Abstract
Evidence shows that treatment by gynecologic oncologists (GOs) increases overall survival among women with ovarian cancer. However, specific strategies for institutions and community-based public health programs to promote treatment by GOs are lacking. To address this, we conducted a literature review to identify evidence-based and promising system- and environmental-change strategies for increasing treatment by GOs, in effort to ensure that all women with ovarian cancer receive the standard of care. We searched for English-language literature published from 2008 to 2018. We used PubMed, PubMed Central, OVID, and EBSCO for peer-reviewed literature and Google and Google Scholar for gray literature related to increasing receipt of care by GOs among ovarian cancer patients. Numerous suggested and proposed strategies that have potential to increase treatment by GOs were discussed in several articles. We grouped these approaches into five strategic categories: increasing knowledge/awareness of role and importance of GOs, improving models of care, improving payment structures, improving/increasing insurance coverage for GO care, and expanding or enhancing the GO workforce. We identified several strategies with the potential for increasing GO care among ovarian cancer patients, although currently there is little evidence regarding their effectiveness across US populations. Public health programs and entities that measure delivery of quality health care may pilot the strategies in their populations. Certain strategies may work better in certain environments and a combination of strategies may be necessary for any one entity to increase GO ovarian cancer care. Findings, lessons learned, and recommendations from implementation projects would inform community and public health practice.
Keywords: ovarian cancer, gynecologic oncologist, referral
Introduction
Ovarian cancer is the fifth leading cause of cancer death among women in the United States1 and the second most common type of female reproductive cancer. More women die each year from ovarian cancer than from cervical and all other types of uterine cancer (including endometrial) combined.2 Women’s lifetime risk for developing ovarian cancer is 1 in 78,3 and women with a family history of ovarian, breast, or colon cancer may be at increased risk.4 Because ovarian cancer often presents with nonspecific symptoms such as frequent urination and back pain, most patients are not diagnosed until they have reached an advanced stage.5,6 No early detection or screening methods have been found to reduce overall mortality in women with ovarian cancer.7 The US Preventive Services Task Force recommends against annual screening, because available evidence indicates screening does not reduce mortality and can lead to unnecessary surgical interventions in women without high risk of ovarian cancer.8,9
In contrast, treatment for ovarian cancer is well defined, and studies have shown that adherence to standard of care protocols lead to improved survival among patients.10 The evidence-based standard of care is defined as receipt of surgery, chemotherapy, and testing for germline mutations.10 There are some known disparities in ovarian cancer treatment. Factors such as older age, black race, the presence of multi-morbidity, low socioeconomic status, and rural location have been associated with not receiving standard care, which leads to a lower survival rate.11–15 Significant predictors of whether women receive standard care include (1) treatment by a gynecologic oncologist (GO) and (2) treatment in a high-volume or low-volume hospital or cancer center.10 As a result, several organizations, including the Centers for Disease Control and Prevention (CDC), the Society for Gynecologic Oncologists (SGO), the American College of Obstetricians and Gynecologists (ACOG), and the National Comprehensive Cancer Network (NCCN), have consistently recommended that treatment for ovarian cancer be provided by a GO.10,16
In 2016, in an effort to improve ovarian cancer research and care, CDC commissioned the National Academies of Sciences, Engineering, and Medicine (NASEM, formerly the Institute of Medicine [IOM]) to develop a comprehensive report10 on ovarian cancer and provided specific recommendations for diagnosis, treatment, and supportive care along the survivorship trajectory for ovarian cancer. The report identified receipt of care from a GO as “a key message that is ready for dissemination” and recommended that newer pathways of dissemination and implementation (e.g., social media and telemedicine) be evaluated to determine effectiveness.10
To assist with increasing dissemination and implementation of this key message, we conducted a review of the literature to identify evidence-based and promising system- and environmental-change practices that facilities or community-based public health programs across the country might employ to increase ovarian cancer care receipt from a GO.
Materials and Methods
We conducted a review of peer-reviewed and gray literature to identify promising practices and evidence-based strategies for increasing receipt of care from a GO by women with ovarian cancer. As a secondary focus to this review, we also searched for barriers and facilitators to care by a gynecologist oncologist. We searched PubMed, PubMed Central, OVID, EBSCO, Google, and Google Scholar using three search strings: (1) “ovarian cancer” AND “gynecologic oncologist”; (2) “gynecologic oncologist” AND “barrier”; and (3) “gynecologic oncologist” AND “access.” The searches were limited to sources published in English within the last 10 years (2008–2018). We included all studies published in English, including those based on populations outside the United States. Because this literature search is not considered research, it was exempt from review by CDC’s Internal Review Board.
Results from the peer-reviewed and gray literature searches were reviewed for eligibility in a multiple-step process (Fig. 1). One reviewer (D.N.) sequentially screened the titles, abstracts, and articles for information regarding approaches or strategies to increase receipt of ovarian cancer care from a GO, as well as information regarding facilitators or barriers to receipt of ovarian cancer care from a GO. The same reviewer obtained the full text for the 64 peer-reviewed articles and 26 gray literature articles. Relevant data from the 48 eligible resources—35 peer-reviewed articles and 13 gray literature articles—were extracted into Microsoft Word tables. Two reviewers (D.N. and J.L.M.) were responsible for extracting data from the eligible published literature and the eligible gray literature. For each set, the reviewers coded eight of the same peer-reviewed articles and gray literature articles, and then discussed their coding and discrepancies to establish consensus. The remaining articles were independently coded by one of the reviewers.
FIG. 1.
