Abstract
Background
Among the world, the most frequently discovered and fatal cancer in women is breast cancer (BC). From the perspective of public health, estimating the BC risk linked to dairy intake may aid in comprehensive management. In epidemiological research data on the association between eating dairy foods and the risk of BC are conflicting. Therefore, we sought to assess the link between dairy food consumption and the development of BC.
Main text
To summarize and quantify the most recent findings on consuming milk or other dairy foods and the development of BC, we performed a systematic literature review. We checked through several databases for relevant publications published in English up to January 2022. Of the 82 articles identified, only 18 met the inclusion criteria and were analyzed. Nine Prospective, seven Retrospective and two Cross-Sectional studies were finally identified.
Conclusions
Overall, dairy consumption was inversely associated with the risk of developing breast cancer. Future studies will help elucidate the role of dairy products in human health, and their use within a balanced diet should be considered.
KEY MESSAGES
The effect of different types of dairy products, and possible dose-response relationships on BC risk remains unknown.
Estimating BC risk associated with dairy consumption may help to take the decision-making of physicians and public health policy in developing preventive strategies to reduce its occurrence.
This systematic review was conducted to assess dairy consumption and BC risk.
Overall, inverse associations were found when looking at dairy consumption and BC risk.
Keywords: Breast cancer, Dairy products, Milk products, Systematic review
1. Introduction
Among the world, the most frequently discovered and fatal cancer in women is BC [1]. BC has now overtaken lung cancer as the world’s mostly commonly-diagnosed cancer [2]. Every 14 s, a woman is diagnosed with BC somewhere in the world. In 2020, more than 2.3 million women were diagnosed with BC worldwide and 685,000 died [1]. Diet and lifestyle are two of the most modifiable aspects of a person’s life that are thought to be effective cancer prevention strategies [3–6]. On the one hand, lifestyle changes like minimizing sedentary behavior [7], consuming less alcohol [8], and smoking less [8] are thought to lower BC risk. In one sense, dietary choices influence cancer incidence and health [9]. Several recent investigations on the association between food and BC have been undertaken. There is some evidence that the Mediterranean diet [10], is associated with reduced BC risk. Various studies on the impact of milk products [11], dietary fiber [12], and soy products [13] on BC risk. Furthermore, higher intakes of dairy calories and dairy milk were associated with a greater risk of BC [9].
Abundant research on the influence of milk products on BC risk has yielded results; however, they were inconsistent. The anticarcinogenic characteristics of calcium, vitamin D, and lactoferrin are cited as supporting the basic theory that a dairy diet reduces BC risk. These compounds are mostly found in dairy products, and research suggests that they could help to decrease the BC risk. Contrarily, the consumption of dairy products has been connected to a higher chance of developing BC. The high usage of dairy products could indicate a greater consumption of dietary fat, saturated fat in particular, which is linked to a higher risk of developing BC. In addition, milk contains several pollutants and compounds that may be hazardous to human health, including estrogen, which has been associated with increased replication abnormalities of DNA and mitotic activity, and insulin-like growth factor I (IGF-I), which promotes BC cellular proliferation [14].
In conclusion, the consequence of various dairy foods on the incidence of development of BC, as well as any dose-response correlations, remain undefined. As a result, the goal of this review was to summarize the association between milk product intake and BC risk. This is significant because assessing the BC risk linked with dairy consumption may aid in physician and public health policy decision-making. The main goals of the current research were to conduct a systematic review on the association between the consumption of dairy foods and BC development, and the relation between each type of milk product and BC risk during the last 15 years from 1st Jan 2008 to 31st January 2022.
2. Methodology
2.1. Study protocol and registration
This systematic review adhered to the Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA) standards. The protocol was submitted for inclusion in the international prospective register of systematic reviews (PROSPERO) (CRD42022304654).
2.2. Sources of data
A search of pertinent studies evaluating the link between the consumption of milk products and the development of BC released during the last 15 years from 1st January 2008 to 31st January 2022 was carried out in international databases (SCOPUS, PubMed (MEDLINE), The Cochrane, Google Scholar, and Science Direct).
2.3. Search strategy
Each database was given its own set of controlled vocabulary terms to use. The search criteria were MeSH terms and text phrases associated with the association, as well as breast cancer and dairy products, using a combination of the following keywords: (‘breast neoplasms’ OR ‘breast cancer’ OR ‘breast tumor’ OR ‘BC’) AND (‘milk’ OR ‘dairy’ OR ‘dairy products’). Two datasets were used to examine the search method (Google Scholar and PubMed), and its capacity to locate known pertinent papers in each database was further improved. To search for additional relevant information in the lists of references from the contained publications, a forward and reverse link chain of the included research was done.
2.4. Eligibility criteria
The following were developed as specific conditions for eligibility:
2.4.1. Inclusion criteria
All studies that are included are observational studies for example; (cross-sectional, case-control, cohort, and longitudinal).
Consumption of milk products was the study’s main exposure (containing all forms of yogurt, cheese, milk, and milk products), and the finding was the risk of development of BC.
