Abstract
Spontaneous coronary artery dissection (SCAD) is an under-recognized cause of acute coronary syndrome that predominantly affects women in adulthood and is the leading cause of acute myocardial infarction in pregnancy. The most common clinical presentation is ST-segment elevation myocardial infarction (STEMI) or non-STEMI, followed by cardiogenic shock (∼2%), sudden cardiac death (0.8% in autopsy series), cardiac arrest, ventricular arrhythmias (∼5%), and Takotsubo syndrome. The prevalence of SCAD in the general population is largely uncertain due to underdiagnosis. Oral contraceptives, post-menopausal therapy, and infertility treatments are recognized associated factors. The pathological substrates (fibromuscular dysplasia) and triggers (especially emotional stress) are commonly present in affected women. The few cases with a precise genetic aetiology occur in the context of syndromic and non-syndromic connective tissue diseases. The only true certainty in SCAD is the overwhelming prevalence in women. The first event as well as the recurrence (up to 30%, which varies depending on the definition) is largely unpredictable. The treatment strategy is highly individualized and requires extensive additional study in order to optimize outcomes and prevent major adverse cardiovascular events in affected individuals. We have known about SCAD for nearly a century, but we still do not know how best to prevent, diagnose, and treat it, making SCAD a highly important and unmet clinical need.
Keywords: Spontaneous coronary artery dissection, Pregnancy-related death, Fibromuscular dysplasia, Genetics
Introduction
Spontaneous coronary artery dissection (SCAD) is defined as an ‘epicardial coronary artery dissection that is not associated with atherosclerosis or trauma and is not iatrogenic’.1 Spontaneous coronary artery dissection is an important yet under-recognized cause of acute coronary syndrome (ACS) and constitutes up to 4% of all ACS cases.1 It occurs predominantly in middle-aged women without conventional risk factors for atherosclerotic coronary artery disease. Spontaneous coronary artery dissection is the cause of acute myocardial infarction (AMI) in 22–43% of women ≤50 years of age2 and is the most common cause of pregnancy-associated AMI (43%).3 There are limited data, however, that have shed light on the precise aetiology, genetic basis, and predictors of SCAD recurrence. This review summarizes the definition and classification of SCAD, known associated factors and triggers, underlying diseases, potential toxic contributors (e.g. drugs), diagnosis and treatment, and recurrence rate and risk, in addition to what we delineate as familial vs. non-familial and syndromic vs. non-syndromic SCAD.
Clinical issues
Clinical presentation
The most common recognized clinical manifestation of SCAD is AMI in the context of ST-segment elevation myocardial infarction (STEMI) or non-STEMI (NSTEMI).1 Less typical manifestations at onset include cardiogenic shock (∼2%),4 sudden cardiac death (SCD)5 (0.8% in autopsy series of SCD),6 cardiac arrest,1,7 ventricular arrhythmias (∼5%),1 and Takotsubo syndrome. The most common symptoms include chest pain with potential radiation to the left arm or neck, nausea/vomiting, dyspnoea, and diaphoresis. Early symptoms are often ignored, and there is a latency period between symptom onset and medical attention. Symptoms post-SCAD are similarly common, and often include chest pain even in the absence of a recurrent event. Troponin levels are generally increased, but can be normal.8
Diagnosis and classification
Spontaneous coronary artery dissection should be considered in women with a paucity of atherosclerotic risk factors and who present with ACS. This clinical suspicion warrants immediate assessment with urgent coronary angiography.1 Spontaneous coronary artery dissection is classified into three distinct angiographic types. Type 1 SCAD is characterized by contrast entering the false lumen, which is seen in less than one-third of patients. Type 2 SCAD is the most common, seen in up to two-thirds of patients, and has the appearance of a long, smooth, and diffusely narrowed segment with an intra-mural haematoma. This type carries the highest risk of being undetected on angiography. Type 3 SCAD is the least common and can mimic atherosclerotic lesions given its focal appearance.9 The diagnostic confirmation of Types 2 and 3 SCAD may require intra-coronary imaging including optical coherence tomography and intra-vascular ultrasound (IVUS).10 Cardiac coronary tomography angiography is not recommended to be a first-line imaging modality of SCAD because small and non-proximal dissections can be missed.1,10
Treatment
