data and for providing advice on data management, and language editor Lone Niedziella for revising the manuscript.
Abbreviations
- ATC
Anatomical Therapeutic Chemical Classification System
- CI
Confidence interval
- CRS
Danish Civil Registration System
- DAGs
Directed acyclic graphs
- DNPR
the Danish National Prescription Registry
- DPCR
the Danish Psychiatric Central Register
- GP
General practitioner
- IQI
Interquartile interval
- IR
Incidence rate
- IRR
Incidence rate ratio
- NPR
Danish National Patient Register
- SES
Socioeconomic status
Authors’ contributions
CB contributed to the design of the study and drafted the manuscript. AP, CWA, AF, ARP, and PV contributed to the design and critically reviewed the manuscript. The authors read and approved the final manuscript.
Funding
This work was supported by the Novo Nordisk Foundation (Agreement Number: NNF18OC0052136 and NNF18OC0031194), Aarhus University, and the Toyota Foundation, Denmark. The authors have no affiliation with the funders, and the funders had no role in initiating or in carrying out this research.
Data Availability
The data that support the findings of this study were used under license from Statistical Denmark and are not publicly available. Similar data are available for researchers upon application to Statistics Denmark (www.dst.dk/en).
Declarations
Ethical approval and guidelines
This study was approved by the Danish Data Protection Agency (file no. 2016-051-000001). No further clearance was needed as this was an observational study (no human subjects involved) based on de-identified register data. The study was conducted in accordance with the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) guidelines [46].
Consent for publication
Not applicable.
Competing interests
None to declare.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.World Health Organization. Multimorbidity. Geneva. ; 2016. ISBN 978-92-4-151165-0.
- 2.Chua YP, Xie Y, Lee PSS et al. Definitions and Prevalence of Multimorbidity in Large Database Studies: A Scoping Review.Int J Environ Res Public Health. 2021;18(4). [DOI] [PMC free article] [PubMed]
- 3.Xu X, Mishra GD, Jones M. Evidence on multimorbidity from definition to intervention: an overview of systematic reviews. Ageing Res Rev. 2017;37:53–68. doi: 10.1016/j.arr.2017.05.003. [DOI] [PubMed] [Google Scholar]
- 4.Johnston MC, Crilly M, Black C, et al. Defining and measuring multimorbidity: a systematic review of systematic reviews. Eur J Public Health. 2019;29(1):182–9. doi: 10.1093/eurpub/cky098. [DOI] [PubMed] [Google Scholar]
- 5.World Health Organization. World Report on Ageing and Health. 2015.
- 6.MacRae C, Henderson D, Guthrie B, Mercer S. Multimorbidity and comorbidity patterns in the English National Health Service. Cell Rep Med. 2022;3(12):100863. doi: 10.1016/j.xcrm.2022.100863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bell C, Prior A, Frølich A, et al. Trajectories in Outpatient Care for People with Multimorbidity: a Population-Based Register Study in Denmark. Clin Epidemiol. 2022;14:749–62. doi: 10.2147/CLEP.S363654. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wolff DL, Von Plessen C, Waldorff FB, et al. Time trends in patients managed simultaneously in multiple hospital outpatient specialty clinics for chronic diseases: a register-based cross-sectional study. J Comorb. 2019;9:2235042X19831907. doi: 10.1177/2235042X19831907. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Muggah E, Graves E, Bennett C, et al. The impact of multiple chronic diseases on ambulatory care use; a population based study in Ontario, Canada. BMC Health Serv Res. 2012;12:452. doi: 10.1186/1472-6963-12-452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Schiøtz ML, Høst D, Christensen MB, et al. Quality of care for people with multimorbidity - a case series. BMC Health Serv Res. 2017;17(1):745. doi: 10.1186/s12913-017-2724-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Salisbury C, Johnson L, Purdy S, et al. Epidemiology and impact of multimorbidity in primary care: a retrospective cohort study. Br J Gen Pract. 2011;61(582):e12–21. doi: 10.3399/bjgp11X548929. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ørtenblad L, Meillier L, Jønsson AR. Multi-morbidity: a patient perspective on navigating the health care system and everyday life. Chronic Illn. 2018;14(4):271–82. doi: 10.1177/1742395317731607. [DOI] [PubMed] [Google Scholar]
- 13.Moffat K, Mercer SW. Challenges of managing people with multimorbidity in today’s healthcare systems. BMC Fam Pract. 2015;16:129. doi: 10.1186/s12875-015-0344-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Quinaz Romana G, Kislaya I, Cunha Goncalves S, et al. Healthcare use in patients with multimorbidity. Eur J Public Health. 2020;30(1):16–22. doi: 10.1093/eurpub/ckz118. [DOI] [PubMed] [Google Scholar]