Studies were conducted in the last 15 years from 1st January 2008 to 31st January 2022.
Only studies reported in English-language.
Studies were conducted on women diagnosed with BC as well as those who were not.
2.4.2. Exclusion criteria
Conference proceedings, case reports, qualitative research, and opinion articles, as well as studies that do not include full-text articles, book chapters, and editorials.
Studies in which the main goal was to look at the link between eating dairy foods and other malignancies.
Studies with inadequate data, and unrelated outcomes.
Studies not published in English.
2.5. Data extraction
Each database’s search outcomes were downloaded either in NBIB (.nbib) format or a common tag format established by Research Information Systems (.ris). In databases (like Google Scholar) where downloading all search results at once is not possible, sections of the results were retrieved, added to the library of the EndNote, and removing duplicates were all done. After removing duplicates, the result of the search was transferred as a Text File (*.txt) and then converted into an Excel worksheet (.xlsx). To discover possible publications of interest, Titles and abstracts underwent an initial screening. The full texts of papers that could have qualified were downloaded and reevaluated for inclusion/exclusion standards. To eliminate bias in study selection, eligibility was assessed in duplication and independently. The full-text review was followed by a comprehensive examination of the reasons why certain papers were excluded. Following studies identification, their data were abstracted in Microsoft Excel format using a pre-designed, pre-piloted computerized data abstraction form to evaluate the value of the research and to synthesize the available evidence. To reduce the possibility of errors, data abstractions were carried out independently. The research title, name of the author, publication’s year, country, sample size, study design, age, methodology of dietary assessment, dairy product type, and result were all abstracted.
Data were obtained from all publications that contained the same study where there were several ones, however, only the most recent and ‘complete’ data were used. The data were reviewed after overlaps in the obtained data were resolved. Research flow diagrams based on PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) were created to display the results of literature screening and search.
2.6. Quality analysis
In this review, quality was assessed independently and in duplicate by two independent reviewers using a standardized critical appraisal method for quality evaluation. All disagreements were settled through discussion, which included the participation of a third review author.
3. Study results
3.1. Selection methods
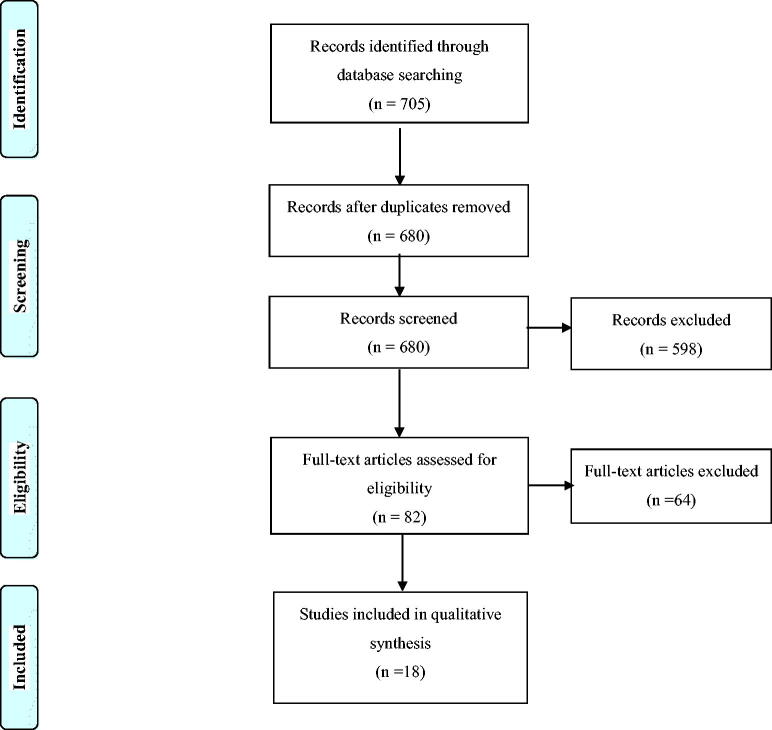
In our preliminary search of the database, 705 articles were found. Following the exclusion of duplicate papers, 680 publications were assessed based on titles and abstracts, with 82 papers qualifying for full-text review. In all, 82 full-text papers were reviewed for eligibility, with 18 of them relating to the relationship between BC and dairy product intake between 2008 and 2022 (Figure 1: PRISMA Flow of information diagram).
Figure 1.
Preferred Reporting Items for Systematic Reviews and Meta-Analyses (The PRISMA) flowchart.
3.2. Characteristics of studies for systematic review
We assessed 18 observational studies on the relationship between the consumption of milk products and the hazard of the development of BC in this systematic literature review. Five of the 18 articles were done in the United States, three in Iran, two in Spain, one each in the Netherlands, French, China, Korea, Japan, Poland, and Algeria another was from European Perspective Investigation into Cancer and Nutrition. Among 18 studies, 9 were prospective studies, 7 were retrospective studies, and 2 were cross-sectional. Dairy results are separated into cheese, milk, yogurt high-fat, and low-fat products.