Appropriate management of SCAD relies on precision diagnosis and aims at controlling symptoms, improving outcomes, and preventing recurrence. However, the treatment of SCAD is highly individualized.11 Spontaneous healing seems to occur weeks to months after the acute episode in most cases. In a large multi-centre series, most SCAD patients were treated conservatively (84.3%), 14.1% of patients underwent percutaneous coronary intervention (PCI), and 0.7% of patients had coronary artery bypass surgery (CABG).12 There are no guidelines for treating SCAD-related ACS, and current treatment strategies are based on expert opinion.13 The general trend of first-line treatment is medical therapy alone.1,4,13 Antiplatelet therapy and beta-blockers are usually initiated in haemodynamically stable patients. The potential risk of dissection and intra-mural haematoma precludes the safe administration of thrombolytic therapy. Angiotensin-converting enzyme inhibitors or angiotensin-receptor blockers are administered in patients with significant LV dysfunction, and statin therapy is recommended only in patients with pre-existing dyslipidaemia or known atherosclerotic disease. Although PCI may be complicated by the risk of iatrogenic catheter–induced dissection and propagation of SCAD, patients with STEMI are more frequently treated with IVUS-guided primary PCI (31 vs. 16%, P < 0.001). Optical coherence tomography should be considered as a second option due to the risk of dissection propagation related to dye infusion during pullback.14 Finally, CABG is uncommonly performed and considered in patients with left main coronary artery dissection or multi-vessel disease after failed primary PCI.1
Recurrence
The term ‘recurrence’ can describe the extension of the dissection along the same vessel or a de novo dissection affecting different segments of the same coronary artery (CA) or different CAs. Although the risk of recurrence of SCAD is up to 30%,1,12 a recent prospective observational study reported recurrence in 2% of cases over a median follow-up of 2 years.15 A recurrent myocardial infarction in up to 10%, including 2.4% de novo recurrent SCAD, occurred over a median follow-up of 3 years in another recent multi-centre prospective observational study.16 Coronary artery tortuosity has been reported to be a risk factor for recurrence.17
Pathogenesis
Spontaneous coronary artery dissection is not attributable to a single identified pathogenic mechanism. There is heterogeneity in terms of triggers, circumstances, and underlying predisposing disorders. The hormonal hypothesis/contribution is of course of pertinence, given the overwhelming prevalence of SCAD in women. Fibromuscular dysplasia (FMD), chronic inflammatory and autoimmune diseases, genetic causes related to monogenic syndromes associated with arterial dissection risk, hypertension, and physical and emotional triggers have been reported.
Female sex hormones
Spontaneous coronary artery dissection can occur in both childbearing and post-menopausal age, in both multiparous (>4 pregnancies) and nulliparous women, in uncomplicated pregnancies (70% in the early post-partum) as well as in complicated pregnancies (eclampsia and pre-eclampsia).3,18 Administration of exogenous hormones is a potential risk factor, including oral contraception, post-menopausal therapy, and infertility treatments.19 During pregnancy, hormonal changes, vasomotor tone, increased blood volume, and flow modifications may contribute to transient epicardial coronary artery fragility that may constitute a potential substrate favouring the occurrence of SCAD.1,3,12 Pregnancies of women carriers of defects in genes associated with known heritable arteriopathies must be monitored and protected even if the arterial disease has not yet clinically manifested. This suggestion also applies to pregnancies of women who are members of families in which a SCAD event has occurred, irrespective of the identification of the genetic causes. Spontaneous coronary artery dissection has to be included in the list of causes of cardiovascular death in pregnancy, and together with peripartum cardiomyopathy, Takotsubo syndrome, arrhythmias, and aortic dissection, they account for up to one-third of all pregnancy-related maternal deaths.20
Fibromuscular dysplasia
Fibromuscular dysplasia is a non-atherosclerotic, non-inflammatory arteriopathy that primarily manifests as beading (multi-focal FMD) or focal lesions in medium- or small-sized arteries, although the clinical phenotype of FMD has recently expanded to include arterial dissection, aneurysm, and tortuosity.21 Approximately 80–90% of patients with FMD are women. Up to 86% of screened patients with SCAD have FMD. The diagnosis of FMD is made via imaging in the form of angiography, computed tomographic/magnetic resonance angiography, or duplex ultrasound. In a study addressing the prevalence of FMD among 50 SCAD patients, 12% had >1 dissected coronary artery. A total of 86% of SCAD patients had an FMD of ≥1 non-coronary artery.22 In addition, FMD was recently noted to be an independent predictor of 3-year major adverse cardiovascular events (MACE) in patients with SCAD.16
Systemic autoimmune and inflammatory diseases
Although chronic inflammatory and autoimmune diseases have been reported in patients with SCAD, the association is not common (4.7%).12 Specifically, SCAD has been described in case reports of patients with various systemic inflammatory diseases, including systemic lupus erythematosus, rheumatoid arthritis, Crohn’s disease, inflammatory bowel disease, polyarteritis nodosa, sarcoidosis, Churg–Strauss syndrome, Wegener granulomatosis, Kawasaki disease, cryoglobulinemia, hypothyroidism, thyroid storm, and autoimmune thyroiditis.1,12,23
Autoimmune diseases are more common in female patients, and causation has not yet been established.