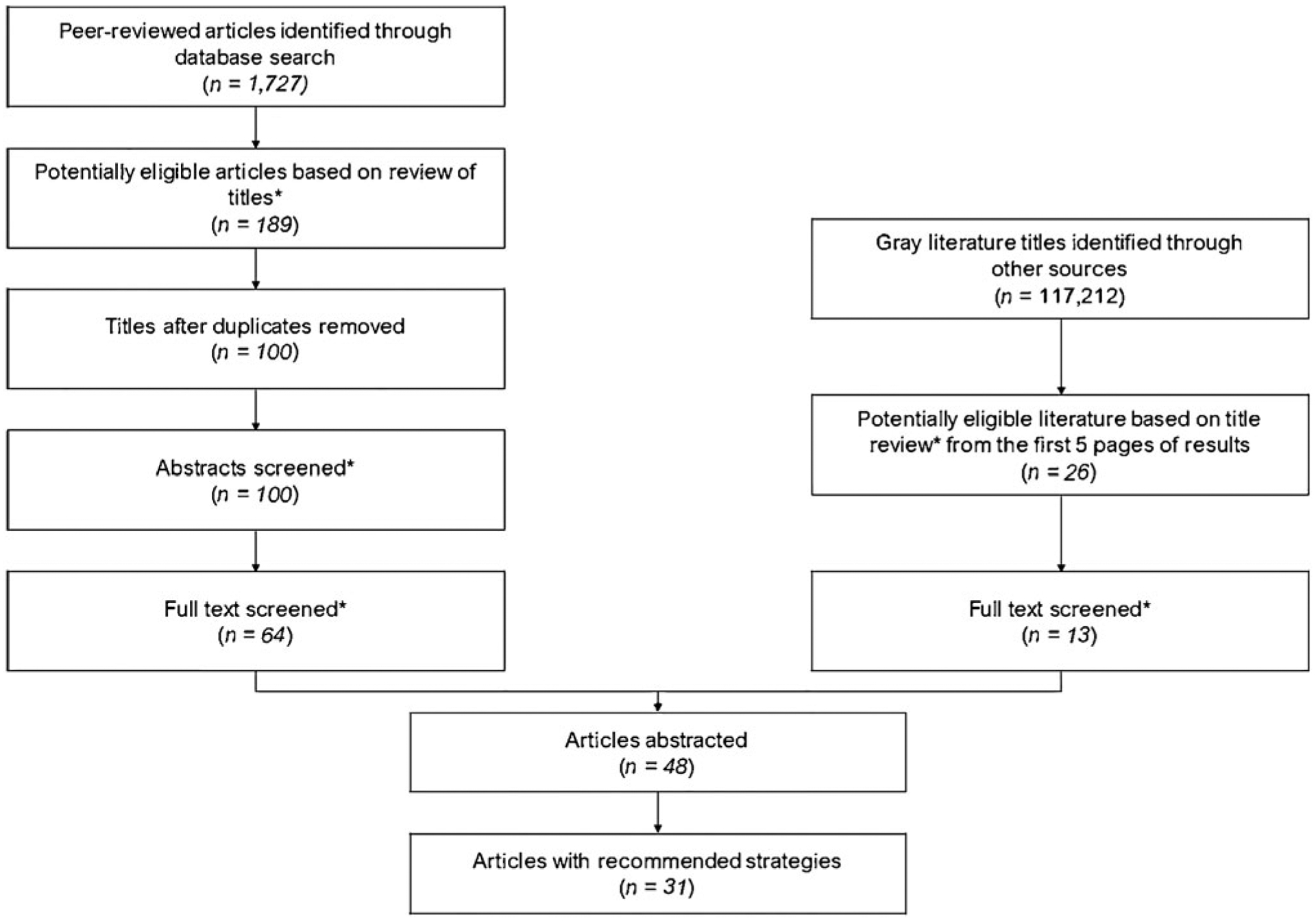
Multistep review process for peer-reviewed and gray literature. *At each stage, the title, abstract, or article was assessed for evidence of the following: (1) published in English. (2) Published within the past 10 years (2008–2018). (3) Included information regarding facilitators or barriers to receipt of ovarian cancer care from a GO. (4) Included information regarding recommended strategies to increase receipt of ovarian cancer care from a GO. Articles that did not appear to meet these criteria or include the requisite information were excluded. GO, gynecologic oncologist.
Following abstraction of the peer-reviewed and gray literature, we grouped the approaches from 31 articles into five strategic categories. It is important to note that a cursory review of these articles indicated a lack of evidence for implementation of promising practices. As a result, we expanded our review to include approaches suggested by the authors. In many cases, the approaches identified were mentioned or proposed within the Discussion section of published articles and pertained to challenges the authors identified through their study. We present these as proposed approaches that may have the potential to increase receipt of care by a GO among women with ovarian cancer.
Results
Of the 48 eligible peer-reviewed and gray literature articles reviewed, 31 mentioned or proposed approaches related to one or more strategies to increase receipt of care by GOs. The remaining abstracted articles did not propose approaches, but were used to identify facilitators and barriers regarding the availability and involvement of GOs. The proposed approaches or interventions identified aligned with the following five strategies:
Increasing knowledge/awareness of the role and importance of GOs (n = 12),
Improving models of care (n = 24),
Improving payment structures (n = 1),
Improving/increasing insurance coverage for GO care (n = 2), and
Expanding or enhancing the GO workforce (n = 7).
Increasing knowledge and awareness of GOs
Twelve studies proposed approaches aimed at increasing knowledge and awareness of health care providers, patients, and the public, as well as approaches for partnership development and enrichment related to gynecologic oncology care. Table 1 describes the approaches identified for this strategy. One approach included provider education. Several sources proposed educating health care providers regarding the role and importance of GOs to increase the likelihood that women with ovarian cancer are referred to a GO for treatment.10,17–24 Furthermore, these studies noted it may be useful to increase awareness and knowledge among specific subspecialties of health care providers. For example, one study noted that most gynecologists in community hospitals were reluctant to provide routine referrals for women with ovarian cysts to oncology centers because they thought it would limit their range of clinical activities.25 Another study found that fewer than 50% of primary care physicians refer women with suspected ovarian cancer directly to GOs. Among primary care physicians, those in family practice were significantly less likely than internal medicine counterparts to refer women to GOs.23,26 Educating providers on the benefits of treatment and care by a GO can increase referrals to GOs, thereby increasing the number of ovarian cancer patients who receive the evidence-based standard of care.
Table 1.