3.3. Dairy products and breast cancer risk
Analyzing epidemiological research that looked at the link between ingestion of dairy foods and the hazard of development of BC. According to what has been found so far, there is a lot of variety in how data on dairy consumption is gathered and reported. While some research separates down dairy product consumption into subcategories like milk, cheese, and yogurt, some studies report overall dairy product intake. In other studies, high-fat milk products were evaluated independently from low-fat milk products. Table 1 summarizes the selected studies that investigated dairy product intake in relation to BC, arranged by date of publication [9,15–31]. On the relationship between BC and total dairy products, five cohort studies [15,18,19,22,29], six case-control studies [17,20,23,25,28,31], and one cross-sectional research [21] were published. Among the cohort studies, one [15] found that BC and milk product intake were statistically significantly inversely related. In contrast, four other studies [18,19,22,29] did not demonstrate such a relationship. The case-control study findings were inconclusive, with an inverse association reported in four studies [20,23,25,28], a positive association reported in one research [31], and no association reported in one study [17]. According to the cross-sectional study, women who consume dairy foods have a lower risk of developing BC than women who do not consume total dairy products.
Table 1.
Study characteristics, exposure levels, ORs, HR, RR (95% CI), and results of published studies on dairy products intake in relation to breast cancer risk.
| No. | Study title | Author’s name, and year of publication | Country | Study design | Sample size | Dairy product type | Exposure levels | ORs, HR, RR (95% CI) | Results |
|---|---|---|---|---|---|---|---|---|---|
| 1. | Dairy Consumption and Incidence of Breast Cancer in the ‘Seguimiento Universidad de Navarra’ (SUN) Project [15] | Aguilera-Buenosvinos et al. (2021) | Spain | Prospective | 10,930 women follow-up period of 12.1 years. confirmed 119 incident BC cases |
-Total dairy | 3–4 servings per day | 0.49 (0.29–0.84) | Females in the 2nd and 3rd quartiles of whole dairy intake showed a significant inversely proportional relationship. |
| -Whole-fat dairy | 1.6 servings per day | 1.09 (0.63–1.87) | They observed no associations between BC and whole-fat dairy consumption. | ||||||
| -Low-fat dairy | 1.7 servings per day | 0.55 (0.32–0.92) | Compared with women in the low-fat dairy consumption category, women with moderate intake had significantly higher total BC. | ||||||
| 2. | Dairy, soy, and risk of BC: those confounded milk [9] | Fraser et al. (2020) | USA | Prospective | 52,795 women follow-up period of 7.9 years confirmed 1057 new BC women | -Milk | 0.63 kcal/g | 1.50 (1.22–1.84) | Higher dairy milk consumption was related. No relationships were found with cheese or yogurt. |
| -Cheese | 3.2–3.9 kcal/g | 0.89 (0.69–1.14) | |||||||
| -Yogurt | 0.6–0.9 kcal/g | 0.98 (0.82–1.17) | |||||||
| 3. | Milk Consumption Decreases Risk for Breast Cancer in Korean Women under 50 years of Age: Results from the Health Examinees Study [16] | Shin et al. (2019) | Korea | Prospective | 78,320 participant follow-up period of 6.3 years confirmed 359 BC | -Milk | ≥1 serving/day | 0.58 (0.35, 0.97) | In women under the age of 50, increased milk intake was related with a decreased incidence of BC (p = .0195). This interaction, however, was not statistically significant. In either age group, we found no link between BC risk and yogurt or cheese consumption. |
| -Cheese | ≥2 serving /week | 1.43 (0.69, 2.96) | |||||||
| -Yogurt | ≥1 serving/day | 1.03 (0.61, 1.74) | |||||||
| 4. | Effect of dairy products intake on breast cancer risk: A case-control study in Algeria [17] | Maliou et al. (2018) | Algeria | Case control | 184 BC cases and 184 controls | -Total dairy | 418.97 g/d | 1.50 (0.77–2.92) | Each type of dairy product may affect BC risk differently. Milk consumption was related to higher risk; however, total and fresh cheese was linked with reducing the risk of BC development. |
| -Milk | 254.49 g/d | 2.61 (1.32–5.16) | |||||||
| -Yogurt | 84.87 g/d | 0.60 (0.31–1.15) | |||||||
| -Cheese | 39.00 g/d | 0.38 (0.18–0.78) | |||||||
| 5. | Dairy Consumption in Adolescence and Early Adulthood and Risk of Breast Cancer [18] | Farvid et al. (2018) | Boston, USA | Prospective | 90,503 premenopausal women follow-up confirmed 3191 cases of invasive BC were identified from 1991 through 2013. Among women with adolescent dietary intake, 1318 cases of invasive BC from 1998 through 2013. | -Total dairy | 1 serving/day | 1.02 (0.97–1.07) | The consumption of total dairy food in adolescence and adulthood was shown to be unrelated to the overall risk of BC (per serving per day in adolescence. |
