Abstract
Blunt cardiac injury is caused by large deceleration forces seen in motor vehicle accidents and can range from non–life-threatening arrhythmias to potentially fatal cardiac conditions such as valve disruption. A 28-year-old man presented following a motor vehicle accident involving direct blunt-force chest trauma. He developed papillary muscle rupture resulting in mitral valve dysfunction. Diagnosis was delayed due to concomitant chest pathology. Diagnosis of cardiac valvular injuries may be difficult due to concomitant injuries in a trauma patient. Though rare, papillary muscle rupture should be included in the differential diagnosis following blunt thoracic trauma, particularly involving persistent hypoxemia.
Keywords: Blunt cardiac injury, mitral valve injury, papillary muscle rupture
Blunt cardiac injury (BCI) covers a diverse set of presentations including new onset arrhythmias, septal and valvular injuries, coronary artery injuries, myocardial infarction, and myocardial rupture. BCIs often have a delayed diagnosis and can be seen with sternal fractures and concomitant chest wall injuries. Herein we present a rare case of papillary muscle rupture secondary to BCI.
CASE DESCRIPTION
A 28-year-old man presented as a restrained driver after a high-speed motor vehicle collision with airbag deployment and prolonged extrication time. On initial exam, his blood pressure was 87/42 mm Hg; heart rate, 95 beats/min; oxygen saturation, 93% on room air; and Glasgow coma score, 13. He had a right hip deformity. He was transfused 3 units of blood and 1 L of saline. A Focused Assessment with Sonography in Trauma exam was negative. Computed tomography (CT) imaging of the head, neck, chest, abdomen, and pelvis confirmed an anterior longitudinal tear at C2, bilateral pulmonary contusions, left second, third, and eighth rib fractures, left apical pneumothorax, splenic contusion, and right posterior hip dislocation with an acetabular fracture (Figure 1). Reduction of the right hip fracture dislocation was performed under conscious sedation.
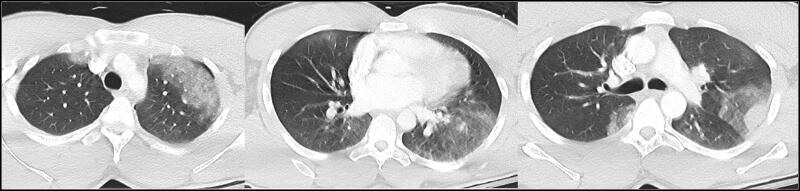
Figure 1.
Multiple cuts from the initial chest CT obtained on presentation showing diffuse bilateral pulmonary contusions.
The patient subsequently became hypoxic, requiring endotracheal intubation, and developed acute respiratory distress syndrome. Bedside bronchoscopy and CT angiography failed to identify a cause of ongoing hypoxemia. He was transitioned to airway pressure release ventilation mode, nitric oxide was initiated, and he was placed in prone position in an attempt to improve oxygenation. Initially his hypoxemia improved, but that was followed by intermittent episodes of desaturation and development of frothy, pink sputum. Transthoracic echocardiogram (TTE) visualized a prolapse of the anterior mitral valve leaflet, a dilated left atrium, and severe mitral regurgitation with an ejection fraction of 65%. A transesophageal echocardiogram revealed papillary muscle rupture of the mitral valve (Figure 2).
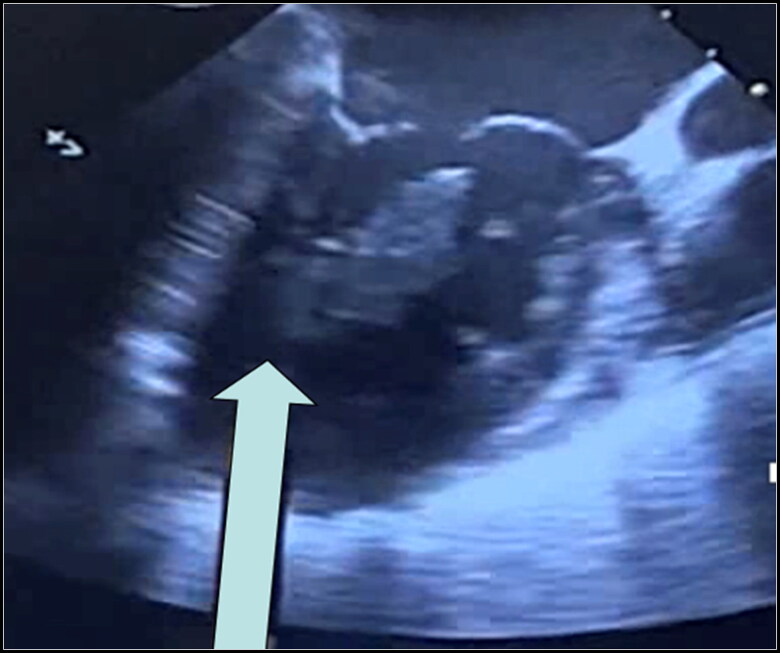
Figure 2.