- 15.Frølich A, Ghith N, Schiøtz M, et al. Multimorbidity, healthcare utilization and socioeconomic status: a register-based study in Denmark. PLoS ONE. 2019;14(8):e0214183. doi: 10.1371/journal.pone.0214183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Mair FS, May CR. Thinking about the burden of treatment. BMJ. 2014;349:g6680. doi: 10.1136/bmj.g6680. [DOI] [PubMed] [Google Scholar]
- 17.Rosbach M, Andersen JS. Patient-experienced burden of treatment in patients with multimorbidity - A systematic review of qualitative data. PLoS ONE. 2017;12(6):e0179916. doi: 10.1371/journal.pone.0179916. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Barnett K, Mercer SW, Norbury M, et al. Epidemiology of multimorbidity and implications for health care, research, and medical education: a cross-sectional study. Lancet. 2012;380(9836):37–43. doi: 10.1016/S0140-6736(12)60240-2. [DOI] [PubMed] [Google Scholar]
- 19.Mbuya-Bienge C, Simard M, Gaulin M, et al. Does socio-economic status influence the effect of multimorbidity on the frequent use of ambulatory care services in a universal healthcare system? A population-based cohort study. BMC Health Serv Res. 2021;21(1):202. doi: 10.1186/s12913-021-06194-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Lueckmann SL, Hoebel J, Roick J, et al. Socioeconomic inequalities in primary-care and specialist physician visits: a systematic review. Int J Equity Health. 2021;20(1):58. doi: 10.1186/s12939-020-01375-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Lund Jensen N, Pedersen HS, Vestergaard M, et al. The impact of socioeconomic status and multimorbidity on mortality: a population-based cohort study. Clin Epidemiol. 2017;9:279–89. doi: 10.2147/CLEP.S129415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Figueroa JF, Papanicolas I, Riley K et al. International comparison of health spending and utilization among people with complex multimorbidity.Health Serv Res. 2021. [DOI] [PMC free article] [PubMed]
- 23.Cezard G, McHale CT, Sullivan F, et al. Studying trajectories of multimorbidity: a systematic scoping review of longitudinal approaches and evidence. BMJ Open. 2021;11(11):e048485. doi: 10.1136/bmjopen-2020-048485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kuwornu JP, Lix LM, Quail JM, et al. Measuring care trajectories using health administrative databases: a population-based investigation of transitions from emergency to acute care. BMC Health Serv Res. 2016;16(1):565. doi: 10.1186/s12913-016-1775-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Pan Z, Xu W, Li Z et al. Trajectories of Outpatient Service Utilisation of Hypertensive Patients in Tertiary Hospitals in China.Int J Environ Res Public Health. 2020;17(3). [DOI] [PMC free article] [PubMed]
- 26.Statistics Denmark D. Available from: https://www.dst.dk/da/Statistik/dokumentation/. Accessed June 30, 2022.
- 27.Pedersen CB. The danish Civil Registration System. Scand J Public Health. 2011;39(7 Suppl):22–5. doi: 10.1177/1403494810387965. [DOI] [PubMed] [Google Scholar]
- 28.Schmidt M, Schmidt SAJ, Adelborg K, et al. The danish health care system and epidemiological research: from health care contacts to database records. Clin Epidemiol. 2019;11:563–91. doi: 10.2147/CLEP.S179083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Thygesen LC, Ersbøll AK. When the entire population is the sample: strengths and limitations in register-based epidemiology. Eur J Epidemiol. 2014;29(8):551–8. doi: 10.1007/s10654-013-9873-0. [DOI] [PubMed] [Google Scholar]
- 30.Lynge E, Sandegaard JL, Rebolj M. The danish National Patient Register. Scand J Public Health. 2011;39(7 Suppl):30–3. doi: 10.1177/1403494811401482. [DOI] [PubMed] [Google Scholar]
- 31.Mors O, Perto GP, Mortensen PB. The danish Psychiatric Central Research Register. Scand J Public Health. 2011;39(7 Suppl):54–7. doi: 10.1177/1403494810395825. [DOI] [PubMed] [Google Scholar]
- 32.Johannesdottir SA, Horváth-Puhó E, Ehrenstein V, et al. Existing data sources for clinical epidemiology: the danish National Database of reimbursed prescriptions. Clin Epidemiol. 2012;4:303–13. doi: 10.2147/CLEP.S37587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Prior A, Fenger-Grøn M, Larsen KK, et al. The Association between Perceived stress and mortality among people with multimorbidity: a prospective Population-Based Cohort Study. Am J Epidemiol. 2016;184(3):199–210. doi: 10.1093/aje/kwv324. [DOI] [PubMed] [Google Scholar]
- 34.UNESCO. International Standard Classification of Education 11th revision. Available from: http://uis.unesco.org/en/topic/international-standard-classification-education-isced. Accessed June 30, 2022.