| -Low-fat dairy | 1 serving/day | 1.00 (0.94–1.06) | |||||||
| -High-fat dairy. | 1 serving/day | 0.97 (0.93–1.02) | |||||||
| 6. | Animal foods and postmenopausal breast cancer risk: a prospective cohort study [19] | Marcondes et al. (2018) | Netherlands | Prospective | 3209 women follow-up period of 17 years confirmed 199 BC cases. | -Total dairy | 420 (SD 229.7) g/d | 0·99 (0·65, 1·50) | There was no consistent link established among dairy intake and the risk of development of BC. |
| -Cheese | 34 (SD 19.8) g/d | 1·19 (0·79, 1·78) | |||||||
| -Milk | 305 (SD 212.9) g/d | 1·31 (0·87, 2·00) | |||||||
| -Yogurt | 68 (range 1–991.3) g/d | 0·97 (0·65, 1·45) | |||||||
| 7. | Usual Consumption of Specific Dairy Foods Is Associated with Breast Cancer in the Roswell Park Cancer Institute Data Bank and Biorepository [20] | McCann et al. (2017) | USA | Case-Control | 1941 BC cases and 1237 controls | -Total dairy | ≥ 42 serving\month | 0.85 (0.68–1.06) | Total dairy consumption and yogurt consumption had an inverse relationship with BC, whereas other cheese had a positive relationship. Our findings imply that some dairy foods may influence BC risk. |
| -Milk | ≥ 28 serving\month | 0.96 (0.75–1.24) | |||||||
| -Yogurt | ≥ 14 serving\month | 0.61 (0.46–0.82) | |||||||
| -Cheese | ≥ 14 serving\month | 1.53 (0.99–2.34) | |||||||
| 8. | Breast cancer - Analysis of the selected risk factors [21] | Plagens-Rotman et al. (2017) | Poland | Cross-Sectional | 762 women (79 BC cases and 683 healthy women). | -Total dairy products | 125 g/day | 0.58 (0.30, 1.11) | Women who consumed 125 g of dairy food per day had a lower risk compared to women who did not consume it. |
| 9. | Dietary patterns and breast cancer risk in a prospective Japanese study [22] | Kojima et al. (2016) | Japan | Prospective | 23,172 women follow-up period of 16.9 years confirmed 119 incidences of BC |
-Total dairy | High | 1.32 (0.70–2.49) | Dairy consumption was not associated with an increased risk of BC development. |
| 10. | Dietary Patterns and Risk of Breast Cancer in Women in Guilan Province, Iran [23] | Ahmadnia et al. (2016) | Iran | Case-Control | 225 BC cases and 225 controls | -Milk and dairy products | 2–3 glass/day | 0.6 (0.4–0.9) | Daily intake of two to three cups of milk and milk food, as opposed to more than three glasses of milk products, lowered BC risk by 40%. |
| 11. | Dietary habits contributing to breast cancer risk among Iranian women [24] | Mobarakeh et al. (2014) | Iran | Case-Control | 53 BC cases and 40 controls | -Milk | High intake | 17.45 (2.19–138.98) | Women who consume full-fat dairy products, including milk and cheese, have a significantly increased the risk of development of BC than women who did not consume. |
| -Yogurt | 6.8 (2.08–22.17) | ||||||||
| -Cheese | 6.88 (1.44–32.77) | ||||||||
| 12. | Is dairy intake associated to breast cancer? A case-control study of Iranian women [25] | Bahadoran et al. (2014) | Iran | Case-Control | 275 women (100 cases and 175 controls). | -Total dairy | > 680 g/d | 0.14 (0.04–0.38) | As overall dairy consumption increased, the risk of development of BC decreased (p < .001). |
| -Low-fat dairy | > 680 g/d | 0.10 (0.03–0.34) | A decreased incidence of BC was also observed when low-fat dairy consumption was increased (p < .001). | ||||||
| -High-fat dairy | < 224g/d | 0.22 (0.07–062) | Reduced the risk of BC was linked to a lesser consumption of high-fat dairy products. | ||||||
| 13. | Calorie intake, olive oil consumption, and mammographic density among Spanish women [26] | García-Arenzana et al. (2014) | Spain | Cross-Sectional | 3548 women (Premenopausal (n = 811); Postmenopausal (n = 2737) |
-Whole milk | > 200 g/d | 1.10 (1.00-1.20) | Higher whole milk consumption was linked to a higher mammography density associated with BC risk. |
| 14. | Consumption of dairy and meat in relation to breast cancer risk in the Black Women’s Health Study [27] | Genkinger et al. (2013) | Boston, USA | Prospective | 52,062 women follow-up period of 12 years confirmed 1,268 incident BC cases | -Whole milk | ≥ 250 g/week | 0.96 (0.73–1.26) | Association of BC with whole milk was not statistically significant. Furthermore, there was a moderate not significant inverse association between hard cheese and yogurt consumption and BC risk. |
| -Cheese | ≥ 75 g/week | 0.88 (0.68–1.12) | |||||||
| -Yogurt | ≥ 454 g/week | 0.91 (0.71–1.17) | |||||||
