Abstract
Supporting the global eradication of wildpoliovrisu (WPV), this project aimed to provide polio and measles vaccines to a population frequenty missed by immunization services and campaigns, ethnic Somali children living among mobile populations within Kenya’s Northeastern Region. Additionally, nutritional support, albendazole (for treatment of intestinal parasites) and vitamin A were provided to improve children’s health and in accordance with regional vaccination campaign practices. To better understand movement patterns and healthcare-seeking behaviors within this population, we trained community-based data collectors in qualitative and geospatial data collection methods. Data collectors conducted focus group and participatory mapping discussions with ethnic Somalis living in the region. Qualitative and geospatial data indicated movement patterns that followed partially definable routes and temporary settlement patterns with an influx of ethnic Somali migrants into Kenya at the start of the long rainy season (April–June). Community members also reported concerns about receiving healthcare services in regional health facilities. Using these data, an 8-week vaccination campaign was planned and implemented: 2196 children aged 0–59 months received polio vaccine (9% had not previously received polio vaccine), 2524 children aged 9–59 months received measles vaccine (27% had not previously received measles vaccine), 113 were referred for the treatment of severe acute malnourishment, 150 were referred to a supplementary feeding program due to moderate acute malnourishment, 1636 children aged 12–59 months were provided albendazole and 2008 children aged 6–59 months were provided with vitamin A. This project serves as an example for how community-based data collectors and local knowledge can help adapt public health programming to the local context and could aid disease eradication in at-risk populations.
Keywords: Vaccination, migrants, mobile populations, polio, qualitative research, mapping
Introduction
The Global Polio Eradication Initiative (GPEI) began in 1988 with a resolution by the World Health Assembly to eradicate polio. Today it is an inter-agency partnership led by national governments and six core partners: World Health Organization (WHO), Rotary International, US Centers for Disease Control and Prevention (CDC), United Nations Children’s Fund (UNICEF), Bill and Melinda Gates Foundation, and Gavi, The Vaccine Alliance (Greene et al. 2019; Jorba et al. 2016). In 1988, the three serotypes of wild poliovirus (WPV1, WPV2 and WPV3) paralyzed approximately 1000 children daily. Today, only two countries remain endemic for wild poliovirus type 1 (WPV1): Afghanistan and Pakistan. Nonetheless, polio eradication remains a global challenge due to outbreaks from circulating vaccine-derived poliovirus (cVDPV), emerging when live oral poliovirus vaccine (OPV) strains revert to neurovirulence after prolonged circulation in communities with very low vaccination coverage (Greene et al. 2019; Jorba et al. 2016; Hsu et al. 2016). From July 2019 to February 2020, there were 31 cVDPV2 outbreaks, 24 (77%) of which were on the African continent (Alleman et al. 2020).
In 2019, the WHO immunization monitoring website estimated vaccination coverage for children 1 year of age in Somalia was 42% for the first dose of inactivated polio virus vaccine (IPV1), 47% with three doses of OPV3 (Pol3), 46% with a single dose of measles vaccine, and 42% with three doses of diphtheria, tetanus and pertussis vaccine (DTP3). Such low vaccination coverage poses a critical risk of WPV1 and cVDPV transmission amongst Somali children and surrounding communities. The last WPV1 outbreak in Somalia occurred following WPV1 importation in 2013; this outbreak spread into Garissa County in Kenya’s Northeastern Region (our region of study illustrated in Figure 1) causing 14 WPV1 cases in Kenya (Haydarov et al. 2016). As of July 2020, GPEI reported continued circulation of cVDPV in Somalia with 13 positive sewage samples in 2020 and 16 confirmed cVDPV cases in children since 2018 (GPEI, 2020).
Figure 1.
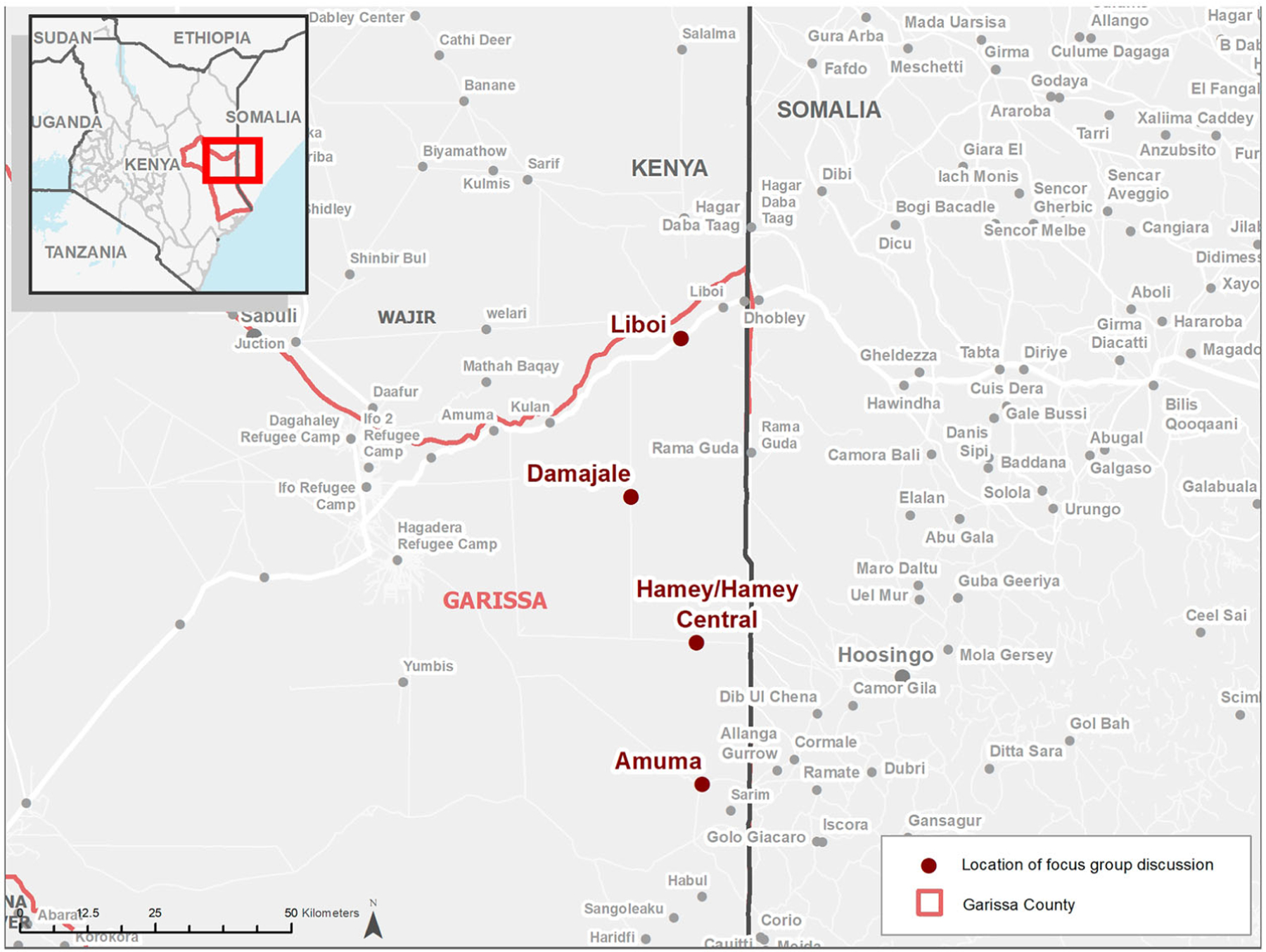
Region of study – Garissa County, Kenya.