Proposed Approaches to Increase Knowledge and Awareness Regarding the Role and Importance of Gynecologic Oncologists
| Author (Year) | Focus of article | Approach | Approach description or focus |
|---|---|---|---|
| Collins et al. (2014)18 | Factors associated with GO use/non-use; facilitators/barriers to GO access; strategies to increase GO care | Provider education | Enhance educational efforts to improve awareness of racial and ethnic disparities as it relates to receipt of care by GO |
| Duska, (2018)17 | Geographic availability of GOs; geographic use of GOs; factors associated with GO use/non-use; facilitators/barriers to GO access; strategies to increase GO care | Provider education | Increase perceived significance of having a GO treat women diagnosed with ovarian cancer |
| Patient education | Educate patients regarding the significance of GO | ||
| Goff et al. (2011)26 | Factors associated with GO use/non-use | Provider education | Educate specific subspecialties (family practice, internal medicine, and obstetrics/gynecology) of health care providers on importance of referral to GO |
| Gostout et al. (2012)23 | Geographic availability of GOs; strategies to increase GO care | Provider education | Educate medical students and primary care providers about the symptoms and benefits of referral to a GO if ovarian cancer is suspected |
| Patient education | Raise awareness of symptoms among women | ||
| Hess et al. (2012)21 | Factors associated with GO use/non-use; strategies to increase GO care | Provider education | Educate primary care providers to recognize potential symptoms of ovarian cancer and make appropriate referrals to minimize the time and resources used to reach an accurate diagnosis |
| National Academies of Sciences, Engineering, and Medicine (2016)10 | Factors associated with GO use/non-use; facilitators/barriers to GO access; strategies to increase GO care | Provider education | Educate and train the health care workforce to ensure consistent implementation of current standards of care for women with ovarian cancer that are linked to quality outcome metrics |
| Peters et al. (2014)25 | Facilitators/barriers to GO access; strategies to increase GO care | Provider education | Educate specific subspecialties (gynecology) of health care providers on importance of referral to GO |
| Rim, (2016)27 | Geographic availability of GOs; geographic use of GOs; factors associated with GO use/non-use; facilitators/barriers to GO access; strategies to increase GO care | Patient education | Educate patients, especially the elderly, about better survival outcomes, guideline-adherent treatment, and high-quality surgical care from GO subspecialty |
| Stewart et al. (2016)19 | Factors associated with GO use/non-use; facilitators/barriers to GO access; strategies to increase GO care | Provider education | Increase primary care physicians’ knowledge and use of OVA1 test to improve appropriate referral rates to GOs |
| Patient education | Educate patients about the importance of receiving ovarian cancer care from GO | ||
| General public education | Educate the general public about the evidence-based recommendation to receive care for ovarian cancer from GO | ||
| Stewart et al. (2013)20 | Strategies to increase GO care | Provider education | Educate providers to help ensure patients receive treatment and clinical care from GOs |
| General public education | Educate the public by providing direct consumer information about the importance of receiving ovarian cancer care from GO | ||
| Partner enrichment and development | Partner with local, state, and national patient advocacy groups to help ensure patients receive treatment and clinical care from GOs | ||
| Stewart et al. (2011)22 | Geographic availability of GOs; factors associated with GO use/non-use; strategies to increase GO care | Provider education | Increase provider knowledge about the importance of referral to GO through the “Inside Knowledge: Get the Facts about Gynecologic Cancer” campaign |
| General public education | Increase public knowledge about the importance of referral to GO through the “Inside Knowledge: Get the Facts about Gynecologic Cancer” campaign | ||
| Urban et al. (2016)24 | Geographic availability of GOs; facilitators/barriers to GO access; strategies to increase GO care | Provider education | GOs should reach out to, collaborate with, and educate colleagues in other medical specialties to optimize the care of patients with ovarian cancer |
GO, gynecologist oncologist; NASEM, National Academies of Sciences, Engineering, and Medicine.
Another approach within this strategy included patient education. Several articles proposed educating patients regarding the role and importance of GOs to increase the likelihood that women with ovarian cancer will inquire about and seek referrals to GOs for treatment.17,19,22,27 One article specifically proposed educating patients on the symptoms of ovarian cancer.23 General public education was another approach, and some sources mentioned educating the general public about the importance of receiving ovarian cancer care from a GO to increase the likelihood that women with ovarian cancer or their caregivers will ask to be referred to a GO for treatment.19,20 Another proposed approach involved increasing knowledge and awareness through partnership development and enrichment, especially with local, state, and national patient advocacy groups. These key entities can provide education to providers, patients, and the general public regarding optimal treatment for gynecologic cancers.20
Improving models of care
Table 2 lists the 25 articles that mentioned or proposed a range of strategies related to improving models of care. One article proposed the centralization/regionalization of care. In this approach, women with ovarian cancer are referred by less-specialized hospitals within a network, region, or defined catchment area to centers with higher patient volumes and interdisciplinary collaboration for their care. Under this model of care, women are referred to specialized units with interdisciplinary collaboration among a team of multiple specialized physicians.17,28–39 One study pilot tested a model of centralization and found that the outcomes of patients seen in the centralized expert centers exceeded the national and international means for quality of treatment.35 Another study found that regional collaboration resulted in GOs attending more surgeries and improved surgical outcomes.38
Table 2.
Proposed Approaches to Improve Models of Care to Increase Gynecologic Care
| Author (Year) | Focus of article | Approach | Approach description or focus |
|---|---|---|---|
| Boyd et al. (2011)29 | Geographic availability of GOs; factors associated with GO use/non-use; strategies to increase GO care | Centralization/regionalization of carea | Centralize care so patients attending municipal hospitals with fewer specialty services can receive quality care from GO at high-volume specialty health center. |
| Sharing of physicians | Sharing of physicians in public and private settings through a shared physician practice model. | ||
| Use of referral systems | Develop and use referral systems to ensure patients with ovarian cancer have the benefits of high-volume surgeons and centers with appropriate ancillary services. | ||
| Bristow et al. (2015)37 | Geographic availability of GOs; factors associated with GO use/non-use; strategies to increase GO care | Centralization/regionalization of care | Implement a national approach of centralization of care for women with ovarian cancer to improve population-based clinical outcomes. The transplant model used in the United States provides a template that could be used to regionalize ovarian cancer care. |
| Canadian Partnership Against Cancer (2018)39 | Strategies to increase GO care | Centralization/regionalization of care | Regionalize care to ensure access to high-volume cancer centers to reduce health disparities and ensure timely access to care. |
| Multidisciplinary care | All women with gynecologic malignancies should have access to multidisciplinary teams and should be operated on and/or have treatment directed by a GO. | ||
| Telemedicine | Ensure access to telehealth to mitigate the risks of geographic isolation and provide care closer to home. | ||
| Collins et al. (2014)18 | Factors associated with GO use/non-use; facilitators/barriers to GO access; strategies to increase GO care | Use of referral systems | Use of electronic health records to collect data that gives a better picture of care received and identify patient barriers and systemic factors to receiving quality gynecologic cancer care. |