| 15. | Dairy products, calcium intake, and breast cancer risk: a case-control study in China [28] | Zhang et al. (2011) | China | Case-Control | 438 BC cases and 438 controls | -Total dairy | 8.15 g/d | 0.73 (0.52–1.02) | High consumption of whole milk and low-fat milk products was found to be inversely related to the risk of BC development (based on whole milk and low-fat milk dry weight, respectively). |
| -High-fat dairy | 5.17 g/d | 0.84 (0.60–1.17) | |||||||
| -Low-fat dairy | 2.98 g/d | 0.76 (0.56–1.03) | |||||||
| 16. | Adolescent diet in relation to breast cancer risk among premenopausal women [29] | Linos et al. (2010) | USA | Prospective | 39,268 premenopausal women follow-up period of 7.8 years confirmed 455 incident cases of invasive BC | -Full-fat milk | High intake | 1.09 (0.73–1.63) | There was no significant correlation found between total milk or dairy consumption. |
| -Total dairy | 0.90 (0.64–1.27) | ||||||||
| -High-fat milk | 0.95 (0.68–1.35) | ||||||||
| 17. | Meat, eggs, dairy products, and risk of breast cancer in the European Prospective Investigation into Cancer and Nutrition (EPIC) cohort [30] | Pala et al. (2009) | Denmark, France, Germany, Greece, Italy, Norway, Spain, Sweden, the Netherlands, and the United Kingdom | Prospective | 319,826 women follow-up period of 8.8 years confirmed 7119 BC cases | -Whole milk | 150 g/d | 1.06 (0.97, 1.15) | There was no consistent link established between BC risk and dairy product usage. |
| -Cheese | 82.1 g/d | 0.97 (0.89, 1.06) | |||||||
| 18. | Dietary factors and breast cancer risk: a case-control study among a population in Southern France [31] | Bessaoud et al. (2008) | Southern France | Case-Control | 437 BC cases and 922 controls | -Total dairy | 134.3 and 271.2 g/day | 1.57 (1.06–2.32) | Compared to the risk linked with decreased intake (134.3 g/d), the risk of developing BC is associated with higher intake, between 134.3 and 271.2 g/d. |
Several studies showed inverse relationships between low-fat [15,25,28] and high-fat dairy [18,25,28,29]. Many of the epidemiologic studies that have been published have focused on specific types of dairy products. Six cohort studies [9,16,19,27,29,30], four case-control studies [17,20,23,24], and one cross-sectional study [26] investigated the association between BC and whole milk consumption, the findings were inconclusive. Shin et al. found substantial inverse relationships among women [16], McCann et al. on the USA people [20], Ahmadnia et al. on Iranian women [23], and Genkinger et al. in Boston [27]. These findings contradict those of seven previous studies [9,17,19,24,26,29,30] that found a link between increased consumption and BC.
Research findings reporting the risk associated with yogurt were inconclusive. Inverse associations have been reported by McCann et al. [20], reported, while Mobarakeh et al. showed that in one study risk of BC development was increased significantly [24], while no association was reported for [9,16,17,19,27]. Several studies provide similarly varied evidence of the relationship between cheese intake and BC, with findings ranging from a considerably lower risk [17] to no significant link [9,16,17,19,27], to a significantly higher risk [24].
4. Discussion
In this systematic review, we summarized the evidence found regarding the association between dairy product consumption and the risk of BC from 18 observational studies. Among 18 studies, 9 were prospective studies, 7 were retrospective studies, and 2 were cross-sectional.
Whether dairy products play a protective or harmful role against BC occurrence in the female population is still controversial. Generally, the existing epidemiological studies showed an inconsistent association between dairy food intake and the incidence of BC. The findings of this systematic review, which included 18 observational studies conducted in the last 15 years from 1st January 2008 to 31st January 2022, indicated that dairy consumption is inversely and significantly associated with the development of BC was reported in six studies. In contrast, there is only one study showed a positive relationship and five studies showed no relationship. While some components of milk have been attributed a positive association with the risk of BC other components seem to have a protective factor. The role of dairy products in the development of BC is thought that it would be able to be explained by different mechanisms.
Recent works have shown that dairy products have both pro- and anti-carcinogenic effects. Dairy products are rich in calcium, vitamin D, and conjugated linoleic acid, which affect cell proliferation and differentiation and can inhibit tumor development. Conversely, dairy products with high levels of fats, saturated fats, and possibly cancer-causing contaminants like pesticides, estrogen metabolites, and growth factors like IGF-1 raises the risk of BC [11].