An estimated 3 million ethnic Somalis live in Kenya, predominantly in the Northeastern Region, with lower vaccination coverage reported than any other minority population in the country. According to the Kenya’s 2014 Demographic and Health Survey, ethnic Somali children aged 12–23 months in Kenya had OPV vaccine coverage of 78.4%, 13.4% lower than among other Kenyans of the same age group (91.8% coverage). In addition, out of the 4052 children aged 12–23 months surveyed in 2014, 47.6% of those reporting zero vaccinations were ethnic Somali, but only represented 7.8% of the total (Masters et al. 2019). Furthermore, approximately 5% lower coverage was reported in recent measles vaccination campaigns among pastoralist communities in Kenya (a subgroup including Somali migrants) compared to other Kenyans, due mostly to their mobility (Weitzberg 2015).
Somali refugees also move within the area in increasing numbers due to displacement by political and environmental instabilities. The 2017 droughts followed by flooding in 2018 displaced an estimated 5.45 million Somalis throughout the region. In Kenya, as of February 2020, the United Nations High Commissioner for Refugees (UNHCR) website disclosed 217,917 registered Somali refugees seeking asylum and temporarily housed in the Dadaab Refugee Complexes at Dagahaley, Ifo, Ifo 2 and Hagadera camps.
While some Somali refugees and migrants enter Kenya through official border crossings and utilize refugee camps, others use unofficial routes and settle in spaces outside the camps or near established ethnic Somali settlements. The movement and temporary settlement of under-vaccinated mobile Somali populations near and among under-vaccinated ethnic Somali communities in Kenya creates a critical situation where transmission of poliovirus among children is highly likely. Considering these risks, our project sought to conduct a polio vaccination campaign targeting ethnic Somali children living in mobile populations under the age of 5 years in Garissa County within Kenya’s Northeastern Region. Additionally, as high-risk population do not commonly access public health support, we also provided measles vaccinations, vitamin A (which improves measles vaccination response), albendazole (for treatment of intestinal parasites) and nutritional support. This paper outlines our experience planning and conducting the campaign and serves as an example for utilizing community-based data collectors and local knowledge to adapt public health programming to the local context.
Methods
We conducted a series of focus group discussions (FGDs) and participatory mapping exercises in order to better understand temporary settlement habits, migration patterns and health-seeking behaviors of ethnic Somalis living in or traveling through Kenya. We then used this data to plan a polio vaccination campaign targeting the population of interest.
We conducted this project in Garissa County in Kenya’s Northeastern Region. Garissa County is one of three Kenyan counties which border Somalia and has approximately 160 miles of possible entry points for migrant and refugee populations along its Eastern boundary (Figure 1) (Haydarov et al. 2016).
Data collectors and study sites
The International Organization of Migration (IOM) selected data collectors from the region for their language capabilities (able to speak English, Kiswahili and local Somali dialects) and familiarity with community and local leaders. Twenty facilitators and note-takers were trained in qualitative and geospatial data collection methods and split into four sub-regional collection teams. A team consisted of one meeting facilitator, two note-takers, one organizer for crowd control and task management, and one alternate in case of availability challenges. Each data collection team was assigned to one sub-region (Amuma, Damajale, Liboi and Hamey) in Garissa County, Kenya.
Focus group discussions and participatory mapping
In consideration of the distance between FGD locations and general inaccessibility in the region, data collectors were expected to be able to conduct 2 FGDs per day over the span of 5 days in November 2018. In total, we expected 40 focus groups, 10 in each of the sub-regions, with 10 participants per FGD. Data collection teams chose the focus group locations and participants through convenience and purposeful sampling with attention on local knowledge holders in ethnically Somali communities. FGDs included community members available at the time of data collection but also individuals identified from the following subgroups: community youth, women, religious leaders, market vendors, healthcare providers and settlement leaders. Facilitators divided focus groups by gender due to cultural sensitivity and to support open dialogue.
Attendance sheets showed 10 participants per FGD. No names were collected of FGD participants, only demographics of age, gender and community position. A consent form was read at the start of all FGDs and all participants verbally agreed to participate. While FGD participants volunteered to take part in the discussion, they were informed that they could leave the meeting at any time or choose to not answer any question without fear of retribution. FGD facilitators conducted all discussions in the local Somali dialect.
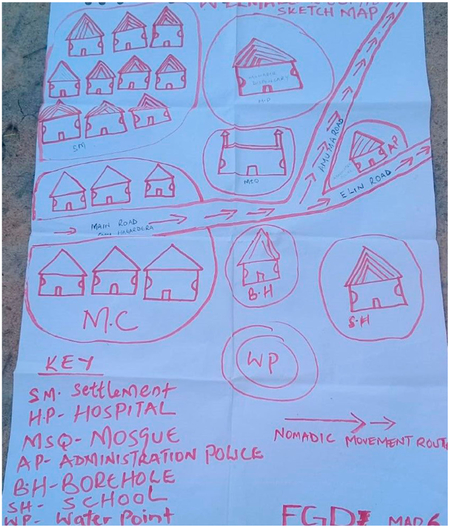
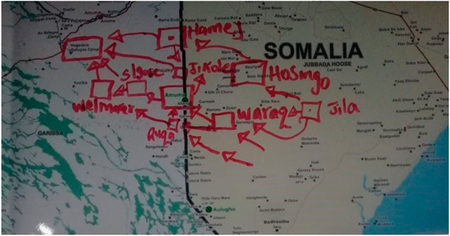
FGD facilitators posed four main questions with 18 probing questions, designed to assure participants spoke to the key aspects needed for planning a successful campaign. The four main questions focused on: (1) Somali migration and settlement patterns in the Northeastern Region, (2) movement patterns within Kenya and across the border with Somalia, (3) healthcare-seeking behaviors and (4) relationships with regional refugee camps (questions available in Appendix A). Six of the probing questions called for participants to annotate points of reference on maps. Facilitators used the maps throughout the discussion and asked participants to draw points of interest, a technique known as participatory mapping, to encourage more thorough conversations about migration and settlement patterns as well as to better understand local spatial knowledge of the region. Accommodating various group preferences and experiences with maps, facilitators had the option of using large printed maps of the region or participants were given the option to draw their own community-level maps (see Appendix B).