Genetic arteriopathies
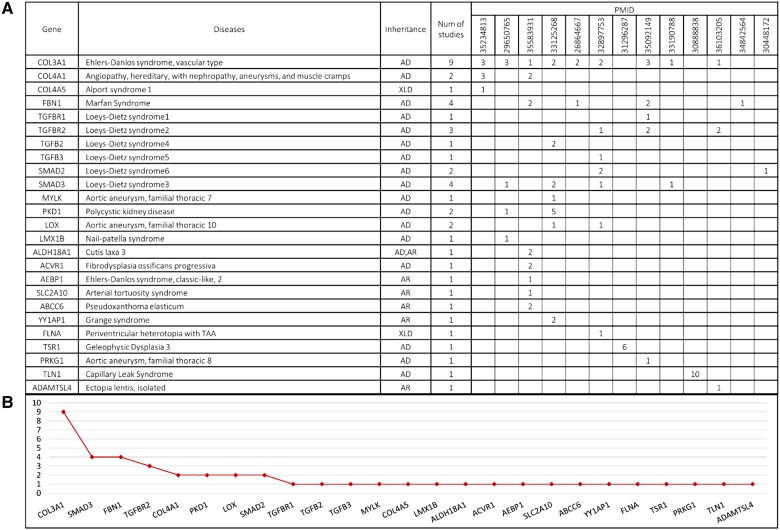
Clinically, SCAD rarely clusters within families with genetic arteriopathies. A positive family history of SCAD is reported in ∼1% of cases,1,2,24 and most cases are sporadic. Despite this limited evidence, genetic causes have been extensively investigated and are plausibly associated with the event in a proportion of patients ranging between 5 and 17%. (References are listed as PMID in Figure 1.) This range is due to multiple factors: patient selection; deep clinical phenotyping encompassing not only the SCAD event but the arterial vascular tree as a whole; and the genetic testing strategy, from single gene to multigene panels, up to whole-exome sequencing. Although research specifically dedicated to the identification of one or more SCAD-specific genes has been carried out, no gene is currently validated whose defects are selectively associated with SCAD. Gene defects tend to occur in syndromic contexts associated with hereditary–familial arterial disease. Among these, COL3A1, whose defects cause vascular Ehlers–Danlos syndrome (EDS IV), is the most common disease gene. Pathogenic variants in COL3A1 are reported from at least nine reputable scientific sources. In an extensive review including data from 737 patients with genetically confirmed EDS IV, 26 patients had SCAD either at the onset or during the course of the disease.25COL3A1 is followed by FBN1, whose genetic defects cause Marfan syndrome, by the genes whose defects cause Loeys–Dietz syndromes 1–6 (TGFBR1, TGFBR2, TGFB3, TGFB2, SMAD3, and SMAD2), and finally by other rare genes associated with syndromic and non-syndromic thoracic aortic aneurism/thoracic acute aortic dissection, including extremely rare diseases such as pseudoxanthoma elasticum.26 Genetic disorders were discovered to be an independent predictor of 3-year MACE in patients with SCAD.16 The identification of the genetic causes of SCAD also impacts the risk of dissection at extracoronary sites. It sheds light on clinically relevant disease manifestations (e.g. risk of bowel or uterine rupture in EDS IV), which warrant select/serial monitoring. Furthermore, the detection of pathogenic variants in the proband facilitates family screening, which allows for the identification of affected asymptomatic family members as well as young healthy carriers of the putative genetic defect.
Figure 1.
The figure includes a table (A) and a graphical view (B) of the number and PMID of scientific reports describing genetic defects identified in spontaneous coronary artery dissection. Numbers in PMID columns refer to the number of reported cases. Genes reported more than once include COL3A1, SMAD3, FBN1, COL4A1, PKD1, LOX, and TGFBR2. Other genes are reported once but are well known to be associated with syndromic and non-syndromic connective tissue diseases and include TGFB2, TGFB3, MYLK, SMAD2, COL4A5, LMX1B, ALDH18A1, ACVR1, AEBP1, SCL2A10, ABCC6, YY1AP1, FLNA, and PRKG1. Other genes (TSR1 and TLN1) are provisional and still unconfirmed.