| Cowan et al. (2016)33 | Geographic availability of GOs; geographic use of GOs; factors associated with GO use/non-use; facilitators/barriers to GO access; strategies to increase GO care | Centralization/regionalization of carea | Centralize GO services. Centers and providers with less experience should reach out to more specialized providers/hospitals to ensure patients are receiving appropriate care. |
| Duska (2018)17 | Geographic availability of GOs; geographic use of GOs; factors associated with GO use/non-use; facilitators/barriers to GO access; strategies to increase GO care | Centralization/regionalization of care | Coordination of local and centralized services, with the most complex components of care provided in tertiary settings or centers of excellence. |
| Guest operations | Send GO faculty to outreach hospitals to conduct surgery, inpatient consults, and outpatient clinical services. | ||
| Patient navigation | Engage a patient navigator to help patients navigate complex cancer systems. | ||
| Telemedicine | Virtual tumor board with virtual teleconferencing and digital transfer of radiology and pathology images to allow for in-depth review of cases and discussion of treatment recommendations by multidisciplinary group of experts. | ||
| Fung-Kee et al. (2015)34 | Strategies to increase GO care | Centralization/regionalization of care | Centralize care to ensure multidisciplinary care and surgery by GO to improve survival outcomes for ovarian care patients. |
| Horvath et al. (2010)42 | Strategies to increase GO care | Multidisciplinary carea | Use multidisciplinary care in which physicians from multiple specialties attend to the same patient population. There are many advantages to the model, including reduced time to treatment, coordinated treatment plans, increased patient and physician satisfaction, and increased enrollment into clinical trials. |
| Keyver-Paik et al. (2016)35 | Strategies to increase GO care | Centralization/regionalization of care | Centralize ovarian cancer care to increase the volume of patients being treated in hospitals with adequate infrastructure. |
| Multidisciplinary carea | Multidisciplinary practice and centralization of care resulted in improved quality of care received in patients participating in the program. | ||
| Minis et al. (2015)28 | Facilitators/barriers to GO access; strategies to increase GO care | Centralization/regionalization of care | Centralize care in centers with higher patient volumes and interdisciplinary collaboration and utilize referrals from less-specialized hospitals within a network, region, or defined catchment area to ensure comprehensive care for women with gynecologic cancer. |
| National Academies of Sciences, Engineering, and Medicine (2016)10 | Strategies to increase receipt of care from GO | Patient navigation | Explore patient navigation systems to allow women to be more engaged in their own care. |
| Telemedicine | Telemedicine can help remote patients become more involved in their care. Teleoncology can make oncologists more capable of helping care for patients in areas not located near high-volume centers. | ||
| Peters et al. (2014)25 | Facilitators/barriers to GO access; strategies to increase GO care | Guest operationsa | GOs from oncology centers should travel to community hospitals to perform cancer surgery there, together with local gynecologists. |
| Ramzan et al. (2018)43 | Geographic availability of GOs; factors associated with GO use/non-use; facilitators/barriers to GO access; strategies to increase GO care | Telemedicine | Use of tele-oncology to provide cancer care remotely through virtual tumor boards, video-based intraoperative consults, and remote supervision of chemotherapy administration. |
| Ricci et al. (2017)31 | Geographic availability of GOs; factors associated with GO use/non-use; facilitators/barriers to GO access; strategies to increase GO care | Centralization/regionalization of care | Centralize gynecologic oncology care at high-volume centers with the infrastructure, expertise, and ancillary support services necessary for excellent patient care. |
| Rim (2016)27 | Geographic availability of GOs; geographic use of GOs; factors associated with GO use/non-use; facilitators/barriers to GO access; strategies to increase GO care | Telemedicine | A virtual method of interfacing points of the health care process, telemedicine may be used for both physician-to-physician video-consulting as well as provider-patient post-operative follow-up. |
| Patient navigation | Patient navigation is a proven method of improving patient awareness and the patient’s experience with the clinical system. The goal of patient navigation is in improving access to treatment services and ensuring receipt of timely, quality cancer care. | ||
| Shalowitz et al. (2015)44 | Geographic availability of GOs; geographic use of GOs; facilitators/barriers to GO access; strategies to increase GO care | Telemedicine | Provide remote cancer care to improve access to care in rural or underserved areas through virtual treatment conferences, remote ordering and supervision of chemotherapy, virtual tumor boards, telepathology, communication with local providers for surgeries at remote sites, and inpatient rounding through videoconference. |
| Sinno et al. (2017)30 | Factors associated with GO use/non-use; facilitators/barriers to GO access; strategies to increase GO care | Centralization/regionalization of care | Utilize a centralized care model for women with advanced ovarian cancer to ensure a larger proportion of women receive care at high-volume ovarian cancer centers. |
| Use of referral systems | Develop and use referral systems to ensure patients are getting to high-volume, centralized ovarian cancer centers. | ||
| Society of Gynecologic Oncology (2013)41 | Strategies to increase receipt of care from GOs | Use of a patient-centered medical home model | Structured ovarian cancer care like a patient-centered medical home with a single provider with training in gynecologic cancer coordinating multidisciplinary care. |
| Multidisciplinary care | Ovarian cancer treatment should include multidisciplinary team of specialists, including GOs, radiation oncologists, medical oncologists, primary care physicians, advanced practice providers, oncology nurses, oncology pharmacists, genetic counselors, physical therapists, and additional supportive care providers. | ||
| Use of referral systems | Improve electronic health record systems to facilitate access and coordination of care. | ||
| Telemedicine | Use of telehealth systems to facilitate and coordinate care with patients and providers. | ||
| Developing centers of excellence in gynecologic oncology | Provide incentives for hospitals to become centers of excellence in gynecologic oncology. | ||
| Stewart et al. (2011)22 | Geographic availability of GOs; factors associated with GO use/non-use; strategies to increase GO care | Patient navigation | Cancer planners can assist with alleviating disparities through navigation of ovarian cancer patients to GOs. |
| Stewart et al. (2014)32 | Geographic availability of GOs; facilitators/barriers to GO access; strategies to increase GO care | Centralization/regionalization of care | Reorganization of gynecologic cancer care to connect major comprehensive cancer centers that have GOs with smaller satellite hospitals without GOs to facilitate multidisciplinary care for patients in the smaller centers. |
| Stewart et al. (2016)19 | Factors associated with GO use/non-use; facilitators/barriers to GO access; strategies to increase GO care | Patient navigation | Assistance of patients with communication and transportation needs following a diagnosis could help increase the numbers of women receiving care from GOs following a diagnosis. |
| Telemedicine | Telemedicine, which would allow GOs to consult on patient cases through phone and/or videoconferencing, has been suggested to alleviate geographic disparities. | ||
| University of Colorado (2019)40 | Strategies to increase GO care | Guest operations | Create travel systems for GO specialists to be available in rural/shortage areas when needed. |
| van Altena et al. (2013)38 | Strategies to increase GO care | Centralization/regionalization of carea | Studied a regional collaboration in the Netherlands to optimize epithelial ovarian cancer treatment. GOs from the university center conducted surgery in community hospitals when ovarian cancer was considered based on the risk of malignancy index or clinical suspicion. |
| Woo et al. (2012)36 | Geographic availability of GOs; factors associated with GO use/non-use; facilitators/barriers to GO access; strategies to increase GO care | Centralization/regionalization of care | Centralize care to specialized centers to increase survival outcomes among women with ovarian cancer. |
Approach evaluated by authors.