TEE with white arrow denoting rupture of the papillary muscle off the ventricular wall.
The patient was subsequently transferred to a facility where extracorporeal membrane oxygenation (ECMO) was initiated. After stabilization, he underwent mitral valve replacement with a 31 mm mechanical bileaflet prosthesis. ECMO was weaned over the next week with decannulation on postoperative day 7 and extubation shortly after. He was discharged to an acute rehabilitation center on postoperative day 26. TTE performed 2 weeks postoperatively demonstrated a left ventricular ejection fraction of 60% with a normally functioning mitral valve prosthesis.
DISCUSSION
BCIs can have multiple manifestations and are often associated with other injuries in the chest and remainder of the body.1 The true incidence of BCI is unknown, with ranges varying from 8% to 76% due to lack of standardization of diagnostic criteria.2 Additionally, many patients are relatively asymptomatic and have missed injuries or die in the prehospital setting.
Valvular injury is a rare form of BCI. The most frequently injured valve is the aortic valve, followed by the mitral and tricuspid valves.3 Papillary muscle rupture, chordae tendineae rupture, and valve leaflet lacerations can result in mitral valve injury, resulting in hemodynamic instability.4 Valvular prolapse, rupture, and severe regurgitation is caused by injury secondary to the compressive forces of the thoracic and abdominal cavity. It has been shown that intraventricular pressures exceeding 320 mm Hg cause increased susceptibility to cardiac valve rupture.5 Mitral valve injury occurs when blunt trauma occurs during early systole, when the mitral valve closes and there is isovolumetric contraction.5 It is possible that the presence of preexisting mitral valve prolapse may increase the risk for papillary rupture after blunt thoracic trauma.
Symptoms of BCI may be acute or subacute as cardiac wall stress further exacerbates valvular injury. Patients may present with new-onset arrhythmias, hypotension, and hemodynamic instability.6 There is currently no gold standard for the diagnosis of BCI. Current literature suggests maintaining a high index of suspicion with serial electrocardiogram evaluations and cardiac enzyme measurements.3 Diagnosis of valvular injury can be further investigated by echocardiogram. TTE is a safe and effective diagnostic modality with minimal limitations due to patient habitus, position, or operator technique. Transesophageal echocardiography is considered more sensitive for valvular pathology. More than half of all traumatic mitral valve injuries will require operative intervention as either a repair or valve replacement.7,8
In conclusion, accurate diagnosis and successful treatment of papillary muscle rupture involves a high index of suspicion. Timely diagnosis and prompt clinical intervention allows for an improved prognosis in patients with BCI.
Disclosure statement/Funding
The authors report no funding or conflicts of interest. The patient has given permission for this case to be published.
References
- 1.Legome E, Kadish H.. 2019. Initial evaluation and management of blunt cardiac injury. UpToDate. www.uptodate.com/contents/cardiac-injury-from-blunt-trauma. Updated November 30, 2021. Accessed March 2, 2022.
- 2.Singh S, Heard M, Pester JM, Angus LD.. Blunt cardiac injury. In: Faizi Z, ed. StatPearls. Treasure Island, FL: StatPearls Publishing; October 28, 2022. [PubMed] [Google Scholar]
- 3.Clancy K, Velopulos C, Bilaniuk JW, et al; Eastern Association for the Surgery of Trauma. Screening for blunt cardiac injury: an Eastern Association for the Surgery of Trauma practice management guideline. J Trauma Acute Care Surg. 2012;73(5 Suppl 4):S301–S6. doi: 10.1097/TA.0b013e318270193a. [DOI] [PubMed] [Google Scholar]
- 4.Cordovil A, Fischer CH, Rodrigues ACT, et al. Papillary muscle rupture after blunt chest trauma. J Am Soc Echocardiogr. 2006;19(4):469.e1-3. doi: 10.1016/j.echo.2005.12.005. [DOI] [PubMed] [Google Scholar]
- 5.McDonald ML, Orszulak TA, Bannon MP, Zietlow SP.. Mitral valve injury after blunt chest trauma. Ann Thorac Surg. 1996;61(3):1024–1029. doi: 10.1016/0003-4975(95)01034-3. [DOI] [PubMed] [Google Scholar]
- 6.Kan CD, Yang YJ.. Traumatic aortic and mitral valve injury following blunt chest injury with a variable clinical course. Heart. 2005;3(1):198–200. doi: 10.1016/S1569-9293(03)00267-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Pasquier M, Sierro C, Yersin B, Delay D, Carron PN.. Traumatic mitral valve injury after blunt chest trauma: a case report and review of the literature. J Trauma. 2010;68(1):243–246. doi: 10.1097/TA.0b013e3181bb881e. [DOI] [PubMed] [Google Scholar]
- 8.Fedak P, McCarthy PM, Bonow RO.. Evolving concepts and technologies in mitral valve repair. Circulation. 2008;117(7):963–974. doi: 10.1161/CIRCULATIONAHA.107.702035. [DOI] [PubMed] [Google Scholar]