Hypertension
Hypertension is common in SCAD survivors (45% of cases). It is one of the traditional risk factors identified post-SCAD along with hypercholesterolaemia. Patients with SCAD and hypertension are older, more often post-menopausal, and have more extensive coronary artery involvement than SCAD patients with normal blood pressure.27,28 Hypertensive SCAD patients undergoing revascularization exhibit an increased risk of procedural-related complications.
Stressors and triggers
Intense physical or emotional stress is a potential contributor or trigger of SCAD. A large multi-centre study reported emotional stress in 50.3% and physical stress in 28.9% (9.8% lifting >50 pounds),11 confirming prior values of emotional stress (56.5% of 168) reported in a smaller series by the same authors.12 In other series, however, the prevalence of emotional stress was lower (26.0%), demonstrating that the qualitative and quantitative evaluation of the stressors can be variable. In any case, traditional female-associated risk factors for SCAD, such as depression, anxiety, emotional stress, and migraines, are more common in women than in men. Illicit drug use, in particular cocaine and amphetamine abuse, can further contribute. Finally, the co-occurrence of SCAD and stress cardiomyopathy, although anecdotally reported, suggests the possibility that intense stressors, more frequent in women, may be similar in the two conditions.29,30
Considerations
Although some risk factors and triggers are known, SCAD is an acute coronary event that cannot be predicted yet. Known ‘predisposing’ conditions are not sufficient to identify women at risk for a first event and for recurrence. Even in the presence of precise causes such as pathogenic defects in genes associated with heritable arterial diseases, definite protection of the coronary tree is challenging since there is no evidence that SCAD is preceded by aneurysmal dilatation of the coronary arteries as can occur at other arterial sites.
Future efforts should focus on the precise diagnosis of SCAD, especially Types 2 and 3 (standard intra-coronary imaging implementation?), in all acute non-atherosclerotic coronary syndromes in women, and on the annotation of prodromal symptoms, circumstances, and drugs as well as underlying systemic diseases, with the goal of collecting data more so than drawing absolute conclusions. While we have known about SCAD for almost a century,31 we still do not know how best to prevent, diagnose, and treat it, rendering it an important and unmet clinical need.
Contributor Information
Alexandra Smirnova, Transplant Research Area and Centre for Inherited Cardiovascular Diseases, Scientific Department, Fondazione IRCCS Policlinico San Matteo, Pavia, Italy.
Flaminia Aliberti, Transplant Research Area and Centre for Inherited Cardiovascular Diseases, Scientific Department, Fondazione IRCCS Policlinico San Matteo, Pavia, Italy.
Claudia Cavaliere, Transplant Research Area and Centre for Inherited Cardiovascular Diseases, Scientific Department, Fondazione IRCCS Policlinico San Matteo, Pavia, Italy.
Ilaria Gatti, Transplant Research Area and Centre for Inherited Cardiovascular Diseases, Scientific Department, Fondazione IRCCS Policlinico San Matteo, Pavia, Italy.
Viviana Vilardo, Transplant Research Area and Centre for Inherited Cardiovascular Diseases, Scientific Department, Fondazione IRCCS Policlinico San Matteo, Pavia, Italy.
Carmelina Giorgianni, Transplant Research Area and Centre for Inherited Cardiovascular Diseases, Scientific Department, Fondazione IRCCS Policlinico San Matteo, Pavia, Italy.
Chiara Cassani, Department of Clinical, Surgical, Diagnostic and Pediatric Sciences, University of Pavia, Pavia, Italy; Unit of Obstetrics and Gynecology, IRCCS Policlinico S. Matteo Foundation, Pavia, Italy.
Alessandra Repetto, Division of Cardiology, Fondazione IRCCS Policlinico S. Matteo, Pavia, Italy.
Nupoor Narula, Division of Cardiology, Department of Medicine, Weill Cornell Medical College, New York, USA.
Lorenzo Giuliani, Transplant Research Area and Centre for Inherited Cardiovascular Diseases, Scientific Department, Fondazione IRCCS Policlinico San Matteo, Pavia, Italy.
Mario Urtis, Transplant Research Area and Centre for Inherited Cardiovascular Diseases, Scientific Department, Fondazione IRCCS Policlinico San Matteo, Pavia, Italy.