Vaccination and nutrition campaign
IOM and American Refugee Committee (ARC), a humanitarian and disaster relief organization, implemented an 8-week vaccination campaign (April–May 2019) based on data collected from the FGDs and mapping. The campaign targeted children under 5 years of age in Garissa County, Kenya. IOM oversaw the campaign logistics and ARC staffed the field vaccination teams. Because of ARC’s experience working in security compromised areas, IOM worked jointly with ARC in the vaccination activities through engagements with local authorities, ministry of health and other implementing actors.
The campaign provided the following services: bivalent OPV [bOPV] (against types 1 and 3) for children aged 0–59 months, measles vaccine for children aged 9–59 months, Albendazole (for treatment of intestinal parasites) for children aged 12–59 months and vitamin A for children aged 6–59 months. The campaign also provided malnutrition screening and referral for nutritional supplementation targeting children under 5 years of age. Even though the population of interest was ethnic Somali mobile populations, during the 8-week campaign the vaccination team included every child under the age of 5. Considering a regional population of 37,498, the campaign aimed to vaccinate approximately 6750 children, as the under 5 population was estimated at 18% of the total population.
Vaccination status was recorded according to parental or caregivers’ recall. No ethnic or citizenship demographics were collected due to sensitivities around national identities and limited time available to the vaccination teams. Vaccination sites were determined based on key points of interest suggested by FGD participants: migration routes, temporary settlement locations and areas potentially lacking healthcare services. IOM and ARC also allowed vaccinators to use snowball sampling, where existing study participants suggest additional study participants, and vaccinated in areas reported to have active nomad presence while in the field.
Data management
Following the FGDs, the data collection team consolidated notes, verified responses based on a mutual agreement of content, and translated responses into English in a predetermined dialogue table format. The table format included columns for question number, speaker number, dialogue and observation notes. Teams shared their deliverables within 1 week of collection. Deliverables from each FGD included a completed dialogue table and a JPEG image of the completed map since physical maps could not easily be collected (see Appendix B).
Qualitative data was transcribed into Microsoft Word© and then weekly data quality-checked using Microsoft Excel©, inspecting for duplication using conditional formatting to highlight exact duplicates. As part of our accountability framework, any exact duplicate responses were removed prior to analysis because exact replication is indicative of data falsification. Additionally, analysis did not intend to look at frequencies, meaning that the removal of duplicates also provided less dense data for qualitative analysis without distorting any research objectives. Analysts then entered the cleaned FGD transcripts into NVivo© and coded to key themes by question and subregion.
A Geographic Information Systems (GIS) specialist digitized the information drawn on the annotated paper map during FGDs into ArcGIS in an iterative process of referencing the annotated maps, the FGD notes, and publicly available spatial databases that contain precise coordinates of towns and health facilities. After digitizing, the specialist mapped the data to illustrate key locations and travel routes mentioned during FGDs. Key stakeholders reviewed initial maps to verify accuracy of locations and routes that were digitized. Field staff provided final maps to vaccination teams for use in the vaccination campaign.
Vaccination teams tracked the number of children receiving the interventions (i.e. number of polio doses given per vaccination site) on paper and then transferred daily totals into Microsoft Excel© tables. The tables were then submitted after each campaign week and reviewed for inconsistencies (i.e. vaccination totals exceeding the number of children seen during the week).
Results
After the accountability and data quality check, only the first 20 FGDs were used in qualitative analysis as the second half appeared duplicative. Due to time limitations and funding, we could not go back and increase the numbers or investigate the error.
Regional settlement structure
All FGD participants were Somali and belonged to the following clans: Ogaaden clan, its sub-clan Auliyahan and smaller sub-clans (Figure 2). Amuma respondents from all four focus group locations (Welmarer, Sadah Gose, Jikole and Durte) identified themselves within the Somali-Ogaaden clan. Respondents from Hamey (Homajo, Dagadey, Barkinta and Bula) focus groups and Damajale (Magudo, Damajale Abek, Abdisugow and central Damajale) focus groups identified as Ogaaden and its sub-clan Auliyaan. Liboi focus group participants were Auliyahan as well as ‘rare clans and sub-clans’ (Daresema, Mohame Zubeir, Bahgeri and Marehaan).
Figure 2.