Vitamin D and calcium are metabolically interrelated and highly correlated dietary factors. Experimental studies have shown their anti-carcinogenic effects are carried out through several mechanisms, such as inhibition of proliferation, induction of apoptosis and autophagic cell death and suppression of angiogenesis, demonstrating that vitamin D can have a crucial role in tumor suppression [32,33]. Additionally, Vitamin D has been discovered to have antiproliferative effects in BC cell lines by causing cell cycle arrest in phase G0/G1 [34,35]. As a result, growth-inhibiting hormones such transforming growth factor B are elevated whereas growth-promoting hormones like IGF-I are downregulated. Because of its antiproliferative properties, 1,25 (OH) D encourages morphological and biochemical modifications linked to apoptosis, such as cell shrinkage, DNA breakage, and chromatin condensation [34]. To lower the risk rate of BC, we therefore hypothesize that dairy products may have a preventive effect on female populations through several of the aforementioned routes.
Consuming yogurt or fermented dairy products was linked to a decreased incidence of BC. In terms of nutrition, yogurt is superior to milk since it contains probiotics, protein, calcium, riboflavin, vitamin B6, and vitamin B12 [36]. In a murine model, the probiotic Lactobacillus acidophilus, which is found in yogurt, may modify the immune response to BC.
Regarding whole milk consumption, our findings showed that seven studies were linked to a higher risk in the study group, while four studies were linked to a lower risk in the study population. Numerous studies show a consistent pattern in the association between cheese eating and BC, with findings ranging from a noticeably decreased risk to no discernible risk link to a significantly higher risk.
There are various hypothesized methods through which dairy products may increase BC risk in a good or negative way. The following are the main hypotheses that link the intake of milk products to an increased risk of BC: (1) A high dairy intake could indicate high-fat consumption in general, particularly saturated fat has been linked to an increased risk of BC; (2) Pesticides and other possibly cancer-causing substances may be present in milk products; and (3) It has been shown that the IGF-I found in milk encourages BC cellular growth.
Another hypothes linking excessive dairy consumption to an increased risk of BC focuses on contaminants in milk products, particularly pesticides [37]. Other researchers have made an effort to relate dietary components to blood organochlorine concentrations, which are environmental poisons that are frequently referred to as ‘endocrine disruptors.’ Nevertheless, there isn’t enough proof to support the link between BC and circulating organochlorine concentrations [38–40].
Outwater et al. [41] suggested that IGF-1, a protein found in both cow milk and human, could be probably relate between milk intake and BC risk. It has been shown that IGF-I promotes BC cell growth [42]. Furthermore, malignant transformation caused by a cellular or viral oncogene can be prevented by removing or obstructing of IGF-I receptors from the cellular membrane, thus IGF-1 plays an important role in cellular transformation [42]. According to these researchers, dairy cows are regularly given bovine growth hormone (bGH) in order to produce more milk, thus increases the amounts of IGF-I that is produced in the milk [43]. Outwater et al. came to the conclusion that due to the fact that IGF-I is not eliminated during pasteurization, it is possible it will not be broken down during digestion in the gastrointestinal system [41].
Variation in reported consumption levels between populations is another essential factor to consider when analyzing epidemiologic data. There is currently no standard way for classifying the intakes of milk product, Consequently, a number of studies have done fair comparisons based on intake quantiles within their study group. Due to widely variation in estimated consumption amongst groups, what is considered ‘high’ in one may be considered ‘low’ in another. The investigators failed to record the level of intake inside each quantile in some circumstances, making it hard to compare outcomes across studies with roughly the same amount of consumption.
Several pathways involved in the development of BC may be impacted by the micro- and macronutrients found in dairy products, however, in general, the risk is neither increased nor decreased. As a result, more research on the link between consuming of milk products and BC risk, including hormonal and environmental variables in addition to micronutrients, is needed.
5. Conclusion
In conclusion, dairy products intake was inversely associated with the risk of BC in most studies. Despite several intriguing theories about the linkage between consuming milk product and the development of BC, ingestion of milk or other milk products does not strongly associate with the development of BC, according to the existing epidemiologic research. Diet is considered a modifiable risk factor for BC. These findings may therefore help to inform decision-making in public health policy. Knowledge gaps are made predictable and deserve considerable attention to clarify prevention efforts globally.
Supplementary Material
Funding Statement
The researchers themselves provided funding for this project, and an incentive grant from GIPS-PhD: 311/PPSP/4404818.
Data availability statement
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Ethical approval
This systematic review is a part of Ph.D. literature and ethical approval was obtained from the Helsinki committee to carry out the study in Gaza Strip, approval number PHRC/HC/699/20 is its meeting on 2020/02/03 Annex (1). Furthermore, ethical approval was obtained from the Human Research Ethics Committee, USM, JEPeM USM Code: (USM/JEPeM/20020122 on 13th January 2022) Annex (2).