Yukio Ozaki, Department of Cardiology, Fujita Health University Hospital, Toyoake, Japan.
Francesco Prati, UniCamillus, Saint Camillus International University of Health Sciences, Rome, Italy; Centro per la Lotta Contro L’Infarto—CLI Foundation, Rome, Italy.
Eloisa Arbustini, Transplant Research Area and Centre for Inherited Cardiovascular Diseases, Scientific Department, Fondazione IRCCS Policlinico San Matteo, Pavia, Italy.
Michela Ferrari, Transplant Research Area and Centre for Inherited Cardiovascular Diseases, Scientific Department, Fondazione IRCCS Policlinico San Matteo, Pavia, Italy.
Funding
Research on coronary artery disease and heritable arteriopathies is supported by continuous RC funds on heritable connective tissue diseases from the Italian Ministry of Health to the Fondazione IRCCS Policlinico San Matteo, n. 221-rcr2000b-8 and n. 888-rcr2017i-71 projects; project RCR-2019-23669116_001 (CV-PREVITAL) from the Italian Ministry of Health; Telethon grant n.GGP08238 for Marfan Syndrome; FRRB grant n.CP2_14/2018 for coronary artery disease and monogenic arteriopathies.
Data availability
No new data were generated or analysed in support of this research.
References
- 1. Hayes SN, Kim ESH, Saw Jet al. . Spontaneous coronary artery dissection: current state of the science: a scientific statement from the American Heart Association. Circulation 2018;137:e523–e557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Saw J, Aymong E, Mancini GBJet al. . Non-atherosclerotic coronary artery disease in young women. Can J Cardiol 2014;30:814–819. [DOI] [PubMed] [Google Scholar]
- 3. Elkayam U, Jalnapurkar S, Barakkat MNet al. . Pregnancy-associated acute myocardial infarction: a review of contemporary experience in 150 cases between 2006 and 2011. Circulation 2014;129:1695–1702. [DOI] [PubMed] [Google Scholar]
- 4. Kim YH, Kim SH, Lim SY, Song WH, Ahn JC. Simultaneous and spontaneous multivessel coronary artery dissection presenting as congestive heart failure. Heart Vessels 2011;26:338–341. [DOI] [PubMed] [Google Scholar]
- 5. Melez İE, Arslan MN, Melez DOet al. . Spontaneous coronary artery dissection: report of 3 cases and literature review hormonal, autoimmune, morphological factors. Am J Forensic Med Pathol 2015;36:188–192. [DOI] [PubMed] [Google Scholar]
- 6. Hill SF, Sheppard M. Non-atherosclerotic coronary artery disease associated with sudden cardiac death. Heart 2010;96:1119–1125. [DOI] [PubMed] [Google Scholar]
- 7. Seidl S, Rickli H, Rogowski Set al. . Long-term follow-up of medically treated patients with spontaneous coronary artery dissection: a prospective, Swiss single-centre cohort study. Swiss Med Wkly 2021;23:151. [DOI] [PubMed] [Google Scholar]
- 8. Lindor RA, Tweet MS, Goyal KAet al. . Emergency department presentation of patients with spontaneous coronary artery dissection. J Emerg Med 2017;52:286–291. [DOI] [PubMed] [Google Scholar]
- 9. Saw J. Coronary angiogram classification of spontaneous coronary artery dissection. Catheter Cardiovasc Interv 2014;84:1115–1122. [DOI] [PubMed] [Google Scholar]
- 10. Tweet MS, Gulati R, Williamson EE, Vrtiska TJ, Hayes SN. Multimodality imaging for spontaneous coronary artery dissection in women. JACC Cardiovasc Imaging 2016;9:436–450. [DOI] [PubMed] [Google Scholar]
- 11. Tweet MS, Eleid MF, Best PJet al. . Spontaneous coronary artery dissection: revascularization versus conservative therapy. Circ Cardiovasc Interv 2014;7:777–786. [DOI] [PubMed] [Google Scholar]
- 12. Saw J, Starovoytov A, Humphries Ket al. . Canadian spontaneous coronary artery dissection cohort study: in-hospital and 30-day outcomes. Eur Heart J 2019;40:1188–1197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Alfonso F, Bastante T, Rivero Fet al. . Spontaneous coronary artery dissection. Circ J 2014;78:2099–2110. [DOI] [PubMed] [Google Scholar]