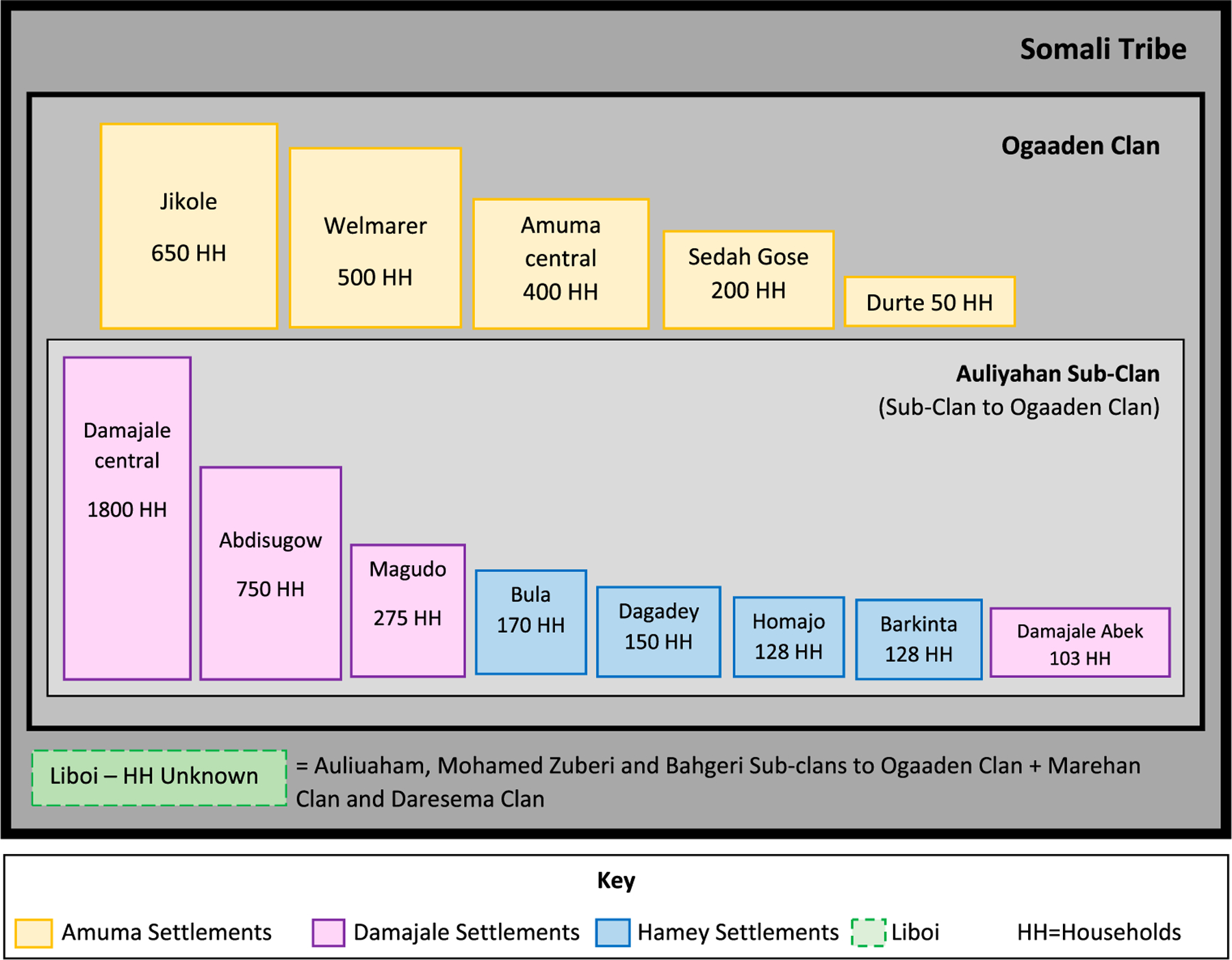
Reported clan affiliations and number of households by location.
To estimate the number of total households (HHs) by area, FGD participants were asked to report how many HHs were in their area; the median number was selected if a range was provided across several focus groups. According to the FGD participants, the approximate number of HHs was 1400 in Amuma, 9300 in Liboi, 576 in Hamey and 2984 in Damajale. HH size by FGD location and clan affiliation are presented in Figure 2. This data reflects the number of HHs at the time of the FGDs in November 2018. A majority of FGD participants asserted that the Somali migrant population does not come into the area until the long rainy season beginning in April (as opposed to the short rainy season in October–November). Therefore, the HH numbers were likely higher at the time of the vaccination campaign that occurred in April 2019 than estimated in the FGDs.
Somali mobile population migratory patterns
According to the FGD participants, Somali mobile populations crossed into the Amuma and Hamey subregions predominantly through unofficial border crossings and moved along roadways in a northwestern direction toward the Dadaab Refugee Complex. Participants from both areas also noted that the communities along the route were primary transit points (Welmarer, Sadahgose, Amuma, Ruqa, Hamey, Jikole), with Somalis predominantly coming from Waraq, Aden Santur, Dadelema, Hosingow, Dagdoma, Dobley and Kismayo. FGD participants in Jikole suggested many nomadic and pastoralist people moved within Kenya from Amuma and Hamey settlements and proceeded into other areas within Kenya such as Welmarer and the Hagadera Refugee Camp (Figure 3).
Figure 3.
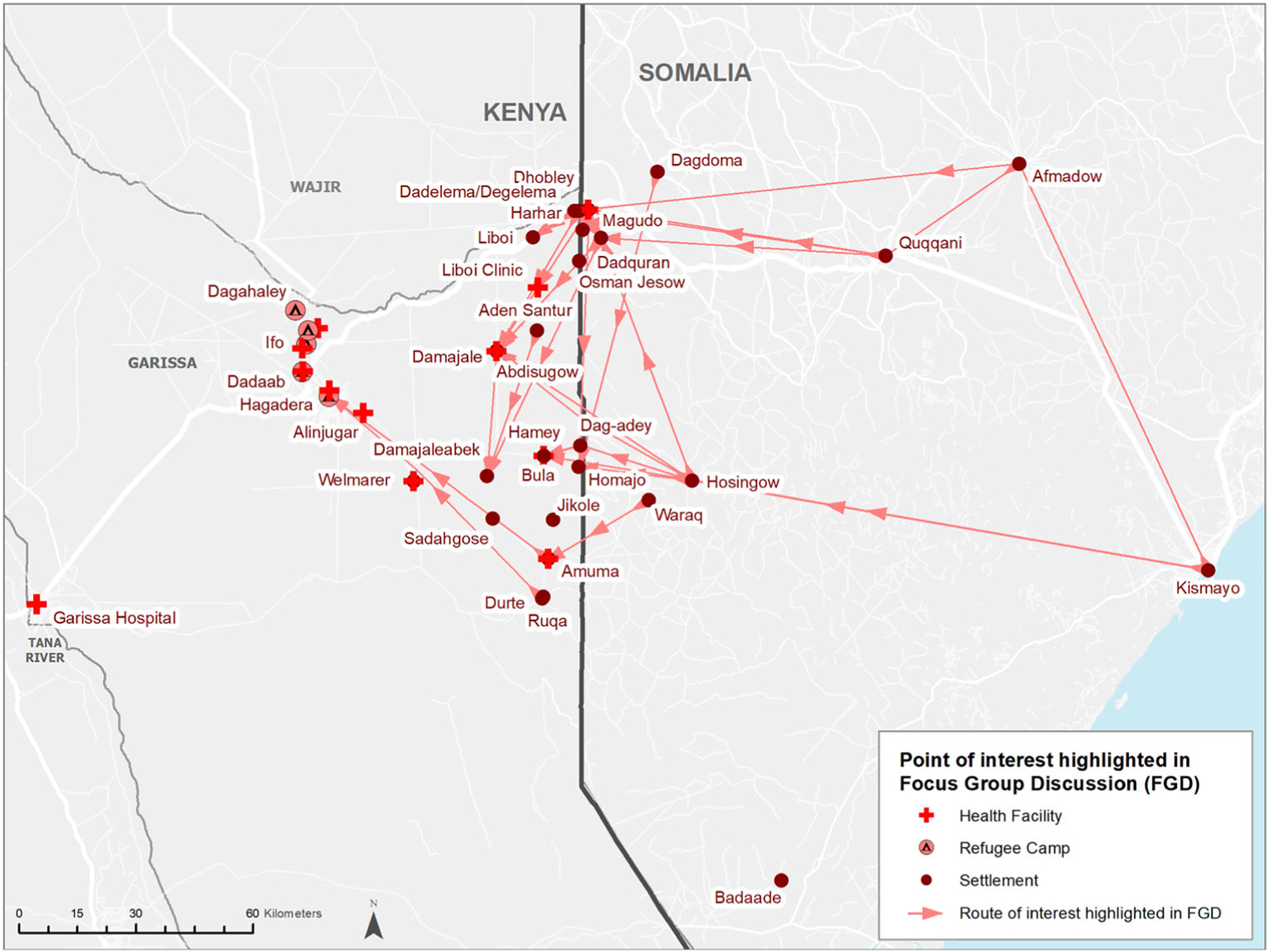
Somali mobile population migration routes by FGD participants.