GO, gynecologist oncologist.
A study conducted in the Netherlands suggested the use of guest operations. In this approach, GOs from the oncology centers traveled to community hospitals to perform cancer surgery alongside the local gynecologists.25 Other articles also proposed creating traveling systems for GO cancer specialists to be available in rural/shortage areas when needed.17,40 In addition, sharing physicians in public/private settings (or the shared physician practice model) is where specialists and subspecialists see patients and conduct procedures in both public and private hospitals.29 One study investigated this approach and found a clear benefit to the shared physician practice model; patients who typically use public hospitals were more likely to be considered “urgent” or “emergent” when admitted to a private hospital.29 The use of a patient-centered medical home model is another proposed approach, in which care is coordinated by a single health care provider (a “team captain”) with multidisciplinary training in gynecologic cancer.41 Several resources mentioned the use of multidisciplinary care for ovarian cancer. In this approach, practitioners from multiple specialties create a consolidated ovarian cancer care plan that includes the treatment recommendations of all care team members.35,39,41,42
To ensure patients with ovarian cancer have the benefits of high-volume surgeons and centers with appropriate ancillary services, several articles also mentioned the development and use of referral systems.29,30 In addition, enhancements to electronic health systems can enable the collection of information on patient barriers and systemic factors that may influence the receipt of quality gynecologic cancer care and facilitate the development and use of these referral systems.18,41 Patient navigation, or assisting patients with communication and transportation needs, following a diagnosis, was mentioned as another approach that could help increase the numbers of women receiving care from GOs.10,17,19,22,27 Some sources proposed telemedicine, which allows GOs to consult on patient cases through phone and/or videoconferencing. The authors suggested that this approach would be especially helpful in geographic areas where the number of available GOs is low.10,17,19,27,29,39,41,43,44 Finally, one article proposed encouraging the development of centers of excellence in gynecologic oncology by providing hospitals with incentives for improving models of care.41
Improving payment structures, improving or increasing insurance coverage for GO care, and expanding or enhancing the GO workforce
Table 3 describes the articles that proposed or mentioned approaches aimed at improving payment structures, improving/increasing insurance coverage, and expanding the GO workforce. One article that proposed improving payment structures identified three approaches to address this strategy. The first of these involves implementing reimbursement policies that discourage receipt of ovarian cancer care from nonspecialized health care providers, indicating that providers who are not GO specialists should not treat women with gynecologic cancer.41 The second approach involves implementing reimbursement policies that encourage multidisciplinary care to reward optimization of the care team process. This approach as stated in the article suggests that the team captain should be compensated for coordinating the care required for women with gynecologic cancer. In addition, care by ancillary service providers should be appropriately valued and compensated. Such efforts are likely to decrease the cost of care as a result of better utilization of health care resources, avoidance of unnecessary diagnostic studies, and reduction in emergency room visits and hospitalizations.41
Table 3.
Proposed Approaches to Improve Payment Structures, Improve or Increase Insurance Coverage for Gynecologic Care, and Expand or Enhance the Gynecologic Workforce
| Author (Year) | Focus of article | Approach | Approach description or focus |
|---|---|---|---|
| Approaches to improve payment structures | |||
| Society of Gynecologic Oncology (2013)41 | Strategies to increase GO care | Implement reimbursement policies that discourage receipt of ovarian cancer care from non-specialized health care providers | Reimbursement policies should be changed to discourage providers who do not have specialty training in gynecologic oncology from providing care to women with gynecologic cancer. |
| Implement reimbursement policies that encourage multidisciplinary care | Reimbursement policies should reward optimization of the care team process. The team captain should be compensated for coordinating the care required for women with gynecologic cancer. Care by ancillary service providers should be appropriately valued and compensated. | ||
| Develop and test new physician payment methods | There is no difference in compensation when care is provided by specialists with the best training and most experience in gynecologic cancer in comparison to when that care is provided by those who do not have specialized training in gynecologic cancer. There is also limited reimbursement for coordination of care, adherence to management guidelines, meeting benchmarks on meaningful quality parameters, and achieving good patient satisfaction. New physician payment methods should be developed and tested to ensure that women with gynecologic cancer are provided the highest quality, well-coordinated care. | ||
| Approaches to improve/increase insurance coverage for gynecologic care | |||
| Duska (2018)17 | Geographic availability of GOs; geographic use of GOs; factors associated with GO use/non-use; facilitators/barriers to GO access; strategies to increase GO care | Allow GOs to appeal insurance claim denials | Other subspecialties are allowed to appeal coverage denials. Allowing GOs to appeal coverage denials may help improve insurance coverage for gynecologic care. |
| University of Colorado (2019)40 | Strategies to increase receipt of care from GO | Include coverage for travel expenses for patients who must travel to receive gynecological cancer treatment | Insurance plans could start subsidizing travel costs for gynecological cancer treatment. |
| Approaches to expand or enhance the gynecologic workforce | |||
| Canadian Partnership Against Cancer (2018)39 | Strategies to increase GO care | Expanding fellowship training programs | Make a concerted effort to expand fellowship training programs to include the gynecologic oncology specialty. |
| Cass et al. (2016)45 | Strategies to increase GO care | Promoting the gynecologic oncology specialty within medical schools and residency programs through career guidance and mentorship by senior GOs | Encourage medical schools and residency programs to focus specifically on promotion of the gynecologic oncology specialty through mentorship and career guidance within their programs as an approach to increasing the volume of GOs within the United States. These activities can help to minimize stress and burnout within the field. |
| Collins et al. (2014)18 | Factors associated with GO use/non-use; facilitators/barriers to GO access; strategies to increase GO care | Expanding fellowship training programs | Train a more diverse oncology workforce; enhance educational efforts and awareness of racial and ethnic disparities. |
| Minig et al. (2015)28 | Facilitators/barriers to GO access; strategies to increase GO care | Expanding fellowship training programs | Expand fellowship training programs worldwide. |
| National Academies of Sciences, Engineering, and Medicine (2016)10 | Factors associated with GO use/non-use; facilitators/barriers to GO access; strategies to increase GO care | Use of academic detailing | Academic detailing is peer-to-peer educational outreach; traditionally, its goal is to improve clinical practice in a targeted area, usually one involving patient care. Academic detailing can be used to increase the number of physicians who specialize in gynecologic oncology. |
| Ovarian Cancer Research Alliance (n.d.)46 | Strategies to increase GO care | Utilize survivors in teaching students | Bring ovarian cancer survivors and caregivers into medical education programs to educate future health care providers about ovarian cancer by sharing stories of diagnosis, treatment, and survivorship, along with facts about the disease. |
| Society of Gynecologic Oncology (2013)41 | Strategies to increase GO care | Reviewing/revising hospital credentialing policies | Change hospital credentialing policies to discourage providers who do not have specialty training in GO from providing care to women with gynecologic cancer. |
GO, gynecologist oncologist.