- 35.Bell C, Frølich A, Appel CW, et al. Improving health care for patients with multimorbidity: a mixed-methods study to explore the feasibility and process of aligning scheduled outpatient appointments through collaboration between medical specialties. Int J Integr Care. 2022;22(1):17. doi: 10.5334/ijic.6013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Prior A, Vestergaard CH, Ribe AR, et al. Chronic care services and variation between danish general practices: a nationwide cohort study. Br J Gen Pract. 2022;72(717):e285–92. doi: 10.3399/BJGP.2021.0419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Wagner EH, Grothaus LC, Sandhu N, et al. Chronic care clinics for diabetes in primary care: a system-wide randomized trial. Diabetes Care. 2001;24(4):695–700. doi: 10.2337/diacare.24.4.695. [DOI] [PubMed] [Google Scholar]
- 38.Olthof M, Groenhof F, Berger MY. Continuity of care and referral rate: challenges for the future of health care. Fam Pract. 2019;36(2):162–5. doi: 10.1093/fampra/cmy048. [DOI] [PubMed] [Google Scholar]
- 39.Li C, Zhou R, Yao N, et al. Health Care utilization and unmet needs in chinese older adults with multimorbidity and functional impairment. J Am Med Dir Assoc. 2020;21(6):806–10. doi: 10.1016/j.jamda.2020.02.010. [DOI] [PubMed] [Google Scholar]
- 40.Vetrano DL, Palmer K, Marengoni A, et al. Frailty and Multimorbidity: a systematic review and Meta-analysis. J Gerontol A Biol Sci Med Sci. 2019;74(5):659–66. doi: 10.1093/gerona/gly110. [DOI] [PubMed] [Google Scholar]
- 41.Juul-Larsen HG, Christensen LD, Bandholm T, et al. Patterns of Multimorbidity and differences in Healthcare utilization and complexity among acutely hospitalized medical patients (≥ 65 Years) - a latent class Approach. Clin Epidemiol. 2020;12:245–59. doi: 10.2147/CLEP.S226586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Wennberg JE. Unwarranted variations in healthcare delivery: implications for academic medical centres. BMJ. 2002;325(7370):961–4. doi: 10.1136/bmj.325.7370.961. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Kailasam M, Guo W, Hsann YM, et al. Prevalence of care fragmentation among outpatient attending specialist clinics in a regional hospital in Singapore: a cross-sectional study. BMJ Open. 2019;9(3):e022965. doi: 10.1136/bmjopen-2018-022965. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Ho IS, Azcoaga-Lorenzo A, Akbari A, et al. Examining variation in the measurement of multimorbidity in research: a systematic review of 566 studies. Lancet Public Health. 2021;6(8):e587–e97. doi: 10.1016/S2468-2667(21)00107-9. [DOI] [PubMed] [Google Scholar]
- 45.Pefoyo AJ, Bronskill SE, Gruneir A, et al. The increasing burden and complexity of multimorbidity. BMC Public Health. 2015;15:415–015. doi: 10.1186/s12889-015-1733-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Strengthening the Reporting of Observational Studies in. Epidemiology (STROBE) guidelines. Available from: https://www.strobe-statement.org/. Accessed June 30, 2022.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data that support the findings of this study were used under license from Statistical Denmark and are not publicly available. Similar data are available for researchers upon application to Statistics Denmark (www.dst.dk/en).