Damajale respondents listed 5 official border crossing routes and 10 unofficial routes for Somali migrants while Liboi respondents highlighted the following as the official route: Harhar–Liboi; and unofficial routes: Sariraha–Sidedle and Degelema–Magudo into the region. Aden Santur, Dagelema, Hosingow, Dobley, Qoqani, Afmadow, Badaade and Kismayo; and settling mainly in Abdisugow, Magudo and Damajale abeq Liboi FGD participants predominantly noted origin locations as Magudo, Osman Jesow, Dadquran, Baqur, Harhar, Dagelema, Wellburco, Dobley and Getho; and temporary settlement locations as Magudo and Aden Santur.
FGD participants in Amuma, Liboi and Damajale explained that Somali mobile populations tended to arrive annually in the long rainy season of April to June (as opposed to the short rainy season in October–November). Duration of temporary settlements ranged from weeks to the full duration of the rainy season. Damajale participants noted that Somali populations settle in Kenya for a range of 1–6 months while those in Amuma reported shorter durations of a few days or weeks. Three FGDs in Damajale highlighted that Somalis moved into Kenya when there is human–human disease transmission (e.g. polio, measles, diarrheal diseases) in their area. They also fled drought, inter-clan wars and animal disease outbreaks. Participants from the Homajo region of Hamey revealed they came into their area when food relief was locally provided.
Hamey subregion FGDs indicated the widest variety of reasons for migration as well as factors that affected durations of stay. Respondents in half of the FGDs in Hamey stated that Somali migrants moved into their area during the dry seasons (Barkinta, Bula and Dagadey) while the other half mentioned the short rainy season. They also moved out of the area for fear of disease-carrying Tsetse flies or pressure from local security personnel. Those that moved during the dry season appeared to stay for shorter durations, as brief as 1 month, while the short rainy season groups stayed for the full duration of the rains.
Somali migrant relationships with refugee camps
Many Somali nationals entered refugee camps and visited the livestock market, accessed health care and food aid, visited relatives and purchased goods. Amuma FGD participants indicated migratory patterns in a Northwestern direction toward Hagadera Refugee Camp in Fafi Sub-county (Figure 3). Damajale, Hamey and Liboi FGDs indicated the movement of Somali migratory groups toward Ifo, Ifo 2 and Dagahley Refugee Camps in Dadaab Sub-county.
Liboi FGD participants suggested a strong relationship between the camps and healthcare-seeking behaviors of Somali migrants as they were referred to the Ifo refugee camp for healthcare emergencies by regional staff. Additionally, pastoralist families settled near the camps more long-term because of lost livestock due to drought or disease, while others sought immunization. One example of this observation is quoted here from a Liboi FGD participant, ‘4 Nomadic pastoral families migrated from Liboi (71 KM) on March 2018 and settled near Ifo Refugee Camps 2018 to stay for 11 months for livestock trading, food shopping, pasture and water, immunize their children. [FGD Participant in Liboi]’.
Regional healthcare access and views
The following types and numbers of health facilities were reported accessible in the region of study: hospitals (6), clinics (2), health centers (4) and dispensaries (3). According to respondents, all reported healthcare facilities cared for all age and gender groups and provided multiple services. Seven facilities (58%) provided vaccination services (for routine immunization), four facilities (36%) provided nutritional support, and two facilities provided polio vaccination (but possibly not all the routine immunization services) (Hamey dispensary and Hagardera International Rescue Committee (IRC) Hospital).
Facilities without emergency services in Amuma referred patients to Dadaab and Hagadera hospitals. Patients in Welmarer were referred to Garissa hospital but patients paid out-of-pocket for services. Damajale FGD participants sought advanced medical care at the following facilities: Dadaab Hospital, Damajale Health Center, Hagardera Hospital and Ifo 2 Hospital. Hamey FGD participants outlined healthcare access points based on settlements: Homajo – Dadaab Sub-county Hospital and refugee camp; Dagadey – Dobley health center; Barkinta – Hagadera hospital; Bula – Dadaab and Hagadera hospitals (IRC Hospital).
FGD participants in Liboi suggested, unlike the reports from the other three FGDs, that patient nationality determined their referral location, ‘Referral areas for advanced needs are taken to DADAAB refugee camps (78 km) for Somali nationality while those with Kenyan nationality are referred to Dadaab level 4 hospital via Liboi health center’ and ‘Dobley nursing home for Somali nationality while those with Kenyan nationality are referred to Dadaab level 4 hospital via Liboi health center’. Other referral locations noted in Liboi FGDs were Médecins Sans Frontières Dagahley hospital, IRC Hagadera hospital, Kenya Red Cross Society Ifo Hospital.
The FGD participants’ main concern around health in their communities was a lack of resources and health services (e.g. health clinics, latrines, safe water, ambulances, vaccines and nutrition care). In fact, FGD participants stated that one reason for not seeking care at facilities was an assumed lack of resources (e.g. a lack of drugs). Additionally, FGD participants expressed a large concern about diseases (e.g. polio, cholera, measles and animal diseases) entering the country with Somali migrant populations.