The article also proposed developing and testing new physician payment methods to ensure that the highest quality care is delivered to women with gynecologic cancer. Specifically, the article stated that there is currently no difference in compensation when care is provided by the best and most-experienced specialists versus when care is provided by those without specialized training in gynecologic cancer. The article also stated that limited reimbursement exists for coordination of care, adherence to management guidelines, meeting benchmarks on meaningful quality parameters, and achieving good patient satisfaction.41 Developing and testing new payment methods could increase access to GOs. Specifically, the article noted that there is currently no difference in compensation when care is provided by specialists with the best training and most experience in gynecologic cancer compared to when care is provided by those who do not have specialized training in gynecologic cancer. There is also limited reimbursement for coordination of care, adherence to management guidelines, meeting benchmarks on meaningful quality parameters, and achieving good patient satisfaction.41 Developing and testing new payment methods could increase access to GOs.
Two articles mentioned approaches to improving and increasing insurance coverage for gynecologic oncology care. One source proposed allowing GOs to appeal insurance coverage denials, an option that is available to other subspecialties.17 Another source proposed including insurance plan coverage for travel expenses for patients who must travel to receive gynecological cancer treatment, including subsidizing travel costs for cancer treatment.40 Both of these approaches may increase access to and use of gynecologic care by ovarian cancer patients.
Finally, several articles mentioned approaches aimed at expanding or enhancing the GO workforce. In particular, some authors proposed a concerted effort to expand fellowship training programs to include the gynecologic oncology specialty as a means of increasing the workforce in this area.18,28,39 The use of academic detailing, which involves peer-to-peer outreach to improve the quality of care and to build priority for change in clinicians and leadership, is another potential approach that could be used to increase the number of physicians who specialize in gynecologic oncology.10 Encouraging medical schools to focus specifically on promoting the gynecologic oncology specialty within their medical schools and residency programs could be yet another approach to increase the volume of GOs within the United States.45
Utilizing survivors in teaching students is another proposed approach. For example, Survivors Teaching Students®, developed by the Ovarian Cancer Research Alliance, brings ovarian cancer survivors and caregivers into medical education programs to educate future health care providers about ovarian cancer by sharing stories of diagnosis, treatment, and survivorship, along with facts about the disease. Medical/health care students interact with and learn from ovarian cancer survivors in a classroom setting.46 Finally, one article proposed reviewing/revising hospital credentialing policies to discourage providers who do not have specialty training in gynecologic oncology from providing care to women with gynecologic cancer.41
Discussion
We found several potentially promising approaches and strategies for increasing GO care of ovarian cancer patients. While minimal evidence for the implementation and efficacy of these proposed approaches exists in the literature, they provide a valuable framework for public health programs and quality cancer care improvement entities to follow. Studies aimed at implementation of these proposed strategies by public health programs and other entities could provide evidence for which strategy may work best in a certain population of patients or providers. Specific adaptation of these strategies to an environment or population, and implementation of various combinations of strategies (such as increasing education and referrals), may yield necessary data regarding the most effective way to bring about sustained improvements in ovarian cancer care within a particular population.
To meet the standard of care and ensure that all patients with ovarian cancer are treated by a GO, no one model of care will likely serve all patients in all settings. A multicomponent approach would be a key consideration when implementing any intervention or strategy aimed at increasing standard treatment among women diagnosed with ovarian cancer. For example, different approaches for a particular race or ethnicity would likely be necessary to bring about improvement. In addition, women in rural settings may not have access to a GO or a high-volume cancer center, so different approaches may be needed to increase access for women in these remote locations.
There are several resources available that can help tailor strategies for disadvantaged populations. The Guide to Community Preventive Services is a collection of evidence-based findings to assist public health practitioners in selecting evidence-based interventions to promote health and prevent disease, injury, disability, and premature death in their communities, and includes recommended interventions focused on reducing health equities.47 Although it does not address ovarian cancer specifically, the guide offers considerations for implementing interventions with strong evidence of effectiveness for breast and cervical cancer. This guidance can inform adaptations to strategies for ovarian cancer (e.g., patient navigation and telemedicine for rural populations). In addition, CDC developed the Inside Knowledge: Get the Facts about Gynecologic Cancer campaign to increase knowledge of risk factors, symptoms, and treatment recommendations of ovarian cancer among health care providers and the public.16 Several National Comprehensive Cancer Control Program (NCCCP) awardees have partnered with the Inside Knowledge campaign to effectively reach traditionally underserved populations in the United States, including black women.3 Their efforts may inform adaptations for other target audiences.
Globally, there are multiple approaches that other countries are taking to increase access to and receipt of care by a GO among women diagnosed with ovarian cancer. The United Kingdom and Australia are both piloting approaches to collect data related to diagnosis, treatment, and outcomes from all ovarian cancer cases nationwide to identify trends and gaps in ovarian cancer care and use this information to improve patient care nationwide.48.49 In addition, multiple European countries, including areas in the United Kingdom, Denmark, and the Netherlands, have begun using multidisciplinary care teams and centralization of services, where all patients with ovarian cancer are referred to high-volume centers to receive their care by teams that include multiple specialized physicians.34 These strategies are not currently being implemented in the United States. This type of service centralization is likely easier to implement in countries where there is one health care system, compared to the United States, where patients may be served by different types of health systems or may have different types of insurance coverage for certain services.11,35 In addition, the type and use of electronic health records by different health systems or data reporting agencies may vary significantly, making it more difficult to collect standardized data to monitor services being provided.11
In the United States, public health and community-based programs provide support for ensuring that evidence-based recommendations are followed. CDC’s NCCCP is an ideally situated public health program to support implementation of the proposed approaches we identified in our review to increase GO care among ovarian cancer patients. The program consists of a diverse group of cancer control partners from academia, government, and nongovernment organizations across the United States, in every state and several tribes and jurisdictions. These coalitions of partners come together to work on current and emerging cancer issues, including cancer prevention, early detection, survivorship, and disparities, through implementation of environmental approaches, community-clinical linkages, and health system changes. Our literature review highlights several potentially promising approaches—provider, patient, and public education; partner enrichment; and patient navigation—that could be integrated into the activities conducted by NCCCP. NCCCP programs also have close connections to and understanding of their local community, health care systems, and health care providers; an emphasis on improving the quality of life among those diagnosed with cancer; experience using environmental and health system change strategies to address issues in cancer control; and existing multisector partnerships that have been used to support implementation of evidenced-based interventions. Furthermore, working through NCCCP practitioners ensures that data, knowledge, and information generated through implementation of these strategies are useful and meaningful for public health.