- 14. Mahmood MM, Austin D. IVUS and OCT guided primary percutaneous coronary intervention for spontaneous coronary artery dissection with bioresorbable vascular scaffolds. Cardiovasc Revasc Med 2017;18:53–57. [DOI] [PubMed] [Google Scholar]
- 15. Garcia-Guimaraes M, Masotti M, Sanz-Ruiz Ret al. . Clinical outcomes in spontaneous coronary artery dissection. Heart 2022;108:1530–1538. [DOI] [PubMed] [Google Scholar]
- 16. Saw J, Starovoytov A, Aymong Eet al. . Canadian spontaneous coronary artery dissection cohort study: 3-year outcomes. J Am Coll Cardiol 2022;80:1585–1597. [DOI] [PubMed] [Google Scholar]
- 17. Eleid MF, Guddeti RR, Tweet MSet al. . Coronary artery tortuosity in spontaneous coronary artery dissection: angiographic characteristics and clinical implications. Circ Cardiovasc Interv 2014;7:656–662. [DOI] [PubMed] [Google Scholar]
- 18. Tweet MS, Hayes SN, Codsi Eet al. . Spontaneous coronary artery dissection associated with pregnancy. J Am Coll Cardiol 2017;70:426–435. [DOI] [PubMed] [Google Scholar]
- 19. Iyasere C, Potdar N. Spontaneous coronary artery dissection associated with infertility treatment. Cureus 2022;14:e29587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Keepanasseril A, Pfaller B, Metcalfe A, Siu SC, Davis MB, Silversides CK. Cardiovascular deaths in pregnancy: growing concerns and preventive strategies. Can J Cardiol 2021;37:1969–1978. [DOI] [PubMed] [Google Scholar]
- 21. Gornik HL, Persu A, Adlam D, et al. . First international consensus on the diagnosis and management of fibromuscular dysplasia. J Hypertens 2019;37:229–252. Erratum in: J Hypertens 2021;39:1932. [DOI] [PubMed] [Google Scholar]
- 22. Saw J, Ricci D, Starovoytov A, Fox R, Buller CE. Spontaneous coronary artery dissection: prevalence of predisposing conditions including fibromuscular dysplasia in a tertiary center cohort. JACC Cardiovasc Interv 2013;6:44–52. [DOI] [PubMed] [Google Scholar]
- 23. Camacho Freire SJ, Díaz Fernández JF, Gheorghe LLet al. . Spontaneous coronary artery dissection and hypothyroidism. Rev Esp Cardiol (Engl Ed) 2019;72:625–633. [DOI] [PubMed] [Google Scholar]
- 24. Kaadan MI, MacDonald C, Ponzini Fet al. . Prospective cardiovascular genetics evaluation in spontaneous coronary artery dissection. Circ Genom Precis Med 2018;11:e001933. [DOI] [PubMed] [Google Scholar]
- 25. Pepin MG, Schwarze U, Rice KM, Liu M, Leistritz D, Byers PH. Survival is affected by mutation type and molecular mechanism in vascular Ehlers-Danlos syndrome (EDS type IV). Genet Med 2014;16:881–888. [DOI] [PubMed] [Google Scholar]
- 26. Tarr I, Hesselson S, Iismaa SEet al. . Exploring the genetic architecture of spontaneous coronary artery dissection using whole-genome sequencing. Circ Genom Precis Med 2022;15:e003527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Franke KB, Nerlekar N, Marshall H, Psaltis PJ. Systematic review and meta-analysis of the clinical characteristics and outcomes of spontaneous coronary artery dissection. Int J Cardiol 2021;322:34–39. [DOI] [PubMed] [Google Scholar]
- 28. Alfonso F, García-Guimaraes M, Alvarado Tet al. . Clinical implications of arterial hypertension in patients with spontaneous coronary artery dissection. Coron Artery Dis 2022;33:75–80. [DOI] [PubMed] [Google Scholar]
- 29. Blazak PL, Holland DJ, Basso T, Martin J. Spontaneous coronary artery dissection, fibromuscular dysplasia, and biventricular stress cardiomyopathy: a case report. Eur Heart J Case Rep 2022;6:ytac125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Takeuchi M, Okada T, Ikegami Y, Nakamoto Y, Idei N, Ohashi N. A breastfeeding woman with spontaneous coronary artery dissection and possible Takotsubo syndrome: a case report. Medicine (Baltimore) 2021;100:e25775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Pretty HC. Dissecting aneurysm of coronary artery in a woman aged 42: rupture. Br Med J 1931;1:667. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
No new data were generated or analysed in support of this research.