Focusing specifically on vaccination services, FGD respondents in Amuma and Liboi mentioned vaccination and nutrition services being available in their area, but Damajale and Hamey participants perceived a lack of vaccination and nutrition services in some of their settlements. FGD participants from the following areas revealed a lack of vaccination services: Damajale central, Damajaleabek, Magudo (Damajale), Dagadey (Hamey). FGD respondents from the following areas specifically mentioned a fear of the influx of polio (from Somalia): Dagadey (Hamey), Liboi, Magudo (Damajale), Abdisugow (Damajale) and Damajale central. In the Bula area of Hamey FGD participants noted stock-outs of measles and BCG vaccines at health facilities.
Polio vaccination campaign planning and implementation
The campaign occurred at the beginning of the long rainy season (April) when FGD participants reported there would be a migrant influx in the region. Twenty-four vaccination sites were determined based on key points of interest suggested by FGD participants: migration routes, temporary settlement locations, and areas potentially lacking healthcare services (Figure 4). Vaccinators also visited an additional five areas that were identified during the vaccination campaign with active migrant presence including: Benaney Qoqar and kiwanjayarey in Hamey; and Sidekotkot, Sheb ad and Ali dagane in Damajale. In total, the campaign reached 29 sites with the following Ogaaden sub-clan affiliations: Auliyahan (25), Mohamed Zubeir (2), Maqabul (1) and Abdalla (1) representing the same clan affiliations of focus group participants.
Figure 4.
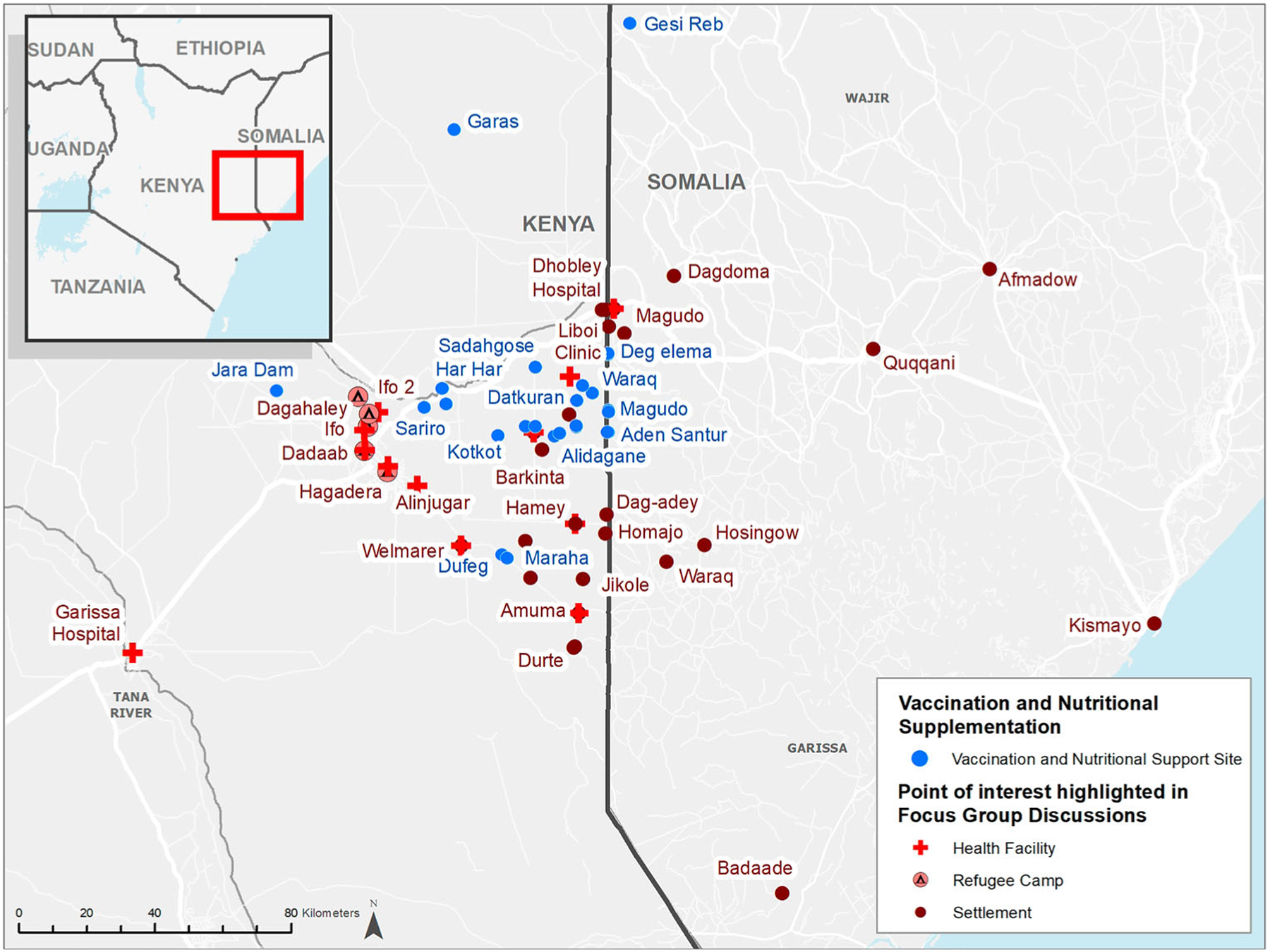
Vaccination and nutritional supplementation locations.
During the 8-week campaign, vaccinators administered 2196 doses of bOPV and 2524 doses of measles vaccine to children. According to parental recall, 192 (9%) of bOPV doses were given to zero-dose children (first dose ever received) and 670 (27%) of the measles doses were zero-dose (Table 1). Additionally, 1636 children aged 12–59 months were provided albendazole and 2008 children aged 6–59 months were provided with vitamin A, which is standardly given with routine immunization vaccinations every 6 months for children within this age group.
Table 1.