There are some limitations to this literature review. First, it was not a systematic review. In addition, there was limited evidence of effectiveness for the identified strategies and approaches that were included, which made it difficult to assess which strategies may be most appropriate for particular populations.
Conclusion
According to NASEM, receiving ovarian cancer treatment from a GO is key recommendation ready to be disseminated and implemented widely to improve survival. Our findings from this literature review begin this process by identifying several potential strategies for implementation. As the evidence for implementation of effective strategies continues to build, these potentially promising strategies may be incorporated into sustainable public health practices implemented throughout the United States.
Acknowledgment
The authors would like to thank Ms. Julia Schaeman for her assistance with reviewing the published studies included in this article.
Funding Information
This work was supported, in part, by contract no. 200-2018-F-03524 from the Centers for Disease Control and Prevention (CDC) to ICF. The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention or ICF.
Footnotes
Author Disclosure Statement
No competing financial interests exist.
References
- 1.U.S. Cancer Statistics Working Group. U.S. Cancer Statistics Data Visualizations Tool, based on 2019 submission data (1999–2017): U.S. Department of Health and Human Services, Centers for Disease Control and Prevention and National Cancer Institute, 2020. Available at: www.cdc.gov/cancer/dataviz. Accessed January 3, 2021.
- 2.Committee Opinion No. 716 Summary: The role of the obstetrician-gynecologist in the early detection of epithelial ovarian cancer in women at average risk. Obstet Gynecol 2017;130:664–665. [DOI] [PubMed] [Google Scholar]
- 3.Stewart SL, Harewood R, Matz M, et al. Disparities in ovarian cancer survival in the United States (2001–2009): Findings from the CONCORD-2 study. Cancer 2017; 123(Suppl 24):5138–5159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Torre LA, Trabert B, DeSantis CE, et al. Ovarian cancer statistics, 2018. CA Cancer J Clin 2018;68:284–296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Gajjar K, Ogden G, Mujahid MI, Razvi K. Symptoms and risk factors of ovarian cancer: A survey in primary care. ISRN Obstet Gynecol 2012;2012:754197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ryerson AB, Eheman C, Burton J, et al. Symptoms, diagnoses, and time to key diagnostic procedures among older U.S. women with ovarian cancer. Obstet Gynecol 2007; 109:1053–1061. [DOI] [PubMed] [Google Scholar]
- 7.Henderson JT, Webber EM, Sawaya GF. Screening for Ovarian Cancer: An Updated Evidence Review for the US Preventive Services Task Force. Evidence Synthesis No. 157. Rockville, MD: Agency for Healthcare Research and Quality (US), 2018. [PubMed] [Google Scholar]
- 8.American Cancer Society. Cancer facts & Figures 2018–Special section: Ovarian cancer, 2018. Available at: https://www.cancer.org/research/cancer-facts-statistics/all-cancer-facts-figures/cancer-facts-figures-2018.html Accessed February 18, 2019.
- 9.US Preventive Services Task Force, Grossman DC, Curry SJ, et al. Screening for ovarian cancer: US Preventive Services Task Force recommendation statement. JAMA 2018;319:588–594. [DOI] [PubMed] [Google Scholar]
- 10.National Academies of Sciences, Engineering, and Medicine (NASEM), Committee on the State of the Science in Ovarian Cancer Research; Board on Health Care Services; Institute of Medicine. Ovarian cancers: Evolving paradigms in research and care. Washington, DC: National Academies Press (US), 2016. [PubMed] [Google Scholar]
- 11.Long B, Chang J, Ziogas A, Tewari KS, Anton-Culver H, Bristow RE. Impact of race, socioeconomic status, and the health care system on the treatment of advanced-stage ovarian cancer in California. Am J Obstet Gynecol 2015; 212:468.e1–468.e9. [DOI] [PubMed] [Google Scholar]
- 12.Cliby WA, Powell MA, Al-Hammadi N, et al. Ovarian cancer in the United States: Contemporary patterns of care associated with improved survival. Gynecol Oncol 2015; 136:11–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hodeib M, Chang J, Liu F, et al. Socioeconomic status as a predictor of adherence to treatment guidelines for early-stage ovarian cancer. Gynecol Oncol 2015;138:121–127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.O’Malley CD, Shema SJ, Cress RD, et al. The implications of age and comorbidity on survival following epithelial ovarian cancer: Summary and results from a Centers for Disease Control and Prevention study. J Womens Health (Larchmt) 2012;21:887–894. [DOI] [PubMed] [Google Scholar]
- 15.Cress RD, Bauer K, O’Malley CD, et al. Surgical staging of early stage epithelial ovarian cancer: Results from the CDC-NPCR ovarian patterns of care study. Gynecol Oncol 2011;121:94–99. [DOI] [PubMed] [Google Scholar]
- 16.Rim SH, Polonec L, Stewart SL, Gelb CA. A national initiative for women and healthcare providers: CDC’s Inside Knowledge: Get the Facts About Gynecologic Cancer campaign. J Womens Health (Larchmt) 2011;20:1579–1585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Duska LR. Access to quality gynecologic oncology care: A work in progress. Cancer 2018;124:2680–2683. [DOI] [PubMed] [Google Scholar]
- 18.Collins Y, Holcomb K, Chapman-Davis E, Khabele D, Farley JH. Gynecologic cancer disparities: A report from the Health Disparities Taskforce of the Society of Gynecologic Oncology. Gynecol Oncol 2014;133:353–361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Stewart SL, Townsend JS, Puckett MC, Rim SH. Adherence of primary care physicians to evidence-based recommendations to reduce ovarian cancer mortality. J Womens Health (Larchmt) 2016;25:235–241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Stewart SL, Lakhani N, Brown PM, Larkin OA, Moore AR, Hayes NS. Gynecologic cancer prevention and control in the National Comprehensive Cancer Control Program: Progress, current activities, and future directions. J Womens Health (Larchmt) 2013;22:651–657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hess LM, Stehman FB, Method MW, Weathers TD, Gupta P, Schilder JM. Identification of the optimal pathway to reach an accurate diagnosis in the absence of an early detection strategy for ovarian cancer. Gynecol Oncol 2012; 127:564–568. [DOI] [PubMed] [Google Scholar]