Authors contributions
Conceptualization, H.M.A., I.A.N., J.O., O.M.SH., N.A.L., N.S., KH.M.SH., A.J.SH., R.B.M., T.A.D.A., and M.A.A.; Methodology, I.A.N., H.M.A., J.O., O.M.SH.; Validation, H.M.A., O.M.SH., KH.M.SH., and M.A.A.; Data curation, H.M.A., J.O., I.A.N., O.M.SH., and N.S.; Writing—original draft preparation, H.M.A., and O.M.SH.; Writing—review and editing, H.M.A., I.A.N., J.O., O.M.SH., N.A.L., N.S., KH.M.SH., A.J.SH., R.B.M., T.A.D.A., and M.A.A. All authors revised the manuscript and approved the final version to be submitted. This work is part of H.M.A. PhD dissertation research in Universiti Sains Malaysia.
Disclosure statement
No potential conflict of interest was reported by the author(s).
References
- 1.World Health Organization. Breast cancer. 2021. Available from: https://www.who.int/news-room/fact-sheets/detail/breast-cancer
- 2.World Health Organization . Breast-cancer-now-most-common-form-of-cancer-who-taking-action. 2021. Available from: https://www.who.int/news/item/03-02-2021-breast-cancer-now-most-common-form-of-cancer-who-taking-action
- 3.Barzaman K, Karami J, Zarei Z, et al. . Breast cancer: biology, biomarkers, and treatments. Int Immunopharmacol. 2020;84:1. [DOI] [PubMed] [Google Scholar]
- 4.Li Y, Li S, Meng X, et al. . Dietary natural products for prevention and treatment of breast cancer. Nutrients. 2017;9(7):728. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Mourouti N, Kontogianni MD, Papavagelis C, et al. . Diet and breast cancer: a systematic review. Int J Food Sci Nutr. 2015;66(1):1–9. [DOI] [PubMed] [Google Scholar]
- 6.Nagini S. Breast cancer: current molecular therapeutic targets and new players. Anticancer Agents Med Chem. 2017;17(2):152–163. [DOI] [PubMed] [Google Scholar]
- 7.Godinho-Mota JCM, Gonçalves LV, Mota JF, et al. . Sedentary behavior and alcohol consumption increase breast cancer risk regardless of menopausal status: a case-control study. Nutrients. 2019;11(8):1871. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Sun Q, Xie W, Wang Y, et al. . Alcohol consumption by beverage type and risk of breast cancer: a dose-response meta-analysis of prospective cohort studies. Alcohol Alcohol. 2020;55(3):246–253. [DOI] [PubMed] [Google Scholar]
- 9.Fraser GE, Jaceldo-Siegl K, Orlich M, et al. . Dairy, soy, and risk of breast cancer: those confounded milks. Int J Epidemiol. 2020;49(5):1526–1537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Turati F, Carioli G, Bravi F, et al. . Mediterranean diet and breast cancer risk. Nutrients. 2018;10(3):326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.He Y, Chen P, Zhou F, et al. . The relationship between dairy products intake and breast cancer incidence: a meta-analysis of observational studies. BMC cancer. 2021;21(1):1109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Chen S, Chen Y, Ma S, et al. . Dietary fibre intake and risk of breast cancer: a systematic review and meta-analysis of epidemiological studies. Oncotarget. 2016;7(49):80980–80989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Varinska L, Gal P, Mojzisova G, et al. . Soy and breast cancer: focus on angiogenesis. Int J Mol Sci. 2015;16(5):11728–11749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Zang J, Shen M, Du S, et al. . The association between dairy intake and breast cancer in Western and Asian populations: a systematic review and meta-analysis. J Breast Cancer. 2015;18(4):313–322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Aguilera-Buenosvinos I, Fernandez-Lazaro CI, Romanos-Nanclares A, et al. . Dairy consumption and incidence of breast cancer in the ‘seguimiento universidad de navarra’ (SUN) project. Nutrients. 2021;13(2):687. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Shin W-K, Lee H-W, Shin A, et al. . Milk consumption decreases risk for breast cancer in korean women under 50 years of age: results from the health examinees study. Nutrients. 2019;12(1):32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Maliou D, Belmadi D, Saadi W, et al. . Effect of dairy products intake on breast cancer risk: a case-control study in Algeria. Nutr Clin Metab. 2018;32(3):187–194. [Google Scholar]
- 18.Farvid MS, Eliassen AH, Cho E, et al. . Dairy consumption in adolescence and early adulthood and risk of breast cancer. Cancer Epidemiol Biomarkers Prev. 2018;27(5):575–584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Marcondes LH, Franco OH, Ruiter R, et al. . Animal foods and postmenopausal breast cancer risk: a prospective cohort study. Br J Nutr. 2019;122(5):583–591. [DOI] [PubMed] [Google Scholar]