Vaccines and treatments provided during 8-week campaign in Garissa county.
| Vaccine/Treatment | Aged 0–11 months | Aged 1–2 years (≥1 and <2 years) | Aged 2–5 years (≥2 and <5 years) | Total |
|---|---|---|---|---|
| OPV (Zero-Dose) | 152 | 22 | 18 | 192 |
| OPV (Additional Dose) | 460 | 631 | 913 | 2004 |
| Percent OPV (Zero-Dose) | 25% | 3% | 2% | 9% |
| Measles (Zero-Dose) | 482 | 95 | 93 | 670 |
| Measles (Additional Dose) | 0 | 744 | 1110 | 1854 |
| Percent Measles (Zero-Dose) | 100% | 11% | 8% | 27% |
| Vitamin A | 275 | 685 | 1048 | 2008 |
| Albendazole | 0 | 555 | 1081 | 1636 |
Of 2410 children screened for malnourishment, based on the WHO child growth standards and their mid-upper arm circumference index (MUAC), 33 had an MUAC <115 mm (severe wasting), 249 were 115–125 mm (moderate wasting) and 2128 were greater than 125 mm (no wasting) (WHO 2009). Subsequently, 113 children (5%) were referred to government facilities for Outpatient Therapeutic Program (OTP) due to Severe Acute Malnourishment (SAM) and 150 (6%) were referred to a supplementary feeding program due to moderate acute malnourishment.
Discussion
GPEI’s mission is that ‘no child ever again suffers from paralytic poliomyelitis’. One of the challenges in achieving that mission is the identification of migrant populations missed by vaccination campaigns and services. This project sought to partially overcome that challenge by utilizing local knowledge of settlement and migration patterns to reach those Somali mobile populations frequently missed by vaccination services.
FGD data and collaborative relationships with regional facilities also allowed for several key vaccination campaign strategies to be followed in assurance of reaching the target population. First, IOM and ARC engaged with Garissa County’s Department of Health to ensure that the vaccination activities complemented government’s immunization service delivery and supplementary immunization activities in the region. The campaign had static teams placed at major crossing routes and border villages with little to no access to healthcare. These were meant to target children under five years entering the country with their parents as new arrivals or returning from Somalia. Mobile teams were used to target nomadic pastoralist settlements and major water points. Lastly, community mobilizers and other leaders provided mass awareness sessions for the target population.
Although we had the limitation of not being able to define if the children reached by the campaign were from mobile populations, we believe the vaccination campaign reached ethnic Somali children and likely migrant Somali children as well. We come to this conclusion because all chiefs who approved the vaccination campaign in their settlement areas were ethnic Somali and the area is defined as ethnic Somali region according to the Kenyan National Bureau of Statistics (as depicted by the BBC 2013). Thus, since we know the chiefs were Somali and the vaccination campaign was in an ethnically Somali region, we can deduce that most of the children served by the campaigns were ethnically Somali. Additionally, the campaign started with the rainy season when our data suggested Somali migrants would be moving through the region. Since vaccination teams went to areas which our data suggested would have Somali migration, it is likely that some of the children vaccinated were of this sub-population. This is further backed by the research of Van Hear, Bakewell, and Long (2018) which showed that Somali migrants tended to move towards areas of clan affiliations. Consequently, since we know the campaign was in an ethnically Somali region and Somali migrants move to regions with Somali clan affiliations where we conducted the campaigns (at the start of the rainy season), we likely vaccinated some Somali migrant children.
One challenge frequently experienced in delivering immunization services to mobile populations is the inability to map the locations and movement patterns (Kamadjeu et al. 2015; Linard et al. 2010; Weitzberg 2015). This is particularly true in our region of study as many of the smaller settlements in Northeastern Kenya are not in known GIS databases. By using local knowledge, we were able to map the general movement patterns and temporary settlement locations of mobile populations in the region. Also, the community-level maps allowed us to use satellite imagery to identify some locations, based on hand drawn key geographical features such as lakes or road intersections, without known GPS coordinates. While it is likely that some of the settlement map locations we provided for the vaccination campaign were not correctly mapped due to possible misinterpretations of the drawn features, we were still able to define locations to place static and mobile vaccination teams in the absence of known GIS coordinates. A solution to possible mapping errors would be that future campaign planning should work with local populations in several iterations of participatory mapping to create the most accurate depictions of the region to inform public health interventions.
Studying migrants through FGDs and mapping could also allow public health workers to develop clearer understanding of who moves and for what purposes. In this study, we found that most of the Somali migrants in the region identify as pastoralists and that seasonality is the best predictor of movement. Additionally, they reportedly utilize refugee camps for resources (livestock trading, healthcare, vaccinations) while in the country. This suggests that a proportion of the migrants could most likely be targeted annually during the long rainy season and in times of drought, conflict, or high disease burden in Southern Somalia. If the project had the time and resources to continue with additional campaigns, we could have used the data to treat more children at specific intervals in the year.
As our research and that of Van Hear, Bakewell, and Long (2018) suggests, the current systems of identifying communities within national borders does not translate well to providing services for the migratory populations who do not stay within those boundaries. Van Hear, Bakewell, and Long’s (2018) research showed that there are many push and pull factors which facilitate the movement of people inside and across borders and, until regional policy change to support those migrant populations, migrants will independently decide to move to places of opportunity. Similarly, our FGDs showed that some healthcare providers treated the Somali populations differently in the region, as some Somali patients were referred to refugee camp-based healthcare facilities while Kenyan patients were referred to more local healthcare facilities. Our data also showed that some Somali migrants stayed in the region for several months potentially affecting herd immunity in the region but were not likely counted in the regional vaccine coverage rates. As a result, public health authorities could potentially assume the region was not at risk. However, when working toward international public health goals, such as polio eradication, we recommend that ethnic sub-populations be properly tracked and included in public health figures wherever they reside, regardless of their national identity. Additionally, regional teams should coordinate and communicate across borders as various factors, such as drought and conflict, affect the movement of populations from one area to another.
Lastly, healthcare utilization is not always about ease of access. A study by Linard et al. (2010) of the Turkana Region of Northern Kenya showed that nomadic people sometimes choose not to access healthcare due to a multitude of factors (e.g. illiteracy, traditional practices, conservatism). This research layered with the vaccination campaign finding zero-dose children suggests that our population of interest could have similar social or cultural barriers adding to the limited healthcare access. Our focus group discussions disclosed that people do not frequent certain health centers which are perceived to lack quality healthcare services and some health centers refer clients to certain facilities based on their nationality. This could be a contributing factor to why unvaccinated children were found during the campaign, as they may not be seeking immunization or health care services in the region due to distrust or uncertainty of availabilities. More research should be done in this area to better understand the healthcare-seeking behaviors of migratory populations.
A limitation to our study was identifying zero-dose children. During the vaccination campaign, 9% of bOPV doses and 27% of measles doses were given to zero-dose children. However, since these proportions were based on parental recall, we cannot conclude that all these children were confirmed zero-dose, nor that all true zero-dose children were identified. Also, since the first dose of the measles vaccine is given at 9 months of age, some of the reported measles zero-dose children may have just recently reached the age to receive the vaccine.