- 22.Stewart SL, Rim SH, Richards TB. Gynecologic oncologists and ovarian cancer treatment: Avenues for improved survival. J Womens Health (Larchmt) 2011;20:1257–1260. [DOI] [PubMed] [Google Scholar]
- 23.Gostout BS, Pachman DR, Lechner R. Recognizing and treating ovarian cancer. Minn Med 2012;95:40–42. [PubMed] [Google Scholar]
- 24.Urban RR, He H, Alfonso R, Hardesty MM, Gray HJ, Goff BA. Ovarian cancer outcomes: Predictors of early death. Gynecol Oncol 2016;140:474–480. [DOI] [PubMed] [Google Scholar]
- 25.Peters ITA, van Haaften C, Trimbos JB. If the mountain does not come to Mohammad: The significance of guest operations for early stage ovarian cancer. J Gynecol Surg 2014;30:265–272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Goff BA, Miller JW, Matthews B, et al. Involvement of gynecologic oncologists in the treatment of patients with a suspicious ovarian mass. Obstet Gynecol 2011;118:854–862. [DOI] [PubMed] [Google Scholar]
- 27.Rim SH. Ovarian cancer treatment decisions: Accessing gynecologic oncology care [dissertation]. Chapel Hill, NC: ProQuest Information & Learning, 2016. [Google Scholar]
- 28.Minig L, Padilla-Iserte P, Zorrero C. The relevance of gynecologic oncologists to provide high-quality of care to women with gynecological cancer. Front Oncol 2016;5: 308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Boyd LR, Novetsky AP, Curtin JP. Ovarian cancer care for the underserved: Are surgical patterns of care different in a public hospital setting? Cancer 2011;117:777–783. [DOI] [PubMed] [Google Scholar]
- 30.Sinno AK, Li X, Thompson RE, et al. Trends and factors associated with radical cytoreductive surgery in the United States: A case for centralized care. Gynecol Oncol 2017; 145:493–499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Ricci S, Tergas AI, Long Roche K, et al. Geographic disparities in the distribution of the US gynecologic oncology workforce: A Society of Gynecologic Oncology study. Gynecol Oncol Rep 2017;22:100–104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Stewart SL, Cooney D, Hirsch S, et al. The effect of gynecologic oncologist availability on ovarian cancer mortality. World J Obstet Gynecol 2014;3:71–77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Cowan RA, O’Cearbhaill RE, Gardner GJ, et al. Is it time to centralize ovarian cancer care in the United States? Ann Surg Oncol 2016;23:989–993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Fung-Kee-Fung M, Kennedy E, Biagi J, et al. The optimal organization of gynecologic oncology services: A systematic review. Curr Oncol 2015;22:e282–e293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Keyver-Paik MD, Abramian A, Domröse C, et al. Integrated care in ovarian cancer “IgV Ovar”: Results of a German pilot for higher quality in treatment of ovarian cancer. J Cancer Res Clin Oncol 2016;142:481–487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Woo YL, Kyrgiou M, Bryant A, Everett T, Dickinson HO. Centralisation of services for gynaecological cancer. Cochrane Database Syst Rev 2012;2012:CD007945. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Bristow RE, Chang J, Ziogas A, Gillen DL, Bai L, Vieira VM. Spatial analysis of advanced-stage ovarian cancer mortality in California. Am J Obstet Gynecol 2015;213: 43.e1–43.e8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.van Altena AM, van den Akker PAJ, de Hullu JA, et al. Efficacy of a regional network for ovarian cancer care. Obstet Gynecol 2013;122:668–675. [DOI] [PubMed] [Google Scholar]
- 39.Canadian Partnership Against Cancer. Pan-Canadian Standards for Gynecologic Oncology, 2018. Available at: https://g-o-c.org/wp-content/uploads/2015/01/18CPAC_PanCanadian-Standards-for-Gynecologic-Oncology_EN-Final.pdf Accessed February 18, 2019.
- 40.Colorado Women’s Health, University of Colorado. Cancers, such as ovarian, endometrial and uterine, are best treated by a gynecologic oncologist, but millions of women don’t have access to one. Colorado Women’s Health Gynecologic Oncology website. Available at: https://cancer.coloradowomenshealth.com/cancer-care-geographic-barriers/index.html Accessed February 18, 2019.
- 41.Society of Gynecologic Oncology. Creating a New Paradigm in Gynecologic Cancer Care: Policy Proposals for Delivery, Quality and Reimbursement. A Society of Gynecologic Oncology White Paper, February 2013. Available at: https://www.sgo.org/wp-content/uploads/2012/09/Practice_Summit_Report_FINAL.pdf Accessed February 18, 2019.
- 42.Horvath LE, Yordan E, Malhotra D, et al. Multidisciplinary care in the oncology setting: Historical perspective and data from lung and gynecology multidisciplinary clinics. J Oncol Pract 2010;6:e21–e26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Ramzan AA, Behbakht K, Corr BR, Sheeder J, Guntupalli SR. Minority race predicts treatment by non-gynecologic oncologists in women with gynecologic cancer. Ann Surg Oncol 2018;25:3685–3691. [DOI] [PubMed] [Google Scholar]
- 44.Shalowitz DI, Smith AG, Bell MC, Gibb RK. Teleoncology for gynecologic cancers. Gynecol Oncol. 2015;139:172–177. [DOI] [PubMed] [Google Scholar]
- 45.Cass I, Duska LR, Blank SB, et al. Stress and burnout among gynecologic oncologists: A Society of Gynecologic Oncology evidence-based review and recommendations. Gynecol Oncol 2016;143:421–427. [DOI] [PubMed] [Google Scholar]
- 46.Survivors Teaching Students. Ovarian Cancer Research Alliance website. Available at: https://ocrahope.org/get-involved/survivors-teaching-students Accessed February 18, 2019.
- 47.Truman BI, Smith-Akin CK, Hinman AR, et al. Developing the Guide to Community Preventive Services—Overview and rationale. The Task Force on Community Preventive Services. Am J Prev Med 2000;18(1 Suppl):18–26. [DOI] [PubMed] [Google Scholar]
- 48.Public Health England. Ovarian Cancer Audit Feasibility Pilot. Disease Profile in England: Incidence, mortality, stage and survival for ovary, fallopian tube and primary peritoneal carcinomas. National Cancer Registration and Analysis Service website, 2020. Available at: http://www.ncin.org.uk/cancer_type_and_topic_specific_work/cancer_type_specific_work/gynaecological_cancer/gynaecological_cancer_hub/ovarian_cancer_audit_feasibility_pilot_outputs Accessed July 15, 2020.
- 49.Heriot N, Brand A, Cohen P, et al. Developing an Australian multi-module clinical quality registry for gynaecological cancers: A protocol paper. BMJ Open 2020;10: e034579. [DOI] [PMC free article] [PubMed] [Google Scholar]