- 20.McCann SE, Hays J, Baumgart CW, et al. . Usual consumption of specific dairy foods is associated with breast cancer in the roswell park cancer institute data bank and BioRepository. Curr Dev Nutr. 2017;1(3):e000422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Plagens-Rotman K, Piskorz-Szymendera M, Chmaj-Wierzychowska K, et al. . Breast cancer–analysis of the selected risk factors. Eur J Gynaecol Oncol. 2017;38(3):425–430. [PubMed] [Google Scholar]
- 22.Kojima R, Okada E, Ukawa S, et al. . Dietary patterns and breast cancer risk in a prospective Japanese study. Breast Cancer. 2017;24(1):152–160. [DOI] [PubMed] [Google Scholar]
- 23.Ahmadnia Z, Joukar F, Hasavari F, et al. . Dietary patterns and risk of breast cancer in women in Guilan province, Iran. Asian Pac J Cancer Prev. 2016;17(4):2035–2040. [DOI] [PubMed] [Google Scholar]
- 24.Mobarakeh ZS, Mirzaei K, Hatmi N, et al. . Dietary habits contributing to breast cancer risk among Iranian women. Asian Pac J Cancer Prev. 2014;15(21):9543–9547. [DOI] [PubMed] [Google Scholar]
- 25.Bahadoran Z, Karimi Z, Houshiar-Rad A, et al. . Is dairy intake associated to breast cancer? A case control study of Iranian women. Nutr Cancer. 2013;65(8):1164–1170. [DOI] [PubMed] [Google Scholar]
- 26.García‐Arenzana N, Navarrete‐Muñoz EM, Lope V, et al. . Calorie intake, olive oil consumption and mammographic density among Spanish women. Int J Cancer. 2014;134(8):1916–1925. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Genkinger JM, Makambi KH, Palmer JR, et al. . Consumption of dairy and meat in relation to breast cancer risk in the black women’s health study. Cancer Causes Control. 2013;24(4):675–684. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Zhang C-X, Ho SC, Fu J-H, et al. . Dairy products, calcium intake, and breast cancer risk: a case-control study in China. Nutrition and Cancer. 2011;63(1):12–20. [DOI] [PubMed] [Google Scholar]
- 29.Linos E, Willett WC, Cho E, et al. . Adolescent diet in relation to breast cancer risk among premenopausal women. Cancer Epidemiol Biomarkers Prev. 2010;19(3):689–696. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Pala V, Krogh V, Berrino F, et al. . Meat, eggs, dairy products, and risk of breast cancer in the European prospective investigation into cancer and nutrition (EPIC) cohort. Am J Clin Nutr. 2009;90(3):602–612. [DOI] [PubMed] [Google Scholar]
- 31.Bessaoud F, Daurès JP, Gerber M.. Dietary factors and breast cancer risk: a case control study among a population in Southern France. Nutr Cancer. 2008;60(2):177–187. [DOI] [PubMed] [Google Scholar]
- 32.Fleet JC, Desmet M, Johnson R, et al. . Vitamin D and cancer: a review of molecular mechanisms. Biochem J. 2012;441(1):61–76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Cui Y, Rohan TE.. Vitamin D, calcium, and breast cancer risk: a review. Cancer Epidemiol Biomarkers Prev. 2006;15(8):1427–1437. [DOI] [PubMed] [Google Scholar]
- 34.Colston KW, Hansen CM.. Mechanisms implicated in the growth regulatory effects of vitamin D in breast cancer. Endocr Relat Cancer. 2002;9(1):45–59. [DOI] [PubMed] [Google Scholar]
- 35.Narvaez CJ, Zinser G, Welsh J.. Functions of 1α, 25-dihydroxyvitamin D3 in mammary gland: from normal development to breast cancer. Steroids. 2001;66(3–5):301–308. [DOI] [PubMed] [Google Scholar]
- 36.Hadadi E, Taylor W, Li XM, et al. . Chronic circadian disruption modulates breast cancer stemness and immune microenvironment to drive metastasis in mice. Nat Commun. 2020;11(1):3193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Westin JB. Carcinogens in Israeli milk: a study in regulatory failure. Int J Health Serv. 1993;23(3):497–517. [DOI] [PubMed] [Google Scholar]
- 38.Moysich KB, Ambrosone CB, Mendola P, et al. . Exposures associated with serum organochlorine levels among postmenopausal women from Western New York state. Am J Ind Med. 2002;41(2):102–110. [DOI] [PubMed] [Google Scholar]
- 39.Laden F, Neas LM, Spiegelman D, et al. . Predictors of plasma concentrations of DDE and PCBs in a group of US women. Environ Health Perspect. 1999;107(1):75–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.MacIntosh DL, Spengler JD, Ozkaynak H, et al. . Dietary exposures to selected metals and pesticides. Environ Health Perspect. 1996;104(2):202–209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Outwater J, Nicholson A, Barnard N.. Dairy products and breast cancer: the IGF-I, estrogen, and bGH hypothesis. Med Hypotheses. 1997;48(6):453–461. [DOI] [PubMed] [Google Scholar]
- 42.Yu H, Rohan T.. Role of the insulin-like growth factor family in cancer development and progression. J Natl Cancer Inst. 2000;92(18):1472–1489. [DOI] [PubMed] [Google Scholar]
- 43.Prosser CG, Fleet IR, Corps AN.. Increased secretion of insulin-like growth factor I into milk of cows treated with recombinantly derived bovine growth hormone. J Dairy Res. 1989;56(1):17–26. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.