In conclusion, this project exemplified the importance and benefits of collaboration between community-based data collectors and utilization of local knowledge to support outreach of public health interventions. While mobile populations can be challenging to reach for health services, input from residents of established communities along migratory routes can help us better understand patterns of movement and healthcare-seeking behaviors, critical information in reaching these at-risk populations. Additionally, regional teams working across borders, with increased resources at times of suspected increased migration, could reduce disease burden within mobile populations. Such methods could therefore be used in future projects to help improve other public health interventions.
Acknowledgements
We would like to thank Zeinabou Daffe for her support in the development of the data collection methods and Kira Walker for supporting with geocoding and the spatial database development. This project was funded by the US Centers for Disease Control and Prevention through grant #NU2GGH002091.
Funding
This work was supported by Center for Global Health: [Grant Number NU2GGH002091].
Appendices
Appendix A: Focus group questions
(Facilitator should guide participants through the following questions)
- Where are the villages/ communities (locate on map)?
- Who lives in these communities/villages?
- Approximately how many families/people?
- What are the ethnicities/ nationalities of these communities?
- Tell me about the communities which are Somali by origin.
- Which areas are Somali (locate on map)?
- When did they arrive?
- Do you know how long they expect to remain? Will they move with the seasons or will they remain until an event allows or pushes them to move elsewhere?
- Do you know where they came from (locate on map)?
- Have they been here before?
- If so, when and for how long?
- How long do migrants typically stay?
- Do you know where they have settled in other areas (locate on map)?
- Why do migrants leave Somalia (drought, job)?
- Where do people access health care (locate on map)?
- What are they (mobile, hospitals, clinics, traditional healers)?
- Who do they provide services for (pediatric, maternal, adult)?
- What kind of services are provided (vaccination, nutrition)?
- Where are the areas where health services are lacking (locate on map)?
- Are there certain health needs that need to be addressed in these areas (measles, cholera, nutrition)?
Is there anything additional you would like to share about your community, the movement of people in and out of the area? Or about their access to health care?
Appendix B: Participatory Map Examples
Village Level Map
Annotation of Movement Patterns on Large Regional Maps
Footnotes
Disclosure statement
No potential conflict of interest was reported by the author(s).
Disclaimer
The findings and conclusions in this report are those of the author(s) and do not necessarily represent the official position of the Centers for Disease Control and Prevention.
References
- Alleman Mary M., Jorba Jaume, Greene Sharon A., Diop Ousmane M., Iber Jane, Tallis Graham, Goel Ajay, Wiesen Eric, Wassilak Steven GF, and Burns Cara C.. 2020. “Update on Vaccine-Derived Poliovirus Outbreaks—Worldwide, July 2019–February 2020.” Morbidity and Mortality Weekly Report 69 (16): 489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- BBC. 2013. Kenya Election: Maps and Graphics. British Broadcasting Channel (BBC). Accessed September 2020. https://www.bbc.com/news/uk-21592589 [Google Scholar]
- Global Polio Eradication Initiative (GPEI). 2020. Somalia Flash Update: Week 27 2020.
- Greene Sharon A., Ahmed Jamal, Datta S. Deblina, Burns Cara C., Quddus Arshad, Vertefeuille John F., and Wassilak Steven GF. 2019. “Progress Toward Polio Eradication—Worldwide, January 2017–March 2019.” Morbidity and Mortality Weekly Report 68 (20): 458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haydarov Rustam, Anand Saumya, Frouws Bram, Toure Brigitte, Okiror Sam, and Bhui Bal Ram. 2016. “Evidence-Based Engagement of the Somali Pastoralists of the Horn of Africa in Polio Immunization: Overview of Tracking, Cross-Border, Operations, and Communication Strategies.” Global Health Communication 2 (1): 11–18. [Google Scholar]
- Hsu Christopher H., Mahamud Abdirahman, Safdar Rana Muhammad, Ahmed Jamal, Jorba Jaume, Sharif Salmaan, Farag Noha, Martinez Maureen, Tangermann Rudolph H., and Ehrhardt Derek. 2016. “Progress Toward Poliomyelitis Eradication—Pakistan, January 2015–September 2016.” Morbidity and Mortality Weekly Report 65 (46): 1295–1299. [DOI] [PubMed] [Google Scholar]
- Jorba Jaume, Diop Ousmane M., Iber Jane, Sutter Roland W., Wassilak Steven G., and Burns Cara C.. 2016. “Update on Vaccine-Derived Polioviruses—Worldwide, January 2015–May 2016.” Morbidity and Mortality Weekly Report 65 (30): 763–769. [DOI] [PubMed] [Google Scholar]
- Kamadjeu Raoul, Mulugeta Abraham, Gupta Dhananjoy, Hirsi Abdirisak Abshir, Belayneh Asalif, Clark-Hattingh Marianne, Adams Clement, et al. 2015. “Immunizing Nomadic Children and Livestock–Experience in North East Zone of Somalia.” Human Vaccines & Immunotherapeutics 11 (11): 2637–2639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Linard Catherine, Alegana Victor A., Noor Abdisalan M., Snow Robert W., and Tatem Andrew J.. 2010. “A High Resolution Spatial Population Database of Somalia for Disease Risk Mapping.” International Journal of Health Geographics 9 (1): 45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Masters Nina B., Wagner Abram L., Carlson Bradley F., Muuo Sheru W., Mutua Martin K., and Boulton Matthew L.. 2019. “Childhood Vaccination in Kenya: Socioeconomic Determinants and Disparities among the Somali Ethnic Community.” International Journal of Public Health 64 (3): 313–322. [DOI] [PubMed] [Google Scholar]
- Van Hear Nicholas, Bakewell Oliver, and Long Katy. 2018. “Push–Pull Plus: Reconsidering the Drivers of Migration.” Journal of Ethnic and Migration Studies 44 (6): 927–944. [Google Scholar]
- Weitzberg Keren. 2015. “The Unaccountable Census: Colonial Enumeration and its Implications for the Somali People of Kenya.” The Journal of African History 56 (3): 409–428. [Google Scholar]
- World Health Organization. 2009. “WHO Child Growth Standards and the Identification of Severe Acute Malnutrition in Infants and Children: Joint Statement by the World Health Organization and the United Nations Children’s Fund.” [PubMed]


